the 2014 Annual Meeting Scientific Abstract Listing
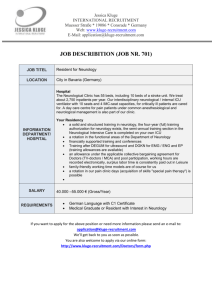
advertisement

Scientific Abstract Listing and Annual Meeting Information April 26 – May 3, 2O14 Philadelphia, PA Connecting All of Neurology Early Registration Deadline: April 3, 2O14 The 66th AAN Annual Meeting Experience breakthrough research, exceptional education programs, and boundless networking opportunities at the AAN Annual Meeting in Philadelphia, PA, April 26–May 3, 2014. 2O14 Deadlines-At-A-Glance Location ¡¡ March 26, 2014: Annual Meeting Hotel Reservation Deadline ¡¡ Pennsylvania Convention Center Philadelphia, PA ¡¡ April 3, 2014: Annual Meeting Early Registration Deadline Headquarter Hotel ¡¡ Marriott Philadelphia Downtown Future Annual Meeting Dates and Locations ¡¡ Washington, DC April 18-25, 2015 ¡¡ Vancouver, BC, Canada April 16-23, 2016 ¡¡ Boston, MA April 22-29, 2017 RED: 14AM Register Online Ad Place in AANnews and Others? 8.25 x 5.4375 4C + Bleed Search, Find, and Register Online Customize Your Week with Easy Online Registration With online registration, you can: Register Book your hotel Plan your itinerary Search for programs by topic or day New! Choose the “Buy All” option to purchase all education courses at one flat rate! AAN.com/view/AM14 Table of Contents Introduction Thursday, May 1 Connecting All of Neurology . . . . . . . . . . . 2 Make the Meeting Your Own . . . . . . . . . . . . . . 3 About Program Listings . . . . . . . . . . . . . . . . 4 What’s Included with Your Registration? . . . . . 6 Look What’s New for 2014 . . . . . . . . . . . . 8 See What’s Back by Popular Demand . . . . . . . . . . 9 Meeting Schedule Overviews Meeting-at-a-Glance . . . . . . . . . . . . . . 10 Scientific Sessions-at-a-Glance . . . . . . . . . 14 2014 Award Recipients . . . . . . . . . . 2014 Research Fellowships . . . . . . . . Annual Meeting Program Schedule . Annual Meeting Programs by Topic . . . . . . . . . . . . . . . . . . . . . 18 . 22 . 24 . 34 Sunday, April 27 Poster Session VI . . . . . . . . . . . . . . . . . . 104 Frontiers in Neuroscience Plenary Session �����������112 Scientific Sessions . . . . . . . . . . . . . . . . . 114 Integrated Neuroscience Sessions . . . . . . . . . . . 116 Poster Session VII . . . . . . . . . . . . . . . . . 118 Scientific Sessions . . . . . . . . . . . . . . . . . 126 Controversies in Neurology Plenary Session �������128 Friday, May 2 Integrated Neuroscience Session . . . . . . . . . . . 130 Clinical Trials Plenary Session��������������������������������������131 Section Topic Controversies/ Integrated Neuroscience . . . . . . . . . . . . . . . 132 Neurology Year in Review Plenary Session . . . 133 Other Interests Integrated Neuroscience Sessions/ Section Topic Controversies . . . . . . . . . . . . . . 42 Poster Session Floor Plan . . . . . . . . . . . . 47 Poster Session I . . . . . . . . . . . . . . . . . . 48 Tuesday, April 29 Poster Session II . . . . . . . . . . . . . . . . . . 56 Presidential Plenary Session ������������������������������������������ 64 Section Topic Controversies . . . . . . . . . . . . . . 65 Scientific Sessions . . . . . . . . . . . . . . . . . 66 Integrated Neuroscience Sessions . . . . . . . . . . . 68 Poster Session III . . . . . . . . . . . . . . . . . . 70 Scientific Sessions . . . . . . . . . . . . . . . . . 78 Hot Topics Plenary Session ��������������������������������������������� 80 2O14 Annual Meeting On Demand . . . . . . . 134 Connect at Social Events . . . . . . . . . . . . 136 Highlights for Students, Residents, and Fellows . 138 Registration and Meeting Information General Information . . . . . . . . . . . . . . 140 Registration . . . . . . . . . . . . . . . . . . . 144 Hotel Reservations . . . . . . . . . . . . . . . 146 Hotel Map and Amenities . . . . . . . . . . . 148 Travel Information . . . . . . . . . . . . . . . . . 150 Exhibitor Listing . . . . . . . . . . . . . . . . . . 152 66th Annual Meeting Committee Members . . . . . . . 155 Meeting Information and Contacts . . . . . . . . . . . 158 Wednesday, April 30 Poster Session IV . . . . . . . . . . . . . . . . . . 81 Contemporary Clinical Issues Plenary Session����� 89 Scientific Sessions . . . . . . . . . . . . . . . . . 90 Integrated Neuroscience Sessions . . . . . . . . . . . 92 Poster Session V . . . . . . . . . . . . . . . . . . 94 Platform Blitzes . . . . . . . . . . . . . . . . . . 102 Fast, Easy Registration Online · AAN.com/view/AM141 Connecting All of Neurology “Welcome to the 66th AAN Annual Meeting! As the world’s largest gathering of neurologists, the AAN Annual Meeting has a long history of connecting all of neurology by bringing together the latest research on the most critical topics facing neurologists. In fact, the meeting not only attracts scientists from around the globe, but it also garners coverage from world-leading media outlets such as the New York Times, Wall Street Journal, USA Today, CNN, NPR, and more. The Annual Meeting is also the go-to place for unparalleled education programming, connecting neurology professionals to nearly 180 courses on 18 topics of interest. With top-tier programming going on every day, all week long, the Annual Meeting is designed to offer customized convenience, no matter what your schedule. So whether you come for a few days—or stay for all eight, you’re bound to have a great experience and leave feeling an even deeper connection to the world of neurology. I look forward to seeing you in historic Philadelphia.” Stefan M. Pulst, MD, FAAN Chair, Meeting Management Committee Key Dates and Deadlines: Hotel Reservation Deadline: Location March 26, 2014 Early Registration Deadline: Pennsylvania Convention Center Philadelphia, PA April 3, 2014 Headquarter Hotel 66th AAN Annual Meeting: Marriott Philadelphia Downtown April 26 –May 3, 2014 Visit AAN.com/view/AM14 Make the Meeting Your Own On Your Schedule The AAN Annual Meeting is designed to be completely customizable so you can make the experience all your own—and on the schedule that works best for you and/or your practice. Consider how your practice might get the most out of this year’s meeting: send half your staff for the first few days, then the other for the remainder of the meeting. With so many exceptional education programs and scientific sessions available in a variety of subspecialties, plus unparalleled networking opportunities—all week long—the AAN Annual Meeting can be tailored to be a perfect fit for you no matter what your interest, career stage, or schedule. ¡¡ For Students and Junior Members The Annual Meeting is essential, providing exposure to a variety of interests, career disciplines, and opportunities to network. ¡¡ For Neurologists The Annual Meeting is the place for top CME programming, breakthrough scientific research, and opportunities to collaborate with neurology’s thought leaders from around the world. ¡¡ For Other Physicians and Advanced Practice Providers The Annual Meeting is ideal for comprehensive updates on the latest advances in the science and treatment of patients with common neurologic conditions such as dementia, stroke, migraine, MS, and more. Fast, Easy Registration Online · AAN.com/view/AM14 3 About Program Listings The program listing has changed for the better Please refer to the key for the following program definitions: C Course (paid education program) CQ Colloquium (education program included with meeting registration) H I P S Highlights in the Field (section-provided overview in their subspecialty or topic of interest) Subspecialty in Focus Track The Subspecialty in Focus Track is a series of six special, intensive topic-specific tracks designed for subspecialists, combining an education course with an Integrated Neuroscience Session. The tracks are divided into a morning and an afternoon portion in a single day. Refer to the Meeting Events Schedule for specific times. Look for the Subspecialty in Focus icons ( ) to identify the tracks of your choice. Integrated Neuroscience Session (scientific session combining invited speakers, data blitz, and poster discussion; included with meeting registration) Poster Session (a hall of posters on a variety of topics. Posters are displayed for 3½ hours, authors will be present for 90 minutes) Scientific Platform Session (didactic session featuring abstracts) New Program Feature Icons These new icons will alert you to features of the program experience: The program is part of a Subspecialty in Focus track The program is included with your registration A registration fee is required The program is one of the AAN Leadership Development sessions Cerebrovascular Disease Sunday, April 27 C33 Prevention of Cardioembolic Stroke in Patients with Nonvalvular Atrial Fibrillation: Recommendations Based on Evidence-based Guidelines and Recent Randomized Trials . . 24 I2 New Antithrombotic Agents for Stroke Prevention . . . . . . . . . . . . . . . 43 Epilepsy Sunday, April 27 C51 Algorithms in the Diagnosis and Treatment of Epilepsy . . . . . . . . . . . . . 25 I1 Temporal Lobe Epilepsy and Febrile Seizures . . . . . . . . . . . . . . . . 42 Child Neurology Monday, April 28 C68 Stroke in Childhood and Adolescence . . . . 25 I4 Recent Advances in Translational Research in Autism . . . . . . . . . . . . . . 45 Sleep Disorders Monday, April 28 C84 Sleep Principles Applied to Neurological Disease . . . . . . . . . . . . . 26 I3 Clocks, Sleep, Brain Health and Disorders: Impact on Mechanism, Expression, and Treatment . . . . . . . . . . . . . . . . . . . 44 Sports Neurology/Government Services Friday, May 2 C142 Concussion in the Military and in Sports . . . 31 I12 Concussion in Sports and the Military . . . 132 Geriatric Neurology Friday, May 2 C153 Imaging and Genomics for Detecting Neurodegenerative Proteinopathy in Clinical Practice . . . . . . . . . . . . . . . . 31 I11 4 2O14 Scientific Abstract Listing and Annual Meeting Information Proteinopathy in Neurodegenerative Disease . . . . . . . . 130 April 26–May 3, 2O14 Philadelphia, PA One Flat Rate and the Entire Education Program is Yours NEW! Registration Buy All option includes access to all the exceptional 2014 Annual Meeting education courses*—in a wide variety of topics—for one flat rate. A great value in CME programming. Select the Buy All Registration Package when you register. Register today at AAN.com/view/AM14. * Skills Workshops and Skills Pavilions excluded from Buy All pricing. Attendee must identify courses to be included as part of “Buy All” purchase. Courses are subject to closure due to reaching maximum capacity. Buy All registration option is only available prior to early registration deadline of April 3, 2014. What’s Included with Your Registration? When planning your week, be sure and take advantage of these FREE education, scientific, practice, advocacy programs, and social events—going on all week long and at no additional cost to you! FREE Programs to help you: Stay current with the latest research and scientific sessions Enhance your practice with educational colloquia Network with colleagues Participate in Academy business Saturday, April 26 CQ1 BRAINS Colloquium: Understanding and Improving Your Bottom Line 2:00 p.m.–5:00 p.m. Sunday, April 27 I1 Temporal Lobe Epilepsy and Febrile Seizures 8:00 a.m.–12:00 p.m. CQ2 Research and Technology Colloquium: From Discovery to Therapy 8:00 a.m.–12:00 p.m. CQ3 Patient Safety Colloquium 9:00 a.m.–12:00 p.m. S1 Section Topic Controversies: ICU EEG Monitoring—Seizures in Critically Ill Patients 1:00 p.m.–2:30 p.m. CQ4 Clinical Research Colloquium 1:00 p.m.–5:00 p.m. I2 New Antithrombotic Agents for Stroke Prevention 1:00 p.m.–5:00 p.m. CQ5 Practice Colloquium: How to Navigate and Succeed in New Payment Models 2:00 p.m.–5:00 p.m. Opening Party 6:00 p.m.–10:00 p.m. Monday, April 28 C61 Residents and Fellows Career Breakfast: The Early Years (registration required) 6:30 a.m.–8:30 a.m. A AN/AANI Business Meeting 8:00 a.m.–8:30 a.m. I3 Clocks, Sleep, Brain Health and Disorders: Impact on Mechanism, Expression, and Treatment 8:00 a.m.–12:00 p.m. 6 CQ6 Education Colloquium 8:30 a.m.–12:00 p.m. Government Relations Committee Meet and Greet 12:00 p.m.–1:30 p.m. S2 Cancelled Exhibit Hall Opening Reception 4:30 p.m.–6:30 p.m. Student Interest Group in Neurology (SIGN) Meeting 4:30 p.m.–6:30 p.m. Consortium of Neurology Residents and Fellows Meeting 5:00 p.m.–6:30 p.m. Residents and Fellows Career Forum and Reception 6:30 p.m.–9:00 p.m. Tuesday, April 29 I4 Recent Advances in Translational Research in Autism 1:00 p.m.–5:00 p.m. AAN/ABPN MOC Informational Session 1:30 p.m.–3:00 p.m. CQ7 Education Research Colloquium 2:00 p.m.–4:30 p.m. CQ8 Health Information Technology Colloquium: Advancements in Technology 2:00 p.m.–5:00 p.m. P1 Poster Session I 3:00 p.m.–6:30 p.m. 2O14 Scientific Abstract Listing and Annual Meeting Information P2 Poster Session II 7:30 a.m.–11:00 a.m. Presidential Plenary Session 9:00 a.m.–12:00 p.m. Exhibit Hall 11:30 a.m.–5:00 p.m. S3 Section Topic Controversies: PFO: Aggressive Treatment or Just Aspirin 1:00 p.m.–2:30 p.m. S4–S13 Scientific Platform Sessions 1:00 p.m.–2:45 p.m. I5 Revolution of Genetic Tools and the Impact on Neurology 1:00 p.m.–5:00 p.m. I6 Peripheral Neuropathies 1:00 p.m.–5:00 p.m. P3 Poster Session III 3:00 p.m.–6:30 p.m. S14–S23 Scientific Platform Sessions 3:15 p.m.–5:00 p.m. Hot Topics Plenary Session 5:30 p.m.–6:30 p.m. Subspecialty in Focus Track Included with registration Registration fee required Wednesday, April 30 Thursday, May 1 P4 Poster Session IV 7:30 a.m.–11:00 a.m. Contemporary Clinical Issues Plenary Session 9:00 a.m.–12:00 p.m. Exhibit Hall 11:30 a.m.–5:00 p.m. S24–S33 Scientific Platform Sessions 2:00 p.m.–3:45 p.m. I7 Emerging Therapeutic Advances in Multiple Sclerosis 2:00 p.m.–6:00 p.m. I8 Clinical Decision Making After the Dust Settles on Clinical Trials 2:00 p.m.–6:00 p.m. P5 Poster Session V 3:00 p.m.–6:30 p.m. S34–S43 Platform Blitzes 4:00 p.m.–5:45 p.m. Current Practice Issues in Neurology 5:30 p.m.–7:00 p.m. Highlights in the Field Sessions 6:00 p.m.–7:00 p.m. Emerging Science Session 6:00 p.m.–7:30 p.m. P6 Poster Session VI 7:30 a.m.–11:00 a.m. Frontiers in Neuroscience Plenary Session 9:00 a.m.–12:00 p.m. Exhibit Hall 11:30 a.m.–3:00 p.m. S44–S53 Scientific Platform Sessions 1:00 p.m.–2:45 p.m. I9 Emerging Concepts in Headache Therapy 1:00 p.m.–5:00 p.m. I10 The Global Burden of Neurological Diseases 1:00 p.m.–5:00 p.m. P7 Poster Session VII 3:00 p.m.–6:30 p.m. S54–S63 Scientific Platform Sessions 3:15 p.m.–5:00 p.m. Highlights in the Field Sessions 5:30 p.m.–6:30 p.m. Controversies in Neurology Plenary Session 5:30 p.m.–7:00 p.m. Friday, May 2 I11 Proteinopathy in Neurodegenerative Disease 8:00 a.m.–12:00 p.m. Clinical Trials Plenary Session 12:00 p.m.–1:30 p.m. S64 Section Topic Controversies: Pain: Methods of Treatment 1:00 p.m.–2:30 p.m. I12 Concussion in Sports and the Military 1:00 p.m.–5:00 p.m. Neurology Year in Review Plenary Session 5:30 p.m.–7:00 p.m. Closing Party 7:30 p.m.–9:00 p.m. Extend Your Experience with These Annual Meeting Resources Academy Central: Your one-stop shop for AAN products, services, and more American Brain Foundation: Support cures for brain disease and see the future of neurology Neurology Career Center in Academy Central and the Exhibit Hall: Meet employers, search for jobs, and get career tools Resident/Medical Student Rush Line: Free education program tickets, first-come, first-served Annual Meeting Mobile App: Lite version available now. Full version available March 2014. Annual Meeting On Demand: The digital library of content from the 2014 AAN Annual Meeting educational programs Residents’ Experience: A unique place to network, find information, and participate in informal presentations specifically geared to those in the early stages of their career International Experience: New! Provides an opportunity for international attendees to network and participate in discussions on a variety of topics Fast, Easy Registration Online · AAN.com/view/AM14 7 Look What’s New for 2014 Buy All Registration Option Meet to Eat Take advantage of this new option to purchase all your favorite education courses for one flat rate! Hurry—the BUY ALL* option is only available until the April 3 early registration deadline. See page 144 for more information, including Buy All exclusions and price. You’ll notice something new in the poster sessions this year: A selection of posters will be presented on large monitors, to allow authors to best highlight visually compelling elements such as images and videos. Looking for another way to network with other neurology professionals? Try a Meet to Eat event Monday, April 28–Thursday, May 1. Meet to Eat events facilitate a gathering of attendees in a casual dinner setting. Choose one of the four nights and the AAN will make a 7:00 p.m. dinner reservation for you and other AAN Annual Meeting attendees who signed up for the same night at one of Philadelphia’s highly recommended restaurants. Meet new people, make new connections, and enjoy a great meal! This service is free of charge; attendees are responsible for the cost of the meal. Please contact Kristine Mitchell at (612) 928-6062 or kmitchell@aan.com for more information. Clinical Research Track Platform Blitzes For attendees interested in a research career, the AAN has organized a track of programs with that emphasis. Utilizing a similar format to the popular Emerging Science Session, these dynamic sessions will feature five-minute author presentations followed by five-minutes of questions and answers. The session will conclude with all authors participating in a panel discussion. New Digital ePosters More Opportunities to Network ¡¡ The hour between 12:00 p.m. and 1:00 p.m. will be free from courses and sessions each day, making it easy for you to find time to meet with colleagues ¡¡ Connect with colleagues before, during, and after the meeting with the Annual Meeting LinkedIn Group at AAN.com/view/AMLinkedIn . ¡¡ The International Experience provides a place for international attendees to gather, network, and participate in discussions on a variety of topics. The International Experience is open Saturday, April 26 through Friday, May 2. * Skills Workshops and Skills Pavilions excluded from BUY ALL pricing. Attendee must identify courses to be included as part of “BUY ALL” purchase. Courses are subject to closure due to reaching maximum capacity. BUY ALL registration option is only available prior to early registration deadline of April 3, 2014. 8 2O14 Scientific Abstract Listing and Annual Meeting Information See What’s Back by Popular Demand These always-popular scientific programs are included free with your registration! Section Topic Controversies Integrated Neuroscience Sessions (INS) AAN Sections will debate controversies related to a specific Sectionrelated topic. This format will feature two speakers arguing a side of the topic, followed by a rebuttal and question and answer period. These well-attended sessions offer an in-depth look at subspecialty areas using a variety of presentations, including data blitz sessions, poster rounds, and invited speaker sessions. AAN Plenary Sessions Get essential updates covering the past year in your subspecialty or topic of interest. Sections will provide overviews in their areas, featuring scientific and educational abstracts, journal articles, subspecialty society updates, tips, resources, and more. AAN Plenary Sessions are the signature scientific sessions of the Annual Meeting covering critical issues, hot topics, highlights, and significant advances in neurology from the last year. This year’s sessions showcase an outstanding lineup of premier lecturers, chosen by their peers. Join us as they address the latest controversies, breakthroughs, and advances in neuroscience. Sessions run Tuesday, April 29 through Friday, May 2. Scientific Poster and Platform Sessions Poster Session QR Codes Browse more than 2,500 poster and platform presentations covering the latest research on a wide range of interest areas in neurology. Sessions run Monday, April 28 through Thursday, May 1. The QR code is one of the most popular types of two-dimensional barcodes. The QR tag can be scanned by smart phones or tablets and will link the attendee to the selected poster via AAN’s mobile access. Once the QR tag is scanned, the attendee’s mobile device will link to the poster title, authors, and links to the abstract, poster PDF, and audio file. An attendee can scan a multitude of posters to see the corresponding content. Highlights in the Field **Please note that each poster presenter needs to provide permission for his or her poster information to be accessible in the online poster viewing site. Fast, Easy Registration Online · AAN.com/view/AM14 9 Meeting Schedule Overviews Meeting-at-a-Glance Saturday April 26 Sunday April 27 6:00 a.m. C20–C26 6:30 a.m.–8:00 a.m. 7:00 a.m. 8:00 a.m. C27–C35 C1–C4 CQ2 8:00 a.m.–12:00 p.m. 8:00 a.m.–12:00 p.m. 8:00 a.m.–12:00 p.m. Integrated Neuroscience 8:00 a.m.–12:00 p.m. 9:00 a.m. C5–C7 C36 9:00 a.m.–5:00 p.m. 9:00 a.m.–12:00 p.m. 9:00 a.m.–12:00 p.m. 9:00 a.m.–5:00 p.m. CQ3 10:00 a.m. C37–C41 C42–C44 10:00 a.m.–12:00 p.m. 11:00 a.m. 12:00 p.m. OPEN HOUR 12:00 p.m.–1:00 p.m. 1:00 p.m. C8–C11 1:00 p.m.–5:00 p.m. S1 CQ4 C45–C53 Integrated Section Topic 1:00 p.m.–5:00 p.m. 1:00 p.m.–5:00 p.m. Neuroscience 1:00 p.m.–5:00 p.m. Controversies 1:00 p.m.–2:30 p.m. 2:00 p.m. 3:00 p.m. OPEN HOUR 12:00 p.m.–1:00 p.m. CQ1 CQ5 2:00 p.m.–5:00 p.m. 2:00 p.m.–5:00 p.m. C12–C19 3:00 p.m.–5:00 p.m. 4:00 p.m. 5:00 p.m. 6:00 p.m. Opening Party 6:00 p.m.–10:00 p.m. 7:00 p.m. 8:00 p.m. Current as of 2/10/2014 –Programs and dates are subject to change Monday April 28 Tuesday April 29 C54–C60 C61 C89–C94 6:30 a.m.–8:00 a.m. 6:30 a.m.–8:30 a.m. (Free, Registration Required) 6:30 a.m.–8:00 a.m. State Society Leadership Roundtable 6:30 a.m.–8:30 a.m. 7:00 a.m.–8:30 a.m. AAN/AANI Business Mtg C62–68 8:00 a.m.–8:30 a.m. 8:00 a.m.–12:00 p.m. CQ6 Run/Walk for Brain Research Integrated Neuroscience P2 Poster Session II 7:30 a.m.–11:00 a.m. 8:00 a.m.–12:00 p.m. 8:30 a.m.–12:00 p.m. C69–70 C71–C76 9:00 a.m.–12:00 p.m. 9:00 a.m.–5:00 p.m. Presidential Plenary Session C77 9:00 a.m.–12:00 p.m. 9:30 a.m.–12:00 p.m. C78–C79 10:00 a.m.–12:00 p.m. Exhibit Hall 11:30 a.m.–5:00 p.m. OPEN HOUR 12:00 p.m.–1:00 p.m. S2 Cancelled C80–C85 CQ7 CQ8 C86–C87 2:00 p.m.–4:30 p.m. 2:00 p.m.–5:00 p.m. 2:00 p.m.–5:00 p.m. 1:00 p.m.–5:00 p.m. Integrated Neuroscience 1:00 p.m.–5:00 p.m. Government Relations Committee Meet & Greet 12:00 p.m.–1:30 p.m. AAN/ABPN MOC Informational Session OPEN HOUR 12:00 p.m.–1:00 p.m. S3 S4–S13 C95–C99 Integrated Section Topic 1:00 p.m.–2:45 p.m. 1:00 p.m.–5:00 p.m. Neuroscience 1:00 p.m.–5:00 p.m. Controversies 1:00 p.m.–2:30 p.m. C100 2:00 p.m.–5:00 p.m. 1:30 p.m.–3:00 p.m. P1 Poster Session I 3:00 p.m.–6:30 p.m. P3 Poster Session III S14–S23 3:15 p.m.–5:00 p.m. 3:00 p.m.–6:30 p.m. Exhibit Hall Opening Reception 4:30 p.m.–6:30 p.m. Hot Topics Plenary Session 5:30 p.m.–6:30 p.m. Residents and Fellows Career Forum and Reception 6:30 p.m.–9:00 p.m. Corporate Therapeutic Updates 7:00 p.m.–10:00 p.m. Paid Programs/Events Programs/Events Included with Registration Additional Events Meeting-at-a-Glance Wednesday April 30 Thursday May 1 C101–C107 C114–C119 6:30 a.m.–8:00 a.m. 6:30 a.m.–8:00 a.m. 6:00 a.m. 7:00 a.m. 8:00 a.m. P4 Poster Session IV P6 Poster Session VI 7:30 a.m.–11:00 a.m. 9:00 a.m. 7:30 a.m.–11:00 a.m. Contemporary Clinical Issues Plenary Session Frontiers in Neuroscience Plenary Session 9:00 a.m.–12:00 p.m. 9:00 a.m.–12:00 p.m. 10:00 a.m. 11:00 a.m. Exhibit Hall 12:00 p.m. 1:00 p.m. Exhibit Hall 11:30 a.m.–5:00 p.m. AAN/American Brain Foundation Awards Luncheon 11:30 a.m.–3:00 p.m. OPEN HOUR OPEN HOUR 12:00 p.m.–1:00 p.m. 12:00 p.m.–1:30 p.m. S44–S53 C120–C123 Integrated 1:00 p.m.–5:00 p.m. Neuroscience 1:00 p.m.–2:45 p.m. 1:00 p.m.–5:00 p.m. 2:00 p.m. S24–S33 C108–113 2:00 p.m.–3:45 p.m. 2:00 p.m.–6:00 p.m. C124–125 Integrated Neuroscience 2:00 p.m.–5:00 p.m. 2:00 p.m.–6:00 p.m. 3:00 p.m. P5 Poster Session V 3:00 p.m.–6:30 p.m. 4:00 p.m. Current Practice Issues in Neurology Highlights in the Field Sessions 6:00 p.m.–7:00 p.m. Corporate Therapeutic Updates 7:00 p.m.–10:00 p.m. 8:00 p.m. 3:15 p.m.–5:00 p.m. 3:00 p.m.–6:30 p.m. 4:00 p.m.–5:45 p.m. 5:30 p.m.–7:00 p.m. 7:00 p.m. S54–S63 S34–S43 Platform Blitzes 5:00 p.m. 6:00 p.m. P7 Poster Session VII Emerging Science Session 6:00 p.m.–7:30 p.m. Highlights in the Field Sessions 5:30 p.m.–6:30 p.m. Controversies in Neurology Plenary C126–131 Session 6:00 p.m.–9:00 p.m. 5:30 p.m.–7:00 p.m. Current as of 2/10/2014 –Programs and dates are subject to change Friday May 2 Saturday May 3 C132–C137 C154–C158 C159 6:30 a.m.–8:00 a.m. 6:30 a.m.–8:00 a.m. C138–C142 Integrated 8:00 a.m.–12:00 p.m. Neuroscience C160–C165 6:30 a.m.–8:30 a.m. 8:00 a.m.–12:00 p.m. 8:00 a.m.–12:00 p.m. C143–C148 C166 9:00 a.m.–5:00 p.m. 9:00 a.m.–12:00 p.m. C167–169 10:00 a.m.–12:00 p.m. Clinical Trials Plenary Session 12:00 p.m.–1:30 p.m. OPEN HOUR 12:00 p.m.–1:00 p.m. S64 C149–C153 Integrated 1:00 p.m.–5:00 p.m. Neuroscience Section Topic 1:00 p.m.–5:00 p.m. Controversies 1:00 p.m.–2:30 p.m. Neurology Year in Review Plenary Session 5:30 p.m.–7:00 p.m. Paid Programs/Events Closing Party 7:30 p.m.–9:00 p.m. Programs/Events Included with Registration Additional Events Scientific Sessions-at-a-Glance Sunday, April 27, 2014 S8 8:00 a.m.–12:00 p.m. I1 Temporal Lobe Epilepsy and Febrile Seizures . . . . . . . . . . . . 42 1:00 p.m.–2:30 p.m. S1 Section Topic Controversies: ICU EEG Monitoring: Seizures in Critically Ill Patients . . . . . . . . . . 42 S9Sleep ¡¡ Presentation of the Sleep Science Award ¡¡ Presentation of the Wayne A. Hening Sleep Medicine Investigator Award 1:00 p.m.–5:00 p.m. I2 New Antithrombotic Agents for Stroke Prevention . . . . . . . . . 43 S10 Monday, April 28, 2014 8:00 a.m.–12:00 p.m. I3 Clocks, Sleep, Brain Health and Disorders: Impact on Mechanism, Expression, and Treatment . . . . . . . . . . . . . . . . 44 1:00 p.m.–2:30 p.m. S2 Cancelled 1:00 p.m.–5:00 p.m. I4 Recent Advances in Translational Research in Autism . 45 3:00 p.m.–6:30 p.m. P1 Poster Session I . . . . . . . . 48–55 Tuesday, April 29, 2014 7:30 a.m.–11:00 a.m. P2 Poster Session II . . . . . . . . 56-63 9:00 a.m.–12:00 p.m. Presidential Plenary Session . . . . . . . . . . . . . 64 Features the AAN’s premier lecture awards for clinically relevant research and a presentation by a leading lecturer. Top researchers speak on some of the most significant findings in neurology in 2014. 1:00 p.m.–2:30 p.m. S3 Section Topic Controversies: PFO: Aggressive Treatment or Just Aspirin . . . . . . . . . . . . . 65 1:00 p.m.–2:45 p.m. Scientific Platform Sessions . . . 66–67 S4 MS and CNS Inflammatory Disease: Clinical Trials S5 Cerebrovascular Disease and Interventional Neurology: Pre-hospital, Telemedicine, and Related Topics S6 Neuromuscular Disease: Gene Therapy S7 Parkinson’s Disease: Preclinical and Clinical Therapeutics Aging, Dementia, and Cognitive and Behavioral Neurology: PET Imaging ¡¡ Presentation of the Potamkin Prize for Research in Pick’s, Alzheimer’s Disease, and Related Diseases HIV, PML, and Cerebral Malaria ¡¡ Presentation of the Bruce S. Schoenberg International Award in Neuroepidemiology S11 Neuro Trauma, Critical Care, and Sports Neurology Cerebrovascular Disease and Interventional Neurology: Epidemiology and Risk Factors S13 MS and CNS Inflammatory Disease: MRI Atrophy Measures and Correlations 1:00 p.m.–5:00 p.m. I5 Revolution of Genetic Tools and the Impact on Neurology . . . 68 1:00 p.m.–5:00 p.m. I6 Peripheral Neuropathies . . . . . 69 3:00 p.m.–6:30 p.m. P3 Poster Session III . . . . . . . . 70–77 3:15 p.m.–5:00 p.m. Scientific Platform Sessions . . . 78–79 S14 MS and CNS Inflammatory Disease: Animal and In Vitro Studies S15 Cerebrovascular Disease and Interventional Neurology: Clinical and Imaging Biomarkers and Genetics S16 Neuromuscular and Clinical Neurophysiology (EMG): Clinical Trials and Therapy S17 Parkinson’s Disease: Genetics and Epidemiology S18 Aging, Dementia, and Cognitive and Behavioral Neurology: Behavioral Neuroscience S19 Neuro-ophthalmology/Neuro-otology I S20 Pain and Palliative Care ¡¡ Presentation of the Mitchell B. Max Award for Neuropathic Pain S12 S21 Neurorehabilitation and Neural Repair iPosters, a virtual poster hall, that transforms your poster hall into an online and mobile experience—both during a meeting and long after. ¡¡ Online, interactive, fully searchable poster database with the ability to magnify the poster content for detailed viewing, contact the author directly with comments or questions, bookmark posters for easy access on return visits, and much more. 14 ¡¡ New this year: Poster authors have the ability to record a 5- to 7-minute summary of their poster. This summary will be linked to the author’s iPoster submission and will give viewers the ability to hear about the poster from the author, in addition to viewing at it. 2O14 Scientific Abstract Listing and Annual Meeting Information S22Neuro-oncology S23 MS and CNS Inflammatory Disease: Novel Therapeutics ¡¡ Presentation of the John Dystel Prize for Multiple Sclerosis Research 5:30 p.m.–6:30 p.m. Hot Topics Plenary Session . . . . . . . . . . . . . . 80 Features translational research related to clinical issues of importance. Four outstanding physician-scientists provide summaries of their recent research findings and describe the clinical implications of the results. Wednesday, April 30, 2014 7:30 a.m.–11:00 a.m. P4 Poster Session IV . . . . . . . . 81–88 9:00 a.m.–12:00 p.m. Contemporary Clinical Issues Plenary Session . . . . . . . . . . . . . . . . . . . . . . 89 Highlights issues most critical to practicing neurologists, including abstracts related to new therapeutic developments, clinical applications of basic and translational research, and innovative technical developments. Commentary and discussion follow each presentation. 2:00 p.m.–3:45 p.m. Scientific Platform Sessions . . . 90–91 S24 Diet and Hormonal Influences in MS S25 Cerebrovascular Disease and Interventional Neurology: Hemorrhage, Aneurysms, and Vascular Malformations S26 Biomarkers in Neuromuscular Diseases S27 Dystonia, Tremor, and Other Movement Disorders ¡¡ Presentation of the Movement Disorders Research Award S28 Aging, Dementia, and Cognitive and Behavioral Neurology: Dementia Genetics ¡¡ Presentation of the Norman Geschwind Prize in Behavioral Neurology S29 Epilepsy and Clinical Neurophysiology: Inflammation, Status Epilepticus, and Genetics ¡¡ Presentation of the Dreifuss-Penry Epilepsy Award S30 Education, Research, and History ¡¡ Presentation of the Lawrence C. McHenry Award: An Award for the History of Neurology ¡¡ Presentation of the S. Weir Mitchell Award S31 General Neurology I S32 Headache: Basic Science and Imaging ¡¡ Presentation of the Harold Wolff-John Graham Award: An Award for Headache/Facial Pain Research S33 Cognition Fatigue in MS 2:00 p.m.–6:00 p.m. I7 Emerging Therapeutic Advances in Multiple Sclerosis . . . . . . . . . . 92 2:00 p.m.–6:00 p.m. I8 Clinical Decision Making After the Dust Settles on Clinical Trials . . 93 3:00 p.m.–6:30 p.m. P5 Poster Session V . . . . . . . .94–101 4:00 p.m.–5:45 p.m. Platform Blitzes . . . . . . . . . 102–103 S34 MS and CNS Inflammatory Disease: Risk Factors for MS Disease and Course S35 Cerebrovascular Disease and Interventional Neurology: Issues in Acute Treatment S36 Neuromuscular Disease: Clinical S37 Clinical Aspects of Parkinson’s Disease S38 Aging, Dementia, and Cognitive and Behavioral Neurology: Plasma and Other Biomarkers S39 Neuro-ophthalmology/Neuro-otology II S40 General Neurology II S41 Headache: Clinical S42 Child Neurology I S43 Epilepsy and Clinical Neurophysiology (EEG): Cognition 6:00 p.m.–7:00 p.m. Highlights in the Field H1 Child Neurology H2Epilepsy H3Geriatric H4 Headache & Facial Pain H5 Movement Disorders H6 Multiple Sclerosis H7 Neural Repair & Rehabilitation H8Neuro-oncology H9Neuro-ophthalmology/Neuro-otology H10Sleep H11 Sports Neurology 6:00 p.m.–7:30 p.m. Emerging Science Session Thursday, May 1, 2014 7:30 a.m.–11:00 a.m. P6: Poster Session VI . . . . . . 104–111 9:00 a.m.–12:00 p.m. Frontiers in Neuroscience Plenary Session . . 112 Focuses on translational research related to clinical issues of importance. Six physician scientists outline their recent research findings, along with the clinical implications. 1:00 p.m.–2:45 p.m. Scientific Platform Sessions . . 114–115 S44 MS and CNS Inflammatory Disease: Neuroimaging I S45 Cerebrovascular Disease and Interventional Neurology: Rehabilitation, Recovery, and Complications S46 Neuromuscular Disease: Genetics, Pathogenesis, and Measures Fast, Easy Registration Online · AAN.com/view/AM1415 Scientific Sessions-at-a-Glance S47 Movement Disorders: Huntington’s Disease, Ataxia, and Wilson’s Disease ¡¡ Presentation of the Jon Stolk Award in Movement Disorders for Young Investigators S48 Aging, Dementia, and Cognitive and Behavioral Neurology: MRI Imaging Practice, Policy, and Ethics Epilepsy and Clinical Neurophysiology (EEG): Electrophysiology, Imaging and Functional Connectivity ¡¡ Presentation of the Founders Award S49 S50 S51 Cerebrovascular Disease and Interventional Neurology: Large Vessel Atherosclerotic Disease ¡¡ Presentation of the Michael S. Pessin Stroke Leadership Prize S52 General Neurology III S53 MS and CNS Inflammatory Disease: Biomarkers and Therapeutic Mechanisms 1:00 p.m.–5:00 p.m. I9 Emerging Concepts in Headache Therapy . . . . . . . . . 116 1:00 p.m.–5:00 p.m. I10 The Global Burden of Neurological Diseases . . . . . . . 117 3:00 p.m.–6:30 p.m. P7 Poster Session VII . . . . . . 118–125 3:15 p.m.–5:00 p.m. Scientific Platform Sessions . . 126–127 S54 MS and CNS Inflammatory Disease: Neuroimaging II S55 Pediatric Stroke and Stroke in the Young S56 Anterior Horn Disease ¡¡ Presentation of the Sheila Essey Award: An Award for ALS Research S57 S58 S59 S60 S61 S62 S63 Movement Disorders: Imaging Aging, Dementia, and Cognitive and Behavioral Neurology: Clinical Aspects Epilepsy and Clinical Neurophysiology (EEG): Reproduction, Health Care Delivery, and Co-morbidities Child Neurology II Muscle Disease: Gene Therapy and Models Cerebrovascular Disease and Interventional Neurology: Cognitive and Behavioral Neuromyelitis Optica and Autoimmune Encephalitis 5:30 p.m.–6:30 p.m. Highlights in the Field H12 Adult Intellectual and Developmental Disabilities H13 Endovascular and Interventional Neurology, and Stroke and Vascular Neurology H14 Women’s Issues in Neurology H15 Critical Care 5:30 p.m.–7:00 p.m. Controversies in Neurology Plenary Session . . . . . . . . . . . . . . . . . . . . . . 128 The program features experts discussing the most current and controversial issues in neurology. It is set up as a series of debates in which two speakers argue opposing sides of a single topic, followed by a rebuttal. Each round concludes with a 10-minute question and answer period. Friday, May 2, 2014 8:00 a.m.–12:00 p.m. I11 Proteinopathy in Neurodegenerative Disease . . . . 130 12:00 p.m.–1:30 p.m. Clinical Trials Plenary Session . . . . . . . . . . . . 131 This mid-day session covers important clinical topics that affect patient care identified from other society meetings. The latest updates within several clinical trials conducted over the course of the last year will be presented with an open panel discussion at the conclusion. 1:00 p.m.–2:30 p.m. S64 Section Topic Controversies: Pain: Methods of Treatment . . . . 132 1:00 p.m.–5:00 p.m. I12 Concussion in Sports and the Military . . . . . . . . . . . . 132 5:30 p.m.–7:00 p.m. Neurology Year in Review Plenary Session . . 133 This plenary session will feature six speakers, each focusing on the latest research that has happened in the last year within a specific subspecialty topic. QR Code ¡¡ The QR code is one of the most popular types of twodimensional barcodes. The QR tag can be scanned by smart phones or tablets and will link the attendee to the selected poster via AAN’s Mobile access. Once the QR tag is scanned, the attendee’s mobile device will link to the poster title, authors, and links to the abstract, poster PDF, and audio file. An attendee can literally scan a multitude of posters to see the corresponding content. Please note that each poster presenter needs to provide permission for their poster information to be accessible in the online poster viewing site. 16 2O14 Scientific Abstract Listing and Annual Meeting Information 2014 Award Recipients AAN Alliance Awards John Dystel Prize for Multiple Sclerosis Research Founders Award Presented by the American Academy of Neurology and the National Multiple Sclerosis Society and made possible through a special contribution for the John Dystel Multiple Sclerosis Research Fund at the National Multiple Sclerosis Society. Sponsored by the American Brain Foundation and endowed by the Alliance Founders and S. Weir Mitchell Permanent Endowment. Recipient: Shennan Weiss, MD, PhD / New York, NY S50: Epilepsy and Clinical Neurophysiology (EEG): Electrophysiology, Imaging, and Functional Connectivity Thursday, May 1, 1:00 p.m. Resection of Ictal Phase Locked HFOs is Correlated With Outcome Following Epilepsy Surgery S. Weir Mitchell Award Sponsored by the American Brain Foundation and endowed by the Alliance Founders and S. Weir Mitchell Permanent Endowment. Recipient: Michael Fox, MD, PhD / Newton, MA S30: Education, Research, and History Wednesday, April 30, 2:30 p.m. Lesion-Based Network Analysis: Identifying Distributed Effects of Peduncular Hallucinosis Lesions A.B. Baker Award for Lifetime Achievement in Neurologic Education Recipient: Barry Arnason, MD / Chicago, IL S23: MS and CNS Inflammatory Disease: Novel Therapeutics Tuesday, April 29, 3:15 p.m. Sheila Essey Award: An Award for ALS Research Presented by the American Academy of Neurology and The ALS Association and supported through the philanthropy of the Essey Family Fund and The ALS Association. Recipient: Jeremy Shefner, MD, PhD / Syracuse, NY S56: Anterior Horn Disease Thursday, May 1, 3:15 p.m. American Brain Foundation Chair’s Award Sponsored by the American Brain Foundation. Recipient: Linda M. Selwa, MD, FAAN / Ann Arbor, MI Funded by and endowment created by matching funds from the A.B. Baker Family Trust and Novartis Pharmaceuticals. Norman Geschwind Prize in Behavioral Neurology Recipient: Jerome Posner, MD, FAAN / New York, NY CQ6: Education Colloquium Monday, April 28, 8:30 a.m. Sponsored by the American Academy of Neurology and the AAN Behavioral Neurology Section and endowed through the Dr. Geschwind’s family, friends, and colleagues; Pfizer Inc; and the Society for Behavioral and Cognitive Neurology. AAN Award for Creative Expression of Human Values in Neurology Recipient: Roy Hamilton, MD, MS / Philadelphia, PA S28: Aging, Dementia, and Cognitive and Behavioral Neurology: Dementia Genetics Wednesday, April 30, 2:00 p.m. Sponsored by the Neurology Ethics, Law, and Humanities Committee. Recipient: Jorge L. Almodovar-Suarez, MD / Manchester, NH Mitchell B. Max Award for Neuropathic Pain Dreifuss-Penry Epilepsy Award Sponsored by the American Academy of Neurology and endowed by the United States Cancer Pain Relief Committee, the Mayday Fund, and friends of Dr. Mitchell Max. Sponsored by the American Academy of Neurology and endowed by members of the AAN Epilepsy Section; Abbott Laboratories, Inc.; Cephalon, Inc.; Cyberonics, Inc.; Elan Pharmaceuticals, Inc.; GlaxoSmithKline; Novartis Pharmaceuticals; Ortho-McNeil Neurologics; Pfizer Inc; Shire US, Inc; and UCB Pharma. Recipient: Kathleen Foley, MD / New York, NY S20: Pain and Palliative Care Tuesday, April 29, 3:15 p.m. Recipient: Catherine Schevon, MD, PhD / New York, NY S29: Epilepsy and Clinical Neurophysiology: Inflammation, Status Epilepticus, and Genetics Wednesday, April 30, 2:00 p.m. 18 2O14 Scientific Abstract Listing and Annual Meeting Information Jon Stolk Award in Movement Disorders for Young Investigators Lawrence C. McHenry Award: An Award for the History of Neurology Sponsored by the American Academy of Neurology and endowed by Kyowa Pharmaceuticals, Inc.; Lineberry Research; Quintiles; and Dr. Dennis Gillings. Sponsored by the American Academy of Neurology. Recipient: Alice Chen-Plotkin, MD / Philadelphia, PA S47: Movement Disorders: Huntington’s Disease, Ataxia, and Wilson’s Disease Thursday, May 1, 1:00 p.m. Association of Indian Neurologists in America (AINA) Lifetime Achievement Award Endowed by the Association of Indian Neurologists in America (AINA). Recipient: Avindra Nath, MBBS, FAAN / Bethesda, MD During the AINA Business Meeting Tuesday, April 29, 2014, at 7:15 p.m. International Scholarship Award Sponsored by the American Academy of Neurology International Subcommittee. Recipients: Mohammadkazem Bakhshandeh Bali / Tehran, Iran Recipients: Farrah Mateen, MD, PhD / Boston, MA Christopher Boes, MD / Rochester, MN S30: Education, Research, and History Wednesday, April 30, 2:00 p.m. “Pinheads”: Neurological Disorders at the Greatest Show on Earth Medical Student Essay Awards Sponsored by the American Academy of Neurology. Extended Neuroscience Award Recipient: Ran (Richard) Liu, MSc / Coquitlum, BC, Canada P2: Poster Session II Tuesday, April 29, 7:30 a.m. Voice Discrimination and Recognition in Patients with Prosopagnosic Complaints G. Milton Shy Award in Clinical Neurology Recipient: David Asuzu, PhD / New Haven, CT P2: Poster Session II Tuesday, April 29, 7:30 a.m. HAT Score Outperforms 7 other Hemorrhagic Transformation Scores Prasanna Venkatesan Eswaradass / Salem, India Meng-Shan Tan / Qingdao, China Teng Jiang / Qingdao, China Yael Hacohen / London, United Kingdom Ruth Dobson / London, United Kingdom Recipient: Trent Hodgson / Chicago, IL P2: Poster Session II Tuesday, April 29, 7:30 a.m. Subspecialization in Neurology: Historical Perspectives on Current Challenges Marta Campagnolo / Padova, Italy Saul R. Korey Award in Experimental Neurology Dimitra Papadimitriou / Athens, Greece Chiara Dalla Torre / Padova, Italy Julieta Arena / Buenos Aires, Argentina Alberto Martinez / Campinas, Sao Paulo Francisco Varela / Buenos Aires, Argentina Recipient: Jessica Shields / New Orleans, LA P2: Poster Session II Tuesday, April 29, 7:30 a.m. Probing the Interaction of the Ipsilateral Posterior Parietal Cortex with the Premotor Cortex Using a Novel Transcranial Magnetic Stimulation Technique Jorge jesús Llibre / Havana, Cuba International Experience Monday, April 28, 1:00 p.m. Roland P. Mackay Award in Historical Aspects Minority Scholars Program Sponsored by a grant from the Allergan Foundation. Recipients: Marcella Evans / University of California School of Medicine Gregory R. Franklin, II / Medical University of South Carolina Daniel A. Cristancho / Perelman School of Medicine at the University of Pennsylvania Fast, Easy Registration Online · AAN.com/view/AM14 19 2014 Award Recipients Laura C. Ramirez / Temple School of Medicine Palatucci Advocacy Leadership Forum Advocates of the Year Jason Neal, PhD / Columbia University, College of Physicians and Surgeons Sponsored by the AAN Government Relations Committee. Shekinah Nefreteri Elmore / Harvard Medical School Patient Safety Award Julian Flores / Harvard Medical School Sponsored by Professional Risk Management Services, Inc., management of The Neurologists’ Program. H. Westley Phillips / Perelman School of Medicine University of Pennsylvania Recipients: Shelly Ozark, MD / Charleston, SC Physician Patient Safety Award Sara Dawit / University of Kansas School of Medicine Catherine Elaine Norise / Perelman School of Medicine University of Pennsylvania Movement Disorders Research Award Sponsored by the American Academy of Neurology, the Parkinson’s Disease Foundation, and the AAN Movement Disorder Section and endowed by the Parkinson’s Disease Foundation. Recipient: Eduardo Tolosa, MD, PhD / Barcelona, Spain S27: Dystonia, Tremor, and Other Movement Disorders Wednesday, April 30, 2:00 p.m. Neuroscience Research Prize Sponsored by the American Academy of Neurology, the American Brain Foundation, and the Child Neurology Society. Recipients: Charlotte Herber / Pound Ridge, NY Stefanie Henry / Brooklyn, NY Lisa Michaels / Plano, TX P3: Poster Session III Tuesday, April 29, 3:00 p.m. Child Neurology Neuroscience Research Prize Recipient: Donn Dexter, MD, FAAN / Eau Claire, WI Michael S. Pessin Stroke Leadership Prize Sponsored by the American Academy of Neurology and endowed by Dr. Pessin’s family, friends, and colleagues. Recipient: Hooman Kamel, MD / New York, NY S51: Cerebrovascular Disease and Interventional Neurology: Large Vessel Atherosclerotic Disease Thursday, May 1, 1:00 p.m. Potamkin Prize for Research in Pick’s, Alzheimer’s, and Related Diseases Sponsored by the American Academy of Neurology, the American Brain Foundation, and funded through the philanthropy of the Potamkin Family. Recipient: M. Marsel Mesulam, MD / Chicago, IL S8: Aging, Dementia, and Cognitive and Behavioral Neurology: PET Imaging Tuesday, April 29, 1:00 p.m. American Academy of Neurology President’s Award Sponsored by the American Academy of Neurology. Recipient: Guy McKhann, MD / Baltimore, MD Sponsored by the American Academy of Neurology, the American Brain Foundation, and the Child Neurology Society. Recipient: Laura Herman / Fort Lauderdale, FL Note: The recipient will attend the 43rd Child Neurology Society Annual Meeting in Columbus, OH 20 Julio Rojas-Martinez, MD, PhD/ Dallas, TX Resident Patient Safety Award 2O14 Scientific Abstract Listing and Annual Meeting Information Quality Award H. Richard Tyler Award Recipients: Dheeraj Khurana, MD / India Practicing Physician Quality Award Sponsored by the American Academy of Neurology and the AAN Archive Committee. Recipient: Edward J. Fine, MD, FAAN / Buffalo, NY Laura Rosow, MD / San Francisco, CA Resident Quality Award Kenneth M. Viste Jr., MD, Patient Advocate of the Year Award Neuroendocrine Research Award Sponsored by the American Academy of Neurology and supported by friends of Dr. Andrew Herzog. Recipient: Stafford Lightman, MB BCHir, MRCP, PhD, FRCP / Bristol, United Kingdom Bruce S. Schoenberg International Award in Neuroepidemiology Endowed by gifts from Dr. Viste’s colleagues, friends, and patients. Recipient: Anthony G. Alessi, MD, FAAN / Norwich, CT Harold Wolff-John Graham: An Award for Headache/Facial Pain Research Sponsored by the American Academy of Neurology and endowed by Endo Pharmaceuticals. Endowed by GlaxoSmithKline, Inc. Recipient: Devender Bhalla, PhD / Limoges, France S10: HIV, PML, and Cerebral Malaria Tuesday, April 29, 1:00 p.m. Recipient: Jakob Møller Hansen, MD, PhD / Los Angeles, CA S32: Headache: Basic Science and Imaging Wednesday, April 30, 2:00 p.m. Wayne A. Hening Sleep Medicine Investigator Award Sleep Science Award Sponsored by the American Academy of Neurology and the AAN Sleep Section and endowed by Cephalon, Inc. Recipient: Claudia Trenkwalder, MD / Kassel, Germany S9: Sleep Tuesday, April 29, 1:00 p.m. Sponsored by the American Academy of Neurology and endowed by UCB, Inc.; Lilly USA; Elite Home Medical & Respiratory, Inc.; Raleigh Neurology Associates; and friends of Dr. Wayne A. Hening. Recipient: Aleksandar Videnovic, MD, MSc / Boston, MA S9: Sleep Tuesday, April 29, 1:15 p.m. “[The Annual Meeting Science Programs] are amazing. The poster sessions are inspiring. You get these young researchers just starting, and they come out with beautiful things that just blow you away. ” Kathleen M. Fitzgerald, MD Eugene, OR Fast, Easy Registration Online · AAN.com/view/AM1421 2014 Research Fellowships American Brain Foundation Clinical Research Training Fellowships Cosponsored by the American Academy of Neurology and the American Brain Foundation. Recipients: Brian Edlow, MD Massachusetts General Hospital Stefanie Geisler, MD Washington University, Saint Louis Eyal Kimchi, MD, PhD Massachusetts General Hospital Svjetlana Miocinovic, MD, PhD UT Southwestern Medical Center Lidia Maria Moura, MD Massachusetts General Hospital Peter Pressman, MD University of California San Francisco Lucia Rivera Lara, MD Johns Hopkins University School of Medicine Rainer von Coelln, MD, PhD University of Maryland School of Medicine Susan S. Spencer Clinical Research Training Fellowship in Epilepsy Cosponsored by the American Brain Foundation, the American Epilepsy Society, and the Epilepsy Foundation. Recipient: Colin Josephson, MD, MSc University of Calgary Clinical Research Training Fellowship in the Neurologic Application of Neurotoxins Funded by the Allergan Foundation. Recipients: Srikant Rangaraju, MD Emory University Valerie Rundle Gonzales, MD University of Florida College of Medicine American Brain Foundation Practice Research Training Fellowship Cosponsored by the American Academy of Neurology and the American Brain Foundation. Recipient: David Hwang, MD Yale School of Medicine Clinical Research Training Fellowship in Ataxia Cosponsored by the American Brain Foundation and the National Ataxia Foundation. Recipient: Padmaja Vittal, MD, MS Rush University Medical Center Clinical Research Training Fellowship in MS Cosponsored by the American Brain Foundation and Biogen Idec. Recipient: Bardia Nourbakhsh, MD University of California San Francisco Robert Katzman, MD. Clinical Research Training Fellowship in Alzheimer’s Research Cosponsored by the American Brain Foundation and the Alzheimer’s Association. Recipient: Elissios Karageorgiou, MD University of California San Francisco Clinician-Scientist Development Three-Year Award in Multiple Sclerosis Cosponsored by the American Brain Foundation and the National Multiple Sclerosis Society. Recipient: Matthew Schindler, MD, PhD University of Pennsylvania Clinician-Scientist Development Three-Year Award in Myasthenia Gravis and Related Disorders of the Neuromuscular Junction Cosponsored by the American Brain Foundation and the Myasthenia Gravis Foundation of America. Recipient: Ricardo Roda, MD, PhD New York University Clinician-Scientist Development Three-Year Award in Parkinson’s Disease Cosponsored by the American Brain Foundation and the Parkinson’s Disease Foundation. Recipient: Amber Van Laar, MD University of Pittsburgh Medical Center Lawrence M. Brass Stroke Research Postdoctoral Fellowship Cosponsored by the American Brain Foundation and the American Heart Association/American Stroke Association. Recipient: Amin Khalifeh Soltani, MD, MPH University of California San Francisco School of Medicine 22 2O14 Scientific Abstract Listing and Annual Meeting Information New! Clinical Research Track The outlined programs below are part of the new Clinical Research Track for the 2014 AAN Annual Meeting. For more information on the programs below, please visit the Annual Meeting Program Search at AAN.com/view/SearchAM. To register for the programs please visit: AAN.com/view/register. Saturday, April 26 C7 Research Career Development Symposium: How to Be Successful in Academic Neuroscience 9:00 a.m.–5:00 p.m. This program is designed for academic neurologists who are early in the development of a clinician scientist career. The focus is on strategies for earning a mentored career development award. Sunday, April 27 CQ2 Research and Technology Colloquium: From Discovery to Therapy 8:00 a.m.–12:00 p.m. Academic, industry, and regulatory representatives will address challenges in the drug development process from drug discovery through clinical trials. Faculty will facilitate a discussion with the attendees on how to advance laboratory findings to novel therapies. CQ4 Clinical Research Colloquium 1:00 p.m.–5:00 p.m. This colloquium provides a brief introduction to the clinical trial, the cohort study, and the case-control study with emphasis on their complementarities and their relative strengths and weaknesses. Monday, April 28 C79 Strategic Grant Writing 10:00 a.m.–12:00 p.m. Faculty will emphasize strategies for devising strong lab- or patient-based research proposals, from establishing the importance of the research question to developing a strong, biologically based hypothesis, and demonstrating the capability of carrying the study to completion. Futures in Clinical Research Luncheon 12:00 p.m.–2:00 p.m. Provides information on a career in clinical research and an opportunity to interact with senior clinical researchers for students, residents, and fellows. Must sign up to attend. For more details and to register, contact Nate Kosher at nkosher@aan.com. Tuesday, April 29 Futures in Clinical Research Luncheon Mentoring Sessions 12:00 p.m.–1:30 p.m. Mentoring sessions for students, residents, and fellows in seven subspecialty areas: Child Neurology, Epilepsy, Headache, Multiple Sclerosis, Muscular Dystrophy, Neurocritical Care, and Parkinson’s Disease. Must sign up to attend. I5 Revolution of Genetic Tools and the Impact on Neurology 1:00 p.m.–5:00 p.m. This program will provide an integrative journey through the revolution in molecular genetics and associated technologies and their immediate and long-term applications, including a broad perspective on the promise genomic medicine holds, an introduction to the spectrum of genomic information that can be interrogated, perspectives on ethical challenges, and the practical perspective of a neurologist using genomic information. Wednesday, April 30 I8 Clinical Decision Making After the Dust Settles on Clinical Trials 2:00 p.m.–6:00 p.m. Once a trial establishing the efficacy of a new treatment is published, many questions remain to be answered before a neurologist can apply that new knowledge in a way to produce the full health benefit for individual patients and across that neurologist’s entire practice. In this session, research in key areas that are critical to consider is illustrated, and the current status of each of these areas in neurology is summarized. For more details and to register, contact Nate Kosher at nkosher@aan.com. Included with registration Registration fee required April 26 – May 3, 2014 Philadelphia, PA Annual Meeting Program Schedule For full course information please reference the 2014 Annual Meeting Registration and Advance Program or view the Annual Meeting Program Search at AAN.com/view/SearchAM. Saturday, April 26 8:00 a.m.–12:00 p.m. Clinical Approach to Muscle Disease C1 How to Analyze Spells by Video-EEG C2 Assessment of Rapidly Progressive Dementias C3 and Related Neurologic Conditions Resident Basic Science I: Neuropathology C4 9:00 a.m.–5:00 p.m. Clerkship and Program Directors Conference C5 The Practice of Neurology: Issues in C6 Coding and Reimbursement Research Career Development Symposium: C7 How to Be Successful in Academic Neuroscience 1:00 p.m.–5:00 p.m. Evaluation and Management of Autonomic Disorders C8 Differential Diagnosis of Neurologic Infections C9 C10 Approach to Sleep Symptoms: Sleepy or Sleepless C11 Resident Basic Science II: Neuroanatomy 2:00 p.m.–5:00 p.m. CQ1 BRAINS Colloquium: Understanding and Improving Your Bottom Line 3:00 p.m.–5:00 p.m. C12 The Dystonias: Diagnosis, Treatment, and Update on Causes C13 Practice Survival for Neurologists: Business Strategies for Success C14 Preventing a First Stroke: What Every Neurologist Needs to Know C15 Top 10 Neuro-ophthalmic Diagnoses You Can’t Afford to Miss C16 Multiple Sclerosis Essentials C17 Attention Deficit Hyperactivity Disorder Across the Lifespan C18 Therapy of Headache C19 Controversies in Brain Death Determination Sunday, April 27 6:30 a.m.–8:00 a.m. C20 Neuro Flash: MRI and Multiple Sclerosis C21 Neuro Flash: Acute Stroke Management C22 You Make the Call—An Interactive, Multimedia, Case-based Approach to Learning EMG 24 C23 Hyperkinetic Movement Disorders: Diagnosis and Treatment C24 Global Health Challenges: Neurology in Developing Countries C25Creativity C26 Introduction to Genetics 8:00 a.m.–12:00 p.m. CQ2 Research and Technology Colloquium: From Discovery to Therapy 8:00 a.m.–12:00 p.m. C27 Clinical EMG I C28 Botulinum Toxins: Practical Issues and Clinical Uses for Neurologists C29 Multiple Sclerosis Overview I: Basic and Translational Science C30 Sleep for the Practicing Neurologist C31 Resident Basic Science III: Neuropharmacology C32 Child Neurology I C33 Prevention of Cardioembolic Stroke in Patients with Nonvalvular Atrial Fibrillation: Recommendations Based on Evidence-based Guidelines and Recent Randomized Trials C34 Neuroimaging for the General Neurologist: Brain C35 Life Reimagined I1 Temporal Lobe Epilepsy and Febrile Seizures . . 42 9:00 a.m.–12:00 p.m. CQ3 Patient Safety Colloquium 9:00 a.m.–12:00 p.m. C36 EEG in Children: Developmental Maturation, Variants, Epilepsy Syndromes, and Identification of Surgical Candidates 9:00 a.m.–5:00 p.m. C37 Therapy in Neurology C38 Neurologic Intensive Care C39Neuro-ophthalmology C40 Spine Neurology: Assessment and Management of Common Spine Disorders C41 Neurophysiologic Intraoperative Monitoring Skills Workshop 10:00 a.m.–12:00 p.m. C42 Vascular Cognitive Impairment and Dementia: Current Status and Future C43 E/M: Minimize Mistakes, Maximize Reimbursement C44 Update on Ataxias 2O14 Scientific Abstract Listing and Annual Meeting Information Subspecialty in Focus Track Leadership Development 1:00 p.m.–2:30 p.m. S1 Section Topic Controversies: ICU EEG Monitoring—Seizures in Critically Ill Patients . 42 1:00 p.m.–5:00 p.m. CQ4 Clinical Research Colloquium 1:00 p.m.–5:00 p.m. C45 Clinical EMG II C46 Non-Alzheimer’s Dementia C47 Multiple Sclerosis Overview II: Clinical Advances C48 Autoimmune Neurology C49 Child Neurology II C50 Core Concepts in Pain Management C51 Algorithms in the Diagnosis and Treatment of Epilepsy C52 Neuroimaging for the General Neurologist: Spine and Peripheral Nerve C53 Clinical Usefulness of Botulinum Toxin and Treatment of Dystonia Skills Pavilion I2 New Antithrombotic Agents for Stroke Prevention . . . . . . . . . . . . . . . . . . . . . . 43 2:00 p.m.–5:00 p.m. CQ5 Practice Colloquium: How to Navigate and Succeed in New Payment Models Included with registration Registration fee required 7:00 a.m.–8:30 a.m. State Society Leadership Roundtable Leadership representatives of state neurological societies are invited to discuss challenges, strategies, and practices related to state society creation and maintenance. Discussion will be facilitated by Academy staff. Participants will learn from the experiences of established societies and be introduced to the resources available from the Academy. 8:00 a.m.–8:30 a.m. A AN/AANI Business Meeting All members are invited to attend the meeting to take part in the Academy business. 8:00 a.m.–12:00 p.m. C62 Continuum ® Test Your Knowledge: A Multiple-Choice Question Review C63 Primer of Behavioral Neurology C64 Introduction to Primary Headache Disorders C65 Neurologic Complications of Systemic Cancer C66 Teleneurology and Technologies C67 Infections of the Nervous System I: Common Infections C68 Stroke in Childhood and Adolescence I3 Clocks, Sleep, Brain Health and Disorders: Impact on Mechanism, Expression, and Treatment . . . 44 6:00 p.m.–10:00 p.m. Opening Party . . . . . . . . . . . . . . . . . . . . . . . . . . . . 136 Join your friends and colleagues for an exciting evening filled with entertainment. Each registered meeting attendee will receive one free ticket to these events. Guest tickets are available through registration for $50. 8:30 a.m.–12:00 p.m. CQ6 Education Colloquium Monday, April 28 9:00 a.m.–5:00 p.m. C71 Movement Disorders C72 Neurology Update I C73 Clinical EEG C74 Genetics in Neurology C75 Women in Leadership (must apply) C76 EMG Skills Workshop: Basic 6:30 a.m.–8:00 a.m. C54 Morning Report: Lumbar Radiculopathy, Lumbar Spinal Stenosis, Low Back Pain, and Post-Laminectomy Syndrome C55 Morning Report: Memory Disorders C56 Neuro Flash: Neuro-ophthalmology C57 Small Fiber Neuropathies: Sensory, Autonomic and Both C58 Hallucinations in Parkinson’s Disease C59 Career Development for Clinician Educators C60 Prognostication in the Era of Hypothermia 6:30 a.m.–8:30 a.m. C61 Resident and Fellow Career Breakfast: The Early Years (registration is required) 9:00 a.m.–12:00 p.m. C69 Improving Accuracy of Dementia Diagnosis: Case Studies with Both Imaging and Neuropathology C70 Controversies in Multiple Sclerosis Therapy 9:30 a.m.–12:00 p.m. C77 Philanthropy 101 10:00 a.m.–12:00 p.m. C78 Tales from the Front Cover: Effective Book Writing and Publishing for Neurologists C79 Strategic Grant Writing 12:00 p.m.–1:30 p.m. Government Relations Committee Meet and Greet Fast, Easy Registration Online · AAN.com/view/AM1425 Annual Meeting Program Schedule 1:00 p.m.–2:30 p.m. S2Cancelled 9:00 a.m.–12:00 p.m. Presidential Plenary Session . . . . . . . . . . . . . 64 1:00 p.m.–5:00 p.m. C80 Stroke in Young Adults C81 Chronic Migraine Education Program C82 Sports Neurology: Non-Concussion Overview C83 Infections of the Nervous System II: Advanced and Emerging Infections C84 Sleep Principles Applied to Neurological Disease C85 Improving Your Leadership Skills: A Practical Approach I4 Recent Advances in Translational Research in Autism . . . . . . . . . . . . . . . . . . . . . 45 F eatures the AAN’s premier lecture awards for clinically relevant research and a presentation by a leading lecturer. Top researchers speak on some of the most significant findings in neurology in 2014. 1:30 p.m.–3:00 p.m. AAN/ABPN MOC Informational Session 2:00 p.m.–4:30 p.m. CQ7 Education Research Colloquium Presidential Lecture: James L. Bernat, MD, FAAN Dartmouth Hitchcock Medical Center, Lebanon, NH Challenges to Ethics and Professionalism Facing the Contemporary Neurologist George C. Cotzias Lecture: Endowed by Roche Pharmaceuticals. Stefan M. Pulst, MD, FAAN University of Utah, Salt Lake City, UT Degenerative Ataxias: From Genes to Therapies Sidney Carter Award in Child Neurology Lecture: Endowed by an anonymous donor. Darryl C. De Vivo, MD, FAAN Columbia University Medical Center, New York, NY Rare Diseases and Neurological Phenotypes 2:00 p.m.–5:00 p.m. CQ8 Health Information Technology Colloquium: Advancements in Technology 2:00 p.m.–5:00 p.m. C86 ICD-10-CM: Essentials of Understanding and Implementation C87 Eye Movement Disorders: A Systematic Approach to the Evaluation of Diplopia 3:00 p.m.–6:30 p.m. Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 P1 4:30 p.m.–6:30 p.m. Exhibit Hall Opening Reception 6:30 p.m.–9:00 p.m. Residents and Fellows Career Forum and Reception Tuesday, April 29 Robert Wartenberg Lecture: David M. Holtzman, MD, FAAN Washington University School of Medicine, St. Louis, MO Alzheimer’s Disease in 2014: Mapping a Road Forward 11:30 a.m.–5:00 p.m. Exhibit Hall 1:00 p.m.–2:30 p.m. S3 Section Topic Controversies: PFO: Aggressive Treatment or Just Aspirin . . . . . . . . 65 1:00 p.m.–2:45 p.m. Scientific Platform Sessions . . . . . . . . . . . . . . . 66–67 S4 MS and CNS Inflammatory Disease: Clinical Trials 6:30 a.m.–8:30 a.m. 2014 AAN Run/Walk for Brain Research . . . . 137 6:30 a.m.–8:00 a.m. C89 Neuro Flash: Epilepsy C90 Therapy of Multiple Sclerosis C91 Advances in Autism Spectrum Disorders and Intellectual Disability: From Genetics to Clinical Practice C92 The Neurology of Social Behavior C93 Therapy of Neuromuscular Disease C94 Borderlands of Neurology and Internal Medicine 7:30 a.m.–11:00 a.m. P2 Poster Session II . . . . . . . . . . . . . . . . . . . . 56–63 26 S5 Cerebrovascular Disease and Interventional Neurology: Pre-hospital, Telemedicine, and Related Topics S6 Neuromuscular Disease: Gene Therapy S7 Parkinson’s Disease: Preclinical and Clinical Therapeutics S8 Aging, Dementia, and Cognitive and Behavioral Neurology: PET Imaging ¡¡ Presentation of the Potamkin Prize for Research in Pick’s, Alzheimer’s Disease, and Related Diseases S9Sleep ¡¡ Presentation of the Sleep Science Award ¡¡ Presentation of the Wayne A. Hening Sleep Medicine Investigator Award 2O14 Scientific Abstract Listing and Annual Meeting Information Subspecialty in Focus Track Leadership Development S10 HIV, PML, and Cerebral Malaria ¡¡ Presentation of the Bruce S. Schoenberg International Award in Neuroepidemiology S11 Neuro Trauma, Critical Care, and Sports Neurology S12 Cerebrovascular Disease and Interventional Neurology: Epidemiology and Risk Factors S13 MS and CNS Inflammatory Disease: MRI Atrophy Measures and Correlations 1:00 p.m.–5:00 p.m. C95 Deep Brain Stimulation Management C96 The History of Certain Disorders of the Nervous System C97 Emergency Neurology C98 Practical Legal Issues for Neurologists C99 Epilepsy Skills Pavilion I5 Revolution of Genetic Tools and the Impact on Neurology . . . . . . . . . . . . . . . . . . 68 I6 Peripheral Neuropathies . . . . . . . . . . . . . . . . . . 69 2:00 p.m.–5:00 p.m. C100 The Intractable Headache Patient 3:00 p.m.–6:30 p.m. Poster Session III . . . . . . . . . . . . . . . . . . . . 70–77 P3 3:15 p.m.–5:00 p.m. Scientific Platform Sessions . . . . . . . . . . . . . . . . 78–79 S14 MS and CNS Inflammatory Disease: Animal and In Vitro S15 S16 S17 S18 S19 S20 Studies Cerebrovascular Disease and Interventional Neurology: Clinical and Imaging Biomarkers and Genetics Neuromuscular and Clinical Neurophysiology (EMG): Clinical Trials and Therapy Parkinson’s Disease: Genetics and Epidemiology Aging, Dementia, and Cognitive and Behavioral Neurology: Behavioral Neuroscience Neuro-ophthalmology/Neuro-otology I Pain and Palliative Care ¡¡ Presentation of the Mitchell B. Max Award for Neuropathic Pain S21 Neurorehabilitation and Neural Repair S22Neuro-oncology S23 MS and CNS Inflammatory Disease: Novel Therapeutics ¡¡ Presentation of the John Dystel Prize for Multiple Sclerosis Research Included with registration Registration fee required 5:30 p.m.–6:30 p.m. Hot Topics Plenary Session . . . . . . . . . . . . . . 80 Features translational research related to clinical issues of importance. Four outstanding physician-scientists provide summaries of their recent research findings and describe the clinical implications of the results. Oleg Butovsky, PhD Brigham and Women’s Hospital/Harvard Medical School, Boston, MA Identification of a Unique Molecular and Functional Microglia Signature in Health and Disease Jerome H. Chin, MD, PhD, MPH Alliance for Stroke Awareness and Prevention Project (ASAPP), San Anselmo, CA The Global Epidemic of Stroke: Sounding the Alarm Dennis W. Dickson, MD Mayo Clinic, Jacksonville, FL Emerging Concepts in Chronic Traumatic Encephalopathy David Eidelberg, MD, FAAN Feinstein Institute for Medical Research, Manhasset, NY Functional Connectivity and Functional Imaging in Movement Disorders 7:00 p.m.–10:00 p.m. Corporate Therapeutic Updates . . . . . . . . . . . . . . . 147 Industry-sponsored, non-CME programs will be offered and are open to attendees at no charge. They will provide an opportunity for pharmaceutical companies, device companies, or other neurologicrelated organizations to share information regarding their current therapies and projects in the pipeline in accordance with standards set for industry by the FDA. Wednesday, April 30 6:30 a.m.–8:00 a.m. C101 Neuro Flash: Child Neurology C102 Balance and Gait Disorders C103 Therapy of Stroke C104 Nystagmus: An Organized Approach C105 Differential Diagnosis of Dementia: Linking Clinical Syndromes to Biomarkers C106 Integrative Management of Multiple Sclerosis C107 Brain Computer Interfaces: Frontiers in Neurology and Neuroscience 7:30 a.m.–11:00 a.m. P4 Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 Fast, Easy Registration Online · AAN.com/view/AM14 27 Annual Meeting Program Schedule 9:00 a.m.–12:00 p.m. Contemporary Clinical Issues Plenary Session . . . . . . . . . . . . . . . . . 89 Highlights issues most critical to practicing neurologists, including abstracts related to new therapeutic developments, clinical applications of basic and translational research, and innovative technical developments. William K. Mountford, PhD Premier Research Services, Wilmington, NC Comparison of Thrombolytic Treatment for Acute Ischemic Stroke Pre- and Post-Telemedicine Implementation in the Spoke Hospital Setting Discussant: Lee H. Schwamm, MD Massachusetts General Hospital, Boston, MA David R. Jacoby, MD, PhD BioMarin Pharmaceutical Inc., Novato, CA Epigenetic Therapy for Friedreich’s Ataxia: A Phase I Clinical Trial Scientific Platform Sessions . . . . . . . . . . . . . . . 90–91 S24 Diet and Hormonal Influences in MS S25 Cerebrovascular Disease and Interventional Neurology: Hemorrhage, Aneurysms, and Vascular Malformations S26 Biomarkers in Neuromuscular Diseases S27 Dystonia, Tremor, and Other Movement Disorders S28 S29 S30 William Herring, MD, PhD Merck Research Laboratories, North Wales, PA Clinical Profile of the Orexin Receptor Antagonist Suvorexant for the Treatment of Insomnia in Phase-3 Clinical Trials Discussant: Phyllis C. Zee, MD, PhD Northwestern University Medical School, Chicago, IL S31 Jonathan Stone, MB, ChB, FRCP, PhD Western General Hospital, Edinburgh, United Kingdom Functional (Psychogenic) Disorders in Neurology Kenneth L. Marek, MD Institute for Neurodegenerative Disorders, New Haven, CT Parkinson’s Disease Progression Marker Initiative: Developing a Translational Toolbox for PD Progression Commentary and discussion follow each presentation. 11:30 a.m.–5:00 p.m. Exhibit Hall 28 2:00 p.m.–3:45 p.m. Discussant: Tetsuo Ashizawa, MD, FAAN University of Florida, Gainesville, FL David B. Goldstein, PhD Duke University, Durham, NC Direct to Consumer Genetic Testing 12:00 p.m.–1:30 p.m. American Academy of Neurology and American Brain Foundation Awards Luncheon . . . . . 137 S32 S33 ¡¡ Presentation of the Movement Disorders Research Award Aging, Dementia, and Cognitive and Behavioral Neurology: Dementia Genetics ¡¡ Presentation of the Norman Geschwind Prize in Behavioral Neurology Epilepsy and Clinical Neurophysiology: Inflammation, Status Epilepticus, and Genetics ¡¡ Presentation of the Dreifuss-Penry Epilepsy Award Education, Research, and History ¡¡ Presentation of the Lawrence C. McHenry Award: An Award for the History of Neurology ¡¡ Presentation of the S. Weir Mitchell Award General Neurology I Headache: Basic Science and Imaging ¡¡ Presentation of the Harold Wolff-John Graham Award: An Award for Headache/Facial Pain Research Cognition Fatigue in MS 2:00 p.m.–6:00 p.m. C108 Neurologic Issues in Pregnancy C109 Emergency Room Neuro-ophthalmology C110 Sports Concussion and Other Mild Concussive Injuries C111 Bedside Evidence-based Medicine: How to Deconstruct Articles in Order to Take Care of Patients C112 Neuromuscular Bedside Rounds Skills Pavilion C113 Acute Stroke Alert Skills Pavilion I7 Emerging Therapeutic Advances in Multiple Sclerosis . . 92 I8 Clinical Decision Making After the Dust Settles on Clinical Trials . . . . . . . . . . . . . . . 93 3:00 p.m.–6:30 p.m. Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 P5 4:00 p.m.–5:45 p.m. Platform Blitzes . . . . . . . . . . . . . . . . . . . . . . 102–103 S34 MS and CNS Inflammatory Disease: Risk Factors for MS Disease and Course S35 Cerebrovascular Disease and Interventional Neurology: Issues in Acute Treatment 2O14 Scientific Abstract Listing and Annual Meeting Information Subspecialty in Focus Track Leadership Development S36 Neuromuscular Disease: Clinical S37 Clinical Aspects of Parkinson’s Disease S38 Aging, Dementia, and Cognitive and Behavioral Neurology: S39 S40 S41 S42 S43 Plasma and Other Biomarkers Neuro-ophthalmology/Neuro-otology II General Neurology II Headache: Clinical Child Neurology I Epilepsy and Clinical Neurophysiology (EEG): Cognition 5:30 p.m.–7:00 p.m. Current Practice Issues in Neurology The interactive Current Practice Issues in Neurology session “Do Payer Rankings Keep You at the Top of the Class or Give You a Failing Grade” will give neurologists a chance to hear directly from both a CMS Medical Officer and a private payer Medical Director to gain a better understanding of how to properly interpret their details from the Quality and Resource Use Reports (QRUR) and physician designation programs; how to determine if the information is accurate; the importance of ensuring your rating is accurate; what the steps to take are if there are discrepancies with their information; and navigate through and utilize the CMS Physician Compare website and other available resources. The Academy is pleased to offer this event to continue developing a positive, constructive dialogue with payers at the physician level. Thursday, May 1 6:30 a.m.–8:00 a.m. C114 Morning Report: Multiple Sclerosis C115 Neuro Flash: Palliative Care for the Practicing Neurologist C116 Learning Movement Disorders in Hindsight: Lessons from My Patients C117 Principles of Genomic Medicine: Whole Exome Sequencing in Neurologic Disease C118Neurotoxicology C119 Syndromes of Autonomic Dysfunction in Children and Adolescents 7:30 a.m.–11:00 a.m. P6 Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 9:00 a.m.–12:00 p.m. Frontiers in Neuroscience Plenary Session . . 112 Focuses on translational research related to clinical issues of importance. Six physician scientists outline their recent research findings, along with the clinical implications. 6:00 p.m.–7:00 p.m. Included with registration Registration fee required Highlights in the Field Sessions S . Thomas Carmichael, MD, PhD David Geffen School of Medicine at UCLA, Los Angeles, CA Tissue Environments for Brain Repair Albert Lo, MD, PhD H1 Child Neurology Brown University, Providence VA Medical Center, Providence, RI Opportunities and Challenges of Robot Assisted and Facilitated Neurorecovery H2Epilepsy H3Geriatric H4 Headache & Facial Pain H5 Movement Disorders H6 Multiple Sclerosis H7 Neural Repair & Rehabilitation William Seeley, MD UCSF, San Francisco, CA Network-based Neurodegeneration H8Neuro-oncology Cori Bargmann, PhD H9Neuro-ophthalmology/Neuro-otology Rockefeller University, New York, NY Using Fixed Circuits to Generate Flexible Behaviors H10Sleep H11 Sports Neurology 6:00 p.m.–7:30 p.m. Emerging Science Session 7:00 p.m.–10:00 p.m. Corporate Therapeutic Updates . . . . . . . . . . . . . . . 147 Industry-sponsored, non-CME programs will be offered and are open to attendees at no charge. They will provide an opportunity for pharmaceutical companies, device companies, or other neurologic-related organizations to share information regarding their current therapies and projects in the pipeline in accordance with standards set for industry by the FDA. Bruce R. Rosen, MD, PhD Harvard Medical School, Boston, MA Advances in Mapping Human Brain Connectivity: The Human Connectome Project aiken Nedergaard, MD, DMSc M University of Rochester Medical Center, Rochester, NY The Nightlife of Astrocytes Fast, Easy Registration Online · AAN.com/view/AM14 29 Annual Meeting Program Schedule 11:30 a.m.–3:00 p.m. Exhibit Hall 1:00 p.m.–2:45 p.m. Scientific Platform Sessions . . . . . . . . . . . . . . 114–115 S44 MS and CNS Inflammatory Disease: Neuroimaging I S45 Cerebrovascular Disease and Interventional Neurology: Rehabilitation, Recovery, and Complications S46 Neuromuscular Disease: Genetics, Pathogenesis, and Measures S47 Movement Disorders: Huntington’s Disease, Ataxia, and Wilson’s Disease ¡¡ Presentation of the Jon Stolk Award in Movement Disorders for Young Investigators S48 Aging, Dementia, and Cognitive and Behavioral Neurology: MRI Imaging S49 Practice, Policy, and Ethics S50 Epilepsy and Clinical Neurophysiology (EEG): Electrophysiology, Imaging and Functional Connectivity ¡¡ Presentation of the Founders Award S51 Cerebrovascular Disease and Interventional Neurology: Large Vessel Atherosclerotic Disease ¡¡ Presentation of the Michael S. Pessin Stroke Leadership Prize S52 General Neurology III S53 MS and CNS Inflammatory Disease: Biomarkers and Therapeutic Mechanisms 1:00 p.m.–5:00 p.m. C120 Consultations in the Medical Surgical ICU C121 Office Orthopedics for the Neurologist C122 Traumatic Brain Injury C123 Neuro-ophthalmology and Neurovestibular Exam Lab Skills Pavilion I9 Emerging Concepts in Headache Therapy . . . . . . . . 116 I10 The Global Burden of Neurological Diseases . . . . . . . 117 S59 Epilepsy and Clinical Neurophysiology (EEG): Reproduction, Health Care Delivery, and Co-morbidities S60 Child Neurology II S61 Muscle Disease: Gene Therapy and Models S62 Cerebrovascular Disease and Interventional Neurology: Cognitive and Behavioral S63 Neuromyelitis Optica and Autoimmune Encephalitis 5:30 p.m.–6:30 p.m. Highlights in the Field Sessions H12 Adult Intellectual and Developmental Disabilities H13 Endovascular and Interventional Neurology, and Stroke and Vascular Neurology H14 Women’s Issues in Neurology H15 Critical Care 5:30 p.m.–7:00 p.m. Controversies in Neurology Plenary Session . . 128 The program features experts discussing the most current and controversial issues in neurology. It is set up as a series of debates in which two speakers argue opposing sides of a single topic, followed by a rebuttal. Each round concludes with a 10-minute question and answer period. Does Preventing Relapses Protect Against Progressive MS? Pro: Maria Trojano, MD University of Bari, Bari, Italy Con: Helen Tremlett, PhD, BPharm University of British Columbia, Vancouver, BC, Canada Is Intervention for Asymptomatic AVM Useful? Pro: Robert M. Friedlander, MD UPMC Presbyterian, Pittsburgh, PA 2:00 p.m.–5:00 p.m. C124 Clinical E-Pearls C125 Status Epilepticus Con: J. P. Mohr, MD, FAAN Columbia University, New York, NY 3:00 p.m.–6:30 p.m. Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 P7 Should Neurologists Prescribe Marijuana for Neurological Disorders? Pro: Barbara S. Koppel, MD, FAAN Metropolitan Hospital, Rye, NY 3:15 p.m.–5:00 p.m. Scientific Platform Sessions . . . . . . . . . . . . . . 126–127 S54 MS and CNS Inflammatory Disease: Neuroimaging II S55 Pediatric Stroke and Stroke in the Young S56 Anterior Horn Disease ¡¡ Presentation of the Sheila Essey Award: An Award for ALS Research S57 Movement Disorders: Imaging S58 Aging, Dementia, and Cognitive and Behavioral Neurology: Clinical Aspects 30 2O14 Scientific Abstract Listing and Annual Meeting Information Con: John C. M. Brust, MD, FAAN Columbia University, New York, NY Subspecialty in Focus Track Leadership Development 6:00 p.m.–9:00 p.m. C126 Case Studies: Unusual Diagnostic and Management of Cases in Neuromuscular Disease C127 Case Studies: Unusual Movement Disorders C128 Case Studies in Behavioral Neurology: Focus on Frontotemporal Degeneration C129 Case Studies: Multiple Sclerosis C130 Case Studies: Neurologic Consultations in Cancer Patients C131 Test Your Knowledge: A Case-based Approach to Neuroimaging Friday, May 2 6:30 a.m.–8:00 a.m. C132 Neuro Flash: Approach to Acute CNS Infections C133 The Spectrum of Motor Neuron Disease C134 Parkinson’s Disease Management: Pearls, Pitfalls, and Future Prospects C135 Continued Challenges of the Neurohospitalist Model of Care C136 Important Drug Interactions for Neurologists and Psychiatrists C137 Mild Cognitive Impairment: Implications for Clinicians 8:00 a.m.–12:00 p.m. C138 Parkinson’s Disease and Movement Disorders Update C139 Neuromyelitis Optica: Scientific and Clinical Update C140 Hot Topics in Headaches and Related Disorders C141 Neurodevelopmental Disabilities Across the Lifespan C142 Concussion in the Military and in Sports I11 Proteinopathy in Neurodegenerative Disease . 130 9:00 a.m.–5:00 p.m. C143 Peripheral Neuropathy C144 Neurology Update II C145 Cerebrovascular Disease C146 Clinical Epilepsy C147 Dementia Update C148 Neuromuscular Ultrasound Skills Workshop Included with registration Registration fee required 12:00 p.m.–1:30 p.m. Clinical Trials Plenary Session . . . . . . . . . . . . 131 This mid-day session covers important clinical topics that affect patient care identified from other society meetings. The latest updates within several clinical trials conducted over the course of the last year will be presented with an open panel discussion at the conclusion. Michael Wall, MD, FAAN University of Iowa, Iowa City, IA The Idiopathic Intracranial Hypertension Treatment Trial: A Multicenter, Double-Blind, Randomized Clinical Trial Comparing Acetazolamide and Placebo on Visual Outcome Mark R. Gilbert, MD The University of Texas MD Anderson Cancer Center, Houston, TX Anti-angiogenic Therapy for Glioblastoma: A Randomized, Double-Blinded Phase III Trial of Bevacizumab in Newly Diagnosed Patients Aaron E. Miller, MD, FAAN Mt. Sinai School of Medicine, New York, NY TOPIC: Efficacy and Safety of Once-daily Oral Teriflunomide in Patients with First Clinical Episode Consistent with Multiple Sclerosis Jeffrey L. Saver, MD, FAAN UCLA School of Medicine, Los Angeles, CA FAST-MAG Trial in Acute Ischemic Stroke David Dodick, MD Mayo Clinic, Phoenix, AZ CGRP Monoclonal Antibody LY2951742 for the Prevention of Migraine: A Phase 2, Randomized, Double-Blind, Placebo-Controlled Study Peter Goadsby, MD, PhD University of California, San Francisco, CA Randomized, Double-blind, Placebo-controlled Trial of ALD403: An Anti-CGRP Peptide Antibody in the Prevention of Frequent Episodic Migraine 1:00 p.m.–2:30 p.m. S64 Section Topic Controversies: Pain: Methods of Treatment . . . . . . . . . . . . . . . . 132 1:00 p.m.–5:00 p.m. C149Neuro-otology C150 Neuro-oncology: Primary Brain Tumors C151 Hot Topics in Sleep Neurology C152 Symptomatic Management in Multiple Sclerosis C153 Imaging and Genomics for Detecting Neurodegenerative Proteinopathy in Clinical Practice I12 Concussion in Sports and the Military . . . . . 132 Fast, Easy Registration Online · AAN.com/view/AM14 31 Annual Meeting Program Schedule 5:30 p.m.–7:00 p.m. Neurology Year in Review Plenary Session . . 133 This plenary session will feature six speakers, each focusing on the latest research that has happened in the last year within a specific subspecialty topic. Anne H. Cross, MD Washington University School of Medicine, St. Louis, MO Multiple Sclerosis Peter Goadsby, MD, PhD UCSF, San Francisco, CA Headache/Pain Robert C. Griggs, MD, FAAN University of Rochester, Rochester, NY Neuromuscular Kathleen M. Shannon, MD Rush University Medical Center, Chicago, IL Movement Disorders David M. Greer, MD Yale University School of Medicine, New Haven, CT Neurocritical Care Todd E. Golde, MD, PhD University of Florida Collage of Medicine, Gainesville, FL Alzheimer’s Disease 7:30 p.m.–9:00 p.m. Closing Party . . . . . . . . . . . . . . . . . . . . . . . . . . . 136 Join us at the festive Closing Party, where former NFL star-turnedsinger and Public Leadership in Neurology Award-winner Ben Utecht will enchant you with his inimitable vocal stylings. Saturday, May 3 6:30 a.m.–8:00 a.m. C154 Update on Endovascular Treatment of Cerebrovascular Diseases C155 Cumulative Sports Concussion and Risk of Dementia C156 Evaluation and Therapy of Restless Legs Syndrome and Periodic Limb Movements in Sleep C157 Therapy of Epilepsy C158 Psychogenic Movement Disorders 6:30 a.m.–8:30 a.m. C159 Challenging Headache Cases 8:00 a.m.–12:00 p.m. C160 Neuromuscular Junction Disorders C161 Neurologic Complications of Medical Disease C162 Diagnostic Dilemmas in Multiple Sclerosis C163Myelopathies C164 Practical Psychopharmacology for Neurologists C165 Critical Care EEG Monitoring 9:00 a.m.–12:00 p.m. C166 Interpretation of Polysomnography for the Practicing Neurologist 10:00 a.m.–12:00 p.m. C167 Mitochondrial Disorders in Neurology C168 Therapy of Movement Disorders: A Case-based Approach C169 Common Neurologic Problems in Adults with Intellectual and Developmental Disabilities Current as of 2/13/2014 –Subject to change “With every Annual Meeting that I attend I always come away from the scientific conferences with something new and different to add to my care and treatment of patients with neurologic diseases.” Christopher J. Prusinski, DO Melbourne, FL 32 2O14 Scientific Abstract Listing and Annual Meeting Information Annual Meeting Programs by Topic For full course information please reference the 2014 Annual Meeting Registration and Advance Program or view the Annual Meeting Program Search at AAN.com/view/SearchAM. Please refer to the key for the following program definitions: C Course P Poster Session CQ Colloquium H Highlights in the Field S Scientific Platform Session/Section Topic Controversies Aging, Dementia, Cognitive, and Behavioral Neurology C3 Assessment of Rapidly Progressive Dementias and Related Neurologic Conditions C17 Attention Deficit Hyperactivity Disorder Across the Lifespan C25 Creativity C42 Vascular Cognitive Impairment and Dementia: Current Status and Future C46 Non-Alzheimer’s Dementia C55 Morning Report: Memory Disorders C63 Primer of Behavioral Neurology C69 Improving Accuracy of Dementia Diagnosis: Case Studies with Both Imaging and Neuropathology P1 Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 C92 The Neurology of Social Behavior Poster Session II . . . . . . . . . . . . . . . . . . . . 56–63 P2 Presidential Plenary Session . . . . . . . . . . . . . 64 Aging, Dementia, and Cognitive and S8 Behavioral Neurology: PET Imaging . . . . . . . . . . . . 66 Poster Session III . . . . . . . . . . . . . . . . . . . . 70–77 P3 S18 Aging, Dementia, and Cognitive and Behavioral Neurology: Behavioral Neuroscience . . . . . 78 C105 Differential Diagnosis of Dementia: Linking Clinical Syndromes to Biomarkers Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 P4 S28 Aging, Dementia, and Cognitive and Behavioral Neurology: Dementia Genetics . . . . . . . . 90 Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 P5 S38 Aging, Dementia, and Cognitive and Behavioral Neurology: Plasma and Other Biomarkers . . 102 Geriatric Neurology Highlights in the Field . . . . . . . . 29 H3 Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 P6 Frontiers in Neuroscience Plenary Session . . . . 112 S48 Aging, Dementia, and Cognitive and Behavioral Neurology: MRI Imaging . . . . . . . . . . . 114 C122 Traumatic Brain Injury Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 P7 S58 Aging, Dementia, and Cognitive and Behavioral Neurology: Clinical Aspects . . . . . . . . . . 126 34 I Integrated Neuroscience Session C128 Case Studies in Behavioral Neurology: Focus on Frontotemporal Degeneration C137 Mild Cognitive Impairment: Implications for Clinicians I11 Proteinopathy in Neurodegenerative Disease . 130 C147 Dementia Update C153 Imaging and Genomics for Detecting Neurodegenerative Proteinopathy in Clinical Practice Neurology Year in Review Plenary Session . . . . 133 C155 Cumulative Sports Concussion and Risk of Dementia C164 Practical Psychopharmacology for Neurologists Cerebrovascular Disease and Interventional Neurology C14 Preventing a First Stroke: What Every Neurologist Needs to Know C21 Neuro Flash: Acute Stroke Management C33 Prevention of Cardioembolic Stroke in Patients with Nonvalvular Atrial Fibrillation: Recommendations Based on Evidence-based Guidelines and Recent Randomized Trials I2 New Antithrombotic Agents for Stroke Prevention . . . . . . . . . . . . . . . . . . . . . . 43 C60 Prognostication in the Era of Hypothermia C68 Stroke in Childhood and Adolescence C80 Stroke In Young Adults P1 Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 P2 Poster Session II . . . . . . . . . . . . . . . . . . . . 56–63 S3 Section Topic Controversies: PFO: Aggressive Treatment or Just Aspirin . . . . . . . . . . . 65 S5 Cerebrovascular Disease and Interventional Neurology: Pre-hospital, Telemedicine, and Related Topics . . . . . . 66 S12 Cerebrovascular Disease and Interventional Neurology: Epidemiology and Risk Factors . . . . . . . . . . . . . . . 67 P3 Poster Session III . . . . . . . . . . . . . . . . . . . . 70–77 S15 Cerebrovascular Disease and Interventional Neurology: Clinical and Imaging Biomarkers and Genetics . . . . . . 78 C103 Therapy of Stroke P4 Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 Contemporary Clinical Issues Plenary Session . . 89 2O14 Scientific Abstract Listing and Annual Meeting Information Subspecialty in Focus Track Leadership Development S25 C113 P5 S35 P6 S45 S51 P7 S55 S62 H13 C135 C145 C154 Cerebrovascular Disease and Interventional Neurology: Hemorrhage, Aneurysms, and Vascular Malformations . 90 Acute Stroke Alert Skills Pavilion Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 Cerebrovascular Disease and Interventional Neurology: Issues in Acute Treatment . . . . . . . . . . . . . . . . . 102 Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 Frontiers in Neuroscience Plenary Session . . . . 112 Cerebrovascular Disease and Interventional Neurology: Rehabilitation, Recovery, and Complications . . . . . . . 114 Cerebrovascular Disease and Interventional Neurology: Large Vessel Atherosclerotic Disease . . . . . . . . . . 115 Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 Pediatric Stroke and Stroke in the Young . . . . . . . . . 126 Cerebrovascular Disease and Interventional Neurology: Cognitive and Behavioral . . . . . . . . . . . . . . . . . 127 Endovascular and Interventional Neurology, and Stroke and Vascular Neurology Highlights in the Field . . 32 Controversies in Neurology Plenary Session . . . 128 Continued Challenges of the Neurohospitalist Model of Care Cerebrovascular Disease Clinical Trials Plenary Session Update on Endovascular Treatment of Cerebrovascular Diseases Child Neurology and Developmental Neurology C17 C32 C36 C49 C68 C80 I4 P1 C91 P2 P3 C101 P4 S42 Attention Deficit Hyperactivity Disorder Across the Lifespan Child Neurology I EEG in Children: Developmental Maturation, Variants, Epilepsy Syndromes, and Identification of Surgical Candidates Child Neurology II Stroke in Childhood and Adolescence Stroke in Young Adults Recent Advances in Translational Research in Autism . . . . . . . . . . . . . . . . . . . . . 45 Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 Advances in Autism Spectrum Disorders and Intellectual Disability: From Genetics to Clinical Practice Poster Session II . . . . . . . . . . . . . . . . . . . . 56–63 Presidential Plenary Session . . . . . . . . . . . . . 64 Poster Session III . . . . . . . . . . . . . . . . . . . . 70–77 Neuro Flash: Child Neurology Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 Child Neurology I . . . . . . . . . . . . . . . . . . . . . . 103 Included with registration Registration fee required H1 Child Neurology Highlights in the Field . . . . . . . . . . 29 C119 Syndromes of Autonomic Dysfunction in Children and Adolescents Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 P6 Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 P7 S60 Child Neurology II . . . . . . . . . . . . . . . . . . . . . . 127 C141 Neurodevelopmental Disabilities Across the Lifespan Epilepsy/Clinical Neurophysiology (EEG) C2 I1 C36 C41 S1 C51 C73 P1 C89 P2 C99 P3 P4 S29 P5 S43 H2 P6 S50 C125 P7 S59 C146 C157 C165 How to Analyze Spells by Video-EEG Temporal Lobe Epilepsy and Febrile Seizures . . 42 EEG in Children: Developmental Maturation, Variants, Epilepsy Syndromes, and Identification of Surgical Candidates Neurophysiologic Intraoperative Monitoring Skills Workshop Section Topic Controversies: ICU EEG Monitoring: Seizures in Critically Ill Patients . . . . . . . . . . . . . . 42 Algorithms in the Diagnosis and Treatment of Epilepsy Clinical EEG Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 Neuro Flash: Epilepsy Poster Session II . . . . . . . . . . . . . . . . . . . . 56–63 Epilepsy Skills Pavilion Poster Session III . . . . . . . . . . . . . . . . . . . . 70–77 Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 Epilepsy and Clinical Neurophysiology: Inflammation, Status Epilepticus, and Genetics . . . . . 91 Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 Epilepsy and Clinical Neurophysiology (EEG): Cognition . 103 Epilepsy Highlights in the Field . . . . . . . . . . . . . . . 29 Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 Epilepsy and Clinical Neurophysiology (EEG): Electrophysiology, Imaging, and Functional Connectivity . 115 Status Epilepticus Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 Epilepsy and Clinical Neurophysiology (EEG): Reproduction, Health Care Delivery, and Co-morbidities 127 Clinical Epilepsy Therapy of Epilepsy Critical Care EEG Monitoring General Neurology C19 Controversies in Brain Death Determination C20 Neuro Flash: MRI and Multiple Sclerosis C24 Global Health Challenges: Neurology in Developing Countries Fast, Easy Registration Online · AAN.com/view/AM14 35 Annual Meeting Programs by Topic C26 Introduction to Genetics H13 C29 Multiple Sclerosis Overview I: Basic and Translational Science Endovascular and Interventional Neurology, and Stroke and Vascular Neurology Highlights in the Field . . 32 H14 Women’s Issues in Neurology Highlights in the Field . . . 32 C34 Neuroimaging for the General Neurologist: Brain Controversies in Neurology Plenary Session . . . 128 C37 C131 Test Your Knowledge: Therapy in Neurology A Case-based Approach to Neuroimaging C48 Autoimmune Neurology C52 Neuroimaging for the General Neurologist: Spine and Peripheral Nerve C136 Important Drug Interactions for C62 Continuum Test Your Knowledge: A Multiple-Choice Question Review C144 Neurology Update II C69 Improving Accuracy of Dementia Diagnosis: Case Studies with Both Imaging and Neuropathology C153 Imaging and Genomics for Detecting Neurodegenerative Proteinopathy in Clinical Practice C161 Neurologic Complications of Medical Disease C72 Neurology Update I C74 Genetics in Neurology C78 Tales from the Front Cover: Effective Book Writing and Publishing for Neurologists P1 Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 C91 Advances in Autism Spectrum Disorders and Intellectual Disability: From Genetics to Clinical Practice C94 Borderlands of Neurology and Internal Medicine C9 Differential Diagnosis of Neurologic Infections Presidential Plenary Session . . . . . . . . . . . . . 