interChange Provider Message: Hospital Billing/APC – updated
advertisement

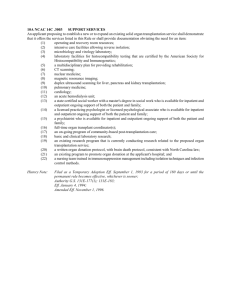
interChange Provider Important Message Hospital interChange Updated as of 12/09/2015 *all red text is new for 12/09/2015 Ambulatory Payment Classification (APC) Scheduled for March 1, 2016 DSS will move from the current system of hospital outpatient payment methodology based on Revenue Center Codes (some paid based on fixed fees, some based on a ratio of costs to charges) to a prospective payment system based on the complexity of services performed. This change is scheduled for March 1, 2016. Hospitals can refer to the Hospital Modernization Web page on the www.ctdssmap.com Web site for information pertaining to the APC implementation. Please send all APC related questions to Hewlett Packard Enterprise at the following e-mail address: ctxixhosppay@hpe.com. The following document was recently added to the Hospital Modernization Web page: • APC FAQs added 10/14/2015 Outpatient Hospital APC Workshop The topics include: • Provider Bulletin • Payment Methodology • Addendum B • Three (3) Day Rule • Hospital Billing Changes • Hospital Modernization Web Page • Upcoming Changes and Training • FAQs Connecticut Hospital Association, 110 Barnes Road, Wallingford, CT Friday December 11, 2015 1:00 PM – 4:00 PM Hospital Based Practitioners Workshop The topics include: • Provider Bulletin • Enrolling a Physician Group • Re-enrollment of Hospital Based Practitioners • Professional Billing • Physician Fee Schedule • Remittance Advice • Upcoming Changes and Training • FAQs Internet Virtual Classroom Training Wednesday January 6, 2016 1:00 PM – 4:00PM Internet Virtual Classroom Training Tuesday January 12, 2016 9:00 AM – 12:00PM interChange Provider Important Message To register for these workshops, visit the www.ctdssmap.com Web site and go to the Hospital Modernization Web page and click on Outpatient Hospital APC December or Hospital Based Practitioners Workshop under Important Messages – Connecticut Hospital Modernization. To register, click on the registration link for either the Virtual classroom or face to face workshop at CHA. Provider Bulletin 2015-91 - Update to Revenue Center Codes (RCC) Requiring a Valid CPT or HCPCS on Outpatient Claims and a Change in Prior Authorization Requirements for certain RCCs The Department of Social Services (DSS) is adding the requirement of a valid CPT/HCPCS when the following RCCs are billed: 273 – 274, 277, 470-472 and 479. All claim details with these RCCs that are not billed with a valid CPT/HCPCS code will deny for Explanation of Benefit (EOB) code 390 “Revenue Center Code Requires a HCPCS/Procedure Code.” This change is effective for dates of service January 1, 2016 and forward on outpatient claims. In addition, effective for dates of service January 1, 2016 and forward, hospitals will no longer need to obtain prior authorization for RCCs 470, 471, 472 and 479. Provider Bulletin 2015-82 - Three (3) Day Rule: Outpatient Stay Prior to Inpatient Admission The purpose of this provider bulletin is to inform providers that the Department of Social Services (DSS) will be implementing new Explanation of Benefit (EOB) codes in the Connecticut Medical Assistance Program (CMAP) to enforce restrictions on outpatient claims when the date of service is within 3 days (2 days plus the admission date) prior to an inpatient admission. For admissions on or after November 1, 2015, all diagnostic and non-diagnostic outpatient services, (including psychiatric diagnostic services) other than maintenance renal dialysis, physical therapy, occupational therapy, speech therapy and audiology, provided by the hospital or an entity wholly owned or wholly operated by the hospital 3 days (2 days plus the admission date) prior to the inpatient claim, will post and pay with EOB code 5077 “Inpatient stay denied due to a paid outpatient claim within 3 days prior to inpatient admission” or EOB code 5078 “Outpatient claim denied due to a paid inpatient claim within 3 days after an outpatient claim.” If the hospital is able to attest that the outpatient claim is unrelated to the inpatient hospital claim and are clinically distinct and independent from the reason for admission, the hospitals should bill with Condition Code 51 “Attestation of Unrelated Outpatient Non-diagnostic Services” on their outpatient claim. The post and pay status therefore enables hospitals to identify claims that will start denying for admissions on or after March 1, 2016 if the outpatient claim is billed separately and not billed with the inpatient stay. The informational EOB codes will post to the hospital’s Remittance Advice (RA). Claims Reprocessing Hewlett Packard Enterprise previously identified an issue where outpatient claims with Revenue Center Codes (RCCs) requiring Prior Authorization (PA) processed without a PA on file. Hewlett Packard Enterprise resolved this issue on October 2, 2015 and claims submitted April 1, 2015 to October 5, 2015 were identified and re-processed. The RCCs that require PA will now deny with Explanation of Benefit (EOB) code 3003 “Prior Authorization is Required for Payment of this Service” if there wasn’t