Handout 2 - Health Care Compliance Association

CRIMINAL LIABILITY FOR MEDICARE OVERPAYMENTS
Daniel S. Reinberg
FOLEY & LARDNER LLP
CHIC_1256987.1
•
•
•
•
•
This statute makes it a felony punishable by a maximum of five years in prison and a fine of $250,000 for individuals or $500,000 for corporations who “having knowledge of the occurrence of any event affecting (A) his initial or continued right to any such benefit or payment . . . conceals or fails to disclose such benefit or payment either in a greater amount or quantity than is due or when no such benefit or payment is authorized.”
OIG interprets this statute as requiring disclosure of all known overpayments, regardless of whether the overpayment was initially obtained innocently or through fraud. See e.g., OIG Compliance
Guidance for Hospitals , 63 Fed. Reg. 8,987, 8,998 (February 23, 1998)
(stating that “failure to repay overpayments within a reasonable period of time could be interpreted as an intentional attempt to conceal the overpayment from the Government, thereby establishing an independent basis for a criminal violation with respect to the hospital, as well as any individuals who may have been involved.”)
Section 1320a-7b(a)(3) is arguably ambiguous as to the meaning of the term “fraudulently to secure.” Thus, it is unclear whether a provider who innocently receives an overpayment develops the required fraudulent intent by failing to disclose the overpayment once the provider discovers it.
While there are no reported federal decisions interpreting this statute, it has been used by the U.S. Department of Justice in the past to support criminal charges against providers. In addition, the statute was discussed but not definitively interpreted in United States ex rel. Thompson vs.
Columbia/HCA Health Care Corporation , 20 F. Supp. 1017 (D.C.S.D.
Tex. 1988), a qui tam action under the FCA. In that case, the relator alleged, among other things, that the defendants’ failure to disclose prohibited referrals constituted fraud and fraudulent concealment in violation of this statute. 20 F. Supp. at 1019.
There is an arbitration decision of retired California State Court Judge
Richard Byrne in connection with Certus Corp.’s attempt to unwind its acquisition of Healthcare Financial Advisors, Inc. holding that this statute does not apply to innocently obtained and non-recurring overpayments.
•
However, with no similar holding in federal court, most experts agree that it is too risky not to disclose known overpayments regardless of how obtained.
DOJ and OIG are likely to view this statute as creating a “continuing offense,” meaning that each day in which a provider fails to disclose a known overpayment presents a new offense. Under this theory, the government could argue that overpayments received many years in the past nonetheless could result in current violations of Section 1320a-
7b(a)(3) if known and not disclosed.
CHIC_1256987.1
•
•
•
•
This statute makes it a felony punishable by fines, imprisonment of up to ten years, or both for anyone who knowingly and willfully executes (or attempts to execute) a scheme to defraud any health care benefit program, or to obtain money or property from a health care benefit program through false or fraudulent pretenses, representations or promises.
This statute applies to schemes directed against not only federal health care programs (i.e., Medicare, Medicaid and Tricare) , but also private health care benefit programs that impact upon interstate commerce. See e.g., United States v. Baldwin , D.D.C. No. 02-0323 (PLF) (August 14,
2003) (indictment for scheme to defraud Kaiser Foundation Health Plan
Inc., a non profit health maintenance organization); United States v.
Murphy , N.D. Tex, No. 4:02-CR-011-Y (defendant physician convicted in
May 2003 of submitting more than one million dollars in fraudulent medical claims to insurance companies between 1996 and 2000 for services he did not provide or supervise at medical clinics located in health clubs).
In the case of the failure to disclose a known overpayment, the government may view the failure to disclose the overpayment as evidence of fraudulent intent present at the time the initial claims were submitted.
In cases where the overpayment undeniably resulted from an innocent mistake, the government may still seek to define a “scheme” to defraud in terms of the concealment that occurs after knowledge of the overpayment.
For instance, providers who are audited by outside auditors are routinely asked questions that should reasonably call for disclosure of the overpayment to the auditors. In instances where this information is withheld from the auditors or false information is provided to the auditors, the government likely will view this as active concealment and, thus, evidence of a scheme to defraud beginning at least at the time of the concealment.
2
•
•
•
These statutes, which parallel the health care fraud statute set forth above, impose criminal penalties for the use of the mail, private courier, or interstate wire service (including telephone, fax machine or computer) to conduct a scheme to defraud another of money or property.
