Segmental disorders of the nephron
advertisement

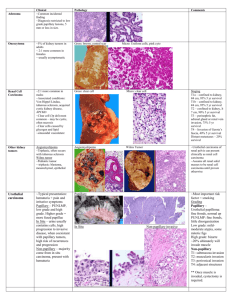
Published online before print July 9, 2007 The British Institute of Radiology, doi: 10.1259/bjr/20129205 The British Journal of Radiology REVIEW ARTICLE Segmental disorders of the nephron: histopathological and imaging perspective 1 S R PRASAD, MD, 2V R NARRA, MD, 1R SHAH, MD, 3P A HUMPHREY, J R CATENA, MD, 1N C DALRYMPLE, MD and 2C L SIEGEL, MD MD, PhD, 4 J JAGIRDAR, MD, 1 1 Department of Radiology, University of Texas Health Science Center @ San Antonio, San Antonio, TX, 2Department of Radiology, Mallinckrodt Institute of Radiology, St Louis, MO, 3Department of Pathology, Washington University in St Louis, St Louis, MO, and 4Department of Pathology, University of Texas Health Science Center @ San Antonio, San Antonio, TX, USA ; ABSTRACT. Recent advances in molecular genetics and immunocytochemistry have clarified the cell of origin in many renal disorders. Several renal disorders are thought to involve specific segments of the nephron. Renin-secreting tumours arise from juxtaglomerular cells. Clear cell and papillary renal cell carcinoma (RCC) recapitulate the epithelium of the proximal tubules [1]. Oncocytoma and chromophobe RCC differentiate towards Type A and Type B intercalated cells of the cortical collecting duct, respectively [1]. Medullary collecting ducts are the target sites for the development of autosomal recessive polycystic kidney disease, collecting duct carcinoma and medullary carcinoma [2, 3]. Renal papillae are susceptible to unique changes such as necrosis or papillitis. The segmental disorders of the nephrons are summarized in a table and depicted in a figure (Table 1, Figure 1). The purpose of our article is threefold: to illustrate the imaging findings of renal disorders that show segmental involvement of the nephron, to describe proximal and distal nephron disorders and to correlate imaging findings of some entities with histopathological features. Introduction The nephron is the structural and functional unit of the kidney. There are approximately 1.3 million nephrons in each kidney [4]. There are two types of nephrons based on their location within the kidney. The cortical nephrons comprise 85% of nephrons and contain glomeruli located in the cortex with short loops of Henle. The juxtamedullary nephrons (15% of nephrons) have glomeruli in the juxtamedullary regions of the cortex and long loops of Henle [4]. The anatomical parts of the nephron include the glomerulus, the juxtaglomerular apparatus, the proximal convoluted tubule (PCT), the loop of Henle and the distal convoluted tubule (DCT). The collecting duct is the conduit of formed urine into the pelvicalyceal system. Embryologically, the nephrons are derived from the nephrogenic blastema, and the collecting ducts develop from the ureteric bud. Background functional histology of the juxtaglomerular apparatus The glomerulus serves as a size- and charge-dependant barrier to filtration of proteins and large molecules Address correspondence to: Dr Srinivasa Prasad, MD, Abdominal Radiology, UTHSCSA, 7703 Floyd Curl Drive, San Antonio, TX 78229, USA. E-mail: prasads@uthscsa.edu Recipient of Silver Medal at the 2005 ARRS meeting (Ref: E 247). The British Journal of Radiology, Month 2007 Received 22 September 2006 Revised 9 January 2007 Accepted 15 January 2007 DOI: 10.1259/bjr/20129205 ’ 2007 The British Institute of Radiology [4]. Each glomerulus consists of an anastomosing network of capillaries that invaginates the dilated, proximal blind end of the nephron, the Bowman’s capsule. Juxtaglomerular (JG) cells are specialized smooth muscle cells in the wall of the afferent arteriole that maintain blood pressure homeostasis. The specialized tubular (DCT) cells of the macula densa act as chemoreceptors to detect sodium concentration and influence renin secretion by the JG cells [4]. Nephronal disorders isolated to the juxtaglomerular apparatus Juxtaglomerular cell tumours (‘‘reninomas’’) Juxtaglomerular cell tumours (JGCTs) are extremely rare benign renal neoplasms. The cell of origin of JGCTs is the modified smooth muscle cell termed the ‘‘myoendocrine cell’’ that shows actin and CD34 immunoreactivity [5]. Since the first description of JGCT by Robertson et al in 1967 [6], less than 100 cases have been reported. JGCTs commonly affect young people; peak age of incidence is in the second and third decades. JGCTs are twice as common in women as in men. Patients usually present with severe hypertension, hyperaldosteronism and hypokalaemia [7]. On gross pathology, JGCT appears as a well-circumscribed, yellow-tan, solitary solid tumour [8]. Haemorrhage is typically seen at the cut surface, and necrosis is notably 1 of 10 S R Prasad, V R Narra, R Shah et al Table 1. Overview of the segmental pathology of the nephron Pathology Segment of the nephron implicated Juxtaglomerular cell tumour