Direct Injury to Right Coronary Artery in Patients Undergoing
advertisement

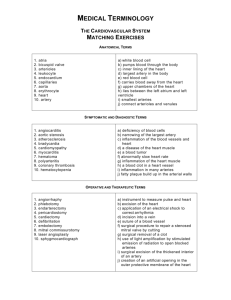
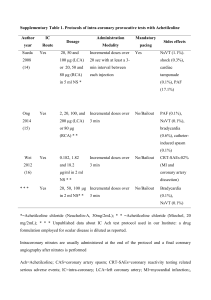
Direct Injury to Right Coronary Artery in Patients Undergoing Tricuspid Annuloplasty ADULT CARDIAC Pablo Díez-Villanueva, MD, Enrique Guti errez-Iba~ nes, MD, Gregorio P. Cuerpo-Caballero, MD, Ricardo Sanz-Ruiz, MD, Manuel Abeytua, MD, Javier Soriano, MD, Fernando Sarnago, MD, Jaime Elízaga, MD, PhD, Angel Gonz alez-Pinto, MD, PhD, and Francisco Fern andez-Avil es, MD, PhD n, Instituto de Investigación Sanitaria Gregorio Mara~ n, Department of Cardiology, Hospital General Universitario Gregorio Mara~ no no Universidad Complutense de Madrid; Departments of Cardiovascular Surgery and Anesthesiology, Hospital General Universitario n, Madrid, Spain Gregorio Mara~ no Background. Direct injury to the right coronary artery as a result of reparative operation on the tricuspid valve is a rare, probably underdiagnosed, but serious complication, which often involves dramatic clinical consequences. So far, only five cases have been described in the literature. Methods. We describe our single-center experience of this complication, and review and analyze relevant clinical and anatomic considerations related to this entity. Cases previously reported in the literature were also reviewed. Results. We describe four cases of direct injury to the right coronary artery in patients undergoing tricuspid annuloplasty (DeVega annuloplasty, 3; ring annuloplasty, 1) in our institution since 2005. All patients had right ventricular dilatation and severely dilated tricuspid annulus. Right coronary artery occlusion always occurred between the right marginal artery and the crux of the heart. Patients presented with hemodynamic or electrical instability. Coronary flow could be restored in 2 patients (percutaneously 1; surgically 1), both of whom finally survived, while it was not technically possible in the other 2 (1 died). Conclusions. Occlusion of the right coronary artery in patients undergoing tricuspid annuloplasty is a rare complication that may occur if great annulus dilatation is present, thus altering both normal annular geometry and the relationship between the right coronary artery and the tricuspid annulus, particularly when DeVega annuloplasty is performed. Such an entity should be considered in the immediate postoperative period in an unstable patient, especially when complementary tests support this diagnosis. Prompt recognition and treatment can positively affect the patient’s outcome, most often by means of an emergency revascularization strategy. S Both cardiogenic shock and electrical instability may complicate the course of patients undergoing reparative surgery of the tricuspid valve (TV). Direct injury to the right coronary artery (RCA) is a rare but serious complication, probably underdiagnosed, which often entails dramatic clinical consequences. We describe our single-center experience of this complication, and review the literature to analyze relevant clinical and anatomic considerations. econdary or functional tricuspid regurgitation (TR) is the most common type of TR, most often related to leftsided myocardial or valve heart disease, principally advanced mitral valve disease [1]. The TR is secondary to right ventricular (RV) enlargement and tricuspid annulus dilatation, causing impaired proper leaflet coaptation, which results in valve insufficiency [2, 3]. In case of moderate or severe TR or dilated annulus, tricuspid valve annuloplasty (TA) performed at the time of mitral valve surgery improves both TR and RV function and remodeling [4–6], and consequently prognosis in the short and long term [7–9]. The number of tricuspid interventions has greatly increased during the last several years, usually being performed in the context of other cardiac operations [10]. Surgical technique has greatly evolved during the last decades, with great acceptance of valve repair, which is the technique of choice [9, 11]. The two most widely used repair techniques