64 C24 C97 Emergency Neurology Global Health Challenges: Neurology in Developing Countries I5 Revolution of Genetic Tools and the Impact on Neurology . . . . . . . . . . . . . . . . . . 68 C67 Infections of the Nervous System I: Common Infections P3 Poster Session III . . . . . . . . . . . . . . . . . . . . . . 77 Hot Topics Plenary Session . . . . . . . . . . . . . . 80 P2 Poster Session II . . . . . . . . . . . . . . . . . . . . 56–63 P4 Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 S10 HIV, PML, and Cerebral Malaria . . . . . . . . . . . . . . 67 Contemporary Clinical Issues Plenary Session . . 89 Hot Topics Plenary Session . . . . . . . . . . . . . . 80 S31 General Neurology I . . . . . . . . . . . . . . . . . . . . . 91 P4 Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 I8 Clinical Decision Making After the Dust Settles on Clinical Trials . . . . . . . . . . . . . . . 93 I10 The Global Burden of Neurological Diseases . . . . . . . 117 C108 Neurologic Issues in Pregnancy P5 Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 S40 General Neurology II . . . . . . . . . . . . . . . . . . . . 103 C117 Principles of Genomic Medicine: Whole Exome Sequencing in Neurologic Disease C118Neurotoxicology C119 Syndromes of Autonomic Dysfunction in Children and Adolescents P6 Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 Frontiers in Neuroscience Plenary Session . . . . 112 S52 General Neurology III . . . . . . . . . . . . . . . . . . . . 115 C121 Office Orthopedics for the Neurologist C124 Clinical E-Pearls 36 Neurologists and Psychiatrists C164 Practical Psychopharmacology for Neurologists C167 Mitochondrial Disorders in Neurology C169 Common Neurologic Problems in Adults with Intellectual and Developmental Disabilities Global Health and Infectious Disease C83 Infections of the Nervous System II: Advanced and Emerging Infections C132 Neuro Flash: Approach to Acute CNS Infections Headache C18 Therapy of Headache C64 Introduction to Primary Headache Disorders C81 Chronic Migraine Education Program P1 Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 S3 Section Topic Controversies: PFO: Aggressive Treatment or Just Aspirin . . . . . . . . . . . 65 C100 The Intractable Headache Patient S32 Headache: Basic Science and Imaging . . . . . . . . . . 91 P4 Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 S41 Headache: Clinical . . . . . . . . . . . . . . . . . . . . . 103 P7 Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 H5 Headache and Facial Pain Highlights in the Field . . . . . 29 H12 Adult Intellectual and Developmental Disabilities Highlights in the Field . . . . . . . . . . . . . 32 P6 Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 I9 Emerging Concepts in Headache Therapy . . . . . . . . 116 2O14 Scientific Abstract Listing and Annual Meeting Information Subspecialty in Focus Track Leadership Development P7 Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 C140 Hot Topics in Headaches and Related Disorders C158 Psychogenic Movement Disorders C168 Therapy of Movement Disorders: A Case-based Approach Neurology Year in Review Plenary Session . . . . 133 C159 Challenging Headache Cases Included with registration Registration fee required MS and CNS Inflammatory Disease Movement Disorders C16 C12 The Dystonias: Diagnosis, Treatment, and Update on Causes C23 Hyperkinetic Movement Disorders: Diagnosis and Treatment C28 Botulinum Toxins: Practical Issues and Clinical Uses for Neurologists Multiple Sclerosis Essentials C20 Neuro Flash: MRI and Multiple Sclerosis C29 Multiple Sclerosis Overview I: Basic and Translational Science C47 Multiple Sclerosis Overview II: Clinical Advances C70 Controversies in Multiple Sclerosis Therapy P1 Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 C44 Update on Ataxias C90 Therapy of Multiple Sclerosis C53 Clinical Usefulness of Botulinum Toxin and P2 Poster Session II . . . . . . . . . . . . . . . . . . . . 56–63 S4 MS and CNS Inflammatory Disease: Clinical Trials . . . . 66 S13 MS and CNS Inflammatory Disease: MRI Atrophy Measures and Correlations . . . . . . . . . 67 Treatment of Dystonia Skills Pavilion C58 Hallucinations in Parkinson’s Disease C71 Movement Disorders P1 Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 P3 Poster Session III . . . . . . . . . . . . . . . . . . . . 70–77 P2 Poster Session II . . . . . . . . . . . . . . . . . . . . 56–63 S14 S7 Parkinson’s Disease: Preclinical and Clinical Therapeutics . . . . . . . . . . . . . . . . . . . . 66 MS and CNS Inflammatory Disease: Animal and In Vitro Studies . . . . . . . . . . . . . . . . . . . . . 78 S23 C95 Deep Brain Stimulation Management MS and CNS Inflammatory Disease: Novel Therapeutics . . . . . . . . . . . . . . . . . . . . . 79 P3 Poster Session III . . . . . . . . . . . . . . . . . . . . 70–77 S17 Parkinson’s Disease: Genetics and Epidemiology . . . . . 78 Hot Topics Plenary Session . . . . . . . . . . . . . . 80 C101 Neuro Flash: Child Neurology C102 Balance and Gait Disorders C106 Integrative Management of MS P4 Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 S24 Diet and Hormonal Influences in MS . . . . . . . . . . . 90 S33 Cognition Fatigue in MS . . . . . . . . . . . . . . . . . . 91 I7 Emerging Therapeutic Advances in Multiple Sclerosis . . 92 P5 Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 S34 MS and CNS Inflammatory Disease: Risk Factors for MS Disease and Course102 Multiple Sclerosis Highlights in the Field . . . . . . . . . 29 P4 Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 Contemporary Clinical Issues Plenary Session . . 89 S27 Dystonia, Tremor, and Other Movement Disorders . . . . 90 H6 P5 Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 C114 Morning Report: Multiple Sclerosis S37 Clinical Aspects of Parkinson’s Disease . . . . . . . . . 102 P6 Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 H5 Movement Disorders Highlights in the Field . . . . . . . 29 S44 MS and CNS Inflammatory Disease: Neuroimaging I . . 114 C116 Learning Movement Disorders in Hindsight: S53 MS and CNS Inflammatory Disease: Biomarkers and Therapeutic Mechanisms . . . . . . . . 115 P6 Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 P7 Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 S47 Movement Disorders: Huntington’s Disease, Ataxia, and Wilson’s Disease . . . . . . . . . . . . . . . 114 S54 MS and CNS Inflammatory Disease: Neuroimaging II . . 126 S63 Neuromyelitis Optica and Autoimmune Encephalitis . . 127 P7 Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 Controversies in Neurology Plenary Session . . . 128 S57 Movement Disorders: Imaging . . . . . . . . . . . . . . 126 C129 Case Studies: Multiple Sclerosis Lessons from My Patients C127 Case Studies: Unusual Movement Disorders C139 Neuromyelitis Optica: Scientific and Clinical Update C134 Parkinson’s Disease Management: Pearls, Pitfalls, and Future Prospects C138 Parkinson’s Disease and Movement Disorders Update Clinical Trials Plenary Session . . . . . . . . . . . . 131 C152 Symptomatic Management in Multiple Sclerosis Neurology Year in Review Plenary Session . . . . 133 Neurology Year in Review Plenary Session . . . . 133 C162 Diagnostic Dilemmas in Multiple Sclerosis Fast, Easy Registration Online · AAN.com/view/AM14 37 Annual Meeting Programs by Topic Neuro Trauma, Critical Care, and Sports Neurology C38 Neurologic Intensive Care S1 Section Topic Controversies: ICU EEG Monitoring: Seizures in Critically Ill Patients . . 42 P4 S26 C112 P5 C82 Sports Neurology: Non-Concussion Overview S36 S3 Section Topic Controversies: PFO: Aggressive Treatment or Just Aspirin . . . . . . . . 65 P6 S11 Neuro Trauma, Critical Care, and Sports Neurology . . . 67 C97 Emergency Neurology P7 Hot Topics Plenary Session . . . . . . . . . . . . . . 80 S56 S46 C101 Neuro Flash: Child Neurology S61 C109 Emergency Room Neuro-ophthalmology C126 C110 Sports Concussion and Other Mild Concussive Injuries P5 Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 H15 Critical Care Highlights in the Field . . . . . . . . . . . . 29 H11 Sports Neurology Highlights in the Field . . . . . . . . . 29 C120 Consultations in the Medical Surgical ICU C121 Office Orthopedics for the Neurologist C122 Traumatic Brain Injury C142 S64 Concussion in the Military and in Sports Section Topic Controversies: Pain: Methods of Treatment . . . . . . . . . . . . . . . . 132 I12 Concussion in Sports and the Military . . . . . 132 Neurology Year in Review Plenary Session . . . . 133 C155 Cumulative Sports Concussion and Risk of Dementia C165 Critical Care EEG Monitoring Neuromuscular and Clinical Neurophysiology (EMG) C1 Clinical Approach to Muscle Disease C8 Evaluation and Management of Autonomic Disorders C22 You Make the Call—An Interactive, Multimedia, Case-based Approach to Learning EMG C27 Clinical EMG I C45 Clinical EMG II C57 Small Fiber Neuropathies: Sensory, Autonomic and Both C76 EMG Skills Workshop: Basic S2 Cancelled P1 Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 C93 Therapy of Neuromuscular Disease P2 Poster Session II . . . . . . . . . . . . . . . . . . . . 56–63 S6 Neuromuscular Disease: Gene Therapy I . . . . . . . . . 66 I6 Peripheral Neuropathies . . . . . . . . . . . . . . . . . . 69 P3 Poster Session III . . . . . . . . . . . . . . . . . . . . 70–77 S16 Neuromuscular and Clinical Neurophysiology (EMG): Clinical Trials and Therapy . . . . . . . . . . . . . . . . . 78 38 C133 C143 C148 C160 Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 Biomarkers in Neuromuscular Diseases . . . . . . . . . . 90 Neuromuscular Bedside Rounds Skills Pavilion Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 Neuromuscular Disease: Clinical . . . . . . . . . . . . . 102 Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 Neuromuscular Disease: Genetics, Pathogenesis, and Measures . . . . . . . . . . . . . . . 114 Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 Anterior Horn Disease . . . . . . . . . . . . . . . . . . . 126 Muscle Disease: Gene Therapy and Models . . . . . . . 127 Case Studies: Unusual Diagnostic and Management of Cases in Neuromuscular Disease The Spectrum of Motor Neuron Disease Peripheral Neuropathy Neuromuscular Ultrasound Skills Workshop Neurology Year in Review Plenary Session . . . . 133 Neuromuscular Junction Disorders Neuro-oncology C65 Neurologic Complications of Systemic Cancer Poster Session III . . . . . . . . . . . . . . . . . . . . 70–77 P3 S22Neuro-oncology . . . . . . . . . . . . . . . . . . . . . . 79 Neuro-oncology Highlights in the Field . . . . . . . . . . 29 H8 Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 P7 C130 Case Studies: Neurologic Consultations in Cancer Patients Clinical Trials Plenary Session . . . . . . . . . . . . 131 C150 Neuro-oncology: Primary Brain Tumors Neuro-ophthalmology/Neuro-otology C15 Top 10 Neuro-ophthalmic Diagnoses You Can’t Afford to Miss C39Neuro-ophthalmology C56 Neuro Flash: Neuro-ophthalmology S2 Cancelled C87 Eye Movement Disorders: A Systematic Approach to the Evaluation of Diplopia Poster Session II . . . . . . . . . . . . . . . . . . . . 56–63 P2 S19 Neuro-ophthalmology/Neuro-otology I . . . . . . . . . . 79 C104 Nystagmus: An Organized Approach C109 Emergency Room Neuro-ophthalmology S39 Neuro-ophthalmology/Neuro-otology II . . . . . . . . . 103 H9Neuro-ophthalmology/Neuro-otology Highlights in the Field . . . . . . . . . . . . . . . . . . . . 29 Poster Session VI . . . . . . . . . . . . . . . . . . . 104–111 P6 2O14 Scientific Abstract Listing and Annual Meeting Information Subspecialty in Focus Track Leadership Development Included with registration Registration fee required C123 Neuro-ophthalmology and Neurovestibular Exam Lab Skills C61 Resident and Fellow Career Breakfast: The Early Years Clinical Trials Plenary Session . . . . . . . . . . . . 131 C66 Teleneurology and Technologies C75 Women in Leadership Philanthropy 101 Pavilion C149Neuro-otology C77 Neuro-rehabilitation C85 C40 Spine Neurology: Assessment and Management of Common Spine Disorders C54 Morning Report: Lumbar Radiculopathy, Improving Your Leadership Skills: A Practical Approach CQ8 Health Information Technology Colloquium: Advancements in Technology Lumbar Spinal Stenosis, Low Back Pain, and Post-Laminectomy Syndrome C86 ICD 10-CM: Essentials of Understanding and Implementation P1 Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 Presidential Plenary Session . . . . . . . . . . . . . 64 S21 Neurorehabilitation and Neural Repair . . . . . . . . . . 79 C98 Practical Legal Issues for Neurologists P4 Poster Session IV . . . . . . . . . . . . . . . . . . . . 81–88 C107 Brain Computer Interfaces: Frontiers in Neurology and Neuroscience C111 Bedside Evidence-based Medicine: H7 Neural Repair and Rehabilitation Highlights in the Field . 29 Frontiers in Neuroscience Plenary Session . . . . 112 C122 Traumatic Brain Injury How to Deconstruct Articles in Order to Take Care of Patients C115 Neuro Flash: Palliative Care for the Practicing Neurologist C163Myelopathies S49 C135 Continued Challenges of the Pain and Palliative Care Neurohospitalist Model of Care C40 Spine Neurology: Assessment and Management of Common Spine Disorders Research Methodology, Education, and History C50 Core Concepts in Pain Management C54 Morning Report: Lumbar Radiculopathy, Lumbar Spinal Stenosis, Low Back Pain, and Post-Laminectomy Syndrome S20 Pain and Palliative Care . . . . . . . . . . . . . . . . . . . 79 P7 Poster Session VII . . . . . . . . . . . . . . . . . . 118–125 C115 Neuro Flash: Palliative Care for the Practicing Neurologist S64 Practice, Policy, and Ethics . . . . . . . . . . . . . . . . . 115 Section Topic Controversies: Pain: Methods of Treatment . . . . . . . . . . . . . . . . . . . 132 C4 Resident Basic Science I: Neuropathology C7 Research Career Development Symposium: How to Be Successful in Academic Neuroscience C11 Resident Basic Science II: Neuroanatomy CQ2 Research and Technology Colloquium: From Discovery to Therapy C31 C35 Life Reimagined CQ4 Clinical Research Colloquium C59 Practice, Policy, and Ethics Resident Basic Science III: Neuropharmacology Career Development for Clinician Educators CQ6 Education Colloquium C5 Clerkship and Program Directors Conference C75 Women in Leadership C77 Philanthropy 101 C6 The Practice of Neurology: Issues in Coding and Reimbursement C78 Tales from the Front Cover: Effective Book Writing and Publishing for Neurologists and Improving Your Bottom Line C79 Strategic Grant Writing C13 Practice Survival for Neurologists: Business Strategies for Success Futures in Clinical Research Luncheon (Registration Required) . . . . . . . . . . . . . . . . . . . 23 C19 Controversies in Brain Death Determination C85 Improving Your Leadership Skills: A Practical Approach CQ1 BRAINS Colloquium: Understanding CQ3 Patient Safety Colloquium C43 E/M: Minimize Mistakes, Maximize Reimbursement CQ5 Practice Colloquium: How to Navigate and Succeed in New Payment Models CQ7 Education Research Colloquium P1 Poster Session I . . . . . . . . . . . . . . . . . . . . 48–55 C88 Hot Topics in Education (Tentative) Fast, Easy Registration Online · AAN.com/view/AM14 39 Programs by Topic Futures in Clinical Research Luncheon Mentoring Sessions (Registration Required) . C96 The History of Certain Disorders of the Nervous System Revolution of Genetic Tools and I5 the Impact on Neurology . . . . . . . . . . . . . . . . . . S30 Education, Research, and History . . . . . . . . . . . . . Clinical Decision Making After the I8 Dust Settles on Clinical Trials . . . . . . . . . . . . . . . Subspecialty in Focus Track Leadership Development 23 68 91 93 Sleep C10 Approach to Sleep Symptoms: Sleepy or Sleepless C30 Sleep for the Practicing Neurologist Clocks, Sleep, Brain Health and Disorders: I3 Impact on Mechanism, Expression, and Treatment . . . 44 Sleep Principles Applied to C84 Neurological Disease S9Sleep . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 67 Contemporary Clinical Issues Plenary Session . . 89 Poster Session V . . . . . . . . . . . . . . . . . . . .94–101 P5 H10 Sleep Highlights in the Field . . . . . . . . . . . . . . . . 29 S64 Section Topic Controversies: Pain: Methods of Treatment . . . . . . . . . . . . . . . . . . . 132 C151 Hot Topics in Sleep Neurology C156 Evaluation and Therapy of Restless Legs Syndrome and Periodic Limb Movements in Sleep C166 Interpretation of Polysomnography for the Practicing Neurologist “[At the Education Programs] I like to hear what other people are doing, even if it only confirms that we are doing the up-to-the-date thing. I learn some new ideas, things that have worked, things that haven’t worked. The best part is that [the AAN has] put everything on the web or app, which is new. Major improvement.” David Kauffman, MD Scarsdale, NY 40 Included with registration Registration fee required 2O14 Scientific Abstract Listing and Annual Meeting Information Sunday, April 27 Temporal Lobe Epilepsy and Febrile Seizures I1 8:00 a.m.–12:00 p.m. Coordinators: Shlomo Shinnar, MD, PhD, FAAN and Tallie Z. Baram, MD, PhD Invited Speaker Session: 8:00 a.m.–10:30 a.m. 8:00 a.m.–8:45 a.m. Epidemiological Aspects of Febrile Seizures, Febrile Status Epilepticus and Temporal Lobe Epilepsy Dale C. Hesdorffer, PhD 8:45 a.m.–9:30 a.m. What Are the Causal Relationships of Febrile Seizures / FSE and Temporal Lobe Epilepsy? Challenges and Emerging Answers Tallie Z. Baram, MD, PhD 9:30 a.m.–10:15 a.m. Febrile Status Epilepticus and Temporal Lobe Epilepsy: Insights from a Multi-Center Prospective Study Shlomo Shinnar, MD, PhD, FAAN 10:15 a.m.–10:30 a.m. Questions and Answers Poster Rounds: 10:30 a.m.–11:30 a.m. I1-1.001 Sequential Versus Simultaneous Polytherapy in the Treatment of Status Epilepticus Claude Wasterlain, Roger Baldwin, Jerome Niquet, Lucie Suchomelova I1-1.002 Mismatch of Structural and Functional Reorganization In Language Network asSCX Left Temporal Lobe Epilepsy Shigetoshi Takaya, Naoaki Tanaka, Hesheng Liu, Douglas Greve, Claus Reinsberger, Andrew Cole, Emad Eskandar, Steven Stufflebeam I1-1.003 Influences of Temporal Lobe Epilepsy and Temporal Lobe Resection on Olfactory Function Richard Doty, Isabelle Tourbier, Taehoon Kim, Jonathan Silas, Paul Moberg, Ashwini Sharan, Michael Sperling, Bruce Turetsky I1-1.004 Physiologic and Cortical Response to Acute Psychosocial Stress in Left Temporal Lobe Epilepsy Jane Allendorfer, Heidi Heyse, Lucy Mendoza, Jerzy Szaflarski I1-1.005 Graph Theory Based Functional Connectivity in Lateralized Temporal Lobe Epilepsy Sharon Chiang, John Stern, Jerome Engel, Harvey Levin, Zulfi Haneef I1-1.006 Factors Independently Associated with Anxiety and Depression in Epilepsy Heidi Munger Clary, Marla Hamberger I1-1.007 Efficacy of Transcranial Direct Current Stimulation on Working Memory and Mood in Patients with Temporal Lobe Epilepsy Anli Liu, Orrin Devinsky, Andrew Bryant, Ashlie Jefferson, Daniel Friedman, Mouhsin Shafi, William Barr, Daniel Press, Susan Herman, Margaret O’Connor, Steven Schachter, Alvaro PascualLeone I1-1.008 Utility of CT Perfusion (CTP) Imaging in Seizures: A Retrospective Analysis and Literature Review Aunali Khaku, Vishunmurthy Hedna, Michael Waters I1-1.009 Serum IL6, IL1β and IL1Ra Levels in Patients With Epilepsy Irem Fatma Uludag, Tarik Duksal, Yasar Zorlu, Feriha Ozkaya, Guldal Kirkali I1-1.010 Is Presurgical MEG Useful in Intractable Temporal Lobe Epilepsy? Helen Barkan, Shannon Sparrow, Ann Marie Collier, Michael Funke Data Blitz: 11:30 a.m.–12:00 p.m. 11:30 a.m. I1-2.001 11:35 a.m. I1-2.002 The Role of Toll-Like Receptor 3 in Epileptogenesis Felix Benninger, Adi Gross, Israel Steiner, Daniel Offen, Eitan Okun Human Mesial Temporal Lobe Single Neuron Dynamics During Recruitment Into a Generalizing Seizure Amrit Misra, Xianda Long, Ashwini Sharan, Michael Sperling, Karen Moxon 11:40 a.m. I1-2.003 Association Between Human Herpes Virus 6 and Hippocampal Volume in Mesial Temporal Lobe Epilepsy William Theodore, Emily Leibovitch, Bridgette Billioux, Sierra Germeyan, David Kalikhman, Sara Inati, John Heiss, Kareem Zaghloul, Steven Jacobson 11:45 a.m. I1-2.004 Virtual Car Accident Rates of Epilepsy Patients are Significantly Increased by Interictal Generalized Spike Waves Heinz Krestel, Andreas von Allmen, Christian Liechti, Maja Steinlin, Johannes Mathis, Nirkko Arto S1 Section Topic Controversies: I CU EEG Monitoring: Seizures in Critically Ill Patients 11:50 a.m. I1-2.005 Correlation Between MRI Findings of Mesial Temporal Sclerosis and Histopathological Findings Judy Li, Steve Chung 1:00 p.m.–2:30 p.m. 1:00 p.m.–1:05 p.m.Introduction: Kimford J. Meador, MD, FAAN 42 1:05 p.m.–1:45 p.m. Debate: Most Critically Ill Patients Should Undergo Continuous EEG Monitoring Pro: Lawrence J. Hirsch, MD, FAAN Con: Frank W. Drislane, MD, FAAN 1:45 p.m.–2:25 p.m. Debate: All Seizures in Critically Ill Patients Should Be Aggressively Treated and Stopped As Soon As Possible Pro: Stephan A. Mayer, MD Con: Peter W. Kaplan, MBBS, FRCP, FAAN 2:25 p.m.–2:30 p.m. Concluding Remarks: Kimford J. Meador, MD, FAAN 2O14 Scientific Abstract Listing and Annual Meeting Information Integrated Neuroscience Sessions/Section Topic Controversies New Antithrombotic Agents for Stroke Prevention 1:00 p.m.–5:00 p.m. Sunday April 27 I2 Coordinators: Seemant Chaturvedi, MD, FAAN, FAHA and Antonio Culebras, MD, FAAN, FAHA Invited Speaker Session: 1:00 p.m.–3:30 p.m. 1:00 p.m.–1:10 p.m.Introduction Antonio Culebras, MD, FAAN, FAHA 1:10 p.m.–1:40 p.m. The “New” Oral Anticoagulants for Stroke Prevention Cathy A. Sila, MD, FAAN 1:40 p.m.–2:10 p.m. Periprocedural Management of Antithrombotic Therapy Jose Biller, MD, FAAN, FACP, FAHA 2:10 p.m.–2:20 p.m.Break 2:20 p.m.–2:50 p.m. Management of Bleeding Complications Julius Latorre, MD 2:50 p.m.–3:15 p.m. Potential Futures Uses of Novel Oral Anticoagulants Mukul Sharma, MD 3:15 p.m.–3:30 p.m.Discussion Poster Rounds: 3:30 p.m.–4:30 p.m. I2-1.001 Effect of Apixaban on All-Cause Mortality in Atrial Fibrillation: An Imputed Placebo Analysis John McMurray, Robert Hart, Greg Flaker, Renato Lopes, Junyuan Wang, Michael Hanna, John Alexander, Christopher Granger, Lars Wallentin I2-1.002 Risk of Bleeding from Antithrombotic Agents (AT) in Patients with Cerebral Cavernous Malformations (CCMs). Robert Wityk I2-1.003 Diagnostic Yield of I2-1.006 The Incidence of Secondary I2-1.004 Stroke in Very Old I2-1.007 Neuroanatomical Correlates Prolonged Cardiac Rhythm Monitoring in Cryptogenic Stroke Rizwan Kalani, Richard Bernstein, Yvonne Curran, Ilana Ruff, Shyam Prabhakaran Patients Drini Dobi, Mira Kapisyzi, Jera Kruja I2-1.005 Cryptogenic Stroke with No Cause Demonstrates the Outcome Prediction Utility of TOAST Classifications in a Large Stroke Patient Sample Tyler Scullen, Dominique Monlezun, Jr, Alexander George, James Siegler, Melissa Schwickrath, Ramy El Khoury, Sheryl Martin-Schild Stroke Prevention Medication Following Hospitalization for Ischemic Stroke Justin Blackburn, Hong Zhao, Meredith Kilgore, Karen Albright of Atrial Fibrillation: A Longitudinal MRI Study Aveen Saed, Nudrat Tasneem, Malik Adil, Mushtaq Qureshi, Adnan Qureshi I2-1.009 Warfarin Associated Intracerebral Hemorrhage in Hong Kong Chinese Kay Cheong Teo, Neeraj R Mahboobani, Raymand Lee, David CW Siu, Raymond Cheung, Shu Leong Ho, Gary KK Lau, Koon Ho Chan I2-1.010 Stroke Patients and Diagnostic Testing—the Weekend Waiting Game! Sally Mathias, Jessica Lee I2-1.008 Etiologies of Intracerebral Hemorrhages from 2009-2012 at Mayo Clinic-Rochester James Klaas, Sherri Braksick, Robert Brown, Alejandro Rabinstein, Jennifer Fugate Data Blitz: 4:30 p.m.–5:00 p.m. 4:30 p.m. I2-2.001 Oral Anticoagulant Therapy Is Associated with Cerebral Microbleeds Saloua Akoudad, Sirwan Darweesh, Maarten Leening, Peter Koudstaal, Albert Hofman, Aad Van Der Lugt, Bruno Stricker, Mohammad Ikram, Meike Vernooij 4:35 p.m. I2-2.002 Mobile Cardiac Outpatient Telemetry Identifies Occult Atrial Fibrillation After Cryptogenic Stroke Erin Ingala, Jenny Jara, Emily Fessler, Brett Cucchiara, Steven Messe, Michael Mullen, Allyson Prasad, Mathew Hutchinson, Scott Kasner 4:40 p.m. I2-2.003 Use of Apixaban and Warfarin in Patients Undergoing Procedures: Insights from ARISTOTLE Renato Lopes, David Garcia, Daniel Wojdyla, Paul Dorian, John Alexander, Lars Wallentin, Fernando Lanas, Michael Hanna, Claes Held, Christopher Granger 4:45 p.m. I2-2.004 4:50 p.m. I2-2.005 Infarction Volume in Patients with Atrial Fibrillation: The Impact of Left Ventricular Stiffness Hee-Seung Ahn, Wi-Sun Ryu Direct Thrombin Inhibitors May Have a Decreased Risk of Intracerebral Hemorrhage Compared with Older Anticoagulants Sindhu Ravipati, Daniel Woo, Padmini Sekar, Charles Moomaw, Matthew Flaherty, Jennifer Osborne Fast, Easy Registration Online · AAN.com/view/AM14 43 Monday, April 28 I3 Clocks, Sleep, Brain Health and Disorders: Impact on Mechanism, Expression, and Treatment 8:00 a.m.–12:00 p.m. Coordinators: Bradley V. Vaughn, MD, FAAN and Phyllis C. Zee, MD, PhD Invited Speaker Session: 8:00 a.m.–10:30 a.m. 8:00 a.m.–8:10 a.m.Introduction Phyllis C. Zee, MD, PhD 8:10 a.m.–8:40 a.m. Neurobiology of Sleep and Wake Regulation Clifford B. Saper, MD, PhD, FAAN 8:40 a.m.–9:10 a.m. The Role of Circadian Rhythm Dysfunction in Huntington Disease A. Jennifer Morton 9:10 a.m.–9:45 a.m. Bi-directional Relationship Between Sleep, Circadian Rhythms, and Neurodegeneration David M. Holtzman, MD, FAAN 9:45 a.m.–10:15 a.m. Circadian Rhythm and Sleep in Epilepsy Mark S. Quigg, MD 10:15 a.m.–10:30 a.m. Questions and Answers Poster Rounds: 10:30 a.m.–11:30 a.m. I3-1.001 A Novel Capability for I3-1.003 Diffusion Tensor Imaging I3-1.002 Poor Sleep and White I3-1.004 Investigating the Night to Monitoring Cerebral and Systemic Hemodynamics, ECG and Actigraphy During Sleep Vladimir Ivkovic, Gary Strangman, Quan Zhang Matter Quality Among Middle Aged Adults Kristine Yaffe, Jasmine Nettiksimmons, Lenore Launer, Stephen Sidney, Mercedes Carnethon, Kristine Knutson, Diane Lauderdale, Cora Lewis, Nick Bryan as a Biomarker for REM Sleep Behavior Disorder and Parkinson’s Disease Matthew Brodsky, John Grinstead, David Lahna, Jeffrey Pollock Night Variability of REM Without Atonia in Parkinson’s Disease Samuel Bolitho, Sharon Naismith, Ron Grunstein, Zoe Terpening, Moran Gilat, Simon Lewis I3-1.005 Multiple Sclerosis Reported Fatigue: Obstructive Sleep Apnea and Abnormalities in Sleep Architecture in a Community Cohort Mark Gudesblatt, Myassar Zarif, Barbara Bumstead, Lori Fafard, Marijean Buhse, Steven Brass, Konstantina Bardhi, Steven Xian I3-1.006 Diazepam Useful in ESES Treatment Mirret El-Hagrassy, Chulaka Gunasekara, Yaman Eksioglu I3-1.007 Sleep Abnormalities in Children with Dravet Syndrome Radhika Dhamija, Maia Erickson, Erik St Louis, Suresh Kotagal I3-1.008 Nocturnal Melatonin Regulation in Post-Traumatic Vegetative State: A Possible Role for Melatonin Supplementation? Pietro Guaraldi, Elisa Sancisi, Giovanna Calandra-Buonaura, Chiara La Morgia, Valerio Carelli, Cameli Olivia, Alberto Battistini, Pietro Cortelli, Roberto Piperno I3-1.009 The Efficacy of Gabapentin Enacarbil (GEn) in Adult Patients with Severe Primary Restless Legs Syndrome (RLS): Pooled Analyses from 3 Randomized Trials Daniel Lee, William Ondo, Alon Avidan, Diego García-Borreguero, Mark Jaros, Richard Kim, Gwendoline Shang Data Blitz: 11:30 a.m.–12:00 p.m. 11:30 a.m. I3-2.001 Distinct Innervation Patterns of the Melanin Concentrating Hormone Neurons from the Basal Forebrain Structures Minjee Kim, Lindsay Agosstinelli, Thomas Scammell 11:35 a.m. I3-2.002 Comparing Periodic Limb Movements in Sleep in Subjects with and without Waking Paretic/Plegic Limbs Mark Dyken, Miriam Zimmerman, Kyoungbin Im, Deborah Lin-Dyken, Christine Glenn, Mark Blumberg, Robert Rodnitzky, Greta Sokoloff 11:40 a.m. I3-2.003 11:45 a.m. I3-2.004 Exploring The Neural Circuitry of REM Sleep Behavior Disorder In Parkinson’s Disease Using Functional MRI Samuel Bolitho, James Shine, Sharon Naismith, Ron Grunstein, Peter Bell, Simon Lewis Bright Light Therapy Improves Excessive Daytime Sleepiness Associated with Parkinson’s Disease Aleksandar Videnovic, Angelica Marconi, Teresa Kuhta, Scott Miskevics, Phyllis Zee S2 Cancelled 44 2O14 Scientific Abstract Listing and Annual Meeting Information 11:50 a.m. I3-2.005 Antibodies Against the Cell Adhesion Molecule Iglon5 Identify a Novel Tauopathy with NREM/REM Parasomnia and Sleep Breathing Disorder Carles Gaig, Lidia Sabater, Ellen Gelpi, Luis Bataller, Jan Lewerenz, Estefania Torres-Vega, Angeles Contreras, Bruno Giometto, Yaroslau Compta, Cristina Embid, Isabel Vilaseca, Alex Iranzo, Joan Santamaria, Josep Dalmau, Francesc Graus 1:00 p.m.–2:30 p.m. Integrated Neuroscience Sessions/Section Topic Controversies I4 Recent Advances in Translational Research in Autism 1:00 p.m.–5:00 p.m. Coordinators: Margaret L. Bauman, MD, FAAN and Martha R. Herbert, MD, PhD Invited Speaker Session: 1:00 p.m.–3:30 p.m. 1:00 p.m.–1:10 p.m.Introduction Autism Spectrum and Epilepsy Spectrum Frances E. Jensen, MD 1:40 p.m.–2:10 p.m. GI and Autism from Research and Clinical Point of View Kara Gross, MD 2:10 p.m.–2:40 p.m. Autism, GI, MET Genes, and Connectivity Theory Pat Levitt, PhD 2:40 p.m.–3:10 p.m. Mitochondrial Dysfunction, Purinergic Signaling, ASD, and Clinical Trials Robert Naviaux, MD, PhD 3:10 p.m.–3:30 p.m. Questions and Answers Monday April 28 1:10 p.m.–1:40 p.m. Poster Rounds: 3:30 p.m.–4:30 p.m. I4-1.001 SHANK3 Overexpression Causes Manic-like Behavior with Unique Pharmacogenetic Properties Jimmy Holder, Huda Zoghbi I4-1.002 Predictors of Response to I4-1.004 Knockout of p75NTR in Cerebellar Purkinje Cells Results in an Autism-like Murine Phenotype Nina Schor, Deborah Cory-Slechta, Louis Lotta, Katherine Conrad Propranolol for Social Functioning in Autism Spectrum Disorder David Beversdorf, Rachel Zamzow, Brad Ferguson, Tamera Martin, Morgan Lewis, Janine Stichter I4-1.005 Resting State EEG Serves I4-1.003 Cognitive and I4-1.006 Behavioral Profiles of Developmental Predictors of ASD in Infants with Tuberous Sclerosis Complex. Shafali Jeste, Joyce Wu, Damla Senturak, Mustafa Sahin, Charles Nelson as a Promising Biomarker of Cognitive and Language Function in Young Children with ASD. Kevin McEvoy, Shafali Jeste Children and Adolescents with Specific Language Impairment and High Functioning Autism Marisela Dy, Angela Ballantyne, Doris Trauner I4-1.007 Mean EEG Coherence in Infants at Risk for Autism Spectrum Disorder April Levin, Marc Shi, Helen Tager-Flusberg, Charles Nelson I4-1.008 Genetic Animal Models I4-1.010 Intrinsic Excitability Defects in Specific Subtypes of Medial Prefrontal Cortex Pyramidal Neurons in a Mouse Model of Autism Audrey Brumback, Vikaas Sohal of Autism Based on Shank/ Mutation Molecules to Potential Therapeutics Craig Powell I4-1.009 Autistic Symptoms in a Geriatric Population with Mild Cognitive Impairment and Early Dementia Danielle Crawford, Erin Abner, Paul Glaser, Gregory Jicha Data Blitz: 4:30 p.m.–5:00 p.m. 4:30 p.m. I4-2.001 Abnormal White Matter Connectivity in Children with Autism or Sensory Processing Disorder: Overlap and Divergence. Elysa Marco, YiShin Chang, Julia Owen, Shivani Desai, Julia Harris, Susanna Hill, Anne Arnette, Pratik Mukherjee 4:35 p.m. I4-2.002 4:40 p.m. I4-2.003 Delayed Low Level Visual Processing in Infants with Tuberous Sclerosis Complex (TSC) Pilar Pichon, Jordan Ko, Charles Nelson III, Shafali Jeste Value of Routine EEG in Autistic Patients with Stereotypic Behavioral Movements Ankit Nayyar, Neha Mirchandani, Rebecca Spiegel 4:45 p.m. I4-2.004 High-Functioning Autistic Children Have Abnormal Stapedial Reflexes Richard Lukose, Randy Kulesza, Kevin Brown, Barber Carol 4:50 p.m. I4-2.005 Reduction in Retinal Nerve Fiber Layer Thickness in Young Adults with Autism Spectrum Disorders Matteo Pardini, Leonardo Emberti Gialloreti, Francesca Benassi, Sara Marciano, Mario Amore, Maria Giulia Mutolo, Maria Cristina Porfirio, Paolo Curatolo “[The Annual Meeting is] so exciting because you see the faces of the people whose papers you have read. People are usually accessible and you can network with them.” Salvatore Di Mauro, MD New York, NY Fast, Easy Registration Online · AAN.com/view/AM1445 Introducing ePosters! The new ePoster session will take place in the poster hall, April 28 through May 1 and will feature digital presentations of select scientific posters. This new format will allow authors to feature compelling visual components, such as: ¡ Images ¡ Video ¡ 3D Models For location of the ePoster session, see the poster session floor plan on the next page. April 26 – May 3, 2014 Philadelphia, PA Poster Session Floor Plan Poster Session Schedule Monday, April 28 P1 Poster Session I 3:00 p.m.–6:30 p.m. 5:00 p.m.–6:30 p.m.* ePosters Tuesday, April 29 015 014 013 012 011 P2 Poster Session II 7:30 a.m.–11:00 a.m. 7:30 a.m.–9:00 a.m.* 016 017 018 019 020 P3 Poster Session III 3:00 p.m.–6:30 p.m. 5:00 p.m.–6:30 p.m.* Wednesday, April 30 P4 Poster Session IV 7:30 a.m.–11:00 a.m. 7:30 a.m.–9:00 a.m.* P5 Poster Session V 3:00 p.m.–6:30 p.m. 5:00 p.m.–6:30 p.m.* Thursday, May 1 P6 Poster Session VI 7:30 a.m.–11:00 a.m. 7:30 a.m.–9:00 a.m.* P7 Poster Session VII 3:00 p.m.–6:30 p.m. 5:00 p.m.–6:30 p.m.* 021 022 023 024 025 026 027 028 029 030 060 059 058 057 056 055 054 053 052 051 061 062 063 064 065 066 067 068 069 118 117 116 115 114 113 112 111 110 119 120 121 122 123 124 125 126 127 176 175 174 173 172 171 170 169 168 177 178 179 180 181 182 183 184 185 234 233 232 231 230 229 228 227 226 235 236 237 238 239 240 241 242 243 292 291 290 289 288 287 286 285 284 293 294 295 296 297 298 299 300 301 350 349 348 347 346 345 344 343 342 031 032 033 034 035 036 037 038 039 040 050 049 048 047 046 045 044 043 042 041 070 071 072 073 074 075 076 077 078 079 109 108 107 106 105 104 103 102 101 100 128 129 130 131 132 133 134 135 136 137 167 166 165 164 163 162 161 160 159 158 186 187 188 189 190 191 192 193 194 195 225 224 223 222 221 220 219 218 217 216 244 245 246 247 248 249 250 251 252 253 283 282 281 280 279 278 277 276 275 274 302 303 304 305 306 307 308 309 310 311 341 340 339 338 337 336 335 334 333 332 080 081 082 083 084 085 086 087 088 089 099 098 097 096 095 094 093 092 091 090 138 139 140 141 142 143 144 145 146 147 157 156 155 154 153 152 151 150 149 148 196 197 198 199 200 201 202 203 204 205 215 214 213 212 211 210 209 208 207 206 254 255 256 257 258 259 260 261 262 263 273 272 271 270 269 268 267 266 265 264 312 313 314 315 316 317 318 319 320 321 331 330 329 328 327 326 325 324 323 322 Poster Board Size All posters are 4 feet high by 6 feet wide. 010 009 008 007 006 005 004 003 002 001 Discussion Posters *First authors stand by posters Fast, Easy Registration Online · AAN.com/view/am14 47 Monday, April 28 P1 Poster Session I First Authors stand by Posters from 5:00 p.m.–6:30 p.m. 3:00 p.m.–6:30 p.m. oster Discussion Session: Aging, Dementia, and Cognitive and Behavioral P Neurology I Utilizing a guided tour format, topic experts will lead attendees around the ten posters in the poster discussion session and facilitate questions with poster authors during the 90-minute author stand-by time. P1.001 Complementary and Alternative Medicine Use Among Patients with Cognitive Impairment in Singapore Wahab Hameed, Simon Kang Seng Ting P1.004 Aerobic Physical Exercise Stabilizes Cognitive Status in NonDemented Elderly: An In-Patient Pilot Study. Manuel Seijo-Martinez, José María Cancela Carral, Ayán Pérez Carlos P1.007 P1.002 P1.005 P1.008 Museum-based Creative Arts Programming Is Associated with Less Dementia Patient Apathy and Better Caregiver Well-being Hannah Roberts, Carolyn Halpin-Healy, Rebecca McGinnis, James Noble P1.003 Evaluation of a Multidisciplinary “Brain Fitness Program” for Treatment of Cognitive Impairment with Aging Majid Fotuhi, Mark Trullinger, Brooke Lubinski, Mehdi Ghasemi Comparative Effectiveness of an Advanced Treatment Protocol for Dementia Versus Standard Community Care Emilymarie Clionsky P1.006 Extended-release Daily Memantine Provides Increasing Cumulative Benefits Across Clinical Domains Over 24 Weeks in Patients with Moderate to Severe Alzheimer’s Disease: An Analysis of Area Under the Curve Alireza Atri, Suzanne Hendrix, Vojislav Pejovic, Stephen Graham Predictors of Response to 13.3 mg/24 h Rivastigmine Patch in Patients with Severe Alzheimer’s Disease Martin Farlow, Carl Sadowsky, Drew Velting, Xiangyi Meng, Zahur Islam Efficacy of 13.3 mg/24 h versus 4.6 mg/24 h Rivastigmine Patch on Activities of Daily Living in Severe Alzheimer’s Disease: A Factor Analysis Joseph Micca, Drew Velting, Xiangyi Meng P1.009 Cognitive Efficacy of 13.3 mg/24 h versus 4.6 mg/24 h Rivastigmine Patch in Severe Alzheimer’s Disease: Severe Impairment Battery Factor Analysis Steven Ferris, Richard Isaacson, Drew Velting, Xiangyi Meng P1.010 Bayesian Longitudinal Modeling on Placebo Data from Alzheimer’s Disease Clinical Studies YunFei Chen, Richard Mohs, Ying Ding, Paul Aisen, Ronald Thomas NEW! e Poster Session: Movement Disorders I The ePoster session will feature a selection of posters to be presented digitally, rather than in the traditional format. Authors will be able to take advantage of the format to highlight compelling visual features such as images and videos. See poster map on page 47 for location. P1.011 Validation of a Functional Biomarker of Brain Energy Deficit in Huntington Disease Fanny Mochel, Isaac Mawusi Adanyeguh, Daisy Rinaldi, Romain Valabregue, Alexandra Durr, Pierre-Gilles Henry P1.012 Correlating OCT Changes with Disease Severity and Cognitive Status in Parkinson’s Disease Shirin Vartak, Thomas Guttuso, Jesper Hagemeier, Cheryl Kennedy, Rebecca Melia, Ellen Carl, David Lichter, Robert Zivadinov General Neurology I P1.021 AML Presenting as Autonomic Autoimmune Ganglionopathy Joel Phillips, Elmoatazbellah Ibrahim, Mirela Cerghet, Naganand Sripathi, Javier Arias-Stella III P1.022 Extensor Posturing and a Cingulate Gyrus Lesion: An Unusual Case Atul Ramesh, Daniel Labovitz, Shouri Lahiri, Alexis Boro 48 P1.013 Deep Brain Stimulation in X-linked Dystonia-Parkinsonism (DYT3/ Lubag): Partial Results from a Prospective Trial of 12 Cases Aloysius Domingo, Norbert Brüggemann, Roland Dominic Jamora, Cid Diesta, Jose Aguilar, Simone Zittel, Anne Weissbach, Dirk Rasche, Alexander Münchau, Raymond Rosales, Lillian Lee, Volker Tronnier, Christine Klein P1.015 P1.014 Progressive Supranuclear Palsy (PSP): Diagnosis Through Skin Biopsy Ildefonso Rodriguez-Leyva, Ana Calderon-Garcidueñas, Martha Santoyo, Erika Chi, Verónica Medina-Mier, Maria Jimenez-Capdeville P1.016 P1.023 P1.025 Neurologic Imaging and Electroencephalogram Findings After Chasing the Dragon Kelly Andrzejewski, Michael Devereaux P1.024 Trends in Outcome and Cost of Hospitalization of Mechanically Ventilated Adult Myasthenia Gravis Patients from 1992 to 2009 Weizhen Wang, Ankit Pahwa, Nizar Souayah Parkinson Risk in Ashkenazi Jewish Gaucher Patients and GBA Heterozygotes: Is There a Gene Dose Effect? Roy Alcalay, Tama Dinur, Timothy Quinn, Karina Sakanaka, Oren Levy, Cheryl Waters, Stanley Fahn, Tsvyatko Dorovski, Wendy Chung, Michael Pauciulo, William Nichols, Huma Rana, Manisha Balwani, Louise Bier, Deborah Elstein, Ari Zimran Combined Fenobam and Amantadine Signigficantly Reduce Levodopa-Induced Dyskinesia in the 1-Methyl-4-Phenyl-1,2,3,6Tetrahydropyridine (MPTP)-Lesioned Primate Model of Parkinson’s Disease Maurizio Facheris, Wai Kin D Ko, Elsa Pioli, Qin Li, Steve McGuire, Alison Urkowitz, Audrey Dufour, Erwan Bezard, Todd Sherer Assessment of Mortality in Sporadic Inclusion Body Myositis: A Delphi Panel Technique Victoria Barghout, Mark Price, Olivier Benveniste, Lisa ChristopherStine, Alastair Corbett, Marianne De Visser, David Hilton-Jones, John Kissel, Thomas Lloyd, Ingrid Lundberg, Frank Mastaglia, Tahseen Mozaffar, Merrilee Needham, Jens Schmidt, Kumaraswamy Sivakumar, Carla Demuro, Brian Tseng 2O14 Scientific Abstract Listing and Annual Meeting Information P1.017 Quantifying Musician Performance using MIDI Analysis Before and After EMG-Guided Botulinum Toxin Injections for Focal Task-Specific Dystonia Miriam Sklerov, Sarah Boschung, Seth Pullman P1.018 Kinematic Assessments Effectively Guide Botulinum Neurotoxin Type A Injections For Essential Tremor Treatment Jack Lee, Fariborz Rahimi, Olivia Samotus, Mandar Jog P1.019WITHDRAWN P1.020WITHDRAWN P1.026 Neurologic Involvement in Val122 Ile Familial Amyloidosis Sami Khella, Brian Drachman, Patricia Divito, Michael Polydefkis, Thomas Brannagan, Daniel Judge, Mathew Maurer P1.027 Paraneoplastic Cerebellar Degeneration with Castleman Disease: A Case Report Sarah Lee, Scheherazade Le Poster Session I Search for Autoantibodies Targeting the Nodes of Ranvier in Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP) Panos Stathopoulos, Harry Alexopoulos, Angie Biba, Domna Karagogeos, Marinos Dalakas P1.029 Barriers to Discharge: A Quality Improvement Project Anh-Thu Tran, Thuy-Anh Vu, Sandeep Kahlon P1.030 NAIL-ing the Diagnosis: Real Neurologists Pay Attention to the Nails Shin Beh, Teresa Frohman, Amy Conger, Darrel Conger, Laura Balcer, Peter Calabresi, David Zee, Elliot Frohman P1.031 Cancer Risks Among the Users of Ergot-Derived Dopamine Agonists for Parkinson’s Disease: A Population-Based Case-Control Survey Vinchi Wang, Chao Tzu-Hao P1.032 Modulation of the Default-Mode Network and the Attentional Network by Self-Referential Processes in Patients with Disorder of Consciousness Mirta Villarreal, Verónica Mäki-Marttunen, Lisandro Olmos, Ramón Leiguarda P1.033 P1.042 The Underlying Mechanisms of Autophagy in Age-related Sensitivity to Parkinsonian Pathogenesis Ya-Ping Yang, Hui-Fen Zheng, Cheng-Jie Mao, Fen Wang, Li-Fang Hu, Chun-Feng Liu P1.043 The Role of AlphaSynuclein Oligomerisation in Parkinson’s Disease Sonia Gandhi, Mathew Horrocks, Plamena Stroh, Marthe Ludtmann, Emma Deas, Nicholas, W Wood, David Klenerman, Andrey Abramov P1.044 Generation of Alpha Synuclein (Snca) Cell Models for High-Throughput Drug Screening Using Zinc-Finger Nuclease Technology Warunee Dansithong, Khanh Thai, Sharan Paul, Stefan Pulst, Duong Huynh P1.045 Ataxin-2 (Atxn2) Regulates Rgs8 Expression via Rna Interaction Sharan Paul, Warunee Dansithong, Stefan Pulst P1.046Sodium-Potassium Atpase Inhibitors as Inhibitors of Atxn2 Expression Daniel Scoles, Lance Pflieger, Thomas Dexheimer, David Maloney, Anton Simeonov, Ajit Jadhav, Stefan Pulst Ehlers-Danlos Syndrome and Postural Tachycardia Syndrome: A Relationship Study Daniel Wallman, Anna Hohler, Janice Weinberg P1.047 P1.034 P1.048 Postural Tachycardia Syndrome Associated with Ferritin Deficiency Daniel Wallman, Anna Hohler, Janice Weinberg, Zetta Fayos P1.035 How Safe Is Acute High Dose Corticosteroid Therapy in Neurological Disorders? Itai Lotan, Liora Fireman, Avi Weizman, Israel Steiner P1.036 A Case of Paraneoplastic Cerebellar Degeneration Associated with Non-Cutaneous Metastastic Merkel Cell Carcinoma Cen Zhang, Eric Lancaster P1.037 Expanding the Clinical Spectrum of Neuromyelitis Optica: Three Cases with Brainstem Involvement Faria Amjad, Sean Gratton, Benjamin Osborne, Carlos Mora, Carmelo Tornatore P1.038 Longitudinally Extensive Spinal Cord Osmotic Myelinolysis Lina Rodriguez, Scott Silliman P1.039 A Diagnostic Algorithm for Paroxyasmal Kinesigenic Dyskinesia Jasita Sachar, Krishe Menezes, A. Rothner P1.040 Two-Year Experience of Neuronal Surface Antibodies Mediated Encephalitis Diagnostic Screening in 450 Patients_A Single Center Study from China Lei Liu, Jiawei Wang Movement Disorders: Basic Mechanisms P1.041 Cellular Response to Deep Brain Stimulation in a Rat Model Vinata Vedam-Mai, Massoud Baradaran-Shoraka, Alex Mafdali, Sara Ardila, Eun Mi Kim, Jamie Schwarz, Brent Reynolds, Michael Okun Co-expression Networks in Generation of Induced Pluripotent Stem Cells (Ipscs) Lance Pflieger, Sharan Paul, Fuying Gao, Giovanni Coppola, Stefan Pulst Optical Coherence Tomography in Parkinson’s Disease: Retinal Structural Injury and Insights Into Disease Pathology Aashka Shah, Jessica Chorostecki-Vigrass, Ginny Bao, Fen Bao, Carla Santiago Martinez, Veronica Gorden, Christina Caon, Edwin George, Natalya Shneyder, Navid Seraji-Bozorgzad, Shana Krstevska, Elliot Frohman, Omar Khan P1.049 Rare Variant Pathway Analysis Highlights the Importance of Lysosomal Pathways in Parkinson Disease Jeffery Vance, Karen Nuytemans, Gary Beecham, Vanessa Inchausti, LizMarie Maldonado, Eden Martin, William Perry, Liyong Wang, Margaret Pericak-Vance, William Scott P1.050 The Relationship Between Dietary Intake, Nutrition Status and Huntington’s Disease Severity Esther Cubo, Jessica Rivadeneyra, Natividad Mariscal, Diana Armesto, Ana Mateos, Rafael Camara Neuromuscular Disease: Basic Science P1.051 Neuronal Activity Drives Presynaptic pH Regulation: Insights from Live Fluorescent pH Imaging in Drosophila Melanogaster Motor Nerve Terminals. Adam Rossano, Gregory Macleod P1.052 Familial Amyotrophic Lateral Sclerosis with Novel p62 Immunopositive Intra-Neuronal Nuclear and Axonal Spheroid Inclusions Raphael Schneider, Phedias Diamandis, Lorne Zinman, Ekaterina Rogaeva, Janice Robertson, Julia Keith P1.053 Long-term Electrophysiologic Assessment of a Mild Mouse Model of Spinal Muscular Atrophy Seward Rutkove, Jia Li P1.054 A Mouse Model of Adult Polyglucosan Body Disease (Apbd), a Late Onset Variant of Glycogen Storage Disease Type IV (GSD IV). Hasan Akman, Valentina Emmanuele, Sindu Krishna, Salvatore DiMauro P1.066 P1.055 Paraneoplastic Antibodies in Patients with Amyotrophic Lateral Sclerosis Michael Rosario, Richard Bedlack P1.067 P1.056Autopsy-proven P1.068 Amyotrophic Lateral Sclerosis Coexisted with Parkinson Disease: A Novel Association of TDP-43 Proteinopathy and α-Synucleinopathy Yuishin Izumi, Hiroyuki Sumikura, Koji Fujita, Masaki Kamada, Yoshimitsu Shimatani, Ryosuke Miyamoto, Hidetaka Koizumi, Yoshimichi Miyazaki, Hiroyuki Hatsuta, Hiroyuki Nodera, Yoshihiko Nishida, Shigeo Murayama, Ryuji Kaji P1.057 Genetic Background Effects on Lifespan of Dynactin P150 Glued Mouse Models of Motor Neuron Disease Terry Heiman-Patterson, Juliann Jiang, Philip Wong, Guillermo Alexander, Elizabeth Blankenhorn P1.058 Oligomerization of ZASP, a Myofibrillar Myopathy Gene Product, in Vitro and in Vivo Lisa Brubaker, Rachel Ohman, Ian Chow, Xiaoyan Lin, Ami Mankodi P1.059 Pathogenic Antigen-Specific Th17 Cells Drive Autoimmunity Myasthenia Gravis Yonghao Cao, Margarita Dominguez-Villar, Robert Amezquita, Shuqiang Liu, Steven Kleinstein, Jonathan Goldstein, Richard Nowak, Kevin O’Connor P1.060 IgG from Guillain-BarréSyndrome (GBS) Patients Alter Autonomic Nerve Fiber Function in Mice Christian Ritter, Ilja Bobylev, Abhijeet Joshi, Gereon Fink, Helmar Lehmann Neuropathy: Animal Models and Experiments P1.061 Characterization of a New Animal Model of Chronic Inflammatory Demyelinating Polyneuropathy Laurent Kremer, Susana Brun, Wissam Beaino, Omar Taleb, Chanh Dao Lam, Nicolas Collongues, Elisabeth Trifilieff, Jerome De Seze P1.062 CCR2 Gene Deletion and Pharmacologic Blockade Ameliorate a Severe Murine Experimental Autoimmune Neuritis Model of Guillain-Barré Syndrome. Eroboghene Ubogu P1.063 Segmental Demyelination in Fig4 Deficiency Bo Hu, Qing Yan, Jun Li P1.064 Phenotype in the Heterozygous R98C Knock-in Mouse Model of CMT1B Is not Improved by Neuregulin 1 Type III Overexpression Yunhong Bai, Chiara Pisciotta, Suola Wang, Xingyao Wu, Laura Feltri, Lawrence Wrabetz, Michael Shy P1.065 Disruption of Myelin Junctions and Increase of Myelin Permeability in PMP22 Deficiency Bo Hu, Jiasong Guo, Yang Yang, Leiming Wang, Jiawen Wu, Sezgi Arpag, Bruce Carter, Ueli Suter Induced Pluripotent Stem Cell Based Models of CMT1A and HNPP Robert Baloh, Irina Epifantseva, Kevin Kim, Shaughn Bell, Sharon Carmona, Sharday Grant, Megan Simpkinson, Matthew Harms, Dhruv Sareen, AKMG Muhammad The Effect of Hyperglycemia on Human Schwann Cells Nizar Souayah, Hongxin Chen The Effect of Glucose on the Response of Peripheral Nerve to Anoxia Mark Stecker, Matthew Stevenson P1.069 Noninvasive Peroneal Sensory and Motor Nerve Conduction Studies in the Rabbit Distal Hindlimb: Feasibility, Variability and Response to Vincristine John Hotson Neuromuscular Disease: Pathogenesis and Pathology P1.070 NADPH Oxidases (NOX) Enzymes Induced Oxidative Stress in CIDP Patients Andrea Calvo, Giuseppe Marrali, Paolina Salamone, Federico Casale, Paolo Cugnasco, Cristina Caorsi, Antonio Amoroso, Leonardo Lopiano, Adriano Chio, Dario Cocito P1.071 New Markers For Demyelination in Diabetic Neuropathy: A Novel Strategy Nizar Souayah, Ankit Pahwa, Hongxin Chen P1.072 Spinal Nerve Root Hypertrophy as Etiology of Back Pain in CIDP Alexis Shaefer, Mohammad Alsharabati, Gwendolyn Claussen, Shin Oh P1.073 Investigating the Amyloid Properties of TDP-43 in ALS and FTLDTDP Shan Desai, Eileen Bigio P1.074 Pulsatile TH2 Shift of Recovering TCR-Vβ Expanded T-Helper Effector Cells After Initiation of IVIG Treatment in CIDP Martin Russwurm, Michael Pütz, Tine Höft, Kerstin Schlegel, Michael Happel, Christian Eienbröker, Maria Seipelt, Bjorn Tackenberg P1.075 The Investigation of Effects of Alpha Lipoic Acid in the Sciatic Nerve and Brain Tissue of Rats Were Created in Experimental Diabetes Muhammed Said Berilgen, Irem Tasci, Murat Gonen P1.076 Post Mortem Measurement of Intra-Epidermal Nerve Fiber Density: A Novel Research Tool Christopher Taicher, Eugene Dulaney, Felix Eckenstein, Michael Hehir, Waqar Waheed, Julian Sprague, Rup Tandan P1.077 Clinicopathologic Analysis of TDP-43 Expression in the Cerebral Cortex in ALS Ryoko Takeuchi, Mari Tada, Atsushi Shiga, Takuya Konno, Yasuko Toyoshima, Osamu Onodera, Masatoyo Nishizawa, Akiyoshi Kakita, Hitoshi Takahashi P1.078 Morphological and Mechanical Abnormalities Detected in Tissue-Engineered Reconstructed Skin Equivalents Derived from ALS Patients Nicolas Dupre, Peter Gould, Stephan Saikali, Francois Gros-Louis Fast, Easy Registration Online · AAN.com/view/AM14 49 Monday April 28 P1.028 Monday, April 28 Iatrogenic Spinal Cord Infarction in the Central Artery Distribution Following Cervical Foraminotomy Thananan Thammongkolchai, Pichet Termsarasab, Bashar Katirji Autonomic Neuropathy Anterior Horn Cell Disease: Pathogenesis and Pathology P1.090 P1.079 P1.080 Role of NOX2 Enzyme Activity in Neuroinflammation: Preliminary Results in Amyotrophic Lateral Sclerosis and Parkinson’s Disease Andrea Calvo, Paolina Salamone, Giuseppe Marrali, Federico Casale, Giuseppe Fuda, Cristiana Caorsi, Antonio Amoroso, Maurizio Zibetti, Mario Rizzone, Leonardo Lopiano, Adriano Chio P1.081 Fast Skeletal Muscle Troponin Activator Tirasemtiv Increases Muscle Function and Performance in the B6SJLSOD1G93A ALS Mouse Model Fady Malik, Darren Hwee, Adam Kennedy, Julie Ryans, Jeffrey Jasper P1.082 “Reporting Biomarkers” in ALS: Experiences from a Pilot Compassionate Use Program Applying G-CSF—Mobilized Hematopoietic Stem Cells in ALS-Patients Ines Kobor, Dobri Baldaranov, Andrei Khomenko, Siw Johannesen, Jochen Grassinger, Katja Kollewe, Susanne Petri, Jan Kassubek, Albert Ludolph, Michael Deppe, Gerhard Schuierer, Tim-Henrik Bruun, Wilhelm Schulte-Mattler, Ulrich Bogdahn P1.083 Mutations in ERBB4 That Disrupt the NRG-ErbB4 Pathway Cause Autosomal Dominant Familial ALS Type 19 Yuji Takahashi, Yoko Fukuda, Jun Yoshimura, Atsushi Toyoda, Kari Kurppa, Hiroyoko Moritoyo, Veronique Belzil, Klaus Elenius, Guy Rouleau, Asao Fujiyama, Shinichi Morishita, Jun Goto, Shoji Tsuji P1.084 Does Altered Growth Hormone Secretion Underlie the Development of Hypermetabolism in Amyotrophic Lateral Sclerosis: Studies in HSOD1G93A Mice Pamela McCombe, Shyuan Ngo, Frederick Steyn P1.085 Familial Adult Spinal Muscular Atrophy Associated with VAPB Gene Marcos de Freitas, Victor Kosac, Osvaldo Nascimento, Frederico Prado P1.086 Is the Decrease in PGC1Α Detected in ALS Patients an Up Stream Effector or a Byproduct of Mitochondrial Dysfunction? Rawan Albadareen, Russell Swerdlow P1.087 Atypical Features in a Spinal and Bulbar Muscular Atrophy Patient with a 68 CAG Repeat Christopher Grunseich, Ilona Kats, Laura Bott, Ke-lian Chen, Angela Kokkinis, Carlo Rinaldi, Kenneth Fischbeck P1.088 Phosphorylated Tau Is a Candidate Biomarker for Amyotrophic Lateral Sclerosis Murray Grossman, Lauren Elman, Leo McCluskey, Corey McMillan, Ashley Boller, John Powers, Katya Rascovsky, William Hu, Leslie Shaw, David Irwin, Virginia Lee, John Trojanowski 50 P1.089 Carbidopa: A Novel Approach to Treating Paroxysmal Hypertension in Afferent Baroreflex Failure Lucy NorcliffeKaufmann, Jose-Alberto Palma, Jose Martinez, Horacio Kaufmann Cardiac Sympathetic Denervation Without Lewy Bodies in a Case of Multiple System Atrophy Glen Cook, Patricia Sullivan, Courtney Holmes, David Goldstein P1.091 Early Predictors of Delayed Neurocardiogenic Syncope in Tilt Table Testing Mohammed Hussain, Derrick Blackmore, Bilal Qarni, Zaeem Siddiqi P1.092 Gastrointestinal Dysmotility in Postural Tachycardia Syndrome Adam Loavenbruck, Wolfgang Singer, David Sletten, Phillip Low, Adil Bharucha P1.093 Co-Morbidities of Neuropathic Postural Orthostatic Tachycardia Syndrome and of the Autonomic Neuropathies Kamal Chemali, Kevin Mc Neeley P1.094 Delayed Orthostatic Hypotension: Implications for Autonomic Testing and Prognosis Christopher Gibbons, Roy Freeman P1.095 Disproportionate Pupillary Impairment in Diabetic Autonomic Failure Doyle Yuan, Elaine Spaeth, Steven Vernino, Srikanth Muppidi P1.096 Determinants of Vagal Baroreflex sensitivity and Normative Data Naoki Wada, Wolfgang Singer, Tonette Gehrking, David Sletten, Phillip Low Cerebrovascular Disease and Interventional Neurology: Translational Science P1.097 Carotid Wall Tension and White Matter Lesion Katsuhiko Kohara, Yoko Okada, Masayuki Ochi, Tokihisa Nagai, Michiya Igase, Tetsuro Miki P1.098 Effects of Memantine and Clopidogrel Alone and in Combination on Cerebral Ischemia in Rats Hasan Özdemir, Selçuk Ilhan, Caner Demir, Bekir Akgün, Oktay Kapan, Ataş Eser, Muhammed Said Berilgen, Metin Balduz P1.099 Post-stroke Administration of Ethanol and Normobaric Oxygen Preserves Oxidative Metabolism by Modulating Pyruvate Dehydrogenase Complex in Transient and Permanent Ischemic Stroke Omar Elmadhoun, Changya Peng, Xiaokun Geng, Murali Guthikonda, Yuchuan Ding P1.100PKC-δ and Akt Signaling in Reduced Apoptosis by Ethanol After Transient Ischemic Stroke Adam Hafeez, Xiaokun Geng, Murali Guthikonda, Yuchuan Ding P1.101 The Importance Of Measuring Cerebrospinal Fluid Biomarkers In Cardiac Arrest Survivors Hans Rosén, Christoffer Rosén, Ulf Andreasson, Daniel Bremell, Rosemary Bremler, Lars Hagberg, Lars Rosengren, Kaj Blennow, Henrik Zetterberg 3:00 p.m.–6:30 p.m. P1.102 The Effect of Tissue Plasminogen Activator on the Rodent Brain Proteome Zamir Merali, Meah Gao, Tim Bowes, Jian Chen, Andrea Kassner P1.114 P1.103 P1.115 Increased Frequency of Circulating BDBF+ T Regulatory Cells in Subjects with Acute Ischaemic Stroke Pamela McCombe, Jun Yan, Judith Greer P1.104 Hemorheology of Clinically Silent Multifocal Vascular Cerebral Lesions Piotr Kowal, Izabela Siemieniak, Anna Marcinkowska-Gapińska Factor VIII as a Predictor of Stroke Etiology Michael Halstead, Ambert Yeh, Laurie Schluter, Dominique Monlezun, Jr, Alexander George, Corinne Schild, Ramy El Khoury, Sheryl Martin-Schild Neuroprotection Against Ischemic Brain Injury with Methylene Blue Julio Rojas, Erik Plautz, Ann Stowe, Mark Goldberg Cerebrovascular Disease and Interventional Neurology: Ischemic Stroke Subtype P1.105 P1.116 Cerebrovascular Disease and Interventional Neurology: Antiplatelet Agents and Miscellaneous P1.117 Impact of Stroke on Aβ1-40 and Aβ1-42 Plasmatic Levels Solene Moulin, Didier Leys, Susanna SchraenMaschke, Regis Bordet P1.106 A Concentration Response Relationship Between the Active Metabolite of Clopidogrel and its Antiplatelet Activity Francis Gengo, Steve Wolff, Erica Westphal, Michelle Rainka, Vernice Bates P1.107 Topical Diclofenac Does Not Affect the Antiplatelet Properties of Aspirin as Compared to the Intermediate Effects of Oral Diclofenac: a Prospective, Randomized, Complete Crossover Study Francis Gengo, Nezami Brigette, Erica Westphal, Michelle Rainka, Meghan Rowcliffe, Vernice Bates P1.108 Platelet Response to Increased Aspirin Dose in Patients Whose Platelets Were Non-Responsive to Lower Aspirin Doses Erica Westphal, Francis Gengo, Michelle Rainka, Matt Robson, Maurice Hourihane, Vernice Bates P1.109 Clopidogrel Enhances Platelet Responsiveness to Aspirin Erica Westphal, Francis Gengo, Michelle Rainka, Lisa Kurczewski, John Hourihane, Vernice Bates P1.110 Safety and Efficacy of Fondaparinux for Venous Thromboembolism Prophylaxis After Acute Ischemic Stroke Santosh Ramanathan, Konark Malhotra, Chris Hackett, Melissa Tian, Matthew Quigley, David Wright, Crystal Wong, Ashis Tayal P1.111 Primary Prevention of Stroke in Argentina: a Missed Opportunity? Data from the ARENAS Registry Ana Atallah, Osvaldo Fustinoni, Ricardo Beigelman, Maria Zurru, Sebastian Ameriso, Juan Cirio, Guillermo Burry P1.112 Combination Therapy of Intravenous Glycoprotein IIB-IIIA Inhibitors and Tissue Plasminogen Activator for Acute Ischemic Stroke Anshudha Sawhney, Divyanshu Dubey, Chirantan Banerjee P1.113 Updated Meta-analysis of Hemodilution in Acute Ischemic Stroke Timothy Chang, Matthew Jensen 2O14 Scientific Abstract Listing and Annual Meeting Information Cryptogenic Stroke with More than One Cause Versus No Cause by TOAST Classification Lacks Adequate Predictive Power for Stroke Risk Factors and Outcomes Tyler Scullen, Dominique Monlezun, Jr, Alexander George, James Siegler, Melissa Schwickrath, Ramy El Khoury, Sheryl Martin-Schild Compare the Functional Outcome in Ischemic Strokes Based on the TOAST Classification. Anand Patel, Zabeend Mahuwala, Kaustubh Limaye, Nicolas Bianchi, Archana Hinduja, Rajan Patel P1.118 Cryptogenic Stroke with No Cause Demonstrates the Outcome Prediction Utility of TOAST Classifications in a Large Stroke Patient Sample Tyler Scullen, Dominique Monlezun, Jr, Alexander George, James Siegler, Melissa Schwickrath, Ramy El Khoury, Sheryl Martin-Schild P1.119 GCS Greater than NIHSS Baseline and TOAST Predicts Better Outcomes in Stroke Patients Adam Friedant, Dominique Monlezun, Jr, Alexander George, Ramy El Khoury, Sheryl Martin-Schild P1.120 Stroke of Cryptogenic Greater than One Cause_Shared Major and Minor TOAST Classifications Shoichi Shimamoto, Dominique Monlezun, Jr, Tyler Scullen, Alexander George, Corbin Pomeranz, James Siegler, Melissa Schwickrath, Ramy El Khoury, Sheryl Martin-Schild P1.121 Stroke Risk Factors, Subtypes, and 30-Day Case Fatality in Abuja, Nigeria Sunday Bwala P1.122 Seasonal Differences and Circadian Variation in Stroke Occurrence and Stroke Subtypes Rohit Bhatia, Kishan Raj, Mamta Singh, M Padma, Kameshwar Prasad P1.123 Cross-Border Acute Ischemic Stroke Subtype Comparison Between Hispanics and Mexican Mestizos Mario Cerdan-Trevino, Leonel Cantu-Martinez, Ramiro Mora-Villalvazo, Hector Martinez, Richard Hughes, Sharon Poisson P1.124 Hypercoagulability and Vasculitis Unlike Cardioembolic Etiology Predict Bilateral Infarcts David Lorance, Dominique Monlezun, Jr, Alexander George, Sheryl Martin-Schild, Ramy El Khoury Poster Session I P1.125 Utility of Workup for Thrombophilias in a Single Center—A Qualitative Perspective Akshay Shah, Nicolaas Anderson, Kendra Drake, Maria Proytcheva, Bruce Coull Cerebrovascular Disease and Interventional Neurology: Atrial Fibrillation and Miscellaneous P1.126 Thoracoscopic Pulmonary Vein Isolation and Atrial Appendage Ligation (TPVIAL) versus Medical Management in Atrial Fibrillation Patients with Prior Stroke Michael Waters, Vishunmurthy Hedna, Anna Khanna, William Miles, Catherine Price, Ilona Schmalfuss, Debra Robertson, Ashkan Karimi, Thomas Beaver P1.127 Neuroanatomical Correlates of Atrial Fibrillation: A Longitudinal MRI Study Aveen Saed, Nudrat Tasneem, Malik Adil, Mushtaq Qureshi, Adnan Qureshi P1.128 Prognostic significance of Baseline EKG findings and its Association with Future Vascular Event Anmar Razak, Vishal Jani, Syed Hussain, Abraham Maaz, Ali Saeed, Adnan Sadar, Adil Malik, Adnan Qureshi P1.129 Sinus Bradycardia Localizes Where? Johanna Hamel, Trenton Tollefson P1.130 Frequency of Atrial Arrhythmias in Stroke: Prolonged Monitoring of Cardiac Rhythm for Detection of Atrial Fibrillation After a Cerebral Ischemic Event (PEAACE) study Yaseen Ibrahim, Ghazala Basir, Esseddeeg Ghrooda, Askar Mohammad, Nazim Khan, Peter Dobrowolski, Sajad Ghualmhusein, Ashfaq Shuaib P1.131 Diagnostic Yield of Prolonged Cardiac Rhythm Monitoring in Cryptogenic Stroke Rizwan Kalani, Richard Bernstein, Yvonne Curran, Ilana Ruff, Shyam Prabhakaran P1.132 Gaze Deviation in Acute Stroke: Neuroimaging Evidence, Significance and Clinical Correlation Nabeel Herial, Rema Raman, Karin Ernstrom, Clarity Coffman, Konrad Schlick, Karen Rapp, Royya Modir, Dawn Meyer, Thomas Hemmen, Brett Meyer P1.133 Development of National Web-based Registry for Acute Stroke Leopold J Streletz, Naveed Akhtar, Saadat Kamran, Dirk Deleu P1.134 Revascularization in Acute Ischemic Stroke Based on Clinical-Diffusion Mismatch (REVASC): A Planned Phase I Trial Nazli Janjua P1.135 Stroke and Cerebrovascular Risk Factors Knowledge in Patients Admitted to a Cardiovascular Ward. Francisco Muñoz Giacomelli, Maria Gonzalez Toledo, Fatima Pagani Cassara, Agustina Tamargo, Alejandro Thomson, Diego Nadile, Andres Ferre, Francisco Klein Cerebrovascular Disease and Interventional Neurology: Rehabilitation and Recovery P1.136 Inter-individual Variability in Motor and Language Recovery During the Acute Stroke Period Ronald Lazar, Lauren Dunn, Adam Schweber, Daniel Manson, Andrea Lendaris, Randolph Marshall P1.137 Factors Influencing SelfPerception of Recovery from Stroke in Comparison to Objective Assessments T. Keta Hodgson, Randy Sanoff, Gillian Devereux, Star Feudi, Samantha Cherin, Fiona Chatfield, Robin Conwit, Scott Hamilton, Nerses Sanossian, Sidney Starkman, Jeffrey Saver P1.138 Use of HIRREM, a NonInvasive Neurotechnology, Is Associated with Improved Autonomic Function and Decreased Temporal Hemispheric Asymmetry in A 67 Year Old Male with a Recent Stroke Charles Tegeler, Jared Cook, Catherine Tegeler, Sung Lee, Jasmyn Nicholas, Hossam Shaltout P1.139 A Randomized Control Trial of Granulocyte Colony Stimulating Factor (G-CSF) Intervention in Acute Ischemic Stroke to Improve Functional Outcome Sankar Gorthi, Dheeraj Nauwhar, Pawan Gupta, Kaukab Hassan P1.140 Statin Therapy Reduces Oxidized Low Density Lipoprotein and Associate with Favorable Outcome in Patients After Acute Ischemic Stroke NaiWen Tsai P1.141 WITHDRAWN P1.142 Cortical Activity Modulation by Botulinum Toxin Type A in Patients with Post-Stroke Arm Spasticity: Real and Imagined Hand Movement Petr Hlustik, Tomas Veverka, Pavel Hok, Zbynek Tudos, Pavel Otruba, Alois Krobot, Petr Kanovsky P1.143 Satisfaction with Botulinum Toxin Treatment in Post-Stroke Spasticity: Results From Two Cross-Sectional Surveys of Patients and Physicians Djamel Bensmail, Angelika Hanschmann P1.144 Long Lasting Therapeutic Effects of Yoo’s Solution for Ischemic Stroke Seo Hong Yoo Cerebrovascular Disease and Interventional Neurology: Intracranial Disease P1.145 CT Angiography Alone Can Provide Sufficient Angio-Architectual Information About Unruptured Intracranial Aneurysms to Proceed Straight to Treatment David Ben-Israel, David TurkelParrella, Ekaterina Kouzmina, Thomas Marotta, Julian Spears, Airton Leonardo de Oliveira Manoel P1.146 Treatment Trends in Management of Intracranial Stenosis in The Pre- and Post-Sammpris Era Swaroop Pawar, Tanya Turan, George Cotsonis, Michael Lynn, Rahim Wooley, Barney Stern, Colin Derdeyn, David Fiorella, Marc Chimowitz P1.147 Association Between Lipoprotein (a) Levels and Vascular Events in the Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) trial. Swaroop Pawar, Tanya Turan, Marc Chimowitz P1.148 Comparison of Intracranial Stent Placement and Best Medical Treatment Alone for Treatment of Symptomatic Intracranial Stenosis Vikram Jadhav, Mushtaq Qureshi, Adnan Qureshi P1.149 Impact of SAMMPRIS trial on Intracranial Stent Placement: A State Wide Study Farhan Siddiq, Malik Adil, Saqib Chaudhry, Adnan Qureshi P1.150 Trends in Cerebral Blood Flow Velocities of Patients with Intracranial Atherosclerotic Disease Shawna Cutting, Tatjana Rundek, Victor Del Brutto, Sebastian Koch, Ralph Sacco, Jose Romano P1.151 Association Between Intracranial Stenosis and Cerebro-renal Microvascular Damage in a Latin American Cohort. Maria Zurru, Claudia Alonzo, Laura Brescacin, Pigreti Santiago, Luis Camera, Gabriel Waisman, Edgardo Cristiano P1.152 Stroke Among Hospitalized Patients Diagnosed with Vertebrobasilar Insufficiency: A Retrospective Cohort Study Li Yang, Harrison Bai, Xin Zhao, Yanqiao Xiao, Yuanyuan Yang, Scott Kasner, Liming Tan P1.153 Long-term Stroke Recurrence in Patients with Basilar Artery Occlusion. Michael Ruff, Tamika Burrus, Alejandro Rabinstein P1.154 Postprandial Clearance of Oxidized LDL in Stroke-related Atherosclerosis Julia Rothlisberger, NgocAnh Le, Christy Cassarly, Renee Martin, Tanya Turan CNS and Disease Mechanisms in Humans and Animal Models P1.155 Oligodendrocyte Progenitor Cells (OPCs) from Adult Human Brain Expressed Distinct MicroRNAs Compared to OPCs in Development Soo Yuen Leong, Vijayaraghava Rao, Jenea Bin, Pavel Gris, Mugundhine Sangaralingam, Timothy Kennedy, Jack Antel P1.156 Astrocyte-derived VEGF-A Drives Blood-brain Barrier Disruption in CNS Inflammatory Disease. Azeb Argaw, Linnea Asp, Jingya Zhang, Trinh Pham, John Mariani, Dipankar Dutta, Elisabeth Kramer, Napoleone Ferrara, Michael Sofroniew, Gareth John P1.157 Cytokine Influence on Oligodendrocyte Progenitor Cell Proliferation Robert Knobler P1.158 Latent Infection of the Central Nervous System (CNS) and the ‘Inside-Out’ Model of Multiple Sclerosis (MS) Lorne Kastrukoff, Allan Lau, Eva Thomas P1.159 Protease-activated Receptor-1 (PAR-1) and Interleukin-1Beta Act Synergistically in Granzyme b Mediated Neurotoxicity Paul Lee, Avindra Nath P1.160 Myelin Sulfatides Modulate T Cell Function During Autoimmune Demyelination Marcin Mycko, Beata Sliwinska, Maria Cichalewska, Hanna Cwiklinska, Krzysztof Selmaj P1.161 Neuroendocrine Dysregulation of the T Cell Response in Early Multiple Sclerosis Dina Hartmann, Michael Pütz, Kerstin Schlegel, Christian Eienbröker, Michael Happel, Maria Seipelt, Bjorn Tackenberg P1.162 CD16+/Perforin+ Lymphocytes (NK Cells) May Regulate Autoimmunity in Multiple Sclerosis by Cytolysis of Antigen Laden Cells in the Peripheral Blood. Ramesh Nayak, Raymond Jacolik P1.163 Modeling Anti-CD20 Mediated B Cell Depletion Indicates the Role of Treg in the Response to Therapy in MS Pablo Villoslada, Sara MartinezPasamar, Elena Abad, Beatriz Moreno, Nieves Velez de Mendizabal, Ivan MartinezForero, Jordi Garcia-Ojalvo P1.164 Development of Inflammatory Demyelinating Lesions in Mouse CNS After Injection of Cerebrospinal Fluid Derived from Progressive MS Patients Massimiliano Cristofanilli, Daniel Gratch, Benjamin Pagano, Saud Sadiq P1.165 Adult Neural Progenitor Cells Derived from MS Patients Differentiate into MBP Expressing Cells in the Shiverer Mouse Massimiliano Cristofanilli, Benjamin Pagano, Daniel Gratch, Violaine Harris, Tamara Vyshkina, Saud Sadiq P1.166Hyperoxygenation Differentiates Vascular Lesions from Parenchymal Lesions Using Susceptibility Weighted MRI in Mice with Experimental Autoimmune Encephalomyelitis Nabeela Nathoo, James Rogers, V. Wee Yong, Jeff Dunn P1.167 Fgfr1 Ablation in Oligodendrocytes Reduces Disease Severity and Inflammation in the CNS in MOG35-55 Induced EAE Ranjithkumar Rajendran, Mario Giraldo Velasquez, Christine Stadelmann-Nessler, Martin Berghoff P1.168 Brain Distribution of MS565, an Imaging Analogue of Siponimod (BAF312), in Non-human Primates Adriana Tavares, Olivier Barret, David Alagille, Thomas Morley, Caroline Papin, Ralph Maguire, Emmanuelle Briard, Yves Auberson, Gilles Tamagnan P1.169 The Role of Class I Haplotype in the Development of Immune Mediated Brain Atrophy in a Murine MS Model Istvan Pirko, Jeffrey Gamez, Pascal Atanga, Stephanie LaFrance, Aaron Johnson P1.170WITHDRAWN P1.171 Il-11 Induces Th17-Cell Responses in Patients with Relapsing Remitting Multiple Sclerosis (RRMS) Silva Markovic Plese, Xin Zhang, Yazhong Tao, Irena Dujmovic-Basuroski, Jelena Drulovic Fast, Easy Registration Online · AAN.com/view/AM1451 Monday April 28 First Authors stand by Posters from 5:00 p.m.–6:30 p.m. Monday, April 28 P1.172 The Peripheral Network Between Oxidative Stress and Inflammation in Multiple Sclerosis Maira Gironi, Marina Saresella, Vittorio Martinelli, Cristina Cursano, Enrica Mariani, Matilde Vaghi, Federica Piancone, Lucia Moiola, Ivana Marventano, Mario Clerici, Giancarlo Comi, Roberto Furlan P1.185Genome-wide P1.173 P1.186 Impaired Immune Regulatory Function of Natural Killer (NK) Cells in Multiple Sclerosis (MS) Catharina Gross, Andreas Schulte-Mecklenbeck, Anna Rünzi, Antia Posevitz-Fejfar, Heinz Wiendl P1.174 Assessment of a Fluorinated Analog of N-acetylglucosamine to Promote Myelin Regeneration Michael Keough, James Rogers, Ping Zhang, Jason Plemel, Chang-Chun Ling, V. Wee Yong P1.175 Neuroprotective, AntiInflammatory and Immune Tolerizing Properties of Peptides Derived from Diffusion Survival Evasion Protein (DSEP)/ Dermcidin. Jeffrey Greenstein, Timothy Cunningham P1.176 Ingested (Oral) Tocilizumab Inhibits EAE Staley Brod, Victoria Bauer P1.177WITHDRAWN P1.178 Deletion of Virus-specific T-cells Enhances Remyelination in a Model of Multiple Sclerosis Aleksandar Denic, Bharath Wootla, Laurie Zoecklein, Moses Rodriguez P1.179 Amelioration of Experimental Autoimmune Encephalomyelitis by RNA Polymerase 1 Inhibitor: Molecular and Cellular Mechanisms Michael Gurevich, Rina Falb, Anat Achiron P1.180 Stress Induced Angioplasticity Is Protective in Experimental Autoimmune Encephalomyelitis (EAE) Vladimir Katyshev, Nilufer Esen, Svetlana Katysheva, Zakhar Serkin, Paula Dore-Duffy P1.181 Inhibition of Hyaluronan Synthesis Protects Against EAE by Inducing CXCL12 in the CNS Andre Mueller, Bo Hyung Yoon, Saud Sadiq P1.182 Anti-CD20 Therapy Downregulates Lesion Formation and Microglial Activation in Pattern I and Pattern Ii Rat Models of Multiple Sclerosis Daniel Anthony, Alex Dickens, Nicholas Seneca, Sandra Campbell, Begona Checa, Veerle Kersemans, Edward Warren, Matthew Tredwell, Veronique Gouverneur, David Leppert P1.183 Bowman-Birk Protease Inhibitor Induces Tr1 Cells and Suppress Effector Phase of EAE Disease; A Potential NOVEL Therapy for Multiple Sclerosis Farinaz Safavi, Javad Rasouli, Elisabeth Mari, Guang-Xian Zhang, Mohamad Rostami P1.184 Mir-155 Controls T Helper Cell Autoimmunity During Autoimmune Demyelination via Hsp40 Genes Expression Marcin Mycko, Maria Cichalewska, Hanna Cwiklinska, Krzysztof Selmaj 52 Pharmacogenomic Study of Response to Cannabinoids in MS Spasticity Patients Juan Ruiz, Antonio GonzálezPérez, María Isabel Garcia-Sanchez, María Eugenia Saez-Goñi, Macarena Rus Hidalgo, Miguel Lucas, Antonio Alcina, Fuencisla Matesanz, Guillermo Izquierdo Ayuso 3:00 p.m.–6:30 p.m. P1.196Natalizumab-induced Circulating Hematopoietic Stem Cells have Intact Progenitor Capacity Miriam Mattoscio, Benedetta Mazzanti, Simone Dal Pozzo, Richard Nicholas, Omar Malik, Riccardo Saccardi, Paolo Muraro P1.197 Blocking LINGO-1 Does Not Affect Inflammatory Markers in the Cerebrospinal Fluid of Individuals with Multiple Sclerosis Ann Ranger, Soma Ray, Suzanne Szak, Andrea Dearth, Normand Allaire, Diego Cadavid Differential Impact of Natalizumab and Fingolimod on the Alpha-4/Beta-1 Expression-Related Subset Diversity of T Cells Jorg Kraus, Katrin Oppermann, Julia Wanek, Georg Pilz, Peter Wipfler, Johann Sellner, Shahrzad Afazel, Elisabeth Haschke-Becher, Eugen Trinka, Andrea Harrer P1.187 P1.198 Differentiating Plovamer Acetate and Glatiramer Acetate: Efficacy and Mechanism of Action in a Preclinical Model of Multiple Sclerosis Anneli Savinainen, Kenneth Crook, Timothy Crandall, Michelle Seng, Ursula Boschert, Tammy Dellovade P1.188 Steady State Pharmacokinetics of Formulations of XP23829, a Novel Prodrug of Monomethyl Fumarate (MMF), in Healthy Subjects Dmitri Lissin, Wendy Luo, Ezra Tai, Katie Zomorodi, Dan Chen, Son Nguyen, Yongjin Yao, Virna Kim, Joan Zou, Kenneth Cundy P1.189 Preclinical Efficacy and Phase I Clinical Testing of ATX-MS1467, an Antigen-Specific Immunotherapy for Multiple Sclerosis David Wraith P1.190 The Global Neocortical Loss of Neurons in Multiple Sclerosis Daniele Carassiti, Maria Papachatzaki, Francesco Scaravilli, Klaus Schmierer P1.191 Does Axonal Degeneration Depend on Demyelination in Chronic Multiple Sclerosis? Daniele Carassiti, Shaima Al Zawawi, Klaus Schmierer P1.192 Calcitriol and Interferon-beta Treatment Act Synergistically to Induce a Less Inflammatory Response in Stimulated PBMCs Niall Stewart, Ingrid van der Mei, Bruce Taylor, Steve Simpson, Jr. P1.193 Laquinimod Reduces Neuronal Injury Through Inhibiting Microglial Activation Voon Wee Yong, Manoj Mishra, Janet Wang, Michael Keough, Claudia Silva, Yan Fan, Scott Sloka, Liat Hayardeny P1.194 Cognitive Resilience in Multiple Sclerosis: Characterization of Blood Gene Expression Profiles Associated with Preserved Cognitive Function Anat Achiron, Yoram Barak, Michael Polliack, Michael Gurevich MS and CNS Inflammatory Disease: Treatment Mechanisms of Action P1.195 Laquinimod Interferes with the Development of Follicular Helper T Cells and Germinal Center B Cells in Cns Autoimmunity Michel Varrin-Doyer, Ulf Schulze-Topphoff, Kara Pekarek, Scott Zamvil Suppressed Pro-Inflammatory Properties of Circulating B Cells in Patients with Multiple Sclerosis Treated with Fingolimod, Based on Altered Proportions of B-cell Subpopulations Yusei Miyazaki, Masaaki Niino, Toshiyuki Fukazawa, Eri Takahashi, Takayuki Nonaka, Itaru Amino, Jun Tashiro, Naoya Minami, Naoto Fujiki, Shizuki Doi, Seiji Kikuchi P1.199 Interferon-Beta Alters Monocytes and B-cells in Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis. Axtell Robert, Ryan Schubert, Lawrence Steinman P1.200 Therapy with Interferon-Beta has No Impact on the T Cell Receptor Repertoire in MS Patients Thomas Dehmel, Clemens Warnke, Anne Mausberg, Manuel Lopez, Xavier Montalban, Hans Hartung, Bernd Kieseier P1.201 Lymphocyte and Eosinophil Responses in Healthy Subjects Dosed with Tecfidera® and XP23829, a Novel Fumaric Acid Ester (FAE) Lawrence Steinman, Robert Fox, Dmitri Lissin, Katie Zomorodi, Dan Chen, Lee Clark, Kenneth Cundy P1.202 Laquinimod Regulates Inflammatory Gene Induction in a Human Model of Reactive Astrogliosis. Trinh Pham, Jingya Zhang, Jeremy Seto, Boris Hartmann, Liat Hayardeny Nisimov, Gareth John P1.203 Laquinimod Modulates Genes Encoding Cell Migration in Multiple Sclerosis Rina Zilkha-Falb, Michael Gurevich, Liat Hayardeny Nisimov, Anat Achiron P1.204 Dimethyl Fumarate and Monoethyl Fumarate Exhibit Differential Effects on Glutathione, Keap1 and Nrf2 Activation In Vitro Robert Scannevin, Melanie Brennan, Maria Matos, Xiaoping Hronowski, Benbo Gao, Peter Juhasz, Kenneth Rhodes P1.205 Fumarate Esters Are Distinguished by Differential Inhibition of the NF-κB Mediated Proinflammatory Response. Geoffrey Gillard, David Huss, John Anderson, Brian Collette, Andrea Bertolotti-Ciarlet, Robert Scannevin, Jason Fontenot 2O14 Scientific Abstract Listing and Annual Meeting Information P1.206 Dimethyl Fumarate and Monomethyl Fumarate Are Distinguished by Non-Overlapping Pharmacodynamic Effects In Vivo Melanie Brennan, Normand Allaire, David Huss, Patrick Cullen, Alice Thai, Suzanne Szak, Ankur Thomas, Davide Gianni, John Carulli, Jason Fontenot, Brian Wipke, Kenneth Rhodes, Robert Scannevin P1.207 Dimethyl Fumarate and Monoethyl Fumarate Exhibit Differential Pharmacodynamic Effects and Pharmacokinetics In Vivo Robert Scannevin, Suzanne Szak, Kristopher King, Melanie Brennan, Normand Allaire, Patrick Cullen, Alice Thai, Ankur Thomas, Davide Gianni, Alexander Chou, Theresa Hillery, Brian Wipke, Liyu Yang, John Carulli, Huang Chaoran, Kenneth Rhodes P1.208 Immunoregulation During Multiple Sclerosis Relapses. Effects of Intravenous Methylprednisolone. Vincent van Pesch, Nathalie Muls, Christian Sindic P1.209 Arsenicals May Prevent Axonal Loss in Multiple Sclerosis: A Histopathological Study Dimitrios Papadopoulos, Nikolaos Antoniou, Katerina Tsimaratou, Vassilis Gorgoulis, Dimos Dimitrios Mitsikostas, Richard Nicholas P1.210 B Cell Receptor Recognition of Glatiramer Acetate Is Required for Efficacy in Experimental Autoimmune Encephalomyelitis and Results in Differential Cytokine Production in MS Patients Leila Jackson, Sean Selva, Tracy Niedzielko, Timothy Vollmer P1.211 Pharmacokinetics and Pharmacodynamics of RPC1063 and its Metabolites in Healthy Adult Volunteers Gregg Timony, Jennifer Brooks, Jeffrey Hartung, Fiona Scott, Allan Olson, Sheila Gujrathi, Marcus Boehm, Robert Peach P1.212 Gene Expression Studies Comparing Glatiramer Acetate and Proposed Generics Benjamin Zeskind, Fadi Towfic, Jason Funt, Kevin Fowler, Shlomo Bakshi, Eran Blaugrund, Sarah Kolitz, Maxim Artyomov, Michael Hayden, Iris Grossman, Liat Hayardeny, Rivka Schwartz P1.213 HLA Genes and InterferonBeta Preparations Influence Risk of Developing Neutralizing Anti-Drug Antibodies in Multiple Sclerosis Katharina Fink, Jenny Link, Malin Lundkvist, Christina Hermanrud, Izaura Lima, Boel Brynedal, Ingrid Kockum, Jan Hillert, Anna FogdellHahn P1.214 Glatiramer Acetate Treatment Regulates CD44, Receptor for Osteopontin in EAE Mice Sakhina Begum-Haque, Marc Christy, Kiel Telesford, Yan Wang, Eli Kasper, Azizul Haque, Lloyd Kasper P1.215 Teriflunomide Does Not Significantly Affect Primary and Memory Antibody Responses to a Viral Antigen in Mice Andrea Edling, Lisa Woodworth, Adam Stockmann, Tracy Touzjian, Simon Fricker, Bruce Roberts, Johanne Kaplan Poster Session I P1.216 ATX-MS-1467, An Immunotolerizing Agent, Halts Disease Progression and Reduces CNS Inflammation in Rodent Models of Multiple Sclerosis Tammy Dellovade, Stefan Rudin, Alla Zozulya, Blake Tomkinson P1.217 UVB Light Attenuates the Systemic Immune Response in CNS Autoimmunity Johanna Breuer, Nicholas Schwab, Tilman Schneider-Hohendorf, Martin Marziniak, Hema Mohan, Urvashi Bhatia, Catharina Groß, Carsten Weishaupt, Sven Meuth, Karin Loser, Heinz Wiendl P1.218 ONO-4641 (Ceralifimod) Prevents Evoked Potential Deficits in an Animal Model of Multiple Sclerosis Daniel Crawford, Dongzi Yu, Frederic Bernard, Danielle Graham, Ursula Boschert, Tammy Dellovade P1.219 ONO-4641 (Ceralifimod) Reduces MRI Lesions and Prevents Disease Progression in an Animal Model of Multiple Sclerosis Shuning Huang, Ji-Kyung Choi, Audrey Gray, Dongzi Yu, Bruce Jenkins, Joseph Mandeville, Guangping Dai, Ursula Boschert, Tammy Dellovade, Danielle Graham P1.220 Treatment with Anti-mouse CD52 Antibody Is Associated with Preservation of Myelin and Maintenance of Axonal Conduction in the MOG-induced EAE Mouse Model Jianhua Huang, Petti Pang, Nilesh Pande, Michael Turner, Michael LaMorte, Nathalie Chretien, Carrie Garron, Bruce Roberts, Johanne Kaplan, William Siders P1.221 Lipoic Acid Reduces Inflammation in a Mouse Focal Cortical Experimental Autoimmune Encephalomyelitis Model. Priya Chaudhary, Gail Marracci, Danielle Galipeau, Edvinas Pocius, Brooke Morris, Dennis Bourdette P1.225 Application of the 2010 Macdonald’s Criteria to a Cohort of Patients with Clinically Isolated Spinal Cord Syndromes Anne Vandendriessche, Helene Zephir, Olivier Outteryck, Damien Fetter, Nicolas Collongues, Nathalie Derache, Gilles Defer, Patrick Vermersch, Jerome De Seze, David Maltete, Bertrand Bourre P1.226 MRI Phenotypes as Predictors of Clinical Outcomes in Patients with CIS in the Benefit Population Sven Schippling, Dirk Pleimes, Gilles Edan, Xavier Montalban, Mark Freedman, Hans Hartung, David Miller, Frederik Barkhof, Ernst-Wilhelm Radu, Julia Hermann, Christoph Pohl, Rupert Sandbrink, Roland Martin P1.227 Randomized Trial of Minocycline for Clinically Isolated Syndrome and Early Single Relapse Multiple Sclerosis: Study Design, Participant Characteristics, and Recruitment Challenges Luanne Metz, Anthony Traboulsee, David Li, Pierre Duquette, Michael Yeung, Marcelo Kremenchutzky, Galina Vorobeychik, Mark Freedman, Virender Bhan, Gregg Blevins, James Marriott, Francois Grand’Maison, Liesly Lee, Manon Thibault, Misha Eliasziw, V. Wee Yong, Graziela Cerchiaro, Samuel Wiebe, Yan Cheng, Guojun Zhao, Jamie Greenfield, Marites Topor, Andrew Riddehough P1.228 Predicting Response to Interferon Beta-1B Therapy in Patients with Clinically Isolated Syndrome MP Sormani, Frederik Barkhof, Ludwig Kappos, Gilles Edan, Mark Freedman, Xavier Montalban, Hans Hartung, David Miller, Julia Hermann, Vivian Lanius, Karola Beckmann, Rupert Sandbrink, Christoph Pohl, Dirk Pleimes P1.229 Anti-murine CD52 Antibody Treatment Does Not Adversely Affect the Migratory Ability of Immune Cells Evis Havari, Michael Turner, James Dodge, Christopher Treleaven, Lamya Shihabuddin, Bruce Roberts, Johanne Kaplan, William Siders Longitudinal Mixed-Effect Model Analysis of the Association Between Global and Tissue Specific Brain Atrophy and Lesion Accumulation in Patients with CIS Mihael Varosanec, Dana Horakova, Jesper Hagemeier, Niels Bergsland, Michaela Tyblova, Zdenek Seidl, Manuela Vaneckova, Jan Krasensky, Michael Dwyer, Eva Havrdova, Robert Zivadinov P1.223 P1.230 P1.222 Glatiramer Acetate: Shorttime Versus Long-time Administration—A mRNA-Seq Analysis Marc Kuehl, Paul Hammer, Ronny Amberg, Peter Beyerlein, Juergen Faiss MS and CNS Inflammatory Disease: Clinically Isolated Syndromes P1.224 An Integrated Model of Risk Factors for Predicting the Early Occurrence of a Second Attack in Patients with Clinically Isolated Syndromes Vittorio Martinelli, Gloria Dalla Costa, Giovanni Di Maggio, Bruno Colombo, Mariaemma Rodegher, Letizia Leocani, Roberto Furlan, Massimo Filippi, Giancarlo Comi CSF Neurofilament Light Chain Predicts Evolution to MS in Clinically Isolated Syndromes Stefano Zoccolella, Vita Direnzo, Carla Tortorella, Maddalena Ruggieri, Mariangela Mastrapasqua, Pietro Iaffaldano, Maria Trojano P1.231 Possible Prognostic Value of Cerebrospinal Fluid in Clinically Isolated Syndrome Eva Krasulova, Eva Havrdova, David Kemlink, Tomas Uher, Michaela Tyblova, Jana Volna, Katerina Mrazova, Dana Horakova P1.232 Natural History of Clinically Isolated Syndrome on Conversion to Multiple Sclerosis: A Metaanalysis Masako Kinoshita, Masako Daifu, Keiko Tanaka, Masami Tanaka P1.233 Predictors Factora for Risk of Conversion from Clinical Isolated Syndrom to Multiple Sclerosis in a Mixed Brazilian Cohort Juliana Aurencao, Ana Cristina Wing, Regina Maria Alvarenga, Claudia Cristina Vasconcelos P1.234 How Much Earlier Can Multiple Sclerosis be Diagnosed Using the McDonald Criteria? Wallace Brownlee, Josephine Swanton, Olga Ciccarelli, David Miller Aging, Dementia, and Cognitive and Behavioral Neurology: Basic Science P1.235 PACAP Deficit in Alzheimer’s Disease and Protection Against BetaAmyloid Toxicity PengCheng Han, Zhiwei Tang, Jun-Xiang Yin, Thomas Beach, Eric Reiman, Jiong Shi P1.236 Peptidyl-prolyl Isomerase Pin1 as a Potential Target to Protect Synaptic Function in Preclinical Alzheimer’s Disease Emily Ong, Frances Chow, Yuesong Gong, Carol Lippa P1.237 Inhibition of Quinone Oxidoreductase 2 Improves Learning in a Mouse Model of Vascular Dementia Jesse Fitzpatrick, Talaignair Venkatraman, Hana Dawson, Haichen Wang, Daniel Laskowitz, Christopher Lascola Aging, Dementia, and Cognitive and Behavioral Neurology: Biomarkers, Pathology, and Basic Science P1.245 Hereditary Diffuse Leukoencephalopathy with Spheroids (Hdls): Histological Features of Microglia Mari Tada, Takuya Konno, Masayoshi Tada, Ken-ichi Okazaki, Musashi Arakawa, Kyoko Itoh, Toru Yamamoto, Hideaki Yokoo, Nobuaki Yoshikura, Kenji Ishihara, Yasuko Toyoshima, Osamu Onodera, Masatoyo Nishizawa, Takeshi Ikeuchi, Hitoshi Takahashi, Akiyoshi Kakita P1.246 The Antibodies Against Gangliosides as Probable Biomarkers in the Serum of Demented Patients Effrosyni Koutsouraki, Eleni Hatzifilippou, Tania Banaki, Vassiliki Costa, Stavros Baloyannis P1.247 Hippocampal Laminar Distribution of Phospho-Tau Relates to Alzheimer’s Disease and Age of Death Alon Seifan, James Noble, Jesse Mez, Karen Marder, Lawrence Honig P1.248 A Beta-2 Adrenergic Agonist Attenuates Cognitive Deficits in Hippocampus of the Mice Following Systemic Inflammation Hung-Ming Wu, Wan-Yu Huang P1.249 Abnormal Hypothalamic Leptin Signaling Leads to Early Metabolic Dysfunction in Mice Overexpressing the Amyloid Precursor Protein Makoto Ishii, Costantino Iadecola Enhancement of Synaptic Plasticity in Hippocampal Neurons by RNS60, a Novel Therapeutic Containing Charge Stabilized Oxygen-Based Nanostructures. Avik Roy, Saurabh Khasnavis, Khushbu Modi, Supurna Ghosh, Richard Watson, Kalipada Pahan P1.239Amyloid-β Induces NLRP1- P1.250 P1.238 Dependent Neuronal Pyroptosis in Alzheimer’s Disease Meng-Shan Tan, Jin-Tai Yu, Teng Jiang, Xi-Chen Zhu, Hui-Fu Wang, Chuan-Dong Jia, Lan Tan P1.240 Increased Expression of Kv1.3 Channels by Microglia in Alzheimer’s Disease Srikant Rangaraju, Allan Levey P1.241 TREM2 Knockdown Exacerbates Aging-related Neuroinflammation and Cognitive Deficiency in SAMP8 Mice Jiang Teng, Jin-Tai Yu, Lan Tan P1.242 Direct Actions of Granulocyte-Colony Stimulating Factor on Human Neuronal and Monocytic Cell Lines Amanda Pennington, Vasyl Sava, Shijie Song, Niketa Patel, Juan SanchezRamos P1.243WITHDRAWN P1.244 Pathologic Aggregates of Small Nuclear Ribonucleoproteins (Snrnp) Are Present in Familial Alzheimer’s Disease Chad Hales, Eric Dammer, Duc Duong, Hong Yi, Marla Gearing, Allan Levey, James Lah, Nicholas Seyfried Therapeutic Efficacy of D-penicillamine Encapsulated Alginate Nanoparticles in Wistar Rat Model for NonWilsonian Brain Copper Toxicosis Amit Pal, Rajendra Prasad, Rakesh Vasishta, Babu Thapa P1.251 Dopamine in Social Valuation: A Genetic and Pharmacological Study Andrew Kayser, Ignacio Saez, Ming Hsu P1.252 Activation of Cannabinoid Type 2 Receptors in the Ventral Tegmental Area Modulate Dopamine Excitability via M-Type Potassium Channels. Brett Larsen, Ming Gao, Jie Wu P1.253 Insulin-Like Growth Factor-I Receptor Stimulating Activity Is Associated with Dementia Renée de Bruijn, Joseph Janssen, Michael Brugts, Cornelia van Duijn, Albert Hofman, Peter Koudstaal, Mohammad Ikram P1.254 De-efferented Motor Cortex Provides a Viable Source of Neural Activity Command Signals for Centrally-Implanted Brain Machine Interfaces Jose Morales, Karthikeyan Balasubramanian, Kazutaka Takahashi, Nicholas Hatsopoulos Headache: Basic Science P1.255 Interictal Reduced Cranial Parasympathetic Tone in Cluster Headache Hilde Karen Ofte, Therese von Hanno, Karl Alstadhaug Fast, Easy Registration Online · AAN.com/view/AM14 53 Monday April 28 First Authors stand by Posters from 5:00 p.m.–6:30 p.m. Monday, April 28 P1.256 A Survey of Cluster Headache (CH) Sufferers Using Vitamin D3 as a CH Preventative Peter Batcheller P1.257 Optical Imaging of Facial Perfusion in Migraine Jonas Peterson, Lindsay Hunter, Melissa Cortez, Jeremy Theriot, KC Brennan P1.258 The CK1δ T44A Mutation Affects Nociceptive Activation of the Trigeminocervical Complex in an In Vivo Model of Migraine Jan Hoffmann, Margarida Martins-Oliveira, Weera Supronsinchai, Simon Akerman, Michele Lasalandra, Yonglie Zhao, Lina Matsson, Elin Economou-Olsson, Hsien-Yang Lee, Louis Ptacek, Peter Goadsby P1.259 Characterization of Photosensitivity and Pupil Oscillation Rate in Migraine Lindsay Hunter, Jonas Peterson, Melissa Cortez, Jeremy Theriot, K.C. Brennan P1.260 Does Intravenous Hydration Before and After Lumbar Puncture Decrease the Occurrence of Post-Lumbar Puncture Headache? Nidhi Gupta, Agnieszka Kowalska, Justin Smith, Patricia Coyle P1.261 Treatment of Withdrawal Headache in Patients with Medication Overuse Headache (MOH): A Randomized, Single-blinded, Placebo Controlled Study Sabina Cevoli, Giulia Giannini, Valentina Favoni, Elisa Sancisi, Marianna Nicodemo, Stefano Zanigni, Daniela Grimaldi, Giulia Pierangeli, Pietro Cortelli P1.262 Non-invasive Vagal Nerve Stimulation for the Treatment of Headache Attacks in Patients with Chronic Migraine and Medication-overuse Headache Innocenzo Rainero, Paola De Martino, Elisa Rubino, Giovanna Vaula, Salvatore Gentile, Lorenzo Pinessi P1.263 Patient Satisfaction With MAP0004: Results of an Optional Survey During a Long-term Open-label Safety Study Sheena Aurora, Dawn Buse, Biao Lu, Donald Kellerman, Wade Cooper, Shashidhar Kori P1.264 Non Invasive Blood Flow Monitoring with Functional Near Infrared Spectroscopy Correlation with Pain Self-Assessment in Subjects Receiving Infusions for Chronic Migrain David Tabby, Arash Danesh, Ahmad Pourshoghi, Kambiz Pourrezaei Epilepsy and Clinical Neurophysiology (EEG): Basic Science and ICU Monitoring P1.265Androgen-mediated Effects on Ictal Behavior Among Male Rats Is Mediated Through Pregnane Xenobiotic Receptors, which Mediated Neurosteroidognesis Carolyn Koonce, Jennifer Moore, Swarup Mitra, Cheryl Frye P1.266 A Novel Mouse Model of X-linked Epilepsy Ethan Goldberg, Jian Zhou, Douglas Coulter, P. Wang 54 P1.267 Reduction of Tomyson Expression Leads to a Kindling-sensitive Phenotype in a Murine Model of Epilepsy John Slevin, Seth Batten, Elena Matveeva, Sidney Whiteheart, Thomas Vanaman, Greg Gerhardt P1.268 Spontaneous Subarachnoid Hemorrhage: Identifying Predictors of Early Outcome Using Continuous EEG. Caitlin Loomis, Scott Kasner, Michael McGarvey, Sarah Schmitt P1.269 Synchronization Analysis of Depth and Extracranial EEG Seizure Data in Subarachnoid Hemorrhage Ananda-Kriiya Fine, David Albers, J. Michael Schmidt, Deborah Pugin, George Hripcsak, Jan Claassen P1.270 Evolving Patterns on Prolonged EEG Monitoring in Patients with Therapeutic Hypothermia Post-Cardiac Arrest Andres Rodriguez-Ruiz, Brandon Foreman, Hyunmi Choi, Stephan Mayer, Jan Claassen, Sachin Agarwal P1.271 NCSE in Neuro and Medical ICU Patients on Continous EEG Monitoring Mohamed Tom, Miguel FiolElias P1.272 Pharmacologically Induced Burst Suppression in Pediatric and Adult Patients—Varying But Predictable Pattern? Luda Sorin, Brice Jabo, Travis Losey P1.273 Does the Benefit of Therapeutic Hypothermia in Refractory Status Epilepticus Depend on Seizure Etiology? Jessica Fesler, Ryan Hakimi, Shrenik Talsania, Emmaculate Fields P1.274 Role of VEEG Monitoring in Neonates with HIE Undergoing Therapeutic Hypothermia with Correlation of Seizures and Neurodevelopmental Outcome Misbah Salam, Anjum Hashim, Jasmine Singh Neural Repair and Neurorehabilitation: Basic Science P1.275 Autologous Bone Marrow Mononuclear Cells for Patients With Motor Neuron Disease—Safety and Feasibility Study Sankar Gorthi, Pawan Gupta, Satish Kumar, Premkumar Sinha, Harinder Pal Singh P1.276 Development of a Modified Central Nervous System Extracelluar Matrix with Polylysine. Eric Marrotte, Naoir Zaher, Yi Zhang, Michael Chopp, Benjamin Buller P1.277 EEG Characterization of a Cohort of Patients with Disorders of Consciousness: Linking Novel Research Results and Clinical Practice. Peter Forgacs, Mary Conte, Jonathan Victor, Nicholas Schiff P1.278 Gene Therapy with Neurotrophic Factors Improves Recovery After Sciatic Nerve Injury in Mice Mica Glat, Felix Benninger, Tali Ben-Zur, Yael Barhum, Israel Steiner, David Yaffe, Daniel Offen 3:00 p.m.