Each individual use of the mail or interstate wires in furtherance of a scheme to defraud constitutes a separate crime punishable by up to twenty years imprisonment, a fine, or both.
Providers who fail to disclose known overpayments risk the government viewing the failure as evidence of fraudulent intent in the initial submission of the claim or as evidence of a scheme to defraud beginning with the first acts of concealment. This coupled with the use of the mails or interstate wire service can lead to prosecution under these widely used statutes.
•
•
•
•
•
This statute provides for imprisonment of up to five years, a fine, or both, for any person who “makes or presents” any claim to an agency of the
U.S. Government “knowing such claim to be false, fictitious, or fraudulent.”
This statute applies only where the victim is the U.S. Government, including Medicare, Medicaid, and Tricare.
There is no requirement that the submitted claim itself be false on its face, as the statute also includes “fraudulent” claims.
Conspiracies to violate Section 287 are criminalized by Section 286 of
Title 18, and the penalties for conspiracy are twice as severe as what can be imposed under Section 287.
The same theories of liability under the Civil False Claims Act, as discussed below, could lead to criminal liability under this statute for providers who fail to disclose known overpayments.
CHIC_1256987.1
•
This statute makes it a felony punishable by up to five years in prison, a fine, or both, if a health care provider “knowingly and willfully falsifies, conceals, or covers up” a material fact by any “trick, scheme, or device,” or makes “materially false, fictitious, or fraudulent statements or representations,” in connection with the delivery of health care services.
3
•
This statute only applies when a provider’s failure to disclose or refund an overpayment constitutes concealment of a material fact within the meaning of the statute. Given the broad scope of this statute, it arguably could be used by the government to impose a legal duty to disclose and/or refund an overpayment to any payer, particularly in the context of
Medicare Part A benefits.
•
•
•
This statute makes it a felony for any person to embezzle, steal, or
“knowingly convert ... to his use or the use of another,” a “thing of value of the United States or of any department or agency thereof.
The government has successfully prosecuted health care cases under
Section 641 only where the reimbursements were obtained fraudulently in the first instance. See United States v. O’ Brien , 14 F.3d 703, 705 (1 st
Cir.
1994) (convicting defendant of Section 641 offenses for regularly representing various Medicare recipients as bedridden, when, in fact, they were ambulatory, to maximize reimbursement); United States v. Siddiqi ,
959 F.2d 1167 (2 nd
Cir. 1992).
However, the government has successfully prosecuted non-healthcare cases under Section 641 where the recipients of a government overpayment did not act fraudulently in obtaining the overpayment, but should have recognized that they were not entitled to the funds. See
United States v. Irwin , 67 F.3d 670 (8 th
Cir, 1995) (defendant cashed check erroneously issued even though he knew that the government owed him a lesser amount); United States v. McRee , 7 F.3d 976 (11 th
Cir. 1993)
(although the IRS issues an assessment against the defendants, the IRS mistakenly sent a refund check to defendants.) These same theories could easily be applied to providers who knowingly fail to disclose overpayments.
CHIC_1256987.1
•
•
Section 669 makes it a felony punishable by a fine, imprisonment of up to ten years, or both for anyone to “knowingly and willfully” embezzle, steal, intentionally misapply or “otherwise without authority convert” any of the money, property, premium, or other assets of a “health care benefit program.”
In compliance guidance, the OIG has noted that this statute applies not only to Federal health care programs, but to most other types of health care benefit programs. See OIG Compliance Guidance for Individual and
Small Group Physicians , Appendix B (65 Fed. Reg. 59,434, 59,448
(October 5, 2000)).
4
•
Depending on the timing of the discovery of the overpayment by the provider, this statute could also lead to criminal liability for failure to disclose known overpayments.
•
•
•
•
Section 4 of Title 18 makes it a felony where “whoever having knowledge of the actual commission of a [federal felony], conceals and does not as soon as possible make known the same to some judge or other person in civil or military authority under the United States, shall be fined ... or imprisoned not more than three years or both.”
The elements of the crime are: (i) the principal committed and completed the alleged felony, (ii) that the defendant had full knowledge of that fact,
(iii) that the defendant failed to notify the authorities, and (4) that the defendant took an affirmative step to conceal the crime. U.S. v.
Ciambrome , 750 F.2d 1416 (9th Cir. 1985).