a PA on file. These claims appeared on the November 10, 2015 Remittance Advice (RA) with an Internal Control Number (ICN) beginning with region code 52. interChange Provider Important Message Updates to 835 Electronic Remittance Advice (ERA) In a response to a previous request from the hospitals the following update will be made to future 835 ERAs starting with the January 13, 2016 835 ERA. • EOB code 3003 utilizing CARC 204 “This service/equipment/drug is not covered under the patient’s current benefit plan” and Remittance Advice Remark Codes (RARC) N130 “Consult plan benefit documents/guidelines for information about restrictions for this service” will change to CARC 197 “Payment denied/reduced for absence of precertification/authorization and will not have an RARC.” • EOB code 1033 utilizing CARC 16 “Claim/Services lacks information” and RARC N285 “Missing/incomplete/invalid referring provider name” will change to CARC B7 “This provider was not certified/eligible to be paid for this procedure/service on this date of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present” and RARC N570 “Missing/incomplete/invalid credentialing data.” Hospitals are asked to update their auto post systems accordingly. ICD-10 Code sets With the transition to ICD-10 code sets in the Connecticut Medical Assistance Program (CMAP), the Department of Social Services (DSS) has implemented certain new EOB codes effective for dates of service 10/1/2015 forward. Providers can refer to Provider Bulletin 2015-47 for a complete list of these EOB codes. One of the EOB codes is 4039 - The primary diagnosis code is not covered. This EOB code is currently set to a “Post and Pay” status. Providers will see EOB code 4039 on their Remittance Advice (RA) for those claims where they use a primary diagnosis code that has been classified as an unacceptable principal diagnosis code per coding guidelines. Providers should utilize this “Post and Pay” period to determine the correct primary diagnosis code for the conditions they treat. Please refer to coding resources for assistance. The Provider Assistance Center will not be able to assist with coding questions. Office Closure Please be advised, the Department of Social Services (DSS) and Hewlett Packard Enterprise will be closed on Friday, December 25, 2015 in observance of the Christmas holiday and will also be closed on Friday, January 1, 2016 in observance of the New Year’s holiday. Outstanding Questions Inpatient Admissions Following Outpatient or Emergency Department Services Inpatient claims are denying with EOB codes 0671 “DRG Covered/Non-covered Days Disagree with the Statement Period” and 0672 “DRG Accommodation Days Inconsistent with the Header Date Period” for inpatient admissions following outpatient or emergency department services. Also some claims are denying with EOB code 529 “Surgical Procedure Date is Prior to Admission Date.” • Claims examples and questions were sent to the Department for review. DSS stated they are still reviewing as of 12/08/2015. Billing for Emergency Department Professional Services Prior to an Admission interChange Provider Important Message In cases where the client is outpatient or emergency room prior to an admission, the hospitals are requesting to be able to bill for professional fees separately on a CMS-1500. Effective for admission on or after January 1, 2015, hospitals can no longer bill for their inpatient professional fees (RCC 98X) on an inpatient claim and need to bill them on a CMS-1500. • Initial feedback from the DSS, based on Provider Bulletin 2014-88 “Billing for Emergency Department Services”, these policies and procedures will not be modified until the Department modernizes its outpatient hospital reimbursement methodology using Ambulatory Payment Classifications pursuant to section 17b-239(d)(2) of the Connecticut General Statutes. That change is scheduled for implementation on March 1, 2016. Question sent back to the Department for review. DSS stated they are still reviewing as of 12/07/2015. Medicare HMO lab crossover claims not considering the Medicare HMO co-pay. • The Department has agreed that these claims should consider the co-pay amount and is working on updates to the system to allow claims to be considered for payment. Transgender gender clients and the eligibility process. The hospital was asking who they can contact to provide updates to the client’s eligibility in these cases and if they can bill with condition code 45 “Ambiguous Gender Category” to override claims that deny due to gender not matching. • DSS states hospitals can contact the DSS benefits center, but any eligibility updates could require the client to provide this informational change. • System updates will occur in the future to allow condition code 45 to override claims and the hospital important message will be updated when the system is updated. Billing RCC 403 - Screening Mammography. The hospital is billing for RCC 403 twice with procedure code 77052 and G0202. RCC 403 only allows up to the bill amount on the first line (if less than the fixed fee) and denies the second line as a duplicate. In most cases not allowing up to the fixed fee of $117.91. • Hewlett Packard