Clear cell renal cell carcinoma (RCC) Papillary RCC Proximal renal tubular acidosis Mucinous tubular and spindle cell carcinoma Autosomal recessive polycystic kidney disease Medullary sponge kidney Chromophobe RCC Oncocytoma Collecting duct carcinoma Medullary carcinoma Papillary necrosis Autosomal dominant polycystic kidney disease Juxtaglomerular cell (glomerulus) Proximal convoluted tubule Proximal convoluted tubule Proximal convoluted tubule Loop of Henle? Collecting duct Ducts of Bellini Cortical collecting duct; Type B intercalated cell Cortical collecting duct, Type A intercalated cell Medullary collecting duct, principal cell Medullary collecting duct Medullary loop of Henle and medullary collecting duct All segments of the nephron absent. On histological examination, JGCT is composed of sheets of polygonal or spindle-shaped cells. Both thinwalled and the characteristic thick-walled hyalinized blood vessels are frequently found [5]. The presence of rhomboid crystalline forms of protorenin in a renal neoplasm is considered diagnostic of JGCT [5]. JGCTs appear as expansile, homogeneous, solid renal cortical neoplasms that typically measure 2–4 cm in diameter (Figure 2). Although JGCTs are richly perfused, the tumour vessels may show marked luminal narrowing secondary to intimal hyperplasia, possibly due to renin effect [9]. Thus, JGCTs typically appear hypovascular at angiography and contrast-enhanced CT and MRI (10). JGCTs may show delayed contrast enhancement on CT scans [9]. However, imaging findings of JGCTs are indistinguishable from other renal neoplasms on imaging studies. Background functional histology of the proximal convoluted tubule The proximal convoluted tubule (PCT) is a coiled tube that is approximately 15 mm long and 55 mm in diameter [4]. PCT is lined by a simple cuboidal epithelium with a prominent brush border containing numerous tall microvilli [11]. The PCT reabsorbs approximately 65% of the glomerular filtrate via the microvilli [4, 11]. Almost 100% of the filtered glucose and amino acids as well as 60% of the filtered sodium ions are reabsorbed in the PCT [4]. Small proteins, some peptide hormones and bicarbonates are reabsorbed in the PCT as well. Nephronal disorders localized to the proximal convoluted tubule Clear cell renal cell carcinoma (conventional renal cell carcinoma) Clear cell renal cell carcinoma (RCC) is the most common sporadic form of RCC, comprising approximately 70% of RCCs. Clear cell RCC recapitulates the epithelium of the PCTs [1]. Clear cell RCC is seen in patients with von Hippel–Lindau (VHL) disease [12]. It is interesting to note that inactivation of tumour suppressor Figure 1. Schematic diagram representing segmental localization of various renal disorders within the nephron. Different components of the nephrons including the glomerulus, proximal convoluted tubule (blue), distal convoluted tubule (green) and collecting duct (yellow) and their associated conditions are demonstrated (courtesy of Robert Chandler, MD, UTHSCSA, San Antonio, TX). 2 of 10 Figure 2. Juxtaglomerular cell tumour of the kidney. Delayed phase, contrast-enhanced CT scan shows an expansile, relatively homogeneous, hypoattenuating mass in the right kidney (arrows). The British Journal of Radiology Segmental disorders of the nephron when compared with other histological subtypes such as papillary and chromophobe RCCs [8, 17]. Papillary renal cell carcinoma (chromophil renal cell carcinoma) Papillary RCC is the second most frequent RCC subtype accounting for approximately 10–15% of RCCs. The neoplastic cells are reminiscent of the PCT epithelium [1]. Papillary RCC is commonly bilateral and tends to occur more frequently in patients with end-stage renal disease [18]. Papillary RCC appears as a well-circumscribed solid mass. It is histologically characterized by a tubular or papillary growth pattern. Delahunt et al [19] classified papillary RCC into Type 1 and Type 2 based on histology and biological behaviour; Type 2 tumours portend a poorer prognosis than Type 1 tumours. Papillary RCC commonly appears hyperechoic on ultrasound. In contradistinction to most clear cell RCC, papillary RCC typically appear homogeneous and hypovascular, showing a lesser degree of contrast enhancement on dynamic CT and MRI [20, 21] (Figure 4a,b). The presence of byproducts of haemorrhage and necrosis presumably result in low signal intensity of papillary RCC on T2 weighted MRI [22]. Papillary RCC shows a better prognosis than clear cell RCC [17]. It is interesting to note that, despite a common putative origin from the PCT, clear cell RCC and papillary RCC demonstrate different histology, clinicobiological behaviour, imaging findings and prognosis, possibly because of the involvement of distinct oncological pathways [14]. Figure 3. Clear cell renal cell carcinoma. Contrast-enhanced CT scan during corticomedullary phase shows a