are the DeVega pursestring repair (suture technique) and ring or band annuloplasty. (Ann Thorac Surg 2014;97:1300–5) Ó 2014 by The Society of Thoracic Surgeons Material and Methods We reviewed our experience in recent years (2005 through 2012) regarding direct injury to the RCA related to TV repair in patients with functional TR. Cases previously reported in the literature were also reviewed. Moreover, anatomic and pathophysiologic features that may be involved in this entity, as well as surgical considerations, are also considered and explained. Accepted for publication Dec 18, 2013. Results Address correspondence to Dr Díez-Villanueva, Department of Cardioln, C/ Doctor ogy, Hospital General Universitario Gregorio Mara~ no Esquerdo 46, 28007, Madrid, Spain; e-mail: pablo_diez_villanueva@ hotmail.com. Between 2005 and 2012, 499 patients underwent TV surgery in our institution; repair techniques were performed in 450 of them (320 ring annuloplasty, and 130 De Vega Ó 2014 by The Society of Thoracic Surgeons Published by Elsevier Inc 0003-4975/$36.00 http://dx.doi.org/10.1016/j.athoracsur.2013.12.021 Ann Thorac Surg 2014;97:1300–5 DíEZ-VILLANUEVA ET AL CORONARY ARTERY INJURY IN TRICUSPID SURGERY Case 1 A 78-year-old woman with rheumatic valve disease was referred for poor functional class (New York Heart Association III/IV). Her electrocardiogram showed atrial fibrillation. An echocardiogram demonstrated that she had a preserved left ventricular (LV) function, but a dilated RV with mild systolic dysfunction. Severe mitral and aortic stenoses were present, and she had severe TR and annulus dilatation (44 mm). Preoperative coronary arteriography showed calcified arteries, without significant lesions. She underwent mitral and aortic valve replacement with prosthetic mechanical valves (Carbomedics, CM; Sorin Group USA, Inc, Arvada, CO), 25-mm and 21-mm, respectively, and De Vega annuloplasty. Postoperatively, she was initially dependent on low doses of inotropic agents. A transesophageal echocardiogram described hypokinesia in the inferoposterior LV wall (LV ejection fraction, 0.50), poorer RV function than preoperatively assessed, and normal mitral and aortic valve prosthesis function. Significant hemodynamic impairment appeared a few hours later; thus intensive vasoactive drug support and counterpulsation balloon were needed. An electrocardiogram showed inferoposterior infarction, and urgent echocardiography showed severe biventricular dysfunction, with akinetic interventricular septum and inferior and inferoposterior ventricular walls. The patient was then transferred to the catheterization laboratory. Emergent coronary angiography showed the RCA had a subocclusive stenosis at the crux. It was not possible to cross the lesion with a percutaneous coronary intervention wire, thus percutaneous revascularization was not achieved. The patient finally died as a result of cardiogenic shock. Case 2 A 76-year-old woman with a history of rheumatic valve disease, LV dilatation, and poor functional class (New York Heart Association III/IV) was referred for surgery. Electrocardiogram showed atrial fibrillation. An echocardiogram demonstrated that she had mild LV dilatation, with normal function, a slightly dilated RV, and mild systolic dysfunction. Severe mitral and tricuspid regurgitation and a dilated tricuspid annulus (44 mm) were present. Preoperative coronary arteriography showed calcified arteries, without significant lesions. Surgical treatment consisted of mitral valve repair (annuloplasty and neochordae implantation) and De Vega annuloplasty. After unclamping the aorta, the electrocardiogram showed signs of inferior ST-segment elevation, which initially normalized with nitroglycerin. One hour after leaving the operating room, the patient exhibited severe hypotension and new electrocardiographic abnormalities, as well as several episodes of nonsustained ventricular tachycardia. Echocardiogram showed RV dysfunction and dilatation. Emergent coronary arteriography showed multiple obstructive lesions along the middle