Enterprise requested a change to RCC 403 to allow up to the fixed fee of $117.91 and DSS has approved to price at 1 per day. On November 12, 2015 the system was updated to allow up to the fixed fee. Hospitals can begin to adjust their claims to allow up to the fixed fee of $117.91 or wait for the impacted claims with dates of service April 1, 2015 and forward to be identified and reprocessed in a future claim cycle which is tentatively scheduled for the 1st cycle in January 2016. Inpatient delivery stays denying due to lack of prior authorization when the delivery stays do not require prior authorization. Hewlett Packard Enterprise process for delivery stays is based on the primary diagnosis to determine if the primary reason for the stay was a delivery and then overrides the requirements for prior authorization. The hospital’s question and claim examples were submitted to DSS on November 5, 2015 and are awaiting a reply or decision by DSS to determine if there is an issue or if prior authorization is required based on the diagnosis billed. DSS stated they are still reviewing this as of 12/01/2015. interChange Provider Important Message Primary Insurance denying claim due to not receiving information (TPL survey) from client, then billing to Medicaid. • In cases where the primary insurance to Medicaid is denying the claim due to not receiving information from the client the hospital should use the Legal Notice of Subrogation Form (W-81) when initially pursuing commercial health insurance. This puts the insurance company on legal notice that it must make any payment for which it is liable for directly to the provider. • If the hospital does not receive payment within forty-five days, they should fully document that every reasonable attempt was made. The provider must file a request for assistance with the Connecticut Department of Insurance using form W82, Request for Assistance in Obtaining Payments. Department of Insurance will furnish the hospital with a file/case number. • DSS is aware that other insurance carriers never cover some services. In addition, there are some insurance companies that do not provide an actual denial statement or, in some cases, never respond to written requests. To address these problems and to alleviate any unnecessary burden on the provider, DSS implemented the Third Party Billing Attempt, (W-1417). This form documents that the hospital has made every attempt to obtain payment from the other insurance carrier prior to claim submission to the Connecticut Medical Assistance Program. The form may be used in place of a denial voucher for the other insurance carrier, but may not be used in place of a Medicare denial. If the provider has not received any insurance payment within ninety days of the date of the initial claims submission, then the provider may bill the Connecticut Medical Assistance Program. The Department of Insurance file number is required on the W-1417 form. Failure to include the Department of Insurance file number will result in the claim being returned to the provider. These instructions can be found under Provider Manual Chapter 5 “Claim Submission Information” on the www.ctdssmap.com Web site under the hospital modernization page, by clicking on Provider Manuals on the right side of the page. The forms can be downloaded from the www.ctdssmap.com Web site, under Information and then Publications and scrolling down to Third Party Liability Forms. Third party Liability (TPL) HMS Audits The hospitals are questioning the audit process that is taking a lot of time due to high volume of claims selected by this audit. Most of the claims that are selected have a deductible and the other insurance pays zero. The hospitals are questioning why they are asking for primary voucher when the claim clearly states there is a deductible amount owed. If they don’t provide that information in a specific amount of time the claims are voided and the money is re-couped. DSS stated they are still reviewing as of 11/25/2015. Billing the same RCC code on multiple details with different National Drug Codes (NDCs) but with the same HealthCare Common Procedure Coding System (HCPCS) code. • If you need to bill multiple NDCs under the same RCC with the same HCPCS codes, you will need to lump the total charges under the first NDC code and then enter zero charge in the additional RCC line with the NDC codes. Refer to Example below. interChange Provider Important Message • Please refer to provider bulletin 2008-35 “National Drug Codes (NDC) Required for Outpatient Hospital Claims due to the Implementation of the Federal Deficit Reduction Act (DRA) of 2005” or provider bulletin 2008-42 “Most Frequently Asked Questions related to the billing requirements necessary to support and comply with the implementation of the Deficit Reduction Act (DRA) of 2005” for complete instructions on claim submission requirements for submitting National Drug Codes (NDC) required for outpatient hospital claims. Example DOS RCC Units NDC Code 00264196510 63323030201 Procedure Code J3490 J3490 Billed Amt. $750 $500 9/1/2015 9/1/2015 250 250 1 1 9/1/2015 9/1/2015 250 250 2 1 00264196510 63323030201 J3490 J3490 $1250 $0 Change to