Stump the Chump
advertisement

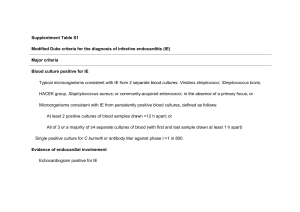
2/24/11 Stump the Chump Discussant (Chump): Harry Hollander, MD Professor of Medicine, UCSF Case 1 Case • KF is a 27 year old previously healthy student at San Francisco State with a 3-4 day history of swollen left cervical lymph nodes, fevers, chills and myalgias • 8/28/2010—SF State health Center and given amoxicillin • 8/29/2010—Felt worse with N,V, higher fevers and was given IM penicillin 1 2/24/11 Case 9/1/2010 presents to UCSF ED › Moderately toxic appearing › 132/62 120 22 39° C › No rash › HEENT—normal w/o tonsilar exudate › Neck—5X5 cm tender L mass › Abdomen—non-tender; no HSM › Lungs—clear › Heart– no murmur › Neurologic exam– normal Case • • • • • WBC 5.1—80%P, 15% L, Plts 233K Cr—0.7; UA < 5 WBC and < 3 RBC LFTs– normal Electrolytes– normal CXR—normal 2 2/24/11 Large necrotic jugulodigastric LN measuring 3.5 cm with enlarged LNs extending down the Internal jugular & posterior cervical chains into the supraclavicular area Case • 9/2/2010 (Day 2) – FNA Lymph node—reactive lymphoid tissue • Cultures – BC & Urine—negative • Started on Zosyn (Pip-Tazo) – Temps now 40.5°C – Repeat CBC—WBC 2.8, Plts 128K, Hct 28% Case • 9/3/2010 (Day 3)—ID consult called • Additional labs – Mono spot– negative – HIV—negative – CMV PCR– undetectable – Toxo—negative – ANA-- <1:40 3 2/24/11 Case • Additional ID history – From Portland – Has a cat at home—been home during the summer but does not remember any scratches/bites – Volunteered at a homeless shelter while on summer break – Cousin with SLE 4 2/24/11 Case • OH YES, AND BY THE WAY Case • Before I came back to school I stopped at Lake Tahoe with some friends. • Mostly in the casinos but did go to the beach • And, I thought this was interesting even though I have no idea what it means but I took a picture of this on my cell phone—is it important 5 2/24/11 CASE • Started on doxycycline and streptomycin • For insurance reasons was transferred to SFGH • And a diagnosis was made Case--DDx EBV HIV CMV Toxo Plague Tularemia TB CSD Strep Staph Lymphoma SLE Castleman’s Disease Kawasaki’s Kikuchi Fujimoto’s Disease 6 2/24/11 What is your most likely diagnosis? A. Castleman’s Disease B. EBV C. HIV D. Kikuchi Fujimoto E. Lymphoma F. Plague G. Toxoplasmosis H. Tularemia Kikuchi Fujimoto Disease or Histiocytic Necrotizing Lymphadenitis Benign cause of lymphadenopathy Female predominance Age range broad (11-80 yrs) but vast majority <30 yrs Cervical LN’s in 80-95% but almost all nodal areas involved Fever in 30-50% Leukopenia (+/- atypical lymphocytes) in 50% Diagnosis by histopathology Course benign, self limited usually several weeks to a month (can be several months) Recurrence, 5% 7 2/24/11 Case 2 Case History • CC: Left wrist pain • 71 year-old man presents with 1 month of swelling, redness, and pain at left wrist • No fever, chills, nightsweats, or weight loss • Denis any trauma • Steroid injection was done with some improvement but pain then progressed 8 2/24/11 Case history continued • PMH – – – – – – • SH HTN Cataracts B-thalasemia trait Gum abscesses – ‘07-’08 Dacrocystitis – ‘09 Pyoderma gangrenosum – ‘10 • Meds – Lisinopril/HCTZ – Multivitamin – Born in Hong Kong – moved to US 40 yrs ago – Lived in midwest US for 15 years – Lives in Mississippi near Memphis, TN (last 25 yrs) – College professor in engineering – No animals – Sex with wife only – Denies IVDU Physical exam • VS: 120#, 123/67, 77, 18, 99% RA • GEN: well appearing, NAD HEENT: oropharynx clear; surgical pupils • LN: no