and distal segments of the RCA. A wire was placed in the artery, and a balloon was used to dilate the obstruction, but the procedure was unsuccessful as the artery became occluded time and time again, probably because of the plication caused by the suture. Hemodynamic stability could finally be achieved with a low dose of inotropic agents and a counterpulsation balloon, so the tricuspid annuloplasty was not undone. Posterior evolution was good. Follow-up echocardiograms showed recovery of RV function. Case 3 A 68-year-old woman was admitted for decompensated heart failure. She had a history of rheumatic valve disease. An electrocardiogram demonstrated that she was in atrial fibrillation. An echocardiogram showed normal LV function, a dilated RV with preserved function, severe Table 1. Cases From Our Seriesa Case Age (y), Sex (M/F) Tricuspid Annulus (mm) Surgery Diagnosis RCA Segment Injured 1 2 78, F 76, F 44 44 DeVega DeVega ECG þ TTE þ shock ECG þ shock Crux Mid 3 4 68, F 69, F 40 41 DeVega Ring ECG þ TEE þ arrhythmia ECG þ TEE þ shock Mid Distal Treatment Result Failed PCI Failed PCI, shock treatment CABG PCI Died Good Good Good a Right ventricular and right atrial enlargement is present in all cases, as is pulmonary hypertension. They are all women between 68 and 78 years old, with a history of rheumatic valve disease. CABG ¼ coronary artery bypass grafting (coronary angiography was performed before patient discharge); ECG ¼ electrocardiogram; percutaneous coronary intervention; TEE ¼ transesophageal echocardiography; TTE ¼ transthoracic echocardiography. PCI ¼ ADULT CARDIAC pursestring repair), and 49 underwent TV replacement. Direct injury to the RCA complicated 4 of those 450 repair operations, as described in the case reports. Severe tricuspid annulus dilatation and right atrial and RV enlargement were present in all patients of our series, as well as severe pulmonary hypertension. Furthermore, RCA occlusion occurred between the right marginal artery and the crux of the heart in all cases. Patient characteristics are summarized in Table 1 (postoperative coronary arteriograms are shown in Fig 1). 1301 1302 DíEZ-VILLANUEVA ET AL CORONARY ARTERY INJURY IN TRICUSPID SURGERY Ann Thorac Surg 2014;97:1300–5 Fig 1. Coronary angiograms of our 4 patients (cases 1 to 4), showing right coronary artery occlusion occurring between the right marginal artery and the crux of the heart in all cases. ADULT CARDIAC mitral valve stenosis and regurgitation, and severe TR, with a dilated annulus (40 mm). Preoperative coronary arteriography showed calcified arteries, without significant lesions. We performed mitral valve replacement with a 27-mm St. Jude mechanical prosthesis valve (St. Jude Medical, Inc, St. Paul, MN) and De Vega annuloplasty. During the postoperative course, while still in the operating room the patient experienced electrical instability (several episodes of ventricular fibrillation). An urgent echocardiogram showed biventricular dysfunction, and the electrocardiogram was compatible with inferior infarction. Because the diagnosis was established in the operating room, coronary artery bypass graft surgery (saphenous vein to RCA) was immediately performed. No complications occurred, although the patient had persisting mild RV dysfunction at discharge. Coronary angiography before discharge showed permeability of the graft; a significant RCA stenosis was observed in the mid segment, which was not present at baseline angiogram. Case 4 A 69-year-old woman with a history of rheumatic valve disease was admitted for worsening functional class. Her electrocardiogram indicated she was in sinus rhythm. An echocardiogram indicated preserved LV function, but she had a severely dilated RV with moderately depressed function, severe mitral valve stenosis and regurgitation, and a severe TR with a dilated annulus (41 mm). Preoperative coronary arteriography showed calcified arteries, without significant lesions. She underwent mitral valve replacement with a biologic prosthesis, the St. Jude Medical Epic heart valve (St. Jude Medical), 29-mm, and implantation of a 30-mm Physio annuloplasty tricuspid ring (Edwards Lifesciences, Irvine, CA). Severe biventricular dysfunction was evident after unclamping the aorta, but the hemodynamic situation improved with high doses of inotropic agents and initial stabilization was achieved. Later on, 2 hours after leaving the operating room, an electrocardiogram showed STsegment elevation in the inferior leads. Emergency coronary angiography showed critical stenosis in the distal RCA. Implantation of a bare metal stent achieved percutaneous revascularization. No further complications occurred after that. The patient exhibited mildly depressed LV function at discharge, with no other echocardiographic remarkable changes. Literature Review To date we found only five case reports in the literature describing direct injury to the RCA related to TR surgery [12–16]; one of them [15] is case 2 of our series, included in Table 1. The other four cases are summarized in Table 2 Ann Thorac Surg 2014;97:1300–5 DíEZ-VILLANUEVA ET AL CORONARY ARTERY INJURY IN TRICUSPID SURGERY 1303 Patient 1 2 3 4 a Age (y), Sex (M/F) Surgery Diagnosis – 64, F 38, M 83, M Ring DeVega Band Band ECG ECG þ TEE ECG þ TEE þ arrhythmia ECG þ TEE þ arrhythmia RCA Segment Injured Treatment Result Non specified Distal Distal Beyond right marginal artery None PCI CABG Failed PCI, shock treatment Died Good Good Good Right ventricular and annular dilatation is present in all cases. No more data were available from patient 1 [12]. Patient 2 was a 64-year-old woman referred for mitral insufficiency and recent onset of dyspnea. She had undergone mechanical aortic valve replacement because of acute endocarditis 14 years before [13]. Patient 3 was a 38-year-old man referred for symptomatic severe mitral regurgitation caused by bacterial endocarditis in a myxomatous mitral valve with significant tricuspid regurgitation and dilated annulus [14]. Patient 4 was an 83-year-old man with mitral valve prolapse in poor functional class [16]. CABG ¼ coronary artery bypass grafting (coronary angiography was performed before patient discharge); ECG ¼ electrocardiogram; percutaneous coronary intervention; TEE ¼ transesophageal echocardiography; TTE ¼ transthoracic echocardiography. (including a brief description of them in the footnote). Three of them underwent annuloplasty ring or band, and one underwent De Vega annuloplasty. Again, RV dilatation and tricuspid annulus dilatation were present in all cases, and RCA occlusion always occurred between the right marginal artery and the crux of the heart. Comment Circumflex artery injury related to mitral annuloplasty has been repeatedly reported [17], but injury to the RCA appears to be a rare complication of TA, often presenting as cardiogenic shock and electrical instability. So far, only five cases had been reported, one of them in our center [15]. From this standpoint, and considering this complication may be underdiagnosed, we reviewed the cases in which this entity complicated TA (cases reported to date in the literature and those discussed in this article). The relationship between the valve complex and surrounding structures is of great importance to optimize surgery outcomes, as detailed elsewhere [18, 19]. Regarding the relationship between the RCA and the TV, it is perceptive to remark on some anatomic considerations. First, the tricuspid annulus is not a consistent collagen structure, so the atrioventricular groove is said to directly fold into the TV leaflets at the vestibule, and the entire parietal attachment of the TV is usually encircled by the RCA running within the atrioventricular groove [20]. Second, the RCA has three well-defined portions (proximal RCA, before the origin of the marginal branch; mid RCA, the segment just beyond the marginal branch; and distal RCA, the segment halfway between the right marginal branch and the origin of the posterior descending artery); the segment delimited by the right marginal artery and the crux is the most closely related to the tricuspid