heterogeneous, hypervascular right renal mass (arrows) with areas of necrosis and haemorrhage (arrowhead). genes such as VHL and fragile histidine triad (FHIT) genes located on chromosome 3 are seen in up to 96% of sporadic clear cell RCCs [13]. Clear cell RCC classically appears golden yellow on gross pathology owing to the presence of abundant intracellular lipid. Histopathologically, clear cell RCC is characterized by glycogen- and lipid-rich clear cells and sinusoidal morphology of thin-walled blood vessels [8]. VHL gene inactivation leading to activation of the hypoxic response (including synthesis of vascular growth factors) is seen in approximately 60–75% of sporadic clear cell RCCs [14]. A majority of clear cell RCCs thus show hypervascularity on catheter angiography and contrast-enhanced CT/MRI [15] (Figure 3). Based on the degree of contrast enhancement of RCCs on helical CT scans (more than 84 Hounsfield units (HU) in the corticomedullary phase and 44 HU in the excretory phase), Kim et al [15] diagnosed clear cell RCC with a specificity of 100% and 91%, respectively. The presence of intracellular fat, a common finding in clear cell RCC, may be documented on opposed phase MRI [16]. Cysts, necrosis, haemorrhage and foci of calcification are frequently seen and contribute to tumour heterogeneity (Figure 4). Calcification is seen in 10–15% of neoplasms. Clear cell RCC exhibits poor prognosis (stage-for-stage) The British Journal of Radiology, Month 2007 Background functional histology of the loop of Henle The thin limbs of the loop of Henle are lined by a simple squamous epithelium; the thick ascending limb is lined by low cuboidal epithelium. The loop of Henle plays a major role in maintaining an osmotic gradient between the cortex and the medulla via the countercurrent multiplier mechanism [4]. Free, passive diffusion of water occurs in the thin limb, while active transport occurs through the cuboidal epithelium of the thick limb. The vasa recta reabsorb the interstitial water enhancing the medullary gradient. Nephronal disorder that may be linked to the loop of Henle Mucinous tubular and spindle cell carcinoma Mucinous tubular and spindle cell carcinoma (MTSCC) is a low-grade polymorphic epithelial carcinoma associated with non-aggressive behaviour and a favourable prognosis [8, 23]. Although the precise histogenesis of the neoplasm is still not established, MTSCC may differentiate towards the loop of Henle [24]. MTSCC was recently recognized as a subtype of RCC. Macroscopically, MTSCC appears as well-circumscribed tumours with uniform, grey or light tan colour [8]. 3 of 10 S R Prasad, V R Narra, R Shah et al Figure 4. (a) Papillary renal cell carcinoma. Contrast-enhanced CT scan during the corticomedullary phase shows a left renal hypoattenuating solid mass (arrow) with foci of calcification (arrowhead). (b) Papillary renal cell carcinoma. Coronal gadoliniumenhanced T1 weighted GRE MRI shows a uniform, hypovascular solid mass (arrow) in the upper pole of the left kidney. Histologically, MTSCC consists of tightly packed, elongated tubules separated by pale mucinous stroma [8]. The spindle cells are characteristic; chronic inflammation, foam cell deposits and areas of necrosis are seen in some cases. MTSCC was previously mistaken for sarcomatoid RCC and other renal sarcomas. Distinct imaging characteristics of MTSCC have not been described in literature. Background functional histology of the collecting duct The collecting tubules and ducts descend into the medullary rays and eventually merge to form the collecting ducts of Bellini, which subsequently enter the pelvicalyceal system. The primary role of the collecting tubules is urinary concentration through passive reabsorption of water that is regulated by antidiuretic hormone (ADH) [4]. The epithelium is simple columnar and contains three cell types, principal cells and Type A and B intercalated cells. The principal cells are involved in ADH-stimulated water reabsorption and sodium reabsorption [4]. Type A intercalated cells contain an adenosine triphosphate (ATP)-dependent hydrogen–potassium ion exchanger that enables secretion of acid against a gradient. Type B intercalated cells contain an apical chloride/ bicarbonate antiporter that allows bicarbonate secretion. Nephronal disorders localized to the cortical collecting duct Oncocytoma Renal oncocytoma is a benign neoplasm thought to differentiate towards Type A intercalated cells of the 4 of 10 cortical collecting duct [1, 25]. Oncocytomas constitute 3– 5% of all adult primary renal epithelial neoplasms. There is no specific sex predilection. Typically, oncocytomas are well-encapsulated tumours with a characteristic mahogany-brown cut surface and a central stellate fibrous scar [8]. Necrosis is extremely rare; haemorrhage may be found in up to 20% of cases. Histologically, oncocytomas are composed of uniform polygonal, mitochondria-rich