LAD • CV: RRR no M • Chest: clear • Abdomen: soft, no organomegaly • Skin: healed ulcer on right shin • MSK: L lateral wrist: warm, swollen, minimal pain to palp. Able to flex/extend w/o much pain 9 2/24/11 Labs • 12>33<316 • Cr and LFTs: wnl • ESR: 43; CRP: 31 MRI arm: hyperintense destructive process centered within the distal ulna causing circumferential endosteal scalloping surrounded by a thick rind of periosteal reaction 10 2/24/11 Bone Biopsy • Pathology: neutrophilic infiltrate suggestive of acute and chronic osteomyelitis • Culture: Proprionobacterium acnes in enrichment broth only 11 2/24/11 Which specialist confirmed the suspected diagnosis? A. Gastroenterologist B. Orthopedic surgeon C. Rheumatologist D. Endocrinologist E. Oncologist History continued • P acnes felt to be contaminant • Based on the multiple recent sterile, neutrophil rich processes… – Gum abscesses – Dacrocystitis – Pyoderma gangrenosum – Sterile osteomyelitis • Concern was raised for non-infectious process Rheumatology consult • Elicited further history of pustular facial rash in 2007-2008 • Son with ankylosing spondylitis and HLAB27+ • Felt that the clinical presentation was consistent with SAPHO syndrome • Patient HLA-B27+ • Rx: Entanercept, wrist improved 12 2/24/11 SAPHO syndrome • Synovitis • Acne • Pustulosis • Hyperostosis • Osteitis • Immune mediated syndrome • Predominated by multiple, sterile, neutrophil rich infiltrates in bone, skin, and joints • Association with HLAB27+ Case 3 Case History • 57 y/o Native American man – Called back to the ED for positive blood cultures • 3 days ago seen in ED for AMS and hyperglycemia which resolved with IV hydration – Two blood cultures were drawn – Patient discharged 13 2/24/11 Case History cont. • Now both blood cultures are positive – BC #1: Klebsiella pneumoniae, E. coli, Yeast, GBS, 2 types viridans strep, CNS and “additional organisms” – BC #2: E coli, 2 types strep, CNS, “additional organisms.” • Further questioning reveals subjective fevers and night sweats for ~3-4 months Other History • • • • • • • • Homeless Chronic alcoholism Insulin-dependent diabetes for 20 years Hx of CVA 10 years ago Seizure disorder s/p cholecystectomy in 1996 GSW to right knee 1/08 Numerous recent admissions, ED visits 14 2/24/11 Recent Admissions • 6 mo PTA: DKA + MRSA bacteremia – BC drawn on day 1, 2 and 4 of admission all positive for MRSA – Day 3: vancomycin started 6/1/08 – Day 7: patient signs out AMA – Returns 3 weeks later: repeat BC all negative Recent Admissions (cont.) • 2 months PTA: DKA and AMS – 1 of 2 BCs postive for CNS, E. coli, viridans strep, Candida tropicalis, corynebacteria – Briefly treated with fluconazole and vancomycin, D/C’d by ID fellow who considered positive BC contaminated – F/u BCs negative Recent Admissions (cont.) • 1 mo PTA: DKA and foot pain – Blood cultures negative – Treated for presumed cellulitis and discharged in good condition • 1 week PTA: seen in ED for AMS – Blood cultures negative 15 2/24/11 Summary of Blood Culture Results • 6 months ago – 7/8 positive for MRSA over a 4 day span – Patients signs out AMA after 5 days of vanco – 2/2 f/u cultures 3 weeks later: negative • 2 months ago – 1 of 2 positive for CNS, Candida tropicalis, cornyebacteria – 2/2 three days later: negative • 1 month PTA: 2/2 negative • 1 week PTA: 2/2 negative Exam • T=35.9 BP 140/80 P 90 RR 16 96% RA • Gen: drowsy, slurring speech • HEENT: multiple facial ecchymoses, PERRLA • CV: RRR, nl S1/S2 No m/r/g • Pulm: LCTA bilaterally. No wheezes • ABD: Diffuse mild TTP. No HSM • Skin: erythematous rash in groin region • Neuro: A&Ox3. CN2-12 intact. 