annulus (Figs 2, 3). The distance between the RCA and the endocardium is particularly small in those areas closest to the tricuspid annulus, especially in the cavotricuspid isthmus in the lower right atrium, with a distance of less than 5 mm in over 80% of patients [21]. Deep suture placement for TA is not indicated given the low wall stress in the right atrium. Therefore, PCI ¼ placement of more superficial stitches, particularly in the “danger zone” (anteroposterior commissure) should greatly decrease the likelihood of injury. In our opinion, there are two likely mechanisms that can explain RCA injury: direct obstruction with the suture, which seems to be more plausible, and kinking of the artery as a result of changes in annular shape. Annulus dilatation may distort the normal RCA course, and severely atherosclerotic arteries (more calcified and rigid) could be more prone to kinking, thus leading to plaque fracture and subsequent obstruction. Dilated annuli, which in turn require more plication, probably have an increased risk of direct RCA injury during TA, especially when performing suture techniques (this complication has not been reported with tricuspid prosthesis because there is no need to purse string the tissue) taking into account the close relationship between the artery and the annulus, as explained before. Risk of RCA occlusion may be minimized by using semirigid rings, applying fewer sutures along the posterior annulus, and avoiding applying the stitches to the atrial wall. Fig 2. Relationship between the right coronary artery and tricuspid valve. The segment delimited by the right marginal artery and the crux is the most closely related to the tricuspid annulus (between the anteroposterior commissure and posterior leaflet). ADULT CARDIAC Table 2. Cases Previously Reported in Literaturea 1304 DíEZ-VILLANUEVA ET AL CORONARY ARTERY INJURY IN TRICUSPID SURGERY ADULT CARDIAC Fig 3. Relationship between the right coronary artery and tricuspid valve. The segment delimited by the right marginal artery and the crux is the most closely related to the tricuspid annulus (between the anteroposterior commissure and posterior leaflet). Patients may present hemodynamic or electrical instability (ventricular arrhythmias) as well as RV or biventricular dysfunction. Nevertheless, this entity is often diagnosed some hours after the patient leaves the operating room. This may be because RCA obstruction is usually incomplete, thus allowing for better hemodynamic tolerance and delayed diagnosis. In case of complete occlusion, diagnosis may be achieved earlier (greater hemodynamic or electrical instability, or earlier and more evident electrocardiogram alterations), even in the operating room itself, as in case 3. Differential diagnosis with RCA occlusion in TA should include other causes of RV dysfunction, such as LV dysfunction, volume overload, pulmonary hypertension, or myocardial stunning caused by extracorporeal circulation, each requiring specific treatment [22]. Also, air emboli [23], considering the origin of the RCA (anterior and cranial), may be present after releasing the aortic crossclamp. Onset of ventricular dysfunction in this case is very early and usually transient, as are electrocardiographic findings. In case of direct RCA injury by the suture, RV dysfunction, characteristically persistent, may sometimes be evident only hours after the surgery, and no apparent ST-segment changes are often noted initially, which may delay the diagnosis. Electrical instability (ventricular arrhythmia) is not uncommon in the early postoperative period, and is usually attributed to electrolyte disturbances, ischemia, or ventricular dysfunction. Ischemia may be related to anemia, bleeding, poor blood oxygenation, or heart failure, but also can occur with preexisting coronary artery disease. Interestingly, obstructive coronary disease is not present in any of the patients of our series, nor in any of the cases previously reported. This is why RCA occlusion should be considered in the early postoperative period