cells arranged in nests, tubules and acini [8]. Immunocytochemistry techniques, staining with Hale’s colloidal iron and cytogenetics help to distinguish oncocytomas from chromophobe RCCs [13]. On cross-sectional modalities, oncocytomas appear as well-circumscribed, homogeneous, smooth-marginated neoplasms (Figure 5). Oncocytoma is usually a solitary lesion with a median size of 4–5 cm [8]. Bilateral and multicentric oncocytomas are seen in renal oncocytosis. A central stellate scar is a characteristic finding seen in up to 54% of oncocytomas (Figure 5) [26]. Central scar and the tumour capsule may be better seen with MRI [27]. A characteristic ‘‘spoke-wheel’’ pattern of vascularity has been described on catheter angiography [26, 28]. In contradistinction to RCC, arteriovenous shunts or contrast puddling are typically absent [28]. However, there is considerable overlap in the imaging findings of oncocytoma and RCC subtypes [29]. Chromophobe renal cell carcinoma Thoenes et al [30] first described chromophobe RCC (CRCC) in 1985 as a distinct variant of RCC on the basis of morphological criteria. CRCC represents between 5% and 7% of adult RCCs [8]. The British Journal of Radiology Segmental disorders of the nephron Figure 5. Bilateral renal oncocytomas. Delayed phase contrast-enhanced CT scan shows bilateral, hypoattenuating solid renal masses (arrows). While the right renal mass is uniformly hypoattenuating, the left renal mass shows the characteristic central stellate scar (arrowhead). CRCC typically appears as solitary, well-circumscribed solid neoplasms. CRCC cells resemble the Type B intercalated cells of the cortical collecting duct [1, 31]. Histopathologically, CRCC displays solid sheets of large polygonal cells with pale reticular cytoplasm, perinuclear clearing and prominent cell membranes. Most CRCC demonstrates diffuse staining with Hale’s colloidal iron. CRCC typically appears hypovascular on contrastenhanced CT and MRI despite the large size [32] (Figure 6). CRCC may appear hypointense on T2 weighted MRI. At catheter angiography, CRCC is commonly hypovascular. A spoke-wheel pattern of contrast enhancement on CT scan has been described recently [33]. CRCC demonstrates a more favourable prognosis and biological behaviour than clear cell RCC [17]. Nephronal disorders localized to the medullary collecting duct Collecting duct carcinoma Collecting duct carcinoma (CDC) is a highly aggressive malignant neoplasm that comprises , 1% of all RCCs [8, 34]. CDC is thought to differentiate towards the principal cells of the medullary collecting duct (a derivative of the ureteral bud). CDC appears as a grey-white infiltrative neoplasm with a medullary epicentre. Histologically, classic CDC is histologically characterized by a tubulopapillary growth pattern, marked desmoplasia and variable mucin production [34]. CDC demonstrates a variegated appearance on crosssectional imaging modalities [3, 35]. Although CDC may appear as expansile masses, it typically exhibits a diffuse infiltrating growth pattern. At sonography, CDC may be hyperechoic or hypoechoic to the renal parenchyma [3, 35] (Figure 7). Typically, CDC appears as a diffusely infiltrative, hypovascular mass on contrast-enhanced CT scan (Figure 8). Calcification may be seen in up to 25% of patients [35]. CDC is frequently hypointense on T2 The British Journal of Radiology, Month 2007 Figure 6. Chromophobe renal cell carcinoma. Coronal, gadolinium-enhanced T1 weighted GRE image of the right kidney during nephrographic phase shows a large, expansile mass (arrows) that shows heterogeneous contrast enhancement (arrowhead). weighted MRI. Imaging findings of a hypovascular, infiltrative mass with a medullary epicentre may suggest the diagnosis of CDC [35]. Most CDCs are clinicobiologically aggressive neoplasms with resultant poor prognosis. Renal medullary carcinoma Renal medullary carcinoma (RMC) is an extremely aggressive malignant neoplasm that develops almost exclusively in young patients with sickle cell trait. First described by Davis et al [2] in 1995, RMC is considered the seventh sickle cell nephropathy. Histological features of RMC mostly mimic those of CDC. It is hypothesized that RMC develops in a background of transitional cell hyperplasia in the renal medulla resulting from chronic hypoxia [2, 36]. At gross pathology, RMC shows a central location and is poorly circumscribed with frequent haemorrhage and necrosis [8]. Histopathologically, RMC is characterized by sheets of poorly differentiated tumour cells that may show reticular and adenoid cystic growth patterns [8]. At imaging, RMC typically appears as ill-defined, infiltrative masses that arise in the renal medulla and 5 of 10 S R Prasad, V R Narra, R Shah et al caliectasis is a frequent associated finding [37]. RMC is typically hypovascular at catheter angiography. Extrarenal metastases to lymph nodes, lung, adrenal