16 2/24/11 Labs 11.0 4.1 35.3 65% N 247 139 103 8 4.3 25 0.4 AST/ALT 25/15 Alk Phos 218 404 UA: 1+ ketones, 3+ glucose, 1+ protein 0 WBCs CXR: negative Hospital Course • Day 1 – More blood cultures: 1/2 + Propionibacterium sp. – Fluconazole administered • Day 2 – Night sweats but no new events – Fluconazole stopped – 2/2 repeat BC: negative • Day 3 – Temp to 39C – Ceftriaxone begun empirically – 1/2 BCs eventually positive for K. pneumoniae 17 2/24/11 Abdominal CT • Focal 2.8 X 2.1 cm low attenuation collection within the omentum of the right lower quadrant with enhancing thickening rim. • Findings may represent abscess or omental implant. • The differential may include epiploic appendagitis or omental infarct At exploratory laparotomy the lesion was found to be a complication of which of the following? A. Diverticulitis of the R colon with abscess B. Omental tuberculoma C. Epiploic appendagitis D. Prior cholecystectomy E. Microperforated appendiceal abscess 18 2/24/11 Dropped Gallstones • Complicates as many as a third of all laparoscopic cholecystectomies • Dropped stones should be recognized as a potential cause of intra-abdominal abscess in any cholecystectomy patient months or even years after the surgery • Dropped stones produce an intra-abdominal abscess in 0.6% to 2.9% of cases of dropped stones Case 4 19 2/24/11 Case History • 69-year old woman from Berne presents new onset maculopapular rash • Recently diagnosed with SLE vs. overlap syndrome w/ dermatomyositis – Had symmetrical polyarthralgias, synovitis of large joints, polyserositis, myositis, and microvascular disturbances – Rx: Prednisone, azathioprine, chloroquine Case History cont. PMH • Hypertensive cardiomyopathy • Malnutrition • Hypercholesteremia • Panic attacks Physical exam • • • • • • • VS: Afebilre, BP 160/95 mmHg, P = 110 GEN: chronically ill appearing Chest: normal Abdomen: no tenderness LAD: none Neuro: normal Skin: Confluent, maculopapular rash on upper trunk, arms and thighs • . 20 2/24/11 Case History continued • Rx: methylprednisolone 125 mg /day with Improvement of rash by day 2 • HD #4: Acute onset headaches and fever • Neurologic exam: Somnolent, slurred speech, difficulty swallowing, right-sided hemiparesis and Babinski sign, mild meningismus Labs • CBC: 11>32<228 • CRP: 61 mg/l (normal <5) • Cr and LFTs: wnl • CSF values (performed after CT scan) – WBC: 41 (95% PMN) – Protein: 125 (< 44) – Glucose: 35 (glucose CSF/serum =0.36) – Lactate: 2.80 (1.20-2.10) 21 2/24/11 MRI on 4th hospital day 22 2/24/11 Etiology of Brain Abscess? A. B. C. D. E. F. Cryptococccus sp Fusarium sp Zygomyces Listeria sp Mycobacterium sp Nocardia sp Subsequent course • Rx: ceftriaxone, amoxicillin, metronidazole • Blood cultures: Listeria monocytogenes • CSF cultures: negative • Antibiotics: amoxicillin + gentamicin • Neurosurgeons elected not to drain lesion • Failure to improve on antibiotics x 7 days • Repeat MRI MRI on 11th hospital day Initial Day 7 of Rx 23 2/24/11 Case history continued • Drainage of abscess in thalamus – Large amounts of pus – Culture negative • Improvement of mental status but persistence of focal neurologic deficits Listeria monocytogenes • Food borne illness: – soft cheeses, food from delicatessen counters • Predisposing conditions: – Immunosuppression – Pregnancy • Clinical manifestations – Febrile gastroenteritis – Sepsis in pregnancy and neonates – CNS infection: meningoencephalitis, romboencephalitis, brain abscess 24