–6:30 p.m. P1.279 Receptor for AGE (RAGE) Expressed in Macrophages and Neurons Regulates Peripheral Nerve Repair After Injury Lingling Rong, Shifang Yan, Arthur Hays, Clifton Gooch, Ann Marie Schmidt P1.280 Evaluation of the Performance of a Brain-Computer Interface Under Two Biofeedback Paradigms Brian Appavu, Jenessa Lancaster, Remy Wahnoun, P. David Adelson P1.281 Evoked and Oscillatory Activity Dynamics in Vegetative State Gonzalo Rivera P1.282 Functional Organization of the Human Auditory Fields: Activation of Auditory Cortex in a Patient with Auditory Agnosia from Traumatic Injury of the Inferior Colliculus, and the Effects of Transcranial Direct Current Stimulation Robert Rafal, Oren Poliva, Patricia Bestelmeyer, Nicholas Davis P1.283 The Therapeutic Capability of Slow-release 4-Aminopyridine for the Treatment of Peripheral Nerve Crush Injury Kuang-Ching Tseng, John Elfar P1.284 Predictors of Change in Quality of Life in Patients with Focal Neurological Damage Following an Outpatient Cognitive Rehabilitation Program Galeno Rojas, Adriana Leis, Natalia Ciufia, Gastón Saux, Carolina Feldberg, Fernando Caceres, Ignacio Demey History of Neurology P1.285 General Wood: Physician, Rough Rider, Ambassador, Presidential Candidate, Patient. Mariza Daras, E. Massey P1.286 Silas Weir Mitchell on Epilepsy Therapy in the Late 19th and Early 20th Centuries David Burkholder, Christopher Boes P1.287 Historical Articles in the Neurology® Journal as a Tool to Raise Awareness about the Importance of Bedside Medicine Raghav Govindarajan, John Morren, Efrain Salgado P1.288 Philadelphia Odd Couple— Silas Weir Mitchell—NeurologistNovelist-Poet and Phillips Brooks— Brahmin Prophet—Sons of 19th Century Rittenhouse Square Benjamin Brooks P1.289 Early Historical and Ethnographic Descriptions of the Properties of Curare in the Spaniards Chronicle. Carolina Vazquez, Francisco Carod P1.290 Charcot-Marie-Tooth Disease (CMT): Historical Perspectives and Evolution Mohamed Kazamel, Christopher Boes P1.291 History of Anti-inflammatories in Headache: Acetanilid, Antipyrin, Phenacetin and Salicyclic Acid Rosen Noah, Dennis Thornton P1.292 Jesuit Bark and Horseback Rides: Thomas Jefferson’s “Fits” as a Window into 18th Century Headache Care Matthew Luedke, E. Massey 2O14 Scientific Abstract Listing and Annual Meeting Information P1.293 Neurology, Volume 1, 1951 William Campbell P1.294 Robert E. Lee’s Last Stand: His Dying Words and the Stroke That Killed Him. Andrew Southerland P1.295 Introduction of the Pulfrich Phenomenon into Clinical Neurology James Lanska, Douglas Lanska, Bernd Remler P1.296 Food for Thought: A Serving of Food-Inspired Eponyms in Neurologic Practice Shin Beh, Teresa Frohman, Amy Conger, Darrel Conger, Peter Calabresi, Laura Balcer, David Zee, Elliot Frohman P1.297 125 Hysterical Years—the Contribution of Charcot’s. Francisco Branco Germiniani, Renato Munhoz, Luciano De Paola, Helio Teive P1.298 Social Network Analysis of Presidents in Neurology Professional Organizations Since 1948 Amar Dhand, Jordan Harp, Stephen Borgatti P1.299 Russell N. DeJong: A Seminal Figure in American Neurology William Campbell P1.300 History of Neurology in Bangladesh Nasheed Jamal, Shrikant Mishra, Bhavesh Trikamji P1.301 Rejected Applications: An Early American Academy of Neurology Struggles to Define its Membership Elan Louis P1.302 Description of the Pulfrich Effect James Lanska, Douglas Lanska, Bernd Remler P1.303 Gerstmann, Sträussler, Scheinker Disease: A Famous Syndrome From an Infamous Period in History Lawrence Zeidman, Matthias Ziller, Michael Shevell P1.304 Zinc-induced Myelopathy Among Smelter Workers in Upper Silesia During the Late 19th Century Douglas Lanska, Bernd Remler P1.305 The Visible Brain: Computed Tomography’s Impact on Neurological Practice Charlene Ong P1.306 Meta-analyses to Investigate Gene-environment Interactions in Neuroepidemiology Ingrid van der Mei, Petr Otahal, Steve Simpson, Bruce Taylor, Tania Winzenberg Neurology Education: Graduate Medical Education P1.307 Simulation Boot Camp for Neurology Residents: A Unique Experience From a Training Perspective Nauman Tariq, Muna Irfan, Jeffrey Willging, Elisabeth Hurliman, Fitzgerald Lisa, Danielle Hart, Carly Dolan, Ezgi Tiryaki P1.308 Educating Future Clinical Research Investigators: An 8-Week Clinical Research Education Course for Neurology Residents Jeanie McGee Poster Session I P1.309 Can Young European Neurologists Comfortably Manage Patients with Traumatic Brain, Spine or Nerve Injuries (Tbi)? Martin Rakusa, Sofya Gak, Yuri Alekseenko, Edvard Ehler, Dafin Muresanu, Josef Opara, Pieter Vos P1.310 Positive Deviance for Improvement of Efficiency and Resident Satisfaction in Neurology Continuity Clinic Julio Rojas -Martinez, Kartavya Sharma, Steven Vernino, Pravin Khemani P1.320 The Rolling Continuity Clinic: A Flexible Scheduling Paradigm Kristin Scott, Warren Carrigan, Heidi Woessner, David Capobianco, Devon Rubin, Elliot Dimberg P1.321 Implementation of Active Learning into the Pre-Clinical Neurology Undergraduate Medical Curriculum John Pula, John Nixon, Meenakshy Aiyer, Jorge Kattah P1.322 Preparing Child Neurology Residents for Inpatient Adult Neurology Emily Johnson, Tracey Milligan Heterogeneity in Neurological Education and Care in Asian and Oceanian Region Man Mohan Mehndiratta, Prachi Mehndiratta, Natasha Gulati, Mohammad Wasay P1.312 P1.323 P1.311 Clinical Neuroscience Podcasts for Family Medicine, Internal Medicine, and Neurology Residents: A Needs Assessment Study Tyson Brust, Michael Yeung P1.313 Trends in American Board of Psychiatry and Neurology Specialties and Neurologic Subspecialties Larry Faulkner, Dorthea Juul P1.314 Quantification of Postural Stability Using Accelerometer and Gyroscopic Measures from the iPad Susan Linder, Joshua Hirsch, Mandy Koop, David Schindler, Anil Thota, Jay Alberts P1.315 Effectiveness of Pairing Weekly Reading Assignments and Quiz with Audience Response System for Neurology Resident Learning Rashedul Hasan, Jennifer Fry, John DeToledo, Jongyeol Kim P1.316 Standardized Evaluation of Didactic Conference Content in Neurology Residency: A New Approach Arthie Jeyakumar, Constantine Farmakidis P1.317 Unsuccessful Lumbar Puncture: Blame it on the Patient, Not the Operator Cory Edwards, Enrique Leira, Pedro Gonzalez-Alegre P1.318 Changing Medical Student Perceptions of Dementia: An Arts-centered Experience Hannah Roberts, James Noble Neurology Education: Graduate Medical Education/ Undergraduate Medical Education P1.319 Computer Generated Checklist Significantly Improves Differential Diagnosis in Neurologic Disease Over Simple Recall Pasquale Finelli, Andrew McCabe High-Fidelity Simulation Versus Traditional Didactic Techniques for Teaching Neurological Emergencies to Neurology Residents: A Feasibility Study. Sachin Agarwal, Neha Dangayach, Priyank Patel, Ashley Roque, Melissa Cappaert, Dennis Fowler, Jan Claassen, Stephan Mayer P1.324 The One-Year Clinician Educator Curriculum: Neurology Residents as Teachers Veronica Santini, Anna Hohler P1.325 Teaching Ophthalmoscopy to Medical Students (TOTeMS) II: A One-Year Retention Study Devin Mackay, Philip Garza, Beau Bruce, Samuel Bidot, Linda Kelly, Emily Graubart, Nancy Newman, Valerie Biousse P1.326 An Interactive Mobile Curriculum for Teaching the HypothesisDriven Neurological Examination Dylan Alegria, Vanja Douglas, Chandler Mayfield, Christy Boscardin, S. Josephson, Daniel Lowenstein, Susannah Cornes P1.327 Neurologists Versus Emergency Physicians: Reliability of a Neurological Script Concordance Test in a Multi-Centre, Cross-disciplinary Setting Derek Soon, Nigel Tan, Derek Heng, Liqi Chiu, Malcolm Madhevan, Charmaine Manauis, Dong Haur Phua, Gominda Ponnamperuma, Kevin Tan P1.328 Methodology for Delivering Feedback to Neurology House Staff on Communication Skills Using AIDET (Acknowledge, Introduce, Duration, Explanation, Thank you) Austin Katona, Elisabeth Kunkel, Jasmine Arfaa, Stephen Weinstein, Christopher Skidmore P1.329 Zygosity Detection by Next Generation Sequencing in a Clinical Laboratory Zhenyuan Wang, Christine DiVincenzo, Christopher Elzinga, Martin Bazinet, Sat Dev Batish, Malgorzata Jaremko, Joseph Higgins Neurology Education and Methodology P1.330 Chasing Veins in Vain? The History of Vessel-Based Aetiological Theories and Pathological Studies in Multiple Sclerosis Aravind Ganesh, Dawn Pearson, Frank Stahnisch P1.331 National Survey of UK Medical Students on the Perception of Neurology Julia Pakpoor, Adam Handel, Giulio Disanto, Richard Davenport, Gavin Giovannoni, Sreeram Ramagopalan P1.332 Comparison of American Academy of Neurology’s online patient Education Materials to Other Common Internet Sources. Anjali Dagar, Vineet Punia, Nitin Agarwal, Wenzhuan He, Machteld Hillen P1.333 Is Formal Faculty Assessment of Bedside Skills Feasible for 3rd Year Medical Students on the Neurology Clerkship? Robert Thompson-Stone, Erika Wexler, Jonathan Mink, Ralph Jozefowicz P1.334 Network for Excellence in Neuroscience Clinical Trials, NeuroNEXT: Increasing Efficiency in Clinical Trial Management Marianne Kearney, Dixie Ecklund, Michael Bosch, Brenda Thornell, Dawn McNeil, Walter Koroshetz, Petra Kaufmann, Christopher Coffey, Merit Cudkowicz P1.335 Use of Mentored Peer Review of Standardized Manuscripts as an Educational Tool for Neurology Residents Roy Strowd, Victoria Wong, Rebeca Aragon-Garcia, Yeseon Moon, Blair Ford, Sheryl Haut, Joseph Kass, Zachary London, Mary Mays, Tracey Milligan, Raymond Price, Patrick Reynolds, David Spencer, Mitchell Elkind P1.336 Scheduled Faculty Modeling of Bedside Skills for 3rd Year Medical Students on the Neurology Clerkship Robert Thompson-Stone, Trenton Tollefson, Ronald Epstein, Ralph Jozefowicz, Jonathan Mink P1.337 Parallel Sequencing of 26 Genes Responsible for Metabolic Myopathy and Rhabdomyolysis Xia Tian, Jing Wang, Margherita Milone, Yanming Feng, Victor Zhang, Lee-jun Wong P1.338 Comprehensive Diagnosis of Congenital Neuromuscular Disorders by Next Generation Sequencing of 236 Genes with Deep Coverage Xia Tian, Wen-Chen Liang, Yanming Feng, Jing Wang, Victor Zhang, Lee-jun Wong, Yuh-Jyh Jong P1.339 Feasibility of Developing a Neurophysiologic Assessment of Concussion Nolan Williams, Jan Enabore, Emily Williams, Donna Roberts, Jonathan Edwards P1.340 ALS Clinical Research Learning Institutes: Empowering PALS to be Research Ambassadors Richard Bedlack, Merit Cudkowicz Child Neurology and Developmental Neurology I P1.341 Continuous Intravenous Valproic Acid as an Abortive Therapy for Pediatric Migraine Muhammad Zafar, Aaron Cook, Alejandra Stewart, Robert Baumann P1.342 Fatal Outcome of Status Epilepticus, Hyperthermia, Rhabdomyolysis, Multi-Organ Failure, and Cerebral Edema After 25I-NBOMe Ingestion Yoshie Umemura, Thomas Andrew, Valerie Jacobs, Andrew Giustini, Lionel Lewis, Jennifer Hanowell, James Filiano P1.343 Whole Genome Sequencing Identifies a Novel Occludin Mutation in Microcephaly with Band-like Calcification and Polymicrogyria that Extends the Phenotypic Spectrum Mahmoud Osman, Elizabeth Ross, Alice Abdel Aleem, Khalid Ibrahim, Ben-Omran Tawfeg, Hussein Kamel P1.344 A Prenatal Presentation of Severe Microcephaly and Brain Anomolies in a Patient with Novel Compound Heterozygous Mutations in the STIL Gene Harvey Bennett, Amy Presti, Darius Adams, Jose Rios P1.345 Sleep Abnormalities in Children with Dravet Syndrome Radhika Dhamija, Maia Erickson, Erik St Louis, Suresh Kotagal P1.346 Utility of Continuous EEG Monitoring in Pediatric Man in the Barrel Syndrome: A Case Report Jessica Goldstein, Bilal Zonjy, Ingrid Tuxhorn, Barbara Bangert, Nancy Bass P1.347 Prediction of Future Seizures in Neonates Who Received Selective Head Cooling for HIE Tiffani McDonough, Juliann Paolicchi, Nikkan Das, Murray Engel, Jeffrey Perlman, Zachary Grinspan P1.348 Value of Routine EEG in Autistic Patients with Stereotypic Behavioral Movements Ankit Nayyar, Neha Mirchandani, Rebecca Spiegel 2015 Education Course Proposal Process 2015 Annual Meeting: Washington, DC The AAN invites you to submit an Education Program suggestion for May 16, 2014. To submit your proposal, please visit the 67th Annual Meeting. Proposals for new programs are due by AAN.com/view/SearchAM. Fast, Easy Registration Online · AAN.com/view/AM1455 Monday April 28 First Authors stand by Posters from 5:00 p.m.–6:30 p.m. Tuesday, April 29 P2 Poster Session II First Authors stand by Posters from 7:30 a.m.–9:00 a.m. 7:30 a.m.–11:00 a.m. Poster Discussion Session: Movement Disorders II Utilizing a guided tour format, topic experts will lead attendees around the ten posters in the poster discussion session and facilitate questions with poster authors during the 90-minute author stand-by time. P2.001Cortico-striatal-thalamic Network Functional Connectivity in Hemiparkinsonism Francesca Caso, Federica Agosta, Iva Stankovic, Alberto Inuggi, Igor Petrovic, Marina Svetel, Giancarlo Comi, Vladimir Kostic, Massimo Filippi P2.002 Neuroanatomical Changes in Parkinson’s Disease: Neuroimaging Evaluation of Pedunculopontine Nucleus Fang Ba, Marguerite Wieler, Myrlene Gee, Wayne Martin P2.003 (18)FDG-PET Scan as a Predictive Marker of Postoperative Apathy After Subthalamic Nucleus Deep Brain Stimulation in Parkinson Disease. Aude Gesquiere-Dando, Eric Guedj, Tatiana Witjas, Frederique Fluchere, Marie Delfini, Laura Mundler, Jean Azulay, Alexandre Eusebio P2.004 Differential Patterns of White Matter Degradation in Relation to Cognitive and Motor Deficits in Parkinson’s Disease Yu Zhang, Norbert Schuff P2.005 Brain Functional Connectomics in Early Parkinson’s Disease Sebastiano Galantucci, Federica Agosta, Iva Stankovic, Alessandro Meani, Igor Petrovic, Marina Svetel, Giancarlo Comi, Vladimir Kostic, Massimo Filippi P2.006 Corpus Callosum Damage and Motor Function in Parkinson’s Disease Sebastiano Galantucci, Federica Agosta, Iva Stankovic, Igor Petrovic, Tanya Stojkovic, Giancarlo Comi, Vladimir Kostic, Massimo Filippi P2.007 Interval Changes of ForebrainCortical Versus Brainstem-thalamic Cholinergic Integrity in Parkinson Disease Progression Nicolaas Bohnen, Martijn Muller, Vikas Kotagal, Kirk Frey, Roger Albin P2.008 Dopaminergic Changes in Corticostriatal Brain Activity and Causal Interactions during Working Memory in Parkinson’s Disease. Kathleen Poston, Sophie YorkWilliams, Weidong Cai, David Everling, Matthew Cruadhlaoich, Michelle Fenesy, Vinod Menon P2.009 Striatal and Extrastriatal Dopamine Transporter Levels Relate to Cognition in Lewy Body Diseases Stephen Gomperts, Marta Marquie Sayagues, Joseph Locascio, Dorene Rentz, Alex Becker, Trey Hedden, Keith Johnson, John Growdon P2.010 Ascending Progression of Grey Matter Atrophy in Parkinson’s Disease Maria Cristina Arci Santos, Lidiane Campos, Rachel Guimaraes, Camila Piccinin, Paula Azevedo, Luiza Piovesana, Brunno Campos, Augusto Amato-Filho, Fernando Cendes, Anelyssa D’Abreu NEW! e Poster Session: Cerebrovascular Disease and Interventional Neurology I The ePoster session will feature a selection of posters to be presented digitally, rather than in the traditional format. Authors will be able to take advantage of the format to highlight compelling visual features such as images and videos. See poster map on page 47 for location. P2.011 PFO Closure for Stroke Prevention. A Brief Meta-analysis Leila Doldan, Manuel Latini, Jeffrey Saver P2.012 Stroke and Etonogestrel/ Ethinyl Estradiol Ring (NuvaRing): Clinical, Radiological, and Prognostic Features. Pirouz Piran, Clotilde Balucani, Brian Tark, Zachary Adler, Steven Levine P2.013 Intracranial Arterial Dissection Daiana Dossi, Mauricio Farez, Julieta Arena, Virginia Pujol Lereis, Guillermo Povedano, Sebastian Ameriso Movement Disorders: Parkinson’s Disease Genetics P2.021Neuropsychological Performance in LRRK2 G2019S Carriers with Parkinson’s Disease Roy Alcalay, Helen Mejia Santana, Anat Mirelman, Rachel Saunders-Pullman, Deborah Raymond, Laurie Ozelius, Avi Orr-Urtreger, Lorraine Clark, Nir Giladi, Susan Bressman, Karen Marder P2.014 Identifying Barriers in Acute Stroke Therapy in Argentina. ARENAS Registry Ana Atallah, Osvaldo Fustinoni, Maria Zurru, Ricardo Beigelman, Juan Cirio, Sebastian Ameriso, Guillermo Burry P2.015 Comparison of Large Vessel Stroke Patient Outcomes Before and After Initiation of On-site Endovascular Stroke Treatment Services Yamin Shwe, Santiago Ortega-Gutierrez, Amy Walker, Irene Boniece, Alejandro Berenstein, Johanna Fifi P2.022 Phenotypic Spectrum of SNCA G209A Mutation Carriers for Familial Parkinson’s Disease in Greece Dimitra Papadimitriou, Roubina Antonelou, Maria Stamelou, Maria Bozi, Matina Maniati, Nikolaos Papagiannakis, Sevasti Bostantjopoulou, Athanassios Leonardos, Sokratis Papageorgiou, Georgios Hadjigeorgiou, Eleni Kapaki, George Tagaris, Alexandros Papadimitriou, Aglaia Athanassiadou, Leonidas Stefanis P2.023 Clinical and Neuroimaging Features of a Patient with Early-onset Parkinson’s Disease with Dementia Carrying SNCA p.G51D Mutation Takayoshi Tokutake, Atsushi Ishikawa, Nahoko Yoshimura, Akinori Miyashita, Ryozo Kuwano, Masatoyo Nishizawa, Takeshi Ikeuchi 56 P2.016 The Utilization of Forced Aerobic Exercise to Augment the Recovery of Motor Function Following Stroke: A Randomized Clinical Trial Susan Linder, Anson Rosenfeldt, Amanda Penko, Jay Alberts P2.018 P2.017 Prediction of Ischemic Brain Penumbra Using Acute MR Information and Inelastic Collision Model Hassan BagherEbadian, Panayiotis Mitsias, James Ewing, Hamid Soltanian-Zadeh P2.019WITHDRAWN P2.024Neuropsychiatric P2.026 Features of GBA-Associated Parkinson Disease Matthew Swan, Robert Ortega, Matthew Barrett, Jeannie Soto-Valencia, Sarah Boschung, Andres Deik Acosta Madiedo, Harini Sarva, Jose Cabassa, Brooke Johannes, Deborah Raymond, Joan Miravite, William Severt, Rivka Sachdev, Vicki Shanker, Susan Bressman, Rachel Saunders-Pullman P2.025 Interest in Genetic Testing in Ashkenazi Jewish Parkinson Disease Patients and Their Unaffected Relatives Manisha Gupte, Roy Alcalay, Helen Mejia Santana, Deborah Raymond, Rachel Saunders-Pullman, Anat Mirelman, Lorraine Clark, Laurie Ozelius, Avi OrrUrtreger, Nir Giladi, Susan Bressman, Karen Marder 2O14 Scientific Abstract Listing and Annual Meeting Information Prognostic Value of CT Angiography in the Hyperacute Phase of Middle Cerebral Artery Stroke. Pigreti Santiago, Maria Zurru, Ariel Luzzi, Laura Brescacin, Claudia Alonzo, Luis Camera, Gabriel Waisman, Edgardo Cristiano P2.020WITHDRAWN Cognitive Signatures of Parkinson’s Disease and Glucocerebrosidase (GBA) Mutation Masud Husain, Nahid Zokaei, Alisdair McNeil, Christos Proukakis, Michelle Beavan, Paul Jarman, Prasad Korlipara, Derralyn Hughes, Atul Mehta, Michele Hu, Anthony Schapira P2.027 Non-motor Symptoms in Genetic Forms of Parkinson Disease EvaJuliane Vollstedt, Christine Klein, Meike Kasten Poster Session II Marrying Direct to Consumer Genetic Data with Remote Phenotypic Assessments in Parkinson Disease E. Ray Dorsey, Kristin Darwin, Samara Mohammed, Sean Donohue, Alyssa Tethal, Meredith Achey, Susan Ward, Elaine Caughey, Nicholas Eriksson, Emily Conley, Bernard Ravina P2.029 Exploring Genetic Influences on Variation in the Phenotypic Expression of Parkinson’s Disease. Naveed Malek, Sarah Marrinan, Nin Bajaj, Roger Barker, Yoav Ben-Shlomo, Catherine Bresner, David Burn, Thomas Foltynie, Huw Morris, Nigel Williams, Nicholas, W Wood, Donald Grosset Movement Disorders: Friedreich’s and Other Inherited Ataxias P2.030 Predictive Equations to Muscle Mass Volume in Patients with Spinocerebellar Ataxia Christiane Leite, Darla Macedo, Maria Schieferdecker, Regina Vilela, Helio Teive, Adriana Moro P2.031 Clinical and Genetic Profile of Brazilian Patients with Late-Onset Friedreich’s Ataxia Alberto Martinez, Conrado Borges, Cynthia Bonilha Da Silva, Adriana Moro, Thiago Rezende, Mariana Moscovich, Renato Munhoz, Walter Arruda, Simone Karuta, Anelyssa D’Abreu, Iscia Lopes-Cendes, Marcondes Franca, Jr., Helio Teive P2.032 Disruption of Binaural Hearing in Spinocerebellar Ataxia Type 13 Michael Waters, Harry Nick, S Subramony, Joel Advincula, Raymond Rosales, Lillian Lee, Tetsuo Ashizawa, Middlebrooks John P2.033 ‘Pseudo-dominant’ Inheritance in Friedreich’s Ataxia: Clinical and Genetic Study of a Brazilian Family Adriana Moro, Alberto Martinez, Mariana Moscovich, Simone Karuta, Renato Munhoz, Walter Arruda, Salmo Raskin, Francisco Germiniani, Helio Teive P2.034 Neurodevelopmental Defects in Spinocerebellar Ataxia Type 13 Linked to the EGF-R Signaling Pathway Swati Khare, Donya Salmasinia, Daniela Arbelaez, Jerelyn Nick, Diego Rincon-Limas, Harry Nick, Pedro Fernandez-Funez, Michael Waters P2.035 When Should We Test Patients with Familial Ataxias for SCA31? Agessandro Abrahao Junior, Jose Pedroso, Kinya Ishikawa, Salmo Raskin, Paulo Sgobbi de Souza, Hidehiro Mizusawa, Orlando Barsottini P2.036 Substantia Nigra Echogenicity Is Correlated with Nigrostriatal Impairment in Machado-Joseph Disease José Luiz Pedroso, Orlando Barsottini P2.037 Children with Friedreich Ataxia Undergoing Spinal Fusion Are at Risk for Arrhythmias Kimberly Lin, David Lynch, John Flynn, Joseph Rossano P2.038 Assessing the Feasibility of Quantitative Gait Analysis as an Outcome Measure for Clinical Trials in Spinocerebellar Ataxias Hokuto Morita, Heather Vincent, Nawaz Hack, Bryan Conrad, Tetsuo Ashizawa, S Subramony, Guangbin Xia Movement Disorders: Dystonia P2.039 The Phenomenology and Natural History of Idiopathic Lower Cranial Dystonia Pichet Termsarasab, Steven Frucht P2.040 Clinical and Genetic Evaluation for DYT1 and DYT6 Genes in Brazilian Patients with Cervical Dystonia Carlos Camargo, Sarah Camargos, Salmo Raskin, Francisco Cardoso, Helio Teive P2.041 Familial and Sporadic Cases of Cervical Dystonia in 88 Patients Carlos Camargo, Sarah Camargos, Nilson Becker, Renato Munhoz, Salmo Raskin, Francisco Cardoso, Helio Teive P2.042 Tricks to Treatments: Sensory Tricks in Dystonia Vesper Ramos, Barbara Karp, Mark Hallett P2.043 The Evaluation of Environmental Factors in the Disease Penetrance of Cervical Dystonia Anna Molloy, Okka Kimmich, Laura Williams, Fiona Molloy, Helena Moore, Daniel Healy, Timothy Lynch, Cathal Walsh, Richard Reilly, Sean O’Riordan, Michael Hutchinson P2.044 Is Geste Antagoniste a Predictive Factor of Effectiveness of Botulinum Toxin A Treatment? Martin Bares, Rastislav Sumec, Pavel Filip P2.045 Brain Structural Changes in Primary Focal Dystonia Lidia Sarro, Francesca Caso, Federica Agosta, Sebastiano Galantucci, Aleksandra Tomic, Marina Svetel, Nikola Kresojevic, Giancarlo Comi, Vladimir Kostic, Massimo Filippi P2.046 Alleviating Maneuvers (Sensory Tricks) in Cervical Dystonia Neepa Patel, John Hanfelt, Laura Marsh, Joseph Jankovic P2.047 Sensory Tricks Reverse Intracortical Facilitation Changes in Cervical Dystonia. A Transcranial Magnetic Stimulation Study Stefano Amadio, Elise Houdayer, Francesca Bianchi, Habtom Tesfaghebriel Tekle, Ivan Urban, Calogera Butera, Roberta Guerriero, Marco Cursi, Letizia Leocani, Giancarlo Comi, Ubaldo Del Carro Movement Disorders: Co-morbidities and Novel Care Models P2.048 Telehealth in the Parkinson’s Disease Subspecialty Clinic: The Key to the Patient-Centered Medical Home Meredith Spindler, Eileen Hummel, Stephanie Pawlowski, Daniel Weintraub, Steven Marcus, Margaret Stineman, James Morley, John Duda, Jayne Wilkinson P2.049 Proof of Concept for Operation House Call for Underserved Parkinson’s Disease Patients Nawaz Hack, Umer Akbar, Amanda Eilers, Valerie RundleGonzalez, Daniel Martinez-Ramirez, Hokuto Morita, Irene Malaty, Michael Okun P2.050 Caregiver Tele-support Group for Parkinson’s Disease: A Pilot Study Shital Shah, Gretchen Glenn, Eileen Hummel, Jane Hamilton, Rebecca Martine, Jayne Wilkinson P2.051 Zung Self Rating Depression Scale in Parkinson’s Disease: A Validity Study in Veterans Aliya Sarwar, Max Hirshkowitz P2.052 MDS-Sponsored Scale Translation Program: Process, Format, and Clinimetric Testing Plan for the MDSUPDRS and UDysRS Christopher Goetz, Glenn Stebbins, Lu Wang, Nancy LaPelle, Sheng Luo, Barbara Tilley P2.053 Prevalence of Non-motor Symptoms in Parkinson’s Disease: A Systematic Review with MetaAnalysis Michele Tagliati, Kallol Chaudhuri, Gennaro Pagano P2.054 The Relationship Between Vitamin D Concentrations and Leg Strength in Persons with Parkinson’s Amie Peterson, Brenna Lobb, Charles Murchison, Joseph Quinn P2.055 Statin Use, Apolipoprotein A1, and Parkinson’s Disease Yosef Berlyand, Roy Alcalay, Christine Swanson, Stanley Fahn, Cheryl Waters, Oren Levy, Stephen Schwartz, Alice Chen-Plotkin P2.056 Obesity Associates with Impaired Quality of Life in Parkinson Disease Vikas Kotagal, Martijn Muller, Nicolaas Bohnen P2.057 Comorbidities and Causes of Death in a Cohort Of 205 Patients with Parkinsonism Mariana Moscovich, Gabriela Boschetti, Adriana Moro, Helio Teive, Renato Munhoz Neuropathy: Genetics and Outcomes P2.058 The Allelic Spectrum of Charcot-Marie-Tooth Disease in Over 17,000 Individuals with Neuropathy Joseph Higgins P2.059 Can Glucose Disorders Affect the Severity of CMT1A Neuropathy? Juliana Algemiro, Rita De Cassia Leal, Charles Lourenco, Waldemar Algemiro, Vanessa Marques, Wilson Marques P2.060 Whole Exome Sequencing Identified a Novel Mutation in PMCA4 Gene for Autosomal Dominant Familial Spastic Paraplegia (ADFSP) in a Chinese Family Wing Lok Ho, Shirley Pang, Miaoxin Li, Michelle Kung, Pak-Chung Sham, Shu Leong Ho P2.061 Early- Versus Late-onset Phenotypes of Transthyretin Val30Met Familial Amyloid Polyneuropathy Valeria Salutto, Valeria Alvarez, Diego Beratti, Fabio Barroso, Claudio Mazia P2.062 Wide Spectrum of Neuropathy in Homozygous and Heterozygous Novel Frameshift MPZ Mutation in a Tunisian Family Youssef Sidhom, Imen Kacem, Yousser Hizem, Mouna Ben Djebara, Amina Gargouri, Eric Leguern, Riadh Gouider P2.063 T118M PMP22 as a Modifier for Hereditary Neuropathy with Liability to Pressure Palsy (HNPP) Nivedita Jerath, Tiffany Grider, Andrea Swenson, Michael Shy P2.064Adrenomyeloneuropathy Diagnosed in a Young Female with Spastic Paraparesis after Full Exome Sequencing Tania Garcia, A Ordoñez Ugalde, Beatriz Quintans, Maria Jesus Sobrido, M. C. Amigo, Eva Costa Arpin, Julio Pardo-Fernandez P2.065 Detection of Copy Number Variation (CNV) in Patients with CMT1A by SNP-Allelotyping Brett Parker, Ryan Alexander, Nathalie Schnetz-Boutaud, Xingyao Wu, Michael Shy, Jun Li P2.066 CMT2A2 Associated with Novel MFN2 Gene Double Missense Mutations in CIS Haatem Reda, Gyorgy Abel, Jayashri Srinivasan P2.067 Health-related Quality of Life by SF-36 in Patients with HNPP compared to Those with CMT1A Tiffany Grider, David Cuthbertson, Shawna Feely, Michael Shy ALS: Genetics and Outcomes P2.068 Madras Pattern Motor Neuron Disease Caused by a Novel Mutation in the UBQLN2 Gene Hacer Durmus, Aslihan Ozoguz, Ozgun Uyan, Feza Deymeer, Piraye Serdaroglu, Nazli Basak, Yesim Parman P2.069 Regional Variation of Causative ALS Genes Summer Gibson, Karla Figueroa, Linh Huynh, Mark Bromberg, Stefan Pulst P2.070 Meta-Analysis of ALS Risk for Ataxin-2 (SCA2) CAG Repeat Alleles Annalese Neuenschwander, Khanh Thai, Karla Figueroa, Stefan Pulst P2.071 Use of Veterans Specific Activity Questionnaire (VSAQ) to Estimate Exercise Tolerance in Ambulatory Amyotrophic Lateral Sclerosis (ambALS) Patients Mohammed Sanjak, Jasmin Headen, Kendall Barrett, Scott Holsten, Velma Langford, Elena Bravver, William Bockenek, Urvi Desai, J Scott Story, Scott C Lindblom, Thomas Paccico, Benjamin Brooks P2.072 Amyotrophic Lateral Sclerosis (ALS) Estimates from National Databases in the United States—2001-2010 Marchelle Sanchez, Paul Mehta, Wendy Kaye, Vinicius Antao, D. Kevin Horton P2.073 Using Mortality Data as a Component of Amyotrophic Lateral Sclerosis (ALS) Surveillance in New Jersey (NJ) Heather Jordan, Jerald Fagliano, Daniel Lefkowitz, Lindsay Rechtman, Wendy Kaye P2.074 Mortality and Cause of Death Among Confirmed ALS Cases, Los Angeles and San Francisco Bay Area Metropolitan ALS Surveillance Project 2009-2011 Susan Paulukonis, Jhaqueline Valle, Natalie Collins, Eric Roberts, Paul English, Wendy Kaye P2.075 Predictors of Early Mortality in Patients with Amyotrophic Lateral Sclerosis Undergoing Elective Percutaneous Endoscopic Gastrostomy or Jejunostomy Placement: The Mayo Clinic Experience Sherri Braksick, Lyell Jones, Jayawant Mandrekar, Sara Hocker Fast, Easy Registration Online · AAN.com/view/AM14 57 Tuesday April 29 P2.028 Tuesday, April 29 P2.076 Predictors of Outcome in Amyotrophic Lateral Sclerosis Elena Ratti, James Berry, Nazem Atassi, Amy Shui, Douglas Hayden, David Schoenfeld, Hong Yu, Robin Conwit, Jeremy Shefner, Merit Cudkowicz P2.077 Investigating the Relationship Between Length of Stay in Hospice Care and Rates of Change on ALS Functional Rating Scale-Revised and FVC in Patients with Amyotrophic Lateral Sclerosis Grace Shen, Lauren Elman, Nabila Dahodwala, Kelly Almasy, Mary Kelley, Leo McCluskey Neuromuscular Junction P2.078 Incidence, Risk Factors and Clinical Features of Myasthenic Crises Chi Yan Lee P2.079 Genetic Predisposition to MuSK -Positive Myasthenia Gravis in Patients from Argentina Claudio Mazia, Marcelo Francisco Rugiero, Valeria Salutto, Pablo Galarza, Flavia Canitano, Adrian Perusco P2.080 Is the Decremental Pattern in Lambert-Eaton Myasthenic Syndrome Different from That in Myasthenia Gravis? Donald Sanders, Lucy Cao, Janice Massey, Vern Juel, Lisa Hobson-Webb, Jeff Guptill P2.081 Incidence of Myasthenia Gravis in an HMO of Buenos Aires, Argentina Marcelo Rugiero, Mariela Bettini, Marcelo Chaves, Diego Giunta, Jimena Vicens, Edgardo Cristiano P2.082 A Role for BAFF Receptor (BAFF-R; Cd268) and its Ligand Variant(S) in Early-onset Myasthenia Gravis Thymus Michael Pütz, Hendrik Döbold, Patrick Stelmach, Kerstin Schlegel, Michael Happel, Wolfgang Oertel, Maria Seipelt, Christian Eienbröker, Bjorn Tackenberg P2.083 Demographics of Ocular Myasthenia Gravis Beau Bruce, Elena Bitrian, Mark Kupersmith, Fritz Zimprich, Jason Peragallo, Thomas Whittaker, Michael Lee P2.084 Prognostic Factors and P2.088 Increased Number of Hassall’s Corpuscles in Myasthenia Gravis Patients with Thymic Hyperplasia Naoko Matsui, Ryuji Kaji P2.089 A Biosensor Assay for the Detection of Muscle Specific Tyrosine Kinase (MuSK) Antibodies in Myasthenia Gravis Patients Zahra Pakzad, Ebrima Gibbs, Tariq Aziz, Joel Oger P2.090 Video-assisted Thoracoscopic Surgery for Myasthenia Gravis Associated with Thymoma: A 13-year Experience Minas Tzagournissakis, Konstantinos Lasithiotakis, Alexandros Andreou, Michalis Mavridis, Vasileios Mastorodemos, Georgios Amoiridis, Andreas Plaitakis, Georgios Chalkiadakis P2.091 Association of Neuromyelitis Optica Following Thymectomy in Myasthenia Gravis: Case Report and Retrospective Literature Review of 16 Patients Sajjad Nasir, V Vedanarayanan, Robert Herndon P2.092 De Novo Mutation in Sodium Channel Gene SCNBA Causes Neuromuscular Junction Disorder in Early Onset Epileptic Encephalopathy Nina Barisic, Sarah Weckhuysen, Peter De Jonghe, Ingo Helbig, Arvid Suls, Vanja Ivanovic, Ivan Lehman, Branka Bunoza, Petra Grdan Predictive Value of Electrophysiology for Detecting Thymic Pathology in Patients with Myasthenia Gravis Tushar Gosavi, G Huang, Stephanie Fook-Chong, Yew Long Lo 58 Succesful Treatment of Carotid-Cavernous Fistula Through a Percutaneous Orbital Approach Ricardo Rangel Guerra Cerebrovascular Disease and Interventional Neurology: Behavioral, Cognitive, and Miscellaneous P2.101 P2.115 Postoperative Seizure Outcomes in Patients with Intracerebral Cavernous Malformations Neha Morparia, Cheolsu Shin, Robert Brown, Teresa Christianson, Kelly Flemming P2.102 Risk of Bleeding from Antithrombotic Agents (AT) in Patients with Cerebral Cavernous Malformations (CCMs). Robert Wityk P2.103 Rare Presentation of Churg-Strauss Syndrome: Intracerebral Hemorrhage, Subdural Hemorrhage and an Intracranial Aneurysm Mandeep Chahil, Justin Morgan, Nicole Gonzales, Tzu-Ching Wu P2.104 Inflammatory Cerebral Amyloid Angiopathy Mimicking an Aggressive Glioma Adam Reynolds, Erica Byrd, Arielle Davis, Mahmud Mossa-Basha, Sandeep Khot P2.105 Cerebrovascular Disease and Interventional Neurology: Childhood and Young Adult A Case of Lambert-Eaton Myasthenic Syndrome Presenting with Severe Autonomic Failure Ugonma Chukwueke, Digvijaya Navalkele, Marisara Dieppa, Jaya Trivedi, Jeffrey Elliott, Steven Vernino P2.095 Influence of Immunosuppressive Medication on TCR Vβ Usage and Thymocyte Maturation Stages in Patients with Early-onset Myasthenia Gravis Christian Eienbröker, Michael Pütz, Kerstin Schlegel, Klaus Gellert, Norbert Sommer, Florian Seitz, Wolfgang Oertel, Bjorn Tackenberg P2.096 P2.087 P2.100 P2.094 Paraneoplastic Myasthenia Gravis associated with Appendiceal Mucinous Neoplasm Nicholas Lanciano, Victoria Lawson, William Arnold P2.085 Low Dose Medication Myasthenia Gravis in the Elderly: Clinical Characteristics, Treatment Considerations, Complications and Prognosis. Marcelo Rugiero, Mariela Bettini, Marcelo Chaves, Hernan Gonorazky, Vanesa Pytel, Edgardo Cristiano P2.114 Predictors of Hemorrhagic Complications from Endovascular Treatment of Cerebral Arteriovenous Malformations Juan Carlos Llibre, Jose Jordan P2.093 Cerebrovascular Disease and Interventional Neurology: Acquired and Congenital Vascular Malformations P2.086 P2.099 Cerebral Amyloid Angiopathy Related Inflammation: Case Reports and Imaging Pitfalls Mark Mcallister, Melissa Armstrong Health-related Quality of Life (HRQol ) in Ocular Myasthenia Gravis (OMG) Giuliana Galassi, Alessandra Ariatti, Marina Stefani, Pietro Miceli, Manuela Tondelli, Francesca Benuzzi, Paolo Nichelli and Long-term Outcome in Myasthenia Gravis Salomi Salins, Barbara Teter, Katelyn Kavak, Nicholas Silvestri, Gil Wolfe 7:30 a.m.–11:00 a.m. Pial Arteriovenous Fistula and Capillary Malformation-Arterial Venous Malformation (CM-AVM) Associated with RASA1 Mutation: 2 Illustrative Cases Deepak Gulati, Sunil Manjila, Nicholas Bambakidis, Asim Shahid P2.097 Intracranial Dural Arteriovenous Fistula Presenting with Recurrent Transient Fluent Aphasia Bardia Nourbakhsh, Julio Rojas -Martinez, Chirantan Banerjee, Roberta Novakovic, Worthy Warnack P2.098 Cerebral Venous Congestion Caused By Cervical Arteriovenous Fistula: A Rare Delayed Complication Following Heart Transplantation Hlynur Georgsson, Annapoorna Bhat, Machteld Hillen P2.106 Etiology and the Cost of Pediatric Stroke William Hamilton, Haijuan Huang, Eric Seiber, Warren Lo P2.107 Intra-arterial Treatment in a Child with Embolic Stroke due to Atrial Myxoma Ido Van Der Wyngaard, Marieke Wermer, Marianne van Walderveen, Geert Lycklama a Nijeholt Hypertensive Disorders in Pregnancy and Future Risk of Stroke: A Systematic Review Aravind Ganesh, Neha Sarna, Rahul Mehta, Eric Smith Undiagnosed Cognitive Impairment Among Patients Referred for Carotid Doppler Evaluation Is Associated with Increased Non-adherence with Medical Treatment of Vascular Risk Factors Angelia Kirkpatrick, Leslie Guthery, Calin Prodan P2.116 Neuro-QOL for Assessment of Cognitive Impairment After Stroke: Comparison with Modified Rankin Scale Rajbeer Sangha, Carlos Corado, Deborah Bergman, Andrew Naidech, David Cella, Richard Bernstein, Yvonne Curran, Shyam Prabhakaran P2.117 The Role of DiffusionPerfusion Mismatch in the Cognitive Changes of Acute Stroke Patients Amanda Ramadan, Melissa Motta, Rebecca Gottesman, Argye Hillis, Richard Leigh P2.118 The Feeling that ‘I Can Say it in My Head’ Predicts Word-byWord Success in Subsequent Aphasia Treatment. William Hayward, Kelli Sullivan, Sarah Snider, Elizabeth Lacey, Rhonda Friedman, Peter Turkeltaub P2.119 An Unusual Cause of Altered Mental Status: Recurrent Cerebral Air Embolism from Atrial-Esophageal Fistula Iftekhar Ahmed, Trenton Myers, James Kim P2.120 Stroke Mortality and its Predictors in Nigeria: Results of a HospitalBased Study Kolawole Wahab, Emmanuel Sanya, Babatunde Ademiluyi, Bello Abiodun, Wemimo Alaofin P2.121 Heart Rate Variability and Vibration Perception Threshold in Healthy Young Adults with Parental History of Type 2 Diabetes Rajesh Goit Measurement of Hemispheric Volume to Detect and Quantify Early Ischemic Changes in Patients with Ischemic Stroke Asif Khan, Mushtaq Qureshi, Bernard Galea, Malik Adil, Muhammad Suri, Adnan Qureshi P2.109 P2.122 P2.108 Stroke in a Young Patient: A Sentinel Presentation of Neurosyphilis and HIV Elizabeth Flaherty, Shawna Cutting P2.110 Cardiovascular Risk Factors in Young Adults with Stroke from the AISYF Study Julieta Mazziotti, Ricardo Reisin P2.111 Left Ventricular Hypertrophy as a predictor of White Matter Hyperintensities in Young Stroke Patients Luciana Catanese, Ashkan Shoamanesh, Helena Lau, Jose Romero, Viken Babikian, Carlos Kase, Aleksandra Pikula P2.112 Ethnic Differences in Ischemic Stroke Subtypes: The Stroke Prevention in Young Adults Study Megh Trivedi, John Cole P2.113 Pregnancy Associated Cerebral Ischemia in Women with Sickle Cell Disease Taqi Zafar, Malik Adil, Muhammad Suri, Adnan Qureshi 2O14 Scientific Abstract Listing and Annual Meeting Information Safety and Tolerability of Gabapentin for Headache After Aneurysmal Subarachnoid Hemorrhage Laxmi Dhakal, Michael Mayes, Alexa Richie, William Freeman P2.123 Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopthy (CADASIL) in Argentina Maximiliano Hawkes, Miguel Wilken, Veronica Bruno, Virginia Pujol Lereis, Guillermo Povedano, Maria Saccoliti, Ana Lia Taratuto, Sebastian Ameriso P2.124 Episodic Aphasia After Subdural Hemorrhage Due to Cortical Spreading Depression: A Case Report Jillianne Grayson, Nirav Shah, Shnehal Patel, Alejandro Forteza Poster Session II Cerebrovascular Disease and Interventional Neurology: Evaluation, Cost, and Quality P2.137 Stroke Patients and Diagnostic Testing—the Weekend Waiting Game! Sally Mathias, Jessica Lee Sex Disparities in Access to Stand Alone Primary Stroke Centers: Can Telemedicine Mitigate This Effect? Catherine Wolff, Amelia Boehme, Tzu-Ching Wu, Michael Mullen, Charles Branas, James Grotta, Sean Savitz, Brendan Carr P2.126 P2.138 P2.125 Which Diagnostic Tests for Stroke Are the Most Costly and May Not be Necessary? Seemant Chaturvedi, Kumar Rajamani, Pratik Bhattacharya P2.127 Implementing a Checklist into Cerebrovascular Service Discharges: A Resident-Driven Quality Improvement Project Kate Daniello, Melissa Rayhill, Ania Busza, Judith Clark, James Otis P2.128 Transient Ischemic Attack: Symptom Patterns and Imaging Associations Elissaios Karageorgiou, David Anderson P2.129 Stroke Patient Length of Stay Benchmarking and Analysis Elizabeth Diebolt, Shannon Sims, James Conners, Vivien Lee P2.130 Comparability of Charges and Payments for Hospitalized Stroke Sebina Bulic, May Kim, Shuhan He, Suzie Kazaryan, Steven Cen, Shannon He, William Mack, Nerses Sanossian Medicare Coverage Increases Odds of In-hospital Mortality But Lack of Insurance Increases Odds of Poor Functional Outcome by Modified Rankin Score (mRS) Adam Friedant, Dominique Monlezun, Jr, Prerana Baranwal, Melisa Valmoria, Amir Shaban, Alexander George, Ramy El Khoury, Sheryl Martin-Schild P2.139 Medicare and VA Patients Have More Inpatient Complications and Less Neuroimaging than Uninsured Patients Prerana Baranwal, Dominique Monlezun, Jr, Mathew Ryan, Denise Pineda, Amir Shaban, Alexander George, Ramy El Khoury, Sheryl Martin-Schild P2.140 Uninsured Patients May Lack Diagnoses for Chronic Diseases That Are Known Stroke Risk Predictors Prerana Baranwal, Dominique Monlezun, Jr, Joel Lanceta, Amir Shaban, Alexander George, Sheryl Martin-Schild, Ramy El Khoury P2.148 Age-specific Incidence Rate for Dementia and Alzheimer’s Disease in NIA-LOAD/NCRAD and EFIGA Families Badri Vardarajan, Kelley Faber, Thomas Bird, David Bennett, Roger Rosenberg, Bradley Boeve, Neill GraffRadford, Alison Goate, Martin Farlow, Robert Sweet, Rafeal Lantigua, Martin Medrano, Ruth Ottman, Daniel Schaid, Tatiana Foroud, Richard Mayeux P2.149 Distinct Genetic Variants in Alzheimer’s Disease and Type 2 Diabetes Sun Ju Chung, Seong Yoon Kim, Juyeon Kim, Mi-Jung Kim, Young Jin Kim, Jae-Hong Lee P2.150 TMEM106B Is a Genetic Modifier of Frontotemporal Lobar Degeneration with C9orf72 Hexanucleotide Repeat Expansions Alice Chen-Plotkin, Michael Gallagher, Eunran Suh, Murray Grossman, Lauren Elman, Leo McCluskey, John Trojanowski, Virginia Lee, Vivianna Van Deerlin P2.151 HDLS Family Case Showing X-Linked Recessive Heredity Hisatomo Kowa, Takeshi Uenaka, Takehiro Ueda, Takashi Matsukawa, Shoji Tsuji, Fumio Kanda, Tatsushi Toda P2.158 Functional Neuroimaging of Sensory Conversion Disorder: The Role of Ancillary Activation Matthew Burke, Omar Ghaffar, W Staines, Jonathan Downar, Anthony Feinstein P2.159 Impaired Processing of Positive and Negative Facial Expressions in Right Hemisphere Stroke Donna Tippett, Cameron Davis, Yessina Gomez, Lydia Trupe, Argye Hillis P2.160 Models for PTSD Subtypes Classification According to Anxiety and Depressive Dominant Symptomatology Chen Ryder, Gal RichterLevin, Radi Shahien P2.161 Longitudinal Volume Loss in Neuroanatomical Regions of Emotion Versus Cognition Peter Pressman, Yuliana Noniyeva, Nicholas Bott, Shubir Dutt, Bruce Miller, Virginia Sturm, Joel Kramer P2.162 Asymmetry of Perceived Emotional Expression in Facial Chimeras Jerry Wei, Steven Sparr Aging, Dementia, and Cognitive and Behavioral Neurology: General Cognition P2.141 P2.152 Show or No-show—That Is the Question: Lack of Outpatient Follow-up a After Acute Stroke. Gauhar Chaudhary, Jessica Lee Adherence with Post-stroke Follow-up Clinic Visits and Factors Influencing Compliance in a Large Urban Hospital. Mohammad El-Ghanem, Peter Jin, Vineet Punia, Wenzhuan He, Machteld Hillen P2.132 P2.142 Aging, Dementia, and Cognitive and Behavioral Neurology: Emotion Primary CNS Lymphoma Versus Intravascular Lymphoma: Differences in Cognitive Presentation Mariel Deutsch, Mario Mendez P2.153 P2.165 P2.131 Use of a Patient Navigation System to Increase Attendance at Stroke Follow-up Appointments Christina Sarris, Aaron Hajart, Ennis Duffis P2.133 Gender Differences in Primary Stroke Center Evaluation and Utilization of rt-PA Michael Mullen, Karen Albright, Amelia Boehme, Scott Kasner, Michael Kallan, Charles Branas, Brendan Carr Risk Factors More Associated with Ischemic Rather Than Hemorrhagic Stroke in Black Africans: Implications for Epidemiologic Transition Mayowa Owolabi, Atinuke Agunloye P2.143 Poor Outcome Among Women Following Intracerebral Hemorrhage Preet Varade, Seemant Chaturvedi, Pratik Bhattacharya Cerebrovascular Disease and Interventional Neurology: Disparity Aging, Dementia, and Cognitive and Behavioral Neurology: Genetics P2.134 P2.144 Are Hispanic Subarachnoid Hemorrhage Patients in Border States Treated Differently Than Those Admitted in Non-Border States? Ameer Hassan, Taqi Zafar, Malik Adil, Muhammad Umair, Ahmed Malik, Wondwossen Tekle, Olive Sanchez, Adnan Qureshi P2.135 Disparities in Access to Primary Stroke Centers: Geography, Not Gender, Race, or Ethnicity Michael Mullen, Ariel Bowman, Douglas Wiebe, Catherine Wolff, Karen Albright, Jason Roy, Laura Balcer, Charles Branas, Brendan Carr P2.136 Are There Disparities in Thrombolytic Treatment and Mortality in Acute Ischemic Stroke in the Hispanic Population Living in Border States Versus Non-Border States? Ameer Hassan, Malik Adil, Taqi Zafar, Muhammad Umair, Wondwossen Tekle, Olive Sanchez, Adnan Qureshi Sanger Sequencing Exons of BDNF Gene Derived from a Latino Sample Sara Dawit, Jazmin Acosta, Mia Champion, Stefanie Velgos, Gabriel Shaibi, Lawrence Mandarino, Nicole Cevette, Richard Caselli, Yonas Geda P2.145 Lack of AGG Interruptions in FMR1 Is Associated with Cognitive Impairment Deborah Hall, Victor Kaytser, Raj Shah, David Bennett, Elizabeth BerryKravis P2.146 Genome-wide Gene-based Analysis of Exome Array Data for Rare Variants in Alzheimer’s Disease Sun Ju Chung, Seong Yoon Kim, Juyeon Kim, MiJung Kim, Young Jin Kim, Jae-Hong Lee P2.147 Expression QTL Studies in LOAD and PSP Brains by Next-generation RNA Sequencing Nilufer Taner, Chen Wang, Minerva Carrasquillo, Mariet Allen, Curtis Younkin, Daniel Serie, Vernon Pankratz, Thuy Nguyen, Li Ma, Kimberly Malphrus, Sarah Lincoln, Ronald Petersen, Neill Graff-Radford, Steven Younkin, Dennis Dickson, Yan Asmann Altered CpG Methylation of APP, MAPT and GSK3B in Sporadic Alzheimer’s Disease Atsushi Iwata, Hiroyuki Hatsuta, Shigeo Murayama, Shoji Tsuji Influence of the Tau Haplotype on Progression and Treatment Response of Neuropsychiatric Symptoms in People with Alzheimer’s Disease Clive Ballard, Anne Corbett, Byron Creese P2.154 Visual Hypoemotionality (Secondary Visual Derealization) in a Patient with a Right Posterior Temporoparietal Lesion David Perez, Sashank Prasad, Diler Acar, Mary-Ellen Meadows, Alexandra Golby, Barbara Dworetzky P2.155 Major Depression as Initial Manifestation of Limbic Lewy Body Dementia a Clinico-pathological Report Bernard Michel, Henri Becker, Jean-Francois Pelissier, Bradley Boeve, Nathalie Sambuchi, Annie Bartolin, Catherine Gallant, Jean-Claude Saint Jean, Hui-Mei Chen, Charles Rouyer, Jean Michel Azorin, Ronald Petersen P2.156 Evaluation of Emotional Blunting in Behavioral Variant Frontotemporal Dementia Compared to Alzheimer’s Disease Aditi Joshi, Joseph Barsuglia, Michelle Mather, Elvira Jimenez, Jill Shapira, Mario Mendez P2.157 Autistic Symptoms in a Geriatric Population with Mild Cognitive Impairment and Early Dementia Danielle Crawford, Erin Abner, Paul Glaser, Gregory Jicha Tuesday April 29 First Authors stand by Posters from 7:30 a.m.–9:00 a.m. P2.163 Diffuse Lewy Body Disease and Associated Balint’s Syndrome: A Case Series Ramsey Falconer, Sean Rogers, Fahd Amjad, Benjamin Osborne P2.164 Using Eye-Movement Trackings to Investigate Mechanisms of Word-object Associations in Primary Progressive Aphasia Mustafa Seckin, Joel Voss, M. Mesulam, Emily Rogalski, Robert Hurley P2.166 Nonverbal Oral Apraxia in Primary Progressive Aphasia and Apraxia of Speech Hugo Botha, Joseph Duffy, Edythe Strand, Jennifer Whitwell, Keith Josephs P2.167 Routine Cognitive Screening in a General Neurology Clinic: Impact on Physician Behavior Michael Rosenbloom, Terry Barclay, Maria Pyle, Amanda Cagan, Ann Hanson, Leah Hanson P2.168 Impaired Grammar in the Speech of Amyotrophic Lateral Sclerosis Collin York, Lauren Elman, Leo McCluskey, Sharon Ash, Murray Grossman P2.169 Unawareness of Partners’ Abilities in Aged Subjects Vahid Behravan, Paul Eslinger, A. Barrett P2.170 Neurobehavioral Disorders in Parkinsonian Patients Without Dopamine Deficits (SWEDD) Amin Demerdash, Kenneth Heilman, Joanna Myers, Chase Mitchell, David Standaert, Frank Skidmore P2.171 A Japanese Family with Idiopathic Basal Ganglia Calcification with Novel SLC20A2 Mutation Presenting with Late-onset Hallucination and Delusion Kensaku Kasuga, Takuya Konno, Masatoyo Nishizawa, Takeshi Ikeuchi Fast, Easy Registration Online · AAN.com/view/AM14 59 Tuesday, April 29 P2.172 Bilingualism Is Associated With Less Severe Cognitive Impairment Claudia Padilla, Elvira Jimenez, Joseph Barsuglia, Aditi Joshi, Edmond Teng, Mario Mendez P2.173 Differential Longitudinal Changes in Cognition Among Amyotrophic Lateral Sclerosis (ALS) Patients Sharon Xie, Katya Rascovsky, Ashley Boller, Xiaoyan Han, Leo McCluskey, Lauren Elman, David Libon, Murray Grossman P2.174 Subjective Cognitive Impairment in a French Sample Bernard Michel, Nathalie Sambuchi, Yonas Geda, Isabelle Muraccioli, Veronique Paban, Elisabeth Jouve, Rolland Sambuc, Hui-Mei Chen, Annie Bartolin, Catherine Gallant, Jean-Claude Saint Jean, Charles Rouyer, Christian Brosset, Jean-Michel Azorin, Beatrice Alescio-Lautier, Ronald Petersen P2.175 Cognitive Decline Is Associated with Progressive Grey Matter Disease in Amyotrophic Lateral Sclerosis (ALS) Christopher Olm, Lauren Elman, Leo McCluskey, Corey McMillan, Murray Grossman P2.176 Neurological Examination Findings in Autistic Adults Bryan Woodruff, Joseph Hentz, Amy Duffy, Elena Pollard, Christopher Smith, Yonas Geda P2.177 Mild Cognitive Impairment: Neuropsychiatric Symptom Prevalence within Cognitive Subtypes and Obesity Ashley Hannah, Andrea Bozoki P2.178 Social and Executive Contributions to Discourse Limitations in Amyotrophic Lateral Sclerosis Anna Menaged, Sharon Ash, Christopher Olm, Corey McMillan, Murray Grossman, Lauren Elman, Leo McCluskey P2.179 Dissociating the Body Schema: Evidence from Two Case Studies Jared Medina, Emily Baumert, Megan Ziegler P2.180 Deficits in Sentence Expression in Amyotrophic Lateral Sclerosis Sharon Ash, Christopher Olm, Corey McMillan, Ashley Boller, David Irwin, Leo McClusky, Lauren Elman, Murray Grossman P2.181 Speaking While Gesturing Adversely Affects Limb Praxis in pAD. A. Barrett, Livingston Dore P2.182 Alabama Brief Cognitive Screener (ABCs): Design and Initial Clinical Experience Marissa Natelson Love, David Geldmacher Epilepsy and Clinical Neurophysiology: Genetics P2.183 CLN6 Mutations Cause Teenage-onset Progressive Myoclonus Epilepsy Danielle Andrade, Tara Paton, Julie Turnbull, Christine Klein, Christian Marshall, Stephen Scherer, Berge Minassian 60 P2.184 Mild Case of UnverrichtLundborg Disease (ULD) Mimicking Juvenile Myoclonic Epilepsy (JME) in Adulthood Eva Andermann, Dina Amrom, Mahmoud Heshmati Moghaddam, Frederick Andermann, Tarja Joensuu, Anna-Elina Lehesjoki P2.185 LGI1 Mutation Presenting as Idiopathic Generalized Epilepsy: Importance of Family History for Genetic Testing Dina Amrom, Frederick Andermann, Hans Atli Dahl, Eva Andermann P2.186Lacosamide-responsive Status Epilepticus and Epileptic Spasm in Fumarase Deficiency France Fung, Patricia Musolino, Ronald Thibert P2.187 Aicardi Syndrome: Long-term Evolution Anfal Ali, Nicky Wu, Felippe Borlot, Timo Krings, Danielle Andrade P2.188 Dravet Syndrome: Seizure Control and Gait in Adults with Different SCN1A Mutations Jennifer Rilestone, Fernando Coelho, Berge Minassian, Danielle Andrade P2.189 The Prognosis of Primary Generalized Epilepsy in Patients with Parental Consanguinity: A One-year Retrospective Study Hussam Assiri, Abdulmajeed Bajunaid, Fawzi Babtain, Muthusamy Velmurugan P2.190 First Time Seizure in Adult Female as Presentation of Ornithine Transcarbamoylase Deficiency: A Case Report and Literature Review Michael Pizzi, Suparna Krishnaiengar P2.191 Unusual Presentation of Left Temporal Lobe Epilepsy Due to Large Sphenoidal Encephalocele and Good Epilepsy Surgery Outcome Tiffany Fisher, Sasaki-Adams Deanna, Hae Won Shin P2.192 Next Step for Personalized Medicine in Epilepsy: Pharmacogenomic Testing-based Antiepileptic Drugs in Refractory Epilepsy Andres Cruz, Pedro Bermejo P2.193 A Novel Gene (Myclonin 3) for Classic Juvenile Myoclonic Epilepsy Dongsheng Bai, Marco Medina, Reyna Duron, Julia Bailey, Maria Alonso, Toshimitsu Suzuki, Miyabi Tanaka, Iris Martinez-Juarez, Adriana Ochoa, Aurelio Jara-Prado, Jose Serratosa, Kazuhiro Yamakawa, Antonio Delgado-Escueta MS and CNS Inflammatory Disease: Treatment Safety P2.194 Teriflunomide Treatment Is Not Associated with Increased Risk of Infections: Pooled Data from the Teriflunomide Development Program Barry Singer, Giancarlo Comi, Aaron Miller, Mark Freedman, Myriam Benamor, Philippe Truffinet P2.195 Cardiovascular Effects of Combined Administration of Siponimod and Popranolol—Importance of Sequencing During Coadministration Shibadas Biswal, Florine Polus, Atul Pawar, Uday Kiran Veldandi, Eric Legangneux 7:30 a.m.–11:00 a.m. P2.196 Short-term and Long-term Effects of Fingolimod on the Cardiovascular Autonomic Nervous System Judith Eisele, Jowita Zwierzanska, Manja Reimann, Silke Prieur, Kristin Haink, Thorsten Schultheiss, Tjalf Ziemssen P2.206 A Case of Hemophagocytic P2.197 P2.207 Good Cardiac Safety in Patients with Relapsing Remitting Multiple Sclerosis Upon First Fingolimod Dose Volker Limmroth, Susanne Hoyer, Stephan Schmidt, Michael Lang, Tjalf Ziemssen P2.198 Successful Detection and Management of Immune Thrombocytopenia in AlemtuzumabTreated Patients with Active RelapsingRemitting Multiple Sclerosis Adam Cuker, Roberto Stasi, Jeffrey Palmer, Pedro Oyuela, David Margolin, Ann Bass P2.199 Thyroid Autoimmune Adverse Events in Patients Treated with Alemtuzumab for Relapsing-Remitting Multiple Sclerosis: Four-year Follow-up of the CARE-MS Studies Cary Twyman, Pedro Oyuela, Jeffrey Palmer, David Margolin, Colin Dayan P2.200 Safety Profile of Delayed- Release Dimethyl Fumarate in RelapsingRemitting Multiple Sclerosis (RRMS): Longterm Interim Results From the ENDORSE Extension Study Ted Phillips, Robert Fox, Krzysztof Selmaj, Ray Zhang, Mark Novas, Marianne Sweetser, Vissia Viglietta, Ralf Gold P2.201 Safety of Using Diseasemodifying Therapy Post-alemtuzumab Treatment in Patients with RelapsingRemitting Multiple Sclerosis in the Core and Extension Phases of CAMMS223, CARE-MS I, and CARE-MS II Studies Keith Edwards, Christopher LaGanke, Pedro Oyuela, Jeffrey Palmer, David Margolin P2.202 Baseline Characteristics and Interim Analysis Results of the Fingolimod Cohort in the Worldwide Post-approval Safety Program (PASSAGE) Paul Giacomini, Helmut Butzkueven, Stanley Cohan, Tomas Olsson, Dietrich Rothenbacher, Belinda Weller, Tjalf Ziemssen, Anu Gupta, Malika Cremer, Tricia Blankenbiller, Erika Rochotte, Davorka Tomic, Philipp Von Rosenstiel, Maria Trojano P2.203 Pooled Safety Data from Four Placebo-Controlled Teriflunomide Studies Thomas Leist, Mark Freedman, Myriam Benamor, Philippe Truffinet, Deborah Dukovic, Giancarlo Comi P2.204 Prospective Evaluation of Development of Skin Rashes in MS Patients Treated with Daclizumab High Yield Process Irene Cortese, Kaylan Fenton, Joan Ohayon, Edward Cowen, John DiGiovanna, Bibiana Bielekova P2.205 Safety and Tolerability of Escalating Doses of Laquinimod, an Oral Immunomodulatory Agent in Development for Treatment of Relapsing-Remitting Multiple Sclerosis Hayrettin Tumani, Tjalf Ziemssen, Friedemann Paul, Martin Marziniak, Nils Richter, Christoph Heesen, Maya Marglit, Yulia Sidi, Tali Gorfine, Yossi Gilgun-Sherki 2O14 Scientific Abstract Listing and Annual Meeting Information Lymphohistiocytosis Syndrome in a Patient with Multiple Sclerosis on Fingolimod Therapy. Pedro Abreu, Carla Peixoto, Claúdia Carvalho, Lurdes Santos, António Sarmento, Maria José Sá A Comparison of the Safety/ Tolerability and Pharmacodynamics of Acthar Gel and Methylprednisolone with Regimens Utilized for the Treatment of MS Exacerbations Stacie Bell, Jennifer Vincent, Vakessa Hammock, Karen Welch, Julia Chung, Mary Nyberg, Patrice Becker, David Young P2.208 Efficacy and Safety of Fingolimod in Hispanic Patients: Pooled Data from Three Phase 3 Clinical Trials Angel Chinea, Regina Alvarenga, Davorka Tomic, Allitia DiBernardo, Xiangyi Meng, Kathleen Hawker P2.209 Alemtuzumab Has Similar Efficacy and Safety in Active RelapsingRemitting Multiple Sclerosis (RRMS) Patients Who Were Treatment-Naive or Who Relapsed on Prior Therapy David Margolin, Bernd Kieseier, Jeffrey Palmer, Tjalf Ziemssen P2.210 Long-term Safety of Fingolimod: Interim Evaluation of Data from the LONGTERMS Trial Jeffrey Cohen, Philipp Von Rosenstiel, Rebecca Gottschalk, Linda Cappiello, Ying Zhang, Ludwig Kappos P2.211 Delayed Third Degree Atrioventricular Block with Pacemaker Placement in a Multiple Sclerosis Patient on Fingolimod Treatment Johann Sellner, Barbara Holl, Peter Wipfler, Vaclav Chroust, Georg Pilz, Maximilian Winhard, Andrea Harrer, Katrin Oppermann, Eugen Trinka, Jorg Kraus P2.212 No Clinically Significant Effect on Pulmonary Function Observed with Siponimod (BAF312) Alone or in Combination with Propranolol in Healthy Adult Subjects Shibadas Biswal, Florine Polus, Atul Pawar, Uday Kiran Veldandi, Eric Legangneux P2.213 Bullous Drug Eruption with Dimethyl Fumarate Amir Khoiny, Noushin Khoiny P2.214 Early Tolerability of Dimethyl Fumarate for Treatment of Multiple Sclerosis Samuel Cohn, Robert Bermel, Robert Fox, Jeffrey Cohen, Daniel Ontaneda P2.215 Report an Unusual Thrombotic Complication Two Months After Starting Fingolimod Nancy Nealon, Nataliya Ternopolska, Halina White P2.216 Tolerability, Safety and Efficacy of Fingolimod in Clinical Pratice Jean-Claude Ongagna, Carole Berthe, Nicolas Collongues, Fréderic Blanc, Jerome De Seze P2.217 GNbAC1, a Humanized Monoclonal Antibody Against the Multiple Sclerosis Associated Retrovirus Envelope Protein, Is Well Tolerated in Patients with Multiple Sclerosis. Tobias Derfuss, Francois Curtin, Alois Lang, Herve Perron, Ludwig Kappos, Patrice LaLive Poster Session II P2.218 The Autonomic Balance Predicts Cardiac Effects After First Dose of Fingolimod Silvia Rossi, Camilla Rocchi, Valeria Studer, Caterina Motta, Benedetta Lauretti, Giorgio Germani, Giulia Macchiarulo, Gerolama Marfia, Diego Centonze P2.219 Electrocardiogram Monitoring After the First Fingolimod Doses Begoña Palazon, Ester Carreon, Rocio Hernandez Clares, Judith Jimenez, Gema Salgado, Encarnación Andreu, Jose Javier Martín, Jose Meca P2.220 Excessive Blood Pressure Increase during Sustained Handgrip Testing Predicts Bradycardia upon Fingolimod Treatment Max Hilz, Ralf Linker, Tassanai Intravooth, Sebastian Moeller, De-Hyung Lee, Stefan Schwab, Julia Koehn P2.221 Safety and Dosing of Autologous Neural Progenitors Injected Intrathecally in Multiple Sclerosis Patients: Results of a Pilot Study Saud Sadiq, Sydney Chirls, Daniel Koffler, Violaine Harris P2.222 The Use of MRI to Monitor the Safety of Anti-LINGO-1: Findings from Phase I Studies in Healthy Volunteers and Subjects with MS Nancy Richert, Isaac Melamed, Hakop Gevorkyan, Lei Xu, Diego Cadavid P2.223 Long-term Safety of Rituximab and Peripheral B-Cell Depletion in Multiple Sclerosis and Other CNS Autoimmune Disorders Anza Memon, Shitiz Sriwastava, Fen Bao, Evanthia Bernitsas, Adil Javed, Christina Caon, Omar Khan P2.224 Reversible Cerebral Vasoconstriction Syndrome and Fingolimod: Culprit or Innocent Bystander Jason Fleming, Matthew West P2.225 Life Threatening Asthmatic Crisis After 6 Months of Fingolimod Treatment Matteo Caporro, Claudio Gobbi, Chiara Zecca P2.226 Tumefactive Multiple Sclerosis in a Patient on Fingolimod YuanKai Lee, Vijay Sawlani, Gordon Mazibrada P2.227 Gastrointestinal Tolerability of Delayed-Release Dimethyl Fumarate in a Multicenter, Open-Label Study of Patients with Relapsing Forms of Multiple Sclerosis Edward Fox, Alberto Vasquez, William Grainger, Tina Ma, Jie Li, Javier Zambrano P2.228 Transient Neurologic Worsening After Initiation of Dimethyl Fumarate Therapy in Progressive Multiple Sclerosis Patients James Stark, Sydney Chirls, Saud Sadiq P2.229 Absence of a Relevant Effect on Cardiac Repolarization in a QT/QTc (TQT) Study of RPC1063, a Novel, Selective S1P1 Receptor Agonist, in Healthy Adult Volunteers Hartung Jeffrey, Allan Olson, Robert Peach, Marcus Boehm, Boaz Mendzelevski, Heather Smith, Christine Pan, Gregg Timony, Sheila Gujrathi P2.230 Dimethyl Fumarate Tolerability and Treatment Adherence Amongst Patients with Multiple Sclerosis Enrolled in Specialty Pharmacy Services. Stephanie Holliday, Alysha Robinson P2.231 Severe Relapse in a Multiple Sclerosis Patient Associated with Ipilimumab Treatment for Metastatic Melanoma Edward Gettings, Chris Hackett, Thomas Scott P2.232 Effects of Therapeutic and Supratherapeutic Doses of Siponimod (BAF312), a Selective S1P1,5 Receptor Modulator, on Cardiac Repolarization: Results of a Thorough QTc (TQT) Study Kasra Shakeri-Nejad, Louise Mooney, Vassilios Aslanis, Uday Kiran Veldandi, Nicole Pezous, Eric Legangneux P2.233 Teriflunomide: Non-Clinical Evaluation Demonstrates no Effect on Sperm DNA or Male Fertility Lynn Davenport, Andreas Czich, Sandrine Turpault Pediatric MS and Other Demyelinating Diseases P2.234 The Symbol Digit Modalities Test Is an Effective Cognitive Screen in Pediatric Onset Multiple Sclerosis (MS) Lauren Krupp, Leigh Charvet, Rebecca Cleary, Kate Bartolotta, Livana Koznesoff, Rachel Beekman, Anita Belman P2.235 Downward Educational Trajectory Is Seen in Children and Young Adults After Diagnosis of Pediatric MS Stephanie Grover, Austin Sye, Berengere Aubert-Broche, Brenda Banwell, Louis Collins, E. Ann Yeh P2.236 Phenotypic and Functional Analysis of Immune Cell Subsets in Pediatric-onset Multiple Sclerosis (MS): Towards Definition of Earliest Disease Mechanisms Mukanthu Nyirenda, Rui Li, Craig Moore, Ayal Rozenberg, Ayman Rezk, Trina Johnson, Dessa Sadovnick, Douglas Arnold, Ruth-Ann Marrie, Brenda Banwell, Amit Bar-Or P2.237 Results of a Population of YOUTH MS; With More Than Ten Years of Follow Up: Some Entity to Think About. C. Curbelo, Maria Curbelo, A. Martínez, G. Rojas, J. Steinberg, A. Carrá P2.238 Fingolimod in Pediatric MS: Design of a Double-blind Study Versus Interferon β-1a IM Tanuja Chitnis, Brenda Banwell, Jutta Gaertner, Goeril Karlsson, Bingbing Li, Martin Bernhard Merschhemke, Norman Putzki P2.239 Evaluation of Thalamic Fraction in Adults with Pediatric-Onset MS Samira Farough, Antonia Ceccarelli, Svetlana Egorova, Tanuja Chitnis P2.240 Clinical and MRI Phenotype of Children with MOG antibodies Cristina Fernandez Carbonell, David Vargas Lowy, Mussalam Alexander, Brian Healy, Katherine McLaughlin, Kai Wucherpfenning, Tanuja Chitnis P2.241 Myelin Oligodendrocyte Glycoprotein (MOG) Auto-antibodies in Children Predicts a Non-MS Course of Acquired Demyelination Syndrome (ADS). Yael Hacohen, Michael Absoud, Kumaran Deiva, Marc Tardieu, Evangeline Wassmer, Ming Lim, Angela Vincent, Patrick Waters P2.249 P2.242 P2.250 Fingolimod to Treat Severe Rate of Agreement for Manual and Automated Techniques for Determination of New T2 Lesions in Children with Multiple Sclerosis and Acute Demyelination Leonard Verhey, Colm Elliott, Helen Branson, Cristina Philpott, Manohar Shroff, Tal Arbel, Brenda Banwell, Douglas Arnold P2.243 Radiologically Isolated Syndrome in Children: Report of 5 Children with Long-Term Follow-Up Mefkure Eraksoy, Zuhal Yapici, Pinar Tekturk, Murat Kurtuncu, Hifzi Ozcan MS and CNS Inflammatory Disease: Progressive Multifocal Leukoencephalopathy Risk P2.244 Low Body Weight as a Potential Surrogate Risk Factor for Progressive Multifocal Leukoencephalopathy John Foley, Mark Gudesblatt, Myassar Zarif, Ellen Lathi P2.245 Lipid-Specific IgM Bands Contribute to Stratify PML Risk in MS Patients Treated with Natalizumab Luisa Villar, Lucienne Costa-Frossard, Thomas Masterman, Oscar Fernandez, Xavier Montalban, Bonaventura Casanova, Guillermo Izquierdo, Francisco Coret Ferrer, Hayrettin Tumani, Albert Saiz, Rafael Arroyo, Katharina Fink, Laura Leyva, Carmen Espejo, Roberto Alvarez-Lafuente, Javier Olascoaga, Javier Olaskoaga Urtaza, Agustin Oterino, Sara Llufriu Duran, Florian Lauda, Clara De Andres, Juan Antonio Garcia-Merino, Ricardo Fernandez-Bolaños, Lamberto Landete Pascual, Eduardo Aguera Morales, Santiago Diaz Nicolas, Manuel Menendez, Laura Navarro, Domingo Perez, Lluis Ramio, Fernando Sanchez Lopez, Pedro Serrano Castro, Alberto Tuñon, Jose Alvarez-Cermeño P2.246 Transient Punctuate Gadolinium-enhancing Lesions Preceding Natalizumab-associated Progressive Multifocal Leukoencephalopathy (PML) Giovanni Castelnovo, Eric Thouvenot, Dimitri Renard, Guillaume Taieb P2.247 Modeling PML Risk in JCV Sero-Negative Natalizumab-Treated MS Patients Robert Carruthers, Tanuja Chitnis, Brian Healy P2.248 Association Between Infratentorial Onset of Progressive Multifocal Leukoencephalopathy (PML) and Long-Term Exposure to Natalizumab (NAT) Robert Hoepner, Jonas Ahlbrecht, Ruth Schneider, Stefanie Dahlhaus, Ortwin Adams, Andrew Chan, Martin Stangel, Ralf Gold Excellent Outcome in Natalizumab-Associated PML Due to Early Diagnosis and Optimal Treatment Georg Pilz, Andrea Harrer, Peter Wipfler, Katrin Oppermann, Johann Sellner, Shahrzad Afazel, Elisabeth Haschke-Becher, Theo Rispens, Desiree van der Kleij, Eugen Trinka, Jorg Kraus Multiple Sclerosis After Natalizumabassociated Progressive Multifocal Leukoencephalopathy: A Valid Option? Elisabeth Maillart, Céline Louapre, Catherine Lubetzki, Caroline Papeix P2.251 Multicenter Retrospective Study of extended Dosing of Natalizumab in Multiple Sclerosis: A Strategy for Mitigating Risk of Progressive Multifocal Leukoencephalopathy While Maintaining Efficacy? Joseph Herbert, Lana Zhovtis Ryerson, Carmelo Tornatore, John Foley, Bianca Weinstock-Guttman, Ilya Kister, Krupa Pandey, Gina Remington, Teresa Frohman, Eugene Major, Sara Qureshi, Shin Beh, Darin Okuda, Puspa Utomo, Channa Kolb, David Hojnacki, Elliot Frohman Tuesday April 29 First Authors stand by Posters from 7:30 a.m.–9:00 a.m. P2.252 Immune Modulation During Natalizumab Treatment of Multiple Sclerosis. Jeffrey Greenstein P2.253 Dynamics of the Anti-JCvirus Antibody Index in an Austrian MS Cohort Peter Wipfler, Andrea Harrer, Georg Pilz, Johann Sellner, Michael Guger, Gerhard Ransmayr, Eugen Trinka, Jörg Kraus MS and CNS Inflammatory Disease: Neuro-Ophthalmology and Optical Coherence Tomography P2.254 Optical Coherence Tomography Correlates of Clinical and Imaging Outcomes in Early Multiple Sclerosis Amir Hadi Maghzi, Nisha Revirajan, Laura Julian, Rebecca Spain, Ellen Mowry, Shuang Liu, Jacqueline Marcus, Chengshi Jin, Ari Green, Charles McCulloch, Daniel Pelletier, Emmanuelle Waubant P2.255 OCT, Visual Function and MRI Measures in Acute Optic Neuritis: Baseline Data from a Clinical Trial Rhian Raftopoulos, Simon Hickman, Ahmed Toosy, Claudia Wheeler-Kingshott, Daniel Altmann, Shahrukh Mallik, David Paling, Marios Yiannakas, Klaus Schmierer, Basil Sharrack, Rose Sheridan, Gavin Giovannoni, David Miller, Raju Kapoor P2.256 Cross-platform Comparison of Retinal Neuronal Layers in Multiple Sclerosis Utilizing a Novel Open-Source Optical Coherence Tomography Automated Segmentation Algorithm Pavan Bhargava, Andrew Lang, Omar Al-Louzi, Aaron Carass, Shiv Saidha, Jerry Prince, Peter Calabresi P2.257 Diffusion Tensor Imaging Correlates of Retinal Nerve Fiber Layer Thinning in Early Multiple Sclerosis Nataliya Ternopolska, Michael Dayan, George Parlitsis, Nancy Nealon, Jai Perumal, Timothy Vartanian, Szilard Kiss, Susan Gauthier Fast, Easy Registration Online · AAN.com/view/AM14 61 Tuesday, April 29 P2.258 Optic Nerve Head Blood Flow Assessment by Optical Coherence Tomography Angiography May Be More Sensitive Than Retinal Nerve Fiber Layer Thickness in Detecting Multiple SclerosisRelated Optic Nerve Dysfunction Rebecca Spain, Xiaogang Wang, Yali Jia, Ou Tan, Dennis Bourdette, David Huang P2.259 In Vivo Assessment Of Retinal Neuronal Layers in Multiple Sclerosis Patients Muhammad Taimur Malik, Brian Healy, Bonnie Glanz, Howard Weiner, Tanuja Chitnis P2.260 Factor Affecting Recovery from Acute Optic Neuritis in Multiple Sclerosis Patients Muhammad Taimur Malik, Brian Healy, Leslie Benson, Pia Kivisakk, Alexander Musallam, Howard Weiner, Tanuja Chitnis P2.261 Retinal Structural Injury Is Worse in African-Americans than Caucasians with Multiple Sclerosis Jessica Chorostecki-Vigrass, Ginny Bao, Fen Bao, Shah Aashka, Carla Santiago Martinez, Alexandros Tselis, Christina Caon, Evanthia Bernitsas, Navid Seraji-Bozorgzad, Elliot Frohman, Omar Khan P2.262 Axonal Protective Role of LINGO-1 Blockade in the Visual System: Results from a Study in Rats and Design of a Phase 2 Clinical Trial for BIIB033, an Anti-LINGO-1 Monoclonal Antibody, in Subjects with a First Episode of Acute Optic Neuritis Diego Cadavid, Laura Balcer, Steven Galetta, Bing Hu, Kwok-Fai So, Blake Pepinsky, Sha Mi P2.263 Color Vision Impairment Is Associated with Disease Severity in Multiple Sclerosis Elena MartínezLapiscina, Santiago Ortiz-Pérez, Elena Fraga, Eloy Martínez-Heras, Iñigo Gabilondo, Sara Llufriu, Santiago Bullich, Marc FiguerasRoca, Albert Saiz, Bernardo SanchezDalmau, Pablo Villoslada P2.264 Quantification of Macular Blood Flow Volume and Microvascular Network in Multiple Sclerosis (MS) Hong Jiang, Delia Cabrera DeBuc, Silvia Delgado, Aizhu Tao, Byron Lam, Jianhua Wang MS and CNS Inflammatory Disease: Neuromyelitis Optica and Neuromyelitis Optica Spectrum Disorders P2.265 Estimated Incidence and Prevalence of Neuromyelitis Optica in the England from 1998 to 2011 Cris Constantinescu, I-Jun Chou, Chang-Fu Kuo, Radu Tanasescu, William Whitehouse P2.266 Aquaporin-4 Antibodypositive Cases Beyond Current Diagnostic Criteria for NMO spectrum Disorders Douglas Sato, Ichiro Nakashima, Toshiyuki Takahashi, Tatsuro Misu, Patrick Waters, Hiroshi Kuroda, Shuhei Nishiyama, Chihiro Suzuki, Yoshiki Takai, Kazuo Fujihara, Yasuto Itoyama, Masashi Aoki P2.268 Anti-Aquaporin-4 Antibodies Without Optic Neuritis or Transverse Myelitis Robert Joshua, Bonnie Keung, Meena Gujrati, Michael Zagardo, Jorge Kattah P2.269 Neuromyelitis Optica with Severe Behavioral Dysregulation: A Case Report Teri Schreiner, Cassie Karlsson, Harrison Levine, Julia Barnes, John Binder, Robin Gabriels, Carol Beresford P2.270 Hydrocephalus in Neuromyelitis Optica Stacey Clardy, Claudia Lucchinetti, Karl Krecke, Vanda Lennon, Orna O’Toole, Brian Weinshenker, Clara Boyd, Stephen Krieger, Corey McGraw, Yong Guo, Sean Pittock P2.271 Presence of HLA DR10 in Mexican Patients with Neuromyelitis Optica (Devic’s Disease) Veronica Rivas, Jose de Jesus Flores, Teresa Corona Vazquez, Julio Granados P2.272 Distinct Acute Spinal Cord Syndrome Between Aquaporin4IGG Seropositive and Seronegative Longitudinally Extensive Transverse Myelitis Samira Apostolos-Pereira, Douglas Sato, Frederico Jorge, Paula Melo, Paulo Marchiori, Dagoberto Callegaro 7:30 a.m.–11:00 a.m. P2.280 The Course Of Ocular Myasthenia Gravis: A Retrospective Study Of 162 Patients Joao Lemos, Lina Nagia, Khawla Abusamra, Brooke Johnson, Wayne Cornblath, Jonathan Trobe, Christopher Glisson, Sunita Yedavally, David Kaufman, Eric Eggenberger P2.281 Role of Mitochondrial Reactive Oxygen Species in Cell Death Caused by Connexin 26 Mutations Associated with Keratitis-ichthyosisDeafness Syndrome Xueshui Guo, Sabrina Yum P2.282 Modified Brainstem Auditory Evoked Responses Are Associated with Elevated Intracranial Pressure in Subjects with Idiopathic Intracranial Hypertension Heather Moss, John Fino, Heeren Patel, James Stone P2.283 Transcranial Direct Current Stimulation for the Treatment of Chronic Tinnitus: A Randomized, Double-Blind, Sham Controlled Study David Benninger, Natassja Pal, Marianne Stephan, Francois Herrmann, Raphael Maire P2.284 Evolution of Macular Findings Is Optic Neuritis Incidence Rising? Evidence from an Epidemiological Study in Barcelona, Spain 20082012 Elena Martínez-Lapiscina, Elena Fraga, Xavier Pastor, Mónica Gómez, Artur Conesa, Raimundo Lozano-Rubí, Bernardo Sanchez-Dalmau, Alvaro Alonso, Pablo Villoslada P2.293 Optical Coherence Tomography Visualization of Optic Nerve Head Structure Detects Acute Changes in the Intracranial Pressure Aashish Anand, Anastas Pass, Eusebia Calvillo, Rosa Tang, Christian Cajavilca, Mian Urfy, Jose Suarez, Chethan Rao, Eric Bershad P2.294 Comparison Rate Between Headshaking Maneuver And Vibration Maneuver in Ageotrophic Horizontal BPPV Hyoung Suk Han, Dae Soo Shin P2.295 Endovascular Treatment of Cerebral Venous Sinus Thrombosis with Combination of Rheolytic Thrombectomy, Angioplasty and tPA Thrombolysis Reversed Severely Elevated ICP Syndrome: A Case Study. Takamasa Higashimori, Joshua Seinfeld, Victoria Pelak on Optical Coherence Tomography (OCT) in Papilledema Farah Villanueva, Fawzi Abukhalil, Mark Morrow P2.296 P2.285 Measuring Transmission Delay P2.297 P2.274 P2.286 Retinal Ganglion Cell Layer P2.298 Neuro-ophthalmology/ Neuro-otology I P2.287 P2.299 P2.273 Myelin Oligodendrocyte Glycoprotein (MOG) Associated Neuromylitis Optica Sprectum Disorder (NMOSD) Presenting with Isolated Absent F Wave Shahpar Nahrir, Naim Kajtazi, Jameelah Saeedi Differential Diagnosis of Transverse Myelitis Maureen Mealy, Daniel Becker, Scott Newsome, John Ratchford, Michael Levy, Carlos PardoVillamizar P2.275 The Characteristics of Square Wave Jerks in Normal Subjects Michael Rosenberg, Anitha Nimma, Gita Pisupati, Neha Rane P2.276 Temporal Aspects of Visual Perception Following Demyelination Gabriel Shear-yashuv, Noa Raz, Shlomo Dotan, Panayiota Petrou, Adi Vaknin-Dembinsky, Netta Levin P2.277 Lamotrigine as an Effective Pharmacotherapy for Ménière’s Disease: A Case Series Lixin Zhang, Merika Wilson P2.278 Diagnostic Algorithm for Approaching Patients with Suspected Giant Cell Arteritis M. Tariq Bhatti, Mays El-Dairi, Alan Proia, Thomas Cummings P2.279 High Resolution Optical Coherence Tomography of the Retina Demonstrates Selective Changes in Individual Retinal Layers in Parkinson’s Disease Irene Gottlob, Anastasia Pilat, Rebecca McLean, Gail Maconachie, Viral Sheth, Yusuf Rajabally, Frank Proudlock Due to Demyelination in INO Alessandro Serra, Margaret Skelly, Manuela Matta, Jonatan Jacobs, Mark Walker, Jeffrey Cohen, R. John Leigh Thinning Within One Month of Presentation for Non-arteritic Anterior Ischemic Optic Neuropathy and Optic Neuritis Mark Kupersmith, Mona Garvin, Jui-Wang Wang, Mary Durbin, Randly Kardon Incidence of Visual Defects in Epileptic Children Treated with Vigabatrin Mohammadkazem Bakhshandeh Bali P2.288 Clinical Characteristics of Recurrent Benign Paroxysmal Positional Vertigo Seung-Han Lee, Jong-Kyung Lee, Yun-Ju Choi, Jae-Myung Kim, Byung-Kun Kim P2.289 Spectral Domain Optical Coherence Tomography Findings in Myotonic Dystrophy. Maria Laura Ester Bianchi, Edoardo Abed, Guglielmo D’Amico, Marcella Masciullo, Gabriella Silvestri P2.290 Diffusion Tensor Imaging Evaluations of Visual Pathways in Multiple Sclerosis Patients with Acute and Chronic Optic Neuritis Ahmet Onur Keskin, Fethi Idiman, Alatas Ozkan, Emel Ada, Ali Osman Saatci, Egemen Idiman P2.291 The Relationship Between Optical Coherence Tomographic (OCT) and Perimetric Findings in Patients with Papilledema Mark Morrow P2.267 Pain at Onset of Neuromyelitis Optica Elizabeth Shuster, Reema Kola, Tori Hysko, Melanie Box 62 P2.292 2O14 Scientific Abstract Listing and Annual Meeting Information Abnormal Electroretinogram in Neuromyelitis Optica Spectrum Disorder Aimee Szewka, Anjali Tannan Unusual Presentation of an Isolated III Cranial Nerve Palsy from Brain Metastasis Saiqa Choudhry, Reuben Valenzuela, Hrachya Nersesyan, Jorge Kattah Analysis of Anatomical and Functional Outcome in Three Months Follow up After a Single Intravitreal Dexamathazone (Ozurdex) Injection in Retinal Vein Occlusion Avathvadi Srinivasan Utility of Optical Coherence Tomography Measurements as a Biomarker for Systemic Lupus Erythematosus with or Without Neuropsychiatric Symptoms Gabrielle Liu, Jacqueline Bernard P2.300 Videoculography (VOG) Findings with 4 Aminopyridine in Downbeat Ny (DBN): Description of 3 Cases Ana Bisonni, Guillermo Videla, Edgardo Cristiano P2.301 Dynamic Formation of Macular Microcysts Independent of Vitreous Traction Changes Timm Oberwahrenbrock, Ella Kadas, Wolf Lagrèze, Friedemann Paul, Alexander Brandt P2.302 Oculomotor Dysfunction Due to Idiopathic Intracranial Hypertension and Thiamine Deficiency Channaiah SrikanthMysore, Blanca Marky CNS Infectious Disease: Miscellaneous P2.303 Predictive Factors of Central Nervous Infection: Prospective Evaluation of 124 Cases with Suspicion of Meningitis. Irene Trevino, Maria Alejandra Gonzalez Duarte, Alberto Avila-Funes P2.304 A Retrospective Study of Presenting Clinical and Laboratory Variables in HIV Negative Tuberculous Meningitis Patients Brian Chisulo Poster Session II P2.305 NELL-2 as a Biomarker in Diagnosing Tuberculous Meningitis: An iTRAQ Based Quantitative Proteomic Analysis of Cerebrospinal Fluid Zesong Yang P2.306Next-Generation Sequencing for Pathogen Discovery in Meningoencephalitis Michael Wilson, Erik Samayoa, Samia Naccache, Sneha Somasekar, Guixia Yu, Joseph DeRisi, Charles Chiu P2.307 Varicella Zoster Virus Lumbar Radiculitis: A Case Report Jazba Soomro, Hesham Allam, Aninda Acharya P2.308 First Case of Familial Creutzfeldt-Jakob Disease Associated with E200K Mutation in Peru: A Case Report Jonathan Eskenazi P2.309 Evoked Potentials in Sarcoidosis Patient Renata Hebel, Zyta Banecka Majkutewicz P2.310 Causes of Encephalitis in Buenos Aires: A Retrospective Cohort Study Wilken Miguel, Mauricio Farez, Ameghino Lucía, Julieta Arena, Angel Cammarota, Martin Alejandro Nogues Bacterial Illnesses of CNS and West Nile Virus P2.311 MRI Ventral Nerve Root Enhancement In 3 Patients Presenting with Lower Extremity Weakness Secondary to West Nile Virus Chirag Patel, Shrikant Mishra, Bhavesh Trikamji, Brian Zipser P2.312 The N-methyl-D-aspartate Receptor Encephalitis Mimicking Bacterial Meningitis Jeremy Ragland, Hannah Goldstein, Barry Czeisler, Jan Claassen, Stephan Mayer, Sachin Agarwal P2.313 Diagnostic Dilemma of Encephalomyelitis Due to Lyme Neuroborreliosis Tiffani Stroup, Sheeraz Daudi, Heeren Patel P2.314 Disseminated Cerebritis with Myelitis by Propionibacterium Acnes in Healthy Elderly Female Jinsan Lee, Sung Hyuk Heo, Dae-Il Chang, Ji Hoon Lee, Seon Hee Bu P2.315Rhombencephalitis Due to Listeria Monocytogens in Immunocompetent Patient Ruchir Shah, Umang Shah, Thomas Bosley P2.316Syphilitic Polyradiculoneuropathy in an Immunocompetent patient Safaa Zahlane, Nissrine Louhab, Najib Kissani P2.317 Widespread Leptomeningeal Involvement in Borreliosis Carolina Maciel, Erwin Wang, Prasad Shirvalkar, Alexander Merkler, Joseph Safdieh P2.318 Arachnoiditis Associated with an Unusual Pathogen: Aerococcus Urinae Kara Steijlen, Shawn Vasoo, Berbari Elie, Carrie Robertson P2.319 PATTERN of Nerve Conduction Study IN leprosy neuropathy Marcia Jardim, Robson Vital, Salim Balassiano, Mariana Hacker, Ximena Illarramendi, Euzenir Sarno P2.320 A Case Report of CNS Whipple’s Disease Daniel Smith Fungi, Parasites, and Other Pathogens P2.321 A Young Woman with Seizures: A Case of Neuroschistosomiasis Eli Zimmerman, Matthew Rose, Liangge Hsu, Alexandra Golby, Rebecca Folkerth, Sandro Santagata, Danny Milner, Shakti Ramkissoon P2.322 A Rare Case of Isolated Intramedullary Cervical Spine Neurocysticercosis That Was Initially Misdiagnosed and Treated as Demyelinating Disease—a Case Report. Crystal Dixon, Yazan Suradi, Rossitza Chichkova P2.323 Meningitis Due to Cryptococcus gattii: First Reported Case of an Emerging Infectious Disease in an Immunocompetent Patient Residing in the Northeast United States Katie Warren, Colum Amory, Ellis Tobin P2.324 The Rhino Without Its Sugar Jasmine Kahlon, Harneet Gahley, Niket Sonpal, Robert Graham P2.325 Necrotizing Cryptococcal Fasciitis of the Lower Extremity: Report of a Case Following Orthotopic Cardiac Transplantation for Systemic Amyloidosis Matthew Cykowski P2.326 CSF and CSF:Serum Ratios of (1,3)-beta-D-glucan Are Lower in Non-Fungal CNS Pathology than Proven or Probable Fungal CNS Disease Jennifer Lyons, Kiran Thakur, Sean Zhang P2.327 Chronic Meningitis by Histoplasma Capsulatum in Immunocompetent Patients: a Diagnostic Challenge Bruna Silva, Alberto Martinez, Marcondes França Jr., Anamarli Nucci, Augusto Penalva-de-Oliveira P2.328 A Case of Ciguatera Poisoning in a New York City Hospital: Learning Points for Hospitals Serving Diverse Immigrant Populations. Neville Jadeja, Ali Haider, Reena Gottesman, Mark Kozicky, Abhinav Nafday, Kyle Kelson, Nana Jinjolava P2.336 P2.329 P2.337 Acute Necrotizing Encephalopathy Caused by Influenza A Leading to a Rapidly Progressive Amnestic Syndrome and Coma Brett McCray, Deborah Forst, Galen Henderson Child Neurology and Developmental Neurology II P2.330 Trends in Outcome and Hospitalization Charges of Pediatric Patients Admitted with Guillain Barre Syndrome Treated with Plasmapheresis in the United States. Data from Kids’ Inpatient Database (KID) 19972009 Weizhen Wang, Wenzhuan He, Nizar Souayah P2.331 Trends in Outcome and Hospitalization Charges for Pediatric Patients Admitted with Guillain Barre Syndrome Treated with Intravenous Immunoglobulin in the United States. Data from Kids’ Inpatient Database (KID), 19972009 Kathleen Sullivan, Ankit Pahwa, Nizar Souayah P2.332 Trends in Outcome and Hospitalization Charges of Pediatric Patients Admitted with Botulism in the United States: A Comparative Analysis Between Kids’ Inpatient Database (KID) and National Inpatient Sample (NIS) Mohammad El-Ghanem, Ankit Pahwa, Nizar Souayah P2.333 The Six-Minute Walk Test Captures Weakness and Gait Abnormalities in Glut 1 Deficiency Syndrome Michelle Blumenschine, Jacqueline Montes, Ashwini Rao, Aliza Alter, Kristin Engelstad, Darryl De Vivo Regional Hippocampal Involvement in Paediatric Multiple Sclerosis: A Radial Mapping MR Study Maria Elisa Morelli, Maria Rocca, Elisabetta Pagani, Lucia Moiola, Angelo Ghezzi, Andrea Falini, Giancarlo Comi, Massimo Filippi MHCI Immune Molecules Are Required for Developmental Synapse Elimination of the Neuromuscular Junction Mazell Tetruashvily, Lisa Boulanger P2.338 NextGen Sequencing as a Tool to Assist in Diagnosis and Expedite Treatment: RAPSN Congenital Myasthenic Syndrome Alvin Das, Dimitri Agamanolis, Bruce Cohen P2.339 A Neonatal Case of Congenital Myasthenic Syndrome with COLQ Mutation Matthew Imperioli, Cristian Ionita, Gyula Acsadi, Andrew Engel Medical Student Essay Award Recipients Tuesday April 29 First Authors stand by Posters from 7:30 a.m.–9:00 a.m. P2.340 Voice Discrimination and Recognition in Patients with Prosopagnosic Complaints Ran (Richard) Liu P2.341 HAT Score Outperforms 7 other Hemorrhagic Transformation Scores David Asuzu P2.342 Subspecialization in Neurology: Historical Perspectives on Current Challenges Trent Hodgson P2.343 Probing the Interaction of the Ipsilateral Posterior Parietal Cortex with the Premotor Cortex Using a Novel Transcranial Magnetic Stimulation Technique Jessica Shields P2.334 Longest Living Reported Case of Congenital Myopathy with Excess of Muscle Spindles Julia Henry, Yael ShilohMalawsky, Stevie Rowe, Zheng Fan P2.335 Muscular Distrophy, Mental Retardation and Deletion 2q37: A Case Report Cristiane Rocha, Carlos Andrade, Isabel Pinheiro, Alzira Carvalho Membership Pays! Did you know? AAN members save 50% or more on Annual Meeting Registration and program fees. Make sure your membership is up-to-date. Join or renew your AAN membership at AAN.com/membership. Fast, Easy Registration Online · AAN.com/view/AM14 63 Tuesday, April 29 Current as of 2/13/2014 Presidential Plenary Session 9:00 a.m.–12:00 p.m. F eatures the AAN’s premier lecture awards for clinically relevant research and a presentation by a leading lecturer. Top researchers speak on some of the most significant findings in neurology in 2014. Moderator: Lisa M. DeAngelis, MD, FAAN Chair, Science Committee Presidential Lecture: James L. Bernat, MD, FAAN Dartmouth Hitchcock Medical Center, Lebanon, NH Challenges to Ethics and Professionalism Facing the Contemporary Neurologist George C. Cotzias Lecture: Endowed by Roche Pharmaceuticals. Stefan M. Pulst, MD, FAAN University of Utah, Salt Lake City, UT Degenerative Ataxias: From Genes to Therapies Sidney Carter Award in Child Neurology Lecture: Endowed by an anonymous donor. Darryl C. De Vivo, MD, FAAN Columbia University Medical Center, New York, NY Rare Diseases and Neurological Phenotypes Robert Wartenberg Lecture: David M. Holtzman, MD, FAAN Washington University School of Medicine, St. Louis, MO Alzheimer’s Disease in 2014: Mapping a Road Forward For Full Abstracts and Bios for Plenary Speakers Visit AAN.com/view/SearchAM 64 2O14 Scientific Abstract Listing and Annual Meeting Information Section Topic Controversies S3 Section Topic Controversies: PFO: Aggressive Treatment or Just Aspirin 1:00 p.m.–2:30 p.m. 1:00 p.m.–1:05 p.m.Introduction Antonio Culebras, MD, FAAN, FAHA 1:05 p.m.–1:30 pm. PFO: Aggressive Treatment John D. Carroll, MD 1:30 p.m.–1:55 p.m. PFO: Just Aspirin Steven R. Messé, MD, FAAN, FAHA 1:55 p.m.–2:05 p.m.Rebuttal John D. Carroll, MD 2:05 p.m.–2:15 p.m.Rebuttal Steven R. Messé, MD, FAAN, FAHA Open Discussion/Conclusion Antonio Culebras, MD, FAAN, FAHA Tuesday April 29 2:15 p.m.–2:30 p.m. Obtaining Your CME and Evaluations To receive CME for education programs or scientific sessions, evaluations must be completed online or via the Annual Meeting mobile app. Wireless internet hotspots will be available at the convention center. Details will be provided prior to the meeting. Education Program Syllabi Full text syllabi and program slides will be available electronically only—online or via the Annual Meeting mobile app. All registered attendees will receive an email notification once syllabi are available. Fast, Easy Registration Online · AAN.com/view/AM14 65 Tuesday, April 29 S4 MS and CNS Inflammatory Disease: Clinical Trials 1:00 p.m. S4.001 Rationale for Advancing Laquinimod for Progressive MS: Evidence from Large Clinical Trials in RRMS Giancarlo Comi, Maria Pia Sormani, Gavin Giovannoni, David Ladkani, Nissim Sasson, Talia Gorfine, Volker Knappertz 1:15 p.m. S4.002 Safety and Tolerability of DelayedRelease Dimethyl Fumarate Administered as Add-On Therapy to Beta Interferons or Glatiramer Acetate in Relapsing-Remitting Multiple Sclerosis (RRMS) Patients Vissia Viglietta, Timothy Vollmer, Ray Zhang, Mark Novas, Sarah Sheikh, Robert Fox 1:30 p.m. S4.003 Peginterferon Beta-1a May Improve Recovery Following Relapses: Data from the Pivotal Phase 3 ADVANCE Study in Patients with RelapsingRemitting Multiple Sclerosis Bernd Kieseier, Thomas Scott, Scott Newsome, Sarah Sheikh, Serena Hung, Xiaojun You, Bjorn Sperling 1:45 p.m. S4.004 Effect of Fingolimod on Macular Volume and Retinal Nerve Fiber Layer Thickness: A One-year Longitudinal Study Pavle Repovic, Dong Won Lee, Steven Hamilton, Eugene May, James Bowen 2:00 p.m. S4.005 Interim Analysis of 2-year Clinical Efficacy and Safety of Peginterferon Beta-1a in Patients with RelapsingRemitting Multiple Sclerosis: Data from the Pivotal Phase 3 ADVANCE Study Aaron Deykin, Douglas Arnold, Serena Hung, Sarah Sheikh, Ali Seddighzadeh, Ying Zhu, Shifang Liu, Bernd Kieseier 2:15 p.m. S4.006 Natalizumab Treatment Improves Walking Speed in MS Patients: A Post Hoc Analysis of AFFIRM Richard Rudick, Michael Hutchinson, Eva Havrdova, Xiaojun You, Diego Cadavid, Shibeshih Belachew 2:30 p.m. S4.007 Peginterferon Beta-1a Significantly Increases the Proportion of Patients with Freedom from Measured Disease Activity in RelapsingRemitting Multiple Sclerosis: Findings from the ADVANCE Study Douglas Arnold, Bernd Kieseier, Sarah Sheikh, Aaron Deykin, Ying Zhu, Xiaojun You, Bjorn Sperling, Serena Hung 66 S5 Cerebrovascular Disease and Interventional Neurology: Pre-hospital, Telemedicine, and Related Topics 1:00 p.m. S5.001 The REliability of MObile TEchnologies for Acute Stroke Neuroimaging Data Interpretation: The REMOTE Study Clotilde Balucani, Sundeep Mangla, Adrian Marchidann, Michael Szarek, Wissa Usama, Yitzchok Lederman, Charles Ramkishun, Lin Wang, Ethan Brandler, Pia Chatterjee, Susan Law, Craig Linden, Gautam Mirchandani, Diana Rojas-Soto, Daniel Rosenbaum, Hyman Shwarzberg, Richard Sinert, Mark Silverberg, Helen Valsamis, Volodymyr Vulkanov, Shahriar Zehtabchi, David Aharonoff, James Gugger, Mohit Sharma, Andrew Truong, Steven Levine 1:15 p.m. S5.002 Mobile Telestroke During Ambulance Transport Is Feasible in a Rural EMS Setting—Pilot Data from the Improving Treatment with Rapid Evaluation of Acute Stroke via Mobile Telemedicine (iTREAT) Study Sherita Chapman, Jason Lippman, Brian Gunnell, Timothy McMurry, Prachi Mehndiratta, Donna Burns, Debra Perina, David Cattell-Gordon, Nina Solenski, Bradford Worrall, Andrew Southerland 1:30 p.m. S5.003 Tablet Computers Address Limitations of Telestroke Systems Steven Rudolph, Susan Law, Holly Morhaim, Jill Slater 1:45 p.m. S5.004 Enrolling Patients in Ambulance Stroke Trials Using Mobile Televideo Consent: Preliminary Experience. Amrit Ahluwalia, Sidney Starkman, Nerses Sanossian, David Liebeskind, Latisha Ali, Lucas Restrepo, May Kim-Tenser, Miguel Valdes-Sueiras, Marc Eckstein, Franklin Pratt, Samuel Stratton, Robin Conwit, Jeffrey Saver 2:00 p.m. S5.005 Strategy to a 5-Minute Door to Needle Time Sarah Parker, Teresa Swanson-Devlin, Jan Jahnel, Clayton McNeil, Arun Talkad, Judith Beck, Deepak Nair, David Wang 2:15 p.m. S5.006 Reducing Time to Treatment—The Role of Stroke Neurologist as First Responder Shelly Ozark, Perette Sabatino, Christine Holmstedt, Tanya Turan 2:30 p.m. S5.007 Novel Graphical Comparative Analyses of 7 Prehospital Stroke Scales Mohit Sharma, Richard Sinert, Steven Levine, Ethan Brandler 1:00 p.m.–2:45 p.m. S6 Neuromuscular Disease: Gene Therapy S7 Parkinson's Disease: Preclinical and Clinical Therapeutics 1:00 p.m. S6.001 Safety Profile and Pharmacokinetic Properties of Eteplirsen in the Treatment of Boys with Duchenne Muscular Dystrophy Jihad Saoud, Jerry Mendell, Louise RodinoKlapac, Zarife Sahenk, Kandice Roush, Loren Bird, Linda Lowes, Lindsay Alfano, Ana Maria Gomez Ramirez, Sarah Lewis, Vinod Malik, Kim Shontz, Christopher Shilling, Peter Sazani, Edward Kaye 1:00 p.m. S7.001 A Large-Scale Non-Human Primate Study of the Safety and Efficacy of Neural Stem Cells Derived from Human Pluripotent Stem Cells Ruslan Semechkin, Rodolfo Gonzalez, Ibon Garitaonandia, Alina Ostrowska, Tatiana Abramihina, Gerald Wambua, Alexander Noskov, Andrew Crain, Maxim Poustovoitov, Francesca Boscolo, Louise Laurent, Evan Snyder, Eugene Redmond 1:15 p.m. S6.002 Results at 96 Weeks of a Phase IIb Extension Study of the Exon-Skipping Drug Eteplirsen in Patients with Duchenne Muscular Dystrophy (DMD) Edward Kaye, Jerry Mendell, Louise Rodino-Klapac, Zarife Sahenk, Kandice Roush, Loren Bird, Linda Lowes, Lindsay Alfano, Ana Maria Gomez Ramirez, Sarah Lewis, Vinod Malik, Kim Shontz, Christopher Shilling, Peter Sazani, Jihad Saoud 1:15 p.m. S7.002 TIGAR Inhibition Rescues Dopaminergic Neurons in Common Forms of Early Onset Parkinson’s’ Disease Oliver Bandmann, Marcus Keatinge, Marc DaCosta, Heather Mortiboys, Laura Flinn 1:30 p.m. S6.003 Results of a Phase 2 Open-Label Study of ISIS-SMNRx in Patients with Infantile (Type 1) Spinal Muscular Atrophy Richard Finkel, John Day, Claudia Chiriboga, Jiri Vajsar, Dawn Cook, Karolina Watson, Shirley Paulose, Rosangel Cruz, Jacqueline Montes, Darryl De Vivo, Mason Yamashita, Dawn McGuire, Katie Alexander, Daniel Norris, Frank Bennett, Kathie Bishop 1:45 p.m. S6.004 Future Clinical and Biomarker Development for SMT C1100, the First Utrophin Modulator to Enter Clinical Trials for Duchenne Muscular Dystrophy (DMD) Jon Tinsley, Neil Robinson, Francis Wilson, Graeme Horne, Kay Davies 2:00 p.m. S6.005 Gene Therapy in a Model of CMT1X Neuropathy Using a Lentiviral Vector Kleopas Kleopa, Alexia Kagiava, Stavros Bashardes, Jan Richter, Christina Christodoulou, Irene Sargiannidou 2:15 p.m. S6.006 Treatment of Experimental CIDP Using Lentivirus Transduced Dendritic Cells Expressing VIP Mehmet Yalvac, William Arnold, Syed-Rehan Hussain, Cilwyn Braganza, K. Reed Clark, Eroboghene Ubogu, Jerry Mendell, Zarife Sahenk 2:30 p.m. S6.007 Schwann Cell-Derived Desert Hedgehog Provides a Neuroprotective Effect Against the Mechanical Stimuli from Compressive Neuropathies Tahseen Mozaffar, James Jung, Derek Frump, Jared Su, Ranjan Gupta 2O14 Scientific Abstract Listing and Annual Meeting Information 1:30 p.m. S7.003 Isradipine Rescues Alpha-synuclein Toxicity in a Zebrafish Model of Parkinson’s Disease by Upregulating Autophagy Mark Stahl, Shubhangi Prabhudesai, Aaron Lulla, Jeff Bronstein 1:45 p.m. S7.004 Phase-3 Clinical Trial of the Adenosine 2a Antagonist Preladenant, Given as Monotherapy, in Patients with Parkinson’s Disease Fabrizio Stocchi, Olivier Rascol, Robert Hauser, Susan Huyck, Anjela Tzontcheva, Rachel Capece, Kenneth Wolski, Tony Ho, Peter Sklar, Christopher Lines, David Michelson, David Hewitt 2:00 p.m. S7.005 Global Long-term Registry on Efficacy and Safety of DUODOPA in Patients with Advanced Parkinson’s Disease in Routine Care (GLORIA): 12-month interim findings Angelo Antonini, Ashley Yegin, Cornelia Preda, Werner Poewe 2:15 p.m. S7.006 Real Life Aerobic Walking Exercise in Parkinson’s Disease Ergun Uc, Kevin Doerschug, Jeffrey Dawson, Joel Kline, Sara Newman, Warren Darling 2:30 p.m. S7.007 Rapid Levodopa Augmentation Following Inhaled CVT-301 Results in Rapid Improvement in Motor Response When Administered to PD Patients in the OFF State Martin Freed, Donald Grosset, Paul Worth, Tanya Gurevich, Tia Defeo-Fraulini, Jerome Moore, Richard Batycky S8 Aging, Dementia, and Cognitive and Behavioral Neurology: PET Imaging 1:00 p.m. Presentation of Potamkin Prize for Research in Pick’s, Alzheimer’s, and Related Diseases Recipient: M. Marsel Mesulam, MD Chicago, IL 1:30 p.m. S8.003 Cerebral Amyloid Related Alterations in Neuronal Metabolism and the Contribution of Multimodal Measures of Vascular Function. Eric McDade, Albert Kim, Timothy Hughes, Beth Snitz, Ann Cohen, Julie Price, Chester Mathis, James Becker, William Klunk, Oscar Lopez 1:45 p.m. S8.004 Integrated Analysis of (123I)FP-CIT (DaTscan; Ioflupane I123 Injection) SPECT Brain Imaging—Diagnostic Effectiveness in Patients with Movement Disorders and/or Dementia Donald Grosset, Igor Grachev, John O’Brien, Ian McKeith, Walker Zuzana, Klaus Tatsch, Eduardo Tolosa, Paul Sherwin, Wolfgang Oertel 2:00 p.m. S8.005 Diagnostic Accuracy of Amyloid and FDG PET in Pathologically-Confirmed Dementia Gil Rabinovici, Manja Lehmann, Howard Rosen, Pia Ghosh, Brendan Cohn-Sheehy, John Trojanowski, Mario Mendez, Harry Vinters, Dennis Dickson, Marilu Gorno-Tempini, Adam Boxer, Joel Kramer, Bruce Miller, Lea Grinberg, William Seeley, William Jagust 2:15 p.m. S8.006 FDG PET, Aging and APOE Genotype in Cognitively Normal Persons David Knopman, Clifford Jack, Heather Wiste, Emily Lundt, Stephen Weigand, Prashanthi Vemuri, Jeffrey Gunter, Val Lowe, Kejal Kantarci, Matthew Senjem, Michelle Mielke, Rosebud Roberts, Bradley Boeve, Ronald Petersen 2:30 p.m. S8.007 Imaging Tau Pathology in vivo in FTLD: Initial Experience with (18F) T807 PET Bradford Dickerson, Kimiko Domoto-Reilly, Daisy Hochberg, Michael Brickhouse, Michael Stepanovic, Keith Johnson Scientific Sessions 1:00 p.m. Presentation of Sleep Science Award Recipient: Claudia Trenkwalder, MD Kassel, Germany 1:15 p.m. Presentation of Wayne A. Hening Sleep Medicine Investigator Award Recipient: Aleksandar Videnovic, MD, MSc Boston, MA 1:30 p.m. S9.003 Bright Light Therapy Improves Excessive Daytime Sleepiness Associated with Parkinson’s Disease Aleksandar Videnovic, Angelica Marconi, Teresa Kuhta, Scott Miskevics, Phyllis Zee 1:45 p.m. S9.004 Distinct Innervation Patterns of the Melanin Concentrating Hormone Neurons from the Basal Forebrain Structures Minjee Kim, Lindsay Agosstinelli, Thomas Scammell 2:00 p.m. S9.005 Antibodies Against the Cell Adhesion Molecule IgLON5 Identify a Novel Tauopathy with NREM/REM Parasomnia and Sleep Breathing Disorder Carles Gaig, Lidia Sabater, Ellen Gelpi, Luis Bataller, Jan Lewerenz, Estefania Torres-Vega, Angeles Contreras, Bruno Giometto, Yaroslau Compta, Cristina Embid, Isabel Vilaseca, Alex Iranzo, Joan Santamaria, Josep Dalmau, Francesc Graus 2:15 p.m. S9.006 The Effects of Obstructive Sleep Apnea on Olfactory Functions Tekeli Hakan, Murat Salihoğlu, Mustafa Kendirli, Aytuğ Altundağ, Melih Cayonu, Mehmet Şenol, Ozdag Fatih S10 HIV, PML, and Cerebral Malaria 1:00 p.m. Presentation of Bruce S. Schoenberg International Award in Neuroepidemiology Recipient: Devender Bhalla, PhD Limoges, France 1:30 p.m. S10.003 Delivery of Tenofovir to the Brain by Novel Nano-Vesicles for the Treatment of Neuro-HIV Eliahu Heldman, Charles Linder, Sarina Grinberg, Mary Popov, Irwin Hollander 1:45 p.m. S10.004 Voxel Based Morphometry Findings in an Irish Cohort of HIV Positive Patients Patricia McNamara, Janice Redmond, Peter Bede, Andrew Fagan, Colm Bergin, Arun Bokde, Colin Doherty 2:00 p.m. S10.005 Development of a Functional Scale for Progressive Multifocal Leukoencephalopathy: The NIH PML Scale Gloria Von Geldern, Irene Cortese, Joan Ohayon, Daniel Reich, Avindra Nath 2:15 p.m. S10.006 Survival of Non-AIDS Progressive Multifocal Leukoencephalopathy Yuri Hanada, Allen Aksamit 2:30 p.m. S10.007 Performance of Cerebrospinal Fluid (CSF) Plasmodium falciparum Histidine-Rich Protein-2 (pfHRP-2) in Prediction of Death in Cerebral Malaria Kiran Thakur, Jimmy Vareta, Kathryn Carson, Terrie Taylor, David Sullivan, Karl Seydel S11 Neuro Trauma, Critical Care, and Sports Neurology 1:00 p.m. S11.001 Axonal Injury, Neuroinflammation and Amyloid Pathology after Traumatic Brain Injury: Making Connections to Neurodegeneration David Sharp, Gregory Scott, Ramlackasingh Anil, Hellyer Peter, Leech Robert, Federico Turkheimer, Paul Matthews, David Brooks 1:15 p.m. S11.002 Evolution of Traumatic Parenchymal Intracranial Hematomas (ICHs): Comparison of High Density and Low Density Components. Sean Wilkes, Erin McCormack, Leah Harburg, Tanya Bogoslovsky, Kimbra Kenney, Dzung Pham, Ramon Diaz-Arrastia 1:30 p.m. S11.003 King-Devick Test Identifies Symptomatic Concussion in Realtime and Asymptomatic Concussion Over Time. Priya Dhawan, Amaal Starling, Lisa Tapsell, Jennifer Adler, Steven Galetta, Laura Balcer, David Dodick 1:45 p.m. S11.004 Prognostic Value of Post-anoxic Myoclonus and Malignant EEG Patterns in Comatose Cardiac Arrest Survivors Treated with Hypothermia Edilberto Amorim, Alexandra Popescu, Maria Baldwin, Yin Zhao, Jon Rittenberger 2:00 p.m. S11.005 Blood Biomarkers for Brain Injury in Concussed Professional Ice Hockey Players Pashtun Shahim, Yelverton Tegner, David Wilson, Jeffrey Randall, Birgitta Kallberg, Kaj Blennow, Henrik Zetterberg 2:15 p.m. S11.006 Increased Connectivity Between the Sensorimotor Cortex and Dorsal Attention Network in Children After Mild to Moderate Traumatic Brain Injury Sarah Risen, Anita Barber, Stewart Mostofsky, Stacy Suskauer 2:30 p.m. S9.007 Nocturnal Melatonin Regulation in Post-Traumatic Vegetative State: A Possible Role for Melatonin Supplementation? Pietro Guaraldi, Elisa Sancisi, Giovanna CalandraBuonaura, Chiara La Morgia, Valerio Carelli, Cameli Olivia, Alberto Battistini, Pietro Cortelli, Roberto Piperno 2:30 p.m. S11.007 Development of a Medical Device for the Rapid Assessment of Concussion Donald Weaver, Ying Tam, Christopher Barden, Ryan D’Arcy, Love Kalra, Lauren Petley, Chen Wei S12 Cerebrovascular Disease and Interventional Neurology: Epidemiology and Risk Factors 1:00 p.m. S12.001 Ascertainment of Stroke Incidence Among Alaskan Native Populations, 2005-2009: The Alaska Native Stroke Registry Bernadette BodenAlbala, Eric Roberts, James Allen, Lisa Bulkow, Brian Trimble 1:15 p.m. S12.002 Racial and Ethnic Disparities in Stroke. Declining Age at Time of Stroke. Analysis of the Nationwide Inpatient Sample 1988-2010 Cynthia Costa, Richard Dubinsky 1:30 p.m. S12.003 Indonesia Stroke Registry Fenny Yudiarto, Mochammad Machfoed, Amir Darwin, Anam Ong, Muhammad Karyana, - Siswanto 1:45 p.m. S12.004 Mobile Cardiac Outpatient Telemetry Identifies Occult Atrial Fibrillation After Cryptogenic Stroke Erin Ingala, Jenny Jara, Emily Fessler, Brett Cucchiara, Steven Messe, Michael Mullen, Allyson Prasad, Mathew Hutchinson, Scott Kasner 2:00 p.m. S12.005 Stroke Severity in Men and Women: What Proportion of the Disparity Can be Explained by Differences in Cardiovascular Risk Factors? Karen Albright, Amelia Boehme, Bisakha Sen, Michael Mullen, Nicole Gonzales, Sean Savitz, Sheryl Martin-Schild 2:15 p.m. S12.006 Less than Ideal: Trends in Cardiovascular Health Metrics Among US Stroke Survivors, NHANES 1988-2010 Michelle Lin, Daniela Markovic, Bruce Ovbiagele, Amy Towfighi 2:30 p.m. S12.007 Incidence and Predictors of Unprovoked Seizures After Stroke Ettore Beghi S13 MS and CNS Inflammatory Disease: MRI Atrophy Measures and Correlations 1:00 p.m. S13.001 A Gender-based 3T MRI Comparison of Brain and Spinal Cord Involvement in Relapsing-Remitting Multiple Sclerosis Antonia Ceccarelli, Gloria Kim, Jennifer Miller, Shahamat Tauhid, Tanuja Chitnis, Mohit Neema, Rohit Bakshi 1:15 p.m. S13.002 Thalamic Atrophy in RIS: MRI Evidence of Early CNS Neurodegeneration Christina Azevedo, Eve Overton, Sankalpa Khadka, Jessica Buckley, Shuang Liu, Mehul Sampat, Orhun Kantarci, Christine Lebrun Frenay, Aksel Siva, Darin Okuda, Daniel Pelletier 1:30 p.m. S13.003 Thalamic Dysfunction Is Associated with Fatigue in Patients with Multiple Sclerosis: A Graph Theory Study Massimo Filippi, Paola Valsasina, Alvino Bisecco, Alessandro Meani, Laura Parisi, Maria Josè Messina, Bruno Colombo, Andrea Falini, Giancarlo Comi, Maria Rocca 1:45 p.m. S13.004 Clinical and Paraclinical Parameters Associated with Brain Atrophy in Newly Diagnosed MS Patients. Bertrand Bourre, Christine Clerc, Frederic Blanc, Vincent Noblet, Stephane Kremer, Julien Lamy, Jean-Paul Armspach, Baradi Brice, Helene Zephir, Olivier Outteryck, Marc Debouverie, Sophie Pittion, Patrick Vermersch, Jerome De Seze 2:00 p.m. S13.005 Magnetic Resonance Imaging Correlates of Clinical Outcomes in Early Multiple Sclerosis Amir Hadi Maghzi, Nisha Revirajan, Laura Julian, Rebecca Spain, Ellen Mowry, Jacqueline Marcus, Shuang Liu, Chengshi Jin, Ari Green, Charles McCulloch, Daniel Pelletier, Emmanuelle Waubant 2:15 p.m. S13.006 Proportion of Patients with Brain Volume Loss Comparable to Healthy Adults in Fingolimod Phase 3 Multiple Sclerosis Studies Nicola De Stefano, Davorka Tomic, Dieter Haering, Allitia Dibernardo, Gordon Francis, Ernst-Wilhelm Radue, Ludwig Kappos 2:30 p.m. S13.007 Spinal Cord Lesion Load Is Associated With Disability Independently From Atrophy In Multiple Sclerosis Hugh Kearney, Rebecca Samson, Marios Yiannakas, Claudia WheelerKingshott, Olga Ciccarelli, David Miller Fast, Easy Registration Online · AAN.com/view/AM14 67 Tuesday April 29 S9 Sleep Tuesday, April 29 I5 Revolution of Genetic Tools and the Impact on Neurology 1:00 p.m.