gland and liver are frequently seen and carry a poor prognosis [8]. Autosomal recessive polycystic kidney disease Autosomal recessive polycystic kidney disease (ARPKD) is an autosomal recessive renal disorder characterized by a variable degree of renal cyst formation and hepatic fibrosis [38]. Patients with infantile disease present at birth with severe renal impairment. At the other end of the spectrum, juvenile patients manifest with liver disease and portal hypertension. Renal disease is not always clinically apparent as only about 10% of the collecting tubules are affected. ARPKD is caused by mutations involving the PKHD1 (polycystic kidney and hepatic disease 1) gene on chromosome 6p [39]. The gene product called polyductin or fibrocystin is presumably involved in cell adhesion or proliferation [40]. Renal cysts are the result of hyperplasia of the secretory epithelia leading to fusiform dilatation of the collecting ducts [38]. The cysts are arranged radially, Figure 7. Collecting duct carcinoma of the kidney. Transverse, right renal sonogram shows an expansile, uniformly hypoechoic solid neoplasm (arrowheads). Arrow shows the right kidney. invade the renal sinus [3, 37] (Figure 9). Uncommonly, RMC may manifest as expansile masses. It is difficult to ascertain the medullary location of large RMC. Isolated Figure 8. Collecting duct carcinoma of the kidney. Nephrographic phase, contrast-enhanced CT scan demonstrates a hypoattenuating, infiltrating neoplasm in the right kidney (arrow) with associated retroperitoneal lymphadenopathy (arrowhead). 6 of 10 Figure 9. Renal medullary carcinoma. Nephrographic phase contrast-enhanced CT scan demonstrates a hypoattenuating, infiltrating neoplasm in the right kidney (arrow) with associated low-density retroperitoneal lymphadenopathy (arrowhead). The British Journal of Radiology Segmental disorders of the nephron perpendicular to the renal capsule. Liver involvement is universally present and is characterized by proliferation and dilatation of small intrahepatic bile ducts as well as periportal fibrosis [38]. The renal findings are summarized here. Sonographic findings include smoothly enlarged kidneys, diffuse, increased echogenicity and loss of the corticomedullary differentiation [41]. High resolution sonography may show dilated, radially oriented medullary tubules, macroscopic cysts and intratubular crystalline foci [42]. Intravenous urography demonstrates decreased excretion of contrast material, enlarged kidneys and striated nephrograms secondary to dilated collecting tubules [41]. Contrastenhanced CT shows striated nephrograms [41]. Fetal MRI demonstrates nephromegaly with high water content and radial striations related to fluid-filled ectatic ducts. Medullary sponge kidney Also referred to as Lenarduzzi–Cacchi–Ricci disease (in the Mediterranean literature), medullary sponge kidney (MSK) is an idiopathic, congenital, developmental abnormality characterized by diffuse or focal ectasia and cyst formation in the intrapyramidal or intrapapillary portion of the medullary collecting duct [43]. Although MSK is mostly sporadic, familial forms of MSK with an autosomal dominant inheritance pattern have been described [44]. MSK is hypothesized to result from disruption of the embryonic interface between the developing ureteral bud and the metanephric blastema [45]. MSK may be associated with other renal conditions such as hemihypertrophy and Beckwith–Wiedemann syndrome [46]. MSK is twice as frequent in women. Patients with MSK may be asymptomatic, and the condition is often discovered incidentally on imaging studies. MSK is usually diagnosed in the third or fifth decades of life during the evaluation of nephrocalcinosis, urinary tract infection or calculus disease. MSK is characterized by multiple, variably shaped subcentimetre cysts within the papillae. Usually, both kidneys and most of the renal pyramids are involved [38]. The cysts are lined by cuboidal, columnar or transitional epithelium. Cysts containing calcific material Figure 11. Medullary sponge kidney. Intravenous urography shows the characteristic medullary ‘‘brush’’ configuration of the dilated collecting ducts in the right kidney (arrows). may show squamous metaplasia. Complications include haematuria, urinary tract infection and calculi [43]. Recurrent calcium nephrolithiasis is a result of complex factors, including urinary stasis, and associated abnormalities such as hypercalciuria, distal renal tubular acidosis and acidification defects [43]. Medullary nephrocalcinosis is a characteristic finding of MSK (Figure 10). Clusters of retained contrast medium within the dilated papillae on intravenous urography (IVU) are diagnostic of MSK [47]. On IVU, radial linear streaking in the renal papillae due to ductal ectasia confers a characteristic ‘‘medullary brush’’ configuration (Figure 11). In severe cases, beaded or striated cavities and