of patients undergoing TA, with or without preexisting coronary disease. Significantly, ventricular pacing may also complicate the diagnosis of any coronary occlusion as ST-segment changes may not be evident. Ann Thorac Surg 2014;97:1300–5 Urgent revascularization of an occluded coronary artery through percutaneous coronary intervention or coronary artery bypass graft surgery is crucial in cardiogenic shock occurring in the context of a myocardial infarction, as restoring normal blood flow greatly improves the prognosis of these patients [24, 25]. Considering all the cases, those from our series and those previously reported, revascularization was not achieved in 4 patients (50%), 2 of whom died (50%). On the other hand, all those patients who underwent revascularization survived. Nonetheless, revascularization in this subset of patients has proved challenging, with a relatively high rate of failure owing to the impossibility of inserting a wire into the artery beyond the surgical stenosis, or failure of the balloon to achieve a lasting and sufficient dilatation of the stenosis. However, in other cases it was possible to stent or bypass the artery, with excellent clinical results. The first cases in our institution increased awareness of this problem, and we established a diagnostic and therapeutic algorithm, shown in Figure 4. Thus, in case of hemodynamic or electrical instability with RV or biventricular dysfunction in the postoperative period owing to persistent ischemia, and after excluding other possible etiologies (previously described), RCA injury should be suspected. If complementary tests (ST-segment changes in electrocardiogram, and abnormal wall motion in echocardiography) support this diagnosis, flow should be restored. Consequently, if such diagnosis is achieved in the operating room (in major obstructions, diagnosis is often achieved earlier), the surgeon can remove the sutures or the ring, thus resolving the occlusion, or perform empiric RCA bypass. In this case, coronary angiography should be performed before discharge to evaluate coronary flow. On the other hand, if diagnosis is done in the postoperative period after leaving the operating room, the Fig 4. Proposed diagnostic and therapeutic algorithm in case of right coronary artery (RCA) injury in tricuspid annuloplasty (TA). * Other causes of instability: prior RV or LV dysfunction, volume overload, pulmonary hypertension, myocardial stunning caused by extracorporeal circulation, air emboli and electrolyte disturbances. DíEZ-VILLANUEVA ET AL CORONARY ARTERY INJURY IN TRICUSPID SURGERY patient should be immediately transferred to the catheterization laboratory to assess and reestablish coronary flow percutaneously. If the percutaneous approach fails, coronary artery bypass graft must be performed. In conclusion, direct injury or occlusion of the RCA by a suture in patients undergoing TA is an infrequent complication, although probably underdiagnosed. Therefore, a high index of suspicion is essential in the postoperative period, and urgent assessment of the coronary circulation is mandatory in every patient with hemodynamic or electrical instability in whom complementary tests (mainly electrocardiogram and echocardiogram) support this possibility. This entity should be especially considered in case of great annulus dilatation and calcified arteries. Revascularization is the treatment of choice, particularly in patients in cardiogenic shock. In some cases it can be performed percutaneously at the time of diagnosis; a surgical approach appears as a valid alternative if a percutaneous approach fails or the diagnosis is made while still in the operating room. commissure, or leaflet procedure? J Thorac Cardiovasc Surg 2010;139:1473–82.e5. The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012;33:2451–96. Vassileva C, Shabosky J, Boley T, Markwell S, Hazelrigg S. Tricuspid valve surgery: the past 10 years from the Nationwide Inpatient Sample (NIS) database. J Thorac Cardiovasc Surg 2012;143:1043–9. Irwin RB, Luckie M, Khattar