–5:00 p.m. Coordinators: Petra Kaufmann, MD and Mark F. Mehler, MD, FAAN Invited Speaker Session: 1:00 p.m.–3:30 p.m. 1:00 p.m.–1:25 p.m. Advances in Epigenetics and their Implications for Understanding and Treating Neurological Disorders Mark Mehler, MD, FAAN 1:25 p.m.–1:50 p.m. How Gene Networks and Systems Biology Informs Our Understanding of Nervous System Disease Daniel Geschwind, MD, PhD 1:50 p.m.–2:15 p.m. New Genetic Tools and Their Impact on the Diagnosis of Neuromuscular Disorders Kenneth Fischbeck, MD 2:15 p.m.–2:40 p.m. Clinical Whole-Exome Sequencing in the Diagnosis of Mendelian Disorders of the CNS Arthur Beaudet, MD 2:40 p.m.–3:05 p.m. Using Genomics in Routine Clinical Care Teri Manolio MD, PhD 3:05 p.m.–3:30 p.m. Advances in Genetics and Impact on the Treatment of Neurological Disease Beverly Davidson, PhD Poster Rounds: 3:30 p.m.–4:30 p.m. I5-1.001 Exome Sequencing Identifies PINCH2 Mutations in Early Onset Autosomal Recessive LGMD with Severe Cardiomyopathy and Triangular Tongues Jodi Warman Chardon, Amanda Smith, John Woulfe, Kawan Rakhra, Elena Pena Fernandez, Chandree Beaulieu, Jeremy Schwartzentruber, Cynthia Hawkins, Matthew Harms, Mei Zhang, Jacek Majewski, Dennis Bulman, Kym Boycott, David Dyment I5-1.002 Genetic and Neuroanatomic Associations in Sporadic Frontotemporal Lobar Degeneration Corey McMillan, Jon Toledo, Brian Avants, Philip Cook, Elisabeth Wood, Eunran Suh, David Irwin, John Powers, Christopher Olm, Lauren Elman, Leo McCluskey, Gerard Schellenberg, Virginia Lee, John Trojanowski, Vivianna Van Deerlin, Murray Grossman I5-1.003 Transcript Profiling Analysis of Alzheimer’s Disease Brains. Mariet Allen, Daniel Serie, Michael Walsh, Sun Zhifu, Saurabh Baheti, Fanggeng Zou, High Seng Chai, Curtis Younkin, Julia Crook, Vernon Pankratz, Minerva Carrasquillo, Asha Nair, Sumit Middha, Sooraj Maharjan, Thuy Nguyen, Li Ma, Kimberly Malphrus, Sarah Lincoln, Gina Bisceglio, Christopher Kolbert, Jin Jen, Ronald Petersen, Neill Graff-Radford, Dennis Dickson, Steven Younkin, Yan Asmann, Nilufer Taner I5-1.004 Novel Mutation in VCP Causes Charcot-Marie-Tooth Type 2 (CMT2) Phenotype Shawna Feely, Michael Gonzalez, Chris Weihl, Michael Shy, Stephan Zuchner I5-1.005 GCH1 Heterozygous I5-1.008 TMEM106B Is a Genetic I5-1.006 Structural and Functional I5-1.009 Expression QTL Studies in Mutation Identified by Whole-ExomeSequencing as a Treatable Condition in a Patient Presenting with Progressive Spastic Paraplegia Zheng Fan, Robert Greenwood, Ana Felix, Yael ShilohMalawsky, Myra Roche, Kristy Crooks, Jonathan Berg, James Evans Implications of Modeling Non Synonymous Mutations in Patients with SCN1A-related Seizure Disorders Mu Gao, Hongyi Zhou, Izabela Karbassi, Khalida Liaquat, Daniel Fischer, Jeffrey Skolnick, Joseph Higgins I5-1.007 The Dissection of High-Penetrance Variants in Extended Late-onset Alzheimer Disease Families by Whole-Exome Sequencing Martin Kohli, Brian Kunkle, Adam Naj, Li-San Wang, Kara Hamilton, William Perry, Regina Carney, Patrice Whitehead, John Gilbert, Eden Martin, Gary Beecham, Jonathan Haines, Gerard Schellenberg, Stephan Zuchner, Margaret Pericak-Vance Modifier of Frontotemporal Lobar Degeneration with C9orf72 Hexanucleotide Repeat Expansions Alice Chen-Plotkin, Michael Gallagher, Eunran Suh, Murray Grossman, Lauren Elman, Leo McCluskey, John Trojanowski, Virginia Lee, Vivianna Van Deerlin LOAD and PSP Brains by Next-generation RNA Sequencing Nilufer Taner, Chen Wang, Minerva Carrasquillo, Mariet Allen, Curtis Younkin, Daniel Serie, Vernon Pankratz, Thuy Nguyen, Li Ma, Kimberly Malphrus, Sarah Lincoln, Ronald Petersen, Neill Graff-Radford, Steven Younkin, Dennis Dickson, Yan Asmann Data Blitz: 4:30 p.m.–5:00 p.m. 4:30 p.m. I5-2.001 Late-onset Alzheimer Disease Neuropathology Genomic Screen Identifies Novel Loci for Neuritic Plaque and Other AD Neuropathology Features Gary Beecham, Kara Hamilton, Gerard Schellenberg, Margaret Pericak-Vance, Thomas Montine 4:35 p.m. I5-2.002 4:40 p.m. I5-2.003 The TREM2 Variant p.R47H Is a Risk Factor for Sporadic Amyotrophic Lateral Sclerosis Matthew Harms, Janet Cady, Erica Koval, Bruno Benitez, Craig Zaidman, Jennifer Jockel-Balsarotti, Peggy Allred, Robert Baloh, John Ravits, Ericka Simpson, Stanley Appel, Alan Pestronk, Alison Goate, Timothy Miller, Carlos Cruchaga TIGAR Inhibition Rescues Dopaminergic Neurons in Common Forms of Early Onset Parkinson’s Disease Oliver Bandmann, Marcus Keatinge, Marc DaCosta, Heather Mortiboys, Laura Flinn 68 4:45 p.m. I5-2.004 Investigation of Transcriptional Regulation at the Alzheimer’s Disease Risk Loci. Michaela Kachadoorian, Mariet Allen, Aditya Karhade, Lester Manly, Fanggeng Zou, High Seng Chai, Curtis Younkin, Julia Crook, Vernon Pankratz, Minerva Carrasquillo, Asha Nair, Sumit Middha, Sooraj Maharjan, Thuy Nguyen, Li Ma, Kimberly Malphrus, Sarah Lincoln, Gina Bisceglio, Christopher Kolbert, Jin Jen, Ronald Petersen, Neill Graff-Radford, Steven Younkin, Dennis Dickson, Nilufer Taner 2O14 Scientific Abstract Listing and Annual Meeting Information 4:50 p.m. I5-2.005 Spinal Muscular Atrophy Phenotype Is Ameliorated Either by SMN Increase or Modulation of Secondary Cell Death Events with RNA Therapy Giulietta Riboldi, Monica Nizzardo, Chiara Simone, Federica Rizzo, Margherita Ruggieri, Serena Pagliarani, Gianna Ulzi, Sabrina Salani, Andrea DalMas, Monica Bucchia, Emanuele Frattini, Giulia Stuppia, Francesca Magri, Nereo Bresolin, Franco Pagani, Giacomo Comi, Stefania Corti Integrated Neuroscience Sessions I6 Peripheral Neuropathies 1:00 p.m.–5:00 p.m. Coordinators: P. James B. Dyck, MD, FAAN and Tahseen Mozaffar, MD, FAAN Invited Speaker Session: 1:00 p.m.–3:30 p.m. 1:00 p.m.–1:10 p.m.Introduction Tahseen Mozaffar, MD, FAAN 1:10 p.m.–1:35 p.m. Role of Anti-Ganglioside Antibodies in Neuropathies, Including Latest Advances Kazim Sheikh, MD 1:35 p.m.–2:00 p.m. Post-Surgical Inflammatory Neuropathies P. James B. Dyck, MD, FAAN 2:00 p.m.–2:25 p.m. Role of Exome and Next Generation Sequencing in Peripheral Neuropathies Christopher J. Klein, MD 2:25 p.m.–2:50 p.m. Neuropathy in Diabetes and the Metabolic Syndrome James W. Russell, MD, MS, FRPC, FAAN 2:50 p.m.–3:15 p.m. Update on Acquired Inflammatory Demyelinating Polyradiculopathies Kenneth C. Gorson, MD 3:15 p.m.–3:30 p.m. Panel Discussion Poster Rounds: 3:30 p.m.–4:30 p.m. Transporter 1 (MCT1) Is Critical for Regeneration in Peripheral Nerves Brett Morrison, Akivaga Tsingalia, Sylvain Lengacher, Luc Pellerin, Pierre Magistretti, Jeffrey Rothstein I6-1.002 Characteristics of Muscle Cramps in Patients with Polyneuropathy Katzberg Hans, Sarah Maxwell, Seint Kokokyi, Hamid Ebadi, Ari Breiner, Vera Bril I6-1.003 Gene Therapy in a Model I6-1.004 Peripheral Edema and Weight Gain in Adult Patients with Painful Diabetic Peripheral Neuropathy (DPN) Receiving Gabapentin Enacarbil (GEn) or Pregabalin Enrolled in a Randomized Phase 2 Trial Anne Calkins, Joseph Shurman, Mark Jaros, Richard Kim, Gwendoline Shang I6-1.005 Deletion of Sarm1 Gene Protects Against Paclitaxel-induced Peripheral Neuropathy Ahmet Hoke, Elliot Turkiew, Nicole Reed of CMT1X Neuropathy Using a Lentiviral Vector Kleopas Kleopa, Alexia Kagiava, Stavros Bashardes, Jan Richter, Christina Christodoulou, Irene Sargiannidou I6-1.006 Peripheral Nerve Amyloidosis: Phenotype, Natural History, and Autonomic Dysfunction in Inherited Versus Acquired Subtypes Adam Loavenbruck, Wolfgang Singer, Paola Sandroni, Michelle Mauermann, P. James B. Dyck, Christopher Klein, Phillip Low I6-1.007 DS-5565 for the Treatment of Diabetic Peripheral Neuropathic Pain: Randomized, Double-blind, Placebo- and Active Comparator-controlled Phase II Study Aaron Vinik, Uma Sharma, Karen Feins, Ching Hsu, Domenico Merante I6-1.009 Is IVIg Therapy Warranted Tuesday April 29 I6-1.001Monocarboxylate in Progressive Lower Motor Neuron Syndromes without Conduction Block? Neil Simon, Gretchen Ayer, Catherine Lomen-Hoerth I6-1.010 Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) Sera Alter Regulators of Schwann Cell Differentiation Abhijeet Joshi, Ilja Bobylev, Christian Ritter, Andre Heinen, Helmar Lehmann I6-1.008 Neuropathy Associated with Nondiabetic Obesity J. Singleton, Eric Volckmann, Timothy Graham, Albert Smith Data Blitz: 4:30 p.m.–5:00 p.m. 4:30 p.m. I6-2.001 Schwann Cell-Derived Desert Hedgehog Provides a Neuroprotective Effect Against the Mechanical Stimuli from Compressive Neuropathies Tahseen Mozaffar, James Jung, Derek Frump, Jared Su, Ranjan Gupta 4:35 p.m. I6-2.002 4:40 p.m. I6-2.003 Neuropathy Improvement Following Peripheral Blood Stem Cell Transplantation for POEMS Syndrome. Chafic Karam, Christopher Klein, Angela Dispenzieri, Jayawant Mandrekar, P. James B. Dyck, Anita D’Souza, Michelle Mauermann 4:45 p.m. I6-2.004 Induced Pluripotent Stem Cell Based Models of CMT1A and HNPP Robert Baloh, Irina Epifantseva, Kevin Kim, Shaughn Bell, Sharon Carmona, Sharday Grant, Megan Simpkinson, Matthew Harms, Dhruv Sareen, AKMG Muhammad 4:50 p.m. I6-2.005 Treatment of Experimental CIDP Using Lentivirus Transduced Dendritic Cells Expressing VIP Mehmet Yalvac, William Arnold, Syed-Rehan Hussain, Cilwyn Braganza, K. Reed Clark, Eroboghene Ubogu, Jerry Mendell, Zarife Sahenk Quantification of Sciatic Nerve Pathology in Inherited Neuropathies via Magnetization Transfer MRI Richard Dortch, Lindsey Dethrage, Audra Hamilton, John Gore, Seth Smith, Jun Li Fast, Easy Registration Online · AAN.com/view/AM14 69 Tuesday, April 29 P3 Poster Session III First Authors stand by Posters from 5:00 p.m.–6:30 p.m. 3:00 p.m.–6:30 p.m. Poster Discussion Session: Epilepsy/Clinical Neurophysiology (EEG) Utilizing a guided tour format, topic experts will lead attendees around the ten posters in the poster discussion session and facilitate questions with poster authors during the 90-minute author stand-by time. P3.001 Antibodies to GABAa Receptor Associate with Seizures, Status Epilepticus, and Remove the Receptors from Synapses Mar Petit, Thais Armangue, Xiaoyu Peng, Rebecca Davis, Lindsey McCracken, Rita Balice-Gordon, Francesc Graus, Josep Dalmau P3.002 Is Generic Drug Quality as Good as Brand? Surveillance Testing of Marketed Lamotrigine Batches and Comparison to Brand Soundarya Vaithianathan, Siddarth Raman, Wenlei Jiang, Tricia Ting, Maureen Kane, James Polli P3.003 Characteristics of Traumatic Fractures in Patients with Epilepsy Franziska Herpich, Kenneth Walsh, Neha Vijayvargiya, Wayne Satz, Mercedes Jacobson P3.004 Utility of Selective Posterior Cerebral Artery Amobarbital Testing in Surgical Evaluation for Patients with Temporal Lobe Epilepsy Courtney Schusse, Wil Schultz, Caleb Pearson, Steve Chung P3.005 Utility of CT Perfusion (CTP) Imaging in Seizures: A Retrospective Analysis and Literature Review Aunali Khaku, Vishunmurthy Hedna, Michael Waters P3.006 Where and How Are the Initial Antiepileptic Drugs Administered to Children Who Develop Refractory Status Epilepticus? Results from the Pediatric Status Epilepticus Research Group (pSERG) Ivan Sanchez Fernandez, Nicholas Abend, Satish Agadi, Ravindra Arya, Rajit Basu, Jessica Carpenter, Kevin Chapman, Nathan Dean, William Gaillard, Tracy Glauser, Howard Goodkin, Michele Jackson, Mohamad Mikati, Katrina Peariso, Geetanjali Rathore, Robert Tasker, Alexis Topjian, David Turner, Angus Wilfong, Korwyn Williams, Tobias Loddenkemper P3.007 The Experience of the GENESS International Consortium to Accelerate Discovery of New Epilepsy Genes Antonio Escueta, Maria Alonso, Marco Medina, Reyna Duron, Julia Bailey, Iris Martinez-Juarez, Miyabi Tanaka, Donsheng Bai, Aurelio Jara-Prado, Adriana Ochoa, Jesus Machado-Salas, Thiery Grisar, Kazuhiro Yamakawa, Elza Targas Yacubian, Laura Guilhoto, Jose Serratosa, Christopher Patterson, Joan Spellman, Jenny Wight, Yu-Chen Lin, Sumia Aftab P3.010 Reversible Intraoperative Neurophysiologic Monitoring Changes Associated with Surgical Retraction Leslie Lee, Sungho Cho, Viet Nguyen, Gary Steinberg, Steven Chang, Robert Dodd, Stephen Ryu, Jaime Lopez P3.008 Serum IL6, IL1β And IL1Ra Levels in Patients with Epilepsy Irem Fatma Uludag, Tarik Duksal, Yasar Zorlu, Feriha Ozkaya, Guldal Kirkali P3.009 Review of Aggression in Adults and Adolescents in Perampanel Phase III Epilepsy Clinical Trials Antonia LoPresti, Alan Ettinger, Haichen Yang, Betsy Williams, Sharon Zhou, Randi Fain, Antonio Laurenza NEW! e Poster Session: Neuromuscular and Clinical Neurophysiology (EMG) I The ePoster session will feature a selection of posters to be presented digitally, rather than in the traditional format. Authors will be able to take advantage of the format to highlight compelling visual features such as images and videos. See poster map on page 47 for location. P3.011 Discriminant Value of 18FDG-PET in Amyotrophic Lateral Sclerosis Adriano Chio, Marco Pagani, Andrea Calvo, Cristina Moglia, Flavio Nobili, Piercarlo Fania, Silvia Morbelli, Consuelo Valentini, Antonio Canosa, Angelina Cistaro P3.012 Cytoplasmic Redistribution of Mutant TDP-43 in a BAC Based Mouse Model of Amyotrophic Lateral Sclerosis Kevin Talbot, David Gordon, Ruxandra Mutihac, Javier AlegreAbarrategui, Lucy Farrimond, Ben Davies, Richard Wade-Martins P3.013 Real-time Video Microscopy to Assess Pathologic Leukocyte-Endothelial Cell Interactions at the Human BloodNerve Barrier In Vitro: A Tool to Guide Specific Drug Therapy for Peripheral Neuropathies Eroboghene Ubogu P3.014 Medical Marijuana Utilization and Perceived Therapeutic Value in Patients with ALS Jacob Kaufman, Kelly Almasy, Ashley Boller, Nabila Dahodwala, Lauren Elman, Mary Kelley, Leo McCluskey 70 P3.015 Looking for an Early Diagnosis in a Late Onset Pompe Disease High Risk Population: a LOPED Study Olimpia Musumeci, Giancarlo la Marca, Severo Pagliardini, M Spada, Cesare Danesino, Giacomo Comi, Elena Pegoraro, Giovanni Antonini, Gianni Marrosu, Rocco Liguori, Lucia Morandi, Maurizio Moggio, Roberto Massa, Sabrina Ravaglia, Antonio Di Muzio, Corrado Angelini, Massimiliano Filosto, Paola Tonin, Giuseppe Di Iorio, Serenella Servidei, Gabriele Siciliano, Tiziana Mongini, Antonio Toscano P3.016 Plasmapheresis Enables Robust Micro-Dystrophin Expression Following Gene Transfer in Subjects with Pre-Existing Immunity Louis Chicoine, Chrystal Montgomery, Thomas Preston, Danielle Griffin, William Bremer, K. Reed Clark, Zarife Sahenk, Christopher Walker, Jerry Mendell, Louise Rodino-Klapac P3.018 Quantitative Ultrasound Provides Insight into How Electrical Impedance Myography Measurements Are Impacted by Disease. Irina Shklyar, Tom Geisbush, Aleksandar Mijailovic, Amy Pasternak, Nicole Visyak, Heather Szelag, Jim Wu, Craig Zaidman, Basil Darras, Seward Rutkove P3.019 Anti-Growth Factor Receptor 3 Antibodies Identify a Sub-Group of Sensory Neuropathy Patients JeanChristophe Antoine, Boutahar Nadia, Véronique Rogemond, Jerome Honnorat, Jean-Phillippe Camdessanche P3.017 Characterization of B-cell Subsets in MuSK Myasthenia Gravis Jeff Guptill, John Yi, Donald Sanders, Amanda Guidon, Sara Sparks, Robyn Osborne, Janice Massey, Vern Juel, Lisa HobsonWebb, Kent Weinhold 2O14 Scientific Abstract Listing and Annual Meeting Information P3.020 Bone Mineral Content as Measure of Bone Health in Ambulatory Boys with Duchenne Muscular Dystrophy Cuixia Tian, Meilan Rutter, Lindsey Hornung, Jane Khoury, Lauren Miller, Jean Bange, Brenda Wong Poster Session III P3.021 A randomized Controlled Trial Comparing Botulinum Toxin Type A Xeomin® and Dysport® for Treatment of Primary Axillary Hyperhidrosis Francesca Pastorelli, Roberto Michelucci, Rosaria Plasmati P3.022 Multiplex Testing of AntiNeural Autoantibodies Lars Komorowski, Kristin Rentzsch, Sandra Saschenbrecker, Bianca Teegen, Christian Probst, Winfried Stoecker P3.023 Brain Lactate in Patients with Autosomal Dominant Adult-Onset Leukodystrophy (ADLD): a 1H-MR Spectroscopy Study. Stefano Zanigni, Caterina Tonon, Claudia Testa, Rossana Terlizzi, Laura Gramegna, Claudio Bianchini, Pietro Guaraldi, Giovanna Calandra Buonaura, Pietro Cortelli, Raffaele Lodi P3.035 Neurological Complications After Kidney Transplantation Kateryna Kurako, Nancy Rosales, Ramon Lugo P3.050 P3.036 P3.051 Relationship Between Bone Mass and Muscle Weakness in Chronic Neurological Diseases Maria Gutierrez, Gabriel Eduardo Rodriguez, Domingo Garcea, Raul Rey, Sandra Lepera, Ercolano Monica, Drnovsek Monica, Kerzberg Eduardo, SIlva Berenice P3.037 Functional Brain Dimorphism in Psychopath Offenders Evidenced by QEEG Analysis Ana Calzada-Reyes, Alfredo Alvarez Amador, Lídice Galán-García P3.038 The Vulpian-Bernhardt Syndrome in the Clinical Spectrum of Amyotrophical Lateral Sclerosis: A Case Report and Literature Review. Armando Jordan, Marie-Catherine Boll P3.039 P3.024 Trigeminal Neuralgia to a Tibial tumour; Four Degrees of Separation Laura Williams, Ronan Killeen, Thomas Crotty, Michael Hutchinson, Christopher McGuigan P3.025 P3.040 Prognosis of Treated Neurosarcoidosis Allen Aksamit, Blake Fechtel, Tyler VanDyck, Andrew Tseng Spinal Cord Compression Associated with a Systemic IgG4 Disease Mohamad Ezzeldin, Ahmad Shawagfeh, Vicki Schnadig, Robert Smith, Xiang Fang P3.026 Conversion of New Active MRI Lesions at 6 Months to T1 Hypointense ‘Black Holes’ at 12 Months in RRMS Subjects from the GALA Study Robert Zivadinov, Joshua Steinerman, Volker Knappertz, Hadas Barkay, Omar Khan P3.027 Olfactory Dysfunction in Chagas’ Disease Fidias Leon-Sarmiento, Edgardo A Bayona, Carlos V Rizzo-Sierra, Alicia Garavito, Maria Fernanda Campos, Richard Doty P3.028 Multiple Sclerosis Comorbidity Study Robert Simpson P3.029 Paclitaxel Affects Axonal Mitochondria in a Murine Model of Chemotherapy-Induced Peripheral Neuropathy Ilja Bobylev, Abhijeet Joshi, Christian Ritter, Ahmet Hoke, Helmar Lehmann P3.030 Using Rapid Reaching Tasks to Reveal the Underlying Mechanisms of Decision Making in Humans Maria Khami P3.031 Acute Focal Dystonia Heralding the Diagnosis of Type 2 Diabetes Mellitus Alok Sachdeva, Deepak Gulati, Michael Devereaux P3.032 Primary Angiitis of the Central Nervous System presented with Tumor-like lesion: A Case Report Yasaman Kianirad, Shyam Prabhakaran P3.033 Utility of Computed Tomogram of Head for Patients with Altered Mental Status Sanjeev Sivakumar, Zakhar Serkin, Camelia Arsene, Ramesh Madhavan, Navid Seraji-Bozorgzad P3.034 A Case of Adult Langerhans Cell Histiocytosis Presenting as Isolated Central Diabetes Insipidus: A Powerful Tool to Detect the Hypophyseal and Extrahypophyseal Involvement Junko Maeda, Junwa Kunimatsu, Sohtaro Mine, Kaoru Aishima, Atsuto Yoshizawa The European Union Is worth saving Anne Hoeritzauer, Gavin McDonnell, Marjo Van Der Knaap Neural Repair and Neurorehabilitation: Clinical P3.041 Hyperbaric Oxygen Therapy Versus Antiepileptic Drugs in the Control of Late Post Traumatic Non Convulsive Epilepsy Refractory to Phenytoin Sherif Abd Elmonem, Soliman Tahon, Ann Abd Elkader, Akram Fayed P3.042 A Compilation of Spasticity Studies Evaluating Onabotulinumtoxin A Payal Patel, Aubrey Manack P3.043 Treating Neglect by Body Movements: A Case Report and Follow-up Study Amit Chaudhari, Kara Pigott, Peii Chen, A. Barrett P3.044 A Preliminary Examination of Psychological and Neuropsychological Outcomes in Patients with Mild Traumatic Brain Injury Shannon McNally, Katherine Lopez, Sarah Levy, John Dsurney, Leighton Chan P3.045 Functional Motor Recovery In Stroke Survivors—Determinants in a Stroke Unit in Sub-Saharan Africa. Frank Imarhiagbe P3.046 Cognitive Training Program for Memory/Executive Reasoning Deficits in Adults with Traumatic Brain Injury Barbara Fisher, Danielle Garges P3.047 Alterations in Muscle Coordination Following Robot-Assisted Gait Training in Hemiparetic Stroke: A Case Series Adam Thrasher, Stanley Fisher P3.048 Comparison of Headache in OEF/OIF Veterans with Traumatic Brain Injury (TBI) against Controls Matched for Age, Sex, Race and Deployment Time James Couch, Kenneth Stewart P3.049 Higher Coated-Platelets in Patients with Mild Traumatic Brain Injury Correlate with Lower Cognitive Screening Performance Calin Prodan, Andrea Vincent, George Dale Patient Registry of Outcomes in Spasticity (PROS) Care World Alberto Esquenazi, Nathaniel Mayer, Stella Lee Fatigue and Functional MRI in Multiple Sclerosis: A Quantitative Coordinate-based Activation Likelihood Estimation Meta-analysis Radu Tanasescu, Cris Constantinescu, Ali Manouchehrinia, Dorothee Auer, Christopher Tench P3.052 White Matter Disease Ratings in Right Hemisphere Stroke Annapoorna Bhat, Marianne Kim, Anne Foundas, Peii Chen P3.053 The Effects of Salsa Dance on Gait and Balance in Multiple Sclerosis Rosalind Mandelbaum, Elizabeth Triche, Susan Fasoli, Albert Lo P3.054 Prospective Assessment of Falls Among People with Multiple Sclerosis and Healthy Matched Controls Rajarshi Mazumder, Charles Murchison, Michelle Cameron P3.055 Brain-Computer Interface Driven Functional Electrical Stimulation System for Overground Walking: A Case Report Christine King, Colin McCrimmon, Po Wang, Cathy Chou, Zoran Nenadic, An Hong Do P3.056 Improvement of Gait Following Walking Based Long-term aerobic Endurance Exercise In Mildly Disabled MS Patients Stephan Schmidt, Marc Wonneberger P3.057 The Potential Diagnostic Approach to Characterize Peripheral Nerve Injury Using 4-AP Kuang-Ching Tseng, John Elfar P3.058 Action Observation Therapy Modifies Structural Brain Plasticity in Healthy Adult Individuals Paolo Preziosa, Maria Rocca, Roberto Gatti, Melissa Petrolini, Roberta Messina, Gabriele Salini, Silvia Fumagalli, Andrea Falini, Giancarlo Comi, Massimo Filippi P3.059 VR-based Training Using Wii Fit Improve Obstacle Crossing Performance and Dynamic Balance in Patients with Parkinson Disease Yingyi Liao, Yea-Ru Yang, Ray-Yau Wang Movement Disorders: Clinical Features of Parkinson’s Disease P3.060 Parkinson’s Disease Among Mexican Americans Aged 74 Years and Older in the Southwestern United States Nicte Mejia, Sunshine Rote, NaiWei Chen, Kyriakos Markides, Soham Al Snih P3.061 Recurrent Falls in Parkinson Disease (PD) Abraham Lieberman, Rohit Dhall, Aman Deep, Narayanan Krishnamurthi, Naomi Salins, Di Pan P3.062 Auditory Processing Abilities of Parkinson Disease Patients Robert Folmer, Jay Vachhani P3.063 Levodopa and Posture— Quantification of Trunk Performance in Parkinson’s Disease Felix Benninger, Alexander Khlebtovsky, Yaniv Roditi, Eldad Melamed, Ruth Djaldetti P3.064 Tactile Cueing Improves Motor Performance and Motor-Cognitive Integration in Parkinson’s Disease Vladimir Ivkovic, Stanley Fisher, William Paloski P3.065 Carotid Artery Thickening and Neurocirculatory Abnormalities in De Novo Parkinson Disease Joong-Seok Kim, Yoon-Sang Oh, Kwang-Soo Lee, In-Uk Song, Yeong-In Kim, Dong-Won Yang, Ja-Seong Koo, David Goldstein P3.066 Effect of Parkinson Disease Age of Onset on Family History Nicholas Hac, Madaline Harrison, G. Wooten, Matthew Barrett P3.067 Discordance Between Medication Apps and Needs of Patients with Parkinson’s Disease Anupama Divakaruni, Melissa Armstrong, Ann GruberBaldini, Lisa Shulman P3.068 Neuroprotection by Sex Steroid Hormones in Parkinson’s Disease Kara Smith, Nabila Dahodwala Tuesday April 29 General Neurology II P3.069 Gender and Dopaminergic Medication Treatment in Early Parkinson Disease Chizoba Umeh, Adriana Pérez, Erika Augustine, Rohit Dhall, Richard Dewey, Zoltan Mari, David Simon, Anne Marie Wills, Chadwick Christine, Jay Schneider, Oksana Suchowersky Movement Disorders: Assessing Parkinson’s Disease P3.070 Motion Sensor Dyskinesia Assessment During Activities of Daily Living Christopher Pulliam, Michelle Burack, Joseph Giuffrida, Thomas Mera P3.071 Walking Capacity (WalkCap) Measured by Six-Minute Walk (6MW) Does Not Demonstrate Fatigue in Patients with Amyotrophic Lateral Sclerosis (ALS), Multiple Sclerosis (MS),and Parkinson Disease (PD) Mohammed Sanjak, Laura Morgan, Ashely Simpson, Scott Holsten, Mark Hirsch, Danielle Englert, Sanjay Iyer, Jill Conway, Michael Kaufman, Elena Bravver, Urvi Desai, Priscilla Russo, Benjamin Brooks P3.072 Quantitative Motor Assessment in Parkinson’s Disease (PD) with the MovAlyzeR® Digital Writing Tablet Alexander Pantelyat, Rebecca Freedman, Stephanie Pawlowski, Adhithi Kesari, Jayne Wilkinson, John Duda, James Morley P3.073 Dynamic Fall-risk Predictors in Parkinson’s Disease Ashutosh Mani, Kari Dunning, Travis Larsh, Cyndy Cox, Amit Shukla, Amit Bhattacharya, Fredy Revilla P3.074 Objective Assessment of Electro-acupuncture Benefit for Improving Balance and Gait in Patients with Parkinson’s Disease Hong Lei, Nima Toosizadeh, Michael Schwenk, Scott Sherman, Stephen Karp, Saman Parvaneh, Esther Esternberg, Bijan Najafi P3.075 Low Health Literacy: An Under-Recognized Obstacle in Parkinson’s Disease Jori Fleisher, James Minger, Whitney Fitts, Nabila Dahodwala Fast, Easy Registration Online · AAN.com/view/AM14 71 Tuesday, April 29 P3.076 Avoiding Ventricular Transgression During DBS Surgery: A Quality Improvement Intervention Meagan Bailey, Roy Strowd, Jessica Tate, Ihtsham Haq, Stephen Tatter, Adrian Laxton, Mustafa Siddiqui P3.077 Sex Differences in Clinical Features of Early, Treated Parkinson Disease Erika Augustine, Rohit Dhall, Adriana Perez, Chizoba Umeh, Oksana Suchowersky P3.089 Can Neuronal Voltage-gated Potassium Channels be Associated with Parkinsonism? Hardik Doshi, Edwin George, Natalya Shneyder Cerebrovascular Disease and Interventional Neurology: Clinical Management P3.090 Is There a Relationship Between Social Phobia and Parkinson’s Disease? Christina Saldivar, Guillermo Moguel-Cobos Factors Associated with 30-day Readmission Rate Among Stroke Patients from 2009-2012 at Two Tertiary Level Hospitals in Metro Portland Area Amit Kansara, Tamela Stuchiner, Elizabeth Baraban, Archit Bhatt P3.079 Pronounced Task Specific Writing Tremor in Parkinson’s Disease Katelyn Smith, Aws Alawi, Joanna Ramiro, Pratap Chand P3.091 Movement Disorders: Other Parkinsonian Disorders P3.092 P3.078 P3.080 Olfactory Impairment and Other Features of Parkinson Disease That Predict Persistent Drug-Induced Parkinsonism James Morley, Stephanie Pawlowski, Alexander Pantelyat, Adhithi Kesari, Ivy Maina, John Duda P3.081 Long-term Levodopa Use in Normal Substantia Nigra Cases Michele Rajput, Ali Rajput, Christopher Robinson, Alexander Rajput P3.082 The Entity of Parkinsonism and Associated Lipomatosis Maria Stamelou, Una-Marie Sheerin, Nicholas, W Wood, Kailash Bhatia P3.083 REM Sleep and Motor Symptoms in Parkinson’s Disease: A Cross Sectional Analysis Abhimanyu Mahajan, Charlene Gamaldo, Rachel Marie Salas, Gregory Pontone, Chizoba Umeh, Liana Rosenthal, Arita McCoy, Zoltan Mari P3.084 Mild Parkinsonian Signs Are a Risk Factor for Falls Nabila Dahodwala, Chinwe Nwadiogbu, Whitney Fitts, Helen Partridge, Jason Karlawish P3.085 A Family with Corticobasal Degeneration, Parkinson’s Disease, Amyotrophic Lateral Sclerosis, and Dementia Shinsuke Fujioka, Monica Sanchez Contreras, Audrey Strongosky, Pawel Tacik, Bradley Boeve, A Stoessl, Matthew Baker, Rosa Rademakers, Dennis Dickson, Zbigniew Wszolek P3.086 Three New Families with Perry Syndrome from Distinct Parts of the World—Novel Mutation and Successful Treatment Attempt of Respiratory Insufficiency Pawel Tacik, Shinsuke Fujioka, Owen Ross, Wolfdieter Springer, Fabienne Fiesel, Felipe Pretelt, Camilo Castañeda Cardona, Alexa Kidd, Michael Hlavac, Anthony Raizis, Michael Okun, Zbigniew Wszolek P3.087 Vascular Parkinsonism in a Tertiary Care Stroke Prevention Clinic: Prevalence and Development of a New Screening Strategy Herbert Manosalva Alzate, Thomas Jeerakathil, Maher Saqqur, Richard Camicioli, Oksana Suchowersky P3.088WITHDRAWN 72 Etiologies of Neurologic Deterioration in the First 30 Days Following Ischemic Stroke Iftekhar Ahmed, Kirstin Hirni, Sakher Albadarin, Neeta Duggal Vertigo and Dizziness in Anterior Circulation Cerebrovascular Disease: A Systematic Review Yun Zhou, Seung-Han Lee, Georgios Mantokoudis, Ali Saber Tehrani, Sarah Ying, Kevin Kerber, Yu-Hsiang Hsieh, Karen Robinson, Daniel Hanley, David Zee, David Newman-Toker P3.093 Risk Factors for Ischemic Stroke Mortality Claudia Alonzo, Maria Zurru, Laura Brescacin, Ariel Luzzi, Luis Camera, Gabriel Waisman, Edgardo Cristiano P3.094 Relation of Serial Hemodynamic and Autonomic changes in Acute Ischemic Stroke to Stroke Type, Location and Outcome. Arunodaya Gujjar, Deepali Jaju, Jacob Poovathur, Mohan Dikshit, Abdullah Al-Asmi P3.095 Cerebral Infarction Occurrence in Settings of Acute Traumatic Injury. Analysis of a Prospective Multicenter Trial Tanya Mohindroo, Malik Adil, Sheharyar Minhas, Adnan Qureshi P3.096 Nonmydriatic Ocular Fundus Photography Among Patients with Focal Neurologic Deficits in an Emergency Department (ED) Beau Bruce, Laurel Vuong, Praneetha Thulasi, Valerie Biousse, David Wright, Nancy Newman P3.097 Peripheral Artery Disease in Patients with Ischemic Stroke: A Cross Sectional Observational Study Attiya Rahman, Syed Akhtar, Qaiser Jamal P3.098 Factors Affecting the Acceptance of Decompressive Craniectomy in Patients with a Malignant Middle Cerebral Artery Infarction Seungnam Son, Jiho Hong, Dae Seob Choi, Min Kyun Oh, Soo-Kyoung Kim, Heeyoung Kang, Ki-Jong Park, Nack-Cheon Choi, Oh-Young Kwon, Byeong Hoon Lim P3.099 NIH Stroke Scale Change Correlates with Length of Stay in Intensive Care Unit Stroke Patients Prashanth Krishnamohan, Qian Fan, Michael Dobbs 3:00 p.m.–6:30 p.m. Cerebrovascular Disease and Interventional Neurology: tPA P3.100 Stroke Outcomes and Usage of IV Alteplase during Pregnancy in the Nationwide Inpatient Sample 20052010 Sarah Song, Bichun Ouyang, Taylor Knopf, James Conners, Shawna Cutting, Vivien Lee, Laurel Smit, Elena Kuklina P3.101 Baseline Body Temperature: Paradoxical Association with Severity and Non-Modification of Treatment Benefit in the NINDS TPA Stroke Trials Seo Hyun Kim, Jeffrey Saver P3.102 Collateral Circulation Recruitment and Failure in Acute Ischemic Stroke Patients Treated with IV rTPA. Leonard Yeo, Prakash Paliwal, Hock Luen Teoh, Chee Seong Seet, Eric Ting, Bernard Chan, Rahul Rathakrishnan, Jonathan Ong, Vijay Sharma P3.103 Direct and Indirect Cost Burden of Stroke Mimics Post Intravenous Tissue Plasminogen Activator (IV-tPA): A Single Center Study Nitin Goyal, Shailesh Male, Ameer Al Wafai, Ramin Zand P3.104 Is the Use of r-tPA in Mild Stroke Patients Cost-Effective? Gregory Guzauskas, Er Chen, Pooja Khatri, Peter Sandercock, Darren Tayama, David Veenstra P3.112 Vessel Wall Characteristics of Bilateral and Unilateral Moyamoya Syndrome using High Resolution Magnetic Resonance Imaging Russell Cerejo, Ferdinand Hui, Stephen Jones, Emmanuel Obusez, Ken Uchino P3.113 Thyrotoxic Graves’ Disease and Moyamoya-like Vasculopathy in Latino Patients: A Case Series Nirav Shah, Gillian Gordon-Perue, Gustavo Ortiz, Alejandro Forteza P3.114 Cephalometric Features of Moyamoya Disease: A Case Control Study Waqas Gilani, Sarwat Gilani, Malik Adil, Adnan Qureshi P3.115 The Association and Treatment of Distal PICA Aneurysms with Posterior Fossa Arteriovenous Malformation: A Case Series David Case, Takamasa Higashimori, Joshua Seinfeld P3.116 Obesity in a Young Adult Stroke Population Jina Youn, Joni Clark P3.117 Erythropoetin associated Posterior Reversible Encephalopathy Syndrome Rajanandini Muralidharan, Madhurima Anne, Elissa Fory, Wirkowski Elizabeth P3.118 P3.105 Reversible Cerebral Vasoconstriction Syndrome in Association with Fingolimod Use Scott Belliston, Nancy Hammond, Jayashree Sundararajan P3.106 Cerebrovascular Disease and Interventional Neurology: Primary and Comprehensive Stroke Centers Effect Of Education to Hospital Staff on Efficiency of Acute Stroke Thrombolysis Dheeraj Khurana, Anish Hirachan, Ashish Bhalla, Sudesh Prabhakaran Etiologies of Neurologic Deterioration Following Intravenous Thrombolysis for Acute Ischemic Stroke. Alex Perchuk P3.107 HAT Score External Validity: A Predictor of Hemorrhagic Transformation After Intravenous Thrombolysis Elizeu Neto P3.108 Determine the Gender Differences in Outcome Following Thrombolysis in Ischemic Stroke. Zabeend Mahuwala, Kaustubh Limaye, Anand Patel, Archana Hinduja, Rajan Patel P3.109 HAT Score Outperforms 7 Other Hemorrhagic Transformation Scores in Ischemic Stroke Patients Treated with Thrombolysis David Asuzu, Karin Nystrom, Janet Halliday, Charles Wira, David Greer, Joseph Schindler, Kevin Sheth Cerebrovascular Disease and Interventional Neurology: Large Vessel Nonatherosclerotic Arteriopathies P3.119 Automated Datamining to Create Stroke Database and Concurrent ‘Managed Alerts’ for Comprehensive Stroke Center Metrics Ramesh Madhavan, Fnu Abhishek, Connie Parliament, Megan Dietrich, Navid Seraji-Bozorgzad, Pratik Bhattacharya P3.120 90 Day Outcomes in Stroke/ Transient Ischemic Attack Patients Receiving Initial or Follow-up Care in a Comprehensive Outpatient Stroke Center Vernice Bates, Erica Westphal, Michelle Rainka, Francis Gengo P3.121 The Impact of a Stroke Prevention Clinic After Discharge for TIA/ Stroke: University Hospitals Case Medical Center Comprehensive Stroke Center Experience Tanzila Shams, Kathleen Vickers, Richard Jung, Cathy Sila P3.122 Quantifying Cerebral Collaterals in Carotid Artery Dissection May Help Stratify Stroke Risk. Andrew Southerland, John Gaughen, Jr., Timothy McMurry, Max Wintermark, Jennifer Majersik, Bradford Worrall Rates of In-hospital Adverse Events and Discharge Outcomes Among Ischemic Stroke Patients Admitted to Joint Commission Primary Stroke Centers in United States Saqib Chaudry, Taqi Zafar, Mohammad Afzal, Mohammad Umair, Mohammad Owais, Gautam Sachdeva, Malik Adil, Vishal Jani, Syed Hussain, Adnan Qureshi P3.111 P3.123 P3.110 Ischemic Stroke and Cervical Artery Dissection. Risk Factors and Functional Outcome in a Single Tertiary Care Hospital: The Clinica Alemana Stroke Registry (RECCA), 1997-2003 Violeta Diaz, Maria Vicuña, Jose Fernandez, Marcela Valenzuela, Pablo Lavados 2O14 Scientific Abstract Listing and Annual Meeting Information Characteristics of Certified Stroke Center Programs Led by Vascular Neurologists Lucas Ramirez, Aaron Krug, Joshua Perese, Gregory Gasparian, Suzie Kazaryan, Nerses Sanossian Poster Session III P3.124 Failed Bedside Dysphagia Screen Predicts Pneumonia Treatment in Acute Stroke: A Resident Quality Initiative Project in a JC-Certified Primary Stroke Center Mohamed-Ali Babi, Mark Gorman, Christopher Commichau, Sharon Kenney, Lakshmi Boyle, Mary Comeau, Steve Hulsey P3.125 Hydration Practices for the Acute Stroke Patient in an Academic, Certified Stroke Center Mona Bahouth, Argye Hillis, Rebecca Gottesman P3.126 Leadership of Certified Stroke Center Programs Lucas Ramirez, Aaron Krug, Joshua Perese, Gregory Gasparian, Suzie Kazaryan, Nerses Sanossian P3.127 Compare the Weekend Effect in Telestroke and Primary Stroke Center. Zabeend Mahuwala, Anand Patel, Kaustubh Limaye, Archana Hinduja, Nicolas Bianchi, Rajan Patel P3.128 Differences in Payment for Inpatient Transient Ischemic Attack Care Between Stroke Center and Non-StrokeCenter Hospitals Shuhan He, Sebina Bulic, Suzie Kazaryan, Steven Cen, May Kim, May Kim, William Mack, Nerses Sanossian MS and CNS Inflammatory Disease: Tools for Clinical Assessment and Therapeutic Response P3.129 Multiple Sclerosis Performance Test: A Reliable, Sensitive, and Meaningful Tool to Quantify MS Related Disability Richard Rudick, Deborah Miller, Francois Bethoux, Stephen Rao, JarChi Lee, Darlene Stough, Christine Reece, David Schindler, Jay Alberts P3.130 Multiple Sclerosis Documentation System MSDS3D— Innovative Management of Patients with Multiple Sclerosis Judith Eisele, Raimar Kern, Suhrbier Alexander, Lars Großmann, Thorsten Schultheiss, Tjalf Ziemssen P3.131 Psychometric Properties of the MSIS-29 and Factors Predicting Score Changes in Clinical Trials: An Analysis of Data from the SELECT Study Glenn Phillips, Jane Castelli-Haley, Shien Guo, Irina Proskorovsky, Jacob Elkins P3.132 The Multiple Sclerosis Performance Test: An Innovative Approach to Measuring MS-Related Manual Dexterity Impairment Francois Bethoux, Richard Rudick, Deborah Miller, Stephen Rao, Jar-Chi Lee, Darlene Stough, Christine Reece, David Schindler, Jay Alberts P3.133 Multiple Sclerosis Decision Model (MSDM): A Multifactorial Model to Monitor Treatment Response and Disease Course in Relapsing Remitting Multiple Sclerosis Martin Stangel, Iris Katharina Penner, Boris Kallmann, Carsten Lukas, Bernd Kieseier, Ralf Gold P3.134 Plasticity-Based Cognitive Remediation in Multiple Sclerosis (MS) Leigh Charvet, Maria Amella, William Scherl, Dana Serafin, Emily Taub, Patricia Melville, Lauren Krupp P3.135 Kinect-based Gait Analysis in Patients with Multiple Sclerosis Janina Behrens, Karen Otte, Sebastian MansowModel, Alexander Brandt, Friedemann Paul P3.136 The Turkish Multiple Sclerosis Walking Scale (MSWS-12v2T): Is it the Same Measure as the Original Version? Hussein Dib, Yusuf Tamam, Murat Terzi, Jeremy Hobart P3.137 Patient Preferences in the Choice of Disease Modifying Drugs for Multiple Sclerosis Arnfin Bergmann, Michael Lang, Christian Ludger Bischoff, Petra Schicklmaier, Hans-Dieter Nolting, Guido Schiffhorst, Julian Rellecke, Erika Kunz P3.138 Identifying Individuals with Multiple Sclerosis in an Electronic Medical Record Kristen Krysko, Noah Ivers, Jacqueline Young, Paul O’Connor, Karen Tu P3.139 Assessment of Disability in Multiple Sclerosis Using the Kinect-Camera System: A Proof-of-Concept Study Marcus D Souza, Christian Kamm, Jessica Burggraaff, Prejaas Tewarie, Ben Glocker, Jonas Dorn, Thomas Vogel, Cecily Morrison, Abigail Sellen, Matthias Machacek, Peter Chin, Bernard Uitdehaag, Antonio Criminisi, Frank Dahlke, Chris Polman, Ludwig Kappos P3.140 Multiple Sclerosis Performance Test: Patients Express High Satisfaction with the Application Deborah Miller, Jar-Chi Lee, Francois Bethoux, Stephen Rao, Jay Alberts, David Schindler, Darlene Stough, Christine Reece, Richard Rudick P3.141 Cultural Adaptation and Evaluation of the Psychometric Properties of the MSTCQ© “MS Treatment Concerns Questionnaire” Spanish Language Version Elvira Munteis, Navarro Guillermo, Jose Meca La Llana, Asuncion Maestre Martinez, Ángel Sempere, Julia Gracia, Antonio Pato P3.142 Validating an Electronic Method for Prospective Fall Counting in People with MS Ashley Downs, Charles Murchison, Rajarshi Mazumder, Michelle Cameron P3.143 The Role of G-tubes In Decreasing UTIs in a Cohort of Patients with Advanced MS Kathleen Healey, Neil Jouvenat, Mac McLaughlin, Lyndsay HartWann, Kristine Rutledge, Rana Zabad P3.144 Graded Response Analysis of the MSIS-29 in Clinical Trial Participants with Relapse-Remitting Multiple Sclerosis Glenn Phillips, Elizabeth Danzie, Kathy Wyrwich P3.145 Comparing Disability of Multiple Sclerosis Cohort in a Tertiary Clinic and Volunteer North American Research Committee on Multiple Sclerosis Registry Using Patient-Derived Multiple Sclerosis Severity Score Ariel Antezana, Joseph Herbert, Eric Chamot, Gary Cutter, Amber Salter, Ilya Kister P3.146 Relationship Between Immunological Markers and Short-term Brain Volume Changes in Patients with Relapsing-Remitting Multiple Sclerosis Receiving Interferon Beta-1a Michael Dwyer, Robert Zivadinov, Yazhong Tao, Xin Zhang, Cheryl Kennedy, Niels Bergsland, Deepa Ramasamy, Jackie Durfee, David Hojnacki, Bianca Weinstock-Guttman, Brooke Hayward, Fernando Dangond, Silva Markovic-Plese P3.153 P3.147 P3.154 Correlations Between Immunological Biomarkers and Conventional and Advanced MRI Measures Following Interferon Beta-1a Treatment for Relapsing-Remitting Multiple Sclerosis Silva Markovic Plese, Yazhong Tao, Xin Zhang, Michael Dwyer, Cheryl Kennedy, Niels Bergsland, Deepa Ramasamy, Jacqueline Durfee, David Hojnacki, Bianca Weinstock-Guttman, Brooke Hayward, Fernando Dangond, Robert Zivadinov P3.148 Burden of Multiple Sclerosis on Caregivers and Patients and Degree of Satisfaction with Current Treatment: The MS-Feeling Study José Meca, Maria Del Mar Mendibe Bilbao MS and CNS Inflammatory Disease: Clinical Trials Outcomes P3.149 Clinical Trial of Helminthinduced Immunomodulatory Therapy (HINT 2) in Relapsing-Remitting Multiple Sclerosis John Fleming, Leslie Hartman, Jane Maksimovic, Sara Nace, Christopher Luzzio, Monica Koehn, Anna Ritter, Todd Risa, Benjamin Lawler, Andrea Maser, Pamela Mundt, Loren Rolak, Thomas Cook, Aaron Field, Zsuzsanna Fabry P3.150 Safety and Efficacy of Teriflunomide for up to 9 Years in Relapsing Forms of Multiple Sclerosis: Update of the TEMSO Extension Trial Mark Freedman, Jerry Wolinsky, Giancarlo Comi, Ludwig Kappos, Tomas Olsson, Aaron Miller, Myriam Benamor, Deborah Dukovic, Jinjun Liang, Philippe Truffinet, Paul O’Connor P3.151 Safety and Efficacy of Siponimod (BAF312) in Patients with Relapsing-Remitting Multiple Sclerosis: Results from Dose-blinded Extension Phase of BOLD Study Ludwig Kappos, Olaf Stuve, Hans Hartung, Mark Freedman, David Li, Bernhard Hemmer, Peter Rieckmann, Xavier Montalban, Tjalf Ziemssen, Brian Hunter, Sophie Arnould, Erik Wallstrom, Krzysztof Selmaj P3.152 24-month Interim Results of PANGAEA: A 5-year Registry Study Evaluating Long-term Safety, Efficacy and Pharmacoeconomic Data of German Multiple Sclerosis Patients on Fingolimod Therapy Tjalf Ziemssen, Maria DiazLorente, Alexandra Fuchs, Christian Cornelissen A Multinational, Multicenter, Randomized, Double-Blind, ParallelGroup, Active-Control Study to Evaluate the Efficacy, Safety, and Tolerability of Oral Laquinimod 0.6mg or 1.2mg QD versus IFNβ-1a in Patients with Relapsing Remitting Multiple Sclerosis Hans-Peter Hartung, Frederik Barkhof, Oscar Fernandez, Jeremy Hobart, Gavin Giovannoni, Maria Pia Sormani, Yuval Dadon, Nissim Sasson, Volker Knappertz Efficacy and Safety of Anti LINGO-1 for the Treatment of Relapsing Forms of Multiple Sclerosis: Design of the Phase 2 SYNERGY Trial Diego Cadavid, Glenn Phillips, Tuan Dong-Si, Jonathan Tran, Lei Xu P3.155 Pilot Trial of Recombinant Human Growth Hormone for Remyelination in Multiple Sclerosis: Current Status and Preliminary Safety Analysis Muriel Stoppe, Barbara Ettrich, Eva Thomae, Juergen Kratzsch, Karl-Titus Hoffmann, Dirk Hasenclever, Florian Then Bergh P3.156 Fingolimod Efficacy and Safety in an African-American Patient Subgroup from FREEDOMS II Patricia Coyle, Bruce Cree, Philippe Cabre, Matilde Inglese, Jai Perumal, Xiangyi Meng, Peter Chin, Ron Hashmonay, Omar Khan P3.157 Predicting Confirmed Disability Progression in MS: Importance of Early on-Treatment MRI Changes on Modeling the CombiRx Trial Database Florent Lalys, Leorah Freeman, John Lincoln, Flavia Nelson, Ponnada Narayana, Stacey Cofield, Tarah Gustafson, Gary Cutter, Fred Lublin, Jerry Wolinsky P3.158 Alemtuzumab Improves Visual Outcomes Versus Subcutaneous Interferon Beta-1a in Patients with Active RelapsingRemitting Multiple Sclerosis (RRMS) Who Relapsed on Prior Therapy: Analysis from the CARE-MS II Study Jennifer Graves, Laura Balcer, Jeffrey Palmer, David Margolin, Steven Galetta P3.159 Effect of Delayed-Release Dimethyl Fumarate on Freedom from Measured Clinical and Neuroradiological Disease Activity in Relapsing-Remitting Multiple Sclerosis (RRMS) Patients: An Integrated Analysis of DEFINE and CONFIRM Eva Havrdova, Ralf Gold, Robert Fox, Ludwig Kappos, J. Theodore Phillips, Annie Zhang, Nuwan Kurukulasuriya, Sarah Sheikh, Vissia Viglietta, Gavin Giovannoni P3.160 4-Year Follow-up of DelayedRelease Dimethyl Fumarate Treatment in Relapsing-Remitting Multiple Sclerosis (RRMS): Integrated Magnetic Resonance Imaging (MRI) Outcomes from DEFINE, CONFIRM, and the ENDORSE Extension Study Douglas Arnold, Robert Fox, Ralf Gold, Eva Havrdova, Ludwig Kappos, Tarek Yousry, Ray Zhang, Minhua Yang, Vissia Viglietta, Sarah Sheikh, David Miller Fast, Easy Registration Online · AAN.com/view/AM14 73 Tuesday April 29 First Authors stand by Posters from 5:00 p.m.–6:30 p.m. Tuesday, April 29 P3.161 Effect of Ceralifimod (ONO-4641), a Sphingosine-1-Phosphate Receptor-1 and -5 Agonist, on Magnetic Resonance Imaging Outcomes in Patients with Multiple Sclerosis: Interim Results from the Extension of the DreaMS Study Amit Bar-Or, Frauke Zipp, Matthew Scaramozza, Timothy Vollmer, Bryan Due, Karthinathan Thangavelu, Tanya Fischer, Krzysztof Selmaj P3.162 Effect of Delayed-Release Dimethyl Fumarate on Health-Related Quality of Life in Relapsing-Remitting Multiple Sclerosis (RRMS) Patients According to Prior Therapy: An Integrated Analysis of the Phase 3 DEFINE and CONFIRM Studies Ludwig Kappos, Robert Fox, Ralf Gold, Mariko Kita, J. Theodore Phillips, Sujata Sarda, Lixian Zhong, Timothy Niecko, Nuwan Kurukulasuriya, Gavin Giovannoni P3.163 Disability Progression in Multiple Sclerosis Patients Treated with Natalizumab in the Long-term STRATA Study Andrew Goodman, Ludwig Kappos, Fred Lublin, Shibeshih Belachew, Madalina Chirieac, Fiona Forrestal, Petra Duda P3.164 Patients Free of Clinical MS Activity in TEMSO and TOWER: Pooled Analyses of Two Phase 3 Placebo-Controlled Trials Tomas Olsson, Giancarlo Comi, Mark Freedman, Aaron Miller, Jerry Wolinsky, Philippe Truffinet, Steven Cavalier, Deborah Dukovic, Paul O’Connor, Ludwig Kappos P3.165 Sustained Improvement in Disability Outcomes with Alemtuzumab in Active Relapsing-Remitting Multiple Sclerosis Patients Who Participated in CARE-MS II: Three-year Follow-up Gavin Giovannoni, David Margolin, Jeffrey Palmer, Joseph Herbert P3.166 Categorical Change in T2 Lesion Volume and Clinical Outcomes in the Phase III FREEDOMS and its Extension Study, Evaluating Fingolimod in Patients with Relapsing-Remitting Multiple Sclerosis Douglas Jeffery, Elisabetta Verdun Di Cantogno, Daniela Meier, Michael Meinel, Peter Chin, William Camu P3.167 A Stabilized Release Neuropeptide exhibits efficacy in a Phase II Double Blind Placebo Controlled Clinical Trial of Secondary Progressive Multiple Sclerosis Christopher Moore, Jeffery Vernes, Deirdre McIntosh, Syed Haq P3.168 Oral versus Intravenous High Doses of Methylprednisolone in Multiple Sclerosis Relapses, a Double Blinded Randomised Controlled Trial (COPOUSEP): Results at 1 Month (Primary End Point) Emmanuelle Le Page, David Veillard, David Laplaud, Rasha Wardi, Christine Lebrun Frenay, Fabien Zagnoli, Sandrine Wiertlewski, Veronique Deburghgraeve, Marc Coustans, Gilles Edan P3.169 Subgroup and Sensitivity Analyses of the Primary Endpoint from the Peginterferon Beta-1a ADVANCE Study: A Pivotal Phase 3 Study in Patients with Relapsing-Remitting Multiple Sclerosis Bernd Kieseier, Douglas Arnold, Ying Zhu, Shifang Liu, Serena Hung, Aaron Deykin, Sarah Sheikh 74 P3.170 A Phase I/II Study of Pixantrone in Patients with an Aggressive RelapsingRemitting or SecondaryProgressive Multiple Sclerosis (PIXAMS) Richard Gonsette, Gilles Edan, Marc Debouverie, Christian Sindic, Jean Christophe Ferre P3.171 Clinical Efficacy of DelayedRelease Dimethyl Fumarate in Minority Patients with Relapsing-Remitting Multiple Sclerosis (RRMS): An Integrated Analysis of the Phase 3 DEFINE and CONFIRM Studies Michael Hutchinson, J. Theodore Phillips, Macaulay Okwuokenye, Nuwan Kurukulasuriya, Ralf Gold, Robert Fox P3.172 FDA-Approved Phase I Clinical Trial of Autologous Neural Progenitors Injected Intrathecally in Multiple Sclerosis Violaine Harris, Daniel Koffler, Sydney Chirls, Saud Sadiq P3.173 4-Year Follow-up of DelayedRelease Dimethyl Fumarate Treatment in Relapsing-Remitting Multiple Sclerosis (RRMS): Integrated Clinical Efficacy Data From DEFINE, CONFIRM, and the ENDORSE Extension Study Ralf Gold, Ted Phillips, Amit Bar-Or, Michael Hutchinson, Ludwig Kappos, Ray Zhang, Minhua Yang, Vissia Viglietta, Sarah Sheikh, Robert Fox P3.174 Efficacy of Fingolimod in Pre-treated Patients with Disease Activity: Pooled Analyses of FREEDOMS and FREEDOMS II Niklas Bergvall, Nicolaos Sfikas, Peter Chin, Davorka Tomic, Philipp Von Rosenstiel, Ludwig Kappos P3.175 Comparative Efficacy of Switching to Natalizumab Versus Switching to Interferon-Beta or Glatiramer Acetate After On-treatment MS Relapse Using Propensity-Matched Registry Data Maria Trojano, Timothy Spelman, Tomas Kalincik, Annie Zhang, Heinz Wiendl, Ludwig Kappos, Shibeshih Belachew, Robert Hyde, Freek Verheul, Francois Grand-Maison, Helmut Butzkueven P3.176 The PREFERMS Study: Evaluating Real-world Patient Retention on Oral Fingolimod Compared with Injectable Disease Modifying Therapies in RelapsingRemitting Multiple Sclerosis Nadia Tenenbaum, Lesley Schofield, Xiangyi Meng, Ralph Kern P3.177 Evaluation of Immunogenicity in Multiple Sclerosis Patients Treated with Daclizumab-HYP During the SELECT and SELECTION Clinical Trials Lakshmi Amaravadi, Alvydas Mikulskis, Manjit McNeill, Katherine Riester, Marianne Sweetser, Jacob Elkins, Gavin Giovannoni P3.178 Assessing a Scoring System to Predict Disease Activity in Patients with Multiple Sclerosis: Post Hoc Analyses of Data from Clinical Trials of Subcutaneous Interferon Beta-1a Mark Freedman, Ali-Frédéric Ben-Amor, Ernesto Aycardi, Delphine Issard, Florence Casset-Semanaz 3:00 p.m.–6:30 p.m. P3.179 Lymphocyte Count Reductions in Relapsing-Remitting Multiple Sclerosis (RRMS) Patients Treated with DelayedRelease Dimethyl Fumarate: An Integrated Analysis of the Placebo-Controlled Studies Robert Fox, Ralf Gold, J. Theodore Phillips, Krzysztof Selmaj, Kartik Raghupathi, Huixing Yuan, John O’Gorman, Mark Novas, Vissia Viglietta, Nuwan Kurukulasuriya P3.189 P3.180 P3.190 Consistent Reduction in the Annualized Rate of Brain Volume Loss Across Phase 3 Core and Extension Trials of Fingolimod in Relapsing Multiple Sclerosis Ernst-Wilhelm Radue, Till Sprenger, Peter Chin, Daniela Piani Meier, Nicolaos Sfikas, Frederik Barkhof P3.181 Lymphocyte Counts Do Not Predict Risk of Subsequent Relapse or Disability Accumulation in AlemtuzumabTreated Relapsing-Remitting Multiple Sclerosis Patients: An Analysis of the CARE-MS Studies Alasdair Coles, Jeffrey Palmer, David Margolin P3.182 Early and Consistent Reduction in Relapses among Patients with Relapsing-Remitting Multiple Sclerosis Receiving Subcutaneous Interferon Beta-1a: A Post-Hoc Analysis of PRISMS Data Mark Cascione, Carol Gaines, Juanzhi Fang, Fernando Dangond, Aaron Miller P3.183 Patient-Reported Outcomes After Therapy Switch to Fingolimod: Post-hoc Subgroup Analysis of the EPOC Study Barry Singer, Mark Gudesblatt, Neetu Agashivala, Stan Li, Simrat Randhawa, Kevin McCague, Luigi Barbato P3.184 Diagnosing Multiple Sclerosis: Analysis of the Output from an Adjudication Panel in the Setting of a MS Diagnostic Assay Clinical Trial Benjamin Greenberg, Nancy Monson, Douglas Bigwood, Eric Eastman P3.185 Four-year Expanded Disability Status Scale (EDSS) Outcomes in Patients Treated with Fingolimod in the Phase 3 and Extension Trial Program Bruce Cree, Jeffrey Cohen, Peter Chin, Shannon Ritter, Daniela Piani Meier, Philipp von Rosenstiel, Ludwig Kappos P3.186 Natalizumab in Patients with Early MS: The STRIVE Study Roumen Balabanov, Jai Perumal, Robert Fox, Denise Campagnolo, Emese Dian, Stefan Lanker, Jiankang Liu, Mary-Jean Fanelli P3.187 Reduction in Brain Atrophy with Extended Daclizumab HYP Treatment: Results of SELECT and the SELECT Extension Study Ernst-Wilhelm Radue, Dusan Stefoski, Ralf Gold, Manjit McNeill, Katherine Riester, Jacob Elkins P3.188 Decrease in T1 Black Hole Volume Over 2 Years of Daclizumab HighYield Process Treatment Jacob Elkins, Eva Havrdova, Manjit McNeill, Katherine Riester, Ernst-Wilhelm Radue 2O14 Scientific Abstract Listing and Annual Meeting Information Clinical Efficacy of DelayedRelease Dimethyl Fumarate in RelapsingRemitting Multiple Sclerosis (RRMS) Patients with Highly Active Disease: An Integrated Analysis of the Phase 3 DEFINE and CONFIRM Studies Michael Hutchinson, Annie Zhang, Minhua Yang, Ray Zhang, Nuwan Kurukulasuriya, Robert Fox, Ralf Gold Do MRI Lesions Predict MS Relapses? Nancy Richert, Fiona Forrestal, Sophia Lee, Petra Duda P3.191 The Vitamin D to Ameliorate Multiple Sclerosis (VIDAMS) Trial Pavan Bhargava, Sonya Steele, Sandi Cassard, Elizabeth Sugar, Daniel Pelletier, Emmanuelle Waubant, Ellen Mowry P3.192 Pharmacokinetics of Vitamin D in Multiple Sclerosis Patients and Healthy Controls. Sonya Steele, Pavan Bhargava, Jacqueline Marcus, Nisha Revirajan, Emmanuelle Waubant, Ellen Mowry P3.193 Efficacy Benefits of Fingolimod 0.5 mg Once Daily in Patients Previously Treated with Glatiramer Acetate: Pooled Analysis of the Phase 3, Placebo-controlled FREEDOMS and FREEDOMS II Studies in Relapsing Multiple Sclerosis Douglas Jeffrey, Ernst-Wilhelm Radue, Goeril Karlsson, Hanzhe Zheng, Philipp Von Rosenstiel, Ludwig Kappos P3.194 Pharmacokinetics and Pharmacodynamics of Peginterferon Beta1a in Patients with Relapsing-Remitting Multiple Sclerosis: Data from the Pivotal Phase 3 ADVANCE Study Xiao Hu, Yue Cui, Joleen White, Ying Zhu, Aaron Deykin, Ivan Nestorov, Serena Hung P3.195 Mediation of the Effect of Laquinimod on Disability Progression in Relapsing-Remitting Multiple Sclerosis (RRMS) Giancarlo Comi, David Ladkani, Timothy Vollmer, Maria Pia Sormani, Yulia Sidi, Volker Knappertz P3.196 MRI Correlates of Disability: Neuroimaging Substudy at 20 Years in the Ongoing US Glatiramer Acetate Open-label Extension Study Omar Khan, Fen Bao, Megha Shah, Gautam Ramesh, Christina Caon, Carla Santiago, Zahid Latif, Rimma Aronov, Imad Zak, Yulia Sidi, Scott Kolodny Aging, Dementia, and Cognitive and Behavioral Neurology: Clinical Aspects P3.197 Validation of a Simple Model for Prediction of Disease Duration in Persons Presenting with Alzheimer Disease: “ Tell Me Doc, How Long do I Have?” Ashleigh Long, Richard Kryscio, Gregory Jicha P3.198 Frontal Release Signs in Adults with Down Syndrome Are Associated with Dementia Gregory Jicha, Mellani Lefta, William Robertson, Elizabeth Head, Frederick Schmitt P3.199 Computerized Cognitive Testing of Individuals with Down Syndrome and Alzheimer Disease Michael Gutman, Ethan Moskovic, Joseph Jeret Poster Session III P3.200 Clinical Features of Mild Cognitive Impairment of the Cerebrovascular Type (MCI-CVD) Gregory Jicha, Laura Hench, Debra Moser, Erin Abner P3.201 Clinical Characteristics of bvFTD Across CDR Stages Kamalini Ranasinghe, Peter Pressman, David Perry, Katherine Rankin, Bruce Miller P3.202 Visual Perception Test Predicts a Pathological Diagnosis of Alzheimer’s Disease in Patients Presenting with Corticobasal Syndrome Clara Boyd, Michael Tierney, Eric Wassermann, Karen Marder, Salvatore Spina, Adrian Oblak, Bernardino Ghetti, Jordan Grafman, Edward Huey P3.203 Mental Status Examination Practices Among Resident and Attending Physicians in Patients Hospitalized for Evaluation of Confusion Serggio Lanata, Brian Ott P3.204 Assessment of Memory in the Clinic: How Useful Is Cued Recall? Christian Bocti, Catherine Liu, Helene Imbeault, Nancy Leblanc, Francis Langlois P3.205 Plasma Levels of HDL and Carotenoids Are Lower in Alzheimer’s Disease Patients with Vascular Comorbidities But Plasma Protein Nitration and Oxidation Is Unaffected Gereon Nelles, Irundika Dias, Daniela Weber, Li Li, Wilhelm Stahl, Tilman Grune, Maria Polidori, Helen Griffiths P3.206 Atypical Antipsychotic Utilization in Dementia Patients at a Long-Term Care Facility: A Retrospective Study Douglas Scharre, Shu-Ing Chang, Haikady Nagaraja, Michael Merjanian, Gail Greenley, Rebecca Davis P3.207 P3.212 The Role of Gender Differences in Dementia Caregiver Risk Carol Lippa, Kate Bowen, Candace Robertson-James, Ana Nunez, Elizabeth Gonzalez P3.213 Normal Cognition in a 99-yearold Man with High Levels of Alzheimer Disease Pathology Kristoffer Nissinen, Barbara Agee Shah, Maria Corrada, Ronald Kim, Szofia Bullain, Claudia Kawas P3.214 Intermittent Temporal Slowing in Cognitively Normal Oldest-old: The 90+ EEG Study Szofia Bullain, Maria Corrada, Dana Greenia, Claudia Kawas P3.215 Neuropsychiatric Symptoms, ApoE4 and the Risk of Incident Dementia: The Mayo Clinic Study of Aging Anna Pink, Jazmin Acosta, Rosebud Roberts, Michelle Mielke, Teresa Christianson, Vernon Pankratz, G Stokin, Bradley Boeve, Yonas Geda P3.216 Cognitive Reserve markers independently predict Cognitive outcomes in patients with SAH Neha Dangayach, Laura Zhaodne, Yaakov Stern, Christina Falo, Sachin Agarwal, Meyers Emma, Jan Claassen, Stephan Mayer Aging, Dementia, and Cognitive and Behavioral Neurology: Executive Function P3.217 Functional Near-Infrared Spectroscopy (fNIR) based Detection of Increased Prefrontal Cortex Activity in Frontotemporal Dementia Jillian Edwards, Tooba Fayyaz, Lauren Scull, Hasan Ayaz, Patricia Shewokis, David Libon, Carol Lippa, Anahita Deboo, Terry Heiman-Patterson Amyloid PET Screening for Enrollment into Alzheimer’s Disease Clinical Trials: Initial Experience in a Phase 1b Clinical Trial Jeff Sevigny, Joyce Suhy, Ping Chiao, Gregory Klein, Joonmi Oh, Derk Purcell, Mehul Sampat, Jerome Barakos P3.218 P3.208 Cognitive and Functional Decline and their Relationship in Patients with Mild Alzheimer’s Disease Hong LiuSiefert, Eric Siemers, Karen Sundell, Karen Price, Baoguang Han, Katherine Selzler, Joel Raskin, Richard Mohs P3.219 P3.209 P3.220 Florbetapir F18 PET Amyloid Neuroimaging and Baseline Characteristics in Patients with Alzheimer’s Dementia Elisabeth Degenhardt, Michael Witte, Michael Case, Peng Yu, David Henley, Helen Hochstetler, Deborah DSouza, Paula Trzepacz P3.210 Impact of Amyloid Beta Imaging on Diagnosis and Clinical Management of Hypothetical Patients with Mild Cognitive Impairment or Dementia. Joshua Cohen, Yue Zhong, Jason Karlawish P3.211 MRI Volumetric Analysis, Cognitive Profiles and Biomarkers in a Sample of Argentina -ADNI patients Marcos Fernandez Suarez, Griselda Russo, Patricio Chrem Mendez, Fernando Ventrice, Ezequiel Surace, Maria Russo, Jorge Campos, Federico Nahas, Gustavo Sevlever, Silvia Vazquez, Ricardo Allegri Strategic Choice In Frontotemporal Dementia: Evidence From The Ultimatum Game Stefano Cappa, Alessandra Dodich, Chiara Cerami, Nicola Canessa, Chiara Crespi, Alessandra Marcone Digit Span: A Comparison of Chinese Versus Alphabetic Language Speakers in Dysexecutive Dementia Patients Simon Kang Seng Ting, Shahul Hameed, Eng-King Tan, Christopher Gabriel, Kinjal Doshi P3.224 Neuroanatomy of GoalDirected Behavior in behavioral variant Frontotemporal Degeneration Lauren Massimo, John Powers, Lois Evans, Brianna Morgan, Corey McMillan, Katya Rascovsky, Paul Eslinger, Mary Ersek, Murray Grossman P3.225 Temporal Discounting of Future Rewards in Behavioral Variant Frontotemporal Dementia (bvFTD) and Alzheimer’s Disease (AD) Katya Rascovsky, Joe Kable, Rebecca Kazinka, Eileen Moran, Christopher Olm, Jenna Glasenberg, Ashley Boller, Joe McGuire, Corey McMillan, Robin Clark, Murray Grossman P3.226 Video Tracking of Cancellation Is Sensitive to Acute Brain Impairment and Disability Lynita Mullins, Victor Mark, Adam Woods, Mary Banasiewicz Epilepsy and Clinical Neurophysiology: Clinical Manifestations P3.227 Epileptic Vertigo and Dizziness—a Systematic Review of the Literature Alexander Tarnutzer, Seung-Han Lee, Karen Robinson, Peter Kaplan, David Newman-Toker P3.228 Whistling Seizure: A Unique Case Report of a Rare Automatism Kaitlyn Lillemoe, Daniel Torres, Anuradha Singh P3.229 Post-ictal Lateralized Hyperkinetic Motor Behavior Brian Beck, Gregory Chang P3.230 Epilepsy Classification in Adults with a First Epileptic Seizure; Experience from a Tertiary Epilepsy Clinic Michael Koutroumanidis, Vasiliki Tsirka, Ioannis Zoukos, Mark Richardson P3.231 Seizures Without Awareness: A Pure Cohort William Tatum, Langston Michael, Kirsten Yelvington, Jerry Shih P3.232 A Stimulating Inner Conversation Daniel Goldenholz, Xiangping Zhou, William Theodore, Kareem Zaghloul, Sara Inati P3.233 Pancytopenia Associated with Shapiro Syndrome in a Patient with Posterior Porencephaly Jordan Schaefer, Amy Crepeau, Vilmarie Rodriguez Transfer of Working Memory Performance Enhancement Induced by Transcranial Direct Current Stimulation (tDCS) Jay Gill, Roy Hamilton P3.234 P3.221 P3.235 Correlation of Executive Dysfunction and Delusions or Hallucinations with Autoimmune and Paraneoplastic Antibodies in Elderly Presenting with Memory Complaints Rhonna Shatz, Wendy Lemere, Lynn Etters, Marina Novikova P3.222 Hyperostosis Frontalis Interna, Causing Frontal Lobe Dysfunction and Refractory Headaches Mitra Assadi Khansare, Marc Duome, Arlan Mintz P3.223 Beyond Words: Pragmatic Inference in the Behavioral Variant of Frontotemporal Dementia Nicola Spotorno, Corey McMillan, Katya Raskovsky, Robin Clark, Murray Grossman Hemimegalencephaly: Adult Evolution Nicky Wu, Felippe Borlot, Anfal Ali, Timo Krings, Andres Lozano, Danielle Andrade New Onset Seizures in Elderly: Clinical Presentation and Etiology of First Ever Seizure Erum Shariff, Majed Alhameed P3.236 Subclinical EEG Seizures as a Predictor of Tumor Progression in Brain Tumor Patients Presenting with Altered Mental Status Meghan Ward, Simran Singh, Irena Garic, Jeffrey Kennedy, Priya Kumthekar, Michael Macken, Elizabeth Gerard, Jeffrey Raizer, Stephan Schuele Epilepsy and Clinical Neurophysiology: AED P3.237 Safety of Eslicarbazepine Acetate in Patients with Refractory PartialOnset Seizures Treated With or Without Concomitant Carbamazepine: A Pooled Analysis of Three Phase III Controlled Studies Selim Benbadis, Victor Biton, Mercedes Jacobson, Eugen Trinka, Mar Carreño, David Blum, Patrício Soaresda-Silva, Helena Gama, Rui Sousa, Todd Grinnell, Raymond Claus P3.238 Effects of Eslicarbazepine Acetate on Cardiac Function in Patients with Refractory Partial-Onset Seizures: A Pooled Analysis of Three Phase III Controlled Studies Inna Vaisleib, Patricia Penovich, Bassel Shneker, Elza Yacubian, David Blum, Helena Gama, Patrício Soaresda-Silva, Todd Grinnell P3.239 Efficacy of Eslicarbazepine Acetate in Patients with Refractory Partial-Onset Seizures Treated With or Without Concomitant Carbamazepine: A Pooled Analysis of Three Phase III Controlled Studies Steve Chung, Gregory Krauss, Michael Sperling, Eugen Trinka, Mar Carreño, David Blum, Patrício Soares-daSilva, Rui Sousa, Todd Grinnell, Hailong Cheng P3.240 Safety of Eslicarbazepine Acetate in Elderly Subjects: A Pooled Analysis of Five Phase II Placebo-controlled Non-Epilepsy Studies Eva Andermann, R. Eugene Ramsay, Elinor Ben-Menachem, David Blum, Helena Gama, Patrício Soaresda-Silva, Todd Grinnell P3.241 Incidence of Allergic Reaction Adverse Events during Adjunctive Treatment with Eslicarbazepine Acetate in Patients with Refractory Partial-Onset Seizures: A Pooled Analysis of Three Phase III Placebo-Controlled Studies Joanne Rogin, Trevor Resnick, Laura Strom, Elinor Ben-Menachem, Silvia Kochen, David Blum, Helena Gama, Patrício Soares-da-Silva, Todd Grinnell P3.242 Conversion to Monotherapy with Eslicarbazepine Acetate in Adults with Partial-Onset Seizures—Results of a North-American Study Michael Sperling, J. Harvey, David Blum, Todd Grinnell P3.243 Co-administration of Carbamazepine with Eslicarbazepine Acetate Decreases Eslicarbazepine Exposure: A Population Pharmacokinetic Analysis Blanca Vazquez, Robert Wechsler, William Rosenfeld, Christian Elger, Pedro Kowacs, Patrício Soares-da-Silva, Joana Moreira, Jahnavi Kharidia, Gary Maier, David Blum, Todd Grinnell P3.244 Pharmacokinetic Rationale for mg-to-mg Overnight Switch from b.i.d. Immediate Release Topiramate (TPM-IR) to Extended-release Once-daily SPN-538 (Trokendi XR™) Jennifer Dugan Stocks, Janet Johnson, Scott Brittain, Paolo Baroldi Fast, Easy Registration Online · AAN.com/view/AM14 75 Tuesday April 29 First Authors stand by Posters from 5:00 p.m.–6:30 p.m. Tuesday, April 29 P3.245 Steady-State Bioequivalence of Extended-release Once-daily SPN-538 (Trokendi XR™) to Immediate-Release Topiramate (TPM-IR, Topamax®) Janet Johnson, Scott Brittain, Jennifer Dugan Stocks, Paolo Baroldi P3.246 Topiramate Pharmacokinetics of Extended-release Once-daily SPN-538 (Trokendi XR™) in the Elderly Welton O’Neal, Scott Brittain, Jennifer Dugan Stocks, Janet Johnson, Paolo Baroldi P3.247Pharmacokinetic- Pharmacodynamic Analysis of Extendedrelease Once-daily Oxcarbazepine Formulation SPN-804 (Oxtellar XR™) in Adults with Epilepsy Scott Brittain, Janet Johnson, Paolo Baroldi P3.248Oxcarbazepine Pharmacokinetics of Extended-release Once-daily SPN-804 (Oxtellar XR™) in the Elderly Welton O’Neal, Scott Brittain, Janet Johnson P3.249 Long-Term Efficacy of Clobazam for Drop Attacks in LennoxGastaut Syndrome Is Consistent Across Patient Age Ranges Jouko Isojarvi, Deborah Lee, Vivienne Shen, Jeffrey Buchhalter P3.250 Patients Treated with Clobazam Experienced Fewer Seizurerelated Injuries Than Placebo Patients During the Phase III CONTAIN Trial in Lennox-Gastaut Syndrome Jouko Isojarvi, Michael Sperling, Deborah Lee P3.251 IV Carbamazepine (CBZ) as Short-Term Replacement Therapy for Oral CBZ in Adults with Epilepsy: Primary Results of a Phase III Safety Trial Suresh Dheerendra, Pavel Klein, Victor Biton, Xiaolin Zhang, Uwa Kalu, Deborah Lee, Jonathan Halford P3.252 Clobazam Response in Patients with Previous Benzodiazepine Use: Subanalysis of the Phase III CONTAIN Trial in Lennox-Gastaut Syndrome (LGS) Deborah Lee, William Rosenfeld, Jouko Isojarvi P3.253 Long-Term Response to Clobazam By Baseline Seizure Frequency in Patients with Lennox-Gastaut Syndrome (LGS) Deborah Lee, James Wheless, Jouko Isojarvi P3.254 Efficacy and Safety of Clobazam in Lennox-Gastaut Syndrome: Completers Analysis of the 15-week, Phase III CONTAIN Trial Joan Conry, Yu-Tze Ng, Guangbin Peng, Deborah Lee, Jouko Isojarvi P3.255 A Comparison Between Pharmacological Treatment of Epileptic Patients with and Without Intellectual Disability. Jonathan Fridhandler, Fernando Coelho, Peter Tai, Nathalie Jette, Danielle Andrade P3.256 How Well Do We Know Our AEDs? Neurology Resident Screening Practices of AED Side Effects Gunjan Narwani, Reena Nanjireddy, Aashit Shah, Maysaa Basha 76 P3.257 Impact of Delayed-Dose Administration of USL255, an Extendedrelease Topiramate Formulation Bob Anders, Qiang Lu, Elizabeth Ludwig, Annie Clark P3.258 Comparison of the Pharmacokinetics of USL255, an Extendedrelease Topiramate, When Sprinkled onto Soft Food or Swallowed Intact Annie Clark, Bob Anders, Mark Halvorsen P3.259 Extended-release Oncedaily SPN-538 (Trokendi XR™) Versus Twice-Daily TPM-IR (Topamax®): Impact of Dosing Irregularities on Topiramate Concentrations Scott Brittain P3.260 Dose Linearity and Dose Strength Equivalence of Extendedrelease Once-daily SPN-538 (Trokendi XR™) Jennifer Dugan Stocks, Erika Roers, Scott Brittain, Paolo Baroldi P3.261 Efficacy, Safety, and Impact on Quality of Life of USL255 in Patients with Refractory Partial-Onset Seizures: The PREVAIL Study Steve Chung, Toufic Fakhoury, Stephan Arnold, Balduin Lawson, Ilan Blatt, Annie Clark, Mark Halvorsen, Venkatesh Nagaraddi, Bob Anders P3.262 Adverse Event Profile of USL255 in Patients with Refractory PartialOnset Seizures: The PREVAIL Study Robert Hogan, Stephan Arnold, Toufic Fakhoury, Bob Anders P3.263 Efficacy of USL255 Across Partial-Onset Seizure Types and Refractory Patient Status: Subgroup Analyses From the PREVAIL Study Ilan Blatt, Venkatesh Nagaraddi, Robert Hogan, Stephan Arnold, Balduin Lawson, Bob Anders, Annie Clark, Mark Halvorsen, Steve Chung P3.264 Early Onset of Efficacy and Safety Outcomes with USL255 Treatment: The PREVAIL Study Venkatesh Nagaraddi, Steve Chung, Stephan Arnold, Annie Clark, Bob Anders, Toufic Fakhoury P3.265 USL255, Extended-release Topiramate, Displays an Improved Pharmacokinetic Profile with Reduced Adverse Events Compared with ImmediateRelease Topiramate Annie Clark, Robert Hogan, Bob Anders P3.266 Comparison of Adverse Effects of USL255 and Commonly Prescribed AEDs: Assessment of Relative Risk Kimford Meador, Frank Gilliam, Robert Hogan, Mary Holmay, Annie Clark, Bob Anders P3.267 Therapeutic Time Window of Perampanel for the Termination of Diazepam-Resistant Status Epilepticus (SE) in a Lithium-Pilocarpine Rat Model Katsutoshi Ido, Takahisa Hanada P3.268 Perampanel Clinical Studies: Analysis of Psychiatric and Behavioral Events Alan Ettinger, Antonia LoPresti, Haichen Yang, Betsy Williams, Sharon Zhou, Randi Fain, Antonio Laurenza 3:00 p.m.–6:30 p.m. P3.269 Effect of Adjunctive Lacosamide on Complex Partial Seizures and Partial Seizures with Secondary Generalization in Adults: Pooled Analysis of Three Open-label Extension Trials Svetlana Dimova, Cindy McShea, Pamela Doty, Konrad Werhahn, Marc De Backer P3.270 Anti-Seizure Effects of Perampanel in Combination with Other Antiepileptic Drugs (AEDs) in a Rat Amygdala Kindling Model Ting Wu, Takahisa Hanada P3.271 Interim Efficacy and Safety Analysis of Adjunctive Perampanel in the Adolescent Population from the Extension Phase of 3 Double-Blind, Placebo-Controlled, Phase 3 (Core) Studies in Patients with Refractory Partial-Onset Seizures Ben Renfroe, Haichen Yang, Betsy Williams, Steven Huang, Antonio Laurenza P3.272 Analysis of Falls in Epilepsy Patients with Partial Onset Seizures in Perampanel Phase 3 Trials Ilo Leppik, Haichen Yang, Betsy Williams, Sharon Zhou, Randi Fain, Antonio Laurenza P3.273 Efficacy and Safety of Adjunctive Perampanel Based on Number of Antiepileptic Drugs at Baseline Tracy Glauser, Antonio Laurenza, Haichen Yang, Betsy Williams, Dongyuan Xing, Randi Fain P3.274 Lacosamide Conversion to Monotherapy for the Treatment of Partialonset Seizures in Adults: Results from a Multicenter, Randomized, Double-blind, Historical-controlled Trial Robert Wechsler, George Li, Jacqueline French, Terence O’Brien, O Neil D’Cruz, Paulette Williams, Melissa Brock P3.275 Lacosamide Added to Existing Monotherapy in Epilepsy Patients with Partial Onset Seizures: Second Interim Analysis of the VITOBA Study Matthias Noack-Rink, Thomas Mayer, Stephan Arnold, Uwe Runge P3.281 Differences in Usage of Clobazam Versus Clonazepam for Epilepsy Daniel Jones, Jouko Isojarvi, Alice Guiraud-Diawara, Vivienne Shen, Patrice Verpillat P3.282 What a “Drop-Out” Reveals About the Nocebo Effect in Patients Tricia Ting, James Polli, Wenlei Jiang P3.283 Hematologic Profile Associated with Newer-generation Anti-epileptic Medications in the Pediatric Population Puja Joshi, Sonam Verma, Anita Sui, Yen-Hong Kuo, Victor Johnson, Richard Sultan P3.284 Long-term Open-label Extension (OLE) Study Evaluating USL255, Once-daily Extended-release Topiramate, in Patients with Partial Onset Seizures: Interim Analysis from PREVAIL OLE Toufic Fakhoury, Robert Hogan, Ilan Blatt, Steve Chung, Bob Anders P3.285 Pharmacokinetics of USL261, a Novel Intranasal Formulation of Midazolam, in Subjects with Epilepsy Lindy Bancke, Heather Dworak, Mark Halvorsen P3.286 Lacosamide Experience in Patients with Lennox-Gastaut Syndrome and Epilepsy Pedro Bermejo, Andres Cruz P3.287 Cortical Mapping of Language in the Basal Temporal Area in Pediatric Patients Undergoing Epilepsy Surgery Evaluation. Christelle Moufawad El Achkar, Joseph Madsen, Jeffrey Bolton, Tobias Loddenkemper Myopathies/Muscle Disease P3.288 Abnormalities of Mitophagy in Sporadic Inclusion-Body Myositis (s-IBM) Muscle Fibers Anna Nogalska, Carla D’Agostino, Mafalda Cacciottolo, King W. Engel, Valerie Askanas P3.289 P3.276 Lacosamide for Uncontrolled Primary Generalized Tonic-clonic Seizures: An Open-label Extension Study Stephen Yates, Robert Wechsler, Cynthia Beller Progressive Ophthalmoplegia with Ocular and Generalized Myopathy with Ragged-Red Fibers, Linear Scleroderma and Contralateral Cerebral Hemiatrophy Walter Haupt, Monika Rabenstein, Anna Brunn, Lothar Burghaus P3.277 Safety and Pharmacodynamics of USL261, a Novel Intranasal Formulation of Midazolam, in Subjects with Epilepsy Robert Hayes, Lindy Bancke, Heather Dworak P3.290 P3.278 P3.291 Can We Trust Standard Healthy Volunteer Data to Assess Generic Drug Quality: Lamotrigine Experience in Patients? James Polli, Tricia Ting, Wenlei Jiang P3.279 Levetiracetam in the Treatment of Epilepsy as Add On or Mono Therapy Sarwer Al-Bajalan, Murad Kamel P3.280 Use of Investigator Training to Improve Seizure Classification in PREVAIL: A Phase 3, Global Study Evaluating USL255, Once-daily Extended-release Topiramate, in Adults with Partial-Onset Seizures Bree DiVentura, Jacqueline French, Bob Anders, Dawn Laine 2O14 Scientific Abstract Listing and Annual Meeting Information Carnitine Deficiency, A Spectrum Disorder: Case Series and Histopathological and Ultrastructural Characterization Amanda Michael, Bassam Malo, Stanley Iyadurai Early Onset and Fulminant Course of Sporadic Inclusion Body Myositis (sIBM): A Case Report Alison Walsh, Goran Rakocevic P3.292 Lipid Storage Myopathy Unmasked by the Antianginal Drug Ranolazine Charles Kassardjian, Duygu Selcen, Georgirene Vladutiu, Lee-jun Wong, Margherita Milone P3.293 Late-onset Pompe Disease: A Case Series. Omar Jawdat, Mamatha Pasnoor, April McVey, Ahmad Abuzinadah, Laura Herbelin, Richard Barohn, Mazen Dimachkie, Majed Dasouki P3.294 Not PFK Deficiency Lydia Sharp, Nadine Romain, Ronald Haller Poster Session III P3.295 Clinical Anatomical and Epidemiologic Study of 11 Patients with McArdle’s Disease Alzira Carvalho, Pâmela Delgado, Miriam Koch, David Feder P3.296 Asymptomatic Pompe Disease: A Study of 6 Patients. Andoni Echaniz-Laguna, Robert-Yves Carlier, Kenza Laloui, Pierre Carlier, Emmanuelle SalortCampana, Jean Pouget, Pascal Laforet Neurologic Complications of Cancer P3.307 Myelitis Following Intrathecal Chemotherapy in Acute Lymphoblastic Leukemia: A Case Report Alicia Parker, Ahmed Yassin, Karin Woodman P3.308 Muscle Disease Atypical Neurological Complications of Ipilimumab Therapy in Patients with Metastatic Melanoma Alicia Parker, Ahmed Yassin, Karin Woodman P3.297 P3.309 Pompe Disease: Distal Myopathy in a Previously Unreported Heterozygous Variant João Dib, Osvaldo Nascimento, Eduardo Davidovich, Ricardo Dornas, Camila Pupe, Bruno Coutinho P3.298 Frequencies of Seven Muscle Enzyme Deficiencies in Samples Tested for Myoglobinuria in a Clinical Laboratory Malgorzata Jaremko, Kaylan Burnham, Maximo Tatis, Jamie Willis, Sat Dev Batish, Joseph Higgins P3.299 A Diagnostic Flowchart for POLG Related Diseases Based on Signs Sensitivity and Specificity Maya Tchikviladzé, Mylène Gilleron, Thierry Maisonobe, Damien Galanaud, Pascal Laforet, Alexandra Durr, Bruno Eymard, Fanny Mochel, Hélène Ogier, Anthony Béhin, Tanya Stojkovic, Bertrand Degos, Isabelle Gourfinkel-An, Frederic Sedel, Mathieu Anheim, Alexis Elbaz, Karine Viala, Marie Vidailhet, Alexis Brice, Claude Jardel, Anne Lombes P3.300 Myopathy as a Cause of Camptocormia: A Prospective Study JeanBaptiste Chanson, Béatrice Lannes, Andoni Echaniz-Laguna P3.301 Serum Cytokine Analysis in Idiopathic Inflammatory Myopathies Diagnosed on the Basis of Pathological Findings Meiko Maeda P3.302 Expanding the Clinical and Genetic Spectrum of MYH7 Related Skeletal Myopathies in the United Kingdom Kathryn Brennan, Anna Sarkozy, Cheryl Longman, Michela Guglieri, Tuomo Polvikoski, Maria Farrugia, Richard Petty, Victoria Murday, Dean John, Steven Hardy, Hanns Lochmuller, Katie Bushby, Volker Straub P3.303 Paroxysmal Vocal Cord Motion Dysfunction Masquerading as Neuromuscular Disorders Darine Kassar, William Arnold, Chad Hoyle, John Kissel A Unique Presentation of Pediatric Stroke Attributed to Intrathecal Methotrexate Mohammed Ilyas, Mitchel Williams P3.310 Nafcillin® and Rifampin® Therapy for MSSA Ventriculitis Associated with CSF Shunt: A Case Report Christopher Goshgarian, Abdulrahman Alwaki, Anibal Lugo, Tamer Abdelhak P3.311 Corneal Confocal Microscopy in Patients with Chemotherapy-Induced Neuropathy Marta Campagnolo, Daniela Lazzarini, Iva Fregona, Mario Cacciavillani, Francesca Bergamo, Raffaele Parrozzani, Edoardo Midena, Chiara Briani P3.312 Characterization of Seizures and Their Response to Treatment in a Cohort of Patients with Glial Tumors in a University Institute José Tafur Canabal, Alejandra Gonzalez Roffo, Valeria Beatriz Kuchkaryan, Victoria Campanucci, Jorge Igirio Gamero, Alejandra Báez, Cecilia Sánchez Retamar, Ignacio Casas Parera P3.313 Epilepsy and Cancer: Ancient Problem in a Top Mortality Illness Bernardo Cacho Diaz P3.314 Palinopsia and Palinacousis Emily Johnson, Mohammad Salajegheh P3.315 Focal Injection of Incobotulinum Toxin A Improves Refractory Local Cancer Pain at the Site of Radiation/ Surgery Rezvan Rostami, Duarte Machado, Diana Richardson, Bahman Jabbari P3.316 Neuropathic Itch as a Presenting Feature of Post-Mastectomy Pain Syndrome Robert Knobler Neuro-oncology: Paraneoplastic Syndromes and Other Antibodymediated Disorders P3.317 P3.304 Myalgia and Hyper-CKemia Due to Novel Homozygous ANO5 Deletion Rajat Lahoria, Thomas Winder, Jie Liu, Margherita Milone Humoral Immune Response Against Neural Antigens in Endometrial Cancer Patients Slawomir Michalak, Karolina Poplawska-Domaszewicz, Agata Paluch, Dariusz Szpurek, Stefan Sajdak, Wojciech Kozubski P3.305 P3.318 Slow Channel Syndrome Leading to Distal Myopathy in a Large Family: Therapeutic Perspectives Corrado Angelini, Giovanni Vazza, Maria Mostacciuolo P3.306 Familial Distal Myopathy Due to PNLPA2 Mutation Corrado Angelini, Daniela Tavian, Elisabetta Tasca, Sara Missaglia The Expression of Neurotrophic Factors in Peripheral Blood Mononuclear Cells and Neurological Complications of Cancer Slawomir Michalak, Joanna Rybacka-Mossakowska, Daria Swiniuch, Joanna Gazdulska, Maria Litwiniuk, Rodryg Ramlau, Wojciech Kozubski P3.320Anti-NMDA-receptor Encephalitis: Case Report of Persistent Anti-NMDAR Antibodies 10 Years from Initial Undiagnosed Presentation Maria Fang-Chun Chen, Michelle Dougherty, Josep Dalmau P3.321 Atypical Encephalitis with Voltage-gated Potassium Channel (VGKC) and N-Methyl-D-Aspartate-Receptor (NMDAR) Antibodies with HIV and Pathologic Confirmation Debra Ehrlich, Atul Ramesh, Steven Herskovitz, Howard Geyer, Patrick Lasala, Karen Weidenheim, Jerome Graber P3.322 Suspected Paraneoplastic Autonomic Neuropathy in a Patient with Newly Diagnosed Glioblastoma Multiforme Alyx Porter, Brent Goodman P3.323 The Population-based Survey of Paraneoplastic Neurological Syndromes in the Czech Republic During the Eight Years´ Period Pavel Stourac, Jana Bednarova, Petra Praksova, Magdalena Hladikova, Krystyna Kantorova Child Neurology and Developmental Neurology III P3.332 Behavioral Profiles of Children and Adolescents with Specific Language Impairment and High Functioning Autism Marisela Dy, Angela Ballantyne, Doris Trauner P3.333 Acute Disseminated Encephalomyelitis in a Pediatric RenalTransplant Recipient. Daniel Vela-Duarte, Eugene Schnitzler, Vikram Prabhu P3.334 An Unusual Prolonged Presentation of Synthetic Cathinone Encephalopathy Responsive to Steroids: A Case Report Rawan Albadareen, Jennifer Lowry, Stephen Thornton, Arezou Heshmati P3.335 A Polio-Like Syndrome in California: Clinical, Radiologic, and Serologic Evaluation of Five Children Identified by a Statewide Laboratory Over a Twelve-Month Period Alexandra Roux, Sabeen Lulu, Emmanuelle Waubant, Carol Glaser, Keith Van Haren P3.324 P3.336 Neuro-oncology: Meningioma, Neurofibromatosis, and Other Non-glial Tumors P3.337 Glioblastoma Multiforme in a Patient with Multiple Sclerosis: A Case Report Carlos Romo, Aline Herlopian, Nabeel Chauhan, Robert Archer, Shirley Ong P3.325 Hormone Replacement Therapy Increases the Risk of Cranial Meningioma Lene Andersen, Soren Friis, Jesper Hallas, Pernille Ravn, Henrik Daa Schrøder, David Gaist P3.326 Clinical and Radiological Response of NF2 Associated Tumours to Bevacizumab in an English Cohort Katrina Morris, Shazia Afridi, Patrick Axon, Gareth Evans, Allyson Parry, Dorothy Halliday, Pieter Pretorius P3.327 Neurofibromatosis 2 with Limited Phenotype in a Kindred with Deletion of Exon 9 in the NF2 Gene. Leif Wiklund, Anna Flodin, Karin Zyk-Zackrisson, Ole Kvorning, Margareta Nordling P3.328 Novel Constitutional Chromosomal Deletion, 4q32.1, in a Patient with Neurofibromatosis Type 1 and Glioblastoma Multiforme Amanda Michael, Colin Hirst, Ryan Miller, Miguel Guzman, Ghazala Hayat P3.329 Diagnostic Dilemma of Bell’s Palsy: Case of Facial Nerve Schwannoma Presenting as Acute Bell’s Palsy Nidhi Mehta, Satinder Kaur, Kelsey West Abnormalities of the Brain Functional Connectome in Pediatric Patients with Multiple Sclerosis Massimo Filippi, Paola Valsasina, Sara Sala, Vittorio Martinelli, Angelo Ghezzi, Pierangelo Veggiotti, Andrea Falini, Giancarlo Comi, Maria Rocca Ten Years in the Making—A Longitudinal Study of Language Development in Children and Adolescents Jerzy Szaflarski, Yingying Wang, Mekibib Altaye, Akila Rajagopal, Anna Byars, Elena Plante, Scott Holland P3.338Magnetoencephalographic Parameters of Fetal Brain Maturation Naim Haddad, Hari Eswaran, Eric Siegel, Curtis Lowery, Rathinasami Govindan, Srinivasan Vairavan Neuroscience Research Prize Recipients P3.339 Evidence of Toll-like Receptor Nine-mediated Amelioration of Amyloid Pathology in a TgSwDI Mouse Model of Alzheimer’s Disease Charlotte Herber P3.340 Promoting Repair of Damaged Corticospinal Tract Stefanie Henry P3.341Pan-neuronal Over-expression of the GCLc Gene to Mitigate Redox Stress and Mitochondrial ETC Complex Dysfunction in Alzheimer’s Disease Lisa Michaels P3.330 Treatment of Pituitary Tumors with Temozolomide: A Case Series Justin Jordan, Tucker Cushing, Jorg Dietrich P3.331 Thoracolumbar Spinal Angiolipoma Demonstrating High Signal on STIR Imaging: A Case Report. Alex Linn, Denny Reyes P3.319 Atypical Neuroimaging Findings in Hodgkin’s Lymphoma Associated with Anti-GAD Antibodies Caelan Ford, Ratna BhavarajuSanka, Rebecca Romero Fast, Easy Registration Online · AAN.com/view/AM14 77 Tuesday April 29 First Authors stand by Posters from 5:00 p.m.–6:30 p.m. Tuesday, April 29 S14 MS and CNS Inflammatory Disease: Animal and In Vitro Studies 3:15 p.m. S14.001 Endothelial TREK1 Potassium Channels Are Critical Regulators of Immune Cell Migration into the CNS Stefan Bittner, Tobias Ruck, Kerstin Goebel, Nico Melzer, Heinz Wiendl, Sven Meuth 3:30 p.m. S14.002 Amyloid Fibril-forming Hexapeptides Modulate the Immune Response and Reduce Symptoms in an Animal Model of Multiple Sclerosis Michael Kurnellas, Jonathan Rothbard, Jill Schartner, Lawrence Steinman 3:45 p.m. S14.003 Contribution of a Dysfunctional RNA Binding Protein, hnRNP A1, to Neurodegeneration in MS Michael Levin, Sangmin Lee, Lidia Gardner, Joshua Douglas, Yoojin Shin, Paul Sawchenko, Stephen Lalor, Benjamin Segal 4:00 p.m. S14.004 A Nasal Anti-CD3 Vaccine Treats a Model of Secondary Progressive MS by Inducing IL-10 Dependent T Regulatory Cells and Regulating CNS Innate Immunity Lior Mayo, Andre Pires Da Cunha, Raymond Sobel, Hans Lassmann, Francisco Quintana, Howard Weiner 4:15 p.m. S14.005 IRX4204: A Highly Selective RXR Agonist Modulates Adaptive Treg Differentiation Independent of RAR, and Effectively Inhibits Central Nervous System Inflammation Elizabeth Nowak, Rosh Chandraratna, Randolph Noelle 4:30 p.m. S14.006 IRX4204: A Clinical Stage, Potent, and Highly Selective RXR Agonist Compound Is Brain Penetrant, and Promotes Differentiation of Oligodendrocyte Precursor Cells (OPCs) In Vitro Martin Sanders, Satish Medicetty, Rosh Chandraratna 4:45 p.m. S14.007 Effects of Polarized Human Lymphocytes and Myeloid Cells on Astrocyte Responses and Oligodendrocyte Differentiation Craig Moore, Nebras Warsi, Qiao Ling Cui, Bryce Durafourt, Jack Antel, Amit Bar-Or 78 S15 Cerebrovascular Disease and Interventional Neurology: Clinical and Imaging Biomarkers and Genetics 3:15 p.m. S15.001 Abnormal Left Ventricular Geometry in Lacunar Stroke: Spectrum, Prevalence and Prognostic Implications in the SPS3 Trial Thalia Field, Lesly Pearce, Nathan ChanSmyth, Sabe De, Gordon Gubitz, Stephen Phillips, Robert Hart, Oscar Benavente 3:30 p.m. S15.002 Infarction Volume in Patients with Atrial Fibrillation: The Impact of Left Ventricular Stiffness Hee-Seung Ahn, Wi-Sun Ryu 3:45 p.m. S15.003 The Collateral Circulation on Day-2 CT Angiography Is a Reliable Predictor of Functional Outcomes in Acute Ischemic Stroke. Leonard Yeo, Prakash Paliwal, Hock Luen Teoh, Bernard Chan, Chee Seong Seet, Eric Ting, Gavin Lim, Venetia Ong, Ganesh Shamugam, Amit Varma, Vijay Sharma 4:00 p.m. S15.004 Identifying Novel Biomarkers of Cerebral Ischemia through the Use of Mass Spectroscopy Paul George, Christopher Adams, Michael Mlynash, Christian Kjaergaard, Calvin Kuo, Stephanie Kemp, Madelleine Garcia, Gregory Albers, Jean-Marc Olivot 4:15 p.m. S15.005 Proteomic Profiling of Acute Stroke Patients Post IV Thrombolysis: Mapping tPA Efficacy in Real Time MingMing Ning, Mary Lopez, David Sarracino, David McMullin, Xiaoying Wang, Ferdinando Buonanno, Eng Lo 4:30 p.m. S15.006 COL4A1 Mutations: Clinical and Radiological Phenotypes in a French Adult Cohort Aurélie Siri, Elisabeth Tournier-Lasserve, Manuelle Mine, Eloi Magnin, Eric Berger, Caroline Arquizan, Xavier Ayrignac, Clarisse Carra-Dalliere, Giovanni Castelnovo, Nicolas De Champfleur, Pierre Labauge, Jean Philippe Neau, Tiphaine Rouaud, Sonia Alamowitch 4:45 p.m. S15.007 An Autosomal Dominant Arteriopathy of the Brain Due to a Novel Mutation in Collagen 4A1 Gene in a Family with Early-onset Stroke and Leukoencephalopathy Matthew Schrag, William Graf, Anna Szekely 3:15 p.m.