associated calculi distort the calyces. Echogenic medullary pyramids due to nephrocalcinosis may be seen on sonography [48]. CT is helpful in evaluating complications including nephrolithiasis, obstruction and pyelonephritis. Nephronal disorders localized to pyramid/ papilla Figure 10. Renal medullary nephrocalcinosis. Longitudinal right renal sonogram demonstrates hyperechoic pyramids (arrows) consistent with medullary nephrocalcinosis. The British Journal of Radiology, Month 2007 Papillary necrosis As the name implies, papillary necrosis is pathologically characterized by ischaemic, coagulative necrosis of 7 of 10 S R Prasad, V R Narra, R Shah et al Figure 12. (a) Autosomal dominant polycystic kidney disease complicated by the development of a renal cell carcinoma. Coronal T2 weighted MRI shows innumerable cysts that replace both the kidneys (arrowheads). Incidentally seen is a hypointense mass in the upper pole of the right kidney (arrows). (b) Autosomal dominant polycystic kidney disease complicated by the development of a renal cell carcinoma. Coronal, gadolinium-enhanced T1 weighted two-dimensional GRE MRI shows predominantly peripheral contrast enhancement of the mass in the upper pole of the right kidney (arrowheads). the renal papillae. Common predisposing risk factors include urinary obstruction, infection, diabetes mellitus, sickle cell disease and analgesic abuse nephropathy [49]. Urinary obstruction results in compression of thinwalled blood vessels that compromises the papillary perfusion. The incidence of papillary necrosis in patients with sickle cell disease and diabetes mellitus is 65% and 24%, respectively [50]. Patients with papillary necrosis present with a wide spectrum of non-specific symptoms and signs including haematuria, pyuria, bacteriuria, polyuria and electrolyte imbalances [51]. Papillary necrosis is bilateral in three-quarters of the cases. The renal medulla is relatively hypoperfused and receives between 2.5 ml min21 g21 (outer medulla) and 0.6 ml min21 g21 tissue (inner medulla) [4]. Compared with this, the renal cortex receives 5 ml min21 g21 tissue. Renal medulla, especially the papillae, are thus at increased risk of ischaemic necrosis. The ischaemic process may be reversible or irreversible. Persistent ischaemia leads to coagulation necrosis, tubular fibrosis, lobar infarcts and sloughing of the papilla [52]. Regional distribution of the medullary vasa rectae and the peripapillary plexus determines the location and degree of papillary necrosis. IVU is a sensitive test to detect papillary necrosis. The peripheral or central portions of the papillae may be involved. The findings on IVU include persistent contrast collections and cavitations within the pelvicalyceal system. Dystrophic calcification of the necrosed papillae may ensue in chronic cases. Sloughed papillae appear as filling defects that may cause obstruction in the urinary system. CT findings of papillary necrosis include illdefined medullary areas of contrast non-enhancement, persistent contrast collections, filling defects in the collecting system and, in late cases, calcification [51, 52]. Multiphase CT may be useful in the detection of early papillary necrosis and to document papillary healing following treatment [51, 52]. Ultrasound may demonstrate urinary obstruction in patients with acute urinary obstruction secondary to sloughed papillae [53]. 8 of 10 Necrosed papillae may appear as soft tissue masses within the collecting system or the ureter on ultrasound [53]. Polysegmental nephronal disorders Pan-nephronal disorder: autosomal dominant polycystic kidney disease Autosomal dominant polycystic kidney disease (ADPKD) is the most common hereditary renal cystic disease that is characterized by multiple expansile, bilateral renal cysts that ultimately lead to renal failure [38]. The cysts are derived from all segments of the nephrons [38]. Eighty-five per cent of ADPKD is a result of genetic mutations in the PKD1 gene located on chromosome 16p [38]. The less common mutation involving the PKD2 gene located on chromosome 4q is seen in 15% of patients [38]. The PKD1 gene product polycystin-1 interacts with polycystin-2, a voltage-activated calcium channel that is encoded by the PKD2 gene, to regulate the cell cycle and intracellular calcium transport. Both proteins are involved in cell–cell and cell–matrix interactions that determine tubular morphogenesis [54]. Cyst formation is focal in ADPKD, affecting , 5% of the nephrons [38]. The cyst growth leads to replacement of the normal parenchyma and interstitial fibrosis. Systemic complications of ADPKD include hypertension, renal failure and intracranial haemorrhage from rupture of berry aneurysms [38]. At imaging, multiple, bilateral, variable-sized renal cysts are identified with some showing haemorrhage [55]. Associated liver cysts are seen in about 70% of patients. In advanced stages, both