An affirmative step to conceal the felony is required for a violation of this statute and a mere failure to make the felony known does not suffice. U.S. v. Warters , 885 F.2d 1266 (5 th
Cir. 1989); U.S. v. Davila , 698 F.2d 715
(5 th
Cir. 1983).
In the context of a failure to disclose a known overpayment, there are many statements made by providers (such as those to auditors) which can be construed as an affirmative step to conceal the overpayment. This could thus be viewed as an unlawful concealment of a violation of 42
U.S.C. § 1320a-7b(a)(3) or any of the fraud statutes cited above.
•
•
This statute imposes criminal penalties upon those who knowingly and willfully make material false statements of fact, or conceal or cover up by trick, scheme or device a material fact to government agencies.
The same types of conduct that are prohibited by Section 1035 discussed above, are also typically prohibited under Section 1001.
II. CIVIL
•
Under the FCA, a person may be liable for knowingly submitting a false or fraudulent claim for payment to the government. In order to impose liability, the government must prove that a “false or fraudulent” claim was
“knowingly” submitted for payment or that a “false record or statement” was made in order to get a false claim paid or approved.
5
CHIC_1256987.1
CHIC_1256987.1
•
•
•
•
•
•
The term “knowingly” in this context means that a person has (a) “actual knowledge” or (b) “acts in deliberate ignorance of the truth or falsity of the information,” or (c) “acts in reckless disregard of the truth or falsity of the information.”
Liability under the FCA includes fines of not less than $5,500 nor more than $11,000 per claim, plus treble damages. FCA liability can also form the basis for administrative sanctions, including exclusion from the
Medicare program.
Even in instances where an overpayment is obtained innocently, meaning that the initial claim submitted was not false on its face, FCA liability can attach under Section 3729(a)(1) based on conduct occurring after discovery of the overpayment. For instance, at least two courts have held that the endorsement and deposit of a government check known to have been issued in error constitutes presentation of a false claim and may subject the recipient to liability under the FCA.
In addition, Section 3729(a)(7), which has become known as the “reverse false claim” provision, serves as a basis for liability if a person
“knowingly makes, uses, or causes to be made or used, a false record or statement to conceal, avoid, or decrease an obligation to pay or transmit money” to the government. Under this section, a fraudulent attempt to reduce an amount owed to the government could constitute a false claim.
Thus, if a provider retains money that it knows it owes to the government, the provider could be liable under Section 3729(a)(7). This argument seems particularly strong for Part A benefits in light of the language of 42
U.S.C. 1395g(a), which indicates that ongoing Medicare payments are to include “necessary adjustments on account of previously made overpayments or underpayments . . . .”
Many providers have been investigated and settled with the government under the FCA based on allegations that they failed to disclose and refund known overpayments, including Allina Health Systems ($16 million settlement), Kerlan-Jobe ($2.5 million settlement), and Montefiore
Medical Center ($12 million settlement).
The government has also sued providers for failing to inquire of false billings to other payors after discovering an error affecting one payor. For instance, Abington Memorial Hospital (“Abington”) repaid Medicaid in
1994 for certain improperly billed laboratory charges. Abington did not check to see if it received similar overpayments from Medicare. The federal government sued Abington arguing that its failure to inquire was an effort to keep itself deliberately ignorant of false billings. A trial in this case is upcoming.
6
•
•
Section 1866(a)(1)(C) of the Social Security Act (42 U.S.C. § 1395cc) requires hospitals and other health care providers to make adequate provisions to refund payments made by the federal government in error.
Providers are required to submit quarterly credit balance reports that identify improper or excess payments made to the provider, and refundable to Medicare. The reporting form contains a certification attesting to the completeness of the disclosed information. If the report identifies an overpayment, the provider is required to repay the Medicare program. Failure to appropriately report outstanding overpayments could be construed as a false statement subject to FCA liabilities or Civel
Monetary Penalties.
In 1998, a qui tam action was filed against Yale University alleging that the institution retained $500,000 in payments that should have been refunded to federal health care programs. United States ex rel. Jackson v.
Yale University School of Medicine , Civil No. 3:97CV02023 AWT (D.
Conn.). The University settled the action for more than $5 million in payments to various public and private insurers, and was required as part of a corrective action plan, to establish a credit balance department whose function was to resolve credit balances in a timely fashion.
