NON-‐ALCOHOLIC FATTY LIVER DISEASE (NAFLD) Fatty liver
advertisement
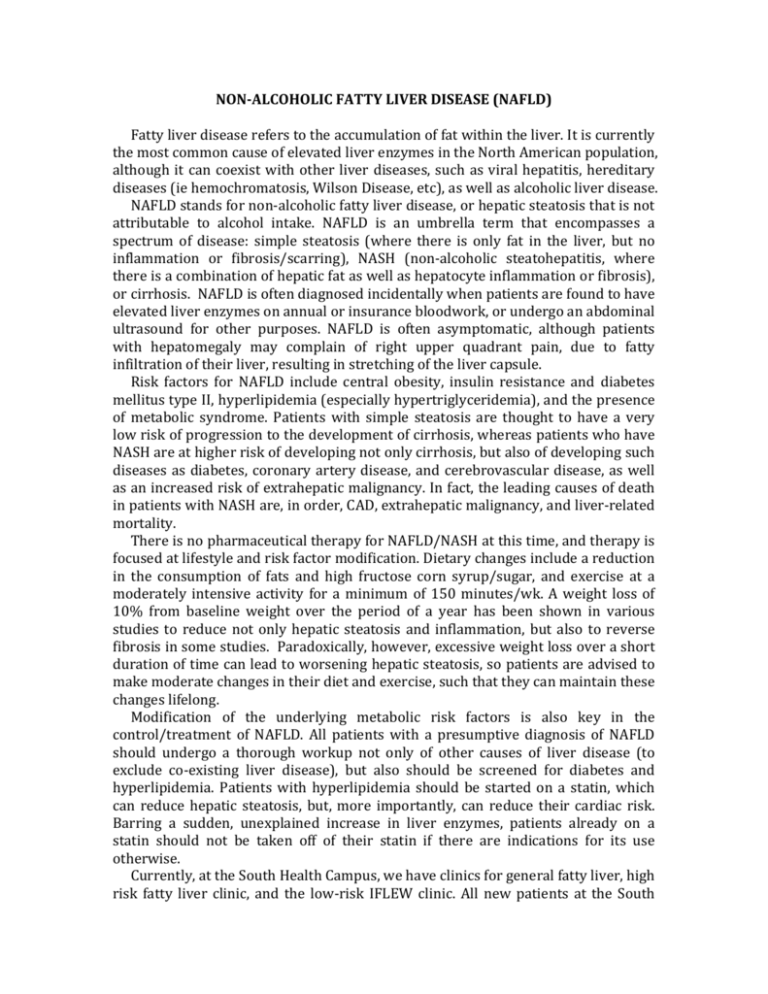
NON-­‐ALCOHOLIC FATTY LIVER DISEASE (NAFLD) Fatty liver disease refers to the accumulation of fat within the liver. It is currently the most common cause of elevated liver enzymes in the North American population, although it can coexist with other liver diseases, such as viral hepatitis, hereditary diseases (ie hemochromatosis, Wilson Disease, etc), as well as alcoholic liver disease. NAFLD stands for non-­‐alcoholic fatty liver disease, or hepatic steatosis that is not attributable to alcohol intake. NAFLD is an umbrella term that encompasses a spectrum of disease: simple steatosis (where there is only fat in the liver, but no inflammation or fibrosis/scarring), NASH (non-­‐alcoholic steatohepatitis, where there is a combination of hepatic fat as well as hepatocyte inflammation or fibrosis), or cirrhosis. NAFLD is often diagnosed incidentally when patients are found to have elevated liver enzymes on annual or insurance bloodwork, or undergo an abdominal ultrasound for other purposes. NAFLD is often asymptomatic, although patients with hepatomegaly may complain of right upper quadrant pain, due to fatty infiltration of their liver, resulting in stretching of the liver capsule. Risk factors for NAFLD include central obesity, insulin resistance and diabetes mellitus type II, hyperlipidemia (especially hypertriglyceridemia), and the presence of metabolic syndrome. Patients with simple steatosis are thought to have a very low risk of progression to the development of cirrhosis, whereas patients who have NASH are at higher risk of developing not only cirrhosis, but also of developing such diseases as diabetes, coronary artery disease, and cerebrovascular disease, as well as an increased risk of extrahepatic malignancy. In fact, the leading causes of death in patients with NASH are, in order, CAD, extrahepatic malignancy, and liver-­‐related mortality. There is no pharmaceutical therapy for NAFLD/NASH at this time, and therapy is focused at lifestyle and risk factor modification. Dietary changes include a reduction in the consumption of fats and high fructose corn syrup/sugar, and exercise at a moderately intensive activity for a minimum of 150 minutes/wk. A weight loss of 10% from baseline weight over the period of a year has been shown in various studies to reduce not only hepatic steatosis and inflammation, but also to reverse fibrosis in some studies. Paradoxically, however, excessive weight loss over a short duration of time can lead to worsening hepatic steatosis, so patients are advised to make moderate changes in their diet and exercise, such that they can maintain these changes lifelong. Modification of the underlying metabolic risk factors is also key in the control/treatment of NAFLD. All patients with a presumptive diagnosis of NAFLD should undergo a thorough workup not only of other causes of liver disease (to exclude co-­‐existing liver disease), but also should be screened for diabetes and hyperlipidemia. Patients with hyperlipidemia should be started on a statin, which can reduce hepatic steatosis, but, more importantly, can reduce their cardiac risk. Barring a sudden, unexplained increase in liver enzymes, patients already on a statin should not be taken off of their statin if there are indications for its use otherwise. Currently, at the South Health Campus, we have clinics for general fatty liver, high risk fatty liver clinic, and the low-­‐risk IFLEW clinic. All new patients at the South Hospital with fatty liver are seen by a dietician after their appointment with their liver doctor for dietary education. Patients with difficult to control diabetes, high cholesterol, or heart disease are seen by a liver specialist and a specialist in General Internal Medicine in order to help treat both the liver disease as well as optimizing treatment of their diabetes and heart disease . Patients who are deemed to be low risk, through a series of tests such as blood work and Fibroscan (a measure of liver stiffness) will be seen in the IFLEW (Introductory Fatty Liver Education Workshop) clinic. In this clinic session, which runs for a full half day, patients will receive education about their disease and what it entails, from a hepatology nurse clinician, education about diet and exercise from a dietician and a YMCA employee, and education about making lifestyle changes from a social worker. In this manner, we hope to reassure and educate patients about their fatty liver disease, and give them the tools to cure themselves of their disease.