kidneys are enlarged with loss of reniform shape and near complete replacement of parenchyma. Renal complications include pyelonephritis, calculus disease, kidney failure and malignancy [38] (Figure 12a,b). The British Journal of Radiology Segmental disorders of the nephron Summary To summarize, recent advances in cytogenetics and molecular biology have shed fresh light on the cells of origin and the pathogenesis of renal disorders. Many renal disorders are now postulated to arise from specific segments of the nephrons and demonstrate characteristic biology and clinical findings. Although there is considerable overlap in the imaging findings of renal disorders arising from different nephronal segments, some disorders exhibit characteristic findings that permit accurate diagnosis. References 1. Polascik TJ, Bostwick DG, Cairns P. Molecular genetics and histopathologic features of adult distal nephron tumors. Urology 2002;60:941–6. 2. Davis CJ, Jr, Mostofi FK, Sesterhenn IA. Renal medullary carcinoma. The seventh sickle cell nephropathy. Am J Surg Pathol 1995;19:1–11. 3. Prasad SR, Humphrey PA, Menias CO, et al. Neoplasms of the renal medulla: radiologic–pathologic correlation. Radiographics 2005;25:369–80. 4. Ganong W. Review of medical physiology. New York: Lange Medical Books/McGraw-Hill, 2005. 5. Martin SA, Mynderse LA, Lager DJ, Cheville JC. Juxtaglomerular cell tumor: a clinicopathologic study of four cases and review of the literature. Am J Clin Pathol 2001;116:854–63. 6. Robertson PW, Klidjian A, Harding LK, Walters G, Lee MR, Robb-Smith AH. Hypertension due to a renin-secreting renal tumour. Am J Med 1967;43:963–76. 7. Conn JW, Cohen EL, McDonald WJ, et al. The syndrome of hypertension, hyperreninemia and secondary aldosteronism associated with renal juxtaglomerular cell tumor (primary reninism). Trans Am Assoc Genitourin Surg 1972;64:47–53. 8. Eble JN, SG, Sesterhenn J, editors. Pathology and genetics of tumours of the urinary system and male genital organs. Lyon, France: IARC Press, 2004. 9. Tanabe A, Naruse M, Ogawa T, et al. Dynamic computer tomography is useful in the differential diagnosis of juxtaglomerular cell tumor and renal cell carcinoma. Hypertens Res 2001;24:331–6. 10. Dunnick NR, Hartman DS, Ford KK, Davis CJ, Jr, Amis ES, Jr. The radiology of juxtaglomerular tumors. Radiology 1983;147:321–6. 11. Young BHJ. Wheater’s functional histology: a text and colour atlas. Edinburgh: Churchill Livingstone, 2000. 12. Choyke PL, Glenn GM, Walther MM, Zbar B, Linehan WM. Hereditary renal cancers. Radiology 2003;226:33–46. 13. Jones TD, Eble JN, Cheng L. Application of molecular diagnostic techniques to renal epithelial neoplasms. Clin Lab Med 2005;25:279–303. 14. Cohen HT, McGovern FJ. Renal-cell carcinoma. N Engl J Med 2005;353:2477–90. 15. Kim JK, Kim TK, Ahn HJ, Kim CS, Kim KR, Cho KS. Differentiation of subtypes of renal cell carcinoma on helical CT scans. AJR Am J Roentgenol 2002;178:1499–506. 16. Outwater EK, Bhatia M, Siegelman ES, Burke MA, Mitchell DG. Lipid in renal clear cell carcinoma: detection on opposed-phase gradient-echo MR images. Radiology 1997;205:103–7. 17. Cheville JC, Lohse CM, Zincke H, Weaver AL, Blute ML. Comparisons of outcome and prognostic features among histologic subtypes of renal cell carcinoma. Am J Surg Pathol 2003;27:612–24. The British Journal of Radiology, Month 2007 18. Ishikawa I, Kovacs G. High incidence of papillary renal cell tumours in patients on chronic haemodialysis. Histopathology 1993;22:135–9. 19. Delahunt B, Eble JN, McCredie MR, Bethwaite PB, Stewart JH, Bilous AM. Morphologic typing of papillary renal cell carcinoma: comparison of growth kinetics and patient survival in 66 cases. Hum Pathol 2001;32:590–5. 20. Choyke PL, Walther MM, Glenn GM, et al. Imaging features of hereditary papillary renal cancers. J Comput Assist Tomogr 1997;21:737–41. 21. Herts BR, Coll DM, Novick AC, et al. Enhancement characteristics of papillary renal neoplasms revealed on triphasic helical CT of the kidneys. AJR Am J Roentgenol 2002;178:367–72. 22. Shinmoto H, Yuasa Y, Tanimoto A, et al. Small renal cell carcinoma: MRI with pathologic correlation. J Magn Reson Imaging 1998;8:690–4. 23. Eble JN. Mucinous tubular and spindle cell carcinoma and post-neuroblastoma carcinoma: newly recognised entities in the renal cell carcinoma family. Pathology 2003;35:499–504. 24. Weber A, Srigley J, Moch H. [Mucinous spindle cell carcinoma of the kidney. A molecular analysis]. Pathologe 2003;24:453–9. 25. Storkel S, Pannen B, Thoenes W, Steart PV, Wagner S, Drenckhahn D. Intercalated cells as a probable source for the development of renal oncocytoma. Virchows Arch B Cell Pathol Mol Pathol 1988;56:185–9. 26. Quinn MJ, Hartman DS, Friedman AC, et al. Renal oncocytoma: new observations. Radiology 1984;153:49–53. 27. Sasaki S, Hayashi Y, Tsugaya M, Okamura T, Sakakura T, Kohri K. [Radiological diagnosis of renal oncocytoma]. Hinyokika Kiyo 1995;41:731–5. 