–5:00 p.m. S16 Neuromuscular and Clinical Neurophysiology (EMG): Clinical Trials and Therapy 3:15 p.m. S16.001 Lack of Correlation Between Biomarker and Clinical Outcome Measures in the Arimoclomol Inclusion Body Myositis Pilot Study Mazen Dimachkie, Pedro Machado, Jianghua He, Yunxia Wang, April McVey, Mamatha Pasnoor, Philip Gallagher, Laura Herbelin, Jeffrey Statland, Adrian Miller, Linda Greensmith, Janice Holton, Michael Hanna, Richard Barohn 3:30 p.m. S16.002 Phase II Trial of Methotrexate in Myathenia Gravis Mamatha Pasnoor, Laura Herbelin, Jianghua He, Mazen Dimachkie, Sharon Nations, Vera Bril, Annabel Wang, John Kissel, Ted Burns, David Saperstein, Jeffrey Rosenfeld, Aziz Shaibani, Carlayne Jackson, Andrea Swenson, James Howard, Namita Goyal, Matthew Wicklund, Joann Miller, Richard Barohn, MSG Methotrexate Study MG Group 3:45 p.m. S16.003 A Single-Blind, Randomized, Controlled Clinical Trial of Exercise in Ambulatory Spinal Muscular Atrophy (SMA) Patients Jacqueline Montes, Samantha Kramer, Sally Dunaway, Megan Montgomery, Brendan Carr, Shirit Rosenberg, Douglas Sproule, Nancy Strauss, Carol Garber, Darryl De Vivo 4:00 p.m. S16.004 Is IVIg Therapy Warranted in Progressive Lower Motor Neuron Syndromes Without Conduction Block? Neil Simon, Gretchen Ayer, Catherine Lomen-Hoerth 4:15 p.m. S16.005 The Effect of Tirasemtiv on Functional Status in Patients with ALS Jeremy Shefner, Jacqueline Lee, Donna Barragan, Lisa Meng, Andrew Wolff, Jinsy Andrews 4:30 p.m. S16.006 Randomized Trial of Rifampicin in MSA: Effect on Autonomic Function Wolfgang Singer, William Cheshire, Robert Fealey, Paola Sandroni, J. Ahlskog, Joseph Matsumoto, James Bower, Melinda Burnett, Andrew McKeon, Tonette Gehrking, Jade Gehrking, Eduardo Benarroch, Phillip Low 4:45 p.m. S16.007 Neuropathy Improvement Following Peripheral Blood Stem Cell Transplantation for POEMS Syndrome. Chafic Karam, Christopher Klein, Angela Dispenzieri, Jayawant Mandrekar, P. James B. Dyck, Anita D’Souza, Michelle Mauermann 2O14 Scientific Abstract Listing and Annual Meeting Information S17 Parkinson's Disease: Genetics and Epidemiology 3:15 p.m. S17.001 Mutations in the GCH1 Gene Are Associated with Parkinson Disease Niccolò Mencacci, Ioannis Isaias, Martin Reich, Christos Ganos, James Polke, Jose Bras, Joshua Hersheson, Maria Stamelou, Alan Pittman, Alastair Noyce, Kin-Ying Mok, Thomas Opladen, Erdmute Kunstmann, Katie Sidle, Mary Sweeney, Henry Houlden, Hodecker Sybille, Amit Batla, Alexander Munchau, Jens Volkmann, Samuel Samnick, Giorgio Marotta, Anna Zecchinelli, Gianni Pezzoli, Andrew Lees, Paulo Alegria, Paul Krack, Florence Cormier, Suzanne Lesage, Alexis Brice, Peter Heutink, Thomas Gasser, Huw Morris, Steven Lubbe, Elisa Majounie, Raphael Gibbs, Andrew Singleton, John Hardy, Stephan Klebe, Kailash Bhatia, Nicholas, W Wood, None International Parkinson’s Disease Genomics Consort 3:30 p.m. S17.002 Age Specific Penetrance of the LRRK2 G2019S Mutation in the Michael J Fox Ashkenazi Jewish (AJ) LRRK2 Consortium Karen Marder, Mingxin Tang, Roy Alcalay, Helen Mejia-Santana, Deborah Raymond, Anat Mirelman, Rachel SaundersPullman, Lorraine Clark, Laurie Ozelius, Avi Orr-Urtreger, Nir Giladi, Susan Bressman 3:45 p.m. S17.003 RER1: A Novel Regulator of AlphaSynuclein Nikolaus McFarland, Hyo-Jin Park, Lauren Ricchiuti 4:00 p.m. S17.004 Apolipoprotein A1 Levels Are Associated with APOA1 Promoter Variation and Influence Parkinson’s Disease Risk Christine Swanson, Katherine Li, Travis Unger, Michael Gallagher, Vivianna Van Deerlin, Pinky Agarwal, James Leverenz, John Roberts, Ali Samii, Rachel Goldmann Gross, Howard Hurtig, Jacqueline Rick, Daniel Weintraub, John Trojanowski, Cyrus Zabetian, Alice Chen-Plotkin 4:15 p.m. S17.005 Prevalence and Predictors of AntiParkinson Drug Use in a Nationally Representative Sample of Medicare Beneficiaries, 2006-2010 Nabila Dahodwala, Allison Willis, Pengxiang Li, Jalpa Doshi 4:30 p.m. S17.006 Serum Cholesterol, Statin, and Parkinson’s Risk in the Atherosclerosis Risk in Communities (ARIC) Study Xuemei Huang, Alvaro Alonso, Xuguang Guo, David Umbach, Richard Mailman, Thomas Mosley, Honglei Chen 4:45 p.m. S17.007 Time Trends in the Incidence of Parkinsonism and Parkinson Disease in Olmsted County, Minnesota Over Thirty Years Rodolfo Savica, Brandon Grossardt, James Bower, J. Ahlskog, Walter Rocca S18 Aging, Dementia, and Cognitive and Behavioral Neurology: Behavioral Neuroscience 3:15 p.m. S18.001 Neuroeconomic Measures of Impaired Decision-Making in Frontotemporal Dementia Winston Chiong, Kristie Wood, Andrew Kayser, Mark D’Esposito, Howard Rosen, Bruce Miller, Joel Kramer 3:30 p.m. S18.002 Strategic Problem Solving in Behavioral Variant Frontotemporal Dementia Laura Baehr, Corey McMillan, Katya Rascovsky, John Powers, Lisa Burkholder, Murray Grossman 3:45 p.m. S18.003 A CSF Signature of Frontotemporal Lobar Degeneration with C9orf72 Repeat Expansions William Hu, Jonathan Glass, Vivianna Van Deerlin, Murray Grossman, Kelly Watts, James Lah, John Trojanowski, Allan Levey 4:00 p.m. S18.004 Cholinergic Integrity and Visual Hallucinations in Parkinson Disease Nicolaas Bohnen, Martijn Muller, Vikas Kotagal, Roger Albin, Kirk Frey 4:15 p.m. S18.005 Neuropsychological Profiles of Voltage-gated Potassium Channel Complex and Other Autoimmune Encephalopathies; More Than Memory Impairment Michael Geschwind, Jeffrey Gelfand, Sarosh Irani, John Neuhaus, Sven Forner, Brianne Bettcher 4:30 p.m. S18.006 Predictors of Response to Propranolol for Social Functioning in Autism Spectrum Disorder David Beversdorf, Rachel Zamzow, Brad Ferguson, Tamera Martin, Morgan Lewis, Janine Stichter 4:45 p.m. S18.007 SHANK3 Overexpression Causes Manic-like Behavior with Unique Pharmacogenetic Properties Jimmy Holder, Huda Zoghbi Scientific Sessions 3:15 p.m. S19.001 Good Vibrations: A Novel Method of Damping Acquired Pendular Nystagmus with Vibration Shin Beh, Amir Kheradmand, Teresa Frohman, Darrel Conger, Amy Conger, Peter Calabresi, Laura Balcer, Elliot Frohman, David Zee 3:30 p.m. S19.002 A Novel Quantitative Bedside Test of Balance Function: the Video Visually Enhanced Vestibulo-ocular Reflex (VVOR) David Szmulewicz, Hamish MacDougall, Elsdon Storey, Ian Curthoys, Michael Halmagyi 3:45 p.m. S19.003 Alice in Wonderland Syndrome: Presenting and Follow-up Characteristics Grant Liu, Alessandra Liu, Jonathan Liu, Geraldine Liu 4:00 p.m. S19.004 Eye Movement Perimetry for Evaluation of Visual Field Loss in Patients with Glaucoma and Recovered Optic Neuritis Matthew Thurtell, David Warren, Alice Xu, Andrew Papendieck, Michael Wall 4:15 p.m. S19.005 Evaluation of Face and Voice Perception and Recognition Impairments in Prosopagnosia Ran (Richard) Liu, Raika Pancaroglu, Charlotte Hills, Bradley Duchaine, Jason Barton 4:30 p.m. S19.006 Vision Testing Is Additive to the Sideline Assessment of SportsRelated Concussion Rachel Ventura, Zoe Marinides, Steven Galetta, James Clugston, Laura Balcer 4:45 p.m. S19.007 Capturing Episodic Vertigo Miriam Welgampola, Corinna Lechner, Hamish Macdougall, Michael Halmagyi S20 Pain and Palliative Care 3:15 p.m. Presentation of Mitchell B. Max Award for Neuropathic Pain Recipient: Kathleen Foley, MD New York, NY 3:30 p.m. S20.002 ALS: Pain in Addition to Anything Else Nathalie Guy, Catherine Cornut Chauvinc, Xavier Moisset, Pierre Clavelou 3:45 p.m. S20.003 Identifying Palliative Care Needs in the Neurological Intensive Care Unit Claire Creutzfeldt, J Curtis 4:00 p.m. S20.004 DS-5565 for the Treatment of Diabetic Peripheral Neuropathic Pain: Randomized, Double-Blind, Placeboand Active Comparator-controlled Phase II Study Aaron Vinik, Uma Sharma, Karen Feins, Ching Hsu, Domenico Merante 4:15 p.m. S20.005 Peripheral Edema and Weight Gain in Adult Patients with Painful Diabetic Peripheral Neuropathy (DPN) Receiving Gabapentin Enacarbil (GEn) or Pregabalin Enrolled in a Randomized Phase 2 Trial Anne Calkins, Joseph Shurman, Mark Jaros, Richard Kim, Gwendoline Shang 4:30 p.m. S20.006 Botulinum Toxin for Muscle Cramps Associated with Diabetic Neuropathy: A DoubleBlind, Placebo-Controlled Study Domenico Restivo, Antonino Pavone, Damiano Gullo, Stefano Jann, Riccardo Vigneri 4:45 p.m. S20.007 Virtual Family Meetings in the ICU Setting: Results from an Audiovisual Conferencing Intervention Adam de Havenon, Casey Petersen, Ali Sultan-Qurraie, Robert Hoesch S21 Neuro-rehabilitation and Neural Repair S22 Neuro-oncology 3:15 p.m. S21.001 Randomized Controlled Trial of Constraint-induced Aphasia Therapy in Patients with Chronic Stroke Jerzy Szaflarski, Jane Allendorfer, Angel Ball, Christi Banks, Aimee Dietz, Kimberly Hart, Christopher Lindsell, Amber Martin, Jennifer Vannest 3:15 p.m. S22.001 A Vaccine Targeting Mutant IDH1 Induces Antitumor Immunity Michael Platten, Theresa Schumacher, Lukas Bunse, Felix Sahm, Stefan Pusch, Jasmin Quandt, Oliver Menn, Matthias Osswald, Angelika Riemer, Philipp Beckhove, Manuel Alexander Friese, Andreas von Deimling, Wolfgang Wick 3:30 p.m. S21.002 Measuring Health-related Quality of Life (HRQOL) During Inpatient Stroke Rehabilitation Pasquale Frisina, Ann Kutlik, Kimberly Hreha, A. Barrett 3:30 p.m. S22.002 Neurocognitive Function (NCF) Substudy and Mini-Mental State Examination (MMSE) Results from the Randomized, Placebo-Controlled Phase III AVAglio Trial of Bevacizumab (BEV) Added to Radiotherapy (RT) and Temozolomide (TMZ) for Newly Diagnosed Glioblastoma Jeffrey S Wefel, Olivier Chinot, Wolfgang Wick, Warren Mason, Roger Henriksson, Frank Saran, Ryo Nishikawa, Cedric Revil, Josep Garcia, Timothy Cloughesy 3:45 p.m. S21.003 Brain Structural and Functional Changes After Action Observation Therapy in Parkinson’s Disease Patients with Freezing of Gait Federica Agosta, Elisa Canu, Elisabetta Sarasso, Mariano Gemma, Alessandro Meani, Antonietta Volonté, Lidia Sarro, Sebastiano Galantucci, Andrea Falini, Giancarlo Comi, Roberto Gatti, Massimo Filippi 4:00 p.m. S21.004 Neuroprotective and Neurorestorative Effects of Thymosin Beta4 Treatment After Traumatic Brain Injury Asim Mahmood, Ye Xiong, Michael Chopp 4:15 p.m. S21.005 Recovery from Brain Injury After Prolonged Disorders of Consciousness: Outcome of Patients Admitted to Rehabilitation with 1-8 Year Follow-up Douglas Katz, Meg Polyak, Daniel Coughlan, Emily Goff, Meline Nichols, Alexis Roche 4:30 p.m. S21.006 Comparison of the Checkerboard P300 Speller Versus the Row-Column Speller in Normal Elderly and an Aphasic Stroke Population Jerry Shih, George Townsend, Dean Krusienski, Kevin Shih, Ryan Shih, Kristin Heggeli, Trevor Paris, James Meschia 4:45 p.m. S21.007 Individualized Treatment with Transcranial Direct Current Stimulation in Patients with Chronic Nonfluent Aphasia Due to Stroke Priyanka Shah, Catherine Norise, Gabriella Garcia, Jose Torres, Olu Faseyitan, Roy Hamilton 3:45 p.m. S22.003 Overview of Arterial Thromboembolic Events (ATEs) in AVAglio, a Randomized, Placebo-controlled Phase III Trial of Bevacizumab, Radiotherapy and Temozolomide (BEV+RT/TMZ) for Newly Diagnosed Glioblastoma Warren Mason, Timothy Cloughesy, Wolfgang Wick, Roger Henriksson, Frank Saran, Ryo Nishikawa, Sunita Dhar, Cedric Revil, Josep Garcia, Olivier Chinot 4:00 p.m. S22.004 Predicting Progressive Gangliogliomas: Early Identification of Those at Risk in a Sample of 156 Consecutive Patients Treated at the Barrow Neurological Institute Glynnis Zieman, Christopher Dardis, Andrea Gomes, Adrienne Scheck, Jennifer Eschbacher, Lynn Ashby 4:15 p.m. S22.005 The Neurologic Assessment in Neuro-Oncology (NANO) Scale: A Tool to Assess Neurologic Function for Integration in the Radiologic Assessment in Neuro-Oncology (RANO) Criteria Lakshmi Nayak, Lisa DeAngelis, Patrick Wen, Alba Brandes, Riccardo Soffietti, Nancy Lin, David Peereboom, Marc Chamberlain, David Macdonald, Evanthia Galanis, James Perry, Kurt Jaeckle, Minesh Mehta, Roger Stupp, Martin Van Den Bent, David Reardon 4:30 p.m. S22.006 Improved Progression Free Survival in 1p/19q Co-deleted Anaplastic Oligodendroglioma Treated with Both Chemotherapy and Radiation Therapy at Diagnosis Jacob Mandel, Courtney Webre, Nicole Shonka, W K Yung, John De Groot S23 MS and CNS Inflammatory Disease: Novel Therapeutics 3:15 p.m. Presentation of John Dystel Prize for Multiple Sclerosis Research Recipient: Barry Arnason, MD Chicago, IL 3:45 p.m. S23.003 A Combination Trial of Estriol Plus Glatimer Acetate in Relapsing-Remitting Multiple Sclerosis Rhonda Voskuhl, HeJing Wang, T.C. Jackson Wu, Nancy Sicotte, Angela Bates, Gary Beaver, John Corboy, Anne Cross, Suhayl Dhib-Jalbut, Corey Ford, Barbara Giesser, Dina Jacobs, Sharon Lynch, Andrew Pachner, Michael Racke, John Ratchford, Anthony Reder, John Rose, Dean Wingerchuk, Margaret Burnett, Chi Hong Tseng, Robert Elashoff 4:00 p.m. S23.004 Effect of Alfacalcidol on Fatigue in MS Patients: A Randomized, Doubleblind Study Yoram Barak, David Magalashvili, Mark Dolev Dolgopiat, David Ladkani, Dalia Nitzani, Zeev Mazor, Anat Achiron 4:15 p.m. S23.005 STREAMS: A Phase 2 Clinical Trial of Autologous Mesenchymal Stem Cells in Active Multiple Sclerosis Rehiana Ali, Stephen Marley, Renuka Palanicawandar, Francesco Dazzi, Richard Nicholas, Paolo Muraro 4:30 p.m. S23.006 The MIRROR Study: A Randomized, Double-blind, Placebo-controlled, Parallel-group, Dose-ranging Study to Investigate the Safety and MRI Efficacy of Subcutaneous Ofatumumab in Subjects with Relapsing-Remitting Multiple Sclerosis (RRMS) Amit Bar-Or, Richard Grove, Daren Austin, Jerry Tolson, Susan Vanmeter, Eric Lewis, Per Solberg Sorensen 4:45 p.m. S23.007 Randomized Controlled Trial of CI Therapy for Progressive MS: Increased Real-world Function and Neuroplasticity on MRI Victor Mark, Edward Taub, Gitendra Uswatte, Gary Cutter, David Morris, Staci McKay, Mary Bowman, Michelle Haddad, Tyler Rickards, Chelsey Sterling 4:45 p.m. S22.007 Ionizing Radiation Arrests Subventricular Zone Neural Precursors in G2/M without Affecting Long-Term Self-Renewal Hongxin Chen, Sonia De Toledo, Matthew Goodus, Azzam Edward, Steve Levison, Nizar Souayah Fast, Easy Registration Online · AAN.com/view/AM14 79 Tuesday April 29 S19 Neuro-ophthalmology/ Neuro-otology I Tuesday, April 29 Current as of 2/13/2014 Hot Topics Plenary Session 5:30 p.m.–6:30 p.m. F eatures translational research related to clinical issues of importance. Four outstanding physician-scientists provide summaries of their recent research findings and describe the clinical implications of the results. Moderator: Aleksandar Videnovic, MD, MSc Member, Science Committee Identification of a Unique Molecular and Functional Microglia Signature in Health and Disease Oleg Butovsky, PhD Brigham and Women’s Hospital/Harvard Medical, Boston, MA The Global Epidemic of Stroke: Sounding the Alarm Jerome H. Chin, MD, PhD, MPH Alliance for Stroke Awareness and Prevention Project (ASAPP), San Anselmo, CA Emerging Concepts in Chronic Traumatic Encephalopathy Dennis W. Dickson, MD Mayo Clinic, Jacksonville, FL Functional Connectivity and Functional Imaging in Movement Disorders David Eidelberg, MD, FAAN Feinstein Institute for Medical Research, Manhasset, NY For Full Abstracts and Bios for Plenary Speakers Visit AAN.com/view/SearchAM 80 2O14 Scientific Abstract Listing and Annual Meeting Information Wednesday, April 30 Poster Session IV P4 Poster Session IV First Authors stand by Posters from 7:30 a.m.–9:00 a.m. 7:30 a.m.–11:00 a.m. Poster Discussion Session: MS and CNS Inflammatory Disease I Utilizing a guided tour format, topic experts will lead attendees around the ten posters in the poster discussion session and facilitate questions with poster authors during the 90-minute author stand-by time. Autologous Hematopoietic Stem Cell Transplantation in Neuromyelitis Optica Jodie Burton, Jan Storek, Fiona Costello, Peter Duggan, Luanne Metz P4.002 Rate Evaluation of 25-Hydroxy-Vitamin D in Neuromyelitis Optica Laurent Kremer, Ilhame Slassi Sennou, Nada Benkirane, Adil Araqi Houssaini, Nicolas Collongues, Jean Baptiste Chanson, Frederic Blanc, MarieCéline Fleury, Arnaud Theulin, Rose-Marie Javier, Jerome De Seze P4.003 Laquinimod Prevents NMOIginduced Disease Exacerbation in a Model of Neuromyelitis Optica. Azeb Argaw, Linnea Asp, Jingya Zhang, Patrick Waters, Liat Hayardeny Nisimov, Michael Levy, Gareth John P4.004 Trial of C1-Esterase Inhibitor in Acute Relapses of Neuromyelitis Optica Michael Levy, Maureen Mealy P4.005 Analysis of the Treatment of Neuromyelitis Optica at the Hospital of the University of Pennsylvania Jose Torres, Amy Pruitt, Clyde Markowitz, Nabila Dahodwala P4.006 Adoptive Transfer of T-cells Reactive to Aquaporin-4 Creates Neuromyelitis Optica Mouse Model Michael Levy, Melina Jones, Hwa Huang, Maureen Mealy P4.007 The Largest Genomics Study of NMO in History: Whole Genome Sequencing of 150 Patients with Neuromyelitis Optica Benjamin Greenberg, Douglas Kerr, Tim Harris, Aaron DayWilliams, John Carulli P4.008 Typical and Atypical Initial Presentations of Neuromyelitis Optica: A Retrospective Study Juebin Huang, Burhan Chaudhry, Kimberly McDonald, V Vedanarayanan, Colette Parker, James Corbett, Robert Herndon P4.009 The Spectrum of Brain MRI Abnormalities in Neuromyelitis Optica Spectrum Disorders Juebin Huang, Burhan Chaudhry, Kimberly McDonald, V Vedanarayanan, Colette Parker, James Corbett, Robert Herndon P4.010 Neuromyelitis Optica and Neuromyelitis Optica Spectrum Disorders: The Evaluation of 70 Patients Followed by Istanbul Bilim University, Department of Neurology Burcu Altunrende, Ayca Altınkaya, Baris Topcular, Kocaslan Meryem, Sadik Server, Sinem Firtina, Sedef Yenice, Gulsen Akman-Demir NEW! e Poster Session: Aging, Dementia, and Cognitive and Behavioral Neurology II The ePoster session will feature a selection of posters to be presented digitally, rather than in the traditional format. Authors will be able to take advantage of the format to highlight compelling visual features such as images and videos. See poster map on page 47 for location. P4.011 PET Amyloid Imaging with Florbetapir Predicts Cognitive Decline in the Oldest-Old Dana Greenia, Claudia Kawas, Michelle Caunca, Szofia Bullain, Maria Corrada P4.012 Assessing Brain System Dysfunction in Amnesic Mild Cognitve Impairment Through MRI-based Connectomics Federica Agosta, Elisa Canu, Sebastiano Galantucci, Alessandro Meani, Giuseppe Magnani, Alessandra Marcone, Andrea Falini, Giancarlo Comi, Massimo Filippi P4.013 Cerebral Blood Flow and White Matter Hyperintensities in Nondemented Elderly Lisa Silbert, Hiroko Dodge, David Lahna, Nutta-on Promjunyakul, William Rooney, Deniz ErtenLyons, Jeffrey Kaye P4.014 Genetic Influences of Survival in the Behavioral Variant of Frontotemporal Degeneration David Irwin, Corey McMillan, Eunran Suh, Katya Rascovsky, Jon Toledo, Virginia Lee, John Trojanowski, Vivianna Van Deerlin, Murray Grossman P4.015 Utility of Amyloid Neuroimaging in Clinical Practice Patricio Chrem Mendez, Gabriela Cohen, Julieta Russo, Marcos Fernandez Suarez, Jorge Campos, Griselda Russo, Janus Kremer, Alejandra Amengual, Silvia Vazquez, Ramon Leiguarda, Gustavo Sevlever, Ricardo Allegri P4.016 Improved Accuracy of the Diagnosis of Early Alzheimer’s Disease Using Combined Measures of Hippocampal Volume and Sulcal Morphology Lorraine Hamelin, Cruz de Souza Leonardo, Fabian Corlier, Helene Corne, Marie Chupin, Bruno Dubois, Michel Bottlaender, Olivier Colliot, Marie Sarazin P4.017 Presence of Microinfarcts at Autopsy Is Associated with Increased Rate of Gray Matter Atrophy on Antemortem MRI Mekala Raman, Matthew Senjem, Jeffrey Gunter, Scott Przybelski, Prashanthi Vemuri, Melissa Murray, Bradley Boeve, David Knopman, Ronald Petersen, Joseph Parisi, Dennis Dickson, Clifford Jack, Kejal Kantarci P4.018 Longitudinal Patterns of Brain Atrophy in Frontotemporal Lobar Degeneration Clinical Syndromes Compared with Alzheimer’s Disease Pilar Ferraro, Federica Agosta, Elisa Canu, Giuseppe Magnani, Alessandra Marcone, Andrea Falini, Giancarlo Comi, Massimo Filippi P4.019 White-Matter Evidences of Corticospinal Pathway Involvement in Frontotemporal Dementia Chiara Crespi, Chiara Cerami, Alessandra Dodich, Alessandra Marcone, Nicola Canessa, Sandro Iannaccone, Massimo Corbo, Christian Lunetta, Elisa Scola, Andrea Falini, Stefano Cappa P4.020 Whole Brain, Voxel Level Analysis of Grey Matter Volume and Time to Incident Mild Cognitive Impairment or Alzheimer’s Disease Lubov Zeifman, William Eddy, Oscar Lopez, Lewis Kuller, Cyrus Raji, James Becker Fast, Easy Registration Online · AAN.com/view/AM1481 Wednesday April 30 P4.001 Wednesday, April 30 General Neurology III P4.021 Lumbar Spine Manifestation of Intracranial Hypotension Brion Reichler, Darius Melisaratos P4.022 Case Report—Multi-focal Intracranial Tuberculoma in the Setting of Miliary TB in an Immunocompetent Patient Ali Saeed, Gautam Sachdeva, Syed Hussain P4.023 Anti-NMDA Receptor Encephalitis Presenting with Atrial Fibrillation Olha Taraschenko, Josep Dalmau, Earl Zimmerman, Mary Ann McKee P4.024 The Gender Divide in Multiple Sclerosis: A Review of the Environmental Factors Influencing the Increasing Prevalence of Multiple Sclerosis in Women Rebecca Klein, Jodie Burton P4.025 Population Based Study of Co-Morbidity of Neurological Autoimmune Diseases and Thyroid Disease in Buenos Aires, Argentina Andres Villa, Florencia Aguirre, Luciana Melamud, Marianna Di Egidio, Ricardo Alonso, Raul Rey P4.026 Lupus-Associated Transverse Myelitis Masquerading as Septic Shock Rahul Dave, Ciro Ramos Estebanez P4.027 Third Ventricular Tumors and Sudden Deterioration: Is Coronary Vasospasm a Missing Link? Marissa Kellogg, Holly Hinson P4.028 Hypoxic Ischemic Brain Injury Following in Hospital Cardiac Arrest— Lessons from Autopsy Harsh Gupta, Archana Hinduja, Sanjeeva Onteddu, Ju Dong Yang P4.029 Multiple Cranial Neuropathy in Paraneoplastic Anti-Hu Antibody Syndrome Thomas Schmidt, Andrew Solomon P4.030 Dysganglionosis as a Cause of Idiopathic Gastroparesis. A New Way to its Diagnosis and Treatment Ulrich Liebetrau, Volker Limmroth, Carl Eisenberger, Anke Brunn, A.J. Dormann P4.031 Quality of Life in Liver Transplant Patients with Neurologic Complications. Maria Gonzalez Toledo, Analia Calle, Fatima Pagani Cassara, Agustina Tamargo, Alejandro Thomson, Diego Nadile, Fernando Gruz, Vladimiro Sinay P4.032 Brain and Liver Iron Accumulation Demonstrated by 1.5-tesla and 3-tesla MRI in Aceruloplasminemia Koji Fujita, Yusuke Osaki, Masafumi Harada, Satoshi Kono, Hiroaki Miyajima, Yuishin Izumi, Ryuji Kaji P4.033 Akinetic Mutism and Parkinsonian Features Progressing to Coma Following a Hypoxic Event with Extended Lucid Interval: Manifestations of Delayed Post-hypoxic Leukoencephalopathy Alden P. Doerner Rinaldi, Eliza Miller, Barry Czeisler, Joshua Willey, Crary John, Jan Claassen, Stephan Mayer, Sachin Agarwal 82 P4.034 A Winged Scapula and Dropped Wrist: Cervical Radiculomyelopathy as an Unusual Presenting Manifestation of Copper Deficiency Sajish Jacob, Harsh Gupta, Robert Archer, Betul Gundogdu P4.035Metachromatic Leukodystrophy Mistaken for Manganese Toxicity in a Patient with Common Variable Immunodeficiency: A New Triad of Devastating Disease? Zubair Ahmed, Hesham Abboud, Edward Manno P4.036 Treatment of Post-Influenza Vaccination-induced Acute Disseminated Encephalomyelitis (ADEM) with Plasma Exchange—a Case Report Mandeep Chahil, Clement Pillainayagam, Paul Schulz P4.037 A Rare Case of Churg Strauss Syndrome associated with Cervical Spine and Brain Involvement Shilpi Mittal, Agnes Acsadi, Lorinda Cruz, Taylor Aglio, Kirsten Ek, Santhanam Lakshminarayanan, Kristen Logee P4.038 Neurology Telemedicine Interest in Arkansas L Greenfield, Maryam Bashiri, Sukanthi Kovvuru P4.039 Subacute Sclerosing Panencephalitis: Case study and Literature Review Danny Estupinan, Nikolaus McFarland P4.040 Thoracic Myelopathy Due to Hypertrophic Pachymeningitis Secondary to Adalimumab Yefim Yushvayev-Cavalier, Warren Zeigler, Mary Ann McKee, Marjorie Bunch, Adolfo Ramirez Zamora Movement Disorders: Parkinson’s Disease Biomarkers P4.041 Longitudinal Quantitative EEG Changes Correlate With Neuropsychological Assessment Decline John Caviness, Joe Hentz, Erika Driver-Dunckley, Christine Belden, Jessica Powell, Michael Ahmadi, Charles Adler P4.042 Glucocerebrosidase Enzyme Activity in GBA1 Mutation Parkinson Disease Robert Ortega, Paola Torres, Sarah Boschung, Matthew Swan, Jeannie Soto-Valencia, Matthew Barrett, Brooke Johannes, Deborah Raymond, Lawrence Severt, Vicki Shanker, Susan Bressman, Gregory Pastores, Rachel Saunders-Pullman P4.043 The BioFIND Study (Fox Investigation For New Discovery Of Biomarkers In Parkinson’s Disease): Design And Methodology Un Kang, Roy Alcalay, Jennifer Goldman, Claire Henchcliffe, Penelope Hogarth, Paul Tuite, Tao Xie, Mark Frasier, Catherine Kopil, Lona Vincent, Nicole Willis, Cindy Casaceli, Alice Rudolph P4.044 Evaluation of the Cutaneous Silent Period in Patients with Parkinson’s Disease Serdar Tasdemir, Hakan Akgun, Mehmet Yucel, Semih Alay, Oguzhan Oz, Umit Ulas, Seref Demirkaya P4.045 Association of Serum Cystatin C Levels on the Progression and Cognition in Parkinson’s Disease Jing Chen, Chunfeng Liu 7:30 a.m.–11:00 a.m. P4.046 Defining Impaired Olfaction in Parkinson’s Disease: a Comparison of Methods. Katherine Grosset, Naveed Malek, Sarah Marrinan, Nin Bajaj, Waiken Chan, Christina Banks, Huw Morris, Roger Barker, Thomas Foltynie, Nicholas, W Wood, Nigel Williams, Yoav Ben-Shlomo, David Burn, Donald Grosset P4.047 An Aptamer-Based Screen of 1000+ Plasma Proteins for Diagnostic Biomarkers in Parkinson’s Disease Benjamine Liu, Christine Swanson, Jacqueline Rick, Daniel Weintraub, Howard Hurtig, John Trojanowski, Alice Chen-Plotkin P4.048 Plasma Long Chain Fatty Acids and Cognition in Parkinson’s Disease Charles Murchison, Joseph Quinn, Brenna Cholerton, James Leverenz, Thomas Montine, Cyrus Zabetian, Kathryn Chung, Amie Peterson, Gene Bowman Movement Disorders: Biomarkers and Treatment P4.049 In Vivo Gastric Detection of α-Synuclein Inclusions in Parkinson’s Disease Alvaro Sanchez, Alberto Rabano, Maria-Jose Catalan, Fernando Canga, Servando Fernandez-Diez, Jaime Herreros-Rodriguez, Elvira Garcia-Cobos, Marina Mata Alvarez-Santull, Lydia LopezManzanares, Mosqueira Antonio J, Lydia Vela, Juan Lopez-Lozano, Eva Lopez-Valdes, Jose Antonio Molina P4.050 Reduction in Post-Botulinum Toxin Flu-like Symptoms After Injection with Incobotulinum Toxin Edwin George, Natalya Shneyder P4.051 Antibody Mediated Movement Disorders and Their Differential Response to Immunomodulatory Therapy Laura Bishop, Mustafa Siddiqui, Jessica Tate, Ihtsham Haq P4.056 Physical Activity and Risk of Comorbid Depression with Parkinson Disease Rui Liu, David Umbach, Yikyung Park, Xuemei Huang, Albert Hollenbeck, Aaron Blair, Honglei Chen P4.057 Hereditary Spastic Paraplegia Due to a Novel Mutation in SPG11 Gene Presenting as Dopa Responsive Dystonia, Parkinsonism and Spasticity Subhashie Wijemanne, Joseph Jankovic P4.058 The Relationship Between Motor Symptom Lateralization and NonMotor Symptoms (NMS) in Parkinson’s Disease Patients Tarannum Khan, Raja Boddepalli, Denny Reyes Movement Disorders: Hyperkinetic Disorders: Chorea and Tic Disorders P4.059 Acute Recurrent, Persistent Hypoglycemia-induced Chorea/Ballism in a Diabetic Patient on Hemodialysis Padmaja Vittal, Cynthia Comella, Kathleen Shannon P4.060 Clinical Pyramidal Signs in a Series of Patients with Huntington’s Disease Emilia Gatto, Virginia Laura Parisi, Ana Sanguinetti, Jose Luis Etcheverry, Gabriel Persi P4.061 Estimating Huntington’s Disease (HD) Onset Using a Low-Cost Balance Assessment Andrew Herndon, Jody Corey-Bloom, Marcella Scholl, Danielle Burt, Sean Huynh, Daniel Goble P4.062 Estimate Huntington Disease Prevalence in Latin America Emilia Gatto, Virginia Laura Parisi, Ana Sanguinetti, Gabriel Persi, Jose Luis Etcheverry P4.063 P4.052 Primary CNS Lymphoma Presenting with a Rapidly Progressive Huntington’s Disease-Like Picture Hesham Abboud, Mohamed Hegazy, Rebecca Kuenzler, David Peereboom P4.053 P4.065 A Comprehensive Approach to Parkinson’s Disease Camille Vaughan, Anna Vandenberg, Felicia Goldstein, Lynn-Marie Trotti, Adriana Hermida, Mary Weeks, Stewart Factor Safety and Efficacy Study of ADS-5102 (amantadine HCl) Extended Release Capsules in Levodopa-Induced Dyskinesia (EASED Study) Rajesh Pahwa, Caroline Tanner, Robert Hauser, Kapil Sethi, Stuart Isaacson, Daniel Truong, Lynn Struck, Mary Jean Stempien, Natalie McClure, Greg Went P4.054 Economic Burden of Parkinson´s Disease in a Population of Monterrey, Mexico Leonel Cantu-Martinez, Jesus Santos-Guzman, Ingrid EstradaBellman, Ramiro Mora-Villalvazo, Erika Salinas-Lezama, Hector Martinez P4.055 Dietary Source of Vitamin D Is Associated with Parkinson Disease and Total Vitamin D Modifies the Genetic Association Between Vitamin D Receptor (VDR) Gene and Parkinson Disease Liyong Wang, Jeffery Vance, Marian Evatt, Lizmarie Maldonado, William Perry, James Ritchie, Gary Beecham, Eden Martin, Jonathan Haines, Margaret Pericak-Vance, William Scott 2O14 Scientific Abstract Listing and Annual Meeting Information P4.064 Psychogenic Movement Disorders in Nonagenarians: Report of Two Cases Stephen Reich, Melissa Armstrong, Ana Sanchez, Roy Fried A Case of Psychogenic Belching Rainer Paine, Mark Hallett P4.066 Social Functioning in Youth with Tourette Syndrome Sarah Pearl Aronow-Werner, Heather Adams, Amy Vierhile, Alyssa Thatcher, Jonathan Mink, Erika Augustine P4.067 Increased Dopamine Receptor Occupancy in People with Tourette Syndrome, Obsessive-Compulsive Disorder, and Neuroleptic Exposure James Brasic, Harvey Singer, Eram Zaidi, Emily Gean, Anil Kumar, Anil Mathur, Rebecca MellingerPilgrim, Vanessa Raymont, Ahmet Dogan, Mohab Alexander, Marika Maris, Gerald Nestadt, Albert Gjedde, Dean Wong Movement Disorders: Essential and Other Tremors P4.068 Clinical and Surface Electromyography (SEMG) Correlation in Tremors Man Mohan Mehndiratta, Munish Kumar, Sanjay Pandey, Dinesh Sharma Poster Session IV P4.069 Decreased EAAT2 Protein Expression in the Essential Tremor Cerebellar Cortex Sheng-Han Kuo, Michelle Lee, Etty Cortes, Jean Paul Vonsattel, Elan Louis, Phyllis Faust P4.070 Genome-Wide Linkage Scan for Essential Tremor: The FASET Study Lorraine Clark, Nora Hernandez, Ruth Ottman, Iuliana Ionita-Laza, Elan Louis P4.071 Case Control Analysis of Spinocerebellar Ataxia (SCA) Loci Repeat Expansion Size in Essential Tremor (ET) Lorraine Clark, Xinmin Liu, Xin Ye, Nora Hernandez, Ruth Ottman, Iuliana IonitaLaza, Elan Louis P4.072 Tacrolimus-Induced Tremor: Switching from Immediate-release (IR-TAC) to LCP-Tacro Extended-release Tacrolimus (LCPT) Reduces Tremor and Improves Quality of Life John Morgan, Anthony Langone, Vincenza Nigro, Shyamal Mehta, Kapil Sethi P4.073 Shaky Handwriting: What Is the Rate of Decline During Prospective Follow-up of Essential Tremor? Elan Louis, Monika Michalec, Art Gillman P4.074 Case Study: First Reported Case of Interferon-alpha Induced Postural and Action Tremor David Rydz, Madeleine Sharp, Stanley Fahn P4.081 Eighteen Month Experience with Diaphragmatic Pacing in ALS: Outcomes, Efficacy and Adversities Margaret Allred, Robert Baloh, Ashraf Elsayegh, Evgeny Tsimerinov, Abirami Muthukumaran, Anishee Shah, Richard Lewis P4.090 P4.082 P4.091 Effects of Cough Augmentation on Pulmonary Morbidity, Survival, and Quality of Life in Patients with Amyotrophic Lateral Sclerosis in Respiratory Failure: A Randomised Trial Muhammad Rafiq, Michael Bradburn, Alison Proctor, Christopher McDermott, Pamela Shaw P4.083 Phrenic Nerve Conduction Studies as a Biomarker of Respiratory Insufficiency in ALS Liberty Jenkins, Sarada Sakamuri, Jonathan Katz, Dallas Forshew, Lee Guion, Dan Moore, Robert Miller P4.084 Vitamin D Is a Prognostic Factor of Amyotrophic Lateral Sclerosis and Confers Protection to Motoneurons in Vitro Camu William, Boris Tremblier, Carine Plassot, Sebastien Alphandery, Celine Salsac, Nicolas Pageot, Raul JuntasMorales, Frederique Scamps, Jean Pierre Daures, Cedric Raoul P4.085 ALS: Trials and Biomarkers Serum Creatinine, a Biomarker for Muscle Mass in Amyotrophic Lateral Sclerosis (ALS), Predicts Loss of Ambulation Measured by ALS Functional Rating Scale-Revised Walking Item Score (ALSFRS-Rw) Benjamin Brooks, Michael Fischer, Mohammed Sanjak, Scott Holsten, Boris Kandinov, William Bockenek, Elena Bravver, Urvi Desai, John Scott Story, Thomas Pacicco, Scott Lindblom, Velma Langford, Kathryn Wright, Amber Ward, Nicole Lucas, Nicole Smith, Mindy Nichols, Cynthia Lary, Joanne Nemeth, Priscilla Russo P4.077 P4.086 P4.075 Tremor Assessment: Correlation Between Clinical and Functional Performance Tests Munish Kumar, Man Mohan Mehndiratta, Sanjay Pandey P4.076 Functional Balance Difficulty in Essential Tremor: The Role of Cognition Ashwini Rao, Arthur Gilman, Elan Louis Tirasemtiv Amplifies Skeletal Muscle Response to Nerve Activation in Humans Fady Malik, Richard Hansen, Vipin Vijayakumar, Stoltz Randall, Roger Enoka, David Morgans, Andrew Wolff P4.078 A Pilot Trial of High Frequency High Dose Granulocyte Colony Stimulating Factor (GCSF) in Patients with Amyotrophic Lateral Sclerosis (ALS) Tuan Vu, Terry McClain, Chuanhai Cao, Natalie Tucker, Brittany Golden, Lara Katzin, Clifton Gooch P4.079 Safety and Tolerability of Systemic Beta-2-Adrenergic Agonist (Albuterol) as Pharmacological Therapy in Non-Invasive Ventilation (NIV) -supported Amyotrophic Lateral Sclerosis (ALS)Patients with Chronic Respiratory Failure Benjamin Brooks, Boris Kandinov, Velma Langford, Scott Lindblom, Mohammed Sanjak, Kathryn Wright, Amber Ward, Scott Holsten, Michael Fischer, Nicole Lucas, Nicole Smith, Mindy Nichols, Cynthia Lary, Joanne Nemeth, Priscilla Russo, William Bockenek, Elena Bravver, Urvi Desai, John Scott Story, Thomas Pacicco P4.080 Bilateral Phrenic Nerve Pacing (PNP) in Amyotrophic Lateral Sclerosis (ALS) Patients: The Mayo Clinic Current Experience Mohamed Kazamel, Ronald Reeves, Eric Sorenson A Clinical Demonstration of an EEG Brain-Computer Interface (BCI) for ALS Patients (VA Cooperative Study #567): Enrollment, Retention, and Adherence Richard Bedlack, Robert Ruff, Domenic Reda, Theresa Vaughan, Helen Shi, Katya Hill, Robert Ringer, Patricia Banks, Tamara Paine, Jonathan Wolpaw Anterior Horn Cell Disease: Biomarkers P4.087 Sensory-motor Circuit Dysfunction in Adult Ambulatory SMA Type 3 Patients Claudia Chiriboga, Louis Weimer, Jonathan Marra, Nicole Holuba LaMarca, Jacqueline Montes, Sally Dunaway, George Mentis, Brian McCabe, Darryl De Vivo P4.088 A Significant Increase of Apparent Diffusion Coefficients in Corticospinal Tracts Differentiates Amyotrophic Lateral Sclerosis from Cervical Spondylotic Myelopaty Yuka Koike, Masato Kanazawa, Kensi Terajima, Kei Watanabe, Naoto Endo, Takayoshi Shimohata, Masatoyo Nishizawa P4.089 Excessive Daytime Sleepiness Does Not Predict the Degree of Sleep Disordered Breathing in ALS: An Autonomic Dysfunction Matrix Urvi Desai Chronological Changes in Cardiac Sympathetic Function in Patients with Ayotrophic Lateral Sclerosis: An Analysis Using Cardiac I-123-MIBG Scintigraphy Yuji Tanaka, Megumi Yamada, Akihiro Koumura, Yuichi Hayashi, Akio Kimura, Takashi Inuzuka Familial Amyloid Polyneuropathy Presenting as Atypical Lower Motor Neuron Disease: A Case Report Fabrizio Salvi, Plasmati Rosaria, Francesca Pastorelli, Claudio Rapezzi P4.092 Uric Acid in Amyotrophic Lateral Sclerosis: No Effect on Outcome in a Population-based Series Antonio Canosa, Andrea Calvo, Davide Bertuzzo, Galmozzi Francesco, Cugnasco Paolo, Pisano Fabrizio, Giancarlo Logroscino, Cristina Moglia, Enrica Bersano, Letizia Mazzini, Adriano Chio P4.093 Sexual Dimorphism in ALS Peter Bede, Marwa Elamin, Susan Byrne, Orla Hardiman P4.094 Subscales of the ALS Functional Rating Scale (ALSFRS-R) as Determinants of Survival in Amyotrophic Lateral Sclerosis (ALS) Katya Rascovsky, Sharon Xie, Ashley Boller, Xiaoyan Han, Leo McCluskey, Lauren Elman, Murray Grossman P4.095 Time to Generalization as a Predictor of Prognosis in ALS. Rosanna Tortelli, Massimiliano Copetti, Federica Siena, Rosa Cortese, Rosa Capozzo, Fabio Pellegrini, Isabella Simone, Giancarlo Logroscino P4.101 Magnetic Resonance Imaging Brachial Plexus Alterations in ALS Patients Edoardo Spinelli, Gerevini Simonetta, Federica Agosta, Nilo Riva, Elisabetta Pagani, Andrea Falini, Giancarlo Comi, Massimo Filippi P4.102 Predominantly C8 Myotomal Electrodiagnostic Findings in Hirayama Disease Timothy Rust, William Arnold, Miriam Freimer P4.103 Electrical Impedance Myography for the Evaluation of the Tongue Musculature in Amyotrophic Lateral Sclerosis. Seward Rutkove, Sanjana Shellikeri, Yana Yunusova, Jordan Green, Lorne Zinman P4.104 Functional Connectivity Measured by Spectral EEG as Potential Biomarker for Amyotrophic Lateral Sclerosis Parameswaran Iyer, Bart Michaels, Edmund Lalor, Richard Reilly, Orla Hardiman, Orla Hardiman P4.105 Multiple System Atrophy and Amyotrophic Lateral Sclerosis in a Family with Hexanucleotide Repeat Expansions in C9orf72 Jill Goldman, Cheryl Waters, Hiroshi Mitsumoto, Thomas Brannagan, Stephanie Cosentino, Edward Huey, ShengHan Kuo Neuromuscular: Electrodiagnostic P4.106 Differences in Denervation Patterns Between Patients with Limb Onset and Bulbar Onset ALS Rocio Garcia Santibanez, Stephen Scelsa Can Follow-up Electrodiagnostic Studies in Patients with CIDP That Improved Following IGIV-C Treatment Predict Relapse After Treatment Discontinuation? Russell Chin, Chunqin Deng, Vera Bril, Norman Latov, Hans Hartung, Ingemar Merkies, Peter Donofrio, Pieter Van Doorn, Marinos Dalakas P4.097 Voxel-based Morphometry (VBM) Study in ALS (Amyotrophic Lateral Sclerosis): Temporal Cortical Damage as a Prognostic Marker Milena Albuquerque, Helen Andrade, Cynthia Silva, Anamarli Nucci, Marcondes Franca, Jr. P4.107 P4.098 P4.108 P4.096 Cognitive Changes and White Matter Tract Damage in the Motor Neuron Disease Spectrum Elisa Canu, Federica Agosta, Edoardo Spinelli, Nilo Riva, Massimiliano Copetti, Adriano Chiò, Stefano Messina, Sandro Iannaccone, Andrea Calvo, Vincenzo Silani, Andrea Falini, Giancarlo Comi, Massimo Filippi P4.099 Non-invasive Imaging of Transplanted Neural Stem Cell Survival in Amyotrophic Lateral Sclerosis Amit Srivastava, Sarah Gross, Piotr Walczak, Camille Bulte, Nicholas Maragakis, Jeff Bulte P4.100 Cortical Hemodynamics Assessment in ALS During Cognitive Testing Using Functional Near Infrared Spectroscopy (fNIR) Tooba Fayyaz, Jillian Edwards, Lauren Scull, Hasan Ayaz, Patricia Shewokis, David Libon, Anahita Deboo, Terry Heiman-Patterson Clinical and Neurophysiological Spectrum of Peripheral Neurotoxicity in Patients with CD30Positive Malignancies, Treated with Brentuximab Vedotin. Rosaria Plasmati, Francesca Pastorelli, Fabrizio Salvi Characteristics and Differential Diagnosis of Neuropathy in a Tertiary Neuromuscular Clinic Hui Gong, Amaiak Chilingaryan, Grigor Harutunian, Nazely Ashikian, Said Beydoun P4.109 The Neurohysiological Phenotype Of AH-TTR Amiloidoses Francesca Pastorelli, Rosaria Plasmati, Claudio Rapezzi, Fabrizio Salvi P4.110 Evaluation of Conduction Slowing in Amyotrophic Lateral Sclerosis: A Novel Approach Zubeda Sheikh, Ankit Pahwa, Hongxin Chen, Nizar Souayah P4.111 IVIG Responsive Motor Neuropathy in the legs: A Diagnostic Challenge Eliz Agopian, Dale Lange P4.112 Absence of Spontaneous Activity in Cervical Paraspinal Musculature in Patients with Multifocal Motor Neuropathy/Motor Neuropathy Nuri Jacoby, Russell Chin, Bridget Carey, Jennifer Langsdorf, Naomi Feuer, Norman Latov Fast, Easy Registration Online · AAN.com/view/AM14 83 Wednesday April 30 First Authors stand by Posters from 7:30 a.m.–9:00 a.m. Wednesday, April 30 P4.113 Diagnostic Utility of Repetitive Nerve Stimulation Test of the Trapezius Muscle in Amyotrophic Lateral Sclerosis Yuki Hatanaka, Takashi Chiba, Hidehiko Okuma, Takamichi Kanbayashi, Midori Kuwabara, Mana Higashihara, Masahiro Sonoo P4.114 A Standardized Grading System for Ulnar Neuropathy at the Elbow. Ebinehita Arhebamen, Faten Abu Ghazal, Dilip Pandey, Lawrence Zeidman P4.115 Association of Autonomic Symptoms in Carpal Tunnel Syndrome with Abnormalities in Sympathetic Skin Responses Anibal Lugo, Faisal Ahmad, Lonni Schultz, Jose Garcia, Abdulrahman Alwaki, Naganand Sripathi Neuropathy: Pathogenesis and Diagnostic Testing P4.116 Reduced Neurofilament Expression in Cutaneous Nerve Fibers of CMT2E Patients Chiara Pisciotta, Yunhong Bai, Kathryn Brennan, Tiffany Grider, Shawna Feely, Suola Wang, Steven Moore, Michael Shy P4.117 Characteristics of Patients Evaluated for Small Fiber Neuropathy with Skin Biopsy David Saperstein, Todd Levine, Glenn Lopate, Mamatha Pasnoor, Kayla Newby P4.118 Comparison of Epidermal Nerve Fiber Density and Quantitative Sudomotor Axon Reflex in Neuropathy Diagnosis Ahmad Abuzinadah, Patricia Kluding, Douglas Wright, Linda D’Silva, Janelle Ryals, Bill Hendry, Omar Jawdat, Laura Herbelin, April McVey, Richard Barohn, Mazen Dimachkie, Mamatha Pasnoor P4.119 Characterisation and Diagnostic Evaluation of Chronic Polyneuropathies Induced by Oxaliplatin and Docetaxel Comparing Skin Biopsy to Quantitative Sensory Testing and Nerve Conduction Studies Thomas Krøigård, Henrik Schrøder, Camilla Qvortrup, Lise Eckhoff, Per Pfeiffer, David Gaist, Soren Sindrup P4.120 Comparison of CIDP and MGUS Associated Neuropathy Patients Nuha Alkhawajah, Samantha Dunnigan, Vera Bril P4.121 Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) Skin Biopsies Gene Expression Analysis Thierry Kuntzer, Adrian Panaite, Puttini Stefania, Susanne Renaud, Andreas Steck P4.122 Chronic Immune-Mediated Demyelinating Polyneuropathy After Cetuximab Sarah Kranick, Tanya Lehky, Christine Chung, Hyunseok Kang P4.123 Peripheral Neuropathy in Primary Sjögren’s Syndrome Camila Leijoto, Osvaldo Nascimento, Frederico Prado, Victor Kosac, Caroline Bittar, Giseli Quintanilha, Carlos Bruno Nogueira, Felipe Vianna 84 P4.124 Peripheral Neuromuscular Manifestations of Sarcoidosis Lipika Nayak, Brennen Bittel, Yunxia Wang, Mazen Dimachkie, Laura Herbelin, April McVey, Richard Barohn, Mamatha Pasnoor P4.125 Monofocal Motor Neuropathy: A Case Series Dipika Aggarwal, Mamatha Pasnoor, Laura Herbelin, Mazen Dimachkie, Richard Barohn, April McVey MS and CNS Inflammatory Disease: Biomarkers P4.126 Cerebrospinal Fluid Protein Expression Profiles in Benign and Aggressive Multiple Sclerosis Ying Liu, Marwan Alahiri, Shivani Agarwal, Saud Sadiq P4.127 Extracellular Vesicles Isolated by Cerebrospinal Fluid as Biomarkers of Inflammation in Multiple Sclerosis and Inflammatory Neurological Diseases Paolo Ragonese, Maria Antonietta Mazzola, Fabiana Geraci, Giuseppina Turturici, Giulia Musso, Rosaria Tinnirello, Vincenzina Lo Re, Sabrina Realmuto, Marianna Lo Re, Paolo Aridon, Giuseppe Salemi, Gabriella Sconzo, Giovanni Savettieri P4.128 Recirculating Phagocytes Are a Novel Source of Biomarkers for Brain Injury Ramesh Nayak, Timothy Vollmer, Roberto Bomprezzi, Raymond Jacolik P4.129 CSF Biomarkers in Tumefactive Multiple Sclerosis and Other Disease Subtypes Ayse Altintas, Hayrettin Tumani, Sinem Yazici, Vera Lehmensiek P4.130 Is KIR4.1 Antibody a Marker of Multiple Sclerosis ? Elodie Nerrant, Mahmoud Charif, Xavier Ayrignac, Clarisse Carra-Dalliere, Giovanni Castelnovo, Celine Salsac, Cedric Raoul, Jean Francois Eliaou, Pierre Labauge, Thierry Vincent P4.131 JCV Antibody Positivity and Status Switching Depends on Assay Cutpoint Florian Deisenhammer, Micheal Auer P4.132 Changes in Immunological Biomarkers in Patients with RelapsingRemitting Multiple Sclerosis Treated with Interferon Beta-1a Xin Zhang, Yazhong Tao, Bianca Weinstock-Guttman, Robert Zivadinov, Brooke Hayward, Fernando Dangond, Silva Markovic Plese P4.133 A Multicentric Crosssectional Study of the Usefulness of Cerebrospinal Fluid-Glial Fibrillary Acidic Protein (CSF-GFAP) in the Diagnosis and Prognosis of Inflammatory Demyelinating Diseases Shuhei Nishiyama, Tatsuro Misu, Yuko Shimizu, Kazumasa Yokoyama, Takashi Kageyama, Yoshiki Takai, Rina Takano, Toshiyuki Takahashi, Juichi Fujimori, Shigeru Satoh, Ichiro Nakashima, Yasuto Itoyama, Kazuo Fujihara, Masashi Aoki P4.134 B Cell Subsets in the Cerebrospinal Fluid of Multiple Sclerosis Patients Christopher Sears, Jerry Lin, Alexandra Berman, Saud Sadiq P4.135 Reduced Level of Sialylated IgG Antibody in the CSF of Patients with Multiple Sclerosis Xiaoli Yu, Kathryn Dennison, Tiffany Pointon, Timothy Vollmer 7:30 a.m.–11:00 a.m. P4.136 CSF Isoelectric Focusing Differentiates Multiple Sclerosis from Other CNS Autoimmune Disorders Abdulradha Alqallaf, Shitiz Sriwastava, Fen Bao, Evanthia Bernitsas, Erica Errigo, Alexandros Tselis, Scott Millis, Christina Caon, Omar Khan P4.137 Can inflammatory Markers from CSF be Helpful in Diagnosis of Multiple Sclerosis? Zuzana Matejcikova, Hana Prikrylova-Vranova, Jana Klosova, Vladimira Sladkova, Jana Zapletalova, Jan Mares, Petr Kanovsky P4.138 Update on MSPrecise: A Novel Diagnostic Test for Multiple Sclerosis Nancy Monson, Eric Eastman, Douglas Bigwood, Mikhail Levin, William Rounds, Lindsay Cowell, Benjamin Greenberg P4.139 Detection of Anti-natalizumab Antibodies in Treated Multiple Sclerosis Patients Using a Biacore™ Platform Fronda Anna, Ebrima Gibbs, Tariq Aziz, Joel Oger P4.140 A One Year Follow-up of JCV Serology with Index Values in a French Natalizumab Treated Multiple Sclerosis Cohort Olivier Outteryck, Hélène Zephir, Arnaud Kwiatkowski, Albert Verier, Didier Ferriby, Marine Viallet, Philippe Devos, Jean-Bertin N’Kuendjo, Olivier Derepeer, Patrick Hautecoeur, Patrick Vermersch P4.148 Pharmacoeconomic and Clinical Characteristics in Patients with Multiple Sclerosis Treated with Disease Modifying Therapies: PEARL—24 Months Results Sylia Moser, Sonja Ortler, Tom van Lokven, Tjalf Ziemssen P4.149 Estimated Productivity Loss amongst U.S. Employees with Multiple Sclerosis Slaven Sikirica, Huanxue Zhou, Vivian Herrera, Jinhee Park, Rahul Sasane P4.150 The Impact of Spasticity Severity on Healthcare Utilization Among MS Patients: A Large-Scale Six-year Follow-up Study Tuula Tyry, Amber Salter, Joan Largent, Ruth-Ann Marrie P4.151 Substantial Declines in Rates of Hospitalization in Multiple Sclerosis: A Population-based Study Ruth-Ann Marrie, Nancy Yu, Aruni Tennakoon, James Marriott, Michael Cossoy, Lawrence Elliott, James Blanchard P4.152 MS Related Employment in Germany After the Introduction of Disease Modifying Drugs Alexei Korchounov P4.153 Nursing Home MS Residents Experience Less Stress and Pessimism Compared to Home-Based NonAmbulatory MS Patients. Zilfah Younus, Irfan Ahsan, Sahil Gupta, Katelyn Kavak, Barbara Teter, Bianca Weinstock-Guttman P4.141 P4.154 P4.142 MS and CNS Inflammatory Disease: Pregnancy and Hormonal Influences Anti-JC Virus Antibody Prevalence in Canadian MS Patients Virender Bhan, Yves Lapierre, Mark Freedman, Pierre Duquette, Daniel Selchen, Vladimir Migounov, Len Walt, Annie Zhang Cerebrospinal Fluid Mononuclear Phagocytes Are Decreased in Number and Express Less IL-10 in Multiple Sclerosis Compared to Values Seen with Normal Controls Shivani Agarwal, Irene Jarchum, Ying Liu, Saud Sadiq P4.143 Fetuin-A, a Cerebrospinal Fluid (CSF) Biomarker of Multiple Sclerosis (MS) Disease Activity, Promotes Immune Cell Infiltration into the CNS Lena Bell, Violaine Harris, Mark Landy, Kristi Clark, Saud Sadiq P4.144 Association Between Immune Cell Neurotrophins Levels and Subcortical Grey Matter Volume in Multiple Sclerosis Patients Alicja Kalinowska-Lyszczarz, Mikolaj Pawlak, Slawomir Michalak, Wlodzimierz Paprzycki, Wojciech Kozubski Cost and Impact Care of MS P4.145 The Economic Impact of Functional Impairment Among Respondents with Multiple Sclerosis: Findings from the US Medical Expenditure Panel Survey Ravi Iyer, Matthew Sussman, Monica Fay, Terrie Livingston, Glenn Phillips, Joseph Menzin P4.146 Peginterferon Beta-1a Reduces Relapse-Associated Costs in Patients with Relapsing-Remitting Multiple Sclerosis Ken O’Day, Kellie Meyer, Matt Mitchell, Sonalee Agarwal, Elizabeth Kinter P4.147 Cost Sharing Among Persons with MS Eric Cheng, Vinita Dora, Miriam Ayad, Alex Chen, Annette Langer-Gould, Susan Ettner 2O14 Scientific Abstract Listing and Annual Meeting Information Satisfaction with Multiple Sclerosis Care in Daily Practice of Patients Without an Immunmodulating Therapy—Results of a Patient Survey (FOLLOW) Volker Heeschen P4.155 Birth Outcomes In Newborns Fathered By Men With Multiple Sclerosis Exposed To Disease-Modifying Drugs Ellen Lu, Feng Zhu, Yinshan Zhao, Mia van der Kop, Anne Synnes, Leanne Dahlgren, Dessa Sadovnick, Anthony Traboulsee, Helen Tremlett P4.156 Gestational Exposure to Natalizumab and Pregnancy Outcomes— Results from a Prospective Cohort with Relapsing Remitting Multiple Sclerosis Neda Ebrahimi, Sandra Herbstritt, Ralph Gold, Lilyana Amezcua, Gideon Koren, Kerstin Hellwig P4.157 Pregnancy and Fetal Outcomes After Paternal Exposure to Disease Modifying Drugs for Multiple Sclerosis Maria Pia Amato, Marta Giannini, Emilio Portaccio, Angelo Ghezzi, Bahia Hakiki, Luisa Pasto’, Lorenzo Razzolini, Chiara Pecori, Andrea Sturchio, Laura De Giglio, Carlo Pozzilli, Damiano Paolicelli, Maria Trojano, Maria Marrosu, Francesco Patti, Gian Luigi Mancardi, Claudio Solaro, Rocco Totaro, Maria Tola, Giovanna De Luca, Alessandra Lugaresi, Lucia Moiola, Vittorio Martinelli, Giancarlo Comi P4.158 Serum Anti-Müllerian Hormone Levels in Reproductive-age Women with Relapsing Remitting Multiple Sclerosis Kerstin Hellwig, Susanne Kollar, Gisa Ellrichmann, Darryl Nousome, Ingo Kleiter, Ralf Gold, Jan Thoene Poster Session IV P4.159 Pregnancy Decisionmaking for Women with Multiple Sclerosis Barbara Teter, Katelyn Kavak, Karen Zakalik, Channa Kolb, Patricia Coyle, Bianca Weinstock-Guttman P4.160 Reproductive Attitudes and Pregnancy in Females with Multiple Sclerosis: Outcomes and Exposure to Disease-Modifying Drugs Ayse Altintas, Bjar Najar, Gokcen Gozubatik-Celik, Sukriye Menku P4.161 Updated Pregnancy Outcomes in Patients and Partners of Patients in the Teriflunomide Clinical Trial Program Lily Jung Henson, Myriam Benamor, Philippe Truffinet, Bernd Kieseier P4.162 Influence of Sex Hormone Ratios on the Clinical Course of Multiple Sclerosis: A Case Study After the First Year of Follow Up. Dimitrios Kitsos, Charis Liapi, Sotirios Tsiodras, Antonios Poulios, Konstantine Voumvourakis P4.163 Menopause in a Longitudinal Clinical Cohort of Women with Multiple Sclerosis. Riley Bove, Brian Healy, Alexander Musallam, Nafiseh Alsharif, Bonnie Glanz, Tanuja Chitnis P4.164 Differencies in the Severity of Multiple Sclerosis Within Gender Determinated by Age at Onset Jimena Míguez, Juan Ignacio Rojas, Liliana Patrucco, Edgardo Cristiano Cognition in MS P4.165 Mismatch Negativity Links to Information Processing in Multiple Sclerosis (MS) Felicia Jackson, Leigh Charvet, Maria Amella, Greg Proudfit, Lauren Krupp P4.166 Cognitive Dysfunction in Patients with Multiple Sclerosis Is Related with Apathy and Depression, But Not Subjective Fatigue Masaaki Niino, Nobuhiro Mifune, Susumu Kusunoki, Yusei Miyazaki, Seiji Kikuchi P4.167 Presence and Significant Determinants of Cognitive Impairment in a Large Sample of Patients with Multiple Sclerosis Martina Borghi P4.168 Predictivity of Executive Functions in Episodic Memory in Multiple Sclerosis Rekha Barthelemy, Bruno Lenne, Dephine Leuse, Arnaud Kwiatkowski, Patrick Hautecoeur P4.169 The Symbol Digit Modalities Test (SDMT) Has Been the Standard Cognitive Measure Used in Multiple Sclerosis (MS) Clinical Trials: How Does It Correlate with Computerized Cognitive Screening Tools? Myassar Zarif, Mark Gudesblatt, Barbara Bumstead, Marijean Buhse, Lori Fafard, Cynthia Sullivan, Jeffrey Wilken, Glen Doniger, Juskaran Chahda P4.170 Cognitive Changes During and After MS Relapses—6 Months FollowUp Katrin Gross-Paju P4.171 Cognitive Evolution in Tysabri (natalizumab)-Treated Multiple Sclerosis Patients Francois Jacques, Brian Harel, Adrian Schembri, Joanne Gale P4.172 Effects of Natalizumab on Cognition and Neurodegeneration in Relapsing-Remitting Multiple Sclerosis Garrick Talmage, Oscar Coppes, Ashley Finch, Christina Sprayberry, Adil Javed, Jacqueline Bernard P4.181 P4.173 P4.182 Multiple Sclerosis and Driving: Cognitive Profile Correlation to Patient Self-Reported Driving Mark Gudesblatt, Myassar Zarif, Barbara Bumstead, Marijean Buhse, Smitha Thotam, Lori Fafard, Jennifer Kalina, Cynthia Sullivan, Jeffrey Wilken, Glen Doniger MS and CNS Inflammatory Disease: Quality of Life P4.174 Quality of Life and Fatigue in Radiologically Isolated Syndrome Christine Lebrun Frenay, Mikael Cohen, Pierre Clavelou P4.175 Cognition and Grey Matter Atrophy Are Predictive of Health Related Quality of Life in Early Treated Patients with Clinically Isolated Syndrome Mikael Cohen, Bruno Brochet, Pierre Clavelou, Emmanuelle Lepage, Patrick Vermersch, Ayman Tourbah, Thibault Moreau, Christine Lebrun Frenay P4.176 Health-Related Quality of Life in US Patients with Relapsing-Remitting Multiple Sclerosis (RRMS) Treated with Delayed-Release Dimethyl Fumarate: An Integrated Analysis of the Phase 3 DEFINE and CONFIRM Studies Mariko Kita, Robert Fox, Ralf Gold, Sujata Sarda, Ravi Iyer, Timothy Niecko, Leslie Meltzer, J. Theodore Phillips P4.177 Peginterferon Beta-1a Treatment Reduces the Impact of Multiple Sclerosis Relapse and Disability Progression on Health-Related Quality of Life: Results from the ADVANCE Trial Elizabeth Kinter, Shien Guo, Arman Altincatal, Irina Proskorovsky, Glenn Phillips, Bjorn Sperling P4.178 Two-Year Interim Analysis of Quality of Life in Patients with RelapsingRemitting Multiple Sclerosis (RRMS) treated with Delayed-Release Dimethyl Fumarate in the ENDORSE Study Mariko Kita, Robert Fox, Ralf Gold, Gavin Giovannoni, J. Theodore Phillips, Sujata Sarda, Macaulay Okwuokenye, Jessica Kong, Ray Zhang, Vissia Viglietta, Sarah Sheikh, Ludwig Kappos P4.179 Interim Results of the Swiss Post Marketing Surveillance Monitoring Quality of Life and Treatment Satisfaction in Patients with Relapsing-Remitting Multiple Sclerosis (SWISSASCENT) Adam Czaplinski, Emilie Jaquiery, Petra Stellmes, Simon Ramseier, Andreas Baumann, Oleg Kurlandchikov, Christian Berger, Michel Chofflon, Franziska Lieder, Sandra Gass, Thomas Maier P4.180 Patient-reported Quality of Life in the BENEFIT Trial Gilles Edan, Ludwig Kappos, Xavier Montalban, Mark Freedman, Hans Hartung, David Miller, Frederik Barkhof, Julia Hermann, Vivian Lanius, Christoph Pohl, Rupert Sandbrink, Dirk Pleimes Multiple Sclerosis: the Need to Understand Patients’ Quality of Life in a Latin American Country Sandra Vanotti, Natalia Ciufia, Cecilia Yastremiz, Maria Saladino, Nora Fernandez Liguori, Alberto Yorio, Fernando Caceres Health-Related Quality of Life in Relapsing-Remitting Multiple Sclerosis (RRMS): Comparison with Other Medical Conditions and Effect of Delayed-Release Dimethyl Fumarate Treatment Sujata Sarda, Glenn Phillips, Julia Gaebler, Nuwan Kurukulasuriya P4.183Patient-Reported Psychological Functioning in Natalizumabtreated Patients with Multiple Sclerosis in US Clinical Practice John Foley, Kavita Nair, Judith Stephenson, Timothy Vollmer, Timothy Niecko, Sonalee Agarwal, Crystal Watson MS and CNS Inflammatory Disease: Disability Progression P4.184 Predicting Disability in the Modern MS Cohort Roland Henry, Esha Datta, Alyssa Zhu, Bagrat Amirbekian, Regina Schlaeger, Refujia Gomez, Rachel Kanner, Caroline Ciocca, Jeffrey Gelfand, Douglas Goodin, Ari Green, Stephen Hauser, Bruce Cree P4.185 The Risk of Progression in MS Depends on the Features of Preceding Relapses: Application to First Generation Immunomodulating Theraphy Helen Tedeholm, Bengt Skoog, Bjorn Runmarker, Anders Odén, Oluf Andersen P4.186 Incomplete Relapse Recovery and Sustained Disability Progression in Multiple Sclerosis in Pittsburgh Edward Gettings, Chris Hackett, Carol Schramke, Thomas Scott P4.187 Clinical Predictors of Expanded Disability Status Scale Rank Change Over 5-Year Intervals in the MSBase Registry Stella Hughes, Timothy Spelman, Maria Trojano, Alessandra Lugaresi, Guillermo Izquierdo, Francois Grand-Maison, Pierre Duquette, Marc Girard, Pierre Grammond, Celia OrejaGuevara, Raymond Hupperts, Cavit Boz, Roberto Bergamaschi, Giorgio Giuliani, Edite Rio, Jeannette Lechner-Scott, Vincent Van Pesch, Gerardo Iuliano, Marcela Fiol, Freek Verheul, Michael Barnett, Mark Slee, Joseph Herbert, Ilya Kister, Norbert Vella, Fraser Moore, Tatjana Petkovska-Boskova, Vahid Shaygannejad, Vilija Jokubaitis, Gavin McDonnell, Stanley Hawkins, Frank Kee, Helmut Butzkueven, Orla Gray P4.188 Predictors of Disability Extremes in Patients with Multiple Sclerosis Treated with Interferon-beta Using the Swedish MS Registry Katharina Fink, Anna Fogdell-Hahn, Jan Hillert P4.189 Previous Disability Has an Influence in Recovery of Multiple Sclerosis Relapses Treated with Methylprednisolone? Cristina Ramo, Laia Grau-López, Maria Tintore-Subirana, Alex Rovira, Lluis Ramio, Luis Brieva, Albert Saiz, Carlos Nos, Antonio Cano, Olga Carmona, Ferran Torres, Jose Vicente Hervas, Xavier Montalban, Joan Costa P4.190 Relationship Between Sustained Expanded Disability Status Scale Progression and Simultaneous Changes in Individual Functional Systems in RelapsingRemitting Multiple Sclerosis Thomas Scott, Bjorn Sperling, Ping Wang, Xiaojun You, Monica Mann P4.191 Evaluating TMS Motor Evoked Potentials in Early Stages of Multiple Sclerosis Aid in Predicting Disability Nilufer Kale, Gulten Ozdemir, Eda Coban, Jale Agaoglu P4.192 Sustained Disability Improvement Associated with Reduced MRI Lesion Burden in Natalizumab-Treated Patients with Multiple Sclerosis Luca Prosperini, Floriana De Angelis, Rosanna De Angelis, Fulvia Fanelli, Carlo Pozzilli P4.193 A Multi-Modal Neurophysiological Evaluation of Primary Progressive Multiple Sclerosis—a Cross Sectional and Longitudinal Cohort Analysis Luke Canham, David Cottrell, Nick Kane, Jonathan Witherick, Kelly Blake, Peter Walsh Aging, Dementia, and Cognitive and Behavioral Neurology: Early Diagnostic Markers P4.194 Normal HDL But Not the HDL from Patients with Coronary Heart Disease Prevent LDL Induced Toxicity in Cultured iCell Neurons. Samra Vazirian P4.195 A Predictive Model for Cognitive Impairment in Individual Patient with Diabetes Mellitus Martin Rakusa, Matej Rakusa, Miro Cokolic P4.196 Mild Cognitive Impairment (MCI)in Parkinson Disease (PD) and Lewy Body Disease(LBD): Who Became to Dementia? Maria Garcia Basalo, Maria Fernandez, Carla Stefani, Waleska Berrios, Diego Bauso, Juan Ignacio Rojas, Edgardo Cristiano, Angel Golimstok P4.197 A portable Non-Invasive Biosensor Based Approach to Actively Assess Cognitive Function in Alzheimer’s Disease (AD) and Beyond Allan Bernstein, Terry Hess, Parham Ghorbanian, Hashem Ashrafiuon, David Devilbiss, Adam Simon P4.198 Cognitive Impairment in Healthy Filipino Adults with MRI Nonspecific White Matter Change Ty Alekzander Talamera, Jacqueline Dominguez, Merceditas Dizon P4.199 Microstuctural Alteration of the Default Mode Network as a Predictor of Cognitive Impairment in Alzheimer’s Disease Marina Weiler, Brunno de Campos, Mateus Nogueira, Tátila Lopes, Benito Damasceno, Fernando Cendes, Marcio Balthazar P4.200 Theory of Mind: a Cognitive Marker of Conversion from Mild Cognitive Impairment to Alzheimer Disease? Noémie Moreau, Stéphane Rauzy, François Viallet, Maud Champagne-Lavau Fast, Easy Registration Online · AAN.com/view/AM1485 Wednesday April 30 First Authors stand by Posters from 7:30 a.m.–9:00 a.m. Wednesday, April 30 P4.201 The Pituitary Adenylate Cyclase Activating Polypeptide Levels Are Associated with Pathological Features of Alzheimer’s Disease Jiong Shi, P Han, L Baxter, W Liang, Z Tang, J Yin, T Beach, R Caselli, E Reiman Aging, Dementia, and Cognitive and Behavioral Neurology: Frontotemporal Lobar Degeneration P4.202 Motor Neuron Dysfunction In Frontotemporal Lobar Degeneration: A Clinical and Neurophysiological Study Chiara Cerami, Alessandra Marcone, Claudio Marangoni, Chiara Crespi, Alessandra Dodich, Nicola Canessa, Sandro Iannaccone, Zamboni Michele, Valeria Golzi, Maria Cristina Giusti, Stefano Cappa P4.203 Do We Need a Change? Utility of Standard Cognitive Screening Instruments in Patients with Amyotrophic Lateral Sclerosis Eileen Moran, Katya Rascovsky, Ashley Boller, Leo McCluskey, Lauren Elman, David Libon, Murray Grossman P4.204 Cognitive Impairment (CI) in Amyotrophic Lateral Sclerosis (ALS): A Clinical Based Study Marcelo Chaves, Maria Garcia Basalo, Mariela Bettini, Maria Fernandez, Edgardo Cristiano, Marcelo Francisco Rugiero, Angel Golimstok P4.205 Cytokine Gene Expression in Peripheral Cells from Patients with Frontotemporal Lobar Degeneration Due to GRN and C9ORF72 Mutation Daniela Galimberti, Chiara Fenoglio, Rossana Bonsi, Maria Serpente, Chiara Villa, Sara Cioffi, Cinzia Barone, Andrea Arighi, Laura Ghezzi, Giorgio Fumagalli, Elio Scarpini P4.206 TDP-43 in Alzheimer’s Disease Is Not Associated with Parkinsonian Features or Clinical FTD Youngsin Jung, Dennis Dickson, Melissa Murray, David Knopman, Bradley Boeve, Ronald Petersen, Keith Josephs P4.207 The Clock Drawing Test in Behavioral Variant Frontotemporal Dementia Versus Alzheimer’s Disease Robin Barrows, Joseph Barsuglia, Donald Eknoyan, Valeriy Sabodash, Mario Mendez P4.208 Clinician Versus Family Caregiver Ratings of Behavioral Variant Frontotemporal Dementia Joseph Barsuglia, Hemali Panchal, Aditi Joshi, Robin Barrows, Michelle Mather, Elvira Jimenez, Mario Mendez 7:30 a.m.–11:00 a.m. Cerebrovascular Disease and Interventional Neurology: Acute Stroke Endovascular Cerebrovascular Disease and Interventional Neurology: Acute Stroke Thrombolysis P4.209 P4.219 “Heparin-Less” Protocol for Endovascular Treatment of Acute Ischemic Stroke Asif Khan, Ameer Hassan, Taqi Zafar, Ahmed Malik, Malik Adil, Muhammad Suri, Adnan Qureshi P4.210 Interim Recanalization in Acute Ischemic Stroke Patients Selected for Endovascular Treatment by CT Angiography Mushtaq Qureshi, Farhan Siddiq, Daraspreet Kainth, Adnan Qureshi P4.211 Troponin Elevation in Intraarterial Stroke Intervention Abhay Kumar, Sonal Mehta, Aws Alawi, Amanda Michael P4.212 Downstream Clot Fragment Migration During Endovascular Clot Extraction Adversely Affects Clinical Outcome James Frey, Carol Darbonne, Joni Clark, Allison Tucker, Christina Chapple P4.213 Intervention Stroke Assessment Scale for Eligibility in Endovascular Therapy (ISASET) Dababneh Haitham, Asif Bashir, Mohammed Hussain, Sara Misthal, Mohammad Moussavi, Jawad Kirmani P4.214 “No Turn Back Approach” to Reduce Treatment Time for Endovascular Treatment of Acute Ischemic Stroke Hossam Egila, Malik Adil, Harris Siddiqi, Nidaullah Mian, Ameer Hassan, Jefferson Miley, Gustavo Rodriguez, Muhammad Suri, Adnan Qureshi P4.215 Thrombus Density Predicts Successful Recanalization with StentRetriever Thrombectomy in Acute Ischemic Stroke Maxim Mokin, Simon Morr, Sabareesh Natarajan, Adnan Siddiqui, Elad Levy P4.216 Optical Bedside Monitoring of Cerebral Blood Flow in Acute Ischemic Stroke Patients During Head of Bed Manipulation Christopher Favilla, Rickson Mesquita, Michael Mullen, Turgut Durduran, Meeri Kim, David Minkoff, Scott Kasner, Greenberg Joel, Arjun Yodh, John Detre P4.217 Endovascular Treatment of Acute Basilar Artery Occlusion Roman Herzig, Tomas Dornak, David Skoloudik, Daniel Sanak, Martin Kuliha, Martin Roubec, Roman Havlicek, Lenka Hajdukova, Martin Kocher, Vaclav Prochazka, Jiri Lacman, Frantisek Charvat, Michal Kral, Tomas Veverka, Jana Zapletalova P4.218 Intra-procedural Heparin Increases Mortality and Reduces Rates of Favorable Outcome in Acute Ischemic Stroke Patients Undergoing Endovascular Treatment Vishal Jani, Avean Saed, Tanya Mohindroo, Mushtaq Qureshi, Syed Hussain, Fareed Suri, Adnan Qureshi Safety of tPA + Transcranial Emission of Low-energy Lasers for Acute Stroke Recovery—Results Thomas Hemmen, Rema Raman, Souvik Sen, Madeleine Geraghty, Karen Rapp, Steven Richeri, Brett Meyer, Justin Zivin, Christopher Fanale P4.220 Thrombolytic Outcomes for Acute Ischemic Stroke in Patients with Primary Brain Tumors in the United States Santosh Murthy, Yogesh Moradiya, Shreyansh Shah, Aditi Shastri, Eric Bershad, Jose Suarez P4.221 Balancing Rapid Treatment Goals with Thorough Laboratory Evaluation in Alteplase Candidates: A Review of a Stroke Center’s Current Practices and Outcomes Stacy Smith, John Volpi P4.222 Serum Albumin Is Associated with Cerebral Hemorrhage in PostIntravenous Thrombolytic Therapy for Acute Stroke: A Retrospective Chart Review Haris Kamal, Ping Li, Kelly Smith, Ghulam Mustafa, Robert Sawyer, Marilou Ching, Bijal Mehta P4.223 Thrombolytic Treatment for Acute Ischemic Stroke Patients with History of Migraine Headaches Ahmed Malik, Malik Adil, Saqib Chaudhry, Adnan Qureshi P4.224 Intravenous Thrombolysis for Acute Ischemic Stroke in the 3- to 4·5-hour Window—the Malabar Experience Karadan Ummer, K. Salam, Mohan Noone, Pradeep Kumar P4.225 The effect of statin pretreatment and Serum Lipid Values on Hemorragic Conversion After rt-PA for Acute Ischemic Stroke Ayaz Khawaja, Michael Lyerly, Gyanendra Kumar, Kara Sands, Reza Bavarsad Shahripour, Andrei Alexandrov P4.226 Can CT Perfusion Identify Patients Unlikely to Show Improvement Following Intravenous Thrombolysis? Dushyant Damania, Nancy Kung, George Koch, Minal Jain, Anunaya Jain, Babak Jahromi Life Threatening Intracranial Hemorrhage as a Consequence of Dobutamine Stress Echocardiography: A Case Report Adithya Sivaraju, Vineet Punia, Machteld Hillen P4.231 Can Transthoracic Echocardiography be Useful Detecting Patent Foramen Ovale in Stroke? The of Valsalva Maneuver Ana Iglesias Mohedano, Fernando Diaz Otero, Andres García Pastor, Raquel Yotti, PIlar Vazquez Alen, Raul Dominguez Rubio, Fernando Romero Delgado, Adriana Muñoz González, Pilar Sobrino García, Yolanda Fernández Bullido, Antonio Villanueva Osorio, Antonio Gil-Nunez P4.232 Cardiac Autonomic Neuropathy, Screening, Staging and Follow-Up, a Five Year Study from a General Hospital Lalitha Rajanala, Sundarachary Nagarjunakonda, Veeramma Doctor P4.233 Cardiac Valve Strands in Ischemic Stroke: Strand Effects and Outcomes of Medical or Surgical Intervention Jennifer Chu, Roderic Fabian P4.234 Review of Cardiac Abnormalities with Hypercoagulable Testing in Ischemic Stroke Patients Nicolaas Anderson, Akshay Shah, Kendra Drake, Maria Proytcheva, Bruce Coull P4.235 Systemic Inflammation Exacerbates Stroke in Patients with Left Ventricular Assist Device Ryo Ohtomo, Atsushi Iwata, Osamu Kinoshita, Jun Shimizu, Minoru Ono, Shoji Tsuji P4.236 Transcranial Doppler to Assess Cerebral Blood Flow in Patients on Extra Corporeal Membrane Oxygenation Sanam Baghshomali, Patrick Reynolds, Aarti Sarwal Cerebrovascular Disease and Interventional Neurology: Endovascular Neurology P4.237 Venous Flow Stagnation in Acute Ischemic Stroke Patients Undergoing Endovascular Treatment Mushtaq Qureshi, Daraspreet Kainth, Adeel Memon, Adnan Qureshi P4.227 P4.238 Cerebrovascular Disease and Interventional Neurology: Cardiac P4.239 Vitreous Hemorrhage as a Complication of IV-tPA Therapy in a Patient with Acute Stroke Laxmi Shah, Thierry Verstraeten, David Wright, Sandeep Rana P4.228 Utility of Pelvic MRV in Evaluation of Patients with Cryptogenic Stroke and PFO Marcey Osgood, Elizabeth Budman, Nils Henninger P4.229 Effect of Patent Foramen Ovale (PFO) Endovascular Closure on Stroke Quality of Life Feeney-Heinzelmann K, MingMing Ning, W Deng, T Wickham, I Inglessis, Eng Lo, I Palacios, Ferdinando Buonanno 86 P4.230 2O14 Scientific Abstract Listing and Annual Meeting Information Functional Status and 5-year Survival Among Elderly Americans: Implications for Patient Selection for Surgical and Endovascular Procedures Ahmed Malik, Malik Adil, Adnan Qureshi Is Hemoglobin A1c (HbA1C) Level an Independent Predictor of Adverse Outcomes in Patients with Acute Ischemic Stroke Undergoing Endovascular Treatment? Mohammad Afzal, Saqib Chaudry, Taqi Zafar, Ali Saeed, Mohammad Owais, Malik Adil, Vikram Jadhav, Ameer Hassan, Syed Hussain, Adnan Qureshi Poster Session IV P4.240 Motor Component of National Institute of Health Stroke Scale Effect on Functional Outcome and Mortality at Discharge in Patient Receiving Endovascular Therapy Sara Misthal, Dababneh Haitham, Asif Bashir, Mohammed Hussain, Mohammad Moussavi, Jawad Kirmani P4.241 Intravenous Thrombolysis Versus Endovascular Treatment for Acute Ischemic Stroke: A Meta-Analysis of Randomized Controlled Trials Nidaullah Mian, Farhan Siddiq, Mushtaq Qureshi, Malik Adil, Asif Khan, Muhammad Suri, Adnan Qureshi P4.253 Case of Occipital Epilepsia Partialis Continua Presenting as Status Migrainosus: Clinical, EEG and Brain MRI Findings Weiwei Dai, Madeleine GriggDamberger P4.254 Efficacy of Lacosamide in Epilepsia Partialis Continua Devanshi Jadhav, Daniel Birnbaum, Kathleen Burger, Mohamad Koubeissi P4.255 Epilepsia Partialis Continua Secondary to Ischemic Stroke, Responsive to the Combination of Levetiracetam and Lacosamide Rebecca Thompson, Najib Murr, Pierre Fayad P4.242 Epilepsy and Clinical Neurophysiology (EEG): Non-Epileptic Seizures and SUDEP P4.243 P4.256 The Future Role of Interventional Neurology—A Survery of Neurology Department Program Directors and Clerkship Directors. John Leschke An Updated CostEffectiveness Analysis (CEA) of r-tPA for Acute Ischemic Stroke (AIS) Treated Within 3 Hours of Symptom Onset Denise Boudreau, Gregory Guzauskas, Darren Tayama, Susan Fagan, David Veenstra P4.244 The Future Role of Interventional Neurology—a Survey of Neurology Department Chairmen. John Leschke P4.245 Performance Metrics for The Interventional Treatment of Acute Ischemic Stroke; Results from a Comprehensive Stroke Center Ali Sultan-Qurraie, Adam de Havenon, Kyra Becker, Deepak Sharma, Danial Hallam, Basavaraj Ghodke, Louis Kim, David Tirschwell Epilepsy and Clinical Neurophysiology (EEG): Status Epilepticus P4.246WITHDRAWN P4.247Non-convulsive Status Epilepticus in Comatose Patients. Alejandro Thomson, Analia Calle, Agustina Tamargo, Maria Gonzalez Toledo, Fatima Pagani Cassara, Diego Nadile, Vladimiro Sinay, Alfredo Thomson P4.248 Early Identification of Status Epilepticus Etiology with a Simple Clinical Tool Vincent Alvarez, Jong Lee, M. Westover, Andrea Rossetti P4.249 Intravenous Versus Non-intravenous Benzodiazepines for the Treatment of Status Epilepticus: A Systematic Review and MetaAnalysis Ahmad Abulaban, Abdussalam Alshehri, Suleiman Kojan, Rakan Bokhari P4.250Benzodiazepine Administration for Seizure Emergencies: A Review Sheryl Haut, Syndi Seinfeld, John Pellock P4.251 Diazepam Useful in ESES Treatment Mirret El-Hagrassy, Chulaka Gunasekara, Yaman Eksioglu P4.252 Temperature Modulation for Refractory Status Epilepticus Barry Czeisler, Sohil Manvar, Gian Marco De Marchis, Deborah Pugin, Andres Fernandez, Brandon Foreman, J. Michael Schmidt, Neeraj Badjatia, Sachin Agarwal, Stephan Mayer, Jan Claassen A Case Series Exploration of a Possible Relationship Between Non-Epileptic Behavioral Spells and Migraine Andrew Tseng, Jeffrey Staab, Ivan Garza, Gregory Cascino P4.257 Relevance of Psychogenic and Epileptic Seizures Coexisting in an Epilepsy Monitoring Unit Population Alan Krumholz, Diane Thomas P4.258 Role of Placebo Induction in Epilepsy Monitoring Unit Ahmed Yassin, Todd Masel P4.259 Diagnostic Yield of Prolonged Electroencephalogram In Pediatric Syncope Patients Cimy Jacob, Alice Daniel, Josiane LaJoie P4.260 The Spectrum of Ictal Asystole: A Case Series David Harris, Maromi Nei P4.261 Age-specific Periictal Electroclinical Features of Generalized Tonic-clonic Seizures and Potential Risk of Sudden Unexpected Death in Epilepsy (SUDEP). Gurmeen Kaur, Joel Freitas, Samden Lhatoo, Guadalupe FernandezBacaVaca, Curtis Tatsouko P4.267 Lamotrigine, a Narrow Therapeutic Index Drug or Not? Wendy Cai, Tricia Ting, James Polli, Michel Berg, Michael Privetera, Wenlei Jiang P4.268 Psychogenic Non-Epileptic Spells: Analysis of Clinical Perspectives and Practice Amy Hessler, Barbara Slevin, Malachy Bishop, Amelia Anderson P4.269 Pharmaceutical Quality Assessment of Generic Lamotrigine Immediate Release (IR) Tablets Kunyi Wu, Daniel Peng, Wenlei Jiang P4.270 The Effect of an Educational Intervention on Compliance with AAN Guidelines for Return Epilepsy Visits: A Quality Improvement Project Gary Nelson, Lynne Kerr, Francis Filloux P4.271 David Versus Goliath: Two Competing US Trials of 3,4-Diaminopyridine (3,4-DAP) in Lambert-Eaton Myasthenic Syndrome (LEMS) Donald Sanders P4.272 Development and Implementation of a Quality Improvement Strategy for Obtaining Muscle Biopsies Utilizing DMAIC Methodology Charles Kassardjian, Michelle Williamson, Dorothy Van Buskirk, Floranne Ernste, Andrea Leep Hunderfund P4.273 Routine Versus Electronic Data Collection in Multiple Sclerosis Patients Wael Richeh, Jesus Lovera, Amparo Gutierrez, Nicole VillemarettePittman, Raisa Martinez P4.274 Cross Validation of Local Labs to Eliminate Reference Lab Testing for Varicella Zoster ELISA: A Model for Reducing Send Out Labs to Improve Care and Lower Cost. Alexander Hartmann P4.275 Does Effective Communication Between Patients and Ordering Physicians Improve Patient Satisfaction and the Quality of Electrodiagnostic Studies? Divpreet Kaur, Yadira VelazquezRodriguez, Aiesha Ahmed P4.262 Practice, Policy, and Ethics: Training and Common Practices in Neurology P4.263 P4.276 Epilepsy, Syncope, and SUDEP, a Small Case Series Camilo Garcia-Gracia, Nancy Rosales, Rachana Gandhi Efficacy and Safety of Vigabatrin in 90 Pediatric and Adult Patients with Epilepsy Dimitrios Arkilo, Caitlin Narusiewicz, Janet Branson, Jennifer Brunn, Carol Hoskin, Patricia Penovich, Michael Frost P4.264 Lacosamide Retention Rates in Pediatric Epilepsy Emily Robbins, Sudha Kessler, Julia Cohen P4.265 Prescribing Trends of Antiepileptic Drugs for Epilepsy Within the Veterans Health Administration Tung Tran, Rizwana Rehman, Aatif Husain Practice, Policy, and Ethics: Epilepsy, Neuromuscular, and Neuroimmunology P4.266 Improving Patient Satisfaction The Neurology Service Sonia Krish, Nicole Harrison, Enedra Allen-Mcbride, Paul Schulz Unplanned Transfers to a Neurological Intensive Care Unit Carl Gold, Stephan Mayer, Laura Lennihan, Joshua Willey P4.277 Who Is Your Neurologist?: Measuring the Efficacy of a Resident Run Continuity Clinic Reshma Gokaldas, Maheep Singh, Robert Fekete P4.278 Improving Patient Hand-Offs in a University Neurology Residency Program Catherine Porter, Lynn Chouhfeh, Alyssa Fiddler, Salomi Salins, Novreen Shahdad, Nicholas Silvestri P4.279 Standardized Patient Handoff Improves Resident Confidence and Patient Safety Justin Jordan, Steven Vernino P4.280 Timeliness of Neurology Consultations in the Emergency Department: A Quality Evaluation Samantha Holden, Steven Lewis P4.281 Lumbar Puncture: a Dying Procedure Among Neurologists? Elizabeth Flaherty, Aimee Szewka P4.282 Physician Compensation and Patient Satisfaction: Unintended Consequences of Policy Misalignment Jack Riggs, Kevin Riggs P4.283 Analysis of Inter-Provider Conflicts in Healthcare Mark Stecker, Mona Stecker Practice, Policy, and Ethics: Stroke, Critical Care, and Other P4.284 Timely Initiation of Therapeutic Hypothermia Following Cardiac Arrest: A Resident-Driven Quality Improvement Project Laura Rosow, S. Josephson P4.285 Re-evaluating Brain Death: The Potential for Treatment and Recovery After Brain Injury Philip Defina, Christine Zakrzewski, Charles Prestigiacomo, Calixto Machado, Peter Bernad, James Halper, Jonathan Fellus P4.286 Are AHA/ASA Stroke Guidelines Evident Enough? Swaroop Pawar, Andrea Boan, M. Kamran Athar, Tanya Turan P4.287 Improving Secondary Stroke Prevention Following Acute Ischemic Stroke: A Practice Improvement Project. Andrea Harriott P4.288 Natural Language Processing Method Accurately Classifies and Extracts Unstructed Data from Stroke Admission and Progress Notes Daniel Franc P4.289 What’s the True Definition of an Adverse Event? Raghav Govindarajan P4.290 Improving Assessment and Documentation of Pain Management at University of Florida—Jacksonville. Denys Shapovalov, Nader Antonios P4.291 Quality Improvement Project on Hand Washing at Memorial Hermann Hospital Jitesh Kar, Kristin Brown, Terry Walker, Janete Sheiner, Janelle Headley, Allison Murphy, Stephanie Cooper, Enedra Allen-McBride, Miriam Morales, Paul Schulz Global Health and Infection P4.292 Helping Haiti: Addressing the Burden of Neurologic Disease Veronica Santini, Anthony Alessi, Elaine Jones, Mill Etienne, Anna Hohler P4.293 Cognitive and Neurodegenerative Disorders in Adults in Africa: A Systematic Review Hannah McLane, Tarun Singhal, Joel Negin, Neelum Aggarwal, Anhar Hassan, Farrah Mateen P4.294 Epidemiology and Etiology of Acute Infectious Neurologic Disease (AIND) in Singapore Kevin Tan, Monica Chan, Nadika Wijesoma, Peng Soon Ng, Ambihai Sivalingam, Tianrong Yeo, Yee-Sin Leo, October Sessions, Eng-Eong Ooi, Duane Gubler, Umapathi Thirunagnam, James Sejvar Fast, Easy Registration Online · AAN.com/view/AM14 87 Wednesday April 30 First Authors stand by Posters from 7:30 a.m.–9:00 a.m. Wednesday, April 30 P4.295NeurologicManifestations of Neglected Tropical Diseases Pooja Raibagkar, Aaron Berkowitz, Bobbi Pritt, E. Tessa Headley-Whyte, Farrah Mateen P4.296 Aspirin for Acute Stroke of Undetermined Etiology in Resource-limited Settings: A Decision Analysis Aaron Berkowitz, M. Westover, Matt Bianchi, Sherry Chou P4.297 Risk Factors for Cerebral Palsy in Botswana David Bearden, Baphaleng Monokwane, Dennis Kolson, Greg Bisson P4.298 Variations in Brain Death Declaration: A Worldwide Survey Sarah Wahlster, Eelco Wijdicks, Pratik Patel, David Greer, Claude Hemphill, Farrah Mateen P4.299 Neurology International Residents Videoconference and Exchange (NIRVE) Mary Jane Lim Fat, Manav Vyas, Jenny Tsai, Mark Kinach, Tim Patterson, Morris Freedman P4.300 International Affiliation as a Tool to Improve the Quality and Safety of Inpatient Care. Experience Neurological Center, the American British Cowdray Medical Center. Mexico City Aurelio Mendez, Roberto Alfonso De Leo-Vargas, Alejandro Alfonso-Díaz, Guillermo ReyesCaballero, Marco Alegria, Patricia ConchaHein, Claudia Cabrera P4.301 International Electives in Neurology Training: A Survey of U.S. and Canadian Program Directors Jennifer Lyons, Mary Coleman, John Engstrom, Farrah Mateen P4.307 Central and Peripheral Markers of Neurodegeneration and Monocyte Activation in HIV-Associated Neurocognitive Disorders Jennifer McGuire, Alexander Gill, Steven Douglas, Dennis Kolson P4.308 The Effects of a Novel Interferon Inhibitor in a Model of HIV Encephalitis William Tyor, Cari Lessing, Ramzi Shawahna, Jennifer Ward, Leonard Maroun P4.309 Biochemical Evidence of Neuronal Injury in HIV Patients with Normal Neurocognitive Function Defines Pre-symptomatic Stage Gloria Von Geldern, Caroline Anderson, Ned Sacktor, Justin McArthur, Avindra Nath P4.310 Establishment of a Multi-disciplinary Platform for HIVinfected Patients with Neurological Complications Renaud Du Pasquier, Samanta Simioni, Deolinda Alves, Reto Meuli, Giorgio Maccaferri, Alexandre Berney, Matthias Cavassini P4.311 Clinical and Bacteriological Features of Central Nervous System Tuberculosis in Patients with HIV-Infection in Siberian Region of Russia Yury Bykov, Tatiana Filippova, Olga Novitskaya Viral Encephalitis and Progressive Multifocal Leukoencephalopathy P4.312 NeuroAIDS Analysis of YouTube as a Source of Information for West Nile Virus Infection Anshudha Sawhney, Divyanshu Dubey, Amod Amritphale, Nupur Amritphale P4.302 P4.313 Risk Factors for Epilepsy in Children with HIV/AIDS in Botswana David Bearden, Greg Bisson, Dennis Kolson, Andrew Steenhoff, Sudha Kessler, Dennis Dlugos P4.303 Stroke in Children with Human Immunodeficiency Virus in Botswana: A Report of Six Cases Esha Khurana, David Bearden P4.304 The Risk of Large-Artery Atherosclerotic Stroke Is Proportionally Greater than Cardioembolic Stroke in HIV-Infected Individuals Compared to HIVUninfected Controls Felicia Chow, Richard Price, Priscilla Hsue, Anthony Kim P4.305 Neurological Disease Presentations in an Out-patient Setting in the Effective Antiretroviral Therapy Era Samitha Fernando, Matthew Poynton, Alex Everitt, Alan Winston P4.306 Deficiency of Brain Heme Oxygenase-1 in HIV-Infected Individuals: Potential Target for Adjunctive Therapy Alexander Gill, Suren Ambegaokar, Colleen Kovacsics, Stephanie Cross, Benjamin Gelman, Dennis Kolson 88 HSV 2 Encephalitis Presenting as Episodic Receptive Aphasia Mohamad Ezzeldin, Ahmed Yassin, Merry Chen P4.314 Diagnostic Delay in a Case of HSV Encephalitis Janhavi Modak, Kevin McMahon, Avinash Prasad P4.315 HHV6 Encephalitis Complicating Post Stem Cell Transplantation Course: A Case Series of Five Leukemic Patients Ahmed Yassin, Tummala Sudhakar P4.316 Eastern Equine Encephalitis in a Patient Treated with Rituximab: Clinical Presentation and Histopathology Shibani Mukerji, Pedro Ciarlini, Sandro Santagata, Umberto De Girolami, Sashank Prasad P4.317 Magnetic Resonance Imaging and Electroencephalograhic Characteristics in Two Cases of Fatal Eastern Equine Encephalitis (EEE) Mohamed-Ali Babi, Angela Applebee, Robert Shapiro, Todd Raleigh, Joseph McSherry P4.318 Thrombocytopenia as a Prognostic Factor in Encephalitis Anthony Asemota, Kiran Thakur, Romergryko Geocadin, Arun Venkatesan 7:30 a.m.–11:00 a.m. P4.319 Progressive Multifocal Leukoencephalopathy Associated with Ofatumumab Presenting as Alexia Without Agraphia: A Case Report Jose Avila, Jennifer Han, Islam Zaydan P4.320 Non-HIV PML: A Case of PML in an Immunocompetent Patient with a Retrospective Review on Non-HIV PML Risk Factors Barbara Graves, William Bambach, Rebecca Hosey, Jonathan Hosey P4.321 A Unique Case of Progressive Multifocal Leukoencephalopathy in a Patient with Chronic Lymphocytic Leukemia Who Has Never Received Chemotherapy Jared Noroozi, Sonia Lal, Brij Ahluwalia-Singh, Ramandeep Sahni Child Neurology and Developmental Neurology IV P4.322 Diagnostic Yield of Pediatric EMG in Myopathic Disorders Partha Ghosh, Eric Sorenson P4.323 Can You Fine Tune the Ketogenic Diet Jessica Selter, Zahava Turner, Sarah Doerrer, Eric Kossoff P4.324 Occipital Headaches and Neuroimaging in Children Joshua Bear, Amy Gelfand, Peter Goadsby, Nancy Bass P4.325 Infantile Cerebral Arterial Calcification Jennifer Chu, Shannon DiCarlo, Robert Zeller P4.326 Efficacy and Tolerability of Intravenous Lacosamide in Children Less Than 12 Years of Age Dimitrios Arkilo, Mary Gustafson, Jason Doescher, Frank Ritter P4.327 Methylphenidate Exerts DoseDependent Effects on Glutamate Receptors and Cognitive Behaviors Jia Cheng, Zhe Xiong, Lara Duffney, Sihang Liu, Zhen Yan P4.328 Neurologic Injury in Isolated Sulfite Oxidase Deficiency Thomas Bosley, Ibrahim Alorainy, Darren Oystreck, Khaled Abu-Amero, Mustafa Salih P4.329 The Epidemiology of Pediatric Open Brain Surgery in the United States. Shalini Selvarajah, Nicholas Carchedi, Edward Hammond, Marcelo Cerullo, Anthony Asemota, Joseph Canner, Eric Schneider P4.330 Hemodynamic Changes Associated with Interictal Epileptiform Activities Using Simultaneous Video Electro-encephalography (EEG)/Near Infrared Spectroscopy (NIRS) in Patient Self Control Study Kumar Sannagowdara P4.331 Management of Choreoathetosis Secondary to Sequential Herpes Simplex Virus Type-1 Infection and Anti-NMDA Receptor Encephalitis in a 6-Month-Old Girl Yefim YushvayevCavalier, Charles Nichter, Adolfo Ramirez Zamora 2O14 Scientific Abstract Listing and Annual Meeting Information P4.332 Eight-year Latency to Diagnosis in an Adolescent with Bilateral Basal Ganglia Germinomas Mimicking a Neurodegenerative Condition Anna Nordvig, Alexis Dallara, Arthur Mandel, Toni Pearson P4.333 3D Kinematic Gait Analysis in Mucopolysaccharidoses Igor Nestrasil, Christopher Fuller, Alia Ahmed, Elsa Shapiro, John Anderson P4.334 Correlation Between MRI Findings of Mesial Temporal Sclerosis and Histopathological Findings Judy Li, Steve Chung P4.335 Familial Episodic Encephalopathy, Dysarthria, and Paralysis Is Associated with a Dominantly Inherited Mutation in ATP1A3 Gyula Acsadi, Richard Young, Tara Newcomb, Benjamin Nelson, Louis Viollet, Kathryn Swoboda P4.336 Genetic Animal Models of Autism Based on Shank/ Mutation Molecules to Potential Therapeutics Craig Powell P4.337 Knockout of p75NTR in Cerebellar Purkinje Cells Results in an Autism-like Murine Phenotype Nina Schor, Deborah Cory-Slechta, Louis Lotta, Katherine Conrad P4.338 Exonic Deletion of SLC9A9 in Autism with Epilepsy Meeta Wagle, Jimmy Holder P4.339 High-Functioning Autistic Children Have Abnormal Stapedial Reflexes Richard Lukose, Randy Kulesza, Kevin Brown, Barber Carol P4.340 Delayed Low Level Visual Processing in Infants with Tuberous Sclerosis Complex (TSC) Pilar Pichon, Jordan Ko, Charles Nelson III, Shafali Jeste P4.341 Mean EEG Coherence in Infants at Risk for Autism Spectrum Disorder April Levin, Marc Shi, Helen Tager-Flusberg, Charles Nelson CNS and Disease Mechanisms in Humans and Animal Models P4.342 B Cells from Blood of Patients with Relapsing-Remitting Multiple Sclerosis Induce Apoptosis in Neurons In Vitro Robert Lisak, Liljana Nedelkoska, Hanane Touil, Joyce Benjamins, Beverly Bealmear, Riu Li, Hetoum Misirliyan, Amit Bar-Or Plenary Session Current as of 2/13/2014 Contemporary Clinical Issues Plenary Session ighlights issues most critical to practicing neurologists, including H abstracts related to new therapeutic developments, clinical applications of basic and translational research, and innovative technical developments. 9:00 a.m.–12:00 p.m. Moderator: Lisa M. DeAngelis, MD, FAAN Chair, Science Committee Comparison of Thrombolytic Treatment for Acute Ischemic Stroke Pre- and PostTelemedicine Implementation in the Spoke Hospital Setting William K. Mountford, PhD Premier Research Services, Wilmington, NC Discussant: Lee H. Schwamm, MD Massachusetts General Hospital, Boston, MA Epigenetic Therapy for Friedreich’s Ataxia: A Phase I Clinical Trial David R. Jacoby, MD, PhD BioMarin Pharmaceutical Inc., Novato, CA Discussant: Tetsuo Ashizawa, MD, FAAN University of Florida, Gainesville, FL Clinical Profile of the Orexin Receptor Antagonist Suvorexant for the Treatment of Insomnia in Phase-3 Clinical Trials William Herring, MD, PhD Merck Research Laboratories, North Wales, PA David B. Goldstein, PhD Duke University, Durham, NC Direct to Consumer Genetic Testing Discussant: Phyllis C. Zee, MD, PhD Northwestern University Medical School, Chicago, IL Jonathan Stone, MB, ChB, FRCP, PhD Western General Hospital, Edinburgh, United Kingdom Functional (Psychogenic) Disorders in Neurology Kenneth L. Marek, MD Institute for Neurodegenerative Disorders, New Haven, CT Parkinson’s Disease Progression Marker Initiative: Developing a Translational Toolbox for PD Progression For Full Abstracts and Bios for Plenary Speakers Visit AAN.com/view/SearchAM Fast, Easy Registration Online · AAN.com/view/AM14 89 Wednesday, April 30 S24 Diet and Hormonal Influences in Multiple Sclerosis 2:00 p.m. S24.001 Increased Archaea Species and Changes with Therapy in Gut Microbiome of Multiple Sclerosis Subjects Sushrut Jhangi, Roopali Gandhi, Bonnie Glanz, Sandra Cook, Parham Nejad, Doyle Ward, Ning Li, Georg Gerber, Lynn Bry, Howard Weiner 2:15 p.m. S24.002 Role of Melatonin in MS Pathogenesis Mauricio Farez, Santiago Mendez Huergo, Iván Mascanfroni, Gabriel Rabinovich, Francisco Quintana, Jorge Correale 2:30 p.m. S24.003 Investigation of Sex Differences in the Association Between Multiple Sclerosis Disease Severity and Hormonal Markers of Vitamin D, Obesity, and Testosterone. Riley Bove, Alexander Musallam, Brian Healy, Pejvak Soltany, Pia Kivisakk, Bonnie Glanz, Philip De Jager, Karen Miller, Tanuja Chitnis 2:45 p.m. S24.004 Body Mass Index and Multiple Sclerosis Risk. The Role of Leptin Jorge Correale, María Eugenia Balbuena Aguirre, Mauricio Farez 3:00 p.m. S24.005 Differential Effects of Vitamin D in GA- Versus IFN-Treated MS Patients Dalia Rotstein, Brian Healy, Muhammad Taimur Malik, Robert Carruthers, Alexander Musallam, Pia Kivisakk, Bonnie Glanz, Tanuja Chitnis 3:15 p.m. S24.006 Delayed−Release Dimethyl Fumarate and Pregnancy: Preclinical Studies and Pregnancy Outcomes Reported During the Clinical Development Program Ralf Gold, J. Theodore Phillips, Eva Havrdova, Amit Bar-Or, Ludwig Kappos, Janet Clarke, Huixing Yuan, Mark Novas, Jie Li, Marianne Sweetser, Nuwan Kurukulasuriya, Vissia Viglietta, Robert Fox 3:30 p.m. S24.007 Aromatic-Turmerone Induces Neural Stem Cell Proliferation In Vitro and In Vivo Michael Schroeter, Joerg Hucklenbroich, Klein Rebecca, Bernd Neumaier, Rudolf Graf, Gereon Fink, Maria Rueger S25 Cerebrovascular Disease and Interventional Neurology: Hemorrhage, Aneurysms, and Vascular Malformations 2:00 p.m. S25.001 Clinical Outcomes of Aneurysmal Subarachnoid Hemorrhage with Cocaine Use in the United States Santosh Murthy, Shreyansh Shah, Yogesh Moradiya, Aditi Shastri, Stelios Smirnakis 2:15 p.m. S25.002 CSF Diversion in Aneurysmal Subarachnoid Hemorrhage: How Low Should We Go? Jennifer Fugate, Alejandro Rabinstein, Eelco Wijdicks, William Freeman, Giuseppe Lanzino 2:30 p.m. S25.003 The SEDAN Score and the Risk of Intracerebral Hemorrhage in Monocenter-Study Toralf Brüning, Mohamed Al-Khaled 2:45 p.m. S25.004 Validation of the ICH Score in Hyperacute Intracerebral Hemorrhage Sebina Bulic, Nerses Sanossian, Sidney Starkman, David Liebeskind, Pablo Villablanca, Scott Hamilton, Robin Conwit, Jeffrey Saver S26 Biomarkers in Neuromuscular Diseases 2:00 p.m. S26.001 Quantitative Muscle Ultrasound: Comparison of Backscatter Versus Grayscale Methods in Duchenne Muscular Dystrophy Patients and Healthy Controls Irina Shklyar, Tom Geisbush, Aleksandar Mijailovic, Amy Pasternak, Nicole Visyak, Heather Szelag, Jim Wu, Basil Darras, Seward Rutkove, Craig Zaidman 2:15 p.m. S26.002 Basal Ganglia Involvement in Amyotrophic Lateral Sclerosis Peter Bede, Marwa Elamin, Susan Byrne, Russel McLaughlin, Kevin Kenna, Alice Vajda, Niall Pender, Daniel Bradley, Orla Hardiman 2:30 p.m. S26.003 Impaired Cortico-Ponto-Cerebellar Networks Underlie Pseudobulbar Affect In Motor Neuron Disorders Mary Kay Floeter, Rohan Katipally, Meredith Kim, Olivia Schanz, Stephen Matthew, Laura Danielian, Tianxia Wu, Edward Huey, Avner Meoded 3:00 p.m. S25.005 Vitamin C Depletion Is Spontaneous Intracerebral Hemorrhage Risk Factor. Stéphane Vannier, Ronzière Thomas, Ferré Jean-christophe, Jean Francois Pinel, Marc Verin 2:45 p.m. S26.004 Pre-symptomatic Loss of Cerebral White Matter Integrity in Those at Genetic Risk of Amyotrophic Lateral Sclerosis Martin Turner, Nicola Filippini, Varan Govind, Peter Andersen, Christine Stanislaw, Eliana Reyes, Sumaira Hussain, Joanne Wuu, Michael Benatar 3:15 p.m. S25.006 Spinal Cord Cavernous Malformations; 62-patient Retrospective Review to Define Disease Natural History Lindsy Williams, Kelly Flemming, Robert Brown 3:00 p.m. S26.005 Profiling of miRNAs in Cerebrospinal Fluid from Patients with Amyotrophic Lateral Sclerosis Akira Machida, Takuya Ohkubo, Atsunobu Tsunoda, Hidenori Matsuo, Yokota Takanori, Hidehiro Mizusawa 3:30 p.m. S25.007 Effect of Hyperosmolar Therapy on Outcome Following Spontaneous Intracerebral Hemorrhage: The ERICH Study Manan Shah, Jennifer Rasmussen, Lee Birnbaum, Charles Moomaw, Padmini Sekar, Jennifer Osborne, Esther Nanez, Anastasia Vashkevich, Daniel Woo 3:15 p.m. S26.006 Diagnostic Utility of p62 Immunohistochemistry for Differentiating s-IBM from PM Chiseko Ikenaga, Jun Shimizu, Hida Ayumi, Shoji Tsuji 3:30 p.m. S26.007 Clinical Patterns in NT5C1A Antibody Positive Sporadic Inclusion Body Myositis Patients Compared to Seronegative Patients Namita Goyal, Farzin Pedouim, Usman Alam, Sameen Enam, Farah Mozaffar, Tahseen Mozaffar 2:00 p.m.