RS. Tricuspid regurgitation: contemporary management of a neglected valvular lesion. Postgrad Med J 2010;86:648–55. Rubens FD, Bedard P, Walley VM. Right coronary artery injury during tricuspid valve annuloplasty. J Cardiovasc Surg (Torino) 1990;31:533–5. Symersky P, de Jong AP, Koch KT, de Beaumont EM, de Mol BA. Purse-string deformity of the right coronary artery: a pitfall in de Vega tricuspid annuloplasty. J Thorac Cardiovasc Surg 2007;133:1086–7. Calafiore AM, Iac o AL, Bartoloni G, Di Mauro M. Right coronary occlusion during tricuspid band annuloplasty. J Thorac Cardiovasc Surg 2009;138:1443–4. Cuerpo GP, Stuart JR, Ruiz M, Pinto AG. Right coronary artery injury as a complication of de Vega tricuspid annuloplasty. Rev Esp Cardiol 2009;62:1501–3. Varghese R, Akujuo A, Adams DH. Right coronary artery injury after tricuspid valve repair. Semin Thorac Cardiovasc Surg 2010;22:189–90. Wykrzykowska J, Cohen D, Zimetabum P. Mitral annuloplasty causing left circumflex injury and infarction: novel use of intravascular ultrasound to diagnose suture injury. J Invasive Cardiol 2006;18:505–8. Rogers JH, Bolling SF. Valve repair for functional tricuspid valve regurgitation: anatomical and surgical considerations. Semin Thorac Cardiovasc Surg 2010;22:84–9. McCarthy PM. Tricuspid valve repair technique. Oper Tech Thorac Cardiovasc Surg 2011;16:97–111. Mill MR, Wilcox BR, Anderson RH. Surgical anatomy of the heart. In: Cohn LH, Jr Edmunds LH, eds. Cardiac surgery in the adult, 2nd ed. New York, NY: McGraw-Hill; 2003:31–52. Al Aloul B, Sigurdsson G, Can I, Li J, Dykoski R, Tholakanahalli M. Proximity of right coronary artery to cavotricuspid isthmus as determined by computed tomography. Pacing Clin Electrophysiol 2010;33:1319–23. Mandarino WA, Winowich S, Gorcsan J 3rd, et al. Right ventricular performance and left ventricular assist device filling. Ann Thorac Surg 1997;63:1044–9. Koul BL, Al-Rashidi F, Roijer A, Meurling C. A new technique to reduce residual air emboli in open left cardiac surgery. J Thorac Cardiovasc Surg 2009;138:1438–9. Hochman JS, Sleeper LA, White HD, et al; SHOCK Investigators, Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock. One-year survival following early revascularization for cardiogenic shock. JAMA 2001;285:190–2. Hochman JS, Sleeper LA, Webb JG, et al; SHOCK Investigators. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA 2006;295:2511–5. We thank Dr Carlos E. Ruiz for his advice and Fernando Díez Villanueva for the illustrations. 9. 10. 11. 12. 13. 14. 15. 16. 17. References 1. Otto CM, Bonow RO. Valvular heart disease. In: Bonow RO, Mann DL, Zipes DP, Libby P, eds. Braunwald’s heart disease: a textbook of cardiovascular medicine, 9th ed. Philadelphia, PA: Elsevier Saunders; 2012:1468–538. 2. Waller BF, Howard J, Fess S. Pathology of tricuspid valve stenosis and pure tricuspid regurgitation—part III. Clin Cardiol 1995;18:225–30. 3. Shiran A, Sagie A. Tricuspid regurgitation in mitral valve disease: incidence, prognostic implications, mechanism, and management. J Am Coll Cardiol 2009;53:401–8. 4. Colombo T, Russo C, Ciliberto GR, et al. Tricuspid regurgitation secondary to mitral valve disease: tricuspid annulus function as guide to tricuspid valve repair. Cardiovasc Surg 2001;9: 369–77. 5. Dreyfus GD, Corbi PJ, Chan KM, Bahrami T. Secondary tricuspid regurgitation or dilatation: which should be the criteria for surgical repair? Ann Thorac Surg 2005;79:127–32. 6. Desai RR, Vargas Abello LM, Klein AL, et al. Tricuspid regurgitation and right ventricular function after mitral valve surgery with or without concomitant tricuspid valve procedure. J Thorac Cardiovasc Surg 2013;146:1126–32.e10. 7. Tang GH, David TE, Singh SK, Maganti MD, Armstrong S, Borger MA. Tricuspid valve repair with an annuloplasty ring results in improved long-term outcomes. Circulation 2006;114(1 Suppl):I577–81. 8. Navia JL, Nowicki ER, Blackstone EH, et al. Surgical management of secondary tricuspid valve regurgitation: annulus, 18. 19. 20. 21. 22. 23. 24. 25. ADULT CARDIAC 1305 Ann Thorac Surg 2014;97:1300–5