28. Duber C, Schweden F, Klose KJ, Storkel S, Engelmann U, Thelen M. [Oncocytoma of the kidney. II. Angiography]. Rofo 1988;148:227–33. 29. Jinzaki M, Tanimoto A, Mukai M, et al. Double-phase helical CT of small renal parenchymal neoplasms: correlation with pathologic findings and tumor angiogenesis. J Comput Assist Tomogr 2000;24:835–42. 30. Thoenes W, Storkel S, Rumpelt HJ. Human chromophobe cell renal carcinoma. Virchows Arch B Cell Pathol Mol Pathol 1985;48:207–17. 31. Storkel S, Steart PV, Drenckhahn D, Thoenes W. The human chromophobe cell renal carcinoma: its probable relation to intercalated cells of the collecting duct. Virchows Arch B Cell Pathol Mol Pathol 1989;56:237–45. 32. Mugiya S, Nagata M, Ozono S, et al. [Ultrasonographic features of chromophobe cell renal carcinoma]. Hinyokika Kiyo 2004;50:865–8. 33. Kondo T, Nakazawa H, Sakai F, et al. Spoke-wheel-like enhancement as an important imaging finding of chromophobe cell renal carcinoma: a retrospective analysis on computed tomography and magnetic resonance imaging studies. Int J Urol 2004;11:817–24. 34. Srigley JR, Eble JN. Collecting duct carcinoma of kidney. Semin Diagn Pathol 1998;15:54–67. 35. Pickhardt PJ, Siegel CL, McLarney JK. Collecting duct carcinoma of the kidney: are imaging findings suggestive of the diagnosis? AJR Am J Roentgenol 2001;176:627–33. 36. Swartz MA, Karth J, Schneider DT, Rodriguez R, Beckwith JB, Perlman EJ. Renal medullary carcinoma: clinical, pathologic, immunohistochemical, and genetic analysis with pathogenetic implications. Urology 2002;60:1083–9. 37. Davidson AJ, Choyke PL, Hartman DS, Davis CJ, Jr. Renal medullary carcinoma associated with sickle cell trait: radiologic findings. Radiology 1995;195:83–5. 38. Bisceglia M, Galliani CA, Senger C, Stallone C, Sessa A. Renal cystic diseases: a review. Adv Anat Pathol 2006;13: 26–56. 9 of 10 S R Prasad, V R Narra, R Shah et al 39. Bergmann C, Kupper F, Schmitt CP, et al. Multi-exon deletions of the PKHD1 gene cause autosomal recessive polycystic kidney disease (ARPKD). J Med Genet 2005;42:e63. 40. Onuchic LF, Furu L, Nagasawa Y, et al. PKHD1, the polycystic kidney and hepatic disease 1 gene, encodes a novel large protein containing multiple immunoglobulinlike plexin-transcription-factor domains and parallel betahelix 1 repeats. Am J Hum Genet 2002;70:1305–17. 41. Lonergan GJ, Rice RR, Suarez ES. Autosomal recessive polycystic kidney disease: radiologic–pathologic correlation. Radiographics 2000;20:837–55. 42. Traubici J, Daneman A. High-resolution renal sonography in children with autosomal recessive polycystic kidney disease. AJR Am J Roentgenol 2005;184:1630–3. 43. Gambaro G, Feltrin GP, Lupo A, Bonfante L, D’Angelo A, Antonello A. Medullary sponge kidney (Lenarduzzi– Cacchi–Ricci disease): a Padua Medical School discovery in the 1930s. Kidney Int 2006;69:663–70. 44. Klemme L, Fish AJ, Rich S, Greenberg B, Senske B, Segall M. Familial ureteral abnormalities syndrome: genomic mapping, clinical findings. Pediatr Nephrol 1998;12:349–56. 45. Gambaro G, Fabris A, Citron L, et al. An unusual association of contralateral congenital small kidney, reduced renal function and hyperparathyroidism in sponge kidney patients: on the track of the molecular basis. Nephrol Dial Transplant 2005;20:1042–7. 46. Choyke PL, Siegel MJ, Oz O, Sotelo-Avila C, DeBaun MR. Nonmalignant renal disease in pediatric patients with Beckwith–Wiedemann syndrome. AJR Am J Roentgenol 1998;171:733–7. 10 of 10 47. Thomsen HS, Levine E, Meilstrup JW, et al. Renal cystic diseases. Eur Radiol 1997;7:1267–75. 48. Toyoda K, Miyamoto Y, Ida M, Tada S, Utsunomiya M. Hyperechoic medulla of the kidneys. Radiology 1989;173: 431–4. 49. Griffin MD, Bergstralhn EJ, Larson TS. Renal papillary necrosis – a sixteen–year clinical experience. J Am Soc Nephrol 1995;6:248–56. 50. Zadeii G, Lohr JW. Renal papillary necrosis in a patient with sickle cell trait. J Am Soc Nephrol 1997;8:1034–9. 51. Lang EK, Macchia RJ, Thomas R, et al. Detection of medullary and papillary necrosis at an early stage by multiphasic helical computerized tomography. J Urol 2003;170:94–8. 52. Lang EK, Macchia RJ, Thomas R, et al. Multiphasic helical CT diagnosis of early medullary and papillary necrosis. J Endourol 2004;18:49–56. 53. Vijayaraghavan SB, Kandasamy SV, Mylsamy A, Prabhakar M. Sonographic features of necrosed renal papillae causing hydronephrosis. J Ultrasound Med 2003;22:951–6quiz 957–8. 54. Gallagher AR, Hidaka S, Gretz N, Witzgall R. Molecular basis of autosomal-dominant polycystic kidney disease. Cell Mol Life Sci 2002;59:682–93. 55. Mosetti MA, Leonardou P, Motohara T, Kanematsu M, Armao D, Semelka RC. Autosomal dominant polycystic kidney disease: MR imaging evaluation using current techniques. J Magn Reson Imaging 2003;18: 210–15. Recipient of Silver Medal at the 2005 ARRS meeting (Ref: E 247). The British Journal of Radiology