–3:45 p.m. S27 Dystonia, Tremor, and Other Movement Disorders 2:00 p.m. Presentation of Movement Disorders Research Award Recipient: Eduardo Tolosa, MD, PhD Barcelona, Spain 2:30 p.m. S27.003 Conversion from AbobotulinumtoxinA to IncobotulinumtoxinA Formulation of Botulinum Toxin: Clinic Experience in 257 Cases Donald Grosset, Elaine Tyrrell, Katherine Grosset 2:45 p.m. S27.004 Clinimetric Testing of the Modules for the Comprehensive Cervical Dystonia Rating Scale (CCDRS) Cynthia Comella, Joel Perlmutter, H. Jinnah, Charles Adler, Richard Barbano, Stewart Factor, Susan Fox, Christopher Goetz, Wendy Galpern, Joseph Jankovic, Laura Marsh, William Mcdonald, Stephen Reich, Ramon Rodriguez, Ami Rosen, William Severt, Tracy Waliczek, Glenn Stebbins 3:00 p.m. S27.005 Focused Ultrasound MR Guided Thalamotomy: 2 Year Follow-Up Safety and Efficacy Data Binit Shah, Diane Huss, Tiffini Voss, Johanna Loomba, Mohamed Khaled, Madaline Harrison, W. Jeffrey Elias 3:15 p.m. S27.006 Predictors of Subjective Disability in Functional Movement Disorders Tracy Fulton, Kathrin LaFaver, Sarah Kranick, Mark Hallett 3:30 p.m. S27.007 Clusterin CSF Levels in Differential Diagnosis of Neurodegenerative Disorders Hana Prikrylova Vranova, Eva Henykova, Michaela Kaiserova, Katerina Mensikova, Miroslav Vastik, Jan Mares, Petr Hlustik, Jana Zapletalova, Miroslav Strnad, David Stejskal, Petr Kanovsky S28 Aging, Dementia, and Cognitive and Behavioral Neurology: Dementia Genetics 2:00 p.m. Presentation of Norman Geschwind Prize in Behavioral Neurology Recipient: Roy Hamilton, MD, MS Philadelphia, PA 2:15 p.m. S28.002 Late-onset Alzheimer Disease Neuropathology Genomic Screen Identifies Novel Loci for Neuritic Plaque and Other AD Neuropathology Features Gary Beecham, Kara Hamilton, Gerard Schellenberg, Margaret Pericak-Vance, Thomas Montine 2:30 p.m. S28.003 Whole-exome Sequencing of Hispanic Early-onset Alzheimer Disease Families Identifies Rare Variants in Multiple Alzheimer-related Genes Christiane Reitz, Brian Kunkle, Badri Vardarajan, Martin Kohli, Adam Naj, Patrice Whitehead, William Perry, Eden Martin, Gary Beecham, John Gilbert, Lindsay Farrer, Jonathan Haines, Gerard Schellenberg, Margaret Pericak-Vance, Richard Mayeux 2:45 p.m. S28.004 The Dissection of High-Penetrance Variants in Extended Late-onset Alzheimer Disease Families by Wholeexome Sequencing Martin Kohli, Brian Kunkle, Adam Naj, Li-San Wang, Kara Hamilton, William Perry, Regina Carney, Patrice Whitehead, John Gilbert, Eden Martin, Gary Beecham, Jonathan Haines, Gerard Schellenberg, Stephan Zuchner, Margaret Pericak-Vance 3:00 p.m. S28.005 Transcript Profiling Analysis of Alzheimer’s Disease Brains. Mariet Allen, Daniel Serie, Michael Walsh, Sun Zhifu, Saurabh Baheti, Fanggeng Zou, High Seng Chai, Curtis Younkin, Julia Crook, Vernon Pankratz, Minerva Carrasquillo, Asha Nair, Sumit Middha, Sooraj Maharjan, Thuy Nguyen, Li Ma, Kimberly Malphrus, Sarah Lincoln, Gina Bisceglio, Christopher Kolbert, Jin Jen, Ronald Petersen, Neill Graff-Radford, Dennis Dickson, Steven Younkin, Yan Asmann, Nilufer Taner 3:15 p.m. S28.006 Investigation of Transcriptional Regulation at the Alzheimer’s Disease Risk Loci. Michaela Kachadoorian, Mariet Allen, Aditya Karhade, Lester Manly, Fanggeng Zou, High Seng Chai, Curtis Younkin, Julia Crook, Vernon Pankratz, Minerva Carrasquillo, Asha Nair, Sumit Middha, Sooraj Maharjan, Thuy Nguyen, Li Ma, Kimberly Malphrus, Sarah Lincoln, Gina Bisceglio, Christopher Kolbert, Jin Jen, Ronald Petersen, Neill Graff-Radford, Steven Younkin, Dennis Dickson, Nilufer Taner 3:30 p.m. S28.007 Screening for NOTCH3 Mutation in Patients with Subcortical Vascular Cognitive Impairment Cindy Yoon, Young-Eun Kim, Jong-Won Kim, Duk L. Na, Chang-Seok Ki, Sang Won Seo 90 2O14 Scientific Abstract Listing and Annual Meeting Information Scientific Sessions S30 Education, Research, and History 2:00 p.m. Presentation of Dreifuss-Penry Epilepsy Award 2:00 p.m. Presentation of Lawrence C. McHenry Award: An Award for the History of Neurology Recipient: Catherine Schevon, MD, PhD New York, NY Recipient: Farrah Mateen, MD, PhD Boston, MA 2:15 p.m. S29.002 The Role of Toll-like Receptor 3 in Epileptogenesis Felix Benninger, Adi Gross, Israel Steiner, Daniel Offen, Eitan Okun 2:30 p.m. S29.003 Association Between Human Herpes Virus 6 and Hippocampal Volume in Mesial Temporal Lobe Epilepsy William Theodore, Emily Leibovitch, Bridgette Billioux, Sierra Germeyan, David Kalikhman, Sara Inati, John Heiss, Kareem Zaghloul, Steven Jacobson 2:45 p.m. S29.004 Sequential Versus Simultaneous Polytherapy in the Treatment of Status Epilepticus Claude Wasterlain, Roger Baldwin, Jerome Niquet, Lucie Suchomelova 3:00 p.m. S29.005 Etiology of Pediatric Refractory Convulsive Status Epilepticus. Results from the Pediatric Status Epilepticus Research Group (pSERG) William Gaillard, Howard Goodkin, Nicholas Abend, Satish Agadi, Ravindra Arya, Rajit Basu, Jessica Carpenter, Kevin Chapman, Nathan Dean, Tracy Glauser, Michele Jackson, Mohamad Mikati, Katrina Peariso, Geetanjali Rathore, Ivan Sanchez Fernandez, Robert Tasker, Alexis Topjian, David Turner, Angus Wilfong, Korwyn Williams, Tobias Loddenkemper Recipient: Christopher Boes, MD Rochester, MN 2:30 p.m. Presentation of S. Weir Mitchell Award Recipient: Michael Fox, MD, PhD Newton, MA 2:45 p.m. S30.004 The Effects of Repeated Quizzing on Long-Term Retention in AAN Annual Meeting Courses Douglas Larsen, Wint Yan Aung, John Corboy, Deborah Friedman, Ann Tilton, Andrew Butler 3:00 p.m. S30.005 Osler, MacNalty, and the Recognition of Encephalitis Lethargica in England Christopher Boes 3:15 p.m. S30.006 Closing the Loop: Mount Sinai Neurology Resident Clinical Acumen Assessment Project Sarah Zubkov, Rachel Brandstadter, Christine Hannigan, Stephen Krieger 3:30 p.m. S30.007 Development of a Simulated Patient Exercise to Improve Acute Stroke Care by Neurology Residents Adam Kelly, Ralph Jozefowicz S31 General Neurology I 2:00 p.m. S31.001 Gadolinium Enhancement in Spondylotic Myelopathy Mimicking Tumors and Inflammation: A Case Series of 56 Patients Eoin Flanagan, Karl Krecke, Richard Marsh, Caterina Giannini, Mark Keegan, Brian Weinshenker 2:15 p.m. S31.002 GLACIER: an Open-label, Randomized, Multicenter Study to Assess Safety and Tolerability of Glatiramer Acetate 40 mg/1mL 3-times Weekly Versus 20 mg/1mL Daily in Patients with Relapsing-Remitting Multiple Sclerosis Wolinsky Jerry, Thor Borresen, Dennis Dietrich, Beverly Gilder, Yulia Sidi, Volker Knappertz, Scott Kolodny 2:30 p.m. S31.003 24-Month Efficacy and Safety of Glatiramer Acetate 40mg/1mL 3-Times Weekly: Open-label Extension Study of the GALA Trial in Subjects with Relapsing-Remitting Multiple Sclerosis Omar Khan, Peter Rieckmann, Alexey Boyko, Krzysztof Selmaj, Hadas Barkay, Scott Kolodny, Robert Zivadinov 2:45 p.m. S31.004 B Cell-specific Signal in Whole Blood and Serum of NatalizumabTreated PML Patients Is Revealed Using Transcript and Protein Profiling Tatiana Plavina, John Carulli, Huo Li, Daniel Park, Raghavendra Hosur, Normand Allaire, Peter Juhasz, Teresa Compton 3:00 p.m. S31.005 Neuroimaging and Clinical Features in Late Onset Alexander Disease Jonathan Graff-Radford, Kara Schwartz, Ralitza Gavrilova, Daniel Lachance, Neeraj Kumar 3:15 p.m. S29.006 Hippocampal Malrotation Is Associated with Chromosome 22Q11.2 Microdeletion Anne Bassett, Timo Krings, Eva Chow, Tim-Rasmus Kiehl, Danielle Andrade 3:15 p.m. S31.006 Dosing Feasibility and Pharmacokinetics by Seizure Type and Status, and Tolerability of Intranasal Diazepam in Adults with Epilepsy Michael Sperling, Hussam Seif Eddeine, Kevin Haas, Gregory Krauss, Herbert Henney III, Adrian Rabinowicz, Gary Bream, David Squillacote, Enrique Carrazana 3:30 p.m. S29.007 Structural and Functional Implications of Modeling Non Synonymous Mutations in Patients with SCN1A-related Seizure Disorders Mu Gao, Hongyi Zhou, Izabela Karbassi, Khalida Liaquat, Daniel Fischer, Jeffrey Skolnick, Joseph Higgins 3:30 p.m. S31.007 Dextromethorphan and Quinidine for Treatment of Pseudobulbar Affect (PBA): Time Course of PBA Episode Remission Andrea Formella, Benjamin Brooks S32 Headache: Basic Science and Imaging 2:00 p.m. Presentation of Harold Wolff-John Graham: An Award for Headache/Facial Pain Research Recipient: Jakob Møller Hansen, MD, PhD Los Angeles, CA 2:15 p.m. S32.002 Ictal Lack of Binding of (11C)Dihydroergotamine to Brain Parenchyma Suggests That the Blood-Brain Barrier Remains Intact During Migraine Attacks Christoph Schankin, Farooq Maniyar, Youngho Seo, Shashidar Kori, Michael Eller, Joseph Blecha, Stephanie Murphy, Till Sprenger, Henry VanBrocklin, Peter Goadsby 2:30 p.m. S32.003 Multi-Center 3T MRI Study of Thalamic Morphology in Migraine Using Label-Fusion-Based Segmentation and Deformation Based Morphometric Surface Analysis Stefano Magon, Arne May, Anne Stankewitz, Peter Goadsby, Amy Tso, Messoud Ashina, Faisal Amin, Christian Seifert, Mallar Chakravarty, Jannis Müller, Till Sprenger 2:45 p.m. S32.004 Enhanced Pain-Induced Activation of Pain Processing Regions in Interictal Episodic Migraine Todd Schwedt, Catherine Chong, Chia-Chun Chiang, Leslie Baxter, Bradley Schlaggar, David Dodick 3:00 p.m. S32.005 Therapeutic Efficacy of Transcranial Direct Current Stimulation in Trigeminal Neuralgia Mark Obermann, Vera Bude, Dagny Holle, Tim Hagenacker, H. Diener, Zaza Katsarava 3:15 p.m. S32.006 Interictal Resting-State Connectivity of the Insula Is Altered in Migraine Without Aura Amy Tso, Andrew Trujillo, Christine Guo, Peter Goadsby, William Seeley 3:30 p.m. S32.007 Autonomic Dysfunction in Migraine: Comparison Between Populations With and Without Orthostatic Intolerance Mark Stillman, Lan Zhou, Fetnad Fouad-Terazi S33 Cognition Fatigue in MS 2:00 p.m. S33.001 Processing Speed Test (PST): A Self-Administered iPad®-Based Tool for Assessing MS-Related Cognitive Dysfunction Stephen Rao, Jay Alberts, Deborah Miller, Francois Bethoux, Jar-Chi Lee, Darlene Stough, Christine Reece, Lyla Mourany, David Schindler, Joshua Hirsch, Richard Rudick 2:15 p.m. S33.002 Structural MRI Corrrelates of Cognitive Impairment in Patients with Multiple Sclerosis: A Multi Center Study Paolo Preziosa, Maria Rocca, Matteo Atzori, Frederik Barkhof, Nicola De Stefano, Christian Enzinger, Franz Fazekas, Antonio Gallo, Hanneke Hulst, Laura Mancini, Xavier Montalban, Elisabetta Pagani, Alex Rovira, Maria Laura Stromillo, Gioacchino Tedeschi, Giancarlo Comi, Massimo Filippi 2:30 p.m. S33.003 A Longitudinal Evaluation of MRI Predictors of Cognitive and Clinical Impairment in Multiple Sclerosis Alfredo Damasceno, Benito Damasceno, Fernando Cendes 2:45 p.m. S33.004 Longitudinal Evaluation of Cognitive Functioning in Pediatric Multiple Sclerosis (MS): Report from the U.S. Pediatric Multiple Sclerosis Network Lauren Krupp, Leigh Charvet, Ellen O’Donnell, Rebecca Cleary, Dana Serafin, Joy Parrish, Laura Julian, Natalie Baruch, Anita Belman, Ralph Benedict, Tanuja Chitnis, Jayne Ness, Moses Rodriguez, Emmanuelle Waubant, Bianca Weinstock-Guttman 3:00 p.m. S33.005 Longitudinal Evidence for Brain Reserve and Cognitive Reserve in Multiple Sclerosis: Larger Maximal Lifetime Brain Growth and Greater Intellectual Enrichment Attenuate Cognitive Decline Over 4.5 Years James Sumowski, Maria Rocca, Victoria Leavitt, Jelena Dackovic, Sarlota Mesaros, Jelena Drulovic, John DeLuca, Massimo Filippi 3:15 p.m. S33.006 Social Cognition in Pediatric Multiple Sclerosis (MS) Leigh Charvet, Rebecca Cleary, Katherine Vazquez, Livana Koznesoff, Kate Bartolotta, Jeremy Benhamroun, Lauren Krupp 3:30 p.m. S33.007 Deep Transcranial Magnet Stimulation Can Improve Depression and Fatigue in Multiple Sclerosis—a Clinical Phase I/IIa Study Sven Schippling, Marina Tiede, Ina Lorenz, Caspar Pfueller, Jan Doerr, Judith Bellmann-Strobl, Abraham Zangen, Friedemann Paul, Gunnar Gaede Fast, Easy Registration Online · AAN.com/view/AM14 91 Wednesday April 30 S29 Epilepsy and Clinical Neurophysiology: Inflammation, Status Epilepticus, and Genetics Wednesday, April 30 I7 Emerging Therapeutic Advances in Multiple Sclerosis 2:00 p.m.–6:00 p.m. Coordinators: Robert J. Fox, MD, FAAN and Eric Klawiter, MD Invited Speaker Session: 2:00 p.m.–4:30 p.m. 2:00 p.m.–2:10 p.m.Introduction 2:10 p.m.–2:35 p.m. Treating Relapsing MS: Choosing Among the Options Myla Goldman, MD 2:35 p.m.–3:00 p.m. Treating Relapsing MS: Risk Stratification and Mitigation Bruce A. C. Cree, MD, PhD, MCR 3:00 p.m.–3:25 p.m. Is No Evidence of MS Disease Activity an Achievable Goal? Robert A. Bermel, MD 3:25 p.m.–3:50 p.m. Treating MS in 2020: Remyelination, Progressive MS, and Beyond Catherine Lubetzki, MD 3:50 p.m.–4:15 p.m. Treating Pediatric MS: Is It Different from Adults? Tanuja Chitnis, MD 4:15 p.m.–4:30 p.m. Questions and Answers Poster Rounds: 4:30 p.m.–5:30 p.m. I7-1.001 S1P Receptor Modulation by Fingolimod Promotes Human Oligodendrocyte Progenitor Cell Differentiation Through Cell-Autonomous and Non-Cell Autonomous Mechanisms via ERK1/2 and p38MAPK Activation Qiaoling Cui, Timothy Kennedy, Guillermina Almazan, Jack Antel I7-1.002 Peginterferon Beta-1a May Improve Recovery Following Relapses: Data from the Pivotal Phase 3 ADVANCE Study in Patients with Relapsing-Remitting Multiple Sclerosis Bernd Kieseier, Thomas Scott, Scott Newsome, Sarah Sheikh, Serena Hung, Xiaojun You, Bjorn Sperling I7-1.003 A Nasal Anti-CD3 Vaccine Treats a Model of Secondary Progressive MS by Inducing IL-10 Dependent T Regulatory Cells and Regulating CNS Innate Immunity Lior Mayo, Andre Pires Da Cunha, Raymond Sobel, Hans Lassmann, Francisco Quintana, Howard Weiner I7-1.004 Differential Effects of Vitamin D in GA- versus IFN-Treated MS Patients Dalia Rotstein, Brian Healy, Muhammad Taimur Malik, Robert Carruthers, Alexander Musallam, Pia Kivisakk, Bonnie Glanz, Tanuja Chitnis I7-1.005 Therapeutic Plasma Exchange in 90 GlucocorticosteroidUnresponsive Patients with Multiple Sclerosis—Prediction of Response Johannes Ehler, Martin Sauer, Sebastian Koball, Steffen Mitzner, Heiko Hickstein, Reiner Benecke, Uwe Zettl I7-1.006 A Phase II Trial of Neuroprotection with Riluzole in Early Relapsing-Remitting MS: Lessons for Future Neuroprotection Trials Emmanuelle Waubant, Amir-Hadi Maghzi, Nisha Revirajan, Rebecca Spain, Laura Julian, Ellen Mowry, Jacqueline Marcus, Shuang Liu, Ari Green, Charles McCulloch, Daniel Pelletier I7-1.007 The MIRROR Study: A Randomized, Double-blind, Placebocontrolled, Parallel-group, Dose-ranging Study to Investigate the Safety and MRI Efficacy of Subcutaneous Ofatumumab in Subjects with Relapsing-Remitting Multiple Sclerosis (RRMS) Amit Bar-Or, Richard Grove, Daren Austin, Jerry Tolson, Susan Vanmeter, Eric Lewis, Per Solberg Sorensen I7-1.009 Laquinimod Reduces Neuronal Injury Through Inhibiting Microglial Activation Voon Wee Yong, Manoj Mishra, Janet Wang, Michael Keough, Claudia Silva, Yan Fan, Scott Sloka, Liat Hayardeny I7-1.010 I7-1.008 Randomized Controlled Alemtuzumab Improves Visual Outcomes Versus Subcutaneous Interferon Beta-1a in Patients with Active Relapsing-Remitting Multiple Sclerosis (RRMS) Who Relapsed on Prior Therapy: Analysis from the CARE-MS II Study Jennifer Graves, Laura Balcer, Jeffrey Palmer, David Margolin, Steven Galetta 5:40 p.m. 5:45 p.m. I7-2.004 5:50 p.m. I7-2.005 Trial of CI Therapy for Progressive MS: Increased Real-World Function and Neuroplasticity on MRI Victor Mark, Edward Taub, Gitendra Uswatte, Gary Cutter, David Morris, Staci McKay, Mary Bowman, Michelle Haddad, Tyler Rickards, Chelsey Sterling Data Blitz: 5:30 p.m.–6:00 p.m. 5:30 p.m. I7-2.001 IRX4204: A Clinical Stage, Potent, and Highly Selective RXR Agonist Compound Is Brain Penetrant, and Promotes Differentiation of Oligodendrocyte Precursor Cells (OPCs) In Vitro Martin Sanders, Satish Medicetty, Rosh Chandraratna 92 5:35 p.m. I7-2.002 A Combination Trial of Estriol Plus Glatimer Acetate in Relapsing-Remitting Multiple Sclerosis Rhonda Voskuhl, HeJing Wang, T.C. Jackson Wu, Nancy Sicotte, Angela Bates, Gary Beaver, John Corboy, Anne Cross, Suhayl Dhib-Jalbut, Corey Ford, Barbara Giesser, Dina Jacobs, Sharon Lynch, Andrew Pachner, Michael Racke, John Ratchford, Anthony Reder, John Rose, Dean Wingerchuk, Margaret Burnett, Chi Hong Tseng, Robert Elashoff I7-2.003 Safety and Tolerability of Delayed-Release Dimethyl Fumarate Administered as Add-on Therapy to Beta Interferons or Glatiramer Acetate in Relapsing-Remitting Multiple Sclerosis (RRMS) Patients Vissia Viglietta, Timothy Vollmer, Ray Zhang, Mark Novas, Sarah Sheikh, Robert Fox 2O14 Scientific Abstract Listing and Annual Meeting Information Deep Transcranial Magnet Stimulation Can Improve Depression and Fatigue in Multiple Sclerosis—a Clinical Phase I/ IIa Study Sven Schippling, Marina Tiede, Ina Lorenz, Caspar Pfueller, Jan Doerr, Judith Bellmann-Strobl, Abraham Zangen, Friedemann Paul, Gunnar Gaede Stopping Disease Modifying Therapy in Progressive Multiple Sclerosis—a Prospective Study Gary Birnbaum Integrated Neuroscience Sessions I8 Clinical Decision Making After the Dust Settles on Clinical Trials 2:00 p.m.–6:00 p.m. Coordinators: Barbara G. Vickrey, MD, MPH, FAAN and Linda S. Williams, MD, FAAN Invited Speaker Session: 2:00 p.m.–4:30 p.m. 2:00 p.m.–2:10 p.m.Introduction 2:10 p.m.–2:40 p.m. Intervention Research on Improving Access to and Quality of Neurologic Care Ray Dorsey, MD, MBA 2:40 p.m.–3:10 p.m. Effectiveness Research in Neurology Seemant Chaturvedi MD, FAAN, FAHA 3:10 p.m.–3:40 p.m. Translating Neurologic Advancements into Practice through Decision Support Eric M. Cheng MD, MS, FAAN 3:40 p.m.–4:10 p.m. Research on Incorporating Patient Preferences in Neurologic Care Adam Kelly, MD 4:10 p.m.–4:30 p.m. Questions and Answers Poster Rounds: 4:30 p.m.–5:30 p.m. Patients’ Preferences for Communication About Advanced Care Planning Keiran Tuck, Lissa Brod, John Nutt, Erik Fromme I8-1.002 Vascular Parkinsonism in a Tertiary Care Stroke Prevention Clinic: Prevalence and Development of a New Screening Strategy Herbert Manosalva Alzate, Thomas Jeerakathil, Maher Saqqur, Richard Camicioli, Oksana Suchowersky I8-1.003 Multiple Sclerosis Documentation System MSDS3D— Innovative Management of Patients with Multiple Sclerosis Judith Eisele, Raimar Kern, Suhrbier Alexander, Lars Großmann, Thorsten Schultheiss, Tjalf Ziemssen I8-1.004Neuro-oncology Telemedicine Follow-up Visits Richard Green, Emily Woyshner, Amanda Hauser Dehaven I8-1.005 Long Term Efficacy of Outpatient Interdisciplinary Treatment for Patients Suffering from Chronic Headaches Mark Stillman, Steven Krause I8-1.006 Adherence to Oral I8-1.008 Treatment Trends in I8-1.007 Influence of CREST on I8-1.009 Antiepileptic Drug 5:40 p.m. I8-2.003 5:50 p.m. 5:45 p.m. I8-2.004 Migraine Preventive Medications Among Patients with Chronic Migraine: Analysis of a Large US Health Insurance Claims Database Zsolt Hepp, David Dodick, Sepideh Varon, Patrick Gillard, Ryan Hansen, Emily Devine CEA and CAS Trends in Women—Do the Results Matter? Shahram Khalid, Sanath Reddy, Seemant Chaturvedi, Kumar Rajamani, Pratik Bhattacharya, Navid SerajiBozorgzad Management of Intracranial Stenosis in the Pre- and Post-sammpris Era Swaroop Pawar, Tanya Turan, George Cotsonis, Michael Lynn, Rahim Wooley, Barney Stern, Colin Derdeyn, David Fiorella, Marc Chimowitz Prescribing for OEF/OIFVeterans with NewOnset Epilepsy: 2008-2010 Mary Jo Pugh, Anne Van Cott, Christine Baca, Megan Amuan Data Blitz: 5:30 p.m.–6:00 p.m. 5:30 p.m. I8-2.001 Identifying Palliative Care Needs in the Neurological Intensive Care Unit Claire Creutzfeldt, J Curtis 5:35 p.m. I8-2.002 Appropriateness of Dopamine Antagonist Prescribing in Hospitalized Patients with Dopamine Requiring Diseases After Implementation of an Automated Prescribing Alert System Marie Morris, Allison Willis, Franklin McCann, Angela Birke, Brad Racette Development and Implementation of a Quality Improvement Strategy for Obtaining Muscle Biopsies Utilizing DMAIC Methodology Charles Kassardjian, Michelle Williamson, Dorothy Van Buskirk, Floranne Ernste, Andrea Leep Hunderfund A Comparison of Co-located and Traditional Outpatient Consultation for the Treatment of ADHD in Two Urban Medical Homes: Costs and Outcomes David Urion I8-2.005 Malformation Risks of Antiepileptic Drug Monotherapies in Pregnancy: An Update From the UK and Ireland Epilepsy and Pregnancy Registers Ellen Campbell, Fiona Kennedy, Aline Russell, W Smithson, Linda Parsons, Beth Irwin, Brenda Liggan, Norman Delanty, Patrick Morrison, Stephen Hunt, John Craig, Jim Morrow Fast, Easy Registration Online · AAN.com/view/AM14 93 Wednesday April 30 I8-1.001 Parkinson’s Disease Wednesday, April 30 P5 Poster Session V First Authors stand by Posters from 5:00 p.m.–6:30 p.m. 3:00 p.m.–6:30 p.m. oster Discussion Session: P Cerebrovascular Disease and Interventional Neurology II Utilizing a guided tour format, topic experts will lead attendees around the ten posters in the poster discussion session and facilitate questions with poster authors during the 90-minute author stand-by time. P5.001 MRI Detection of Blood After Perimesencephalic Subarachnoid Hemorrhage Jordan Samuels, James Conners, Sarah Song, Shawna Cutting, Vivien Lee P5.002 Use of Apixaban and Warfarin in Patients Undergoing Procedures: Insights from ARISTOTLE Renato Lopes, David Garcia, Daniel Wojdyla, Paul Dorian, John Alexander, Lars Wallentin, Fernando Lanas, Michael Hanna, Claes Held, Christopher Granger P5.004 Oral Anticoagulant Therapy Is Associated with Cerebral Microbleeds Saloua Akoudad, Sirwan Darweesh, Maarten Leening, Peter Koudstaal, Albert Hofman, Aad Van Der Lugt, Bruno Stricker, Mohammad Ikram, Meike Vernooij P5.005 The Incidence of Secondary Stroke Prevention Medication Following Hospitalization for Ischemic Stroke Justin Blackburn, Hong Zhao, Meredith Kilgore, Karen Albright P5.006 Effects of Angiopoietin-1 on Hemorrhagic Transformation and Cerebral Edema After Tissue Plasminogen Activator Treatment for Ischemic Stroke Masato Kanazawa, Kunio Kawamura, Tetsuya Takahashi, Hironaka Igarashi, Tsutomu Nakada, Masatoyo Nishizawa, Takayoshi Shimohata P5.008 P5.007 P5.009 The Influence of Obesity on Outcomes After Intravenous Thrombolysis for Acute Ischemic Stroke AV Nickles, Saqib Chaudry, Syed Hussain, M J Reeves P5.003 Effect of Apixaban on AllCause Mortality in Atrial Fibrillation: An Imputed Placebo Analysis John McMurray, Robert Hart, Greg Flaker, Renato Lopes, Junyuan Wang, Michael Hanna, John Alexander, Christopher Granger, Lars Wallentin A Utility-Weighted Modified Rankin Scale: Derivation and Application to Completed Stroke Trials Napasri Chaisinanunkul, Jeffrey Saver, Tudor Jovin, Scott Berry, Roger Lewis, Kennedy Lees, Anthony Furlan, Blaise Baxter, Helmi Lutsep, Marc Ribo, Olav Jansen, Rishi Gupta, Vitor Pereira-Mendes, Raul Nogueira Geography of Stroke Mortality: Hotspotting Areas for Targeted Interventions Catherine Wolff, Michael Mullen, Douglas Wiebe, Charles Branas, Brendan Carr P5.010 Predictors of Neurological Deficit After Endovascular Treatment of Cerebral Arteriovenous Malformations and Functional Repercussion in Prospective Follow-Up Juan Carlos Llibre, Jose Antonio Jordan NEW! e Poster Session: MS and CNS Inflammatory Disease II The ePoster session will feature a selection of posters to be presented digitally, rather than in the traditional format. Authors will be able to take advantage of the format to highlight compelling visual features such as images and videos. See poster map on page 47 for location. P5.011 Therapeutic Plasma Exchange in 90 Glucocorticosteroid-unresponsive Patients with Multiple Sclerosis— Prediction of Response Johannes Ehler, Martin Sauer, Sebastian Koball, Steffen Mitzner, Heiko Hickstein, Reiner Benecke, Uwe Zettl P5.012 MRI Detection of Pial and Subpial Abnormalities in the MS Spinal Cord Hugh Kearney, Marios Yiannakas, Rebecca Samson, Claudia WheelerKingshott, Olga Ciccarelli, David Miller P5.013 Phenotypic Differences in the Distribution of Gray Matter Lesions in Multiple Sclerosis and Their Relevance to Cognition Varun Sethi, Tarek Yousry, Nils Muhlert, Daniel Tozer, Daniel Altmann, Maria Ron, Claudia Wheeler-Kingshott, David Miller, Declan Chard P5.014 EDSS and MSFC Incompletely Capture Patient Reported Disability in a Longitudinal Cohort of Patients with Multiple Sclerosis Carolyn Bevan, Pierre-Antoine Gourraud, Monica Bucci, Regina Schlaeger, Refujia Gomez, Caroline Ciocca, Rachel Kanner, William Stern, Alan Evangelista, Samuel Arnow, Aya Abounasr, Adam Santaniello, Jeffrey Gelfand, H. Von Budingen, Ari Green, Douglas Goodin, Sergio Baranzini, Stephen Hauser, Roland Henry, Bruce Cree 94 P5.015 The Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS): Normative Values with Gender, Age and Education Corrections in the Italian Population Maria Pia Amato, Emilio Portaccio, Claudia Niccolai, Bahia Hakiki, Benedetta Goretti, Andrea Sturchio, Vittorio Martinelli, Monica Falautano, Eleonora Minacapelli, Ugo Nocentini, Chiara Incerti, Maria Marrosu, Eleonora Cocco, Monica Murgia, Giuseppe Fenu, Ferdinando Ivano Ambra, Elisabetta Garofalo, Maurizio Maddestra, Marilena Consalvo, Giovanni Zimatore, Nunzia Alessandra Losignore, Alessandra Lugaresi, Erika Pietrolongo, Rosa Viterbo, Maria Trojano P5.016 Vitamin D as Predictor of Multiple Sclerosis Activity and Progression in Patients with CIS Treated Early with Interferon Beta-1b Alberto Ascherio, Kassandra Munger, Rick White, Karl Kochert, Kelly Claire Simon, Mark Freedman, Hans Hartung, David Miller, Xavier Montalban, Gilles Edan, Frederik Barkhof, Dirk Pleimes, Rupert Sandbrink, Ludwig Kappos, Christoph Pohl P5.017 A Phase II Trial of Neuroprotection with Riluzole in Early Relapsing-Remitting MS: Lessons for Future Neuroprotection Trials Emmanuelle Waubant, Amir-Hadi Maghzi, Nisha Revirajan, Rebecca Spain, Laura Julian, Ellen Mowry, Jacqueline Marcus, Shuang Liu, Ari Green, Charles McCulloch, Daniel Pelletier P5.018 Implicating MicroRNAs as Regulators of Microglia and Astrocyte Responses in Human CNS Inflammatory Disease Craig Moore, Vijayaraghava Rao, Shih-Chieh Fuh, Barry Bedell, Samuel Ludwin, Amit Bar-Or, Jack Antel P5.019 Grey Matter Expression of Fetuin-A Correlates with Cortical Demyelination in Multiple Sclerosis Mark Landy, Ying Liu, Violaine Harris, Saud Sadiq P5.020WITHDRAWN 2O14 Scientific Abstract Listing and Annual Meeting Information Poster Session V P5.035 P5.048 P5.021 The Utility of Paraneoplastic Serology in the Saskatoon Health Region Ilia Poliakov, Gary Hunter Is Intracranial Arterial Involvement a Subgroup of Neuro-Behcet Syndrome? Burcu Zeydan, Ugur Uygunoglu, Melih Tutuncu, Cengiz Yalcinkaya, Ayse Altintas, Sabahattin Saipoglu, Aksel Siva America’s First Epilepsy Journal: Transactions of the National Association of the Study of Epilepsy and Care and Treatment of Epileptics Edward Fine, Alyssa Fiddler Epilepsy and Clinical Neurophysiology (EEG): Epidemiology and Health Care Utilization P5.022 P5.036 P5.049 P5.062 Isolated Cerebral Mucormycosis: A Case Report Monica Dhakar, Mahmoud Rayes, Kupsky Williams, Alexandros Tselis, Gregory Norris P5.023 Role of Neurological Consultation in Evaluating Syncope Adithya Sivaraju, Appaji Rayi, David Marks P5.024 Anomalous Origins of Bilateral Anterior Cerebral Arteries (ACA) from the Cavernous Internal Carotid Arteries (ICA). Swetha Pedavally, Matthew Omojola P5.025 A Case Report of a Transient Lesion of the Splenium Resulting from Vasospasm Secondary to Pituitary Apoplexy Tooba Fayyaz, Jocelyn Cheng P5.026 Rare Neurological Complications After Epidural Anesthesia in Obstetric Patients: 2 Case Reports Gayane Melikyan, Naveed Akhtar, Saadat Kamran, Hassan Al-hail, Dirk Deleu P5.027 Tongue Abnormalities on MRI Associated with Severity and Progression in ALS César Escamilla, Hector Martinez, Jorge Moreno-Cuevas, Maria Teresa Gonzale-Garza, Sergio Salazar Marioni, Alfonso Gil Valadez P5.028 Management Standardization of Limbic Encephalitis and Rapidly Progressive Dementia Elmoatazbellah Ibrahim, Joel Phillips, Andrew Biondo P5.029 Anti-Aquaporin 4 Autoantibodies in Patients with Systemic Lupus Erythematosus Without CNS Involvement: A long-term assessment Ioanna Tatouli, Harry Alexopoulos, Sofia Akrivou, Athanasios Tzioufas, Marinos Dalakas P5.037 Clinical Prodromes of Neurodegeneration in Anderson-Fabry Disease Matthias Löhle, Alan Milligan, Linda Richfield, Heinz Reichmann, Derralynn Hughes, Atul Mehta, Anthony Schapira P5.038 This Is a Novel Case a Variant of Miller-Fisher Syndrome with a Positve Anti-GQ1b Antibody Presenting as Parinaud’s Syndrome. Rick Magun, Jamie Silva P5.039 Evaluating the True Clinical Relevance of Genomic Intervals Associated with Amyotrophic Lateral Sclerosis Kevin Kenna, Russell Mc Laughlin, Susan Byrne, Marwa Elamin, Mark Heverin, Elaine Kenny, Paul Cormican, Derek Morris, Colette Donaghy, Daniel Bradley, Orla Hardiman P5.040 Alcoholic Wernicke’s Encephalopathy with Cranial Nerve XII Involvement on MRI Maya Lichtenstein, Dan Nguyen P5.041 Delayed Recognition of POEMS Hai Chen, Benjamin Greenberg, Steven Vernino First-time Seizure or Seizurelike Presentations in U.S. Adult Emergency Departments 2007-2010 Wenyu Sun, Anbesaw Selassie, Paul Pritchard P5.050 Necessity of Emergency Medical Care for Patients with Epilepsy Presenting with Typical Seizures Timothy Rust, Bassel Shneker P5.051 Economic Outcomes in Patients Receiving Anti-epileptic Drug (AED) Adjunctive Therapy Zhixiao Wang, Xuan Li, Annette Powers, Jose Cavazos Epilepsy and Clinical Neurophysiology: EEG P5.052 Utility of After Hours Emergency Electroencephalograms Ram Narayan, Puneet Gupta, Barbara Voth, Lakshmi Beeravolu, Ryan Hays, Pradeep Modur, Paul Van Ness, Mark Agostini P5.053 Usefulness of Emergent Electro-Encephalogram In Known Epileptic Patients Louise Tyvaert, Marie Girot, Xavier Lenne, Pierre Williate, William Szurhaj, Stephanie Leblanc, Maxime Chochoi, Herve Hubert, Philippe Derambure P5.054 Use of Prolonged VEEG Monitoring in Children with First Unprovoked Seizure Misbah Salam, Anjum Hashim, Jasmine Singh P5.055 Frequent Additional Epileptogenic Abnormalities Detected with Inpatient Long-Term EEG Monitoring Ehtesham Khalid, Shobhit Sinha, Khurram Siddiqui A Presentation of Progressive Multifocal Leukoenceophalopathy Leading to Diagnosis of Underlying Marginal Zone Lymphoma: An Unusual Antecedent Cause of Immunosuppression. Alexander Hartmann, Sara Mayer Epilepsy and Clinical Neurophysiology (EEG): Quality Improvement, Health Care Utilization, and History of Epilepsy P5.030 Multiple Autoimmune Antibody Limbic Encephalitis: A Case in a Pregnant Woman Meha Goyal, Kasey Gildersleeve, Stuart Tomko, Joseph Kass P5.042 Variation in Quality of Epilepsy Care and Association with Seizure Control. Lidia Moura, Jonathan de Jesus, Rogger Andrade, Daniel Hoch Should Idiopathic Generalized Epilepsy be Labeled “generalized” or “System” Epilepsy Syndromes? Istabrak Abdelkefi, Yousser Hizem, Imen Kacem, Mouna Ben Djebara, Amina Gargouri, Olivier Dulac, Riadh Gouider P5.031Hemophagocytic P5.043 P5.057 Lymphohystiocytosis Associated with Encephalitis: Two Case Reports Sheetal Sheth, Carl Gold, Emma Meyers, Amy Jongeling, Stephan Mayer, Sachin Agarwal, Jan Claassen, Brandon Foreman P5.032 Extending the Olive Branch: A Cost-Benefit Analysis of Thymectomy in Myasthenia Gravis Shrikant Mishra, Nasheed Jamal, Poonum Chaturvedi, Bhavesh Trikamji P5.033 Determination of Antibodies to GAD67 and Other Antigens in Patients with GAD65 Antibody-associated Syndromes Núria Gresa-Arribas, Helena Ariño, Lidia Sabater, Eva Caballero, Mercè Alba, Eugenia Martínez-Hernandez, Mar Petit, Albert Saiz, Josep Dalmau, Francesc Graus P5.034 Basal Ganglia Encephalitis and Autoimmune Retinitis Associated with Influenza B Barbara Graves, Jonathan Hosey Implementation of an Easyto-use Database for the Assessment of Physician Performance in Epilepsy Care Rodolfo Callejas, Yamil Matuk-Perez, Daniel Vargas-Mendez, Nephtali CruzReyes, Nelson Garcia, Ildefonso RodriguezLeyva P5.044 Complications in the Epilepsy Monitoring Unit: A Nationwide Study Monica Dhakar, Maysaa Basha P5.045 How Long Is Long Enough? The Utility of Prolonged Inpatient Video EEG Monitoring Brian Moseley, Sandra Dewar, Zulfi Haneef, John Stern P5.046 Epidemiological Pilot Analysis of Epilepsy Patients in a Community Clinic Aims to Inform Effective Care Laura Karas, Corey Goldsmith, Sara Ruppelt, Alica Goldman P5.047 Epilepsy Surgery: Historical Perspective Pawan Rawal P5.056 “Re-build Up” Phenomenon Revisited Hesham Allam, Daniel Weber, Stanley Iyadurai P5.058 Infraslow Delta Co-exists with High Frequency Oscillation in Cases of Ictal Internal Vibration Aura Hisanori Hasegawa P5.059 Quantitative EEG (qEEG) as Marker for Mild Cognitive Impairment (MCI) in Patients with Parkinson’s Disease (PD) Habib Bousleiman, Shaheen Ahmed, Martin Hardmeier, Florian Hatz, Christian Schindler, Volker Roth, Ronan Zimmermann, Ute Gschwandtner, Peter Fuhr P5.060 Triphasic Waves and Epileptiform Correlates on Electroencephalogram Alyssa Fiddler, Osman Farooq, Barbara Teter, Katelyn Kavak, Arie Weinstock P5.061 When Should We Treat Periodic Lateralized Epileptiform Discharges (PLEDS) Ahmad Solaiman, Anza Memon, Maysaa Basha, Lusine Avedian Hospitalization Rates and Early Versus Late Addition of Adjunctive Anti-epileptic Drugs: A Retrospective Study in a Commercially-Insured U.S. Population Fulton Velez, Thirupathi Pattipaka, Maria Malmenäs P5.063 Knowledge About Sudden Unexpected Death in Epilepsy Among Health Personnel, Epilepsy Patients and Their Relatives. A Pilot Survey in Honduras. Reyna Duron, Juan Argenal, Sylvia Gonzalez-Canelo, Dario ZunigaMartinez, Lupe Martinez, Susan PietschEscueta P5.064 A Unique Partnership for Research in Epilepsy Outcomes: The Emory University and UCB Pharma Collaboration Sandra Helmers, Fred Cox, David Thurman, R Faught, Archna Patel, Tracy Durgin, Patty Fritz, Kelly Simontacchi, Akshatha Kalsanka Pai P5.065 Risk of Bone Fractures Among Epilepsy Patients in the United States: An Analysis of a Large Administrative Claims Database Fulton Velez, Joseph Menzin, Michael Munsell, Molly Frean P5.066 Known Epileptic Patients Use of Emergency Departments Marie Girot, Philippe Derambure, Maxime Chochoi, Stephanie Leblanc, Patrick Goldstein, William Szurhaj, Pierre Williate, Xavier Lenne, Eric Wiel, Herve Hubert, Florence Richard, Louise Tyvaert P5.067 Known Epileptic Patients Use of Resources of Emergency Departments Marie Girot, Xavier Lenne, Stephanie Leblanc, William Szurhaj, Maxime Chochoi, Patrick Goldstein, Pierre Williate, Eric Wiel, Herve Hubert, Philippe Derambure, Louise Tyvaert P5.068 Severe Overutilization of the Emergency Department in Patients with Uncontrolled Epilepsy Neha Vijayvargiya, Steven Tobochnik, Kenneth Walsh, Camilo Gutierrez, Wayne Satz, Mercedes Jacobson P5.069 Comparison of Health Care Resource Utilization and Costs in Treatment-Adherent Patients with Epilepsy With and Without Breakthrough Seizures in A U.S. Managed Care Population Charles Makin, Allison Petrilla, Victoria Divino, Vamsi Bollu, Fulton Velez, Shawn Hallinan, Alan Ettinger P5.070 Resource Utilization in Patients with Suspected Psychogenic Non-epileptic Seizures and Drug Resistant Epilepsy in the Harris County Health District Between 2009 and 2012 Brian Wolf, Bonnie Hayashi, Ezekiel Sachs, Colin Van Hook, Dona Murphey, Corey Goldsmith P5.071 The Economic Burden of Uncontrolled Epilepsy: A Retrospective Study in a Commercially-Insured U.S. Population Maria Malmenas, Thirupathi Pattipaka, Vamsi Bollu, Fulton Velez Fast, Easy Registration Online · AAN.com/view/AM14 95 Wednesday April 30 General Neurology IV Wednesday, April 30 P5.072 Real-World Persistence and Treatment Failure Associated with First Line Use of Antiepileptic Drug Treatment in a Large U.S. Managed Care Population Victoria Divino, Allison Petrilla, Shawn Hallinan, Vamsi Bollu, Fulton Velez, Alan Ettinger, Charles Makin ALS: Epidemiology and Registries P5.073 Increased Prevalence of ALS in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans Sasha Zivkovic, Anne Van Cott, Huned Patwa, Mary Jo Pugh P5.074 Verification of Amyotrophic Lateral Sclerosis (ALS) Cases Reported to the State and Metropolitan Area ALS Surveillance Projects Wendy Kaye, Laurie Wagner, Vinicius Antao, Eric Sorenson P5.075 State and Metropolitan Areabased Amyotrophic Lateral Sclerosis (ALS) Surveillance Laurie Wagner, Wendy Kaye, Heather Jordan, Lindsay Rechtman, Maggie Ritsick, Marchelle Sanchez P5.076 The Northeast ALS Consortium (NEALS) Upper Motor Neuron Disease (UMND) Registry Alyssa Murphy, Lorena Loci, Hiroshi Mitsumoto, Catherine Lomen-Hoerth, Yasushi Kisanuki, Jinsy Andrews, Merit Cudkowicz, Nazem Atassi P5.077 Using the National Amyotrophic Lateral Sclerosis Registry as a Subject Recruitment Tool for Research D. Kevin Horton, Vinicius Antao, Paul Mehta P5.078 National ALS Biorepository Feasibility Study Wendy Kaye, Laurie Wagner P5.079 Enhancements to the U.S. National Amyotrophic Lateral Sclerosis (ALS) Registry Paul Mehta, Vinicius Antao, D. Kevin Horton P5.080 Findings from the New Jersey State-wide Amyotrophic Lateral Sclerosis (ALS) Surveillance Project Heather Jordan, Jerald Fagliano, Daniel Lefkowitz, Lindsay Rechtman, Wendy Kaye P5.081 Cognitive Reserve in ALS with Comorbid Frontotemporal Dementia (FTD): A Population-Based Study Antonio Canosa, Anna Montuschi, Barbara Iazzolino, Andrea Calvo, Cristina Moglia, Davide Bertuzzo, Leonardo Lopiano, Gabriella Restagno, Maura Brunetti, Irene Ossola, Anna Lo Presti, Stefania Cammarosano, Adriano Chio P5.084 Physical Activity Profile and Barriers to Physical Activity in Individuals with Myotonic Dystrophy Katy Eichinger, Jeanne Dekdebrun, Nuran Dilek, Shree Pandya, Ding-Geng Chen P5.095 P5.085 P5.096 Brain Gray Matter and White Matter Alterations in Patients with Myotonic Dystrophy 1 Stojan Peric, Federica Agosta, Francesca Caso, Vidosava Rakocevic-Stojanovic, Giancarlo Comi, Vladimir Kostic, Massimo Filippi P5.086 Congenital Centronuclear Myopathy Mimicking Congenital Myotonic Dystrophy Watcharasarn Rattananan, Jill Blandford, Gwendolyn Claussen, Shin Oh, Mohammad Alsharabati P5.087 Electrical Impedance Myography Discriminates Congenital Muscular Dystrophy from Controls Daniel Schwartz, Anam Salman, Janannaz Dastgir, Barbara Lear, Carsten Bonnemann, Tanya Lehky Hereditary Inclusion Body Myositis (IBM2) with a GNE c.2228 T>C Mutation in 3 Saudi Arabian Families. Ahmed Basndwah, Enass AlMowalad, Yousef Al-Said, Edward Cupler P5.098 Immunotherapy for Respiratory Complications of Sporadic Late Onset Nemaline Myopathy (SLONM) with Monoclonal Gammopathy Nancy Rosales, Mihael Varosanec, Ramon Lugo, Richard Prayson, Megan Rahmlow P5.099Human α7 Integrin Gene P5.108 Can Ultrasonography of Median Nerve Differentiate Between Mild, Moderate and Severe Carpal Tunnel Syndrome? Vasudeva Iyer P5.109 The Specificity of Prolonged CMAP Durations and Severe CMAP Reductions in Critical Illness Neuromyopathy Christopher Kramer, Andrea Boon, C. Harper, Brent Goodman P5.110 Longitudinal Quantitative EMG Findings During Reinnervation After Complete Nerve Lesions Christian Krarup, Michel Boeckstyns, Allan Ibsen, Simon Archibald Cerebrovascular Disease and Interventional Neurology: Epidemiology P5.100 Desmin C-terminus Tail Mutation Is a New Cause of Autosomal Dominant Limb-girdle Muscular dystrophy Joshua Lovinger, Anna Szekely, Huned Patwa, Zarife Sahenk Stroke and Non Convulsive Status Epilepticus. A Topographic and Prognosis Description. Francisco Muñoz Giacomelli, Analia Calle, Maria Gonzalez Toledo, Fatima Pagani Cassara, Agustina Tamargo, Alejandro Thomson, Diego Nadile, Francisco Klein P5.090 Neurophysiology/EMG P5.113 Evaluation in 476 Turkish Dystrophinopathy Patients Hacer Durmus, Nihan ErginelUnaltuna, Poda Mehves, Arman Çakar, Ayca Altinkaya, Filiz Guclu-Geyik, Feza Deymeer, Yesim Parman, Asli Tolun, Piraye Serdaroglu Sociodemographic and Health Related Profile of Adults with Duchenne/ Becker Muscular Dystrophy (DBMD): Data from the Muscular Dystrophy Surveillance, Tracking and Research Network (MD STARnet) Shree Pandya, Anil Kumar, Kathy James, Christine Westfield, Emma Ciafaloni, Christopher Cunniff, Paul Romitti, Richard Moxley P5.091 Baseline Performance on 6MWT Correlates with Other Functional Outcomes in a Phase IIb Study of ExonSkipping Antisense Oligonucleotide Eteplirsen for Use in Duchenne Muscular Dystrophy (DMD) Jihad Saoud, Jerry Mendell, Louise Rodino-Klapac, Zarife Sahenk, Kandice Roush, Loren Bird, Linda Lowes, Lindsay Alfano, Ana Maria Gomez Ramirez, Sarah Lewis, Vinod Malik, Kim Shontz, Christopher Shilling, Peter Sazani, Edward Kaye P5.092 P5.093 96 P5.097 Ulnar Palm to Finger Sensory Nerve Conduction Eduardo Davidovich, Osvaldo Nascimento, Bruno Coutinho, Victor Kosac P5.089Genotype-Phenotype Muscular Dystrophies Correlation Between Muscle Histopathology Impairment and Spliceopathy in Myotonic Dystrophies Giovanni Meola, Enrico Bugiardini, Giuliana Rossi, Laura Valentina Renna, Annalisa Botta, Rosanna Cardani Analysis of Myostain and Related Proteins in a Cardiotoxin Injury Muscle Atrophy Model Kenya Murata, Hidefumi Ito P5.107 (ITGΑ7) Delivered by Adeno-Associated Virus Reverses the Phenotype of the Double Knock Out (DKO) Mouse Devoid of Dystrophin and Utrophin Kristin Heller, Chrystal Montgomery, Kim Shontz, Paul Janssen, Reed Clark, Jerry Mendell, Louise Rodino-Klapac Telemedicine in the Home for Veterans with Amyotrophic Lateral Sclerosis Richard Bedlack P5.083 A Novel Form of Nemaline Myopathy Caused by an In-Frame Deletion in TNNT1 Sarada Sakamuri, Carly Siskind, Karolina Watson, Thomas Winder, Hannes Vogel, John Day To Report Clinical Heterogeneity of Facio-scapulo-humeral Muscular Dystrophy in Which Two Patients Presented with Recurrent Facial Palsy Uzma Usman, Bilal Hameed, Johnny Salameh P5.088 Elucidating the Mechanism of Anoctamin 5 Deficiency with a Novel KO Mouse Model Danielle Griffin, Eric Pozsgai, William Grose, Kristin Heller, Jerry Mendell, Zarife Sahenk, Louise Rodino-Klapac P5.082 3:00 p.m.–6:30 p.m. C. Elegans as a model System to Study Nemaline Myopathy Ge Xiong, Ken Choe, David Leung, Hiroshi Qadota, Guy Benian, Desmond Zeng, Karen McFarland, Tetsuo Ashizawa P5.094 A Novel Heterozygous L1453P Mutation in the MYH7 Gene Resulting in Laing Distal Myopathy in an Irish Family Stela Lefter, Orla Hardiman, Russell McLaughlin, Sinead Murphy, Michael Farrell, Aisling Ryan P5.101Intraoperative Neurophysiologic Monitoring with Hoffman Reflex During Thoracic Spine Surgery: A Lesson from a Series of 18 Patients Anteneh Feyissa, Robert Smith, Sudhakar Tummala P5.102 Motor Evoked Potentials From Multiple Recording Sites of the Lower Limbs as a Monitoring Tool of Central Motor Function Walter Troni, Antonio Bertolotto, Federica Melillo, Simona Malucchi, Paola Berchialla, Francesca Sperli, Alessia Di Sapio P5.103 Electrophysiological Findings in Acute Solanum Torvum Toxicity Robert Glover, Daniel Patterson, Nichloas Connors, Silas Smith, Mark Milstein, Michael Swerdlow P5.104 The Pain of Anticipation: Differences Between Expected and Experienced Pain in Electrodiagnostic Testing John Barghols, Samiullah Kundi, David Thompson, Eduardo De Sousa, Calin Prodan P5.105 Levodopa Responsiveness of Blink Reflex Recovery Index: An Objective Method of Differenting Parkinson Disease from Parkinson Plus Syndromes Chandana Gaddipati, Meenakshisundaram Umaiorubahan P5.106 Frequency of Radiculopathy in Patients with Carpal Tunnel Syndrome and Paracervical Pain Rocio Garcia Santibanez, Nabil Altememi, Stephen Scelsa 2O14 Scientific Abstract Listing and Annual Meeting Information P5.111 Cocaine and Ischemic Stroke: Epidemiological and Clinical Characteristics Anand Vaishnav, Kerri Remmel, Kari Moore, Craig Ziegler P5.112 Incidence and Mortality of Ischemic Stroke Subtypes in Joinville, Brazil: A Population-Based Study Marcos Lange, Norberto Cabral, Carla Moro, Alexandre Longo, Anderson Goncalves, Viviane Zetola, Tatjana Rundek P5.114 Incident Cancer in Stroke Survivors: Analysis of the Vitamin Intervention for Stroke Prevention (VISP) Trial Muhammad Suri, Malik Adil, Gustavo Rodriguez, Saqib Chaudhry, Adnan Qureshi P5.115 Time Trends in Transient Ischemic Attack Admission from the Emergency Department Karen Albright, John Donnelly, Michael Mullen, Brett Cucchiara, Justin Blackburn, Alexander Lo P5.116 Temporal Trends in Hospitalization for Transient Ischemic Attack in the United States, 20002010 May Kim-Tenser, Lucas Ramirez, Natalie Valle, Steven Cen, William Mack, Nerses Sanossian, Amy Towfighi P5.117 Education Status and Ischemic Stroke in Young: A Potential Target Towards Future Population Based Preventive Strategies. Anand Vaishnav, Radhika Vaishnav P5.118 Which Metabolic Syndrome Criteria Is More Relevant for the Prediction of Silent Brain Infarction? A Study in a Korean Population Yong Bum Kim, PilWook Chung P5.119 Neurology House Staff Experience Doesn’t Affect Acute Stroke Treatment Gonzalez Castellon Marco, Joshua Stillman, Mitchell Elkind, Randolph Marshall, Joshua Willey Poster Session V P5.120 “On-the-job” Fatal Cardiovascular Events: Analysis of National Institute for Occupational Safety and Health Data Amna Zarar, Aveen Saed, Nudrat Tasneem, Malik Adil, Adnan Qureshi Cerebrovascular Disease and Interventional Neurology: Intracranial Aneurysms and Subarachnoid Hemorrhage P5.121Thromboelastography Determines a Transient Late Hypercoagulable State After Aneurysmal Subarachnoid Hemorrhage Preethi Ramchand, S Frangos, F Quattrone, S Doerfler, K Nawalinski, B Michel, C Ju, S Nyirjesy, N Driscoll, E Maloney-Wilensky, D Sandsmark, Michael Mullen, M Smith, B Pukenas, E Zager, S Stein, Scott Kasner, Joshua Levine, Monisha Kumar P5.122 Inflammation, Nutritional Status and Outcome after Aneurysmal Subarachnoid Hemorrhage Neeraj Badjatia, Aimee Monahan, Amanda Carpenter, Laura Friedman, Jacqueline Zimmerman, J. Michael Schmidt, Jan Claassen, Kiwon Lee, E. Sander Connolly, Stephan Mayer, Wahida Karmally, David Seres P5.123 THE VASOGRADE—A Simple, Reliable Grading Scale for Aneurysmal Subarachnoid Hemorrhage Airton Leonardo de Oliveira Manoel, David Turkel-Parrella, Ekaterina Kouzmina, Simon Abrahamson, Thomas Marotta, Tom Schweizer, Julian Spears, Loch MacDonald P5.124 Clinical Outcomes After High-Grade Aneurysmal Subarachnoid Hemorrhage Airton Leonardo de Oliveira Manoel, David Turkel-Parrella, Alberto Goffi, Victoria McCredie, David Ben-Israel, Ekaterina Kouzmina, Julian Spears, Thomas Marotta, Simon Abrahamson P5.125 Headaches Following Endovascular Treatment of Cerebral Aneurysms: Coil Embolization Versus Flow Diversion Martin Ollenschleger, Michael Mancini, Stephen Ohki, Gary Spiegel P5.126 Rebleeding of a Cerebral Aneurysm During Transcranial Doppler: Hemodynamic Changes and Response to Treatment Eric Marrotte, Tamer Abdelhak, Leonard Melvin, Panayiotis Varelas P5.127 Extensive Proximal Migration of Posterior Communicating Artery Aneurysm Coil Presenting with a Transient Ischemic Attack Ahmed Itrat, Esteban Cheng-Ching, Muhammad Hussain P5.128 Utilization and Outcomes of Ventriculostomy in Non-traumatic Subarachnoid Hemorrhage During Last Decade in United States Yogesh Moradiya, Santosh Murthy, Shreyansh Shah, Sneha Modi P5.129 New Risk Score Improves Vasospasm Prediction following Subarachnoid Hemorrhage Using Markers of Vascular Compliance Aashish Anand, Haitham Hussein, Mustapha Ezzeddine, Joseph Kass, Jose Suarez P5.130 Long Term Survival and Hospital Re-admission Rates in Elderly Patients with Subarachnoid Hemorrhage Treated with Surgical or Endovascular Treatment Saqib Chaudry, Mohammad Afzal, Alexanderos L. Georgiadis, Adnan Qureshi P5.142 Validation of ICH and ICH-GS Scores in an Indian Cohort of Patients with Intracerebral Hemorrhage Treated Medically and with Surgical Interventions Rohit Bhatia, V Sreenivas, Shaily Singh, M. v Padma, Kameshwar Prasad P5.143 Spontaneous Spine Epidural Hematoma Is Most Frequently Idiopathic in Cause Michael Pizzi, Scott Silliman Predictors of the CT Angiography Spot Sign in Deep and Lobar Intracerebral Hemorrhage Farid Radmanesh, Guido Falcone, Christopher Anderson, Thomas Battey, Alison Ayres, Anastasia Vashkevich, Kristin Schwab, Javier Romero, Anand Viswanathan, Steven Greenberg, Joshua Goldstein, Jonathan Rosand, H. Bart Brouwers P5.132 P5.144 Cerebrovascular Disease and Interventional Neurology: Intracerebral Hemorrhage and Other Hemorrhages P5.131 Spinal Epidural Hematoma in a Patient with Repair of Aortic Coarctation Imad Khan, Neha Mirchandani, Laura Donarummo P5.133 Cervico-Dorsal Intramedullary Hematoma in a Patient with Pompe Disease Diego Nadile, Maria Gonzalez Toledo, Agustina Tamargo, Fatima Pagani Cassara, Alejandro Thomson, Francisco Muñoz, Francisco Klein Development of PeriHematomal Edema Measurements in Intracerebral Hemorrhage Sebastian Urday, Lauren Beslow, David Asuzu, Anastasia Vashkevich, Alison Ayres, Thomas Battey, Magdy Selim, Jonathan Rosand, William Kimberly, Kevin Sheth P5.145 P5.134 Intracerebral Hemorrhage Associated with Dietary Supplement Containing DMAA Janet Elgallab, Robert Glover, Deepa Bhupali, David Gordon, Kathryn Kirchoff-Torres The Impact on Radiology Utilization of Disseminating an Analysis on the Value of Neuroimaging Studies in Intracerebral Hemorrhage: The University Hospitals Case Medical Center Comprehensive Stroke Center Experience Tanzila Shams, LeighAnne McCartney, Polly Westerberg, Cathy Sila P5.135 P5.146 Lone Intraventricular Hemorrhage and Intraventricular Hemorrhage Associated with Small Parenchymal Component: Two Different Clinical Entities Ather Taqui, Lauren Koffman, Muhammad Hussain, Ken Uchino Etiologies of Intracerebral Hemorrhages from 2009-2012 at Mayo Clinic-Rochester James Klaas, Sherri Braksick, Robert Brown, Alejandro Rabinstein, Jennifer Fugate P5.153 Clinical Profile of Longitudinally Extensive Transverse Myelitis in Indian Population: A Prospective Study from a Tertiary Teaching Hospital of South India Dhairyawan Pokalkar, Veena Narisetty, Murali Chekuri, Sowjanya Poosarla, Srilatha Sripuram, Sateesh Kumar Kamera P5.154 Common Comorbidities Among Multiple Sclerosis Patients in the United States: An Analysis of In-patient Hospitalizations Anthony Asemota, Han Wang, Shalini Selvarajah, Xuan Hui, Eric Schneider, Arun Venkatesan P5.155 Demographics and Clinical Characteristics of Multiple Sclerosis in Kuwait: An Analysis of the National MS Registry Raed Alroughani, S Ahmed, Jassem Al Hashel P5.156 Familial Multiple Sclerosis Recurrence Risk in Argentina Francisco Varela, Mauricio Farez, María Balbuena Aguirre, Vanesa Nagel, Alejandro Köhler, Jorge Correale P5.157 Excess Mortality in Multiple Sclerosis: A Meta-Analysis of Incidence and Standardized Mortality Rates Radu Tanasescu, Cris Constantinescu, Christopher Tench, Ali Manouchehrinia P5.158 Sociocultural and Demographic Risk Factors for the Development of Multiple Sclerosis in Kuwait Suhail Al-Shammri, Arpita Chattopadhyay, Magdy Girgis, Reema Mathew, Chetana Madala, Abayomi Akanji P5.147 Fever and Transient Neurologic Worsening in Intracerebral Hemorrhage Matthew Maas, Michael Berman, James Guth, Eric Liotta, Shyam Prabhakaran, Andrew Naidech P5.159 Role of Magnetic Resonance Imaging in Non-Lobar Hypertensive Intracerebral Hemorrhage Amir Adeli, Reza Behrouz P5.137 P5.148 CNS Diseases and Differential Diagnosis P5.136 Type of Substance Use Predicts Hemorrhage Versus Ischemia Emma Kaplan, Rebecca Gottesman, Rafael Llinas, Elisabeth Marsh P5.138 Intracerebral Hemorrhage Associated with Oral Phenylephrine Use Brian Tark, Steven Messe, Clotilde Balucani, Steven Levine P5.139 Reversible Cerebral Vasoconstriction Syndrome Presenting as Coital Headache and Intracerebral Hemorrhage Alex Linn, Nancy Rosales, Camilo Garcia-Gracia, Efrain Salgado P5.140 Direct Thrombin Inhibitors May Have a Decreased Risk of Intracerebral Hemorrhage Compared with Older Anticoagulants Sindhu Ravipati, Daniel Woo, Padmini Sekar, Charles Moomaw, Matthew Flaherty, Jennifer Osborne Cerebrovascular Disease and Interventional Neurology: Intracerebral Hemorrhage P5.141 Assessing the Safety and Cost-Effectiveness of Admission of Patients with Intracerebral Hemorrhage (ICH) to a Neurovascular Step Down Unit. Shaheryar Hafeez, Reza Behrouz Intracerebral Hemorrhage Transfer Rates from U.S. Emergency Departments: Findings from the National Hospital Ambulatory Medical Care Survey John Donnelly, Michael Mullen, Karen Albright, Justin Blackburn, Brett Cucchiara, Alexander Lo P5.149 Primary Intraventricular Hemorrhage: A Review with Focus on Diagnostic Testing and Etiologies Ather Taqui, Lauren Koffman, Muhammad Hussain, Ken Uchino P5.150 Yield of Follow-Up Imaging in Workup of Intracerebral Hemorrhage—a Retrospective Chart Review Clifford Meyers, Adam Kelly MS and CNS Inflammatory Disease: Epidemiology P5.151 Clinical and Demographic Profile of Multiple Sclerosis Patients in India: Registry database of MS patients from All India Institute of Medical Sciences(AIIMS), New Delhi Ankit Singhal, Rohit Bhatia P5.152 Unveiling Multiple Sclerosis in Nigeria: The Conundrum of Diagnosis and Access to Disease Modifying Therapies Njideka Okubadejo, Oluwadamilola Ojo, Temitope Lawal, Francis Ojini, Mustapha Danesi The Diagnosis of Multiple Sclerosis in Hispanics Occurs Sooner in the Young Than in Adults Megan Langille, Lilyana Amezcua, Margaret Burnett, Jose Aparicio, Wendy Mitchell P5.160 Clinical and Immunological Features of Hashimoto’s Encephalopathy Presenting with Limbic Symptoms Akiko Matsunaga, Toru Kishitani, Tomoko Muramatsu, Tomomi Kame, Masamichi Ikawa, Osamu Yamamura, Tadanori Hamano, Yasunari Nakamoto, Makoto Yoneda P5.161 Susac’s Syndrome in a 25-year-old Pregnant Woman Yasemin Tashman P5.162 Postcontrast T2-FLAIR: a Useful Tool for Diagnosing and Monitoring Susac Syndrome Irene Cortese, Govind Nair, Joan Ohayon, Luisa Vuolo, Martina Absinta, Pascal Sati, Bibiana Bielekova, Daniel Reich P5.163 MRI in Susac’s Syndrome: A Propos of the Barkhof-Tintore Criteria Sreekanth Koneru, Neil Jouvenat, Kathleen Healey, Rana Zabad P5.164 Long Segment Spinal Cord Involvement as the Initial Clinical Manifestation of Sarcoidosis Jamie Adams, Steven Galetta Fast, Easy Registration Online · AAN.com/view/AM14 97 Wednesday April 30 First Authors stand by Posters from 5:00 p.m.–6:30 p.m. Wednesday, April 30 P5.165 IgG4-Related Disease Manifesting as Middle Cranial Fossa Mass: A Case Report Prerna Malla, Joseph Zachariah, Bashar Katirji P5.166 Catatonia: a Duel of Hashimoto’s Encephalopathy and Anti NMDA Receptor Encephalitis Elena Grebenciucova P5.167 Clinical Manifestations, Imaging Findings, and Immunomodulatory Therapeutic Strategies for Three Patients with Concurrent Stiff Person Syndrome and Cerebellar Ataxia Due to Anti-GAD Antibodies: A Case Series Lauren DeNiro, Jerome Graber, Howard Geyer, Alexis Boro P5.168 Association of Parenchymal and Vascular Damage (Mixed Pattern) in Neurobehçet: A Case Series Study Youness Habtany, Fatima Dany, Nada Benkirane, Bouchra El Moutawakil, Mohamed Abdoh Rafai, Ilham Slassi P5.169 A Rare Autoimmune Encephalitis—Due to DipeptidylPeptidase-like Protein-6 (DPPX) Autoantibody; A Case Report Shawna Suchecki, Laura Risley, Earl Zimmerman, Eric Molho, Era Hanspal, Josep Dalmau P5.170 Cytokine Disarrangement and Increased Soluble Amyloid A (SAA) in Cerebrospinal Fluid (CSF) of Patients with Neurosarcoidosis (NS) Maria ReyesMantilla, Anupama Kumar, Jorjetta Ilieva, Carlos Pardo-Villamizar P5.171 Common Variable Immunodeficiency Mimicking Neurosarcoidosis Konark Malhotra, Santosh Ramanathan, Deeksha Agrawal, Sandeep Rana, Thomas Scott P5.172 Primary Central Nervous System Lymphoma Mimicking Multiple Sclerosis with Spontaneously Remitting Lesions Erin Longbrake, Robert Schmidt, Anne Cross, Enrique Alvarez P5.173Leukoencephalopathy Associated with Levamisole Toxicity from Cocaine Use Nicky Sheldon, Bridget Bagert P5.174 Hematopoietic Stem Cell Transplantation for Adult Cerebral X-linked Adrenoleukodystrophy Wolfgang Köhler, Jörn-Sven Kühl P5.175 Monoclonal B Cell Population in a Patient with Neurosarcoidosis Justine Brink P5.176 TWEAK Stimulation of Microglia and Implications for Neuropsychiatric Lupus Ariel Stock, Chaim Putterman P5.177 Distinguishing ClinicoRadiological Features in Patients with Central Nervous System Tumefactive White Matter Lesions Xuling Lin, Kevin Tan, Lishya Liauw, Aung Soe Tin, Weiling, Eileen Soon, Zhu Yin Shih, Raphael, Boon Ping Toe, Hwee Yee Lee, Wai-Yung Yu P5.178 Memory Disturbance in the Mice Treated with Intraventricular Administration of CSF from NMDAREncephalitis Patients Keiko Tanaka, Yongzhi Li, Nobuo Kato, Tsutomu Takegami 98 P5.179 Anti-NMDA Receptor Antibodies in Neurologic Disease Jessica Panzer, Bailey Baumann, Hiro Furukawa, Noriko Simorowski, Amy Gleichman, David Lynch P5.180 Acute Transverse Myelitis: CSF Determinants in the Differential Diagnostics Laura Kupila, Nina Jaakonmäki, Heini Huhtala, Laura Airas P5.181 A Note of Caution About the Diagnosis and Treatment of Suspected Transverse Myelitis (TM) Jorge Jimenez Arango, Maureen Mealy, Phillipe Gailloud, Carlos Pardo-Villamizar P5.182 Contribution of Fluorodeoxyglucose Positron Emission Tomography (FDG-PET) in Myelitis: A Multicentre Cohort of 13 Cases Jessica Orgeval, Denis Mariano Goulart, Laurent Collombier, Giovanni Castelnovo, Mahmoud Charif, Clarysse Carra, Xavier Ayrignac, Nicolas Gaillard, Mohamed Chbicheb, Dimitri Renard, Guillaume Taieb, Eric Thouvenot, Astrid Corlobe, Nicolas Champfleur, Pierre Labauge P5.183 3:00 p.m.–6:30 p.m. P5.191 Urinary Retention as the Presenting Symptom of West Nile Encephalitis: Report of Two Cases. Rashedul Hasan, John DeToledo P5.204 P5.192 Multiple Mothballs or Multiple Sclerosis: A Diagnostic Dilemma Divyanshu Dubey, Vibhash Sharma, Olaf Stuve P5.205 P5.193 P5.206 Magnetic Resonance Imaging Changes After Plasma Exchange Treatment in Steroid-Refractory Relapses in Multiple Sclerosis and Other CNS Idiopathic Inflammatory Demyelinating Diseases. Jose Meca-Lallana, Rocio Hernandez Clares, Ester Carreon Guarnizo, Adelaida Leon Hernandez, Begoña Palazon Cabanes, Gema Salgado Cecilia, Encarna Andreu Reinon, Judith Jimenez Veiga, Margarita Cacho Perez, Guadalupe Ruiz Merino, Jose Javier Martin Fernandez P5.194 Multiple Sclerosis Diagnosis: A Survey of Neurology Residents’ Knowledge on Current Diagnostic Criteria Salim Chahin, Nikitha Ashok, Raymond Price, Clyde Markowitz Cognitive Deficits, Cerebrospinal Fluid Pleocytosis and White Matter Lesions Following Parvovirus B19 Infection in an Immunocompetent Adult Ariel Antezana, Joseph Herbert, Ilya Kister P5.195 P5.184 P5.196 The Specificity of CSF B Cell Reactivity in HTLV-1 Associated Myelopathy Jerry Lin, Alexandra Berman, Christopher Sears, Saud Sadiq P5.185 Acute Disseminated Encephalomyelitis Following an Acute JC Virus Infection Sean Rogers, Ramsey Falconer, Yasar Torres-Yaghi, Heather Boynton, Chris Sonne, Carlos Mora, Carmelo Tornatore P5.186Paraneoplastic Myelopathy with Positive Antigolgi Autoantibody YuanKai Lee, Sonia Kumari, Gordon Mazibrada P5.187 N-methyl D-aspartate Receptors (NMDAR) Antibodies Associated with Distinct Clinico-Radiological White Matter Syndromes: Clinical Evidence for an Anti-NMDAR Leukoencephalopathy? Yael Hacohen, Michael Absoud, Cheryl Hemingway, Leslie Jacobson, Jean-Pierre Lin, Mike Pike, Sunil Pullaperuma, Ata Siddiqui, Evangeline Wassmer, Camila Buckley, Sarosh Irani, Angela Vincent, Ming Lim P5.188 New Autoantibodies Against Neutral Glycolipids in Encephalomyeloradiculoneuropathy Tatsuro Mutoh, Sayuri Shima, Tomomasa Ishikawa, Akihiro Ueda, Kunihiko Asakura P5.189 The Oxford Experience: Clinical Features and Outcomes of 25 NMDAR-Ab Positive Patients Including Those with Atypical Presentations Katrina Morris, Camilla Buckley, Belinda Lennox, Yael Hacohen, Ester Coutinho, Angela Vincent P5.190 Clinical Features, Diagnostic Findings and Treatment of Susac Syndrome: A Case Series Ivana Vodopivec, Sashank Prasad, Nagagopal Venna Bradycardia Leading to Pacemaker Placement: A Characteristic Prodromal Syndrome of VGKCC/LGI1 Antibody Associated Encephalitis Georges Naasan, Sarosh Irani, Brianne Bettcher, Michael Geschwind, Jeffrey Gelfand MR Imaging Trailing Clinical Expression of Natalizumab-Associated PML in Multiple Sclerosis: A Rare But Serious Diagnostic and Management Problem Christopher Muth, Christian Hernandez, Dusan Stefoski, Roumen Balabanov, Michael Ko P5.197 Predominantly Spinal Phenotype of Relapsing-Remitting Multiple Sclerosis Jacob Cogan, Nataliya Ternopolska, Wendy Vargas, Susan Gauthier, Nancy Nealon, Timothy Vartanian, Jai Perumal Headache: Epidemiology P5.198 Headache in Service Members Deployed to Afghanistan Richard Young, Michael Myslenski, Peter Petrillo P5.199 Distinctive Anatomical and Physiological Features of Migraine Aura Revealed by 18 Years of Recording. Jakob Hansen, Serapio Baca, Andrew Charles P5.200 Chiari Headache Mechanisms: The Role of Neck Spasm and Migraine Fredric Cantor, Jessica Mack, John Heiss P5.201WITHDRAWN P5.202 Developing and Validating the ID-Chronic Migraine (ID-CM) Screening Tool Richard Lipton, Daniel Serrano, Andrew Blumenfeld, David Dodick, Sheena Aurora, Werner Becker, H. Diener, ShuuJiun Wang, Maurice Vincent, Dawn Buse, Joanna Sanderson, Sepideh Varon, Michael Reed P5.203 No Laughing Matter: A Case of Gelastic Migraine Paul Mathew, Carrie Robertson 2O14 Scientific Abstract Listing and Annual Meeting Information A Closer Look at the Patients Who Present to the Emergency Department with Headache Mia Minen, Benjamin Friedman The Case of Migraine with Visual and Olfactory Hallucination Related to Food Allergy Vladimir Klinov, Larisa Syrow Multifocal Multiform Nummular Headache (NH): A Case Report Stephanie Goldberg, Sarah Vollbracht, Brian Grosberg P5.207 Peripartum Pneumocephalus Associated with Epidural Anesthesia for Labor Sudama Reddi, Valentyna Honchar, Matthew Robbins Aging, Dementia, and Cognitive and Behavioral Neurology: Epidemiology P5.208 Learning from our Mistakes: APOE4 Influences Misdiagnosis of Alzheimer’s Disease and Frontotemporal Degeneration Jenna Haley, Corey McMillan, David Irwin, Beth McCarty Wood, Katya Rascovsky, David Wolk, John Trojanowski, Leslie Shaw, Vivianna Van Deerlin, Murray Grossman P5.209 Epidemiology of Tandem Gait Abnormalities in Aging Ilya Bragin, Vijayaleskhmi Nair, Joe Verghese P5.210 Risk Factors for Cognitive Change in Patients with Dementia Due to Alzheimer’s Disease Fabricio Oliveira, Paulo Bertolucci, Marilia Smith, Elizabeth Chen P5.211 Prevalence, Incidence, and Associations between APOE Genotype, Cardiovascular Risk Factor, and Dementia in Cuban Populations Jorge Jesús Llibre Guerra, Milagros Guerra, Juan Carlos Llibre Guerra, Juan Jesús Llibre Rodriguéz P5.212 Cardiac Function and the Risk of Dementia Renée de Bruijn, Maarten Leening, Oscar Franco, Albert Hofman, Peter Koudstaal, Mohammad Ikram P5.213 Long-term Mortality in Incident MCI Subtypes. Data from the NEDICES Cohort Félix Bermejo-Pareja, Alvaro Sánchez-Ferro, Israel Contador Castillo, Elina Boycheva, Rocio Trincado, Sara Llamas, Alejandro Herrero, Fernando Sierra, Alberto Villarejo Galende, Julian Benito-Leon P5.214Plasma β-Amyloid and MRI markers of Structural Brain Aging Sara Kaffashian, Christophe Tzourio, Aicha Soumare, Carole Dufouil, Bernard Mazoyer, Susanna Schraen-Maschke, Luc Buee, Stephanie Debette P5.215 Comparing Cognitive Screening Tools in a Rural Ecuadorian Population: The Atahualpa Project Clinton Wright, Hannah Gardener, Mauricio Zambrano, Victor Del Brutto, Oscar Del Brutto Poster Session V P5.216 Cognitive Impairment, Asymptomatic Carotid Stenosis and Arterial Hypertension in Adult Persons Without a History of Stroke: A PopulationBased Epidemiological Study Petya Mineva, Dimitar Talalaev, Valentin Proychev Aging, Dementia, and Cognitive and Behavioral Neurology: Cerebrovascular Ischemia, Metabolism, and Epidemiology P5.217 Cognitive Enhancer Based Treatment Outcome in Mild to Moderate Alzheimer’s Disease Is Modulated by Severity of White Matter Hyperintensity Kok Pin Ng, Aloysius Ng, Nagaendran Kandiah P5.218 Clinical Predictors of a Higher Cerebrovascular Burden in Dementia: A Clinicopathological Study. Solene Moulin, Julia Salleron, Gauthier Calais, Florence Pasquier, Vincent Deramecourt P5.219 Food Insecurity Is Associated with Development of Faster Cognitive Decline in the Boston Puerto Rican Health Study Janice Wong, Tammy Scott, Yinge Li, Katherine Tucker, Xiang Gao P5.220 Silent Cerebral Ischemia Is Highly Prevalent in AD and Is Independently Associated with Medial Temporal Atrophy Nagaendran Kandiah, Russell Chander, Aloysius Ng, Pryseley Assam P5.221 Effectiveness of Cognitive Enhancers in Alzheimer’s Disease with Concomitant Small Vessel Cerebrovascular Disease. Kok Pin Ng, A Ng, E Heng, S Huang, P Assam, Nagaendran Kandiah P5.222 Burden of Silent Cerebrovascular Disease and Not Acute Infarct Characteristics Determine PostStroke Cognitive Impairment, Both in Small Vessel and Large Vessel Strokes Yen Yeong Poh, Yun Qi Josephine Poh, Aloysius Ng, Maznah Marmin, Yee Lean Ho, Hani Zainal, Nagaendran Kandiah P5.223 Pharmacogenetics of Lipid Metabolism Modulators in Patients with Dementia Due to Alzheimer’s Disease Fabricio De Oliveira, Paulo Bertolucci, Marilia Smith, Elizabeth Chen P5.224 Evidence on Diet Modification for Alzheimer’s Disease and Mild Cognitive Impairment Hilary Glazer, Christine Greer, Dulce Barrios, Christopher Ochner, James Galvin, Richard Isaacson P5.225 Dementia: An Emerging Field in Pakistan Quratulain Khan P5.226 Forgetful But Not Disabled: Predictors of Incident IADL Limitations Pamela Rist, Jessica Marden, Benjamin Capistrant, Qiong Wu, M. Maria Glymour Aging, Dementia, and Cognitive and Behavioral Neurology: Creutzfeldt-Jakob Disease and Subacute Encephalopathies P5.227 A Case of Refractory Hashimoto’s Encephalopathy Demonstrating Improvement with Plasmapheresis Sarah Nelson, Yasir Jassam, Lynne Taylor P5.228 Voltage Gated Calcium Channels Antibody-associated Autoimmune Encephalitis Abdulrahman Alwaki, Anibal Lugo, Christopher Goshgarian, Omar Ahmad, Hebah Hefzy, Panayiotis Mitsias P5.229 Hashimoto Encephalopathy: A Study of Clinical Profile, Radiological and Electrophysiological Correlation in a Tertiary Care Centre in South India Rangasetty Srinivasa, Surya Sharma, J.v. Mahendra, Rohan. Mahale, Madhusudhan B.K P5.230 Reversible Dementia with Myoclonus due to Concurrent HSV-2 and Syphilis Central Nervous System Infection in an Immunocompetent Man. Liliana Robles, Aashish Anand, Joseph Kass P5.238 Paired Comparison Study Distinguishing Parkinsonian Dementia Syndromes from Parkinson’s Disease Douglas Scharre, Shu-Ing Chang, Haikady Nagaraja, Ariane Park, Punit Agrawal, Anahita Adeli, Shannon Linder, Anne Kloos, Deborah Kegelmeyer, Nora Fritz, Maria Kataki P5.239 Education Effects on Rate of Cognitive Decline Compared in Autopsy Confirmed Alzheimer’s, Lewy Body and Vascular Dementia Lyla Mourany, Jagan Pillai P5.240 Cognitive and Behavioral Changes in PSP: Comparison of PSPParkinsonism with PSP-Richardson Syndrome Saria Refai, Linda Hershey, David Thompson, Jennifer Lippoldt P5.241 Direction of Finger Displacement in Parkinson Disease (PD) May Predict the Onset of Dementia Aman Deep, Abraham Lieberman, Rohit Dhall, An Tran, Ming-Jai Liu, Kamala Saha, Naomi Salins, Arshia Sadreddin, Guillermo Moguel-Cobos, John Karis, Narayanan Krishnamurthi P5.242 Presence of Voltage-gated Potassium Channel (VGKC)-complex Antibody in a Case of Genetic Prion Disease Adham Jammoul, Richard Lederman, Jinny Tavee, Yuebing Li Transcranial Sonography(TCS) in Lewy Body Disease (LBD) Versus Other Dementia. Correlation with Clinical Symptoms. Maria Fernandez, Nuria Campora, Waleska Berrios, Juan Ignacio Rojas, Jorge Norscini, Edgardo Cristiano, Angel Golimstok P5.232 P5.243 P5.231 Creutzfeldt-Jakob Disease with Unusual Finding of Significant CSF Pleocytosis Pawan Rawal, Drew Uhrig, Leonardo Almeida, Hassan FathallahShaykh P5.233 Hyperacusis as the Initial Presentation of Creutzfeldt-Jakob Disease Alexander Merkler, Joseph Safdieh P5.234 Increased Interleukin-17 in the Cerebrospinal Fluid in Sporadic CreutzfeldtJakob Disease Koji Fujita, Naoko Matsui, Yukitoshi Takahashi, Yasushi Iwasaki, Mari Yoshida, Tatsuhiko Yuasa, Yuishin Izumi, Ryuji Kaji P5.235 Wernicke-Korsakoff Syndrome Mimicking Sporadic Jakob-Creutzfeldt Disease Serggio Lanata, Pierluigi Gambetti, Michael Geschwind P5.236 Novel Pomegranate Oil NanoEmulsions for the Prevention and Treatment of Neurodegenerative Diseases: The Case of Genetic CJD Ruth Gabizon, Michal Mizrahi, Yael Friedman-Levy, Liraz Larush, Kati Frid, Orli Binyamin, Nina Feinstein, Dvir Dori, Haim Ovadia, Tamir Ben-Hur, Shlomo Magdassi Aging, Dementia, and Cognitive and Behavioral Neurology: Behavioral Neurology of Movement Disorders P5.237 Environmental Predictors of Cognitive Impairment in Parkinson’s Disease Anna Blanken, Mona Beyer, OleBjorn Tysnes, Guido Alves, Jan Larsen, Liana Apostolova Simple Motor Stereotypies Are Not Specific Core Features of Behavioral Frontotemporal Dementia Sara Pompanin, Chiara Formentin, Zarantonello Giulia, Nela Jelcic, Giacomo Rolma, Matteo Tagliapietra, Giovanni Zorzi, Annachiara Cagnin P5.244 Modulation of FeedbackRelated Negativity During Trial-and-error Task in Parkinson Disease: Assessing the Role of Apathy and Depression in Cognitive Deficits René Quilodran, Laura Viñales, Alex Araneda, Irving Santos, Francisco Castilla P5.245 Focused Ultrasound Thalamotomy Modulates Inhibitory Motor Control in Essential Tremor Scott Sperling, Carol Manning, W. Jeffrey Elias, Scott Wylie P5.246 A Common Movement Abnormality in Patients with LGI1 Limbic Encephalitis Is a Manifestation of Tonic Seizures. Danielle Andrade, Peter Tai, Josep Dalmau, Richard Wennberg Movement Disorders: Atypical Parkinsonism P5.247 Clinical Features of Patients with Concomitant Parkinson’s Disease and Progressive Supranuclear Palsy Pathology Heather Rigby, Brittany Dugger, Charles Adler, Thomas Beach, Holly Shill, Erika Driver-Dunckley, Marwan Sabbagh, Lucia Sue, John Caviness P5.248 Three Sib-Pairs of AutopsyConfirmed Progressive Supranuclear Palsy Shinsuke Fujioka, Monica Sanchez Contreras, Audrey Strongosky, Kotaro Ogaki, Nathaniel Whaley, Pawel Tacik, Jay Van Gerpen, Ryan Uitti, Owen Ross, Zbigniew Wszolek, Rosa Rademakers, Dennis Dickson P5.249 Mutational Analysis of COQ2 in Italian Patients with MSA Dario Ronchi, Sara Bonato, Ernesto Di Biase, Valentina Melzi, Ilaria Trezzi, Stefania Corti, Nereo Bresolin, Giacomo Comi, Alessio Di Fonzo P5.250 Hypercapnic Respiratory Failure Is Often Seen in Advanced Progressive Supranuclear Palsy Nobu Komai, Chiho Ishida, Kazuya Takahashi, Atsuro Tagami P5.251 FDG-PET in Pathologically Confirmed 4R-Tauopathy Variants Nicholas Zalewski, Hugo Botha, Jennifer Whitwell, Val Lowe, Dennis Dickson, Keith Josephs P5.252 Human Mirror Neuron System Is the Anatomical Substrate for Imitation Apraxia in Corticobasal Syndrome: (18F)FDG PET and MRI studies HyukJun Yoon, Seok Min Kim, Hyuk Jin Yun, Kyung A Kim, Doris Doudet, Jong-Min Lee, Chong S Lee P5.253 Do Autonomic Studies Help Differentiate Multiple System Atrophy from PD with Dysautonomia in Clinical Practice? Aashoo Mentreddi, Svjetlana Miocinovic, Pravin Khemani, Steven Vernino, Srikanth Muppidi P5.254 Atypical Parkinsonism Following Occult Carbon Monoxide Exposure Shruti Raja, Tara Dutta, Justin Kwan P5.255 A Case of Klinefelter Syndrome Associated with Parkinsonism Lourdes Lago, Henry Moore, Carlos Singer Movement Disorders: Cognition and Parkinson’s Disease P5.256 Which Cognitive Subdomain Is Related with Motor Symptoms in the Early Stage of Parkinson’s Disease? Minjik Kim P5.257 Hallucinations and Dementia in Parkinson’s Disease: Clinically Related But Structurally Distinct Jennifer Goldman, Glenn Stebbins, Doug Merkitch, Vy Dinh, Bryan Bernard, Leyla DeToledo-Morrell, Christopher Goetz P5.258 What Level of Parkinson’s Disease Severity Is Associated with Significant Differences in Cognitive Function? Christian Lachner, Melissa Armstrong, Ann Gruber-Baldini, Erik Barr, Paul Fishman, Stephen Reich, William Weiner, Lisa Shulman P5.259 Association of Cognitive Screening Tests with Disability in Parkinson’s Disease Melissa Armstrong, Erik Barr, Ann Gruber-Baldini, Stephen Reich, Christian Lachner, Paul Fishman, Lisa Shulman Fast, Easy Registration Online · AAN.com/view/AM14 99 Wednesday April 30 First Authors stand by Posters from 5:00 p.m.–6:30 p.m. Wednesday, April 30 P5.260 Long-term Outcomes of Parkinson’s Disease Patients with Normal Cognition. Kara Pigott, Jacqueline Rick, Howard Hurtig, Alice Chen-Plotkin, John Duda, James Morley, Lama Chahine, Nabila Dahodwala, Jori Fleisher, Rizwan Akhtar, Andrew Siderowf, Rachel Goldmann Gross, Sharon Xie, John Trojanowski, Daniel Weintraub P5.261 Parkinson’s Disease Patients with Mild Cognitive Impairment do Not Have Increased Brain Iron Concentrations as Compared to Patients Without Cognitive Impairment Jesper Hagemeier, Thomas Guttuso, Niels Bergsland, Mari HeininenBrown, Ellen Carl, David Lichter, Robert Zivadinov P5.262 Cognitive Deficits in Veterans with Parkinson’s Disease: A National Database Analysis Brandon Barton, Zhiping Huo, Sandra Kletzel, Kevin Stroupe, Christopher Goetz, Frances Weaver P5.263 Cholinesterase Inhibitors for Cognitive Impairment in Patients with Parkinson’s Disease: A MetaAnalysis Gennaro Pagano, Giuseppe Rengo, Michele Tagliati P5.264 Parkinson’s Disease Motor Phenotype Predicts Cognitive Performance David Isaacs, Joshua Herb, Nelleke Van Wouwe, Daniel Claassen P5.265 Lower Education Status Associates with Axial Motor Burden in Parkinson Disease Vikas Kotagal, Roger Albin, Martijn Muller, Robert Koeppe, Kirk Frey, Nicolaas Bohnen Movement Disorders: Sleep and Movement Disorders and Miscellaneous Diagnoses P5.266 Restless Limbs Syndrome (RLS) Presenting as Hemisyndrome: A Case of Dejerine-Roussy Syndrome Responsive to Dopamine Agonists David Dickoff P5.267 Restless Limb Syndrome (R.L.S.): The Real Patient Experience. David Dickoff, Stephanie Dontje P5.268 Effect of Rotigotine Transdermal System on Nocturnal Blood Pressure Changes Associated with Periodic Limb Movements During Sleep in Patients with Restless Legs Syndrome Wolfgang Oertel, Axel Bauer, Werner Cassel, David Rye, Arthur Walters, John Winkelman, Lars Bauer, Lars Joeres, Frank Grieger, Kimberly Moran, Erwin Schollmayer, John Whitesides, Claudia Trenkwalder P5.269 Extrapontine Myelinolysis Presenting as L-DOPA-Unresponsive Parkinsonism Nicolaas Anderson, Akshay Shah P5.270 Effect of IVIg on GAD Epitopes in Patients with Stiff-Person Syndrome: Implications for Other Antibody-Mediated Neurological Disorders Responding to IVIg Penelope Fouka, Harry Alexopoulos, Panagiotis Politis, Marinos Dalakas P5.271 Movement Disorders in Chronic Regional Pain Syndrome (CRPS) Mitesh Lotia, Kathrin LaFaver 100 P5.272 Hyperactivity and Obsessive Compulsive Disorder: An Unusual Presentation in Perry Syndrome. A Clinicopathological Study. Guillaume Lamotte, Françoise Chapon, Gilles Defer P5.273 Factors Influencing Medical Treatment of Parkinsonism with Conflicting DaT Imaging: The Cleveland Clinic Experience Dimitrios Nacopoulos, Srivadee Oravivattanakul, Anwar Ahmed, Hubert Fernandez P5.274 Dopaminergic Neurons Loss in Parkinson’s Disease: How Much Sex Hormones Decline Contribute to? Mahmoud Elhusseiny, Mohamed Sarhan, Mohamed Salama, Mohamed Elgamal, Sherif Shawer, Ahmed Attia, Mohamed Sobh P5.275 Investigating the Night to Night Variability of REM Without Atonia in Parkinson’s Disease Samuel Bolitho, Sharon Naismith, Ron Grunstein, Zoe Terpening, Moran Gilat, Simon Lewis Sleep: Sleep Related Breathing P5.276 Frequency and Causes of Discontinuation of Continuous Positive Airway Pressure Treatment in Multiple System Atrophy Takayoshi Shimohata, Hideaki Nakayama, Masatoyo Nishizawa P5.277 REM Sleep Rebound on a First CPAP Recovery Night in Severe Obstructive Sleep Apnea Patients Raoul Biniaurishvili P5.278 PAP Therapy Boosts REM Dependent Memory Consolidation for Perceptual Skill Learning in Patients with Obstructive Sleep Apnea. Heidi Roth, Chayla Hart, David Sanders, Young Truong, Bradley Vaughn, Robert Stickgold P5.279 Subjective Sleep Quality and Insomnia: Correlation with Cardiovascular Health Status in Community-Dwelling Elders Living in Rural Coastal Ecuador— The Atahualpa Project Pablo Castillo, Oscar Del Brutto, Robertino Mera, Victor Del Brutto P5.280 OSA Is Under-reported in Patients Admitted with Acute Stroke Scott Shorten, Richard Dubinsky P5.281 A Pilot Study Identifying a Unique Pattern on the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) that Predicts Obstructive Sleep Apnea (OSA) in a Dementia Screening Setting Amber Gerber, Donn Dexter P5.282 A Novel Capability for Monitoring Cerebral and Systemic Hemodynamics, ECG and Actigraphy During Sleep Vladimir Ivkovic, Gary Strangman, Quan Zhang P5.283 Diagnostic Thresholds for Quantitative REM Sleep Muscle Densities, Phasic Burst Duration, and REM Atonia Index in REM Sleep Behavior Disorder with Co-morbid Obstructive Sleep Apnea Erik St. Louis, Stuart McCarter, Bradley Boeve, Michael Silber 3:00 p.m.–6:30 p.m. Sleep: Parasomnias and Measurement Technologies P5.284 Cortical Excitability Relation to Periodic Leg Movements (PLMS) and Sleep in Restless Legs Syndrome (RLS) Rachel Marie Salas, Aadi Kalloo, Tiana Krum, Richard Allen P5.285 Sleep Quality, Duration, Insomnia Symptoms, and Prevalence of Sleep Disordered Breathing in Parkinson’s Disease Shirin Shafazand, Douglas Wallace, Silvia Vargas, Henry Moore, Corneliu Luca, Heather Katzen, Bonnie Levin, Carlos Singer P5.286 Comparing Periodic Limb Movements in Sleep in Subjects with and Without Waking Paretic/Plegic Limbs Mark Dyken, Miriam Zimmerman, Kyoungbin Im, Deborah Lin-Dyken, Christine Glenn, Mark Blumberg, Robert Rodnitzky, Greta Sokoloff P5.287 Use of a Non-invasive Neurotechnology, HIRREM, Is Associated with Improved Sleep and Mood in a Heterogeneous Cohort. Jared Cook, Catherine Tegeler, Sung Lee, Hossam Shaltout, Meghan Franco, Charles Tegeler P5.288 Treatment of Restless Legs Syndrome (Willis-Ekbom Disease) with Rotigotine and Pramipexole. Diego GarciaBorreguero, Melissa Sweeney P5.289 The Effect of Prior Exposure to Dopamine Agonists (DA) on Response to Treatment with Gabapentin Enacarbil (GEn) in Adult Patients with Moderate-toSevere Primary Restless Legs Syndrome (RLS): Pooled Analyses from 3 Randomized Trials William Ondo, Neal Hermanowicz, Diego García-Borreguero, Mark Jaros, Richard Kim, Gwendoline Shang P5.290 The Efficacy of Gabapentin Enacarbil (GEn) in Adult Patients with Severe Primary Restless Legs Syndrome (RLS): Pooled Analyses from 3 Randomized Trials Daniel Lee, William Ondo, Alon Avidan, Diego García-Borreguero, Mark Jaros, Richard Kim, Gwendoline Shang P5.294 Kleine-Levin Syndrome with Rapid Cycling—Case Report and Review of the Literature Claudio De Gusmao, Kiran Maski, David Urion P5.295 Sleep Dependent Memory Consolidation in Children with Autism Spectrum Disorders Kiran Maski, Hannah Holbrook, Dara Manoach, Ellen Hanson, Kush Kapur, Robert Stickgold P5.296 Evaluation of the Effect of Modafinil on Cognitive Functions in Patients with Idiopathic Hypersomnia with P300 Mehmet Yaman, Fatıma Karakaya, Hasan Mayda, Ibrahim Guzel, Gokhan Koyuncu, Serdar Oruc P5.297 Sleep and Sleep Disruption in Predator Odor Trauma Model of Posttraumatic Stress Disorder Omar Taranissi, Rishi Sharma, Pradeep Sahota, Mahesh Thakkar P5.298 Sudden Onset of Sleep Due to Bilateral Hypothalamic Lesions in Neuromyelitis Optica Spectrum Disorder Positive for Aquaporin 4 Antibody (AQP4) Hidehiko Okuma, Yuki Hatanaka, Kuwabara Midori, Kanbayashi Takamichi, Masahiro Sonoo Neuro Trauma, Critical Care, and Sports Neurology: Concussion P5.299 A Portable Non-invasive Biosensor Based Approach to Actively Assess Sports Concussion and Mild Traumatic Brain Injury Adam Simon, Janet Van Gelder, Hashem Ashrafiuon, David Devilbiss P5.300 Effect of Concussion and Blast Exposure on Clinical Symptoms Following Deployment of U.S. Military Personnel Mikias Wolde, Briana Perry, Jay Haran, Justin Campbell, Alia Creason, Catalina Sher, Lauren Stentz, Jack Tsao P5.301 Hyperglycemia and Leukocytosis as Predictors of Abnormal Head CT Following Concussion Aakash Bodhit, Yasamin Daneshvar, Pratik Patel, Keith Peters, Latha Ganti P5.291 P5.302 Sleep: Intrinsic Disorders of Sleep P5.303 Subjective Perception of Sleepiness in a Driving Simulator Is Different from Perception in the Maintenance of Wakefulness Test David Schreier, Corinne Roth, Johannes Mathis P5.292 Energy Expenditure in Narcolepsy Patients and Controls Claire Donjacour, Paul Schoffelen, Sebastiaan Overeem, Gert Jan Lammers, Hanno Pijl, Klaas Westerterp P5.293 Respiratory Safety of the Orexin Receptor Antagonist Suvorexant During Sleep in Patients with Compromised Respiratory Function and in Healthy Subjects Matthew Troyer, Naoto Uemura, Jackie McCrea, John Palcza, Mardik Donikyan, Gary Zammit, Rong Liu, Tara Siringhaus, Janice Rowe, Deborah Card, Sabrina Marsilio, Timothy Grant, Russell Rosenberg, John Wagner, Hong Sun 2O14 Scientific Abstract Listing and Annual Meeting Information Validation of a SelfAdministered iPad®- and iPod®-Based Tool for Assessing Information Processing Andrew Russman, Joshua Hirsch, David Schindler, Daniel Burke, Susan Linder, Jay Alberts A Potential Biomarker in Sports-Related Concussion: Brain Functional Connectivity Alteration of the Default-mode Network Measured with Sequential Resting-state fMRI David Zhu, Tracey Covassin, Sally Nogle, Scarlett Doyle, Doozie Russell, Randolph Pearson, Jeffrey Monroe, Christine Liszewski, J DeMarco, David Kaufman P5.304 Structural Imaging Correlations with Memory Assessment and Concussion in Retired NFL Athletes Kyle Womack, Jeremy Strain, Nyaz Didehbani, Heather Conover, Michael Kraut, Munro Cullum, John Hart Poster Session V P5.305 Atlanto-axial Subluxation: Treatable Cause of Post Concussion Syndrome Kevin Crutchfield, Dennis Rivenburgh, Laura Morris, Jenna Werner P5.317 P5.306 Prevalence of Sleep and Psychiatric Disorders in Patients Who Present to the Emergency Department with Concussion Pratik Patel, Aakash Bodhit, Yasamin Daneshvar, Latha Ganti P5.318 P5.307 P5.319 The King-Devick Test Is Vastly Superior to the Symbol Digit Modalities Test as a Sideline Determinant of Concussion in Mixed Martial Arts Fighters Daniel Kantor P5.308 Barriers to Recovery after Concussion Teena Shetty, Kelianne Cummings, Christine Villegas, Erin Manning, Niesha Voigt, Maxwell Singer, Joseph Nguyen P5.309 Post Concussion Delirium in Children: Two Cases Gail Schuman P5.310 fMRI Neuropsychological Battery for Athletes with Concussion David Hubbard, Adam Hampshire, Adrian Owen P5.311 The Utility of Pain Drawings in the Diagnosis and Treatment of Military Post-traumatic Headache Alan Finkel, Juanita Yerry, Brian Ivins, Young Choi P5.312 Clinical Course of Recovery from Concussion in Children 6-12 Years of Age Sarah Risen, Jennifer Reesman, Gayane Yenokyan, Kelly Clark, Beth Slomine, Stacy Suskauer P5.313 Use of a Non-invasive Neurotechnology, HIRREM, Is Associated with Improved Sleep, Mood, and Baroreflex Sensitivity in Athletes with Persisting PostConcussion Symptoms Charles Tegeler, Catherine Tegeler, Jared Cook, Sung Lee, Meghan Franco, Lee Gerdes, Hossam Shaltout Field Utilization of the Cleveland Clinic Concussion iPad Assessment Tool Jay Alberts, Joshua Hirsch, Susan Linder, David Schindler Quantification of the Balance Error Scoring System with an iPad Application David Schindler, Susan Linder, Mandy Koop, Joshua Hirsch, Daniel Kana, Jay Alberts Consequences of Traumatic Brain Injury in Male Ice Hockey Players Ozan Toy, Mill Etienne, Ronald Bogdasarian P5.320 Comparison of Common Football Helmets in Preventing Concussion, Hemorrhage and Skull Fracture Using a Modified Drop Test. John Lloyd, Francis Conidi Neuro Trauma, Critical Care, and Sports Neurology: Traumatic Brain Injury P5.321 A Multiscale Biology Approach in the Identification of Dementia Risks in Subjects with TBI History Giulio Pasinetti, Ke Hao, Drew Helmer P5.322 MEG Findings Correlate to Speech-Language Pathology Deficits in Combat-Related mTBI and PTSD Maria DeGraba, Warren Merrifield, Erin Mattingly, Judy Mikola, Mihai Popescu, Anda Popescu, Alexander Balbir, Thomas Balkin, Joseph Bleiberg, Thomas DeGraba P5.323 Etiology and Epidemiology of Traumatic Brain injury in Relation to Gender Differences Among African American Patients Lien Diep, Robert Farney, Stacy Cary-Thompson, Jean Belcourt, Robert Farney, Janaki Kalyanam, Annapurni JayamTrouth P5.324 P5.314 Onabotulinum Toxin A for the Treatment of Chronic Post-Traumatic Headache in Service Members with a History of Mild Traumatic Brain Injury Juanita Yerry, Alan Finkel, Devon Kuehn, Steven Lewis P5.315 P5.325 Alterations in Network Dynamics Following Blast-induced Mild Traumatic Brain Injury Andrei Vakhtin, Paul Taylor, Corey Ford Thalamic Volumes and Exposure to Head Trauma in Retired Professional Fighters Charles Bernick, Sarah Banks, Nancy Obuchowski, Wanyong Shin, Mark Lowe, Michael Phillips, Michael Modic, Stephen Jones P5.316 Post-traumatic Headache in Soldiers: A Retrospective Record Review of Active Duty Soldiers Presenting to a Military Concussion Care Clinic Center for Evaluation and Treatment of Headache Alan Finkel, Juanita Yerry, Brian Ivins, Young Choi Is There Chronic Brain Damage in Retired NFL Players? Neuroradiology, Neuropsychology and Neurology of 45 Retired Players Ira Casson, David Viano, E. Mark Haacke, Zhifeng Kou, Danielle LeStrange P5.326 Progressive Return to Activity Following Acute mTBI: A Standardized Approach Robert Labutta, Therese West, Helen Coronel, Katherine Helmick P5.327 Interdisciplinary Assessment and Care in Service Members with Combat Related TBI and PTSD Thomas DeGraba, James Kelly, Joseph Bleiberg, Geoffrey Grammer, Jesus Caban, Jennifer Bell, Robert Koffman P5.328 Thromboelastography Defines Late Hypercoagulability After TBI Allie Massaro, Sean Doerfler, Kelsey Nawalinski, Nicolette Driscoll, Connie Ju, Hiren Patel, Sarah Nyirjesy, Francis Quattrone, Suzanne Frangos, Eileen Maloney-Wilensky, Robert Siman, Sean Grady, Sherman Stein, Scott Kasner, Monisha Kumar P5.329 Mid-life Hypometabolism in the Precuneus May Be Associated with Prior History of Traumatic Brain Injury (TBI) Salil Soman, Jauhtai Cheng, Steven Chao, Jennifer Kong, Maheen Adamson, J. Wesson Ashford, Ansgar Furst P5.330 Antiplatelet Agent Use Impacts Mortality But Not Progression of Hemorrhagic Injury After Traumatic Brain Injury Richard Choi, Rajanandini Muralidharan, Connie Ju, Kelsey Nawalinski, Francis Quattrone, Suzanne Frangos, Eileen Maloney-Wilensky, Sue Auerbach, Elsa Lin, Michael Miszczanczuk, Bruce Sachais, Patrick Kim, Scott Kasner, Soojin Park, Joshua Levine, W Kofke, Peter Leroux, Monisha Kumar P5.331 The Natural History of Acute Recovery of Blast-induced Mild Traumatic Brain Injury: A Case Series During War Jason Hawley, David Larres, Elizandro Gonzales, Walter Carr P5.332 A Portable Non-invasive Biosensor Based Approach to Actively Assess Cognitive Function and Mild Traumatic Brain Injury Stephen Martino, Adam Simon, David Devilbiss P5.336 Subarachnoid Hemorrhage— Which Grading Scale Best Predicts Outcome? Kushak Suchdev, Hardik Doshi, Mohammad Ibrahim, Navid SerajiBozorgzad P5.337 How Much Does a Traumatic Brain Injury Cost? Aakash Bodhit, Pratik Patel, Yasamin Daneshvar, Keith Peters, Latha Ganti P5.338 Utility of Non-conventional MRI in Assessing White Matter Damage After Carbon Monoxide Poisoning Hiroshi Kuroda, Kazuo Fujihara, Shigeki Kushimoto, Masashi Aoki P5.339 The Burden of Pediatric Spinal Cord Injury in the United States Shalini Selvarajah, Eric Schneider, Adil Haider, Daniel Becker, Edward Hammond P5.340 Utility of EEG During the Early Hospital Course After Resuscitation from Cardiac Arrest Elizabeth Cahill, David Tirschwell, Glenn Schubert, Mark Holmes, Shahin Hakimian, W. T. Longstreth, Michele Olsufka, Kim Francis P5.341 Study of Pseudobulbar Affect Symptoms in Veterans with Mild Traumatic Brain Injury Jennifer Fonda, Regina McGlinchey, William Milberg, James Rudolph, Phillip Hunt, Matthew Reynolds, Charles Yonan P5.342 Management of Intracranial Hemorrhage and Return to Play in Sports: Cases Without Neurologic Deficit Jose Posas, Vernon Williams P5.343 CNS Injuries Associated with the Sport of Ice Hockey. Ozan Toy, Arielle Berkowitz, Mill Etienne Neuro Trauma, Critical Care, and Sports Neurology: Outcomes P5.333 The Value of Neurocognitive Testing after Mild TBI in the Emergency Department Latha Ganti, Pratik Patel, Aakash Bodhit, Yasamin Daneshvar, Keith Peters P5.334 Ventilator Associated Pneumonia in Neurology and Neurosurgery Intensive Care Unit: Incidence, Risk Factors and Pathogens Man Mohan Mehndiratta, Rajeev Nayak, Sanjay Pandey, Ajay Sharma, Archana Thakur P5.335 Developing an Emergency Department Based Protocol for Evaluating Concussion—a Prospective Observational Study Latha Ganti, Pratik Patel, Aakash Bodhit, Yasamin Daneshvar, Keith Peters Available March 2014! Browse abstracts for the Annual Meeting Scientific Program with the Annual Meeting mobile app available for iPhone®, iPad®, and Android® devices. Abstracts will also be searchable online. Learn more at AAN.com/view/AM14. Fast, Easy Registration Online · AAN.com/view/AM14 101 Wednesday April 30 First Authors stand by Posters from 5:00 p.m.–6:30 p.m. Wednesday, April 30 4:00 p.m.