•
State unclaimed property (or escheat) laws also impose obligations on providers to pay to the state any amounts which the provider is unable to refund to a patient or third party payor within a specified period of time.
Most states have adopted the Uniform Unclaimed Property Act or the
Uniform Disposition of Unclaimed Property Act, with variations although some states have enacted their own unclaimed property statute. It is important to note that these laws do not simply require providers to attempt to locate the owners of overpayments or credit balances. If those owners cannot be located and the funds repaid, these laws require that the funds be paid to the state pursuant to specific procedures. These state unclaimed property laws typically contain a number of complex provisions that describe in detail the duty of the provider to attempt to locate the owner, file reports with, and make refunds to, the state. The laws also detail the penalties for non-compliance.
III. CONSEQUENCES
A. Prison, fines, restitution
C.
D.
Exclusion from the Medicare Program
Civil Monetary Penalties
7
CHIC_1256987.1
F.
G.
Loss of Civil Rights, including the right to vote, to possess a gun, etc.
Statutory Bars to Employment in Certain Industries, including Insurance, Labor
IV. AVOIDING CORPORATE PROSECUTION THROUGH DISCLOSURE
A.
On January 20, 2003, Deputy Attorney General Larry D. Thompson issued to federal prosecutors revised guidelines concerning the criminal prosecution of business organizations (the “Thompson Memorandum”).
B.
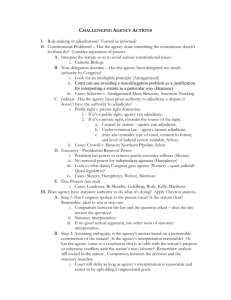
According to the Thompson Memorandum, prosecutors should apply the same factors in determining whether to charge a corporation as they do with respect to individuals. However, given the nature of the corporate "person," the Thompson Memorandum observes that some additional factors are present. As such, prosecutors in conducting an investigation, determining whether to bring charges, and negotiating plea agreements prosecutors should consider the following nine additional factors in reaching a decision as to the proper treatment of a corporate target:
•
The nature and seriousness of the offense, including the risk of harm to the public, and applicable policies and priorities, if any, governing the prosecution of corporations for particular categories of crime;
•
The pervasiveness of wrongdoing within the corporation, including the complicity in, or condonation of, the wrongdoing by corporate management;
•
The corporation's history of similar conduct, including prior criminal, civil, and regulatory enforcement actions against it;
•
The corporation's timely and voluntary disclosure of wrongdoing and its willingness to cooperate in the investigation of its agents, including, if necessary, the waiver of corporate attorney-client and work product protection;
•
•
The existence and adequacy of the corporation's compliance program;
The corporation's remedial actions, including any efforts to implement an effective corporate compliance program or to improve an existing one, to replace responsible management, to discipline or terminate wrongdoers, to pay restitution, and to cooperate with the relevant government agencies;
•
Collateral consequences, including disproportionate harm to shareholders, pension holders and employees not proven personally culpable and impact on the public arising from the prosecution;
•
The adequacy of the prosecution of individuals responsible for the corporation's malfeasance; and
8
CHIC_1256987.1
•
The adequacy of remedies such as civil or regulatory enforcement actions.
C.
The new guidelines place greater emphasis on a corporation's cooperation and voluntary disclosure of wrongdoing. Section VI of the Thompson Memorandum describes the government's current view on what does and does not constitute cooperation and voluntary disclosure by a corporation. In particular, the new guidelines call for corporations:
•
To conduct internal investigations and to disclose their findings to the appropriate authorities;
•
To waive, under appropriate circumstances, the attorney-client and work product protections, both with respect to its internal investigation and with respect to communications between specific officers, directors, and employees and counsel;
•
To refrain from appearing to protect its culpable employees and agents, by, among other things, advancing attorneys' fees to individual targets, retaining the culpable employees without sanction for their misconduct, or providing information to the employees pursuant to a joint defense agreement; and
•
To avoid any conduct that impedes the government's investigation, including overly broad assertions of corporate representation of employees or former employees; inappropriate directions to employees or their counsel, such as directions not to cooperate openly and fully with the investigation . . . ; the direction to decline to be interviewed; making presentations or submissions that contain misleading assertions or omissions; incomplete or delayed production of records; and the failure to promptly disclose illegal conduct known to the corporation.
* * * * *
CHIC_1256987.1
9