–5:45 p.m. Utilizing a similar format to the popular Emerging Science Session, these dynamic sessions will feature five-minute author presentations followed by five-minutes of questions and answers. The session will conclude with all authors participating in a panel discussion. S34 MS and CNS Inflammatory Disease: Risk Factors for MS Disease and Course S35 Cerebrovascular Disease and Interventional Neurology: Issues in Acute Treatment 4:00 p.m. S34.001 Integrating Genetic Burden and Environmental Factors to Stratify Risk for Multiple Sclerosis Zongqi Xia, Alina von Korff, Daniel Reich, Lori Chibnik, Philip De Jager 4:00 p.m. S35.001 Minor Stroke and Rapidly Improving Stroke Symptoms: To Treat or Not to Treat?! Clotilde Balucani, Riccardo Bianchi, Edward Feldmann, Jeremy Weedon, Steven Levine 4:10 p.m. S34.002 A Multivariate Risk Calculator for Multiple Sclerosis and Study of an Endophenotype in Siblings of People with Multiple Sclerosis Ruth Dobson, Joanne Topping, Declan Chard, Klaus Schmierer, Paul Smith, Sreeram Ramagopalan, Gavin Giovannoni 4:10 p.m. S35.002 Expedited Code Stroke Protocol: An Updated Experience Ilana Spokoyny, Rema Raman, Karin Ernstrom, Dawn Meyer, Justin Sattin, Thomas Hemmen, Brett Meyer 4:20 p.m. S34.003 Hormonal Contraceptives and Multiple Sclerosis Susceptibility Kerstin Hellwig, Lie Chen, Annette Langer-Gould 4:30 p.m. S34.004 Population Attributable Fractions and Joint Effects Among Key Risk Factors for Multiple Sclerosis: The Ausimmune Study Ingrid van der Mei, Robyn Lucas, Bruce Taylor, Anne-Louise Ponsonby 4:40 p.m. S34.005 Vaccines and the Risk of Multiple Sclerosis and Other CNS Demyelinating Diseases Annette Langer-Gould, Lie Chen, Sara Tartof, Chun Chao, Hung-Fu Tseng 4:50 p.m. S34.006 Early Relapse-recovery Impacts Progressive Disease Course in Multiple Sclerosis Martina Novotna, Melih Tutuncu, M. Paz Soldan, Daniel Crusan, Elizabeth Atkinson, Orhun Kantarci 5:00 p.m. S34.007 Measuring Enduring Worsening of Multiple Sclerosis in the Combirx Study Fred Lublin, Stacey Cofield, Flavia Nelson, Ponnada Narayana, Tarah Gustafson, Jerry Wolinsky, Gary Cutter 5:10 p.m. S34.008 Are Recent Hispanic Immigrants at Higher Risk of Disability with Multiple Sclerosis? Lilyana Amezcua, Karina Ladezma, Maziar Eslami, Jose Aparicio, Annette Langer-Gould 5:20 p.m. S34.009 CSF1R Gene Screening in a Cohort of 218 Primary Progressive Multiple Sclerosis (PPMS) Patients from the Norwegian and Swedish National PPMS Registries Christina Sundal, Matthew Baker, Virginija Karrenbauer, Kjell-Morten Myhr, Kristoffer Haugarvoll, Shinsuke Fujioka, Hanne Harbo, Jan Aasly, Jan Hillert, Zbigniew Wszolek, Rosa Rademakers, Oluf Andersen 5:30 p.m. Panel Discussion 4:20 p.m. S35.003 Effect of IV rtPA in Mild Strokes in the Third International Stroke Trial (IST3) Pooja Khatri, Darren Tayama, Geoff Cohen, Richard Lindley, Joanna Wardlaw, Sharon Yeatts, Joseph Broderick, Peter Sandercock 4:30 p.m. S35.004 Futile Revascularization After Mechanical Thrombectomy for Acute Ischemic Stroke: Pooled Analysis of the Multi MERCI, TREVO and TREVO 2 Trials Zhong-Song Shi, David Liebeskind, Bin Xiang, Sijian Grace Ge, Lei Feng, Gregory Albers, Ronald Budzik, Thomas Devlin, Rishi Gupta, Olav Jansen, Tudor Jovin, Monika Killer-Oberpfalzer, Helmi Lutsep, Juan Macho, Raul Nogueira, Marilyn Rymer, Wade Smith, Nils Wahlgren, Gary Duckwiler 4:40 p.m. S35.005 Testing the Presumption of Consent to Emergency Thrombolysis for Stroke Winston Chiong, Anthony Kim, Ivy Huang, Nita Farahany, S. Josephson 4:50 p.m. S35.006 Prehospital Factors Associated with Stroke Misdiagnosis by EMS Providers Ethan Brandler, Mohit Sharma, Elizabeth Helzner, Steven Levine 5:00 p.m. S35.007 CT Perfusion Variables Within 4.5 Hours of Stroke: Relating Physiology to Time Since Onset Smriti Agarwal, Tomasz Matys, S Tulasi Marrapu, Jennifer Mitchell, P Simon Jones, Jean-Claude Baron, Elizabeth Warburton 5:10 p.m. S35.008 Acute Stroke Reperfusion Trends in the Expanded Time Window Era Ganesh Asaithambi, Xin Tong, Mary George, Albert Tsai, James Peacock, Russell Luepker, Kamakshi Lakshminarayan 5:20 p.m. S35.009 National Trends in Utilization and Outcomes of Intravenous Thrombolytic Treatment Among Pediatric Patients with Acute Ischemic Stroke in United States Mohammad Afzal, Saqib Chaudry, Taqi Zafar, Mohammad Owais, Malik Adil, Vishal Jani, Gautam Sachdeva, Swaroop Pawar, Syed Hussain, Adnan Qureshi 5:30 p.m. 102 S36 Neuromuscular Disease: Clinical 4:00 p.m. S36.001 ALS-Plus Syndrome: Nonmotor Features in a Large ALS Cohort Shannon Vandriel, Leo McCluskey, Lauren Elman, Ashley Boller, Murray Grossman 4:10 p.m. S36.002 Prevalence, Course and Associations of Depression in ALS: Lack of Worsening With Disease Progression. Nimish Thakore, Erik Pioro 4:20 p.m. S36.003 Secondary Health Conditions Among Males with Duchenne or Becker Muscular Dystrophy (DBMD) Rebecca Napoliello, Natalie Street, Kristin Caspers, Emma Ciafaloni, Christopher Cunniff, Jennifer Donnelly, Deborah Fox, Kathy James, Joyce Oleszek, Christina Westfield 4:30 p.m. S36.004 Thymectomy for Non-thymomatous Myasthenia Gravis: A Propensity Score Matched Study. Carolina Barnett Tapia, Hans Katzberg, Shaf Keshavjee, Vera Bril 4:40 p.m. S36.005 A Distinctive, Delayed Form of Exertional Rhabdomyolysis Lydia Sharp, Ronald Haller 4:50 p.m. S36.006 Neuropathy Associated with Nondiabetic Obesity J. Singleton, Eric Volckmann, Timothy Graham, Albert Smith 5:00 p.m. S36.007 Comparison of Baroreflex Sensitivity to Fall and Rise in Blood Pressure Induced by the Valsalva maneuver Naoki Wada, Wolfgang Singer, Tonette Gehrking, David Sletten, James Schmelzer, Phillip Low 5:10 p.m. S36.008 Peripheral Nerve Amyloidosis: Phenotype, Natural History, and Autonomic Dysfunction in Inherited Versus Acquired Subtypes Adam Loavenbruck, Wolfgang Singer, Paola Sandroni, Michelle Mauermann, P. James B. Dyck, Christopher Klein, Phillip Low 5:20 p.m. S36.009 Is the Rituximab Response in Acetylcholine Receptor Autoantibody Myasthenia Gravis Durable? Kimberly Robeson, Benison Keung, Daniel DiCapua, Jonathan Goldstein, Kevin O’Connor, Richard Nowak 5:30 p.m. Panel Discussion Panel Discussion 2O14 Scientific Abstract Listing and Annual Meeting Information S37 Clinical Aspects of Parkinson's Disease 4:00 p.m. S37.001 Low Diagnostic Accuracy of a Clinical Diagnosis of Early Parkinson’s Disease: Findings of the Arizona Parkinson’s Disease Consortium Charles Adler, Thomas Beach, Joseph Hentz, Holly Shill, John Caviness, Erika DriverDunckley, Marwan Sabbagh, Lucia Sue, Sandra Jacobson, Christine Belden, Brittany Dugger 4:10 p.m. S37.002 Mechanisms of Profound Myocardial Norepinephrine Depletion in Parkinson Disease David Goldstein, Patti Sullivan, Courtney Holmes, Gary Miller, Yehonatan Sharabi, Irwin Kopin 4:20 p.m. S37.003 Determining Optimal Cutoff Scores and Neuropsychological Tests for the Diagnosis of Mild Cognitive Impairment in Parkinson’s Disease Samantha Holden, Bichun Ouyang, Glenn Stebbins, Bryan Bernard, Christopher Goetz, Jennifer Goldman 4:30 p.m. S37.004 Heart Rate Variability in LRRK2 Parkinson’s Disease Samuel Goldman, Birgitt Schuele, Grace Bhudhikanok, Stephanie Cash, Monica Korell, Yamah Amiri, Chen Meng, Kathleen Comyns, Dolores Guest, Linda Rees, Sam Kim, Farah Kausar, Sakunthala Sundarrajan, Emily Drabant Conley, Nicholas Eriksson, Grace Liang, Melanie Brandabur, James Tetrud, J Langston, Caroline Tanner 4:40 p.m. S37.005 What Are the Determinants of Leaving the Workforce in Parkinson’s Disease? Melissa Armstrong, Ann Gruber-Baldini, Stephen Reich, Christian Lachner, Karen Anderson, Paul Fishman, Lisa Shulman 4:50 p.m. S37.006 α-Synuclein in Red Blood Cells Is a Potential Diagnostic Biomarker for Parkinson’s Disease Rodolfo Savica, Roy Dyer, Michelle Mielke, Bryan Klassen, Bradley Boeve, George Klee, J. Ahlskog, Walter Rocca, Marina RamirezAlvarado 5:00 p.m. S37.007 Alpha-Synuclein within Cutaneous Autonomic Nerves in Parkinson Disease: A Biomarker of Disease Severity and Autonomic Dysfunction Christopher Gibbons, Ningshan Wang, Roy Freeman 5:10 p.m. S37.008 Elevated Blood Harmane (1-methyl-9H-pyrido[3,4-b]indole) Concentrations in Parkinson’s Disease Elan Louis, Monika Michalec, Wendy Jiang, Pam FactorLitvak, Wei Zheng 5:20 p.m. S37.009 Oral Inosine Persistently Elevates Plasma Antioxidant Capacity in Early Parkinson’s Disease Shamik Bhattacharyya, Rachit Bakshi, Robert Logan, Alberto Ascherio, Eric Macklin, Michael Schwarzschild 5:30 p.m. Panel Discussion S38 Aging, Dementia, and Cognitive and Behavioral Neurology: Plasma and Other Biomarkers 4:00 p.m. S38.001 A Plasma-based Biomarker Panel Identifies Preclinical Alzheimer’s Disease Mark Mapstone, Massimo Fiandaca, Amrita Cheema, Xiaogang Zhong, Ming Tan, Claudia Kawas, Howard Federoff 4:10 p.m. S38.002 High Accuracy of a MicroarrayBased Blood Test for Alzheimer’s Disease Lucas Restrepo, Phillip Stafford, Stephen Johnston 4:20 p.m. S38.003 Presence of Phosphorylated Tau, Alpha-Synuclein and Amyloid Protein in the Skin of Patients with Clinical Diagnosis of Alzheimer Disease Ildefonso Rodriguez-Leyva, Ana Calderon-Garciduenas, Martha Santoyo, Erika Chi, Verónica MedinaMier, Maria Jimenez-Capdeville 4:30 p.m. S38.004 Increased Plasma Pyroglutamate-3 Amyloid Beta Protein Levels in Older Persons with Down Syndrome (DS) Pankaj Mehta, Bruce Patrick, Marc Barshatzky, David Miller 4:40 p.m. S38.005 Association of Plasma Aβ Levels with MRI Markers of Cerebral Small Vessel Disease Sara Kaffashian, Christophe Tzourio, Aicha Soumare, Carole Dufouil, Fabrice Crivello, Yicheng Zhu, Susanna SchraenMaschke, Bernard Mazoyer, Luc Buee, Stephanie Debette 4:50 p.m. S38.006 An Abeta Oligomer Receptor Antagonist and Antibodies to Specific Target Receptor Epitopes Displace Abeta Oligomers in Alzheimer’s Patient Brain Tissue Sections Susan Catalano, Nicholas Izzo, Courtney Rehak, Raymond Yurko, Kelsie Mozzoni, Colleen Silky, Gary Look, Gilbert Rishton, Hank Safferstein, Tara Spires-Jones 5:00 p.m. S38.007 Prevalence of Lewy-type Synucleinopathy in the Submandibular Gland of Subjects with NeuropathologicallyConfirmed Dementia with Lewy Bodies. Thomas Beach, Charles Adler, Holly Shill, Lucia Sue, Geidy Serrano, Brittany Dugger, Sandra Jacobson, Marwan Sabbagh 5:10 p.m. S38.008 Association of the MAPT with Cerebrospinal Fluid Phosphorylated Tau Levels in Frontotemporal Degeneration Nam Eun Min, Corey McMillan, David Irwin, Virginia Lee, John Trojanowski, Vivianna Van Deerlin, Murray Grossman 5:20 p.m. S38.009 Complement Factor H Is a Biomarker for Mild Cognitive Impairment Not Due to Alzheimer’s Disease Trung Nguyen, Kelly Watts, James Lah, Jonathan Glass, Allan Levey, William Hu 5:30 p.m. Panel Discussion Platform Blitzes 4:00 p.m. S39.001 Pediatric Primary Pseudotumor Cerebri Syndrome (PTCS): New Insights from Detailed Endocrine Assessments Grace Lin, Claire Sheldon, Evanette Burrows, Marianne Chilutti, Shana McCormack, Grant Liu 4:10 p.m. S39.002 White Matter Microstructure Abnormalities in Patients with Dominant Optic Atrophy and OPA1 Mutations Roberta Messina, Maria Rocca, Stefania Bianchi Marzoli, Iacopo Milesi, Maria Lucia Cascavilla, Melissa Petrolini, Andrea Falini, Giancarlo Comi, Massimo Filippi 4:20 p.m. S39.003 Baseline Optical Coherence Tomography (OCT) Measurements in the Idiopathic Intracranial Hypertension Treatment Trial: Correlations and Relationship to Clinical Features Mark Kupersmith 4:30 p.m. S39.004 Opponent Mechanisms of Cone and Melanopsin Pupil Control Geoffrey Aguirre, Manuel Spitschan, Jain Sandeep, David Brainard 4:40 p.m. S39.005 Pre-Existing Afferent Visual System Abnormalities Confound Vigabatrin (VGB) Vision Analyses of Patients with Epilepsy Robert Sergott, Rod Foroozan, Chris Johnson, Deborah Lee, Jouko Isojarvi 4:50 p.m. S39.006 MRI Findings of Elevated Intracranial Pressure in Pseudotumor Cerebri Syndrome With and Without Papilledema Robert Mallery, John Woo, Madhura Tamhankar, Kenneth Shindler, Yin Chen, Eric Medina, Kathleen Digre, Deborah Friedman, Grant Liu 5:00 p.m. S39.007 Four-Year Results from the Sabril® Registry Yield a Low Rate of Discontinuation Secondary to Reports of Visual Deficits Robert Sergott, Rod Foroozan, John Pellock, R Faught, W Shields, Greg Burkhart, Vijay Prabhakaran, Sarah Torri, Deborah Lee, Jouko Isojarvi 5:10 p.m. S39.008 Visual Pathway Structure and Function, Optic Neuritis and Fatigue in Multiple Sclerosis. Salim Chahin, Deborah Miller, Nikitha Ashok, Reiko Sakai, James Wilson, Clyde Markowitz, Dina Jacobs, Ari Green, Peter Calabresi, Elliot Frohman, Steven Galetta, Laura Balcer 5:20 p.m. S39.009 Effects of Stimulating MelanopsinContaining Retinal Ganglion Cells in Migraine Patients Using Multifocal Objective Pupillometry Christian Lueck, Eman Ali, Teddy Maddess, Corinne Carle 5:30 p.m. Panel Discussion S40 General Neurology II 4:00 p.m. S40.001 DPPX Autoantibody: Frequency, Clinical Accompaniments and Outcomes W. Oliver Tobin, Vanda Lennon, Lars Komorowski, Christian Probst, Stacey Clardy, Allen Aksamit, Claudia Lucchinetti, Sean Pittock, Maja Tippmann-Peikert, Elaine Wirrell, Andrew McKeon 4:10 p.m. S40.002 Plasma Lipids and Cerebral Small Vessel Disease Sabrina Schilling, Christophe Tzourio, Carole Dufouil, Yicheng Zhu, Claudine Berr, Annick Alpérovitch, Fabrice Crivello, Bernard Mazoyer, Stéphanie Debette 4:20 p.m. S40.003 Neurocognitive Changes in High-Altitude U-2 Pilots: Relationship to White Matter Hyperintensities Adam Willis, John Sladky, David Tate, Kent McDonald, Joe Wood, Paul Sherman, Peter Kochunov, Stephen McGuire 4:30 p.m. S40.004 Detection of Increased Transcripts of Human Endogenous Retrovirus in Plasma of Patients with Frontotemporal Dementia Associated Amyotrophic Lateral Sclerosis Tariq Alfahad, Allan Levey, Avindra Nath 4:40 p.m. S40.005 Quantification of Sciatic Nerve Pathology in Inherited Neuropathies via Magnetization Transfer MRI Richard Dortch, Lindsey Dethrage, Audra Hamilton, John Gore, Seth Smith, Jun Li 4:50 p.m. S40.006 A Single Mode of Brain Alteration in Blindness. A Multimodal MR Imaging Study. Ritobrato Datta, Noah Benson, Aleksandra Daina, Efstathios Gennatas, Sashank Prasad, Omar Butt, Geoffrey Aguirre 5:00 p.m. S40.007 Subcortical White Matter Hyperintensities on MRI in Two Populations Exposed to Hypobaric Non-Hypoxic Conditions Andrew Robinson, Patrick Grogan, Peter Kochunov, Paul Sherman, Stephen McGuire 5:10 p.m. S40.008 Ascending Paralysis from Rabies 17 Months Following Kidney Transplant Sean Rogers, Mary Denny, Rebecca O’Dwyer Vourganti, Ramsey A. Falconer, Ping Zhai, Friedhelm Sandbrink 5:20 p.m. S40.009 The Effects of Combination Therapy with Sodium Valproate, Peg-alpha Interferon and Prednisolone on Clinical Manifestations of Patients With HTLV-1 Associated Spastic Paraparesis (HAM/TSP) Ali Shoeybi, Reza Boostani, Mohammad Mehdi Etemadi, Seyed Abdolrahim Rezaee, Mehdi Moshfegh 5:30 p.m. Panel Discussion S41 Headache: Clinical 4:00 p.m. S41.001 Combined Concordant Peripheral Neurostimulation for Chronic Migraine Headaches: A Retrospective Analysis of 188 Consecutive Patients Kenneth Reed, Francis Conidi, Robert Bulger, Kelly Will 4:10 p.m. S41.002 Sociodemographic, Disability, and Employment Differences Between Persons with Chronic and Episodic Migraine: Results of the CaMEO (Chronic Migraine Epidemiology and Outcomes) Study Richard Lipton, Daniel Serrano, Dawn Buse, Kristina Fanning, Aubrey Manack, Michael Reed 4:20 p.m. S41.003 Symptom Codes and Opioids: Disconcerting Headache Practice Patterns in Academic Primary Care. K.C. Brennan, Colin Farrell, Gregory Keough, Susan Baggaley, Karly Pippitt, Susan Pohl, Kathleen Digre, Lisa Gren 4:30 p.m. S41.004 Long-term Efficacy of Outpatient Interdisciplinary Treatment for Patients Suffering from Chronic Headaches Mark Stillman, Steven Krause 4:40 p.m. S41.005 Influence of Psychiatric Comorbidities in Migraineurs in the Emergency Department: A Cross Sectional Analysis Mia Minen, Kaloyan Tanev 4:50 p.m. S41.006 Headache Characteristics at Baseline in the Idiopathic Intracranial Hypertension Treatment Trial Deborah Friedman 5:00 p.m. S41.007 Association Between Stress and Headache Frequency Sara Schramm, Susanne Moebus, Nils Lehmann, Ursula Galli, Mark Obermann, Eva Bock, Min-Suk Yoon, H. Diener, Zaza Katsarava 5:10 p.m. S41.008 A Case Report of Acute Intracerebral Vascular Ischemic Stroke After Treatment with Dihydroergotamine in a Patient with New Onset of Migraine New Daily Persistent Headache with Thunderclap Onset Sana Ghafoor, William Young 5:20 p.m. S41.009 Adherence to Oral Migraine Preventive Medications Among Patients with Chronic Migraine: Analysis of a Large US Health Insurance Claims Database Zsolt Hepp, David Dodick, Sepideh Varon, Patrick Gillard, Ryan Hansen, Emily Devine 5:30 p.m. Panel Discussion S42 Child Neurology I 4:00 p.m. S42.001 A Novel Homozygous Mutation of SLC52A3 Gene Associated with Brown-Vialetto-Van Laere Syndrome (BVVL) Sunil Naik, Eisha Chopra, Beth Pletcher, Chirag Gordhan, Xue Ming 4:10 p.m. S42.002 Abnormalities of the Attentional Network Following Traumatic Brain Injury in Pediatric Patients: A fMRI Study Maria Rocca, Sandra Strazzer, Paola Valsasina, Ermelinda De Meo, Erika Molteni, Monica Recla, Susanna Galbiati, Alessandra Bardoni, Giancarlo Comi, Massimo Filippi 4:20 p.m. S42.003 Hypertension Is Associated with Increased Mortality After Ischemic Stroke in Children Alfredo Caceres, Malik Adil, Adnan Qureshi, Lori Jordan 4:30 p.m. S42.004 Neuronal Activity Promotes Oligodendrogliogenesis and Myelination in the Mammalian Brain David Purger, Erin Gibson, Christopher Mount, Andrea Goldstein, Grant Lin, Ingrid Inema, Sarah Miller, Gregor Bieri, J. Bradley Zuchero, Ben Barres, Pamelyn Woo, Hannes Vogel, Michelle Monje 4:40 p.m. S42.005 Identification of New Genes and Pathways for Undiagnosed Infantile Spinal Muscular Atrophy Disorders. Lisa Baumbach-Reardon, Jesse Hunter, Mary Ellen Ahearn, Judith Hall, John Carpten 4:50 p.m. S42.006 Functional Outcome After Perinatal Cerebral Sinovenous Thrombosis: A Prospective Cohort Study Lori Billinghurst, Michael Uohara, Daniel Licht, Rebecca Ichord 5:00 p.m. S42.007 Everolimus Long-Term Efficacy and Safety for the Treatment of Subependymal Giant Cell Astrocytoma (SEGA) Associated With Tuberous Sclerosis Complex (TSC) David Franz, Elena Belousova, Steven Sparagana, E Bebin, Michael Frost, Rachel Kuperman, Olaf Witt, Michael Kohrman, J. Robert Flamini, Joyce Wu, Paolo Curatolo, Petrus de Vries, Noah Berkowitz, Oezlem Anak, Julie Niolat, Sergiusz Jozwiak 5:10 p.m. S42.008 Cognitive and Developmental Predictors of ASD in Infants with Tuberous Sclerosis Complex. Shafali Jeste, Joyce Wu, Damla Senturak, Mustafa Sahin, Charles Nelson 5:20 p.m. S42.009 Memantine for the Treatment of Autism Spectrum Disorder: Overview of the Phase II Clinical Development Program Ephraim Katz, Jordan Lateiner, Allan Spera, Robert Palmer, Stephen Graham 5:30 p.m. Panel Discussion S43 Epilepsy and Clinical Neurophysiology (EEG): Cognition 4:00 p.m. S43.001 A Pilot Study of a Self-Management Intervention for Cognitive Impairment in Epilepsy Tracie Caller, Karen Secore, Robert Ferguson, Robert Roth, Faith Alexandre, Jessica Harrington, Barbara Jobst 4:10 p.m. S43.002 Cognitive Effects of Extended-release Once-daily SPN-538 (Trokendi XR™) Versus b.i.d. Immediate-Release Topiramate (TPM-IR, Topamax®) in Healthy Volunteers Janet Johnson, Scott Brittain, Stefan Schwabe 4:20 p.m. S43.003 Stereotactic Laser Ablation of Hippocampus Leads to Better Cognitive Outcome Than Open Temporal Lobe Resections for the Treatment of Epilepsy Daniel Drane, David Loring, Voets Natalie, Price Michele, Jon Willie, Sandra Helmers, Jeffrey Ojemann, Vaishali Phatak, John Miller, Kimford Meador, Robert Gross 4:30 p.m. S43.004 Virtual Car Accident Rates of Epilepsy Patients Are Significantly Increased by Interictal Generalized Spike Waves Heinz Krestel, Andreas von Allmen, Christian Liechti, Maja Steinlin, Johannes Mathis, Nirkko Arto 4:40 p.m. S43.005 Mismatch of Structural and Functional Reorganization in Language Network in Left Temporal Lobe Epilepsy Shigetoshi Takaya, Naoaki Tanaka, Hesheng Liu, Douglas Greve, Claus Reinsberger, Andrew Cole, Emad Eskandar, Steven Stufflebeam 4:50 p.m. S43.006 Efficacy of Transcranial Direct Current Stimulation on Working Memory and Mood in Patients with Temporal Lobe Epilepsy Anli Liu, Orrin Devinsky, Andrew Bryant, Ashlie Jefferson, Daniel Friedman, Mouhsin Shafi, William Barr, Daniel Press, Susan Herman, Margaret O’Connor, Steven Schachter, Alvaro Pascual-Leone 5:00 p.m. S43.007 Seizures Lower the Pathologic Threshold for the Development of Mild Cognitive Impairment and Early Dementia in Alzheimer’s Disease Ryan Patrick, Erin Abner, Peter Nelson, Gregory Jicha 5:10 p.m. S43.008 Key Pathways for Visual Naming and Object Recognition Revealed by Diffusion Tensor Imaging Probabilistic Tractography in Epilepsy Surgery Patients Daniel Drane, Matthew Glasser, Natalie Voets, Jeffrey Ojemann, Amit Saindane, David Loring, Michele Price, Mirjana Ivanisevic, Vaishali Phatak, Jon Willie, Kimford Meador, John Miller, Robert Gross 5:20 p.m. S43.009 Facial Emotion Processing in Left Temporal Lobe Epilepsy Jane Allendorfer, Heidi Heyse, Lucy Mendoza, Basia Szaflarski, Nancy Cohen, Jerzy Szaflarski 5:30 p.m. Panel Discussion Fast, Easy Registration Online · AAN.com/view/AM14 103 Wednesday April 30 S39 Neuro-ophthalmology/ Neuro-otology II Thursday, May 1 P6 Poster Session VI First Authors stand by Posters from 7:30 a.m.–9:00 a.m. 7:30 a.m.–11:00 a.m. Poster Discussion Session: General Neurology V Utilizing a guided tour format, topic experts will lead attendees around the ten posters in the poster discussion session and facilitate questions with poster authors during the 90-minute author stand-by time. P6.001 Analyses of Neural Autoantibodies by a Clinical Laboratory for the Evaluation of Paraneoplastic and NonParaneoplastic Neuronal Disorders Valerie Brachet, Malgorzata Jaremko, Brian Sansoucy, Sat Dev Batish, Keith Morneau, Zhenyuan Wang, Michael Levy, Kaylan Burnham, Joseph Higgins P6.002 Cross-cultural Comparison of Stigma Toward Mental and Neurological Disorders Laila Gharzai, Jennifer Harney, Suzanne Higgins, Robin High, Liyan Xu, Ashley Reynolds, Douglas Inciarte, Diego Torres-Russotto P6.003 Efficacy of Dalfampridine in Hereditary Spastic Paraplegia: a Prospective Open Study Nicolas Collongues, Matthieu Bereau, Jean Baptiste Chanson, Gregory Tio, Yon Andoni Echaniz Laguna, Christel Depienne, Mathieu Anheim, Jerome De Seze P6.004 Multidisciplinary Management of Cerebral Edema Associated with Fulminant Hepatic Encephalopathy in a Neurosciences Intensive Care Unit Panayiotis Varelas, Riad Ramadan, Chandan Mehta, Marlissa Hawley, Tamer Abdelhak, Mohammed Rehman P6.005WITHDRAWN P6.006 Discharge Delays on an Inpatient Neurology Service Ayush Batra, Joel Salinas, Adam Cohen P6.007 Taking Neurology to the Underserved—a Pilot Initiative in an Urban Homebound Program Ritesh Ramdhani, Michelle Fabian, Ania Wajnberg, Linda DeCherrie, Stephen Krieger P6.008 Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) Sera Alter Regulators of Schwann Cell Differentiation Abhijeet Joshi, Ilja Bobylev, Christian Ritter, Andre Heinen, Helmar Lehmann P6.009 Methotrexate Induced Cerebellar Leukoencephalopathy Christopher Goshgarian, Abdulrahman Alwaki, Anibal Lugo, Kavita Grover P6.010 Subclinical Primary Sjögren’s Syndrome and Associated Peripheral Neuropathy: Optimizing Diagnostic Approach. Etienne Laverse, Amal Samaraweera, Wan Fai Ng, James Miller NEW! e Poster Session: Child Neurology V The ePoster session will feature a selection of posters to be presented digitally, rather than in the traditional format. Authors will be able to take advantage of the format to highlight compelling visual features such as images and videos. See poster map on page 47 for location. P6.011 Recurrent Stroke-like Events Preceding the X-linked Charcot-MarieTooth Disease Diagnosis Tara Kimbason, Arayamparambil Anilkumar, Oleg Bronov P6.012 Abnormal White Matter Connectivity in Children with Autism or Sensory Processing Disorder: Overlap and Divergence. Elysa Marco, YiShin Chang, Julia Owen, Shivani Desai, Julia Harris, Susanna Hill, Anne Arnette, Pratik Mukherjee P6.013 An Abbreviated Exposure to Chronic Hypoxia Is Sufficient to Induce CNS Hypomyelination and Impair Motor Development in Neonatal Mice Jens Watzlawik, Meghan Painter, Louisa Papke, Robert Kahoud, William Carey, Moses Rodriguez P6.014Infraslow Electroencephalography Changes in Infantile Spasms Ken Myers, Luis BelloEspinosa, Morris Scantlebury P6.015 Anti NMDA Receptor Encephalitis (ANMDARE): Outcome in a Cohort of 13 Children Jay Selman General Neurology VI P6.021 Postural Orthostatic Tachycardia Syndrome (POTS) and its associated symptoms Anindita Deb, Karen Morgenshtern, Anna Hohler P6.022 Neurological Sequelae of Varicella Zoster Virus Infection ( VZV): Case Series of Varied Presentations Shamaehah Javed, Maheep Singh, Stephen Marks, Ramandeep Sahni, Brij Ahluwalia-Singh P6.023 Hashimoto’s Encephalopathy Complicated by Cerebellar Ataxia: A Case Report Michael Hossack, Perry Richardson P6.024 Unusual Presentation of Acute Carbon Monoxide Poisoning Shivnaveen Bains, Derrece Reid, Xuemei Huang 104 P6.025 Dabigatran—the Future of Cortical Venous Thrombosis Therapy—a Case Series Study Thomas Mathew, Lobo Alexander, Gosala Sarma, Raghunandan Nadig P6.026 Intrathecal Baclofen Toxicity Mimicking Nonconvulsive Status Epilepticus Glynnis Zieman, Richard Burns P6.027 Case Report: Uncommon Presentation of Neurosarcoidosis Ikjae Lee, Pooja Khatri, Ady Kendler, Jennifer Molano P6.028 Central Pontine and Extrapontine Myelinolysis: Risk Factors and Clinical Expression in Liver Transplanted Patients Silvia Favaretto, Annachiara Cagnin, Cristina Crivellin, Patrizia Boccagni, Umberto Cillo, Patrizia Burra, Marco Senzolo P6.016 Novel Mechanism for Monitoring Cerebral Hemodynamics in Pediatric ECMO David Busch, Ann McCarthey, Jennifer Lynch, Erin Buckley, James Connelly, Maryam Naim, Daniel Licht P6.017 Stiff Person Syndrome in Childhood: SPS-C Recognition and Review Bennett Lavenstein, Sarah Evans, Olga Morozova P6.018 A Rare Case of Microcephaly-Capillary Malformation Syndrome Diagnosed via Whole Exome Sequencing Nassim Zecavati, Reem Saadeh-Haddad, Cesar Santos, Chahira Kozma P6.029 Unusual Case of Delayed Postpartum Preeclampsia Associated with Reversible Splenial Lesion Syndrome Pedro Oliveira, Osama Zaidat P6.030 Hypercholesterolemia and Neurological Diseases Related Mortality in the NEDICES Cohort Fernando SierraHidalgo, Alvaro Sanchez-Ferro, Rocio Trincado, Jaime Díaz Guzmán, Jesús Hernández Gallego, Julian Benito-Leon, Saturio Vega, Felix Bermejo-Pareja P6.031 Atypical Presentation of Posterior Reversible Encephalopathy Syndrome Annapoorna Bhat, Machteld Hillen P6.032 Neurological Disorders In Rosai-Dorfman Disease Coralie Casulli, Nathalie Caucheteux, Agnes Fromont, Caroline Antoniol, Ayman Tourbah, Thibault Moreau 2O14 Scientific Abstract Listing and Annual Meeting Information P6.019 Does Duration of Steroid Treatment Matter in Pdiatric Optic Neuritis? Himali Jayakody, Daniel Bonthius, Reid Longmuir, Charuta Joshi P6.020 Functional Neurological Disorder in the Pediatric Emergency Room: Characteristics, Outcome and Diagnostic Accuracy Claudio De Gusmao, Rejean Guerriero, Miya Bernson-Leung, Danielle Pier, Patricia Ibeziako, Simona Bujoreanu, Kiran Maski, David Urion, Jeffrey Waugh P6.033 Olfactory Function of the Patients with Psoriasis Ercan Karabacak, Hakan Tekeli, Aytuğ Altundağ, Ersin Aydin, Mustafa Kendirli, Murat Salihoglu, Melih Çayonu, Halit Yasar P6.034 The Need for Repeat Diagnostic Testing for the Identification of Ovarian Pathology in a Patient with antiNMDA Receptor Limbic Encephalitis Mona Bahouth, Carlos Pardo-Villamizar, Michael Johnston P6.035 Quality Improvement: Maintaining an Accurate Medication List by Standardizing the Outpatient Medication Reconciliation Method Christina Nguyen, Zhi-Jian Chen Poster Session VI Guillain-Barre in a Small Illinois Community: An Epidemiology Perspective Valerie Arias, Benjamin Claytor, Anand Oroskar, Mujtaba Akhter, Jorge Kattah P6.037 The Epidemiology of Neuromyelitis Optica at a City Hospital in the Bronx, New York Sylvia Mohen, Lenore Ocava P6.038 Symptomatic Vitamin D Deficiency in Dubai Stephanie Ybanez, Tania Tayah P6.039 Hyperkalemic Periodic Paralysis Masquerading as Sleep Paralysis Yelena Gorfinkel Pyatkevich P6.040 POEMS Syndrome Associated with Autoimmune Limbic Encephalitis, an Unusual Occurrence Niraj Arora, Rohini Bhole, Enrique Aradillas P6.041 Neuroscience Education in the Medical College: The Qatar Experience Leopold Streletz, Naim Haddad, Ziad Kronfol, Joseph Safdieh, Basim Uthman P6.042 Posterior Reversible Encephalopathy Syndrome and GuillainBarre Syndrome in a Pregnant Lady: A Case Report from a Tertiary Teaching Hospital of South India Dhairyawan Pokalkar, Veena Narisetty, Sateesh Kamera, Sowjanya Poosarla, Srilatha Siripuram Movement Disorders: Spinocerebellar Ataxias P6.043 Spinal Cord Damage in Machado-Joseph Disease Camila Fahl, Lucas Branco, Felipe Bergo, Iscia LopesCendes, Marcondes Franca, Jr. P6.044 The Evaluation of Swallowing in Patients with Spinocerebellar Ataxia and Oropharyngeal Dysphagia: A Comparison Study of Videofluoroscopic and Sonar Doppler Edna Marcia Abdulmassih, Helio Teive, Rosane Sampaio Santos, Bianca Simone Zeigelboim P6.045 Polysomnographic Findings in Machado-Joseph Disease: Evaluation of 47 Patients José Luiz Pedroso, Diogo Santos, Gilmar Prado, Lucila Prado, Luciane Carvalho, Pedro Braga-Neto, Orlando Barsottini P6.046 De Novo Deletion of AFG3L2 Causing Spinocerebellar Ataxia Type 28 in the Context of Multiple Genomic Anomalies Ken Myers, Jodi Chardon, Kym Boycott P6.047 Coenzyme Q10, Statin, and Spinocerebellar Ataxias Sheng-Han Kuo, Raymond Lo, Karla Figueroa, Stefan Pulst, Susan Perlman, George Wilmot, Christopher Gomez, Jeremy Schmahmann, Henry Paulson, Vikram Shakkottai, Sarah Ying, Theresa Zesiewicz, Khalaf Bushara, Michael Geschwind, Guangbin Xia, S Subramony, Tetsuo Ashizawa P6.048 Audiological Evaluation in Spinocerebelar Ataxia Hélio Teive, Bianca Zeigelboim, Walter Arruda, Ari Jurkiewicz, Denise França, Jair Marques, Hugo Carvalho, Edna Marcia Abdulmassih P6.049 Wide Spectrum of Clinical Presentation of Spinocerebellar Ataxia Type 2 Shilpa Kolli, Anna Sorokin, Duarte Machado P6.050 Widespread Cerebral Cortical Damage in Machado-Joseph Disease Thiago Rezende, Anelyssa D’Abreu, Rachel Guimarães, Iscia LopesCendes, Tátila Lopes, Gabriela Castellano, Marcondes Franca, Jr. P6.051 Dystonia in Machado-Joseph Disease: Clinical Features and Levodopa Response Marcelo Nunes, Alberto Martinez, Iscia Lopes-Cendes, Anelyssa D’Abreu, Marcondes Franca, Jr. P6.052 Treatment of Spinocerebellar Ataxia with Intravenous Immune Globulin (IVIG) Theresa Zesiewicz, Tuan Vu, Kelly Sullivan, Clifton Gooch, Israt Jahan, Christopher Ward, Seok Kim Movement Disorders: Miscellaneous Ataxias P6.053 Paroxysmal Dysarthria and Ataxia After Treatment of Brainstem Encephalitis James Klaas, Christopher Boes, Allen Aksamit P6.054 Sporadic Cerebellar GADAtaxia: A Retrospective Analysis Pezhman Roohani, Adam Rizvi, Sara Mayer, Khalaf Bushara P6.055 Elevated Thyroid Antibody Associated Sporadic Cerebellar Ataxia: A Retrospective Analysis Pezhman Roohani, Jamie Starks, Nik Haliza Nik Hassan, Khalaf Bushara P6.056 Autoimmune Cerebellar Degeneration with Voltage Gated Calcium Channel Antibodies: A Case Report and Study of Antibody Reactivity Marilyn McKasson, Stacey Clardy, Mark Bromberg, Noel Carlson, John Greenlee P6.057 Cerebellar Ataxia with CoQ10 deficiency Due to a Novel Mutation in ADCK3 Emanuele Barca, Olimpia Musumeci, Lorenzo Peverelli, Anna Ciranni, Salvatore DiMauro, Michio Hirano, Catarina Maria Quinzii, Antonio Toscano P6.058 A Novel Spinocerebellar Ataxia with Hematologic Cytopenias: Linkage Analysis and Exome Sequencing Identifies a Candidate Gene Dong-Hui Chen, Piper Below, Youngmee Sul, Mark Matsushita, John Wolff, Emily Bonkowski, Wendy Raskind, Thomas Bird P6.059 iPatax: A New Method for Quantitative Assessment for Motor Coordination of Ataxia Masayoshi Tada, Jun Tokunaga, Takahiro Nagai, Masatoyo Nishizawa, Osamu Onodera P6.060 Mutations in PNPLA6 Cause a Range of Neurodegenerative Phenotypes Stephan Zuchner, Matthis Synofzik, Marie Coutelier, Charles Marques Lourenço, Tobias Haack, Rebecca Schüle, Wilson Marques Junior, Ludger Schols, Giovanni Stevanin P6.061 Spinocerebellar Ataxias with Hypogonadism: Unraveling a Novel Group of Inherited Neurometabolic Disorders Charles Lourenco, Claudia Sobreira, Roberto Giugliani, Stephan Zuchner, Wilson Marques, Jr. P6.062 The Use of Adjustments to Facilitate the Written in Patients Diagnosed with Spinocerebellar Ataxia Thais Canelossi Rosa, Renato Nickel, Paulo Liberalesso, Helio Teive Movement Disorders: Parkinson’s Disease Imaging P6.063 Cognitive Associations of White Matter Hyperintensities in NonDemented Parkinson’s Disease Patients: A Voxel-Wise Lesion Probability Study Elijah Mak, Michael Dwyer, Deepa Ramasamy, Wing Au, Louis Tan, Robert Zivadinov, Nagaendran Kandiah P6.064 A Longitudinal (11C)(±) Dihydrotetrabenazine PET Study of Gender Difference in the Progression of Dopaminergic Dysfunction in the Parkinsonian Caudate Nandhagopal Ramachandiran, Michael Schulzer, Lisa Kuramoto, Jacquelyn Cragg, Vesna Sossi, Raúl de la Fuente-Fernández, A Stoessl P6.065 Hyperechogenicity of Substantia Nigra: A Potential Disease Progression Marker in Early Onset Parkinson’s Disease (EOPD) Balaji Krishnaiah, Kala Venkiteswaran, Vikram Shivkumar, Timothy Gilmour, Nitish Harid, Robert Saadi, Thyagarajan Subramanian P6.066 Mapping Track Density Changes in Nigrostriatal and Extranigral Pathways in Parkinson’s Disease Gaëtan Garraux, Erik Ziegler, Maud Rouillard, Elodie André, Tim Coolen, Johan Stender, Evelyne Balteau, Christophe Phillips P6.067 Subcortical Atrophy Is Associated with Cognitive Impairment in Mild Parkinson’s Disease: A Combined Volumetric and Vertex-Based Shape Analysis Study Elijah Mak, Niels Bergsland, Robert Zivadinov, Kandiah Nagaendran P6.068 Cerebellar Atrophy in Patients with Parkinson´s Disease Using the SUIT Tool for Voxel-Based Morphometry Camila Piccinin, Maria Cristina Santos, Luiza Piovesana, Rachel Guimaraes, Brunno Campos, Lidiane Campos, Paula Azevedo, Fabio Torres, Marcondes Franca Jr, Augusto Amato-Filho, Iscia Lopes-Cendes, Fernando Cendes, Anelyssa D’Abreu P6.069 Quantitative MRI Biomarker Study in Parkinson’s Disease: High-field 1H-MR Spectroscopic and Multi-Modal MRI Longitudinal Study of the Substantia Nigra Navid Seraji-Bozorgzad, Fen Bao, Natalya Shneyder, Edwin George, Carla Santiago Martinez, Veronica Gorden, Shana Krstevska, Christina Caon, Omar Khan P6.070 Accuracy and Diagnosis Cutoff Points of 123I-metaiodobenzylguanidine Myocardial Scintigraphy for Lewy Body Disease Diagnoses in Parkinsonian Syndromes: A Study of 62 Consecutive Patients in an Expert Center. Guillaume Lamotte, Adrien Lebasnier, Denis Agostini, Gilles Defer P6.071 Multi-Modal High-Field MRI Longitudinal Study of the Deep Gray Matter, Frontal Lobe, and Corpus Callosum in Parkinson’s Disease. Raeesa Khan, Fen Bao, Natalya Shneyder, Navid SerajiBozorgzad, Krishna Thakore, Carla Santiago Martinez, Veronica Gorden, Edwin George, Shana Krstevska, Omar Khan P6.072 Therapeutic Occupany of the Dopamine Receptor Agonist Pramipexol in Parkinson´s Disease (18F-Fallypride PET study) Angela Deutschlaender, Christian La Fougere, Guoming Xiong, Kai Bötzel, Paul Cumming Movement Disorders: Deep Brain and Other Stimulation/Imaging and Other Biomarkers P6.073 Stimulating Frontostriatal Circuitry to Treat Motor and Non-Motor Symptoms of Parkinson’s Disease Nolan Williams, Baron Short, Alexandra Jeffery, Emily Williams, Colleen Hanlon, Gregory Sahlem, Jeffery Korte, Gonzalo Revuelta, Mark George P6.074 Tinnitus After Deep Brain Stimulation Surgery, a Case Series Umer Akbar, Geoffrey Panjeton, Patrick Antonelli, Pam Zeilman, Takashi Morishita, Michael Okun P6.075 Clinical Manifestations of Tolerance to Deep Brain Stimulation Deepal Shah, Joohi Jimenez Shahed P6.076 Use of Interleaving in Deep Brain Stimulator Programming in Patients with Movement Disorders Joohi Jimenez Shahed, Olga Waln P6.077 Clinical Significance of Abnormal Electrode Impedance Readings in Deep Brain Stimulation for Treatment of Movement Disorders Olga Waln, Joohi Jimenez Shahed P6.078 A Case of Dystonic Head Tremor Treated with Bilateral Globus Pallidus Pars Interna Deep Brain Stimulation Joanna O’Leary, M Brodsky P6.079 Parkinson’s Disease Is Associated with Enhanced Pain-Related Disability and the Selective Loss of Gray Matter in Subcortical Regions of the Brain Related to Pain Processing Andrew Ahn, Jared Tanner, Ann Horgas, Michael Okun, Catherine Price P6.080 Effect of Laterality in Parkinson`s Disease: A Voxel-based Morphometry Study Maria Cristina Arci Santos, Lidiane Campos, Rachel Guimaraes, Camila Piccinin, Paula Azevedo, Luiza Piovesana, Brunno Campos, Augusto Amato-Filho, Fernando Cendes, Anelyssa D’Abreu Fast, Easy Registration Online · AAN.com/view/AM14 105 Thursday May 1 P6.036 Thursday, May 1 P6.081(18F)FDG PET, (18F)FP-CIT PET and MR Morphometry in Lewy Body Dementia: Comparison with Alzheimer Disease Hyunjin Kim, Seok Min Kim, Hyuk Jin Yun, Sujeong Kim, Doris Doudet, JongMin Lee, Chong S. Lee P6.082 Delivery of GDNF to the Brain by Novel Nanovesicles for the Treatment of Parkinson’s Disease Eliahu Heldman, Sarina Grinberg, Charles Linder, Mary Popov, Irwin Hollander Neuropathy: Imaging and Biomarkers P6.083 High Resolution Ultrasound in Combat-Related Peripheral Nerve Injuries: A Case Series Jonathan Smith, Matthew Miller, Craig Carroll, Walter Faillace, Leon Nesti, Christina Cawley, Mark Landau P6.084 Accuracy of Ultrasound for Diagnosis of Carpal Tunnel Syndrome in Patients with Bifid Median Nerve Jonathan Beary, Seby John, Youran Fan, Steven Shook P6.085 Distinctive Patterns of Sonographic Nerve Enlargement in Charcot-Marie-Tooth type 1A and Hereditary Neuropathy with Pressure Palsies. Stephan Goedee, Geert Brekelmans, Leonard Van den Berg, Leendert Visser P6.086 Peripheral Nerve Ultrasound in Small Fiber Neuropathy Hamid Ebadi, Hans Katzberg, Mylan Ngo, Vera Bril P6.087 Neuromuscular Ultrasound Findings in Eosinophilic Fasciitis Sarah Stone, Lisa Hobson-Webb, Justin Mhoon, Amanda Guidon, Carolina De Jesus-Acosta, Michael Cartwright P6.088 The Value of Including Sweat Gland Nerve Fiber Density (SGNFD) Analysis in the Neuropathy Workup Amiram Katz, Janet Berkley P6.08999mTc-DPD Cardiac Scintigraphy in Familiar Amyloidosis Suzane Ferreira, Caroline Amaral, Osvaldo Nascimento, Claudio Tinoco, Ribeiro Sandra, Victor Kosac, Frederico Prado P6.090 Blood Pressure Dipping During the Deep Breathing Maneuver (BPDB) While Supine May be a Marker of Severe Sympathetic Denervation Alexandru Barboi, Vivialyn Cadell P6.091 Increased Frequency of Rhabdomyolysis in Familial Dysautonomia Jose-Alberto Palma, Lucy Norcliffe-Kaufmann, Felicia Axelrod, Horacio Kaufmann P6.092 Subacute Onset of Severe CIDP Weakness Associated with Tumorlike Nerve Root Involvement: A Case Report Sharon Stoll, Goran Rakocevic Neuromuscular Disease P6.093 Peripheral Neuropathy (PN) in Individuals with Neurofibromatosis Type 1 (NF1) and Plexiform Neurofibromas (PNF) Tanya Lehky, Justin Kwan, Eva Dombi, Andrea Baldwin, Srivandana Akshintala, Andy Gillespie, Brigitte Widemann P6.094 Evaluation of Central and Peripheral Neuropathy in Type 2 Diabetes: A Case-Control Study Prasanna Venkatesan Eswaradass, Ramadoss Kalidoss P6.095 Idiopathic Peripheral Neuropathy and Subsequent Development of Diabetes Mellitus Ritika Mahajan, Molly King P6.096 Opioid Usage in Peripheral Neuropathy: A Population-Based Study E. Matthew Hoffman, Nathan Staff, Christopher Klein P6.097 Reference Attributes of Nerve Conduction and Ethnicity: Comparison in Northern Plain Indians, Mexican Americans and Caucasians Rajat Lahoria, William Litchy, P. James B. Dyck, Jenny Davies, Rickey Carter, Peter Dyck P6.098 A Population-Based Epidemiologic Study of Adult Neuromuscular Disease in the Republic of Ireland Stela Lefter, Orla Hardiman, Aisling Ryan P6.099 Trends in Outcome and Cost of Hospitalization of Elderly Myasthenia Gravis Patients Treated with Plasmapheresis from 1992 to 2009 Sedeek Elmoursi, Mohammad El-Ghanem, Ankit Pahwa, Wenzhuan He, Nizar Souayah P6.100 Emerging Epidemiological Trends of Autoimmune Myasthenia Gravis in Connecticut Matthew Imperioli, Agnes Acsadi P6.101 Fainting in Teenagers Is not Always Faking Sreenivas Avula, Manikum Moodley P6.102 CNS Toxoplasmosis: A Serious Complication of Immunotherapy in the Neuromuscular Patient Dan Bernardo, Nizar Chahin P6.103 Fingolimod (FTY720) Oral for the Treatment of Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP): Study Design of the Phase 3 FORCIDP Trial Hans Hartung, Gen Sobue, Marinos Dalakas, Norman Latov, Jean-Marc Leger, Ingemar Merkies, Eduardo NobileOrazio, Katherine Agoropoulou, Dieter Häring, Lixin Zhang-Auberson, Philipp Von Rosenstiel, Richard Hughes P6.104 Characteristics of Muscle Cramps in Patients with Polyneuropathy Hans Katzberg, Sarah Maxwell, Seint Kokokyi, Hamid Ebadi, Ari Breiner, Vera Bril P6.105 Electrodiagnostic Profile of Demyelination in Diabetic Neuropathy: A novel approach Zubeda Sheikh, Ankit Pahwa, Hongxin Chen, Nizar Souayah 106 7:30 a.m.–11:00 a.m. P6.106 West Nile Virus Encephalomyelityis Simulating Brain Death Channaiah Srikanth-Mysore, John Bertoni, Pariwat Thaisetthawatkul, Matthew White, Jose Americo Fernandes-Filho P6.107 Zoster Associated Limb Paresis (ZALP) Is Associated with Prolonged Weakness and Pain: A Natural History Study Alex Nelson, James Watson, Haatem Reda, Lyell Jones P6.108 Branching Enzyme Deficiency: Expanding the Clinical Spectrum Carmen Paradas, Orhan H. Akman, Carolina Ionete, Heather Lau, Peter Riskind, David Jones, Thomas Smith, Michio Hirano, Salvatore DiMauro P6.109 Oxidative Metabolism During Forearm Exercise in McArdle Disease Ronald Haller, Lydia Sharp, Lauren Phillips, Marta Newby, Phil Wyrick, Katja Heinicke P6.110 The Pattern of Pain in Carpal Tunnel Syndrome Follows a Bell-shaped Curve Benn Smith, Mark Ross, Brent Goodman, Greg Thaera, Jonathan McKinnon P6.111 When Expected Turns Unexpected: A Case of Subacute Progressive Weakness and Paresthesias of the Distal Lower Extremities Following a Brief Diarrheal Episode. Divpreet Kaur, Yadira Velazquez-Rodriguez, Aiesha Ahmed MS and CNS Inflammatory Disease: Neuroimaging P6.112 Clinical Impact of Brain Tissue Damage Quantified by Fully Automated Analysis of MR Images in Patients with Multiple Sclerosis Alaleh Raji, Gerhard Winkler, Lothar Spies, Anja Tewes, Roland Opfer P6.113 Sub-optimal Response to Therapy in Disease-free MS Patients: A Paradox? Fernando Figueira, Gustavo Figueira, Paula Soares P6.114 Longitudinal Effects of Interferon-beta-1a Treatment on Cortical Thickness in Relapsing-Remitting Multiple Sclerosis Patients Anat Achiron, Chen Hoffmann, Yael Nissan, Shmuel Miron P6.115 Associations Between Changes in Ferritin Levels and Susceptibility-Weighted Imaging Filtered Phase in Patients with Relapsing-Remitting Multiple Sclerosis over Six Months Therapy with Interferon Beta-1a Michael Dwyer, Robert Zivadinov, Silva Markovic-Plese, Niels Bergsland, Mari Heininen-Brown, Ellen Carl, Cheryl Kennedy, Bianca Weinstock-Guttman, Brooke Hayward, Fernando Dangond P6.116 Evolution of Corpus Callosum Index in Patients with Relapsing Remiting Multiple Sclerosis Treated with Natalizumab Eva Costa Arpin, Tania Garcia Sobrino, Clara Dominguez Vivero, M. C. Amigo, Jose Prieto, Ana Rodriguez Regal, Manuela Lema Bouzas 2O14 Scientific Abstract Listing and Annual Meeting Information P6.117 Corpus Callosum Volume Change in the First Year Is the Strongest Predictor of 9-year Clinical Disability in Multiple Sclerosis Dana Horakova, Tomas Kalincik, Jan Krasensky, Manuela Vaneckova, Zdenek Seidl, Eva Havrdova P6.118 A New Composite Scale of MRI-defined Disease Severity in Multiple Sclerosis Mohit Neema, Antonia Ceccarelli, Brian Healy, Bonnie Glanz, Shahamat Tauhid, Gloria Kim, Jennifer Miller, Rohit Bakshi P6.119 Fully Automated Detection and Quantification of T1 Hypointense Lesions in Multiple Sclerosis Alaleh Raji, Gerhard Winkler, Lothar Spies, Anja Tewes, Roland Opfer P6.120 Cerebellar and Brain Gray-Matter Damage Predicts Fatigue in Multiple Sclerosis Alfredo Damasceno, Benito Damasceno, Fernando Cendes P6.121 Abnormal White Matter Fraction Predicts Cognitive Dysfunction in Multiple Sclerosis Patients Manuela de Stefano, Francesco Patti, Luigi Lavorgna, Patrizia Montella, Silvia Messina, Chisari Clara Grazia, Domenico Ippolito, Roberta Lanzillo, Giuseppe Salemi, Paola Valentino, Gabriella Coniglio, Maria Buccafusca, Damiano Paolicelli, D’Ambrosio Alessandro, Vincenzo Brescia Morra, Giovanni Savettieri, Bruno Alfano, Antonio Gallo, Isabella Simone, Mario Zappia, Panetta Valentina, Simona Bonavita, Gioacchino Tedeschi P6.122 Diffusional Kurtosis MRI Correlates of Cognitive Functions in Primary-Progressive MS Maria Petracca, Heidi Bender, Colleen Farrell, Roxana Teodorescu, Jonathan Howard, Claire Riley, Johanna Cahall, Franchesca Arias, Michelle Fabian, Fred Lublin, Matilde Inglese P6.123 Functional Correlates of Impaired Working Memory in MS Patients: A Multicentre Study Alvino Bisecco, Maria Rocca, Paola Valsasina, Khaled Abdel-Aziz, Frederik Barkhof, Christian Enzinger, Franz Fazekas, Antonio Gallo, Hanneke Hulst, Xavier Montalban, Nils Muhlert, Gianna Carla Riccitelli, Alex Rovira, Gioacchino Tedeschi, Giancarlo Comi, Massimo Filippi P6.124 Cognitive Reserve in Multiple Sclerosis Modulates Hippocampal Functional Connectivity and Protects from Memory Deficits Maria Rocca, Alessandro Meani, Paola Valsasina, Gianna Carla Riccitelli, Mariaemma Rodegher, Bruno Colombo, Andrea Falini, Giancarlo Comi, Massimo Filippi P6.125 Iron in the Deep Gray Matter: Association with Cognitive Impairment in Multiple Sclerosis Claire Modica, Robert Zivadinov, Michael Dwyer, Niels Bergsland, Andre Weeks, Ralph Benedict P6.126 Brain White Matter Tract Microstructural Alterations in Multiple Sclerosis Patients with Depression and Fatigue: A Diffusion Tensor MRI Study Gianna Riccitelli, Maria Rocca, Emanuele Pravatà, Elisabetta Pagani, Marta Radaelli, Claudio Gobbi, Filippo Martinelli Boneschi, Andrea Falini, Giancarlo Comi, Massimo Filippi Poster Session VI P6.127 Contribution of Global and Regional Damage of the Gray and White Matter to Fatigue in MS Laura Parisi, Maria Rocca, Elisabetta Pagani, Bruno Colombo, Vittorio Martinelli, Andrea Falini, Giancarlo Comi, Massimo Filippi P6.128 Network Efficiency as a Final Common Pathway for Cognitive Deficits in Multiple Sclerosis: A Single Network Graph Theory Study Matteo Pardini, Varun Sethi, Nils Muhlert, Oezguer Yaldizli, Fulvia Palesi, Daniel Altmann, Maria Ron, Claudia Wheeler-Kingshott, David Miller, Declan Chard P6.129 Microstructural Damage to NAWM and GM But Not to Cortical Lesions Contributes to Cognitive Impairment in Multiple Sclerosis: A Diffusion Tensor MRI Study Maria Elisa Morelli, Maria Rocca, Elisabetta Pagani, Paolo Preziosa, Massimiliano Copetti, Mariaemma Rodegher, Federica Esposito, Andrea Falini, Giancarlo Comi, Massimo Filippi P6.130 Patterns of Regional Gray Matter and White Matter Atrophy in “Cortical Multiple Sclerosis” Laura Parisi, Maria Rocca, Flavia Mattioli, Ruggero Capra, Massimo Filippi P6.131 The Rate of New GM Lesion Development Is Similar in all MS Disease Subtypes Rasha Abdel-Fahim, Olivier Mougin, Christopher Allen, Alain Pitiot, Penny Gowland, Nikos Evangelou P6.132 Global and Regional Brain Concentration of Intra- and Extracellular Sodium in MS: A 7 Tesla MRI Study Lazar Fleysher, Roxana Teodorescu, Maria Petracca, Laura Jonkman, Niels Oesingmann, Joseph Herbert, Matilde Inglese P6.133 Accrual and Evolution of Cortical Gray Matter Lesions in People with Relapse-onset Multiple Sclerosis Varun Sethi, Tarek Yousry, Nils Muhlert, Daniel Tozer, Daniel Altmann, Maria Ron, Claudia Wheeler-Kingshott, David Miller, Declan Chard P6.134 MRI-Based Detection and Characterization of Leptomeningeal Contrast Enhancement in Multiple Sclerosis Luisa Vuolo, Martina Absinta, Elizabeth Sweeney, Daniel Reich P6.135 The Use of BigBrain in MS: An Ultrahigh-resolution 3D Template for Grey Matter MRI Segmentation Shuang Liu, Christina Azevedo, Daniel Pelletier P6.136 A Robust and Fast Algorithm for Quantifying Spinal Cord Cross-sectional Area in Myelitis Govind Nair, Winston Liu, Raya Massoud, Daniel Reich, Steven Jacobson P6.137 Relationship Between Spinal Cord Atrophy and Brain Cortical Lesions in Primary-Progressive MS Roxana Teodorescu, Maria Petracca, Colleen Farrell, Jonathan Howard, Claire Riley, Michelle Fabian, Fred Lublin, Matilde Inglese P6.138 The Neurofunctional Basis of Sensorimotor Preservation in Multiple Sclerosis Victoria Leavitt, James Sumowski P6.139 Normal Appearing White Matter Injury in MS Is Affected by the Distance to the Nearest Cortical Lesion Nikos Evangelou, Rasha AbdelFahim, Olivier Mougin, Justina Ruksenaite, Abigail Lazenbury, Penny Gowland, Alain Pitiot Risk Factors for MS Disease and Course P6.140 Level of Homocysteine, Homocysteine Thiolactone and Antibodies Against N-homocysteinylated Proteins in Patients with Multiple Sclerosis Anna Jamroz-Wisniewska, Jerzy Beltowski, Konrad Rejdak, Halina Bartosik-Psujek P6.141 Smoking Cessation and Disability Progression in Multiple Sclerosis: An Observational Cohort Study Cris Constantinescu, Ali Manouchehrinia, Radu Tanasescu, John Britton P6.142 Serum Lipid and Antiphospholipid Antibodies Profiles in Different Phases of Multiple Sclerosis Tatiana Koudriavtseva, Chiara Mandoj, Giovanni Cigliana, Giovanna D’Agosto, Paola Cordiali-Fei, Laura Conti P6.143 Multiple Sclerosis and Premorbid Risk Behaviour: Association Is Not Necessarily Causation Christopher Hawkes, David Boniface P6.144 Vitamin D and Multiple Sclerosis: Are We Still in the Dark? Michael Douglas, Lindsay Durant, Ghaniah Hassan-Smith, James Hodson, John Curnow, Atalanti Tsentemeidou P6.145 Vitamin D Deficiency in Multiple Sclerosis: Possible Influence of Circulating Vitamin D Binding Protein Levels. Suhail Al-Shammri, Abayomi Akanji, Arpita Chattopadhyay, Chetana Madala, Reema Mathew P6.146 Modulating Effects of WT1 on the Relationship Between Interferon-β and Vitamin D Levels in the Patients with Multiple Sclerosis Rui Lin, Steve Simpson, Jr., Jac Charlesworth, Ingrid van der Mei, Leigh Blizzard, Niall Stewart P6.147 The Role of Vitamin D in Optic Neuritis—an Update Jodie Burton, Jessie Trufyn, Chelsia Tung, Misha Eliasziw, Fiona Costello P6.151 Identification of Clostridium Perfringens Epsilon Toxin as a Candidate Trigger for New Lesion Formation in Multiple Sclerosis Timothy Vartanian, Kareem Rumah, Jennifer Linden P6.152 Effects of a Low Fat Plant Based Diet in Multiple Sclerosis (MS): Results of a 1-year Long Randomized Controlled (RC) Study Vijayshree Yadav, Gail Marracci, Edward Kim, Rebecca Spain, Michelle Cameron, Shannon Overs, John McDougall, Jesus Lovera, Dennis Bourdette P6.153 Expression of Multiple Sclerosis Susceptible Loci Genes May Assist in Diagnostic Decision Making Michael Gurevich, Gadi Miron, Erez Hanael, Anat Achiron P6.154 A Multiple SclerosisAssociated Single Nucleotide Polymorphism in the MERTK Receptor Is Correlated with Altered MERTK Expression Trevor Kilpatrick, Michele Binder, Judith Field, Helmut Butzkueven, Melissa Gresle P6.155 Is it Worth it to Study Families with Multiple Sclerosis (MS)? the Case of a Novel Rare Variant in a Novel Unexpected Interferon-stimulated Gene. Filippo Martinelli Boneschi, Federica Esposito, Ana-Maria Osiceanu, Melissa Sorosina, Davide Cittaro, Dejan Lazarevic, Elia Stupka, Giancarlo Comi P6.156 CD58 and Multiple Sclerosis: Genetic Association, Gene Expression and Prognostic Value Michael Hecker, Jana Blaschke, Paul Blaschke, Brit Fitzner, Dirk Koczan, Hans-Juergen Thiesen, Uwe Zettl P6.157 An Analysis of Novel Antibody Repertoires in Patients with Multiple Sclerosis: Do Particular Antibody Genes Recognize Gray Matter Cellular Targets? Ann Ligocki, William Rounds, Min Li, Paul Henson, Donna Graves, Elliot Frohman, Ann Stowe, Jacqueline Rivas, Alyssa Guzman, Sally Ward, Benjamin Greenberg, Nancy Monson P6.158 Molecular Network of ChIPSeq-Based EBNA1-Target Cellular Genes Supports Biological Implications of EBV Persistence in Multiple Sclerosis Jun-ichi Satoh, Yoshihiro Kino MS Symptoms and Comorbidities P6.148 Vitamin D, B-Cell Immunoreactivity, and B-Cell Phenotypes in Cerebrospinal Fluid of Patients with Multiple Sclerosis Brigitte Wildemann, Alexander Schwarz, Mirjam KorporalKuhnke, Sven Jarius, Juergen Haas P6.159 P6.149 P6.160 Dietary Saturated Fatty Acids Promote Differentiation of Th1 and Th17 Cells and Aggravate Neuroinflammation Ralf Linker, Markus Kleinewietfeld, De-Hyung Lee, Dominik Muller, Arndt Manzel P6.150 Sodium Intake Is Associated with Increased Disease Activity in Multiple Sclerosis Mauricio Farez, Marcela Fiol, Maria Gaitan, Francisco Quintana, Jorge Correale Gustatory Dysfunction in Multiple Sclerosis Richard Doty, Isabelle Tourbier, Fidias Leon-Sarmiento, Jayaram Udupa, Bilge Karacali, Gul Moonis, Evan Beals, Laura Fabius, Taehoon Kim, Bala Palecanda, Andre Souza Multiple Sclerosis Reported Fatigue: Obstructive Sleep Apnea and Abnormalities in Sleep Architecture in a Community Cohort Mark Gudesblatt, Myassar Zarif, Barbara Bumstead, Lori Fafard, Marijean Buhse, Steven Brass, Konstantina Bardhi, Steven Xian P6.161 Visual Field Defects in Multiple Sclerosis and Related Disorders Dong Joo Yun, Jae-Gyu Kwak, Byoung-Joon Kim P6.162 Multiple Sclerosis Exacerbation Presenting as Stress Cardiomyopathy Tyler Webb, Tania Reyna, Robert Blair, Robert Foreman P6.163 Headache in Multiple Sclerosis: Features and Implications for Disease Management Jessica Wilcox, David Tabby, Muhammad Hassan Majeed, Branden Youngman P6.164 Neuropathic Pain in Multiple Sclerosis: A Contact Heat Evoked Potential Stimulator (CHEPS) Evaluation Victor Kosac, Osvaldo Nascimento, Frederico Prado, Andre Matta, Eduardo Davidovich, Bruno Coutinho, João Dib P6.165 Longitudinal Changes of Olfactory and Gustatory Function in Patients with Multiple Sclerosis Felix Schmidt, Christian Gertz, Florian Uecker, Lutz Harms P6.166 Multiple Sclerosis Compromises Various Aspects of Female Sexual Function Julia Koehn, Ralf Linker, Tassanai Intravooth, Carl Crodel, Martina Deutsch, De-Hyung Lee, Max Hilz P6.167 Head-up Tilt Test, R-R Interval Variation and Sympathetic Skin Response in the Assessment of the Autonomic Nervous System of Patients With Multiple Sclerosis Hizir Ulvi P6.168 Metabolic Syndrome and Disability in Multiple Sclerosis: A Retrospective Study Idanis Berrios Morales, Chutima Saipetch, Anya Turetsky, Kevin Kane, Neeta Garg, Peter Riskind P6.169 Multiple Sclerosis and Stroke Eleanor Sung, Lilyana Amezcua, Steven Cen, Aaron Krug, Nerses Sanossian P6.170 Prevalence of Thyroid Disease in a Multiple Sclerosis Clinic Cohort Donald Barone, Serge Khelemsky, Decosy Hercules, Kathleen Barone P6.171 A Study of Insulin Resistance in Multiplesclerosis Subjects and Healthy Controls Myla Goldman, Scott Koenig, Rebecca Yeamans, Karen Johnston P6.172 Multiple Sclerosis Patients with Allergies Demonstrate Better Physical Outcomes But Worse Psychological Symptoms. Sahil Gupta, Katelyn Kavak, Barbara Teter, Bianca Weinstock-Guttman P6.173 Right Under Our Noses: Olfactory Pathology in Central Nervous System Demyelinating Diseases Gabriele De Luca, Albert Joseph, Jithin George, Richard Yates, Marie Hamard, Margaret Esiri P6.174 Deterioration or Improvement of Depression in Women Is Associated with Site and Size of Multiple Sclerosis Lesions Klemens Winder, Tobias Engelhorn, Ingrid Wagner, Carl Crodel, Martina Deutsch, Julia Koehn, Ralf Linker, De-Hyung Lee, Max Hilz P6.175 Functional Limitations Associated with Multiple Sclerosis: Findings from the US Medical Expenditure Panel Survey Joseph Menzin, Matthew Sussman, Monica Fay, Terrie Livingston, Glenn Phillips, Ravi Iyer Fast, Easy Registration Online · AAN.com/view/AM14 107 Thursday May 1 First Authors stand by Posters from 7:30 a.m.–9:00 a.m. Thursday, May 1 P6.176 Increased Incidence of Breast Cancer in Multiple Sclerosis: The Influence of Vitamin D and Estrogen in MS-Breast Cancer Concordance Jacquelyn Laplant, Robert Knobler P6.177 Smoking in Multiple Sclerosis Patients Is Negatively Associated with Patient Perceived Psychosocial Factors Katelyn Kavak, Barbara Teter, Bianca Weinstock-Guttman P6.178 Risk of Mood Changes with High Dose Corticosteroid Treatment for Demyelinating Event in Multiple Sclerosis Sarah Morrow, Jennifer Barr, Heather Rosehart, Manera May, Sandra Ulch P6.188 The Outcome of Preconceptual Counselling in Women with Epilepsy. Ellen Campbell, Beth Irwin, Inez Cooke, Stephen Hunt, John Craig, Jim Morrow P6.189 The Effect of Valproate and Lamotrigine Monotherapy on Bone Health in Adult Epileptic Patients Mohammad Alhalabi, Ola Albaghdadi, Zaynab Alourfi, Lama Youssef Epilepsy and Clinical Neurophysiology (EEG): MEG and Imaging P6.190 Epilepsy and Clinical Neurophysiology (EEG): Quality of Life and Comorbidities Response-driven Models based on MRI and SPECT findings on Hippocampus for Lateralization of Temporal Lobe Epilepsy Mohammadreza Nazemzadeh, Jason Schwalb, Kost Elisevich, Hassan Bagher-Ebadian, Hamid Soltanian-Zadeh P6.179 P6.191 Patient and Caregiver Quality of Life in Psychogenic NonEpileptic Seizures Compared to Epileptic Seizures Ioannis Karakis, Georgia Montouris, Charitomeni Piperidou, Marta San Luciano, Kimford Meador, Andrew Cole P6.180 Impact of Seizure Frequency Reduction on Health-Related Quality of Life Among Clinical Trial Subjects with Refractory Partial-Onset Seizures: A Pooled Analysis of Phase III Clinical Trials of Eslicarbazepine Acetate Kathryn Anastassopoulos, Fulton Velez, Rui Sousa, T. Christopher Bond, Xuezhe Wang, David Blum, Joyce Cramer P6.181 Quality of Life and Sleep in Young Male Patients with Epilepsy Hakan Tekeli, Halit Yasar, Semih Alay, Mustafa Kendirli, Mehmet Senol, Turker Turker, Mehmet Saracoglu P6.182 STOP-BANG Screening for Obstructive Sleep Apnea in Epilepsy Joon Kang, Maromi Nei P6.183 Effects of Lacosamide on Sleep Parameters in Healthy Subjects: Results from an Open-label Study John Hudson, Stephen Yates, Paulette Williams, Jeff Guptill, William Byrnes, Neil D’Cruz P6.184 Systematic Review of the Impact of Rapid Eye Movement Sleep on Seizure Frequency Marcus Ng, Milena Pavlova P6.185 Do Antidepressants Make Seizures More or Less Likely in Focal Epilepsy Patients Undergoing Elective EEG Monitoring? Alyssa Brandt, Rachel Godfred, Mihir Parikh, Alan Haltiner, Nicole Fortier, Lisa Caylor, Jehuda Sepkuty, Michael Doherty P6.186 Does Vitamin D Use Alter Seizure Collections During Elective Adult Inpatient Video EEG Monitoring? Alyssa Brandt, Rachel Godfred, Mihir Parikh, Nicole Fortier, Alan Haltiner, Lisa Caylor, Jehuda Sepkuty, Michael Doherty P6.187 Prevalence of Metabolic Syndrome in Valproate-treated Adult Patients with Epilepsy Aleksei Rakitin, Triin Eglit, Sulev Kõks, Margus Lember, Sulev Haldre 108 Subtraction Imaging and MR Co-registration to Increase Diagnostic Yield of Ictal and Interictal SPECT in Localization of Epileptogenic Foci in Patients with Intractable Seizures Zachary Abramson, Asim Choudhri, Hubert Magill, James Wheless P6.192 Magnetic Resonance Grading of Hippocampal Sclerosis in Temporal Lobe Epilepsy Patients Using an Equilibrium Model Hassan Bagher-Ebadian, Mohammadreza Nazem-Zadeh, Jason Schwalb, Abdelrahman Hassane, Hamid Soltanian-Zadeh P6.193 Cerebral Hyperperfusion and Vasodilatory Changes in Acute Seizure— Report of Three Cases Balaji Krishnaiah, Sarita Said Said, Krishnamoorthy Thamburaj P6.194 Quantitative Analyses of EEG with Special Electrodes in TGA Patients Hye Ihn Kim, Jeong-Youn Kim, Chang-Hwan Im, Won-Joo Kim P6.195 WITHDRAWN P6.196 Is Presurgical MEG Useful in Intractable Temporal Lobe Epilepsy? Helen Barkan, Shannon Sparrow, Ann Marie Collier, Michael Funke P6.197 Validation of Magnetoencephalography (MEG) as Presurgical Evaluaiton Tool in Pediatric Patients with Localization-Related Intractable Epilepsy. Helen Barkan, Marie Collier, Shannon Sparrow, Michael Funke P6.198 Comparison of Diagnostic Methods for Optimizing Epilepsy Surgery Outcome Including Magnetoencephalography William Boles, Jane Boggs, Valerie Woodard, Cormac O’Donovan 7:30 a.m.–11:00 a.m. P6.200 F MRI Analysis in Chronic Migraine: Preliminary Report Licia Grazzi, Frank Andrasik, Stefania Ferraro, Susanna Usai, Luisa Chiapparini, Maria Grazia Bruzzone, Gennaro Bussone P6.201 White Matter Microstructure Abnormalities in Paediatric Migraine Patients: In-Vivo Measures of Brain Hyperexcitability? Roberta Messina, Maria Rocca, Bruno Colombo, Elisabetta Pagani, Andrea Falini, Giancarlo Comi, Massimo Filippi P6.202 A Case of Supratrochlear, Supraorbital, and Trigeminal Neuralgia Associated with Neurofibromas of Multiple Cranial Nerves Kristina Lopez, David Watson, Jeffery Hogg P6.203 Mid-life Migraine and Late-life Movement Disorder Symptoms: AGES-Reykjavik Study Ann Scher, G. Ross, Sigurdur Sigurdsson, Melissa Garcia, Larus Gudmundsson, Sigurlaug Sveinbjornsdottir, Vilmundur Gudnason, Lenore Launer Retrospective Analysis of the Predictors of Successful Posterior Fossa Decompression in Patients with Headaches Attributed to Chiari Malformation Naresh Mullaguri, Rahul Khanna, Gulshan Uppal, Prityi Rani, Natasha Kataria, Gauravjot Sandhu, Niranjan Singh P6.213 A Nutrition Intervention for Migraines Anne Bunner, Joseph Gonzalez, Francesca Valente, Ulka Agarwal, Neal Barnard P6.214Individualized Pharmacogenetic Testing Improves Mood and Anxiety Treatment Outcomes in Chronic Migraine Patients Sandeep Vaishnavi, Qian Liu, Liz Griffin, Tim Ramsey, Mark Brennan P6.215 A Live Patient Simulation Model to Effectively Manage Difficult Headache Patients Fermina Pirmohamed P6.216 P6.204 Does the New International Classification of Headache Disorders Affect the Prevalence of Aura in Patients with Migraine ? Hossein Ansari Chronic Migraine with Medication Overuse Is Associated with Low Cognitive Reserve Marian Gomez Beldarrain, Ane Anton Ladislao, Urko Aguirre Larracoechea, Alberto Cabrera Zubizarreta, Isabel Oroz, Carlos GarciaMonco Carra P6.205 P6.217 Barriers to Chronic Migraine Care: Results of the CaMEO (Chronic Migraine Epidemiology and Outcomes) Study Dawn Buse, Richard Lipton, Michael Reed, Daniel Serrano, Kristina Fanning, Aubrey Manack P6.206 Association of the Long Pentraxin PTX3 Gene Polymorphism (rs3815627) With Migraine in Iranian Population Alireza Zandifar, Niloufar Iraji, Maryam Taheriun, Mohamadhasan Tajaddini, Faraidoon Haghdoost, Ehsan Zandifar, Samaneh Zandifar, Shaghayegh Javanmard P6.207 Sinking Bone Flap Causing Paradoxical Orthostatic Headaches Mitra Assadi Khansare, Aimee Walsh, Mandy Binning P6.208 Investigation of Chemokine Receptor CCR2V64Il Gene Polymorphism and Migraine in Iranian Population Alireza Zandifar, Maryam Taheriun, Samira Soleimani, Faraidoon Haghdoost, Mohamadhasan Tajaddini, Samaneh Zandifar, Ehsan Zandifar, Shaghayegh Javanmard Headache: Outcomes P6.209 Idiopathic Intracerebral Hypertension (IIH)/pseudotumor: Removing Less CSF Is Best Franchesca Fiorito-Torres, Melissa Rayhill, Michael Perloff P6.210 Headache: Imaging and Epidemiology Peri Ictal Headache in Epilepsy Natarajan Visvanathan, Ramakrishnan Ramalingam, Radha Mahadevan P6.199 P6.211 Circle of Willis, Cerebral Blood Flow, and White Matter Hyperintensities in Migraine Brett Cucchiara, Ronald Wolf, Lidia Nagae, Scott Kasner, John Detre P6.212 Validating a Definition of Alcohol Sensitivity in Women with Migraine Qinyi Jiang, William Young, Michael Oshinsky, Seokmin Kim, Evan Klein 2O14 Scientific Abstract Listing and Annual Meeting Information Bilateral Pain Hypersensitivity over the Trigeminal Region and Dental Deafferentations in Patients with Classical Trigeminal Neuralgia Nathalie Guy, Béatrice Claise, Pierre Clavelou, Radhouane Dallel Aging, Dementia, and Cognitive and Behavioral Neurology: Structural Imaging P6.218 Diffusion Tensor Imaging in PSEN1-Related Spastic Paraparesis Reveals Widespread White Matter Abnormalities Steffan Soosman, Meredith Braskie, Jeffry Alger, David Wharton, John Ringman P6.219 Shared Vulnerability of Two Synaptically-Connected Medial Temporal Areas to Age and Cognitive Decline: A 7T MRI Study Geoffrey Kerchner, Jeffrey Bernstein, Michelle Fenesy, Gayle Deutsch, Manojkumar Saranathan, Michael Zeineh, Brian Rutt P6.220 White Matter Disease in Behavioral Variant Frontotemporal Dementia Correlates with Risk-taking Behavior John Powers, Corey McMillan, Katya Rascovsky, Lisa Burkholder, Murray Grossman P6.221 The Symmetric and Asymmetric Variant of Microvascular White Matter Disease Bernard Galea, Mushtaq Qureshi, Malik Adil, Muhammad Suri, Adnan Qureshi P6.222 Voxel-based Morphometry Reveals Gray Matter Loss in Patients with Paget’s Disease of the Bone Carrying SQSTM1 Gene Mutations Innocenzo Rainero, Elisa Rubino, Federico D’Agata, Silvia Rossetti, Laura Gastaldi, Mauro Bergui, Laura Orsi, Lorenzo Pinessi, Giancarlo Isaia, Marco Di Stefano Poster Session VI P6.223 Regional Brain Differences in Cortical Thickness Between Patients with Amnesic Mild Cognitive Impairment and Alzheimer`s Disease Dementia Ignacio Demey, Fernando Ventrice, Galeno Rojas, Veronica Somale, Ricardo Allegri, Fabian Bevacqua, Sebastian Lescano P6.224 Hippocampal Subfield Analysis in MCI Patients: Comparing FreeSurfer on 3T MRI with Hand Segmentation on 7T Data Salil Soman, Ansgar Furst, Geoffrey Kerchner Aging, Dementia, and Cognitive and Behavioral Neurology: Language P6.225 Functional Language Lateralization of Primary Progressive Aphasia Variants Zachary Miller, Leighton Hinkley, Danielle Mizuiri, Susanne Honma, Anne Findlay, Bruce Miller, Srikatan Nagarajan, Maria Gorno Tempini P6.226 A Cross-Culturally Valid Assessment of Object Semantics Bonnie Breining, Trisha Lala, Kyrana Tsapkini, Eleni Peristeri, María Macarena Martínez Cuitiño, Facundo Manes, Argye Hillis P6.227 Neural Correlates of Sentence Repetition in the Logopenic Variant of Primary Progressive Aphasia Drew Goldberg, Anna Isenberg, Murray Grossman P6.228 Predictors of Recovery of Chronic Aphasia Aarushi Suneja, Marlis Gonzalez-Fernandez, Argye Hillis P6.229 Syntactic Processing Skills in the Three Variants of PPA Rajani Sebastian, Cameron Davis, Yessenia Gomez, Lydia Trupe, Argye Hillis Aging, Dementia, and Cognitive and Behavioral Neurology: Memory P6.235 Correlation between Cortical Thickness Measurements from Magnetic Resonance Imaging and Cognitive Performance on Episodic and Semantic Memory Tests Ignacio Demey, Galeno Rojas, Veronica Somale, Fernando Ventrice P6.236 Preservation of Spatial Function: Role in Differential Diagnosis of Behavioral Variant Frontotemporal Dementia Anneliese Radke, Tracy Jerard, Joel Kramer, Katherine Possin, Nikolas Block, Alexander Beagle, Bruce Miller P6.237 Validation of the Dynamic Affect Recognition Test (DART): Behavior and Anatomy in Neurodegenerative Disease Anneliese Radke, Babu Adhimoolam, Tal Shany-Ur, Katherine Possin, David Marin, Diana Zackey, Pardis Poorzand, Bruce Miller, Katherine Rankin P6.233 Sensitivity of Consensus Criteria in the Quantitative Classification of Primary Progressive Aphasia Meredith Wicklund, Joseph Duffy, Edythe Strand, Mary Machulda, Jennifer Whitwell, Keith Josephs P6.234 Bilingualism and Language Networks in the Semantic Variant of Primary Progressive Aphasia. Ismael Calandri, Alejandra Amengual, Hernán Chaves, Cecilia Rollán, Mauricio Farez, Liliana Sabe, Cristina Medina, Griselda Russo, Silvia Vazquez, Ricardo Allegri Anabolic Steroids Abuse and Ischemic Stroke: A Case Report and Literature Review Ge Xiong, Arnaldo Velez, Anna Khanna P6.262 P6.248 P6.263 A Case Series of Nonbacterial Thrombotic Endocarditis Associated with Gynecological Malignancies Alice Schabas, Philip Teal, Samuel Yip, Sharanpal Mann P6.249 Pituitary Apoplexy Presenting as Anterior Choroidal Artery Territory Infarct: A Case Report Sasikanth Gorantla, Kasra Maasumi, Jason Felton, Nabeel Dar, Jongyeol Kim P6.250 Lacunar Infarct Presenting Like Axillary Nerve Lesion: A case report Oguzhan Oz, Serdar Tasdemir, Hakan Akgun, Semih Alay, Ahmet Cetiz, Zeki Odabasi, Seref Demirkaya P6.239 White Matter Disease and Cognitive Impairment in FMR1 Premutation Carriers Christopher Filley, Mark Brown, Karen Onderko, Megan Ray, Rachael Bennett, Jim Grigsby P6.252 P6.240 Age Effects on the Neural Basis of Self-Generation in Verbal Paired Associate Learning Jennifer Vannest, Thomas Maloney, Benjamin Kay, Miriam Siegel, Jane Allendorfer, Christi Banks, Jerzy Szaflarski P6.253 P6.241 P6.254 P6.242 18F-FDG-PET Metabolic Patterns in the Semantic Variant of PPA: Functional/Clinical Correlations. SingleSubject 18F-FDG-PET Beyond MRI Daniela Perani, Leonardo Iaccarino, Lucia Guidi, Pasquale Della Rosa, Giuseppe Magnani, Stefano Cappa P6.247 P6.251 P6.231 P6.232 P6.261 Cognitive Deficits of Large-Vessel and Small-Vessel Vascular Dementia Ju-Young Na, Bong-Goo Yoo Language Networks Imaging in Primary Progressive Aphasia in a Latin Population Ismael Calandri, Alejandra Amengual, Hernán Chaves, Cecilia Rollán, Mauricio Farez, Liliana Sabe, Cristina Medina, Zanuzo Patricia, Jorge Campos, Gabriela Cohen, Jorge Calvar, Silvia Vazquez, Ricardo Allegri Impairment in Sentence Comprehension in Patients with the Behavioral Variant of Frontotemporal Degeneration (bvFTD) Rebecca Williams, Katya Rascovsky, Murray Grossman A Case of Akinetopsia Wolfgang Grisold, Sabine Pollanz, Birgit Surböck, Barbara Horvath P6.238 Accentuated Brain Responses During Semantic Object Memory Retrieval in Amnestic Mild Cognitive Impairment as Measured by Event-Related Potentials Hsueh-Sheng Chiang, Raksha Mudar, Justin Eroh, Jeffrey Spence, Athula Pudhiyidath, Jeremy Tanner, Erin Venza, Audette Rackley, Kristin Martin-Cook, Kyle Womack, Elizabeth Bartz, Michael Kraut, John Hart P6.230 P6.246 Relationship Between Dementia Severity Ratings and Memory Accuracy Versus Certainty Matthew Harris, Daniel Kaufer P6.243 Changes of Face Recognition After Medial Temporal Lobe Resection Masoud Majed, Emad Ahmadi, Seyed Mohammad Ghodsi, Sina Tafazoli, Abdol Hossein Abbassian Cerebrovascular Disease and Interventional Neurology: Case Reports P6.244 A Case of Perioperative Stroke Caused by Tumor Embolus. Stella Hughes, Annemarie Hunter, Jamie Campbell, Aidan Brady, Brian Herron, Graham Smyth, Ian Rennie, Stephen Hunt P6.245 Thrombosis of the Vein of Trolard Secondary to Renal Minimal Change Disease: A Case Report and Literature Review Marcelo Rocha, Steven Feske, Allan Ropper Case of Neurosyphilis Presenting as MoyaMoya Syndrome Saima Ali, Soundarya Gowda Two Cases of Malignant Cerebral Edema Related to Systemic Lupus Erythematous Lauren Koffman, Khaled Asi, Ashlee Russo, Dhimant Dani, Edward Manno Case Report: Multiple Scattered Ischemic and Hemorrhagic Strokes after Transarterial Chemoembolization for Hepatocellular Carcinoma Alhamza Al-Bayati, Douglas Smith, Elia Haddad The Clinical Features of Cerebral Vein and Sinus Thrombosis in Male Patients Hongyan Ding, Qiang Dong P6.255 Intracranial Venous Sinus Thrombosis: Report of Three Cases Hans Reyes Garay, Carla Sueldo Feijoo, Jorge Martin Gavidia Chucan P6.256 Generalized Dilative Arteriopathy Without Myopathy: A New Phenotype of Pompe Disease Andoni Echaniz-Laguna, Marc Bataillard, Véronique Quenardelle P6.257 Brain Herniation Due to Mitochondrial Encephalomyopathy, Lactic Acidosis, Stroke Like Events (MELAS) with 3256 Mutation Responsive to Decompressive Craniotomy Chunmei Cui, Robert Schwendimann P6.258 Cerebral Varicella Zoster Vasculopathy Sine Herpete: Atypical Ramsay-Hunt Syndrome presentation in an Immunocompetent Patient Karina Gonzalez Otarula, Verónica Bruno, Virginia Pujol-Lereis, Sebastian Ameriso Amusia: Unique Presentation of Stroke Charu Ramchandani, Fawaz Alsmaan, Heidi Schwarz, Ziad Alkhoury Recurrent Intra-luminal Aortic Thrombus and Ischemic Stroke in a Patient with Essential Thrombocythemia Daniel Vela-Duarte, Murray Flaster Right Hemispheric Acute Ischemic Stroke Secondary to Right Common Carotid Artery Free Floating Thrombus Due to Hypercoagulable State in an Otherwise Healthy 48-year-old Woman. Karen Orjuela, Rick Gill, Luka Vlahovic, Sarkis Morales-Vidal P6.264 Uncomon Cause Stroke: Thalamic Stroke as Initial Presentation of Dunnigan Familial Partial Lipodystrophy (FPLD) Fatai Radji, Elena Leca Radu, Kahina Dannepond, Marie-Laure Nunes P6.265 Is Achondroplasia Linked to Stroke? Harpreet Kaur, Shilpi Mittal, Catherine Hosley P6.266 “Pseudostroke”: Clinically Diagnosed Ischemia Shown to Be Multiple Sclerosis at Autopsy: A Case Report Gulshan Uppal, Natasha Kataria, Prityi Rani, Douglas Miller P6.267 Delayed Cortical Blindness After Cardiac Arrest Anibal Lugo, Abdulrahman Alwaki, Christopher Goshgarian, Justin Belsky, Panayiotis Mitsias P6.268 Case Report—Cerebral Amyloid Angiopathy with Granulomatous Angiitis Ali Saeed, Vibhav Bansal, Howard Chang, Michael Flink, Anmar Razak, Syed Hussain P6.269 Paradoxical Cerebral Embolism from Thrombolysis of a Clotted Arteriovenous Graft Umang Shah, Ruchir Shah P6.270 A Rare Association Between Ulcerative Colitis and Bilateral Thalamic Stroke Sara Misthal, Dababneh Haitham, Asif Bashir, Mohammed Hussain, Mohammad Moussavi, Jawad Kirmani P6.271 Monocular Diplopia After Left Posterior Cerebral Artery Territory Infarction Konstantinos Papadopoulos, Brigitte Capron, Raphael Hourez P6.272 Rapid High Volume CSF Loss: A New Cause of Coma Minjee Kim, Rose Du, Sherry Chou P6.273 Thrombectomy with the Penumbra 5 MAX ACE Achieves More Efficient Recanalization Nazli Janjua, Jeffrey Farkas, Karthikeyan Arcot, Rajesh Kumar, Delbrune Jean, Nikolaos Papamitsakis, Yevgeny Margulis, Subasini Dash, Kenneth Levin, Salman Azhar P6.259 Synthetic Cannabis and Acute Ischemic Stroke Miya Bernson-Leung, Lester Leung, Sandeep Kumar P6.260 A Novel Heterozygous c.164G>C Mutation in the Exon 2 of the NOTCH3 Gene Causing Cadasil Raphael Hourez, Konstantinos Papadopoulos, Guy Bruninx, Yves Sznajer Fast, Easy Registration Online · AAN.com/view/AM14 109 Thursday May 1 First Authors stand by Posters from 7:30 a.m.–9:00 a.m. Thursday, May 1 Cerebrovascular Disease and Interventional Neurology: Risk Factors P6.285 P6.274 P6.286 Visit-to-visit Systolic Blood Pressure Variability Predicts All-cause and Cardiovascular Mortality After Lacunar Infarct Gary Lau, Yuen Kwun Wong, Richard Chang, KC Teo, Sonny Hon, Koon Chan, KL Wat, Raymond Cheung, Leonard Li, David Siu, Shu Leong Ho, Hung Fat Tse P6.275 Medicare’s New Two Midnight Rule for In-patient Status Admission Applied to Transient Ischemic Attack Patients Predicted by Hypertension History and Age Maria Chavez-Keatts, Dominique Monlezun, Jr, Alexander George, Ramy El Khoury, Sheryl Martin-Schild P6.276 High Burden of Brain Microvascular Disease in Difficult-tocontrol Hypertension Maria Zurru, Claudia Alonzo, Laura Brescacin, Ariel Luzzi, Luis Camera, Gabriel Waisman, Edgardo Cristiano P6.277 Comparison of Classical Risk Factors, Lypids, Stress and Depression Among Patients with First Ischemic Stroke and Acute Myocardial Infarction in a Center from Buenos Aires. Dario Lisei, Martin Lopez Vicchi, Gabriel Persi, Matías Failo, Ricardo Iglesias, Maria Ballarino, Sebastian Camerlingo, Virginia Laura Parisi, Emilia Gatto P6.278 Analysis of Comorbidities in Ischemic Stroke Patients Thomas Cochran, Jose Chaves, Eric Fulmer, Dawn Blackhurst, Shannon Sternberg, R. Leacock, Thomas Nathaniel P6.279 Low Density Lipoprotein Receptor Related Protein-1 and 6 Gene Variants and Ischemic Stroke Risk Andrea Harriott, Michael Heckman, Sruti Rayaprolu, Alexandra Soto-Ortolaza, Rainer Malik for METASTROKE Consortium, John Cole, James Meschia, Owen Ross P6.280 Stroke in Very Old Patients Drini Dobi, Mira Kapisyzi, Jera Kruja P6.281 Analysis of the Relation Between Chronic Kidney Disease and Acute Ischemic Stroke. Patricio Blaya, Mariano Borrelli, Mariela Cabrera, Claudia Gonzalez, Walter Gramajo, Javier Rolle, Nestor Estevez, Jorge Gimenez, Cristina Trujillo, Marcelo Mattiazzi P6.282 The Relationship Between Leukocytosis and Time to Neurodeterioration Amelia Boehme, James Siegler, Karen Albright, Alexander George, Dominique Monlezun, Jr, Adam Friedant, Brittany Gouse, T. Beasley, Sheryl Martin-Schild Neuro-ophthalmology/ Neuro-otology II P6.283 Incidence, Seasonality, and Comorbidity in Vestibular Neuritis Ivan Adamec, Magdalena Krbot, Mario Habek P6.284 Retinal Ganglion Cell Injury Precedes RNFL loss in Acute Optic Neuritis John Guy, Vittorio Porciatti, William Feuer, Angela Herro, Byron Lam 110 Gordon Holmes 100 Years Later: Cortical Folding Predicts Retinotopic Organization Noah Benson, Omar Butt, David Brainard, Geoffrey Aguirre Retinal Structure and Function in Adults with Refractory Complex Partial Seizures (rCPS) Treated with Vigabatrin: Initial Results of the Sabril Vision Study Robert Wechsler, Chris Johnson, Robert Sergott, Kenneth Laxer, Yekaterina Dribinsky, Colleen Canavan, Jouko Isojarvi, Deborah Lee P6.287 Vision-Based Concussion Testing in a Youth Ice Hockey Cohort: Effects of Age and Visual Crowding Jennifer Morganroth, Steven Galetta, Laura Balcer P6.288 Saccade Properties and Fixation Instability Differentiate Ataxias Pamela Federighi, Francesca Rosini, Elena Pretegiani, Claudia Vinciguerra, Gabriele Lucii, David Zee, R. John Leigh, Lance Optican, M.T. Dotti, Antonio Federico, Alessandra Rufa P6.289 Quantitative Videooculography to Differentiate Stroke from Vestibular Neuritis in Acute Vertigo—Vestibulo-ocular Reflex Gain Distributions and Optimal Test Thresholds for Diagnosis Ali Saber Tehrani, Georgios Mantokoudis, Amy Wozniak, Karin Eibenberger, Jorge Kattah, Cynthia Guede, David Zee, David Newman-Toker P6.290 Susac’s Syndrome: Five Cases with Predominant Branch Retinal Artery Occlusion Thomas Seifert-Held, Alexander Barounig, Maria Storch, Hans Offenbacher, Martin Weger, Beate Langner-Wegscheider, Franz Fazekas P6.291 Correlation of Acute Phase Reactants and Temporal Artery Biopsy (TAB) in Patients with Giant Cell Arteritis (GCA) Padmaja Sudhakar, Sachin Kedar P6.292 Clinical and Electrophysiological Photostress Recovery Times in Distinguishing Demiyelinating Optic Neuritis And Maculopathy Fethi Idiman, Ahmet Onur Keskin, Mahmut Kaya, Egemen Idiman, Onur Bulut P6.293 A Retrospective Study of Chronic Relapsing Inflammatory Optic Neuropathy (CRION) Padmaja Sudhakar, Sachin Kedar, Joseph Berger P6.294 Eye Movement Features in Rare Hereditary Parkinsonian Syndromes Elena Pretegiani, Gabriele Lucii, Pamela Federighi, Francesca Rosini, Antonio Federico, Alessandra Rufa P6.295 Ocular Motility Disturbances in Orbitofacial Neurofibromatosis Type 1 Thomas Bosley, Ibrahim Alorainy, Jose Morales, Imtiaz Chaudhry, Darren Oystreck P6.296 Neurosurgical Cases with Cortical Vision Loss Followed by Improvement Bonnie Keung, Julian Lin, Jeffrey Klopfenstein, Jorge Kattah P6.297 Optical Coherence Tomography Quadrant Analysis of Retinal Nerve Fiber Layer in Relapsing and Remitting Multiple Sclerosis John Rose, Anette Fjeldstad 7:30 a.m.–11:00 a.m. P6.298 Demyelinating Optic Chiasmopathy Due to Mycobacterium Haemophilum in a Patient with AIDS Alexander Merkler, George Parlitsis, Alison May, Dara Bier, Sara Simpson, Sarju Patel, Ehud Lavi, Audrey Shuetz, Marc Dinkin P6.299 Visual Evoked Potential and Magnetic Resonance Imagine Are More Effective Markers of Multiple Sclerosis Progression Than Laser Polarimetry with Variable Corneal Compensation Ema Kantorova, Peter Žiak, Koyšová Mária, Kamil Zeleňák, Egon Kurča, Mária Hladká, Alexandra Sedláková P6.300 Presence of AQP4 Antibodies Correlates with Negative Outcome of Optic Neuritis Jana Lizrova Preiningerova, Petra Nytrova, Pavel Kuthan, Pavel Diblik, Eva Havrdova P6.301 Evidence of Multi-Domain Mild Cognitive Impairment in Idiopathic Intracranial Hypertension Anat Kesler P6.302 ‘Ping-Pong’ Gaze in Hypoglycemic Encephalopathy Saima Ali, Scott Haines P6.303 Do Not Forget Susac Syndrome in Patients with Unexplained Acute Confusion Michael Star, Maria Bruzzone, Felipe De Alba, Rick Gill, Michael Schneck, Jose Biller P6.304 Clinical Utility of Cervical Vestibular Evoked Myogenic Potential (VEMPc) in Ménière’s disease Guillermo Videla, Ana Bisonni, Jorge Norscini, Edgardo Cristiano P6.305 An Unusual Case Of Idiopathic Intracranial Hypertension Presenting with Simultaneous IIIrd, VIth and V11th Nerve Palsies Akshat Katyayan, Venu Parachuri, Delphin Sallowm, Ryan Walsh P6.306 Restricted Diffusion Imaging in Active Seizure: A Case Report Adnan Subei, Eric Eggenberger P6.307 Presence of AQP4 Antibodies Correlates with Negative Outcome of Optic Neuritis Jana Lizrova Preiningerova, Petra Nytrova, Pavel Kuthan, Pavel Diblik, Eva Havrdova P6.308 Diplopia and Esophoria Induced by Medial Thalamic Deep Brain Stimulation Barbara Kelly Changizi, Catherine Cho, Brian Kopell, Janet Rucker Aging, Dementia, and Cognitive and Behavioral Neurology: Imaging P6.309 Decline in Perceptual Motor Speed and Cognitive Flexibility Associated with Regional Patterns of FDG PET Hypometabolism Alan Lerner, Alok Sachdeva, Curtis Tatsuoka P6.310 A fMRI Graph Theory Study of the Effect of Gender and Aging on Topology of Functional Brain Networks Gianna Riccitelli, Maria Rocca, Paola Valsasina, Alessandro Meani, Federica Agosta, Massimo Filippi 2O14 Scientific Abstract Listing and Annual Meeting Information P6.311 Early Striatal Perfusion Deficits in Autosomal Dominant Alzheimer Disease Detected with Arterial Spin Labeled MRI. Eric McDade, Albert Kim, Jeffrey James, Davneet Minhas, Snezana Ikonomovic, Oscar Lopez, Beth Snitz, Julie Price, James Becker, Chester Mathis, William Klunk P6.312 The Effect of Age of Onset on the Brain Functional Connectivity in Alzheimer’s Disease: A Graph Analysis Study Elisa Canu, Federica Agosta, Sebastiano Galantucci, Alessandro Meani, Giuseppe Magnani, Alessandra Marcone, Andrea Falini, Giancarlo Comi, Massimo Filippi P6.313 Microstructural White Matter Alterations Correlate with Cerebral Amyloid Angiopathy Burden and Cognitive Measures: A DTI/PET Study Yael Reijmer, Panagiotis Fotiadis, Sergi Martinez-Ramirez, Aaron Schultz, Anne Reed, Alison Ayres, Kristin Schwab, Jonathan Rosand, Anand Viswanathan, Keith Johnson, Steven Greenberg, Edip Gurol P6.314 Strategic Choice in Frontotemporal Dementia: A Pilot Study Alessandra Dodich, Chiara Cerami, Nicola Canessa, Chiara Crespi, Alessandra Marcone, Andrea Falini, Stefano Cappa P6.315 Decreased White Matter NAA in Alzheimer’s Disease Navid SerajiBozorgzad, Fen Bao, Krishna Thakore, Omar Khan P6.316 Medial Parietal Cortex GABA Measurements in Alzheimer’s Disease Are Inversely Associated with Functional Response Novraj Dhanjal, Mark McPhail, Marzena Wylezinska, Richard Wise P6.317 Dorsolateral Prefrontal Cortex Modulation by Caudate Dopamine During a Working Memory Task in Parkinson Disease Joseph Masdeu, Daniel Eisenberg, Catherine Hegarty, Brett Cropp, Daniel Rubinstein, Philip Kohn, Karen Berman P6.318 Region Specific Alpha-band Resting-state Functional Connectivity Predicts Focal Cognitive Deficits in Alzheimer’s Disease Spectrum Kamalini Ranasinghe, Leighton Hinkley, Alexander Beagle, Danielle Mizuiri, Anne Dowling, Susanne Honma, Mariel Finucane, Carole Scherling, Bruce Miller, Srikatan Nagarajan, Keith Vossel P6.319 Florbetapir F18 Positron Emission Tomography Identification of Beta-Amyloid in the Living Brain: A Consecutive Clinical Case Series Effie Mitsis, Heidi Bender, Lale Kostakoglu, Josef Machac, Jane Martin, Jennifer Woehr, Martin Goldstein, Mary Sano, Samuel Gandy P6.320 Differences in 11C-PIBPET Imaging Patterns in Patients with Alzheimer’s Disease Without Microbleeds and Those with Cerebral Amyloid Angiopathy Yuichi Hayashi, Jun Shinoda, Nobuaki Yoshikura, Masahiro Waza, Yoshitaka Asano, Akio Kimura, Takashi Inuzuka Poster Session VI First Authors stand by Posters from 7:30 a.m.–9:00 a.m. P6.321 Association Between Longitudinal Increases in Serum Glucose and Metabolic Decline in Azheimer’s Disease-Related Brain Regions Christine Burns, Alfred Kaszniak, Kewei Chen, Wendy Lee, Daniel Bandy, Richard Caselli, Eric Reiman Effects of β-Amyloid Load on White Matter Integrity in Dementia with Lewy Bodies Zuzana Nedelska, Christopher Schwarz, Bradley Boeve, Robert Reid, Scott Przybelski, Jeffrey Gunter, Matthew Senjem, Glenn Smith, Tanis Ferman, Yonas Geda, David Knopman, Ronald Petersen, Clifford Jack, Kejal Kantarci P6.322 P6.323 Florbetapir Scanning Excludes Alzheimer’s Disease in a Retired NFL Player with Delayed Cognitive Impairment Effie Mitsis, Silvana Riggio, Emily D’Antonio, Martin Goldstein, Steven DeKosky, Thomas Naidich, Bradley Delman, Josef Machac, Lale Kostakoglu, Gregory Elder, Mary Sano, Samuel Gandy, Wayne Gordon P6.324 Alzheimer as a Default Mode Network Disease: A Grey Matter, Functional and Structural Connectivity Study Marcio Balthazar, Marina Weiler, Brunno Campos, Thiago Rezende, Benito Damasceno, Fernando Cendes P6.325(18F)FDG PET Evidence of PIB-Positive PET in Individuals with Early- But Not Late-onset Frontotemporal Dementia Eric Brown, Ariel Graff-Guerrero, Sylvain Houle, Alan Wilson, Zahinoor Ismail, Bruce Pollock, Benoit Mulsant, David Tang-Wai, Nicolaas Verhoeff, Morris Freedman, Romina Mizrahi, Tiffany Chow P6.332 P6.327 P6.333 Cavum Septum Pellucidum in Symptomatic Retired Pro-football Players Raquel Gardner, Christopher Hess, Katherine Possin, Brendan Cohn-Sheehy, Joel Kramer, Mitchel Berger, Bruce Miller, Kristine Yaffe, Gil Rabinovici P6.328 Reliable Detection of Striatal Amyloid with (18F) Flutemetamol: Validation with Postmortem Histopathology Thomas Beach, Dietmar Thal, Adrian Smith, Chris Buckley P6.329 Progressive Hippocampus Atrophy in Persons with Mild Cognitive Impairment: A Longitudinal MRI Study Iryna Lobanova, Amna Sohail, Malik Adil, Adnan Qureshi P6.330WITHDRAWN P6.331 Pathologic validation of the EADC-ADNI Harmonized Hippocampal Protocol Liana Apostolova, Chris Zarow, Kristina Biado, Sona Babakchanian, Marina Boccardi, Johanne Somme, Hedieh Honarpisheh, Anna Blanken, Jenny Brook, Spencer Tung, Denise Ng, Jeffrey Alger, Harry Vinters, Martina Bocchetta, Martina Bocchetta, Henri Duvernoy, Clifford Jack, Giovanni Frisoni Dementia with Lewy bodies: Pathological Basis of the Cingulate Island Sign Jonathan Graff-Radford, Melissa Murray, Val Lowe, Bradley Boeve, Tanis Ferman, Scott Przybelski, Timothy Lesnick, Matthew Senjem, Jeffery Gunter, Glenn Smith, David Knopman, Clifford Jack, Dennis Dickson, Ronald Petersen, Kejal Kantarci Progressive Hippocampus Atrophy in Persons with Alzheimer’s Disease: A Longitudinal MRI study Iryna Lobanova, Amna Sohail, Malik Adil, Aveen Saed, Adnan Qureshi P6.334 Genetic Variation Within the Oxidative Phosphorylation Pathway in Stroke and Alzheimer’s Disease Alessandro Biffi, Mert Sabuncu, Rahul Desikan, Schmansky Nick, David Salat, Jonathan Rosand, Christopher Anderson Epilepsy and Clinical Neurophysiology: Autoimmune Epilepsy, Intraoperative Monitoring, and Corticography P6.335 Stereo-electroencephalography Versus Subdural Grids and Depth Electrode Placements: When to Use Which? Adetoun Abisogun, Zianka Fallil, Ashesh Mehta, Cynthia Harden P6.336 Critical Intraoperative Neurophysiologic Monitoring (IONM) Changes Associated with Patient Positioning Maneuvers Leslie Lee, Sungho Cho, Viet Nguyen, John Ratliff, Jongsoo Park, Jaime Lopez P6.337 Does Intraoperative Neurophysiologic Monitoring (IONM) Cause Delays in Surgical Cases? Forough Ghavami, Viet Nguyen, Scheherazade Le, Leslie Lee, Charles Cho, Richard Jaffe, Jaime Lopez P6.338 Fingerprinting Method for Identifying Spatiotemporal-Frequency Motifs in Electrocorticographic Data. Dan Bernardo, Tim Pluta, Hae Won Shin P6.339 Post Resection Electrocorticography Predicts Seizure Outcome—a Multivariate Logistic Analysis Sonia Krish, Omotola Hope, Giridhar Kalamangalam, Jeremy Slater, Nitin Tandon P6.340 The Predictive Value of Electrocorticography in Patients with Mesial Temporal Lobe Epilepsy Undergoing Selective Amygdalohippocampectomy Aline Herlopian, L Greenfield, Bashir Shihabuddin P6.341 Refractory Status Epilepticus: a Report of Two Cases to Illustrate the Significance of GAD Antibody Ayaz Khawaja, Amy Amara P6.342 NMDA Receptor Encephalitis Presenting as Partial Status Epilepticus. Case Report and Discussion Simona Proteasa, Josiane LaJoie, Joseph Maytal P6.343 Is Rasmussen’s Encephalitis a NMDA Encephalitis? A Case Report and Review of Literature Simona Proteasa, Lines Vargas Collado, Shefali Karkare P6.344 Intravenous Immunoglobulin Therapy for Late-Stage Rasmussen’s Encephalitis: Long-Term Seizure Freedom Rahul Dave, Enrique Serrano Thursday May 1 Atypical Medial Temporal Lobe Dysfunction in Prodromal Alzheimer’s Disease Chiara Cerami, Pasquale Della Rosa, Alessandra Dodich, Giuseppe Magnani, Alessandra Marcone, Andrea Falini, Stefano Cappa, Daniela Perani P6.326 2015 Education Course Proposal Process 2015 Annual Meeting: Washington, DC The AAN invites you to submit an Education Program suggestion for May 16, 2014. To submit your proposal, please visit the 67th Annual Meeting. Proposals for new programs are due by AAN.com/view/SearchAM. Fast, Easy Registration Online · AAN.com/view/AM14111 Thursday, May 30 Current as of 2/13/2014 Frontiers in Neuroscience Plenary Session 9:00 a.m.–12:00 p.m. F ocuses on translational research related to clinical issues of importance. Six physician scientists outline their recent research findings, along with the clinical implications. Moderator: Massimo Pandolfo MD Member, Science Committee; Chair, International Subcommittee Tissue Environments for Brain Repair Using Fixed Circuits to Generate Flexible Behaviors S. Thomas Carmichael, MD, PhD David Geffen School of Medicine at UCLA, Los Angeles, CA Cori Bargmann, PhD Rockefeller University, New York, NY Opportunities and Challenges of Robot Assisted and Facilitated Neurorecovery Advances in Mapping Human Brain Connectivity: The Human Connectome Project Albert Lo, MD, PhD Brown University, Providence VA Medical Center, Providence, RI Bruce R. Rosen, MD, PhD Harvard Medical School, Boston, MA The Nightlife of Astrocytes Network-based Neurodegeneration Maiken Nedergaard, MD, DMSc University of Rochester Medical Center, Rochester, NY William Seeley, MD UCSF, San Francisco, CA For Full Abstracts and Bios for Plenary Speakers Visit AAN.com/view/SearchAM 112 2O14 Scientific Abstract Listing and Annual Meeting Information American Academy of Neurology and American Brain Foundation 2O14 Awards Luncheon Join AAN leaders for lunch honoring top accomplishments in the field from enterprising high school students to world-renowned researchers. Seating is limited. Wednesday, April 30 12:00 p.m.-1:30 p.m. Public Leadership in Neurology Award Winner Ben Utecht NFL star-turned-singer Ben Utecht will receive the American Brain Foundation’s 2014 Public Leadership in Neurology Award for his commitment to spreading the word about how concussions and traumatic brain injury have affected his life. After winning a Super Bowl ring in 2007, his career ended unexpectedly after a traumatic brain injury in 2009. Many saw this as an ending, but Ben saw an opportunity to pursue another lifelong passion—singing. April 26 – May 3, 2014 Philadelphia, PA Thursday, May 1 S44 MS and CNS Inflammatory Disease: Neuroimaging I S45 Cerebrovascular Disease and Interventional Neurology: Rehabilitation, Recovery, and Complications 1:00 p.m. S44.001 Leptomeningeal Contrast Enhancement in Multiple Sclerosis: a Possible Marker of Inflammation in the Subarachnoid Space Daniel Reich, Anuradha Rao, Luisa Vuolo, Martina Absinta, Govind Nair, John Butman, Irene Cortese 1:00 p.m. S45.001 Stroke Survivors with Aphasia May Overestimate Communication Skills: Survivor Versus Caregiver Report Vahid Behravan, James Maniscalco, Darlene Williamson, A. Barrett 1:15 p.m. S44.002 Direct MRI Detection of Impending Plaque Development in MS Martina Absinta, Pascal Sati, Govind Nair, Massimo Filippi, Irene Cortese, Daniel Reich 1:15 p.m. S45.002 The Association Between Meeting Life’s Simple 7 Goals and Mortality After Stroke in the US Michelle Lin, Daniela Markovic, Bruce Ovbiagele, Amy Towfighi 1:30 p.m. S44.003 In Vivo PET Imaging of Activated Microglial Cells Can Be Used to Differentiate Between Inactive and Active Chronic Lesions in Progressive Multiple Sclerosis Laura Airas, Eero Rissanen, Jouni Tuisku, Alex Dickens, Daniel Anthony, Juha Rinne 1:30 p.m. S45.003 The Amphetamine-Enhanced Stroke Recovery (AESR) Trial: Primary Part 1 Results Larry Goldstein, Meheroz Rabadi, Michael Reding, Laura Lennihan, David Good, Alexander Dromerick, John Pura, Gregory Samsa 1:45 p.m. S44.004 Myelin-Related Advanced MRI Demonstrates Different Degrees of Change Between Various White Matter Tracts in MS Shannon Kolind, Irene Vavasour, Alexander Rauscher, Andrew Riddehough, David Leppert, Nicolas Seneca, Yinshan Zhao, Roger Tam, A. MacKay, David Li, Anthony Traboulsee 1:45 p.m. S45.004 Hospital Factors Associated with Feeding Tube Placement for US Stroke Inpatients Benjamin George, Adam Kelly, Eric Schneider, Robert Holloway 2:00 p.m. S44.005 Longitudinal Changes in Myelin Water Fraction in New Multiple Sclerosis Lesions Wendy Vargas, Elizabeth Monohan, Sneha Pandya, Michael Dayan, Thanh Nguyen, Ashish Raj, Susan Gauthier 2:15 p.m. S44.006 Ultra-high-resolution Imaging of Brain-free Water for Rapid Atrophy Assessment in MS Katherine Gao, Govind Nair, Irene Cortese, Alan Koretsky, Daniel Reich 2:30 p.m. S44.007 Intracortical Laminar Pathology in the Motor Cortex Is Associated with Tractographically Connected White Matter Injury in Multiple Sclerosis: a Multimodal 7T and 3T MRI Study. Céline Louapre, Sindhuja Govindarajan, Costanza Giannì, Julien Cohen-Adad, Sean Tobyne, Revere Kinkel, Caterina Mainero 114 2:00 p.m. S45.005 Utilization of In-hospital Palliative Care for Ischemic Stroke Deaths in United States Shah Shreyansh, Yogesh Moradiya, Santosh Murthy 2:15 p.m. S45.006 Subjective Judgments of Physicians and Nurses Are More Accurate Than Formal Clinical Scales in Predicting Functional Outcome After Intracerebral Hemorrhage David Hwang, Cameron Dell, Mary Sparks, Tiffany Watson, Carl Langefeld, Mary Comeau, Jonathan Rosand, Thomas Battey, Sebastian Koch, Mario Perez, Michael James, Jessica McFarlin, Jennifer Osborne, Daniel Woo, Steven Kittner, Kevin Sheth 2:30 p.m. S45.007 Efficacy of Single and Multiple Injections of Human Umbilical Tissue-Derived Cells Following Experimental Stroke in Rats Amjad Shehadah, Jieli Chen, Brian Kramer, Alex Zacharek, Yisheng Cui, Cynthia Roberts, Mei Lu, Michael Chopp 1:00 p.m.–2:45 p.m. S46 Neuromuscular Disease: Genetics, Pathogenesis, and Measures 1:00 p.m. S46.001 Exome Sequencing Identifies PINCH2 Mutations in Early Onset Autosomal Recessive LGMD with Severe Cardiomyopathy and Triangular Tongues Jodi Warman Chardon, Amanda Smith, John Woulfe, Kawan Rakhra, Elena Pena Fernandez, Chandree Beaulieu, Jeremy Schwartzentruber, Cynthia Hawkins, Matthew Harms, Mei Zhang, Jacek Majewski, Dennis Bulman, Kym Boycott, David Dyment 1:15 p.m. S46.002 Founder Mutation in the γ-Sarcoglycan Gene Causes Milder Phenotype of Limb-Girdle Muscular Dystrophy Type 2C (LGMD2C) in the Hispanic Population of Puerto Rico Samiah Al-Zaidy, Vinod Malik, Kelley Kneile, Xiomara Rosales, Julie Gastier-Foster, Peter Kang, Basil Darras, Louis Kunkel, Steven Moore, Robert Pyatt, Jerry Mendell 1:30 p.m. S46.003 Novel Mutation in VCP Causes Charcot-Marie-Tooth Type 2 (CMT2) Phenotype Shawna Feely, Michael Gonzalez, Chris Weihl, Michael Shy, Stephan Zuchner 1:45 p.m. S46.004 Ethoxyquin Prevents Development of Neuropathy in Rodent Models of Diabetic Peripheral Neuropathy and HIV-Associated Neuropathy Ahmet Hoke, Nicole Reed, Jing Zhu 2:00 p.m. S46.005 Monocarboxylate Transporter 1 (MCT1) Is Critical for Regeneration in Peripheral Nerves Brett Morrison, Akivaga Tsingalia, Sylvain Lengacher, Luc Pellerin, Pierre Magistretti, Jeffrey Rothstein 2:15 p.m. S46.006 Amyotrophic Lateral Sclerosis Quality Measures Robert Miller, Benjamin Brooks, Rebecca SwainEng, Robert Basner, Gregory Carter, Patricia Casey, Adam Cohen, Richard Dubinsky, Dallas Forshew, Carlayne Jackson, Edward Kasarskis, Nicholas Procaccini, Mohammed Sanjak, Fredrik Tolin 2:30 p.m. S46.007 NeuroBANK™ and Global Unique Patient Identifier Allow for Secure Collaboration, Data Aggregation and Sharing Alexander Sherman, Igor Katsovskiy, Roger Selsov, Ervin Sinani, Jason Walker, James Berry, Jonathan Katz, Merit Cudkowicz 2O14 Scientific Abstract Listing and Annual Meeting Information S47 Movement Disorders: Huntington's Disease, Ataxia, and Wilson's Disease 1:00 p.m. Presentation of Jon Stolk Award in Movement Disorders for Young Investigators Recipient: Alice Chen-Plotkin, MD Philadelphia, PA 1:15 p.m. S47.002 The Huntington’s Disease-Behavioral Questionnaire (HD-BQ): a New Screening Tool for Behavioral Disturbances in HD Jody CoreyBloom, Andrew Herndon, Elizabeth Breen, Sean Huynh, Paul Gilbert 1:30 p.m. S47.003 Selected Health and Life Style Factors and Time to Phenoconversion in Huntington’s Disease Caroline Tanner, Karen Marder, Shirley Eberly, Kevin Biglan, David Oakes, Ira Shoulson 1:45 p.m. S47.004 Safety and Tolerability of Selisistat for the Treatment of Huntington’s Disease: Results from a Randomized, Double-Blind, Placebo-Controlled Phase II Trial Ralf Reilmann, Ferdinando Squitieri, Josef Priller, Carsten Saft, Caterina Mariotti, Sigurd Suessmuth, Andrea Nemeth, Sarah Tabrizi, Oliver Quarrell, David Craufurd, Hugh Rickards, Anne Rosser, Darpo Borje, Tessari Michaela, Szynol Angieszka, David Fischer, Douglas Macdonald, Ignacio Munoz-Sanjuan, Robert Pacifici, Chris Frost, Ruth Farmer, Bernhard Landwehrmeyer, Goran Westerberg 2:00 p.m. S47.005 A Novel Familial Mutation in the CACNA1A Gene Associated with an Episodic Ataxia Type 2 Phenotype Jessica Tate, Mustafa Siddiqui, Ihtsham Haq 2:15 p.m. S47.006 Treatment of Spinocerebellar Ataxia Type 2 (SCA2) with MOE Antisense Oligonucleotides Daniel Scoles, Gene Hung, Lance Pflieger, Khanh Thai, Frank Bennett, Stefan Pulst 2:30 p.m. S47.007 Complete Neurological Recovery in Wilson Disease: Experience with 100 Consecutive Patients Seen from 2005-2013 Annu Aggarwal, Mohit Bhatt S48 Aging, Dementia, and Cognitive and Behavioral Neurology: MRI Imaging 1:00 p.m. S48.001 Focal Cortical Patterns in Hippocampal Sparing AD Reveal Significant Clinical Differences Melissa Murray, Ranjan Duara, Ashley Cannon, Amanda Liesinger, Owen Ross, Ronald Petersen, Bradley Boeve, Neill Graff-Radford, Dennis Dickson 1:15 p.m. S48.002 Subcortical Rather Than Cortical Microinfarcts Are More Strongly Associated with Cerebral Cortical Atrophy on MRI Ling Zheng, Harry Vinters, Wendy Mack, Michael Weiner, Helena Chui 1:30 p.m. S48.003 Microinfarcts Are as Strongly Related to Dementia as Tangles in the Oldest-Old: the 90+ Study Maria Corrada, Claudia Kawas, Szofia Bullain, Joshua Sonnen 1:45 p.m. S48.004 Pattern of Brain Atrophy Rates on Serial MRI in Autopsy-confirmed Dementia with Lewy Bodies Zuzana Nedelska, Tanis Ferman, Bradley Boeve, Scott Przybelski, Timothy Lesnick, Melissa Murray, Jeffrey Gunter, Matthew Senjem, Glenn Smith, Yonas Geda, Jonathan Graff-Radford, David Knopman, Ronald Petersen, Clifford Jack, Joseph Parisi, Dennis Dickson, Kejal Kantarci 2:00 p.m. S48.005 ApoE4 Worsens Hippocampal CA1 Apical Neuropil Atrophy and Episodic Memory Geoffrey Kerchner, Daniela Berdnik, Jadon Shen, Jeffrey Bernstein, Michelle Fenesy, Gayle Deutsch, Tony Wyss-Coray, Brian Rutt 2:15 p.m. S48.006 The EADC-ADNI Harmonized Protocol for Hippocampal Segmentation on Magnetic Resonance: Evidence of Validity Marina Boccardi, Martina Bocchetta, Clarissa Ferrari, Simon Duchesne, Clifford Jack, Giovanni Frisoni 2:30 p.m. S48.007 Genetic and Neuroanatomic Associations in Sporadic Frontotemporal Lobar Degeneration Corey McMillan, Jon Toledo, Brian Avants, Philip Cook, Elisabeth Wood, Eunran Suh, David Irwin, John Powers, Christopher Olm, Lauren Elman, Leo McCluskey, Gerard Schellenberg, Virginia Lee, John Trojanowski, Vivianna Van Deerlin, Murray Grossman Scientific Sessions 1:00 p.m. S49.001 Prospective Study of Cost of Care at Multidisciplinary Centers Adhering to AAN Amyotrophic Lateral Sclerosis (ALS) Practice Parameters Rup Tandan, Kevin Boylan, Todd Levine, Catherine Lomen-Hoerth, Peter Callas, Kimberly Maginnis, Mary Lyon 1:15 p.m. S49.002 Redesigned Stroke Care for a Value Based World: Better Outcomes, Lower Spending Waimei Tai, Lucy Kalanithi, Jared Conley, Arnold Milstein 1:30 p.m. S49.003 Readmission Rates to the UAMS Inpatient Neurology Services Jay Hinkle, Archana Hinduja 1:45 p.m. S49.004 Social Media and Multiple Sclerosis: An Italian Experience Luigi Lavorgna, Manuela De Stefano, Daniela Buonanno, Eboli Simone, Gallo Antonio, Simona Bonavita, Gioacchino Tedeschi 2:00 p.m. S49.005 Appropriateness of Dopamine Antagonist Prescribing in Hospitalized Patients with Dopamine Requiring Diseases After Implementation of an Automated Prescribing Alert System Marie Morris, Allison Willis, Franklin McCann, Angela Birke, Brad Racette 2:15 p.m. S49.006 High Accordance Rate of Neurologist Referrals for Psychogenic Patients with Expert Opinion at the Movement Disorders Screening Clinic at the Human Motor Control Section of the National Institute of Neurologic Disorders and Stroke Vesper Ramos, Monica Anne Faye Villegas, Alina Esquenazi, Mark Hallett 2:30 p.m. S49.007 Limitations of Quantative EEG Analysis in the Adult ICU. Mirhan Ozbalik, Victor Gonzalez-Montoya, Soundarya Gowda, Lawrence Morton S50 Epilepsy and Clinical Neurophysiology (EEG): Electrophysiology, Imaging and Functional Connectivity S51 Cerebrovascular Disease and Interventional Neurology: Large Vessel Atherosclerotic Disease 1:00 p.m. Presentation of Founders Award 1:00 p.m. Presentation of Michael S. Pessin Stroke Leadership Prize Recipient: Shennan Weiss, MD, PhD New York, NY 1:15 p.m. S50.002 Extra-hippocampal Gray Matter Atrophy in Seizure-free Patients with Temporal Lobe Epilepsy With and Without Hippocampal Sclerosis Marina Alvim, Ana Coan, Clarissa Yasuda, Brunno Campos, Fernando Cendes 1:30 p.m. S50.003 Resection of Ictal Phase Locked HFOs Is Correlated with Outcome Following Epilepsy Surgery Shennan Weiss, Robert Connors, Garrett Banks, Guy McKhann Jr, Binsheng Zhao, Christopher Filippi, Ronald Emerson, Andrew Trevelyan, Catherine Schevon 1:45 p.m. S50.004 Human Mesial Temporal Lobe Single Neuron Dynamics During Recruitment into a Generalizing Seizure Amrit Misra, Xianda Long, Ashwini Sharan, Michael Sperling, Karen Moxon 2:00 p.m. S50.005 Functional Connectivity Between Insula, Hippocampus, and Amygdala Investigated Using Cortico-Cortical Evoked Potentials (CCEPs) Bilal Zonjy, Ayham Alkhachroum, Emine Kahriman, Nuria Lacuey, Jonathan Miller, Hans Luders 2:15 p.m. S50.006 Graph Theory Based Functional Connectivity in Lateralized Temporal Lobe Epilepsy Sharon Chiang, John Stern, Jerome Engel, Harvey Levin, Zulfi Haneef 2:30 p.m. S50.007 Physiologic and Cortical Response to Acute Psychosocial Stress in Left Temporal Lobe Epilepsy Jane Allendorfer, Heidi Heyse, Lucy Mendoza, Jerzy Szaflarski Recipient: Hooman Kamel, MD New York, NY 1:15 p.m. S51.002 Vascular Inflammation Imaging with 18F-FDG PET/CT for In-Stent Restenosis After Intracranial Stent Deployment in a Swine Model Zhong-Song Shi, Zhong Liu, Jin-Shan Wang, Dong-Hong Liu, Xin-Chong Shi, Xiang-Song Zhang, De-Ji Chen, Ying Liu, Yan-Qiu Liu, Qing-Yuan Wang, Lei Feng 1:30 p.m. S51.003 Safe Triage to Acute Versus Delayed Carotid Imaging Is Achievable Using ABCD3 Scores Johansson Elias, Jakob Bjellerup, Per Wester 1:45 p.m. S51.004 Frequency of Occurrence Acute Asymptomatic Ischemic Lesions of Brain After CAS. I. Sinitsyn 2:00 p.m. S51.005 Effect of Carotid Revascularization Endarterectomy Versus Stenting Trial Results on Performance of Carotid Artery Stent Placement and Carotid Endarterectomy in United States Farhan Siddiq, Malik Adil, Ahmed Malik, Saqib Chaudhry, Adnan Qureshi 2:15 p.m. S51.006 The Cost Per Stroke Prevented (CPSP) from Symptomatic Carotid Artery Stenosis in Ontario, Canada David Turkel-Parrella, Airton de Oliveira Manoel, Thomas Marotta, Julian Spears 2:30 p.m. S51.007 Delay in the Diagnosis of Basilar Artery Ischemic Stroke Joseph Burns, Rima Sestokas, Christopher Carr, Helena Lau, Deborah Green, Anna Marisa Cervantes-Arslanian, Rony Salem, Carlos Kase S52 General Neurology III 1:00 p.m. S52.001 Intra-spinal Transplantation of Mesenchymal Stem Cell-Neural Progenitor (MSC-NP) in Patients with Amyotrophic Lateral Sclerosis (ALS) Saeed Shahbeigi, Ehsaun Hamediseresht, Nasser Aghadmi, Reza Bakhshandepour, Abbas Najjari, Forough Nejatollahi, Ghazal Jalilzadeh, Sara Samavati, Maliheh Heydari, Toraj Orang, Somaye Noroozi 1:15 p.m. S52.002 Connecting Invasive and Noninvasive Brain Stimulation Michael Fox, Randy Buckner, Andres Lozano, Alvaro Pascual-Leone 1:30 p.m. S52.003 Autoimmunity to Inhibitory Synaptic Proteins in Stiff-Person Spectrum of Symptoms Eugenia MartinezHernandez, Nuria Gresa-Arribas, Mar Petit-Pedrol, Helena Ariño, Albert Saiz, Francesc Graus, Josep Dalmau 1:45 p.m. S52.004 GCH1 Heterozygous Mutation Identified by Whole-ExomeSequencing as a Treatable Condition in a Patient Presenting with Progressive Spastic Paraplegia Zheng Fan, Robert Greenwood, Ana Felix, Yael ShilohMalawsky, Myra Roche, Kristy Crooks, Jonathan Berg, James Evans 2:00 p.m. S52.005 Confirmed: The Antigen of Paraneoplastic Antibodies Previously Named “anti-Tr” Is Delta/Notch-like Epidermal Growth Factor-related Receptor (DNER) Maxwell Greene, Yongjie Lai, Josep Dalmau, Eric Lancaster 2:15 p.m. S52.006 Aphasia as a Complication of CD19Targeted Chimeric Antigen Receptor Immunotherapy Sarah Kranick, Giao Phan, James Kochenderfer, Steven Rosenberg, Avindra Nath 2:30 p.m. S52.007 Does Therapeutic Hypothermia Affect the Prognostic Accuracy of a Clinical Neurological Examination and SSEP? Dragancea Irina S53 MS and CNS Inflammatory Disease: Biomarkers and Therapeutic Mechanisms 1:00 p.m. S53.001 Following Anti-CD20 Treatment Immune-Competent B Cells Reoccur in Bone Marrow and Spleen Before They Can Be Detected in Peripheral Blood Martin Weber 1:15 p.m. S53.002 B Lymphocytes Induce CNS Pathology Involving Reactive Astrogliosis and Oligodendrocyte Loss in a Murine System and in Human Multiple Sclerosis Leila Jackson, Danielle Harlow, Sean Selva, Tracy Niedzielko, Wendy Macklin, Timothy Vollmer 1:30 p.m. S53.003 Increased CSF Level of Monocyte/ Microgrial Activation Maker in Progressive-Multiple Sclerosis Mika Komori, Andrew Blake, Elena Romm, Yen-Chih Lin, Bibiana Bielekova 1:45 p.m. S53.004 S1P Receptor Modulation by Fingolimod Promotes Human Oligodendrocyte Progenitor Cell Differentiation Through Cell-Autonomous and Non-Cell Autonomous Mechanisms via ERK1/2 and p38MAPK Activation Qiaoling Cui, Timothy Kennedy, Guillermina Almazan, Jack Antel 2:00 p.m. S53.005 Chitinase 3-like 1 and Chitinase 3-like 2 as Diagnostic and Prognostic Biomarkers of Multiple Sclerosis Eric Thouvenot, Geoffrey Hinsinger, Nathalie Galeotti, Nicolas Nabholz, Serge Urbach, Valerie Rigau, Christophe Demattei, Sylvain Lehmann, William Camu, Pierre Labauge, Giovanni Castelnovo, David Brassat, Laplaud DavidAxel, Olivier Casez, Joël Bockaert, Philippe Marin 2:15 p.m. S53.006 Dimethyl Fumarate Utilizes Nrf2-independent and Nrf2dependent Pathways for Immune Modulation Ulf Schulze-Topphoff, Michel Varrin-Doyer, Kara Pekarek, Robert Scannevin, Scott Zamvil 2:30 p.m. S53.007 Antibodies Against the Inward Rectifying Potassium Channel KIR4.1 Precede the Onset of Multiple Sclerosis Viola Biberacher, Rajneesh Srivastava, Sudhakar Reddy Kalluri, Lucas Schirmer, Dorothea Buck, Rebecca Selter, Bernhard Hemmer Fast, Easy Registration Online · AAN.com/view/AM14115 Thursday May 1 S49 Practice, Policy, and Ethics Thursday, May 1 I9 Emerging Concepts in Headache Therapy 1:00 p.m.–5:00 p.m. Coordinators: Andrew H. Ahn, MD, PhD and Morris Levin, MD, FAAN Invited Speaker Session: 1:00 p.m.–3:30 p.m. 1:00 p.m.–1:30 p.m. Pathophysiology of Migraine: New Therapeutic Targets Andrew Charles, MD 1:30 p.m.–2:00 p.m. Critical Challenges in the Diagnosis of Headache Peter Goadsby, MD, PhD 2:00 p.m.–2:30 p.m. Opportunities and Controversies in Headache Medicine Richard B. Lipton, MD, FAAN 2:30 p.m.–3:00 p.m. How Comorbidities Set the Agenda for Headache Therapy Deborah I. Friedman, MD, FAAN 3:00 p.m.–3:30 p.m. Neuromodulation: Increasing the Gain on Headache Therapy Morris Levin, MD, FAAN Poster Rounds: 3:30 p.m.–4:30 p.m. I9-1.001 Patient Satisfaction with MAP0004: Results of an Optional Survey During a Long-term Open-label Safety Study Sheena Aurora, Dawn Buse, Biao Lu, Donald Kellerman, Wade Cooper, Shashidhar Kori I9-1.004 Barriers to Chronic Migraine I9-1.002 Optical Imaging of Facial I9-1.005 Bilateral Pain Perfusion in Migraine Jonas Peterson, Lindsay Hunter, Melissa Cortez, Jeremy Theriot, KC Brennan I9-1.003 Therapeutic Efficacy of Transcranial Direct Current Stimulation in Trigeminal Neuralgia Mark Obermann, Vera Bude, Dagny Holle, Tim Hagenacker, H. Diener, Zaza Katsarava Care: Results of the CaMEO (Chronic Migraine Epidemiology and Outcomes) Study Dawn Buse, Richard Lipton, Michael Reed, Daniel Serrano, Kristina Fanning, Aubrey Manack Hypersensitivity over the Trigeminal Region and Dental Deafferentations in Patients with Classical Trigeminal Neuralgia Nathalie Guy, Béatrice Claise, Pierre Clavelou, Radhouane Dallel I9-1.006 Idiopathic Intracerebral Hypertension (IIH)/pseudotumor: Removing Less CSF Is Best Franchesca Fiorito-Torres, Melissa Rayhill, Michael Perloff I9-1.007 Long Term Therapeutic Response of Sphenopalatine Ganglion (SPG) Stimulation for Cluster Headache— Pathway CH-1 Study Miguel Lainez, Rigmor Jensen, Arne May, Charly Gaul, Anthony Caparso, Amy Goodman, Jean Schoenen I9-1.008 White Matter Microstructure Abnormalities in Paediatric Migraine Patients: In-Vivo Measures of Brain Hyperexcitability? Roberta Messina, Maria Rocca, Bruno Colombo, Elisabetta Pagani, Andrea Falini, Giancarlo Comi, Massimo Filippi I9-1.009 Interictal Reduced Cranial Parasympathetic Tone in Cluster Headache Hilde Karen Ofte, Therese von Hanno, Karl Alstadhaug I9-1.010 Treatment of Withdrawal Headache in Patients with Medication Overuse Headache (MOH): A Randomized, Single-blinded, Placebo Controlled Study Sabina Cevoli, Giulia Giannini, Valentina Favoni, Elisa Sancisi, Marianna Nicodemo, Stefano Zanigni, Daniela Grimaldi, Giulia Pierangeli, Pietro Cortelli Data Blitz: 4:30 p.m.–5:00 p.m. 4:30 p.m. I9-2.001 Mid-life Migraine and Late-life Movement Disorder Symptoms: AGES-Reykjavik Study Ann Scher, G. Ross, Sigurdur Sigurdsson, Melissa Garcia, Larus Gudmundsson, Sigurlaug Sveinbjornsdottir, Vilmundur Gudnason, Lenore Launer 4:35 p.m. I9-2.002 Efficacy and Safety of AVP-825, a Novel Breath-Powered™ Powder Sumatriptan Intranasal Treatment, for Acute Migraine Roger Cady, John Messina, Jennifer Carothers, Ramy Mahmoud 4:40 p.m. I9-2.003 Characterization of Photosensitivity and Pupil Oscillation Rate in Migraine Lindsay Hunter, Jonas Peterson, Melissa Cortez, Jeremy Theriot, K.C. Brennan 4:45 p.m. I9-2.004 4:50 p.m. I9-2.005 Chronic Migraine with Medication Overuse Is Associated with Low Cognitive Reserve Marian Gomez Beldarrain, Ane Anton Ladislao, Urko Aguirre Larracoechea, Alberto Cabrera Zubizarreta, Isabel Oroz, Carlos Garcia-Monco Carra Gammacore Device for Treatment of Migraine Attack: Preliminary Data Licia Grazzi, Susanna Usai, Gennaro Bussone 116 2O14 Scientific Abstract Listing and Annual Meeting Information Integrated Neuroscience Sessions I10 The Global Burden of Neurological Diseases 1:00 p.m.–5:00 p.m. Coordinators: Jerome H. Chin, MD, PhD, MPH and Massimo Pandolfo, MD Invited Speaker Session: 1:00 p.m.–3:30 p.m. 1:00 p.m.–1:15 p.m. Global Health and Neurology Jerome H. Chin, MD, PhD, MPH; Massimo Pandolfo, MD 1:15 p.m.–1:45 p.m. Global Epidemiology of Parkinson’s Disease Walter A. Rocca, MD, MPH 1:45 p.m.–2:15 p.m. Neurocysticercosis and Epilepsy Oscar H. Del Brutto MD, FAAN 2:15 p.m.–2:45 p.m. Cerebrovascular Disease in China Yi-Cheng Zhu, MD, PhD 2:45 p.m.–3:15 p.m. Traumatic Brain Injury: The Neglected Global Epidemic Jerome H. Chin, MD, PhD, MPH 3:15 p.m.–3:30 p.m. Questions and Answers Poster Rounds: 3:30 p.m.–4:30 p.m. I10-1.001 Risk Factors for Epilepsy in Children with HIV/AIDS in Botswana David Bearden, Greg Bisson, Dennis Kolson, Andrew Steenhoff, Sudha Kessler, Dennis Dlugos I10-1.002 Comparing Cognitive Screening Tools in a Rural Ecuadorian Population: The Atahualpa Project Clinton Wright, Hannah Gardener, Mauricio Zambrano, Victor Del Brutto, Oscar Del Brutto I10-1.003 The Risk of Large-artery I10-1.004 Incidence and Mortality I10-1.006Neuro-Developmental I10-1.005 Prevalence, Incidence and I10-1.007 Clinical and Bacteriological of Ischemic Stroke Subtypes in Joinville, Brazil: A Population-based Study Marcos Lange, Norberto Cabral, Carla Moro, Alexandre Longo, Anderson Goncalves, Viviane Zetola, Tatjana Rundek Associations Between APOE Genotype, Cardiovascular Risk Factor and Dementia in Cuban Populations Jorge Jesús Llibre Guerra, Milagros Guerra, Juan Carlos Llibre Guerra, Juan Jesús Llibre Rodriguéz Atherosclerotic Stroke Is Proportionally Greater than Cardioembolic Stroke in HIV-infected Individuals Compared to HIVuninfected Controls Felicia Chow, Richard Price, Priscilla Hsue, Anthony Kim Disorders in India—From Epidemiology to Public Policy Donald Silberberg, Narendra Arora, Vinod Bhutani, Maureen Durkin, Shefalli Gulati, Mkc Nair, Jennifer PintoMartin Features of Central Nervous System Tuberculosis in Patients with HIV-Infection in Siberian Region of Russia Yury Bykov, Tatiana Filippova, Olga Novitskaya I10-1.009 A Phone App to Diagnose Epileptic Seizures: A Useful Tool to Reduce the Epilepsy Treatment Gap in Poorer Countries Victor Patterson, Mamta Singh, Hemav Rajbhandari I10-1.010 Hypertension in Rural Uganda: Findings from a Community-Based Screening Project Jerome Chin I10-1.008 Stroke Mortality and Its Predictors in Nigeria: Results of a HospitalBased Study Kolawole Wahab, Emmanuel Sanya, Babatunde Ademiluyi, Bello Abiodun, Wemimo Alaofin Data Blitz: 4:30 p.m.–5:00 p.m. I10-2.001 The Association Between Meeting Life’s Simple 7 Goals and Mortality After Stroke in the US Michelle Lin, Daniela Markovic, Bruce Ovbiagele, Amy Towfighi 4:35 p.m. I10-2.002 4:40 p.m. I10-2.003 Variations in Brain Death Declaration: A Worldwide Survey Sarah Wahlster, Eelco Wijdicks, Pratik Patel, David Greer, Claude Hemphill, Farrah Mateen Indonesia Stroke Registry Fenny Yudiarto, Mochammad Machfoed, Amir Darwin, Anam Ong, Muhammad Karyana, Siswanto 4:45 p.m. I10-2.004 Helping Haiti: Addressing the Burden of Neurologic Disease Veronica Santini, Anthony Alessi, Elaine Jones, Mill Etienne, Anna Hohler 4:50 p.m. I10-2.005 Performance of Cerebrospinal Fluid (CSF) Plasmodium falciparum Histidine-Rich Protein-2 (pfHRP-2) in Prediction of Death in Cerebral Malaria Kiran Thakur, Jimmy Vareta, Kathryn Carson, Terrie Taylor, David Sullivan, Karl Seydel Fast, Easy Registration Online · AAN.com/view/AM14 117 Thursday May 1 4:30 p.m. Thursday, May 1 P7 Poster Session VII First Authors stand by Posters from 5:00 p.m.–6:30 p.m 3:00 p.m.–6:30 p.m. oster Discussion Session: P Neuromuscular and Clinical Neurophysiology (EMG) II Utilizing a guided tour format, topic experts will lead attendees around the ten posters in the poster discussion session and facilitate questions with poster authors during the 90-minute author stand-by time. P7.001 Deletion of Sarm1 Gene Protects Against Paclitaxel-induced Peripheral Neuropathy Ahmet Hoke, Elliot Turkiew, Nicole Reed P7.002 Frequency and Time to Relapse after Discontinuing 6-month Therapy with Intravenous Immunoglobulin or Methylprednisolone in Chronic Inflammatory Demyelinating Polyradiculoneuropathy Eduardo Nobile-Orazio, Dario Cocito, Stefano Jann, Antonino Uncini, Paolo Messina, Ettore Beghi, Giovanni Antonini, Raffaella Fazio, Francesca Gallia, Angelo Schenone, Ada Francia, Davide Pareyson, Lucio Santoro, Stefano Tamburin, Guido Cavaletti, Fabio Giannini, Mario Sabatelli P7.003 Sudoscan as a Diagnostic Tool for Diabetic and Idiopathic Peripheral Neuropathy A. Smith, Margaret Lessard, J. Singleton P7.004 Defective Muscle Mitochondrial Biogenesis in Spinal Muscular Atrophy. Dario Ronchi, Michela Ripolone, Emanuele Barca, Angela Berardinelli, Lucia Morandi, Marina Mora, Andreina Bordoni, Francesco Fortunato, Gigliola Fagiolari, Raffaella Violano, Dionis Vallejo, Stefania Corti, Antonio Toscano, Monica Sciacco, Salvatore DiMauro, Giacomo Comi, Maurizio Moggio P7.005 Genetic Epidemiology of C9ORF72 in ALS: a National Study in Italy Adriano Chio, Stefania Battistini, Andrea Calvo, Claudia Caponnetto, Francesca Conforti, Massimo Corbo, Fabio Giannini, Jessica Mandrioli, Fabrizio Salvi, Gabriele Mora, Mario Sabatelli, Vincenzo La Bella, Giancarlo Logroscino, Isabella Simone, Maria Monsurrò, Letizia Mazzini, Giuseppe Borghero, Francesco Logullo, Christian Lunetta, Paolo Volanti, Maura Pugliatti, Paola Mandich, Sandra D’Alfonso, Silvana Penco, Marcella Zollino, Maria Murru, Gabriella Restagno P7.006 Increased Cerebral Oxidative Stress in Amyotrophic Lateral Sclerosis: A 62 Cu-ATSM PET Study Masamichi Ikawa, Hidehiko Okazawa, Tetsuya Tsujikawa, Tomoko Muramatsu, Toru Kishitani, Tomoko Kamisawa, Akiko Matsunaga, Osamu Yamamura, Tetsuya Mori, Tadanori Hamano, Yasushi Kiyono, Yasunari Nakamoto, Makoto Yoneda P7.008 P7.007 P7.009 The Diagnostic Value of Diffusion Tensor MRI Metrics in Relation to the MND Phenotype Heterogeneity Edoardo Spinelli, Federica Agosta, Nilo Riva, Massimiliano Copetti, Sebastiano Galantucci, Adriano Chiò, Stefano Messina, Sandro Iannaccone, Andrea Calvo, Vincenzo Silani, Andrea Falini, Giancarlo Comi, Massimo Filippi Muscular Dystrophy Association U.S. Neuromuscular Disease Registry—Preliminary Findings Jodi Wolff, Joline Dalton, Valerie Cwik, Annie Kennedy, Michelle Morgan, Jane Larkindale, Alan Beggs, Joshua Benditt, James Berry, Thomas Crawford, Emily Munson, Rachel Richesson, Jeffrey Rosenfeld, Carly Siskind, Kevin Flanigan The Course and Outcome of Pregnancy in Women with Nondystrophic Myotonias Yuliya Snyder, Colleen DonlinSmith, Eva Pressman, Emma Ciafaloni P7.010 Myasthenia and Risk of Cancer: A Population-based Case-control Study Emil Pedersen, Anton Pottegaard, Jesper Hallas, Soren Friis, Klaus Hansen, Poul Erik Jensen, David Gaist NEW! e Poster Session: Neuro-oncology The ePoster session will feature a selection of posters to be presented digitally, rather than in the traditional format. Authors will be able to take advantage of the format to highlight compelling visual features such as images and videos. See poster map on page 47 for location. P7.011 Differential Sensitivity of Oligodendrocyte Precursor Cells and Microglia to Methotrexate in Grey Versus White Matter Lauren Wood, Sarah Miller, Hannes Vogel, Michelle Monje P7.013 P7.012 Functional Expression of K2P Potassium Channels in Tumor Infiltrating Lymphocytes of Malignant Glioma Ole Simon, Thomas Muentefering, Stefan Bittner, Nico Melzer, Heinz Wiendl, Oliver Grauer, Sven Meuth P7.014 General Neurology VII P7.024 Polyneuropathy in Multiple Myeloma Patients Correlate with the Presence of Autoantibodies Adam Niezgoda, Slawomir Michalak, Lidia Gil, Mieczyslaw Komarnicki, Wojciech Kozubski Development of a Mouse Model of Leptomeningeal Metastasis Adrienne Boire, Lisa DeAngelis, Joan Massagué P7.021 Babinski or Withdrawal? A New Way to Decide Sayyed Sohrab, Douglas Gelb P7.022 P7.025 P7.023 Rare Presentation of Eagle’s Syndrome as Bell’s Palsy Nancy Rosales, Rachana Gandhi, Ramon Lugo 118 Paraneoplastic Neurological Syndromes: A Single Institution 10-Year Case Series Amy Chan, Joachim Baehring P7.017 Delayed Diagnosis of Brachial Plexus Neurolymphomatosis in Post-transplant Patient with Diffuse Large B-cell Lymphoma Milena Stosic, Sudhakar Tummala P7.015WITHDRAWN When the Typical Becomes Atypical: Anti-Ri Antibody Associated Paraneoplastic Syndrome WITHOUT Opsoclonus-Myoclonus Yadira VelazquezRodriguez, Divpreet Kaur, Aiesha Ahmed Absent Inferior Vena Cava with Resulting Venous Congestion Causing Intermittent Cauda Equina Dysfunction Carrie Grouse, Steven Lewis P7.016 Diagnostic Confusion About a Confused Patient: A Case of Delayed Post-Anoxic Leukoencephalopathy Syndrome Tammam Dayyoub, Ahmad Riad Ramadan, Panayiotis Mitsias P7.026 Nutritional Intake and Iron Bioavailability in Adolescents with Postural Tachycardia Syndrome Imad Jarjour, Keli Hawthorne, Steven Abrams P7.027 Restoration of Altered Epigenetic Signature by a Quinoline Compound, S4, (2-(2-methylquinolin-4ylamino)-N-phenyl acetamide), Resulting in Inhibition of Alcohol Drinking Tuhin Banerjee P7.028 Mitochondrial Variants in ALS Kevin Kenna, Russell McLaughlin, Susan Byrne, Marwa Elamin, Colette Donaghy, Daniel Bradley, Orla Hardiman P7.029 Refractory IgG4Related Intracranial Hypertrophic Pachymeningitis Bing Liao, Carlos Kamiya Matsuoka, Xiang Fang, Robert Smith 2O14 Scientific Abstract Listing and Annual Meeting Information P7.018 Non-Richter’s Transformation CLL in the CNS: A Case Series Varoon Thavapalan, Lawrence Kenyon, Moshe Mizrahi P7.019 Photodynamic Therapy (PDT) of Brain Tumors Venu Parachuri, Akshat Katyayan, Harry Whelan P7.020 Primary Central Nervous System Lymphoma in Rheumatoid Arthritis Treated with Leflunomide Andrew Bayat, Jeremy Jones, Harris Naina P7.030 Detecting Malingering: The Honest Palm Sign David Black P7.031 Case Report of Weston Hurst Syndrome Rick Magun, John Provias P7.032 A Case of PML After Initiation of Brentuximab Vedotin for CD30 Positive Cutaneous T Cell Lymphoma Judy Jia, Ethan Goldberg, Joseph Berger, Amy Pruitt Poster Session VII Electroencephalographic and Positron Emission Tomography Correlates in Anti-N-methyl-D-aspartate Receptor Encephalitis David Benavides, John Probasco, Beatriz Wills, Angela Wabulya, Gregory Bergey, Peter Kaplan P7.046 P7.034 P7.047 Extra-motor Symptoms in Amyotrophic Lateral Sclerosis. Analysis of 112 Patients Hector Martinez, Jorge Moreno-Cuevas, María-Teresa GonzalezGarza, Arturo Robles Tenorio, César Escamilla Ocañas, Sergio Salazar Marioni, Ubaldo Martínez P7.035Hyperammonemic Encephalopathy in Late-Onset Ornithine Transcarbamylase (OTC) Deficiency Unmasked by Acetaminophen Overuse Heeral Mehta, Danyel Tacker, Anne Josiah, Paola Pergami P7.036 Picture This! A Meta-Analysis Comparing Affective Salience of Words Versus Images Eithan Kotkowski, Peter Fox P7.037 The Belgian Neuromuscular Disease Registry, Results of the 2012 Data Anna Roy, Philip Van Damme, Peter Van den Bergh, Viviane Van Casteren P7.038 Abnormal Near Field Potentials of Brainstem Origin in Parkinson’s Disease (PD) Fidias LeonSarmiento, Rosanna Sobota, Richard Doty P7.039 CXCL10, CCL5 and IL-6 in Cerebrospinal Fluid of Neuropsychologically Unaffected Patients Correlate with Neurofilament H Simon Faissner, Björn Ambrosius, Norbert Brockmeyer, Gabriele Arendt, Ralf Gold, Thomas Grunwald, Andrew Chan P7.040 Prevalence and Predictors of Suicidal Ideation in Epilepsy and Multiple Sclerosis Leah Dickstein, Amy Nowacki, Adele Viguera Movement Disorders: Deep Brain Stimulation for Parkinson’s Disease P7.041 How Thin Can a Deep Brain Stimulation Lead Be? Zhe Li, Khong Siong Ng, Yan Ye, Xiaoping Li P7.042 Wearable Sensors for Quantifying Deep Brain Stimulation Washout Effects on Gait in Parkinson’s Disease Elizabeth Brokaw, Thomas Mera, David Riley, Benjamin Walter, Alberto Espay, Fredy Revilla, Joseph Giuffrida, Dustin Heldman P7.043 How Optogenetics Can Help Improve Deep Brain Stimulation for the Motor Symptoms of Parkinson’s Disease John Eraifej, Hardev Pall P7.044 Neuronal Oscillation Patterns in the Subthalamic Nucleus in Parkinsonia Patients with Off Dystonia Ping Zhuang, Mark Hallett, Li Xiaoyu, Yuqing Zhang, Jianyu Li, Yongjie Li P7.045 Deep Brain Stimulation (DBS) and Oropharyngeal Dysfunction in Parkinson’s Disease (PD): A Case Report Pichet Termsarasab, Winona Tse Impedance Changes Occur During Threshold Measurements in Deep Brain Stimulation Patients Stephen Carcieri, Martin Reich, Frank Steigerwald, Michael Barbe, Ljubomir Manola, Lars Timmermann, Jens Volkmann Atrophy and the Emergence of Induced Side Effects in Deep Brain Stimulation Daniel Martinez-Ramirez, Takashi Morishita, Pam Zeilman, Michael Okun P7.048 Comorbidities and the Outcome of Deep Brain Stimulation Surgery in Parkinson’s Disease Faisal Alsallom, Hesham Abboud, Gencer Genc, Srivadee Oravivattanakul, Anwar Ahmed, Scott Cooper, Michal Gostkowski, Andre Machado, Hubert Fernandez P7.049 A Multiple-Target DBS Strategy for Parkinson’s Disease. MasaAki Higuchi, Takashi Morishita, Kelly Foote, Kelsey Nestor, Justin Hillard, Michael Okun P7.050 Deep Brain Stimulation of the Nucleus Accumbens Has Positive Effects on Parkinson’s Disease-related Apathy Nolan Williams, Baron Short, Emily Williams, Alexandra Jeffery, Suzanne Kerns, Gregory Sahlem, Colleen Hanlon, Gonzalo Revuelta, Istvan Takacs, Mark George Movement Disorders: Surgical Approaches to Parkinson’s Disease P7.051 Acute Lower Urinary Tract Dysfunction After Bilateral STN Deep Brain Stimulation Surgery for PD: Case Reports and Literature Review Richard Salazar, Toby Chai, Paul Fishman, Howard Eisenberg, Stephen Reich P7.052 Determinants of the Frequency of Post-Operative DBS Office Visits Justin Martello, Melissa Armstrong, Ann Gruber-Baldini, Erik Barr, Stephen Reich, Paul Fishman, Lisa Shulman P7.053 Contextual Regulation of Simple Decisions in Parkinson’s Disease: Effects of STN-DBS and L-Dopa Miguel Ulla, Philippe Domenech, Valentin Wyart, Laetitia Silvert, Jean Claude Dreher, Franck Durif P7.054 Interleaving Could be a Better Programming Technique for Parkinson’s Disease and Dystonia Patients Denny Reyes, Michelle Ferreira, Nestor GalvezJimenez, Tarannum Khan P7.058 Impact of Socioeconomic Status on Outcome of Deep Brain Stimulation Surgery for Parkinson’s Disease Gencer Genc, Hesham Abboud, Srivadee Oravivattanakul, Faisal Alsallom, Nicholas Thompson, Scott Cooper, Michal Gostkowski, Andre Machado, Hubert Fernandez P7.059 Effect of Dorsal and Ventral Subthalamic Nucleus Deep Brain Stimulation on Actual and Perceived Sense of Postural Balance Travis Larsh, Jonathan Eskenazi, Enrique Urrea Mendoza, Ashutosh Mani, Amit Bhattacharya, Andrew Duker, Cyndy Cox, Maureen Gartner, Fredy Revilla P7.060 Dorsal and Ventral Subthalamic Nucleus Deep Brain Stimulation Induced Cerebral Blood Flow and Motor Responses Mwiza Ushe, Meghan Campbell, Samer Tabbal, Morvarid Karimi, Johanna Hartlein, Tamara Hershey, Joel Perlmutter Movement Disorders: Dystonia Treatment Movement Disorders: Treatment of Parkinson’s Disease and Other Disorders P7.070 Mayo Clinic Florida Collection of Human Skin Fibroblast Cultures from Patients with Hereditary Neurodegenerative Disorders Zbigniew Wszolek, Pawel Tacik, Shinsuke Fujioka, Audrey Strongosky, Jing Zhao, Takahisa Kanekiyo, Guojun Bu P7.071 P7.072 Cervical Dystonia Patient Registry for Observation of OnabotulinumtoxinA Efficacy (CD PROBE): Treatment Patterns and Subject Disposition P. Charles, Joseph Jankovic, Cynthia Comella, Mark Stacy, Marc Schwartz, Aubrey Manack, Mitchell Brin P7.063ANCHOR-CD (AbobotulinumtoxinA Neurotoxin: Clinical and Health Economics Outcomes Registry in Cervical Dystonia): A Multicenter, Observational Study of Dysport in Cervical Dystonia: Baseline Data and Cycle One Efficacy Data Daniel Truong, Richard Trosch, Cynthia Comella, Jack Chen, Dominic Marchese, Chandra Abbott, Wes Cetnarowski, Alberto Espay P7.064 Clinical Audit of the Efficacy of Xeomin Against Dysport for the Treatment of Dystonia Daveena Meeks, Christopher Clough P7.065 P7.066 Globus Pallidus Versus Subthalamic Nucleus Deep Brain Stimulation For Parkinson’s Disease: A Meta-Analysis Michele Tagliati, Valentina Pecoraro, Giuseppe Rengo, Cristina Motto, Lorenzo Moja, Gennaro Pagano Treatment Outcomes in Cervical Dystonia Patient Registry for Observation of OnabotulinumtoxinA Efficacy (CD PROBE) Joseph Jankovic, Charles Adler, P. Charles, Cynthia Comella, Mark Stacy, Marc Schwartz, Aubrey Manack, Mitchell Brin P7.062 P7.056 P7.057 P7.069 Response to IncobotulinumtoxinA After Resistance to OnabotulinumtoxinA and RimabotulinumtoxinB Vesper Ramos, Barbara Karp, Codrin Lungu, Katharine Alter, Mark Hallett P7.061 Concurrent Bilateral Vim and STN DBS in a Patient with ET/ PD Subhashie Wijemanne, Olga Waln, Joohi Jimenez Shahed Comparison of Screening Tools for Assessing Deep Brain Stimulation Candidacy in Parkinson Disease Kelvin Chou, Robert Coleman, Parag Patil, Vikas Kotagal Stability of Botulinum Toxin A Dosage Over Time in Patients with Hemifacial Spasm, Blepharospasm and Cervical Dystonia/Torticollis. Shira McMahan, Denny Reyes, Tarannum Khan Changes in Troublesome Dyskinesia and its Relationship with Dose in Advanced Parkinson’s Disease Patients Treated with Levodopa-Carbidopa Intestinal Gel Infusion Angelo Antonini, Victor Fung, James Boyd, John Slevin, Coleen Hall, Jordan Dubow, Krai Chatamra, Janet Benesh The Retrospective Evaluation of the Dose of IncobotulinumtoxinA and OnabotulinumtoxinA for the Clinical Management of Cervical Dystonia and Blepharospasm: TRUDOSE Pilot Study Charalampos Tzoulis, Ruth Kent, Adrian Robertson, John Maltman, Chris Purdy, Raf Magar P7.055 P7.068 Deep Brain Stimulation In Patients with Primary Dystonia with GNAL Mutation: A Case Series Harini Sarva, Richard Trosch, Amanda Glickman, Deborah Raymond, Laurie Ozelius, Susan Bressman, Rachel Saunders-Pullman P7.067 Patient experience of Botulinum toxin injections for dystonia and hemifacial spasm: knowledge of diagnosis and treatment David Grosset, Elaine Tyrrell, Katherine Grosset, Donald Grosset Apomorphine Improves Morning Akinesia in Parkinson’s Disease: Interim Analysis of the AM-IMPAKT Trial Stuart Isaacson, William Ondo, Fernando Pagan P7.073 Approach to Treatment of Depression in Parkinson’s Disease: Results from NPF-QII Peter Schmidt, Mark Guttman, Laura Marsh, John Nutt, Tanya Simuni, Eugene Nelson, Jorge Zamudio, Michael Okun P7.074 Pathophysiological Decrease in the Regional Cerebral Blood Flow in Pure Autonomic Failure with Lewy Body Tomoko Kamisawa, Masamichi Ikawa, Yuki Saito, Tomoko Muramatsu, Akiko Matsunaga, Osamu Yamamura, Tadanori Hamano, Shigeo Murayama, Yasunari Nakamoto, Hidehiko Okazawa, Makoto Yoneda P7.075 Complicated Hereditary Paraplegia with Novel B4GALNT1 Mutations Expanding, the Phenotype and Genotype Saeed Bohlega, Salma Wakil, Dorota Monies, Edward Cupler, Layla Bastaki, Brian Meyer P7.076 Spinal Cord Atrophy in Hereditary Spastic Paraplegia Caused by SPG4 Mutations Lucas Branco, Lamas Gustavo, Felipe Bergo, Iscia Lopes-Cendes, Marcondes Franca, Jr. P7.077 Cerebral Damage in SPG4Hereditary Spastic Paraplegia (HSP): a VBM Study Gustavo Lamas, Cynthia Bonilha Da Silva, Thiago Rezende, Iscia Lopes-Cendes, Marcondes Franca, Jr. P7.078 A Novel Objective Brain MRI Assessment Scale for Wilson disease (MAS for WD) Annu Aggarwal, Mihir Munshi, Darshana Sanghvi, Amruta Ravan, Saloni Parekh, Pooja Rane, Mohit Bhatt Fast, Easy Registration Online · AAN.com/view/AM14 119 Thursday May 1 P7.033 Thursday, May 1 P7.079 Dystonia in Machado-Joseph Disease (MJD/SCA3) Is Associated with Thalamic and Brainstem Atrophy Alberto Martinez, Marcelo Nunes, Thiago Rezende, Rachel Guimarães, Anelyssa D’Abreu, Iscia Lopes-Cendes, Marcondes Franca, Jr. Movement Disorders: Parkinson’s Disease Therapy P7.080 IPX066 Dose Conversion from Immediate-Release Carbidopa-Levodopa, Carbidopa-Levodopa+Entacapone, and Controlled-Release Carbidopa-Levodopa in Patients with Advanced Parkinson’s Disease (PD) Ann Hsu, Sarita Khanna, Sherron Kell, Robert Rubens, Suneel Gupta P7.081 Long-term Safety and Maintenance of Efficacy from an Openlabel Extension of the Double-blind Pivotal Study of Levodopa-carbidopa Intestinal Gel (LCIG) in Advanced Parkinson’s Disease Patients Hubert Fernandez, Rejko Krueger, John Slevin, Coleen Hall, Susan Eaton, Jordan Dubow, Krai Chatamra, Janet Benesh P7.082 Improved Motor Performance Associated with Smoother Levodopa Time-Concentration Profiles with DM-1992, a Gastroretentive, Extendedrelease Carbidopa/Levodopa Tablet, in Patients with Advanced Parkinson’s Disease Leonard Verhagen Metman, Natividad Stover, Cuiping Chen, Verne Cowles, Michael Sweeney P7.083 Safety Analyses from Openlabel Clinical Trials of Levodopa-Carbidopa Intestinal Gel in Patients with Advanced Parkinson’s Disease: Events Not Related to Device or Procedure Anthony Lang, Sylvain Chouinard, Cindy Zadikoff, Weining Robieson, Jordan Dubow, Krai Chatamra, Janet Benesh P7.084 OPTIPUMP: Different Treatment Strategies Using Continuous Apomorphine Pump Therapy in Parkinsonian Patients and Their Influence on Patient Quality of Life. A French 6 Month, 145 Patients, Propective, Multicentre, Observational Study Sophie Drapier, Marc Verin, David Devos, Alexandre Eusebio, Emmanuel Roze, Bertrand Degos, Caroline Moreau, Jean Azulay, Francois Viallet, Luc Defebvre, Christine BrefelCourbon, Christine Tranchant, Valérie Fraix, Sébastien Woynar, David Andrieu, Adrien Borsik, Laetitia Mauger, Franck Durif P7.085 Gastrointestinal Safety of the Levodopa-Carbidopa Intestinal Gel Delivery System in Treating Advanced Parkinson’s Patients Michael Epstein, David Johnson, Robert Hawes, Nathan Schmulewitz, Arvydas Vanagunas, Susan Eaton, Krai Chatamra, Weining Robieson, Janet Benesh P7.086 A Novel Approach to Treating Impulse Control Disorders (ICDs) in Parkinson’s Disease (PD)—a Case Series John Liang, Mark Groves, Vicki Shanker 120 P7.087 Phase-3 Clinical Trials of Adjunctive Therapy with Preladenant, an Adenosine 2a Antagonist, in Patients with Parkinson’s Disease Robert Hauser, Fabrizio Stocchi, Olivier Rascol, Susan Huyck, Xianwei Ha, Rachel Capece, Kenneth Wolski, Tony Ho, Peter Sklar, Christopher Lines, David Michelson, David Hewitt P7.088 Post-hoc Analyses of Phase-3 Data with Preladenant, an Adenosine 2a Antagonist, in Patients with Parkinson’s Disease Olivier Rascol, Robert Hauser, Fabrizio Stocchi, Xianwei Ha, Rachel Capece, Kenneth Wolski, Tony Ho, Peter Sklar, Christopher Lines, David Michelson, David Hewitt, Susan Huyck Neuromuscular Disease: Therapy P7.089WITHDRAWN P7.090 The Effect of Intravenous Immunoglobulin on Regulatory T Cells and Disability Progression in Patients with Chronic Inflammatory Demyelinating Polyradiculoneuropathy Jason Thonhoff, Luis Lay, Sharon Halton, David Beers, Ericka Simpson P7.091 Anti-TNF Alpha-induced Neuropathies Pinelopi Tsouni, Olivier Bill, David Benninger, Francois Ochsner, Thierry Kuntzer P7.092 Multicentre, Randomised, Open-label Trial to Compare Efficacy and Tolerance of Prednisone and IVIG in Patients with CIDP on a One-year FollowUp Jean-Philippe Camdessanche, Karine Ferraud, Emmeline Lagrange, Karine Viala, Victor Chan, Nathalie Guy Renouil, Sarah Louis Leonard, Andoni Echaniz-Laguna, Gerard Besson, Francoise Bouhour, Emilien Delmont, Agnes Fromont, Julien Gallard, Armelle Magot, Guillaume Nicolas, David Uzenot, Blanc-Lassere Karine, Tanya Stojkovic, Sandrine Wiertlevski, Boutte Celia, Jean-Christophe Antoine P7.093 Small Fiber Neuropathy in Sarcoidosis: The Cleveland Clinic Experience Zubair Ahmed, Jinny Tavee, Daniel Culver, Joseph Parambil P7.094 Effect of Agmatine Sulfate on Neuropathic Pain Vahid Tohidi, Bahareh Hassanzadeh, Karna Sherwood, Wei Ma, Michael Rosenberg, Varda Gilad, Gad Gilad P7.095 Assessment of 2 Patients with Myotonia Congenita Following Intravenous Lidocaine Treatment Saugat Dey, David Roshal, Luisa Rojas, Robert Schwartzman, Anahita Deboo, Terry Heiman-Patterson P7.096 Angiotensin Receptor Blockade Can Ameliorate Peripheral Nerve Inflammation in Experimental Autoimmune Neuritis Toshiki Fujioka, Hisao Kitazono, Wataru Hagiwara, Masashi Inoue, Shingo Konno P7.097 Agomelatine Increases Muscle Strength and Reduces the Expression of Inflammatory Cytokines in mdx Dystrophic Mice Alzira Carvalho, Vinicius Tondato, Larissa Iamnhuk, Fernanda Gomiero, Giuliana Petri, Pamela Delgado, Beatriz Alves, Fernando Fonseca, David Feder 3:00 p.m.–6:30 p.m. P7.098 Assessment of Bulbar Function in ALS Clinical Trials Richard Smith, Gary Pattee, Erik Pioro, David Schoenfeld Neuromuscular Health Services/ Outcomes Research P7.099 Ig Treatment Outcomes Assessment and Clinical Guidelines Study (the “INSIGHTS Study”): Preliminary Findings on Scope of Practice from the INSIGHTS Database Todd Levine, Jonathan Katz, Richard Barohn, Tahseen Mozaffar, Gil Wolfe, David Saperstein, Lara Katzin, Mazen Dimachkie, Elissa Ritt, Leslie Vaughan, Michelle Greer P7.100 Trends in Outcome and Cost of Hospitalization of Elderly Myasthenia Gravis Patients from 1992 to 2009 Data from Nationwide Inpatient Survey (NIS)1997-2009 Andrew Ji, Ankit Pahwa, Nizar Souayah P7.101 Racial and Ethnic Differences Across Amyotrophic Lateral Sclerosis (ALS) Cases from Three State and Eight Metropolitan Area Surveillance Projects Lindsay Rechtman, Heather Jordan, Laurie Wagner, D. Kevin Horton, Wendy Kaye P7.102 Profile of Medical Care Costs in Patients with Amyotrophic Lateral Sclerosis in Medicare Program and Under Commercial Insurance Lisa Meng, Scott Jordan, Amy Bian, Jinsy Andrews, Jeremy Shefner, Andrew Wolff, Helen Blumen, Kosuke Iwasaki, Bruce Pyenson P7.103 Is Intravenous Immunoglobulin More Cost Effective Than Plasmapheresis in Treatment of Pediatric Myasthenia Gravis Patients? Data from Kids’ Inpatient Database (KID) and Nationwide Inpatient Sample (NIS) Ankit Pahwa, Rania Elenein, Nizar Souayah P7.104 The Safety Profile of Home Infusion of Intravenous Immunoglobulin in Neuroimmunological Disorders Ankit Pahwa, Melissa Allan, Shari O’Connor, Kelly Corl, Nizar Souayah P7.105 Trends in Outcome and Cost of Hospitalization of Adult Myasthenia Gravis. Data Analysis from Nationwide Inpatient Survey (NIS) from 1992 to 2009 Wenzhuan He, Weizhen Wang, Anshul Saxena, Hafiz Khan, Ankit Pahwa, Nizar Souayah P7.106 ALD Connect, an Allinclusive Consortium to Improve Care and Drug Discovery for X-Linked Adrenoleukodystrophy Florian Eichler, Ben Lenail, Keith van Haren, Ali Fatemi, Anthony Gonzalez, Gerald Raymond, Leila Jamal, Joshua Bonkowsky, Sanjay Magavi, John Fink, Tara O’Meara, Robert Brown, Amber Salzman, Alexander Sherman P7.107 Con-focal Microscopy Documents Significant Epidermal Nerve Demyelization in Patients with Clinical Neuropathy But Normal Neurophysiologic Studies Amiram Katz 2O14 Scientific Abstract Listing and Annual Meeting Information P7.108 Validation of Diseasespecific Patient Reported Outcomes in the Home Environment Gretchen Ayer, Lisa Christopher-Stine, Shafeeq Ladha, Tahseen Mozaffar, Yuen So, Michael Hehir, Nicholas Silvestri Neuromuscular Outcome Measures P7.109 Axonal GBS in a Midwest Medical Center; Clinical Characteristics and Outcome Muna Irfan, Pezhman Roohani, Ezgi Tiryaki P7.110 Recommended Cut-off Values for Diagnosis of Carpal Tunnel Syndrome Using Ultrasonography in Females Ha Ra Jeon, Jung Bin Shin, Seong Woo Kim, Hyoung Seop Kim, Ji Sung Hong, Da Wa Jung, Da Sol Ha, Hyo In Kim, Jin Hyoung Lee P7.111 Efficacy and Safety of Home Infusion of Intravenous Immunoglobulin in Multifocal Motor Neuropathy: A Longitudinal Study. Gretchen Ayer, Nizar Souayah P7.112 Efficacy and Safety of Video Assisted Thoracoscopic Surgery Thymectomy for Myasthenia Gravis With and Without Thymoma: A Comparative Study Deepa Dash, V. Goyal, A. Kumar, G. Shukla, M. Behari P7.113 A Retrospective Analysis of Patient-reported Outcomes for 34 Patients with Stiff Person Syndrome Receiving Home IVIG Infusions. Shafeeq Ladha, Gretchen Ayer, Nizar Souayah P7.114 Electrophysiological Motor Unit Function in SMNΔ7 Mice Following SMN Restoration William Arnold, Vicki McGovern, Xiaohui Li, Arthur Burghes P7.115 Neuropathy Signs and Tests in Therapeutic Trials of Transthyretin Amyloidosis Polyneuropathy Narupat Suanprasert P7.116 Retrospective Review of Patients with Sciatic Nerve Palsy After Total Joint Arthoplasty Teena Shetty, Erin Manning, Kelianne Cummings, Christine Villegas, Niesha Voigt, Maxwell Singer, Joseph Nguyen P7.117 Perceived Fatigue and Physiological Fatigue in Spinal Muscular Atrophy (SMA): Are They Related? Sally Dunaway, Jacqueline Montes, Samantha Kramer, Bernadette Podwika, Ashwini Rao, Darryl De Vivo Cerebrovascular Disease and Interventional Neurology: Issues in Acute Stroke Treatment P7.118 The Discharge Modified Rankin Scale Score Correlates with Established Hemorrhagic Transformation Scores in Ischemic Stroke Patients Treated with Thrombolysis David Asuzu, Karin Nystrom, Janet Halliday, Charles Wira, David Greer, David Pritchard, Joseph Schindler, Kevin Sheth Poster Session VII P7.119 Predictors of Hemorrhagic Transformation of Acute Ischemic Stroke: Prospective Validation of a Hemorrhage Risk Model Elisabeth Marsh, Rafael Llinas, Argye Hillis, Rebecca Gottesman P7.120 The Western States Stroke Consortium Telestroke Project Gene Sung, Bart Demaerschalk, Christopher Fanale, Jennifer Majersik, Matthew Grantz, Nobl Barazangi, Dan Capampangan P7.132 Perception of Stroke Symptoms and Utilization of Emergency Medical Systems in Argentina Maximiliano Hawkes, Ismael Calandri, Mauricio Farez, Julieta Arena, Virginia Pujol Lereis, Sebastian Ameriso P7.133 Awareness of Stroke and Knowledge of its Warning Signs and Risk Factors in a Developing Country Omer Sokrab, Ahmed Sokrab, El Fadil Hassan P7.121 “Tele” Phone Medicine—Is Hearing Enough? Rebecca Sugg, Milner Jessica, Alexander Auchus P7.134 P7.122 P7.135 Why Ischemic Stroke Patients Do Not Receive Thrombolytic Treatment? Sourabh Lahoti, Jessica Lee P7.123 Intravenous Thrombolysis Resulting in Acute Ischemic Stroke Recanalization Can Lead to Cerebral Hyperperfusion Syndrome Jonathan Ong, Leonard Yeo, Eric Ting, Arvind Sinha, Hock Luen Teoh, Bernard Chan, Chee Seong Seet, Vijay Sharma P7.124 Cerebral Ischemic Events Associated with Intravenous Thrombolytic Administration in International Joint Efficacy Comparison of Thrombolytics (INJECT) Trial Nudrat Tasneem, Malik Adil, Muhammad Suri, Adnan Qureshi P7.125 A Smartphone Application to Aid in the Evaluation, Treatment, and Clinical Trial Enrollment of the Acute Stroke Patient Claude Nguyen, Tzu-Ching Wu, Andrew Barreto, James Grotta, Sean Savitz Cerebrovascular Disease and Interventional Neurology: Barriers and Opportunities in Acute Stroke Treatment Stroke Awareness in Aseer Region, Community Based Cross Sectional Study Adel Alhazzani Stroke Awareness Among Community Residents in Chicago Subin Mathew, Kathleen O’Neill, Heather Beckstrom, Fredrick Giles, Neelum Aggarwal, Shyam Prabhakaran Cerebrovascular Disease and Interventional Neurology: Intracerebral Hemorrhage Outcome and Mortality P7.136 Hyperacute Neurologic Changes and Outcome after Intracerebral Hemorrhage Matthew Maas, Michael Berman, James Guth, Eric Liotta, Shyam Prabhakaran, Andrew Naidech P7.137 Body Mass Index and Intracerebral Hemorrhage Stephanie Holmes, Rajeev Garg, James Conners, Vivien Lee P7.138 Predictors of Inpatient Mortality After Intracerebral Hemorrhage. Analysis of US Nationwide Inpatient Sample Database. Vijayakumar Javalkar, Robert Schwendimann, Anil Nanda P7.139 Where Are Opportunities to Increase Intravenous Thrombolysis in Current Practice? George Koch, Nancy Kung, Dushyant Damania, Minal Jain, Anunaya Jain, Curtis Benesch, Babak Jahromi Being Overweight or Obese Is Associated with Lesser Disability After Intracerebral Hemorrhage Neha Dangayach, Gian Marco De Marchis, Harpreet Grewal, Rachel Bruce, Aarti Chhatlani, Christina Falo, E. Sander Connolly, Sachin Agarwal, Jan Claassen, Michael Schmidt, Stephan Mayer P7.127 P7.140 P7.126 Intravenous Thrombolysis Onset to Treatment Time Has a Small Effect on In-hospital Outcomes in Acute Ischemic Stroke Konark Malhotra, Santosh Ramanathan, Chris Hackett, Matt Quigley, Melissa Tian, Jack Protetch, Crystal Wong, David Wright, Ashis Tayal P7.128 Modified Helsinki Model Reduced Stroke Thrombolysis Delays in a Resource Limited, Non-Metropolitan Australian Hospital (RLNMAH) Nirosen Vijiaratnam, Elizabeth Mackey, Hans Tu, Zelko Matkovic, Tissa Wijeratne Risk Factors and Outcomes of Prolonged Hospitalization After Intracerebral Hemorrhage in United States Yogesh Moradiya, Santosh Murthy, Shreyansh Shah, Sneha Modi P7.141 Antiplatelet Drugs Resumption After Antiplatelet-Related Intracerebral Hemorrhage In Chinese Kay Cheong Teo, Gary Lau, Raymand Lee, Richard SK Chang, David CW Siu, Gilberto KK Leung, Raymond Cheung, Shu Leong Ho, Koon Ho Chan P7.142 An Initiative to Improve Door to Needle Time for Stroke Thrombolysis in Chicago Shyam Prabhakaran, Kathleen O’Neill Warfarin Associated Intracerebral Hemorrhage in Hong Kong Chinese Kay Cheong Teo, Neeraj R Mahboobani, Raymand Lee, David CW Siu, Raymond Cheung, Shu Leong Ho, Gary KK Lau, Koon Ho Chan P7.130 P7.143 P7.129 Quality Improvement Project: Improving the Time To Treatment in Inpatient Acute Ischemic Stroke John Liang, Rocio Garcia Santibanez, Amy Walker, Irene Boniece P7.131 The Presence of Neurology Impacting Door to Needle Time in Acute Stroke Donna Kurowski, Oscar Soto Blood Transfusion Does Not Improve Outcomes in Patients with Spontaneous Intracerebral Hemorrhage Wazim Mohamed, Sanath Reddy, Sanjeev Sivakumar, Gregory Norris, Mohammad Ibrahim P7.144 Seasonal Variation in the Incidence and Mortality of Intracerebral Hemorrhage. Anand Patel, Archana Hinduja, Jamil Dibu, Eugene Achi, Rajan Patel P7.145 Intracerebral Hematoma Volume Measurement Using ITK-SNAP Software: Initial Experience Monika Mishra, Priyank Shukla, Aakash Bodhit, Ganesh Asaithambi, Arnaldo Velez, Christian Rosado, Mohit Mishra, Pradeepan Saravanapavan, S Khan, V Reddy, Vishunmurthy Hedna Cerebrovascular Disease and Interventional Neurology: Predictors of Outcome After Ischemic Stroke P7.146 Natural Autoantibodies in the Serum of Post-stroke patients with Different Clinical Outcomes Alla Guekht, Eugene Gusev, Vera Alferova, Natalia Gulyaeva, Alexander Poletaev, Alexander Yakovlev P7.147 Impact of Stroke Location on Stroke Outcome Archana Hinduja, Kaustubh Limaye, Anand Patel, Zabeend Mahuwala P7.148WITHDRWN P7.149 Predictors of Outcome in Patients with Acute M2 Occlusion Muhib Khan, Jiaying Zhang, Majaz Moonis, Richard Goddeau, Nils Henninger P7.150 Elderly Non-Demented Patients Have Better Outcome with Reperfusion Therapy Than Demented Patients Following Ischemic Stroke Neeta Duggal, Trenton Myers, James Kim, Iftekhar Ahmed P7.151 Diastolic Function of Heart and Outcomes After Ischemic Stroke Ahn Hee Seung, Ryu Wi-Sun P7.152 Combined Elevation of FVIII and von Willebrand Factor Predicts Risk for Worse Outcomes in Patients with Acute Ischemic Stroke (AIS) Alyana Samai, Dominique Monlezun, Jr, Alexander George, Lauren Dowell, Laurie Schluter, Ramy El Khoury, Sheryl Martin-Schild P7.153 Leukoaraiosis Is Associated with Impaired Functional Recovery and Outcome After Mild Ischemic Stroke. Sanjeeva Onteddu, Artin Minaeian, Richard Goddeau, Nils Henninger P7.154 Does the Magnitude of the Electrocardiogram QT Interval Dispersion Predict Stroke Outcome? Yitzchok Lederman, Leah Steinberg, Clotilde Balucani, Charles Philip, Jason Lazar, Jeremy Weedon, Gautam Mirchandani, Giovanna Viticchi, Lorenzo Falsetti, Mauro Silvestrini, James Gugger, David Aharonoff, Pirouz Piran, Zachary Adler, Steven Levine P7.155 Areas of Cerebral Ischemia Have Increased Propensity to Convert to Infarct Among Diabetics Wazim Mohamed, Sanath Reddy, Pratik Bhattacharya Cerebrovascular Disease and Interventional Neurology: Post-Stroke Function P7.156 Return to Driving Following Stroke Shelly Ozark, Andrea Boan, Tanya Turan, Charles Ellis, Daniel Lackland, David Bachman P7.157 Evaluation of Sexual Functions of Women with Stroke Haluk Gumus, Halim Yilmaz, Sema Yilmaz P7.158 NIHSS Score May Help Predict Health Literacy Levels After Acute Ischemic Stroke Kalina Sanders, Carmen Smotherman, Scott Silliman P7.159 Dysphagia in Patients with Acute Ischemic Stroke Mohamed AlKhaled, Christine Matthis, Georg Royl P7.160 Relative Importance of Stroke Sequelae According to Patients and Caregivers. Victor Urrutia, Brenda Johnson, Argye Hillis P7.161 BMI Impact in Neurological Diseases Jora Xhaxho, Sokrat Xhaxho, Drini Dobi, Jera Kruja P7.162 The Association of Clinical Factors and Highly-Sensitive C-Reactive Protein (hsCRP) with Depression in Stroke Patients Ahmed Itrat, Sandra Griffith, Nicolas Thompson, George Tesar, Irene Katzan P7.163 Proteomics Reveals the Dysregulation of Lipid Metabolism in the Plasma of Post Stroke Depression Patients Jun Mu P7.164 Correlation of NIH Stroke Scale Change and Vascular Risk Factors in Acute Stroke Patients Prashanth Krishnamohan, Michael Dobbs Cerebrovascular Disease and Interventional Neurology: Carotid Disease P7.165 Rates and Predictors of Five Year Survival in Asymptomatic Medicare Beneficiaries Undergoing Carotid Revascularization Muhammad Suri, Saqib Chaudhry, Adnan Qureshi P7.166 Influence of CREST on CEA and CAS Trends in Women—do the Results Matter? Shahram Khalid, Sanath Reddy, Seemant Chaturvedi, Kumar Rajamani, Pratik Bhattacharya, Navid SerajiBozorgzad P7.167 Carotid Artery Stent Placement and Carotid Endarterectomy in Patients with Dialysis Dependent Renal Failure Malik Adil, Fahad Saeed, Adnan Qureshi P7.168 Basilar TIAs of Symptomatic Carotid Artery Stenosis Felix Veloso P7.169 Symptomatic Carotid NearOcclusion with String Sign Incurs a Very High Risk of Stroke Elias Johansson, Per Wester P7.170 Carotid Artery Stenosis and Randomized Controlled Trials—Should We Abandon the Gold Standard Akshal Patel, Gary Gronseth, Michael Glantz Fast, Easy Registration Online · AAN.com/view/AM14121 Thursday May 1 First Authors stand by Posters from 5:00 p.m.–6:30 p.m Thursday, May 1 P7.171 Early and Long-term Outcome After Carotid Endarterectomy Is Determined Not by Coexisting Traditional High Risk But by Risk of Coronary Heart Disease Only Sung Hyuk Heo, Hyojung Nam, Jinsan Lee, Dae-Il Chang, Seon Hee Bu P7.172 Are Carotid Artery StenosisIsolated and Carotid Artery-Plus Two Distinct Entities? Vishal Jani, Adil Malik, Syed Hussain, Adnan Qureshi P7.173 Pituitary Apoplexy: An Unusual Complication of Carotid Endarterectomy Sandrine Jeangette, Denis Bataille, Guy Bruninx, Christo Chaskis, Raphael Hourez P7.174 Association of Resting Heart Rate with Cerebrovascular Risk Factors and Carotid Artery Stenosis. Syed Hussain, Vishal Jani, Adnan Safdar, Anmar Razak, Mounzer Kassab, Malathi Rao, Asif Khan, Adil Malik, Adnan Qureshi Headache: Treatment P7.175 Assessment of Cardiovascular Safety in Cynomolgus Monkeys Following IV Administration of LBR-101 Sarah Walter, Michele Bronson, Marcelo Bigal P7.176 Spinning Out of Control: The Black Box of Basilar and Hemiplegic Migraine Regina Krel, Paul Mathew, Warren Spinner, Shivang Joshi P7.184 Incidence of Adverse Events with MAP0004 Does Not Increase with Increased Frequency of Dosing: Results from a Long-Term Phase 3 Study Paul Winner, Sylvia Lucas, Biao Lu, Emilee Connors, Frederick Freitag, Shashidhar Kori P7.185 SUNCT Syndrome Responding to OnabotulinumtoxinA Injections: A Case Report Jina Youn, Kerry Knievel P7.186 The Durability of OnabotulinumtoxinA for the Treatment of Chronic Migraine: CLARITY Pilot Study Andrew Blumenfeld, Andrew Inocelda, Cedric Cunanan, Chris Purdy, Laura Dalfonso, Raf Magar P7.187 Headache and Treatment of Unruptured Intracranial Aneurysms Julieta Arena, Maximiliano Hawkes, Mauricio Farez, Lucia Pertierra, Alejandro Kohler, Dario Benito, Maria Goicochea, Virginia Pujol Lereis, Juan Miranda, Sebastian Ameriso P7.188 Incobotulinumtoxin A for the Preventive Treatment of Chronic Migraine Headaches Patrick Grogan, Andrew Robinson, Wendy Chao, Aven Ford P7.189 The IV Pharmaokinetics of Single and Multiple Doses of LBR-101 in Healthy Volunteers Sarah Walter, Rafael Escandon, Marcelo Bigal P7.190 P7.177 Safety and Tolerability of LBR-101, a Humanized Monoclonal Antibody That Blocks the Binding of CGRP to Its Receptor—Results of the Phase 1 Program Rafael Escandon, Michele Bronson, Sarah Walter, Marcelo Bigal P7.178 P7.191 Randomized Controlled Trial: Targeted Neck Cooling in the Treatment of the Migraine Patient Alexandra Gabriel, Jon Brown, Melvin Yee Successful Treatment of Spontaneous Low-Pressure Headache Due to Prominent Cervical CSF Leak with Cervical Epidural Blood Patch Eugene Wang, Dajie Wang P7.179 Intranasal Capsaicin (IC) Rapidly Relieves the Pain of Migraine and Other Severe Headaches Maria Alexianu, Anjan Chatterjee P7.180 An Inpatient Course of Intravenous Dihydroergotamine Use for New Daily Persistent Headache Michael Eller, Amy Gelfand, Nina Riggins, Peter Goadsby P7.181 Cerebral Blood Flow Velocity in Migraine and Tension-type Headache Patients Sebnem Karacay Ozkalayci, Ceyla Irkec, Bijen Nazliel P7.182 A Randomized, Open-label, Parallel Two-arm Study Evaluating the Efficacy of H.P. Acthar Injection Gel in the Treatment of Adults with Intractable Chronic Migraine Laszlo Mechtler, John Rothrock, Roger Cady, Peter McAllister P7.183 Trigeminal Trophic Syndrome with Intractable Pain, Successfully Treated with Spinal Cord Stimulation Erin Golden, Carrie Robertson, John Moossy, Paola Sandroni, Ivan Garza 122 High Asymmetric Dimethylarginine Levels in Migraine During the Interictal Period Aylin Reyhani, Yahya Celik, Talip Asil, Hakan Karadag, Ozgur Gunduz, Necdet Sut P7.192 Effects of Antiepileptic Drugs on Spreading Depression in the Chick Retina: Implications for Migraine Prophylaxis Joao De Moraes P7.193 Lamotrigine as a Prophylactic Treatment for Migraine-Associated Vertigo: A Case Series Lixin Zhang, Merika Wilson, Lisa Yamagishi 3:00 p.m.–6:30 p.m. P7.198 Cardiovascular and Hemodynamic Parameters in Women Following IV Administration of LBR101, a Monoclonal Antibody Against CGRP Marcelo Bigal, Abbas Alibhoy, Michele Bronson, Sarah Walter, Rafael Escandon P7.199 Efficacy and Safety of High Dose of Intravenous Methylprednisolone in Cluster Headache Patients Not Responders to Oral Therapy Elisa Rubino, Paola De Martino, Giovanna Vaula, Salvatore Gentile, Lorenzo Pinessi, Innocenzo Rainero P7.200 Safety of Dihydroergotamine Use in Patients with Symptoms of Hemiplegic or Basilar Type Migraine Brad Klein, Wael Hanna, Bhuvin Buddhdev, Mary Naglak P7.201 Long Term Therapeutic Response of Sphenopalatine Ganglion (SPG) Stimulation for Cluster Headache— Pathway CH-1 Study Miguel Lainez, Rigmor Jensen, Arne May, Charly Gaul, Anthony Caparso, Amy Goodman, Jean Schoenen P7.202 Peripheral Nerve Blocks for Pregnant Patients with Headache Shravya Govindappagari, Tracy Grossman, Ashlesha Dayal, Brian Grosberg, Sarah Vollbracht, Matthew Robbins P7.203 Efficacy and Safety of AVP-825, a Novel Breath-Powered™ Powder Sumatriptan Intranasal Treatment, for Acute Migraine Roger Cady, John Messina, Jennifer Carothers, Ramy Mahmoud P7.204 Initial Management of Migraine Headaches with Oral Medications in a Pediatric Emergency Unit Bhooma Aravamuthan, Kristine Williams, Soe Mar MS and CNS Inflammatory Diseases: Treatment P7.205 An Observational Comparison of Natalizumab and Fingolimod Using JCV Serology to Randomize Therapy Robert Carruthers, Dalia Rotstein, Brian Healy, Tanuja Chitnis, Howard Weiner, Guy Buckle P7.206 Cardiac Side Effects of Dihydroergotamine Erin Bange, Robert Rennie, Betts Patti-Ann, Christina Szperka Fingolimod Is Not Able to Inhibit Multiple Sclerosis Disease Reactivation After Natalizumab Discontinuation Marco Capobianco, Alessia Di Sapio, Simona Malucchi, Maria Malentacchi, Manuela Matta, Francesca Sperli, Alessandra Oggero, Antonio Bertolotto P7.196 Gammacore Device for Treatment of Migraine Attack: Preliminary Data Licia Grazzi, Susanna Usai, Gennaro Bussone P7.207 P7.197 P7.208 P7.194 A Critical Evaluation of Migraine Trigger Site Deactivation Surgery Paul Mathew P7.195 Transient Exacerbation Of Headache In Patients Receiving Intravenous Dihydroergotamine For Inpatient Management Of Chronic Migraine Does Not Alter Outcomes Michael Eller, Amy Gelfand, Nina Riggins, Christoph Schankin, Peter Goadsby Stopping Disease Modifying Therapy in Progressive Multiple Sclerosis—a Prospective Study Gary Birnbaum Comparison of Switching to Natalizumab Versus Remaining on Interferon-Beta or Glatiramer Acetate After On-Treatment MS Relapse Using Propensity-Matched Registry Data Timothy Spelman, Tomas Kalincik, Fabio Pellegrini, Annie Zhang, Maria Trojano, Heinz Wiendl, Ludwig Kappos, Robert Hyde, Shibeshih Belachew, Freek Verheul, Francois Grand-Maison, Helmut Butzkueven 2O14 Scientific Abstract Listing and Annual Meeting Information P7.209 Natalizumab in Multiple Sclerosis with Spinal Involvement Chiara Zecca, Christian Kamm, Gianna Carla Riccitelli, Mirjam Heldner, Matteo Caporro, Claudio Staedler, Claudio Gobbi P7.210 Impact of Natalizumab Treatment for Multiple Sclerosis on Patientreported Physical Functioning Over 3 Years in US Clinical Practices Timothy Vollmer, John Foley, Kavita Nair, Judith Stephenson, Timothy Niecko, Sonalee Agarwal, Crystal Watson P7.211 Relapse Rates Among Patients with Multiple Sclerosis Who Switch from Interferon Therapy to Fingolimod or Glatiramer Acetate: A Retrospective US Claims Database Analysis Raquel Lahoz, Niklas Bergvall, Neetu Agashivala, Ashish Pradhan, Gorana Capkun, Jonathan Korn, Allison Petrilla, Swapna Karkare, Catherine Balderston McGuiness, Charles Makin P7.212 Reactivation During Switch from Natalizumab to Fingolimod: Is it Predictible? Adil Maarouf, Anne Laure Pernelet, Adrien Maitrot, Nathalie Caucheteux, Laure Daelman, Marie-Pierre Chaunu, Laurent Pierot, Ayman Tourbah P7.213 Multiple Sclerosis Symptom Recrudescence Is Common at the End of the Natalizumab Dosing Cycle John Ratchford, Regina Brock-Simmons, Amanda Augsburger, Sonya Steele, Kristie Mohn, Mandi Rhone, Jinyan Bo, Kathleen Costello P7.214 Estimating the Onset of Efficacy with Teriflunomide in Patients with Relapsing Forms of Multiple Sclerosis Jerry Wolinsky, Deborah Dukovic, Philippe Truffinet, Ludwig Kappos P7.215 A Five-year Clinical Follow-up Study of Patients with Multiple Sclerosis Who Started Natalizumab Luca Prosperini, Valeria Barletta, Laura De Giglio, Fulvia Fanelli, Giovanna Borriello, Carlo Pozzilli P7.216 Natalizumab Therapy, How to Treat How to Stop: The TY-STOP Study Marinella Clerico, Stefania De Mercanti, Federico Piazza, Eleonora Virgilio, Dario Gned, Vincenzo Brescia Morra, Roberta Lanzillo, Luca Amato, Mario Quarantelli, Angelo Ghezzi, Anna Bianchi, Damiano Baroncini, Giuseppe Salemi, Sabrina Realmuto, Maria Teresa Ferrò, Francesca Vitetta, Giulia Superti, Paola Cavalla, Mariangela D’Onghia, Damiano Paolicelli, Irene Schiavetti, Maria Pia Sormani, Lorenzo Pinessi, Maria Trojano, Luca Durelli P7.217 Recommendations for Fingolimod Treated Patients Vacinated for Varicella Zoster Virus. Sergio Stecchi, Cinzia Scandellari, Liliana Gabrielli, Tiziana Lazzarotto P7.218 Treatment Satisfaction After Switching to Fingolimod Directly from an Injectable Therapy Edward Fox, Keith Edwards, John Burch, Kevin McCague, Luigi Barbato Poster Session VII P7.219 Adherence to, and Effectiveness of, Treatment with Subcutaneous Interferon Beta-1a in Relapsing Multiple Sclerosis Patients Using RebiSmart™ for Self-Injection: Final Results of the One-Year International, Observational SMART Study Antonios Bayas, Jean-Christophe Ouallet, Boris Kallmann, Raymond Hupperts, Ulrich Fulda, Kurt Marhardt P7.220 Improved Estimation of Treatment Effects: Analysis of Time to Recurrent Relapse with Fingolimod or Intramuscular Interferon Beta-1a Treatment Using the Proportional Means Model Xiangyi Meng, M. Zahur Islam, Peter Chin, Nadia Tenenbaum, Gary Cutter P7.221 Switching from Injectable Therapy Leads to High Continuation Rate on Fingolimod Yves Lapierre, Daniel Selchen, Virginia Devonshire, Robyn Schecter P7.222 Relapse Rates Among Patients with a History of Relapses Treated with Fingolimod Compared with Interferons or Glatiramer Acetate for the Treatment of Multiple Sclerosis: A Retrospective US Claims Database Analysis Jonathan Korn, Niklas Bergvall, Raquel Lahoz, Neetu Agashivala, Ashish Pradhan, Gorana Capkun, Allison Petrilla, Swapna Karkare, Catherine Balderston McGuiness, Charles Makin P7.223 Efficacy of Fingolimod Therapy Does Not Depend on the Individual Body Mass Index in Patients with MS Thomas Dehmel, Clemens Warnke, Anne Mausberg, Kathleen Wolffram, Maria Diaz-Lorente, Hans Hartung, Bernd Kieseier P7.229 Marburg Variant Multiple Sclerosis, Responsive to Natalizumab Acutely and Chronically Sara Mayer, Adam Carpenter, Pezhman Roohani P7.230 Fingolimod Treatment In Relapsing-Remitting Multiple Sclerosis Patients: A Clinical Practice Experience Rocco Totaro, Gianfranco Costantino, Roberta Fantozzi, Paolo Bellantonio, Caterina Di Carmine, Aurora Fuiani, Ciro Mundi, Stefano Ruggieri, Antonio Carolei P7.231 Prospective Evaluation of Persistence, Treatment Adherence, Quality of Life, and Treatment Satisfaction in Patients Treated with an Intramuscular Interferon Beta-1a Autoinjector in a RealWorld Clinical Setting Antonio Salgado, Veit Becker, Raymond Hupperts, Claes Martin, Sergio Slawka, Xiaojun You, Bjorn Sperling P7.232 Comparison of Efficacy and Treatment Satisfaction of Patients on Baseline Therapy or Fingolimod: Results of the Interim Analysis of Two German Registry Studies PANGAEA and PEARL Tjalf Ziemssen, Sylia Moser, Alexandra Fuchs, Christian Cornelissen P7.233 Fingolimod First-dose Effects in Patients with Relapsing-Remitting Multiple Sclerosis Concomitantly Treated with Serotonin-Specific Reuptake Inhibitors Robert Bermel, Ron Hashmonay, Xiangyi Meng, Philipp Von Rosenstiel, Nicolaos Sfikas, Simrat Randhawa, Daniel Kantor P7.234 Positive Response to Alemtuzumab (ALE) Rescue Immunotherapy in a High Disability, Treatment-Refractory Multiple Sclerosis (MS) Cohort Samuel Hunter, Heli Hunter, Daniel Kantor Systematic Literature Review and Network Meta-Analysis of Pegylated Interferon Beta-1a and Disease Modifying Therapies for Relapsing/Remitting Multiple Sclerosis Keith Tolley, Michael Hutchinson, Andrew Pachner, Elizabeth Kinter, Bjorn Sperling, Xiaojun You, Ping Wang, Ankush Taneja, Mohd. Kashif Siddiqui P7.225 P7.235 P7.224 Persistence and Adherence of Fingolimod Compared with Other DiseaseModifying Therapies for the Treatment of Multiple Sclerosis: A Retrospective US Claims Database Analysis Jonathan Korn, Niklas Bergvall, Raquel Lahoz, Neetu Agashivala, Ashish Pradhan, Gorana Capkun, Allison Petrilla, Swapna Karkare, Catherine Balderston McGuiness, Charles Makin P7.226 Clinical Predictors for Fingolimod (Gilenya) Treatment Response in Multiple Sclerosis Patients Dalia Rotstein, Muhammad Taimur Malik, Brian Healy, Howard Weiner, Tanuja Chitnis P7.227 Changes in Natalizumab Treatment Patterns and Association with Relapse Outcomes: A Retrospective Study Robert McQueen, Brieana Buckley, Terrie Livingstone, Timothy Vollmer, John Corboy, Kavita Nair, Jonathan Campbell P7.228 A Two-Year Retrospective Analysis of Rituximab Therapy in Secondary-Progressive Multiple Sclerosis Christopher Perrone, Biljana Beretich, Peter Riskind, Carolina Ionete Treatment Satisfaction, Adherence and Behavioral Assessment in Patients De-Escalating from Natalizumab to Interferon Beta Claudio Gobbi, Gianna Riccitelli, Pasquale Calabrese, Emanuele Pravatà, Ursula Candrian, Charles Guttmann, Chiara Zecca P7.236 The Providence MS Center’s Dimethyl Fumarate (DMF) Registry Kyle Smoot, Bobbie Lee Roth, Chiayi Chen, Kiren Kresa-Reahl, Leah Gaedeke, Stanley Cohan P7.237 Pharmacokinetics of Laquinimod, an Oral Immunomodulatory Agent in Development for The Treatment of Relapsing-Remitting Multiple Sclerosis Hayrettin Tumani, Tjalf Ziemssen, Friedemann Paul, Martin Marziniak, Nils Richter, Christoph Heesen, Yossi GilgunSherki, Tali Gorfine, Ofer Spiegelstein, Emil Samara, Yulia Sidi, Dorit Mimrod P7.238 Clinical And Radiological Activity During The Fingolimod Treatment Prescribed After Natalizumab. A Multiple Sclerosis Unit Experience Rocio Hernandez Clares, Ester Carreon, Begoña Palazon, Encarnación Andreu, Jose Javier Martin, Jose Meca La Llana P7.239 Safety and Efficacy in Patients Receiving Natalizumab Therapy in Hungary Tunde Csepany, Lovas Gabor, Bencsik Krisztina, Csilla Rozsa, Magdolna Simo, Krisztina Kovacs, Samuel Komoly, Peter Barsi, Zoltan Mor P7.240 Subcutaneous Interferon Beta1a Decreases the Evolution of GadoliniumEnhancing Lesions Into Chronic Black Holes in Relapsing Multiple Sclerosis Anthony Traboulsee, David Li, Yinshan Zhao, Roger Tam, Guojun Zhao, Yan Cheng, Andrew Riddehough, Fernando Dangond, Juanzhi Fang, Ludwig Kappos P7.241 Risk Factors for Relapses After Switching from Natalizumab to Fingolimod Joachim Havla, Robert Hoepner, Christian Eienbröker, Bjorn Tackenberg, Kerstin Hellwig, Ingrid Meinl, Ralf Gold, Reinhard Hohlfeld, Tania Kuempfel, Ingo Kleiter P7.242 Short-term Follow-up of Central Motor Conduction Failure in Relapsing Multiple Sclerosis Patients Undergoing High-dose Steroid Treatment Alessia Di Sapio, Antonio Bertolotto, Federica Melillo, Simona Malucchi, Paola Berchialla, Francesca Sperli, Walter Troni P7.243 Epidemiological Study to Identify Factors That Influence Clinical Decision Making in Patients with Relapsing Remitting Multiple Sclerosis (RRMS) After at Least 2 Years of Treatment with Immunomodulators in Germany (EPIDEM) Stephan Schmidt, Petra Schicklmaier, Christine Winterstein, Wettmarshausen Christine, Matthias Meergans, Colin Wernsdoerfer Treatment of Specific Multiple Sclerosis Symptoms P7.244 Dalfampridine Real World Utilization and Efficacy Assessment Sylvia Klineova, Joshua Friedman, Colleen Farrell, Christine Hannigan, Fred Lublin, Stephen Krieger P7.245 Aspirin Is Unlikely to Have a Clinically Meaningful Effect on Multiple Sclerosis-Related Fatigue: Data from a Randomized Controlled Trial Dean Wingerchuk, Mark Keegan, Elizabeth Shuster, Jonathan Carter, Joe Hentz, Greg Thaera, Melissa Cortez, Moses Rodriguez P7.246 Effects of Prolonged-Released Fampridine on Walking Parameters, Upper Limb Function, Fatigue and Quality of Life Etienne Allart, Anne Benoit, Anne Blanchard, Helene Zephir, Olivier Outteryck, Arnaud Lacour, Patrick Vermersch P7.247 Prolonged-release Fampridine (Fampyra®) Post-marketing Experience in the Alsace Region Jean-Claude Ongagna, Carole Berthe, Nicolas Collongues, Frederic Blanc, Jerome De Seze P7.248 Long-Term Course and Clinical Assessment Parameters of Patients with Multiple Sclerosis Under Dalfampridine Tobias Ruck, Stefan Bittner, Nico Melzer, Heinz Wiendl, Matthias Schilling, Sven Meuth P7.249 Monotherapy with THC/ CBD Spray in Multiple Sclerosis Induced Spasticity Juergen Koehler, Walter Poellmann, Wolfgang Walter Feneberg, Martin Meier P7.250 Use of Medical Marijuana for Symptoms of Multiple Sclerosis (MS) Among Participants of the Pacific Northwest MS Registry (PNWMSR) Tamela Stuchiner, Elizabeth Baraban, Chiayi Chen, Stanley Cohan P7.251 Attenuation of Dimethyl Fumarate-related Gastrointestinal Symptoms with Montelukast Carmelo Tornatore, Faria Amjad P7.252 25G Sprotte Needle Strongly Reduces the Risk of Post-Lumbar Puncture Headache in Clinical Practice. Antonio Bertolotto, Francesca Sperli, Marco Capobianco, Maria Malentacchi, Annalisa Pulizzi, Simona Malucchi P7.253 A Double-blind Placebo Controlled Study of the Effect of BetaAlanine, a Nonessential Amino-Acid, on Neurologic, Motor Function, Quality of Life, and Fatigue in Patients Diagnosed With Multiple Sclerosis John Kanter, Elizabeth Keiner, Arielle Biwer, Elizabeth Coughlin, Brittany DiFabio, Donya Salmasinia, Michael Ormsbee, John Giannini, Charles Maitland Neuro-oncology: CNS Metastases and Complications of Treatment P7.254 Brain Metastases In Ovarian Cancer—a Comprehensive Review. Shabnam Pakneshan, Damoun Safarpour, Fattaneh Tavassoli, Bahman Jabbari P7.255 A Case of Primary Meningeal Melanoma Bhaskar Roy, Fatmah Al Zahmi, Richard Danialan, Srinivas Mandavilli P7.256 Isolated Primary CNS Infiltrative Parenchymal Histiocytosis with Intraventricular Hemorrhage Eric Mittelmann, Patrick LaSala, Karen Weidenheim, Jerome Graber P7.257 Brainstem Glioma 8 Years After External Beam Radiotherapy for Pituitary Macroadenoma: Correlation with Radiation Treatment Dose and Volume Salim Abboud, Leo Wolansky, Sunil Manjila, Simon Lo, Bahaudden Arafah, Warren Selman, Lisa Rogers P7.258 Effects of Ionizing Radiation on Human Microglial Cells Hongxin Chen, Sonia De Toledo, Edward Azzam, Nizar Souayah Neuro-oncology: Primary CNS Lymphoma and Other Hematologic Malignancies P7.259 Salvage Therapy with Bendamustine for Methotrexate Refractory Recurrent Primary CNS Lymphoma: A Retrospective Case Series Marc Chamberlain Fast, Easy Registration Online · AAN.com/view/AM14 123 Thursday May 1 First Authors stand by Posters from 5:00 p.m.–6:30 p.m Thursday, May 1 P7.260 Primary Natural Killer/T-cell Lymphoma Presenting as Leptomeningeal Disease Carlos Kamiya-Matsuoka, Bing Liao, Yun Gong, Merry Chen, Karin Woodman, Nathan Fowler, Charles Conrad P7.261 Rituximab and Bendamustine for CNS Involvement by Chronic Lymphocytic Leukemia Geraldine Faivre, Samuel Singer, Lisa DeAngelis, Ariela Noy, Antonio Omuro P7.262Neurolymphomatosis: Heterogenous Presentations Daniel Winkel P7.263 VEGF and Pentraxin-3 Levels in POEMS Syndrome: A 2-Year Longitudinal Study. Chiara Dalla Torre, Marina Scarlato, Federica Lessi, Marta Campagnolo, Marta Lucchetta, Susanna Ruggero, Elisabetta Toffanin, Angelo Manfredi, Mario Ermani, Fausto Adami, Chiara Briani P7.264 Bing-Neel Syndrome: Presentation of Three Unusual Patients Louis Royer-Perron, François Moreau, Sylvie Gosselin P7.265 Central Neuropathy in a Patient with Waldenstrom’s Macroglobulinemia: Should You Suspect Bing-Neel Syndrome Even in the Absence of Abnormal Brain Imaging? Neha Gupta Neuro-oncology: Primary CNS Tumors: Gliomas P7.266 Hormone Replacement Therapy and Risk of Glioma: A Nationwide Nested Case-Control Study Lene Andersen, Soren Friis, Jesper Hallas, Pernille Ravn, David Gaist P7.267 Epilepsy and Clinical Neurophysiology (EEG): Surgery and Neurostimulation Aging, Dementia, and Cognitive and Behavioral Neurology: Attention/Neglect P7.275 P7.286 Outcome of Intracranial EEG Monitoring and Surgery in MRI-negative Temporal Lobe Epilepsy Ricky Lee, Marietta Hoogs, David Burkholder, Max Trenerry, Joseph Drazkowski, Jerry Shih, William Tatum, Gregory Cascino, Elaine Wirrell, Gregory Worrell, Elson So P7.276 Comparison of Seizure Outcome After Selective Amygdalohippocampectomy in Adult Versus Pediatric Onset Temporal Lobe Seizures Aradia Fu, Steve Chung P7.277 Reasons for Delayed Temporal Lobe Epilepsy Surgery Aditi Narechania, Paz Abergel, Irena Garic, Michael Macken, Elizabeth Gerard, Stephan Schuele P7.278 Surgical Outcome of Parietal Lobe Epilepsy Anna-Marieta Moise, Janice Jordan, Lola Morgan, Linda Leary, Kameel Karkar, Octavian Lie, Jose Cavazos, JeanLouis Caron, Alexander Papanastassiou, Charles Szabo P7.279 Electrical Stimulation of the Anterior and Centromedian Nucleus of Thalamus for Treatment of Refractory Epilepsy—Report of Four Cases Wei Hu, Bryan Klassen, Kendall Lee, Daniel Clayton, Squire Stead P7.280 Deep Brain Stimulation for the Management of Seizures in MECP2 Duplication Syndrome. Fabio Nascimento, Hanna Faghfoury, Timo Krings, Anfal Ali, Jonathan Fridhandler, Andres Lozano, Richard Wennberg, Danielle Andrade Relationship Between CD44v6 and E-cadherin Expression in Human Primary Brain Tumors Leslaw Zub, Boguslaw Paradowski, Julia Bar, Anna LisNawara, Leszek Noga, Michal Jelen P7.281 P7.268 A Novel Therapeutic Target for Treatment of Malignant Brain Tumors Nazanin Majd, Kazutaka Sumita, Hirofumi Yoshino, Dillon Chen, Atsuo Sasaki P7.282 P7.269 P7.283 Posterior Fossa Recurrences of Supratentorial WHO Grade II and III Gliomas Robert Terziev, Gregorio Petrirena, Jean-Yves Delattre P7.270 Posterior Fossa Tumours in Children as Seen in a Tertiary and Referral Hospital in Sub-Saharan Africa Victor Kwasi P7.271 Oligodendroglial Gliomatosis Cerebri Exhibiting Leptomeningeal and Nerve Root Involvement Grace Mcmacken, Brian Herron, Ailsa Fulton P7.272 A Case Report: Primary Glioblastoma of the Pineal Regina Krel, Yana Krutoshinskaya, Arthur Rosiello, Roberta Seidman, Agnes Kowalska P7.273 Aggressive Medical Care at the End of Life (EOL) in Glioblastoma (GBM): The 5-year Memorial Sloan-Kettering Cancer Center (MSKCC) Experience Alexis Dallara, Alan Carver, Eli Diamond 3:00 p.m.–6:30 p.m. The Efficacy of VNS in Patients with Pharmacoresistant Epilepsy of Temporal Versus Extra-temporal Locations Abuhuzeifa Abubakr, Ilse Wambacq Prospective Memory After Mesial Temporal Resection Carla Adda, Luiz Henrique Castro, Carmen Jorge, Rosa Valerio, Hung Wen Database Systems and Online Tools for Early Referral to Epilepsy Surgery Evaluation in Mesial Temporal Lobe Epilepsy Rodolfo Callejas, Ildefonso Rodriguez-Leyva P7.284 Association Between Chronobiology of Seizures and Hemispheric Laterality in Patients Who Underwent Surgery for Refractory Epilepsy Anca Popescu, Amrit Misra, Maromi Nei P7.285 Vagal Nerve Stimulation and Cortical Source Localization in Pre- and Post-operation EEG Data: A Case Study Hakan Ekmekci, Mastaneh Torkamani Azar, Ali Okatan, Serefnur Ozturk Memantine Effects on Attention in FXTAS: A Double-blind ERP Study Jinchen Yang, Annette Rodriguez, Merve Avar, Ryan Brill, Christa Simon, Yu-Qiong Niu, Ashley Royston, Randi Hagerman, John Olichney P7.287 The Mind’s Eye: Effects of Aging, Hemispace and Movement Direction on Estimates of Distance Tigran Kesayan, Adam Falchook, John Williamson, Kenneth Heilman Emergence of New Responders to Treatment and New Adverse Events in Clinical Trials of Pregabalin in Diabetic Peripheral Neuropathy and Postherpetic Neuralgia Parsons, Birol Emir P7.300 Contact Heat Evoked Potentials Stimulator (CHEPS) in the Assessement of Painful Leprosy Neuropathy Camila Pupe, Osvaldo Nascimento, Marcos Freitas, Eduardo Davidovich, Caroline Bittar, Ricardo Dornas, Bruno Coutinho P7.301Pharmacological, Predictors of Recovery of Allocentric and Egocentric Neglect: The Role of Education Joseph Posner, Lydia Trupe, Cameron Davis, Yessenia Gomez, Donna Tippett, Argye Hillis Pharmacokinetics and Safety Profiles of DS-5565, a Novel α2δ Ligand Tomihisa Yokoyama, Naohisa Arakawa, Yuki Domon, Fumihiko Matsuda, Tatsuya Inoue, Yutaka Kitano, Makoto Takahashi, Naotoshi Yamamura, Kiyonori Kai P7.289 P7.302 P7.288 Spatial Neglect Commonly Occurs After Traumatic Brain Injury Peii Chen, Irene Ward, Kimberly Hreha, Yan Liu, Ummais Khan P7.290 Changes of Vertical and Horizontal Pseudoneglect with Aging Nicholas Milano, Anouchka Douyon, Adam Falchook, Kenneth Heilman P7.291 Effects of Gaze, Head and Hand Location on Motor Function: Evidence from TMS in Normal Subjects H. Coslett, Olu Faseyitan, Jared Medina, Michael Iannacone P7.292 Things Look Up With Aging Anouchka Douyon, Adam Falchook, Kenneth Heilman, Nicholas Milano P7.293 Leftward Where Bias and Rightward Distraction in Chronic Neglect. A. Barrett, Kelly Goedert, Mooyeon Oh-Park P7.294 Spatial Neglect and Parkinson Disease Adam Falchook, Liliana Salazar, Dan Neal, Tigran Kesayan, John Williamson, Irene Malaty, Nikolaus McFarland, Michael Okun, Ramon Rodriguez, Aparna WagleShukla, Kenneth Heilman P7.295 Apparent Body Size Alters Motor Function H. Coslett, Jared Medina, Olu Faseyitan Pain and Palliative Care P7.296 Central Nervous System Safety and Tolerability of DS-5565: A Randomized, Double-Blind, Placebo- and Active Comparator-controlled Phase II Study in Diabetic Peripheral Neuropathic Pain Aaron Vinik, Uma Sharma, Karen Feins, Ching Hsu, Domenico Merante P7.297 Pharmacologic and Non-Pharmacologic Treatments of Adolescents with Chronic Tension-type Headache. Peter Przekop, Allison Przekop P7.298 Efficacy of Pregabalin in the Treatment of Prediabetic Neuropathic Pain Maria Alejandra Gonzalez Duarte, Karla Cardenas-Soto, Monica Lem, Cinthia Castillo, Christopher Gibbons, Roy Freeman P7.274 Neuro-oncology Telemedicine Follow-up Visits Richard Green, Emily Woyshner, Amanda Hauser Dehaven 124 P7.299 2O14 Scientific Abstract Listing and Annual Meeting Information An Assessment of Pain Reports in Amyotrophic Lateral Sclerosis Using Three Large Data Sets Helen Stephens, Stephanie Felgoise, Susan Walsh, Zachary Simmons P7.303 Parkinson’s Disease Patients’ Preferences for Communication About Advanced Care Planning Keiran Tuck, Lissa Brod, John Nutt, Erik Fromme P7.304 Quality of Care in the Recognition and Management of Pain Syndromes at the Emergency Room of a Tertiary Hospital from January 2010-December 2010 (A Needs Assessment) Ma. Alma Carandang, Amado San Luis P7.305 Mindfulness-Based Therapies in the Treatment of Somatization Disorders: A Meta-Analysis Lakhan Shaheen P7.306 False Localizing Exam in a Lumbar Spinal Epidural Abscess (SEA): Right Paraspinal Pain and Contralateral Leg Weakness Pavis Laengvejkal, Inhyup Kim, Kunut Kijsirichareanchai, Sahawat Tantikittichaikul, John DeToledo P7.307 The PRIZM (Patient Registry of Intrathecal Ziconotide Management) Study for Patients with Severe Chronic Pain Michael Saulino, David Caraway, Eric Grigsby, Michael Leong, Richard Rauck, Timothy Deer, Philip Kim, Mark Wallace, Gladstone MCDowell, Sonja Hokett, Sarah Alvarez-Horine, Geertrui Vanhove P7.308 Relationship Between Pharmacokinetics and Urine Drug Screen for Opioids: A Method to Determine Efficacy, Safety and Abuse Fadi Delly, Gulshan Oberoi, Rudram Muppuri, Shushovan Chakrabortty P7.309 Persistent Na+ and K+ Channel Dysfunctions After Chronic Exposure to Insecticides and Pyridostigmine Bromide Nan Jiang, Thomas Nutter, Brian Cooper P7.310 Pain Profiles in Small Fiber Neuropathy Maria Alejandra Gonzalez Duarte, Karla Cárdenas-Soto, Mónica Lem, Cinthia Castillo, Enoe Cruz-Martinez Poster Session VII P7.311 Contact Heat Evoked Potentials Stimulator (CHEPS) and Thermal Quantitative Sensory Testing (QST) in the Assement of Atypical Orofacial Pain Bruno Coutinho, Osvaldo Nascimento P7.312 Shifts in Pain Severity Categories Among Patients with Painful Diabetic Peripheral Neuropathy or Postherpetic Neuralgia Treated with Pregabalin Parsons Bruce, Birol Emir P7.313 Pharmacokinetics of DS-5565, a Novel α2δ Ligand, in Rats and Monkeys, and Assessment of DDI Risk Naotoshi Yamamura, Makiko Yamada, Makoto Takahashi, Minoru Uchiyama, Hiroko Koda, Tsuyoshi Mikkaichi, Yumi Nishiya, Tomoyo Honda, Naohisa Arakawa, Yuki Domon, Thomas Fischer, Juergen Mueller P7.314 Suicide in a Woman Diagnosed with Bulbar Predominant Amyotrophic Lateral Sclerosis: A Case Report and Literature Review Maggie McNulty, John-Michael Li, Madhu Soni P7.315 Approaching the Mechanisms Underlying Analgesia Induced by High Voltage Electrical Stimulation of Lumbosacral Nerve Roots Walter Troni, Federica Melillo, Alessia Di Sapio, Antonio Bertolotto P7.316 The Palliative Care Needs of Patients Living with Life-Limiting Neurological Illness Marvin Chum, Valerie Schulz, Christopher Watling, Teneille Gofton P7.317 Combined Supraorbital (SONS) and Occipital Nerve Stimulation (ONS) for Intractable Post-Herpetic Neuralgia Robert Bulger, Francis Conidi, Kenneth Reed P7.318 The Need for Early Recognition of Complex Regional Pain Syndrome to Facilitate Early Effective Treatment Jacquelyn Laplant, Robert Knobler Child Neurology and Developmental Neurology VI P7.319 Abnormal Measures of White Matter Integrity in Newborns with Hypoxic Ischemic Encephalopathy (HIE) Paola Pergami, Tania Nanavati, Bob Hou, Panitan Yossuck, Ashley Smith, Jeffrey Carpenter, Mark Haut P7.320 A Noninvasive Neurotechnology, HIRREM, Is Associated with Symptom Reduction and Improved Cardiovascular Autonomic Measures in Adolescents with POTS Catherine Tegeler, John Fortunato, Jared Cook, Sung Lee, Meghan Franco, Charles Tegeler P7.321 A Novel SUCLA2 Mutation Associated with a Complex Childhood Movements Disorder Caterina Garone, Juliana Gurgel-Giannetti, Simone SannaCherchi, Sindu Krishna, Ali Naini, Catarina M Quinzii, Michio Hirano P7.322 An Unusual Presentation of Neuropathy Secondary to Leprosy (Hansen’s disease) Derrece Reid, Debra Byler, Kimberly Harbaugh, Jennifer Baccon P7.323 Increased Coherence Between the Basal Ganglia and Motor Cortex in a Rat Model of Pediatric Asphyxial Cardiac Arrest. Bhooma Aravamuthan, Michael Shoykhet P7.324Neuro-Developmental Disorders in India—From Epidemiology to Public Policy Donald Silberberg, Narendra Arora, Vinod Bhutani, Maureen Durkin, Shefalli Gulati, Mkc Nair, Jennifer PintoMartin P7.325 Rituximab Therapy as a First-line Immunosuppressive Treatment in Children with Neuromyelitis Optica Spectrum Disorder: A Single-center Experience. Giulia Longoni, Brenda Banwell, Massimo Filippi, E. Ann Yeh P7.326Periventricularlaminar Heterotopia (PLH): Characterization in a Series of 18 Patients Dina Amrom, Firas Fahoum, Francois Dubeau, Gary Clark, Eugen Boltshauser, Paolo Curatolo, Renzo Guerrini, Ruben Kuzniecky, Anne Tsai, Parul Jayakar, Mitsuhiro Kato, A Barkovich, Donatella Tampieri, Denis Melancon, Frederick Andermann, Eva Andermann, William Dobyns P7.327 A Case Report of 4H Syndrome Probably Caused by a Heterozygous Abnormality of the POLR3A Gene with Preserved Intellectual Function Kuwabara Midori, Yuki Hatanaka, Takamichi Kanbayashi, Hidehiko Okuma, Masahiro Sonoo, Hirotomo Saitsu, Naomichi Matsumoto P7.328 Sideroflexin-4 Defects Cause a New Infantile Mitochondrial Disorder Affecting Hematopoietic and Central Nervous Systems. Caterina Garone, Gordon J Hildick-Smith, Jeffrey D Cooney, Laura S Kremer, Tobias B Haack, Jonathan N Thon, Non Miyata, Daniel Lieber, Sarah Calvo, Orhan H. Akman, Yvette Y Yen, Nicholas C Huston, Diana S Branco, Dhvanit I Shah, Matthew L Freedman, Carla M Koehler, Joseph E Italiano, Andreas Merkenschlager, Skadi Beblo, Tim Strom, Thomas Meitinger, Peter Freisinger, Alice Donati, Holger Prokisch, Vamsi Mootha, Barry Paw, Salvatore DiMauro P7.329 Intrinsic Excitability Defects in Specific Subtypes of Medial Prefrontal Cortex Pyramidal Neurons in a Mouse Model of Autism Audrey Brumback, Vikaas Sohal P7.330 A Comparison of Colocated and Traditional Outpatient Consultation for the Treatment of ADHD in Two Urban Medical Homes: Costs and Outcomes David Urion P7.331 Ehlers-Danlos Type IV Presenting with a Peroneal Neuropathy Amitha Ananth, Yaping Yang, Seema Lalani, Lotze Timothy P7.332 Patients with Electrical Status Epilepticus in Sleep and Normal Magnetic Resonance Imaging Have Smaller Thalamic Volume than Controls Ivan Sanchez Fernandez, Alireza Akhondi-Asl, Jacquelyn Klehm, Simon Warfield, Jurriaan Peters, Tobias Loddenkemper P7.333 Brainstem Disconnection Syndrome in a Patient with Fetal Alcohol Syndrome Chandan Mehta, Rajkumar Agarwal, Ajay Kumar, Mohsin Maqbool P7.334 Cerebrospinal Fluid Opening Pressure in a Pediatric Demyelinating Disease Cohort Sona Narula, Grant Liu, Robert Avery, Brenda Banwell, Amy Waldman P7.335 Soto-like Syndrome and Cortical Malformation Associated with Chromosome 19p13.2 Microdeletion Including Nuclear Factor-1X (NFIX) Swati Karmarkar, Ina Amarillo, Douglas Larsen P7.337 Neurocognitive and Psychological Profiles of Children with Idiopathic Epilepsy Adel Eladl, Hoda Atwa P7.338Multi-domain Neurodevelopmental Delays in Multiple Gestation and Singleton Preterm Infants Imad Jarjour, Laila Jarjour, Alexandra Sibley P7.339 Retrospective Review of Inpatient Headache Admissions: Looking AT Determinants of a Successful Admission Arnold Sansevere P7.340 Resting State EEG Serves as a Promising Biomarker of Cognitive and Language Function in Young Children with ASD. Kevin McEvoy, Shafali Jeste P7.341 Pathology of the Neurovascular Unit in Cerebral X-linked Adrenoleukodystrophy Sandra Jimenez, Patricia Musolino, Tracey Suter, Florian Eichler P7.342 Cortical Involvement in Early and Late Stages of Metachromatic Leukodystrophy Jan-Mendelt Tillema, Marloes Derks, Petra Pouwels, Pim de Graaf, Frederik Barkhof, Marjo Van Der Knaap, Nicole Wolf P7.343 Stroke due to Extracranial Internal Carotid Artery Dissection After Roller Coaster Rides in a 4-year-old Boy Amre Nouh, Daniel Vela-Duarte, Thomas Grobelny, George Hoganson, David Pasquale, Jose Biller P7.344 Video EEG Monitoring in Infants: Predictors of Subclinical Seizures in the ICU Setting Eileen Broomall, Anna Mrelashvili, Elaine Wirrell Movement Disorders: Other Parkinsonian Disorders P7.345 Case Study with Video Clips: Midbrain Dysfunction and Restoration in a 30-year-old Woman with Hydrocephalus Sarah Dolgonos, Emmanuelle Schindler, Joshua Lovinger, Duarte Machado P7.336 Efficacy of EPA Enriched Phosphatidylserine-Omega-3 (Vayarin) on Children with ADHD Stephanie Nguyen, Cindy Nguyen, Robert Chudnow, Van Miller, Anthony Riela, Gerald So, Patricia Mireles, Lina Shah Obtaining Your CME and Evaluations To receive CME for education programs or scientific sessions, evaluations must be completed online or via the Annual Meeting mobile app. Wireless internet hotspots will be available at the convention center. Details will be provided prior to the meeting. Fast, Easy Registration Online · AAN.com/view/AM14125 Thursday May 1 First Authors stand by Posters from 5:00 p.m.–6:30 p.m Thursday, May 1 S54 MS and CNS Inflammatory Disease: Neuroimaging II S55 Pediatric Stroke and Stroke in the Young 3:15 p.m. S54.001 The Origin of Chronic T2* and Phase Rims in MS Lesions: A Longitudinal 7T MRI Study Martina Absinta, Pascal Sati, Massimo Filippi, Daniel Reich 3:15 p.m. S55.001 Moyamoya Disease in Children: Results of the International Pediatric Stroke Study Sarah Lee, Michael Rivkin, Adam Kirton, Gabrielle DeVeber, Jorina Elbers 3:30 p.m. S54.002 Is Primary Progressive Multiple Sclerosis a Disease Entity of its Own? Preliminary Results of a 7T MRI Study Joseph Kuchling, Ivan Bozin, Jan-Markus Dörr, Lutz Harms, Berit Rosche, Thoralf Niendorf, Friedemann Paul, Tim Sinnecker, Jens Wuerfel 3:30 p.m. S55.002 Intraoperative Neurophysiologic Monitoring of Surgical and Endovascular Treatment of Pediatric Arteriovenous Malformations Viet Nguyen, Santiago Avila, Leslie Lee, Sungho Cho, Scheherazade Le, Jaime Lopez 3:45 p.m. S54.003 Early Neuronal Damage in the Cervical Cord of Patients with Primary Progressive Multiple Sclerosis Demonstrated by MR Spectroscopy and Q-space Imaging Khaled Abdel-Aziz, Torben Schneider, Bhavana Solanky, Claudia Wheeler-Kingshott, Day Brian, Marios Yiannakas, Daniel Altmann, Amy Peters, Alan Thompson, Olga Ciccarelli 4:00 p.m. S54.004 Relationships Between Quantitative Spinal Cord MRI and Retinal Layers in Multiple Sclerosis Jiwon Oh, Elias Sotirchos, Shiv Saidha, Anna Whetstone, Min Chen, Scott Newsome, Kathleen Zackowski, Jerry Prince, Marie Diener-West, Daniel Reich, Peter Calabresi 4:15 p.m. S54.005 Cortical Lesions in Multiple Sclerosis Correlate with Retinal Pathology as Measured by Optical Coherence Tomography Daniel Harrison, Anna Whetstone, Omar Al-Louzi, Peter Calabresi 4:30 p.m. S54.006 The Effect of Cardiovascular Risk Factors on Lesion Burden and Brain Atrophy in Multiple Sclerosis Natalie Kappus, Bianca Weinstock-Guttman, Jesper Hagemeier, Cheryl Kennedy, Rebecca Melia, Ellen Carl, Deepa Ramasamy, Maryia Cherneva, Jackie Durfee, Niels Bergsland, Michael Dwyer, Channa Kolb, Murali Ramanathan, Robert Zivadinov 4:45 p.m. S54.007 Early Clinical and MRI Predictors of Time to Second Attack and Disability in Children with Acute Demyelinating Syndromes: Findings from a Prospective National Cohort Study Leonard Verhey, Ruth-Ann Marrie, Amit Bar-Or, Dessa Sadovnick, Manohar Shroff, Douglas Arnold, Brenda Banwell 126 3:45 p.m. S55.003 Marijuana Use and the Risk of Ischemic Stroke: The Stroke Prevention in Young Adults Study Tara Dutta, Kathleen Ryan, Yuching Cheng, Steven Kittner, John Cole 4:00 p.m. S55.004 Trends in Substance Abuse Preceding Stroke in Young Adults: An Update Felipe De Los Rios La Rosa, Dawn Kleindorfer, Jane Khoury, Joseph Broderick, Kathleen Alwell, Charles Moomaw, Pooja Khatri, Opeolu Adeoye, Matthew Flaherty, Daniel Woo, Jane Eilerman, Simona Ferioli, Brett Kissela 4:15 p.m. S55.005 Thrombophilia in Young Patients with Cerebrovascular Disease. AISYF Study Luciana Leon Cejas, Ricardo Reisin 4:30 p.m. S55.006 Long Distance Travel Potentiates Other Novel Risk Factors in PFO Related Strokes—“Economy Class Strokes” MingMing Ning, D Sena, K Feeney, T Wickham, M Elia, W Deng, I Chou, J Hung, L Chen, I Inglessis-Azuaje, S Silverman, R Schainfeld, D McMullin, G Dec, E Lo, I Palacios, F Buonanno 4:45 p.m. S55.007 Oral Contraceptive Use and Incident Stroke in Women with Sickle Cell Disease Taqi Zafar, Malik Adil, Muhammad Umair, Saqib Chaudhry, Amna Zarar, Muhammad Suri, Adnan Qureshi 3:15 p.m.–5:00 p.m. S56 Anterior Horn Disease 3:15 p.m. Presentation of Sheila Essey Award: An Award for ALS Research Recipient: Jeremy Shefner, MD, PhD Syracuse, NY 3:45 p.m. S56.003 HuR Is Essential for TDP43 Expression Through Posttranscriptional Mechanisms: Implications for Motor Neuron Toxicity and ALS Liang Lu, Lei Zheng, Ying Si, Shin Oh, Peter King 4:00 p.m. S56.004 GGGGCC Repeat Expansion of C9ORF72 Is Toxic via Sequestration of RNA Binding Proteins and Consequent Disruption of RNA Splicing Johnathan CooperKnock, Matthew Walsh, Adrian Higginbottom, J Robin Highley, Joanna Bury, Mark Dickman, Magnus Rattray, Paul Heath, Matthew Wyles, Paul Ince, Stephen Wharton, Stuart Wilson, Janine Kirby, Guillaume Hautbergue, Pamela Shaw 4:15 p.m. S56.005 The TREM2 Variant p.R47H Is a Risk Factor for Sporadic Amyotrophic Lateral Sclerosis Matthew Harms, Janet Cady, Erica Koval, Bruno Benitez, Craig Zaidman, Jennifer Jockel-Balsarotti, Peggy Allred, Robert Baloh, John Ravits, Ericka Simpson, Stanley Appel, Alan Pestronk, Alison Goate, Timothy Miller, Carlos Cruchaga 4:30 p.m. S56.006 Spinal Muscular Atrophy Phenotype Is Ameliorated Either by SMN Increase or Modulation of Secondary Cell Death Events with RNA Therapy Giulietta Riboldi, Monica Nizzardo, Chiara Simone, Federica Rizzo, Margherita Ruggieri, Serena Pagliarani, Gianna Ulzi, Sabrina Salani, Andrea DalMas, Monica Bucchia, Emanuele Frattini, Giulia Stuppia, Francesca Magri, Nereo Bresolin, Franco Pagani, Giacomo Comi, Stefania Corti 4:45 p.m. S56.007 iPSC-derived Neural Stem Cells Ameliorate the Phenotype of Spinal Muscular Atrophy with Respiratory Distress Type 1 (SMARD1) Stefania Corti, Chiara Simone, Monica Nizzardo, Federica Rizzo, Margherita Ruggieri, Sabrina Salani, Monica Bucchia, Paola Rinchetti, Chiara Zanetta, Irene Faravelli, Erika Monguzzi, Francesca Magri, Nereo Bresolin, Giacomo Comi 2O14 Scientific Abstract Listing and Annual Meeting Information S57 Movement Disorders: Imaging 3:15 p.m. S57.001 Abnormal Transcallosal Motor Projections In Cervical Dystonia: An fMRI and Tractographic Analysis Jeff Waugh, Jake Kuster, Jacob Levenstein, Woodman Sandra, Trisha Multhaupt-Buell, Makris Nikos, Lewis Sudarsky, Hans Breiter, Nutan Sharma, Anne Blood 3:30 p.m. S57.002 Dopamine Transporter Imaging in Essential Tremor With and Without Parkinsonian Features Olga Waln, Ying Wu, Reid Perlman, Anh Kim Van, Juliet Wendt, Joseph Jankovic 3:45 p.m. S57.003 Diffusion Tensor Imaging as a Biomarker for REM Sleep Behavior Disorder and Parkinson’s Disease Matthew Brodsky, John Grinstead, David Lahna, Jeffrey Pollock 4:00 p.m. S57.004 Midbrain Microstructural Atrophy Associated with Parkinson’s Disease Motor and Cognitive Symptoms Using 7-Tesla MRI Kathleen Poston, Laura Santoso, Jeffrey Bernstein, Matthew Cruadhlaoich, David Everling, Sophie YorkWilliams, Michelle Fenesy, Michael Zeineh, Geoffrey Kerchner 4:15 p.m. S57.005 Exploring the Neural Circuitry of REM Sleep Behavior Disorder in Parkinson’s Disease Using Functional MRI Samuel Bolitho, James Shine, Sharon Naismith, Ron Grunstein, Peter Bell, Simon Lewis 4:30 p.m. S57.006 The ‘Swallow Tail’ Appearance of the Healthy Nigrosome—a New Accurate Test of Parkinson’s Disease: a Case-Control and Retrospective Cross-Sectional MRI Study at 3T Stefan Schwarz, Mohammed Afzal, Paul Morgan, Nin Bajaj, Penny Gowland, Dorothee Auer 4:45 p.m. S57.007 Mapping Regional Grey and White Matter Damage in Patients with Progressive Supranuclear Palsy Syndrome Francesca Caso, Federica Agosta, Maria Antonietta Volontè, Daniele Martinelli, Lidia Sarro, Francesca Spagnolo, Andrea Falini, Giancarlo Comi, Massimo Filippi S58 Aging, Dementia, and Cognitive and Behavioral Neurology: Clinical Aspects 3:15 p.m. S58.001 Alzheimer Patients Show Significant Disturbance in Water Influx Into CSF Space Strongly Supporting β-amyloid Clearance Hypothesis Tsutomu Nakada, Hironaka Igarashi, Yuji Suzuki, Ingrid Kwee 3:30 p.m. S58.002 Medical Risk Factors For Frontotemporal Degeneration: Analysis of the NACC Uniform Dataset Mariel Deutsch, Mario Mendez, Edmond Teng 3:45 p.m. S58.003 Cholesterol, Statins and the Risk of Dementia in the Oldest-Old: The 90+ Study Marcella Evans, Claudia Kawas, Maria Corrada 4:00 p.m. S58.004 The Effect of Triglycerides on Cognitive Function in Aging Adults: A Cross-Sectional Study Vishnu Parthasarathy, Darvis Frazier, Laura Jastrzab, Linda Chao, Helena Chui, Brianne Bettcher, Joel Kramer 4:15 p.m. S58.005 Association of Type 2 Diabetes Cognitive Impairment Is Mediated by Brain Atrophy Rosebud Roberts, David Knopman, Scott Przybelski, Michelle Mielke, Kejal Kantarci, Vernon Pankratz, Yonas Geda, Bradley Boeve, Walter Rocca, Ronald Petersen, Clifford Jack 4:30 p.m. S58.006 Factor Scores for Brain Reserve, Alzheimer and Vascular Pathology Are Independent Risk Factors for Dementia in a Populationbased Cohort Study: The Kame Project Amy Borenstein, James Mortimer, Eric Larson 4:45 p.m. S58.007 Impaired Cerebral Autoregualtion Is Associated with a Greater 7-year Decline in Gait Speed in an Elderly Population: The MOBILIZE Boston Study Farzaneh Sorond, Sushmita Purkayastha, Lewis Lipsitz, Suzanne Leveille Scientific Sessions 3:15 p.m. S59.001 Malformation Risks of Antiepileptic Drug Monotherapies in Pregnancy: An Update from the UK and Ireland Epilepsy and Pregnancy Registers Ellen Campbell, Fiona Kennedy, Aline Russell, W Smithson, Linda Parsons, Beth Irwin, Brenda Liggan, Norman Delanty, Patrick Morrison, Stephen Hunt, John Craig, Jim Morrow 3:30 p.m. S59.002 Congenital Malformations in Infants Born to Women with Epilepsy at Boston Medical Center Gina Deck, Alexandra Lovett, Neil Nadkarni, Georgia Montouris 3:45 p.m. S59.003 Drivers for Epilepsy Readmissions: A Retrospective Cohort Study Tracie Caller, Jasper Chen, Jessica Harrington, Barbara Jobst 4:00 p.m. S59.004 Antiepileptic Drug Prescribing for OEF/OIFVeterans with New-onset Epilepsy: 2008-2010 Mary Jo Pugh, Anne Van Cott, Christine Baca, Megan Amuan 4:15 p.m. S59.005 Factors Independently Associated with Anxiety and Depression in Epilepsy Heidi Munger Clary, Marla Hamberger 4:30 p.m. S59.006 Comparison of Heart Rate Variability Parameters Between Partial and Idiopathic Generalized Epilepsy Patients in the Interictal Period Kadriye Agan, Aslihan Ergun, Altug Cincin, Damla Ozbek Cetinkaya, Hatice Omercikoglu Ozden, Alper Kepez, Osman Yesildag, Ipek Midi 4:45 p.m. S59.007 Influences of Temporal Lobe Epilepsy and Temporal Lobe Resection on Olfactory Function Richard Doty, Isabelle Tourbier, Taehoon Kim, Jonathan Silas, Paul Moberg, Ashwini Sharan, Michael Sperling, Bruce Turetsky S60 Child Neurology II 3:15 p.m. S60.001 Evidence of Impaired Age-expected Growth and Atrophy of the Cerebellum in Pediatric Patients with Monophasic Acquired Demyelinating Syndrome and Multiple Sclerosis Katrin Weier, Vladimir Fonov, Bérengère Aubert-Broche, Douglas Arnold, Brenda Banwell, D. Collins S61 Muscle Disease: Gene Therapy and Models 3:15 p.m. S61.001 Restoration of Dystrophin Expression in a Novel Duchenne Mouse Model, the Dup2 Mouse, by IresMediated Translation of a Highly Functional N-truncated Dystrophin Protein Kevin Flanigan, Adeline Vulin-Chaffiol, Nicolas Wein, Paul Janssen 3:30 p.m. S60.002 Incidence of Early Seizures with Levetiracetam Prophylaxis in Children After Traumatic Brain Injury Melissa Chung, Nicole O’Brien 3:30 p.m. S61.002 β-Sarcoglycan Gene Transfer Leads to Functional Improvement in a Model of LGMD2E Eric Pozsgai, Danielle Griffin, Kristin Heller, Jerry Mendell, Louise Rodino-Klapac 3:45 p.m. S60.003 Incidence of Epilepsy Following Perinatal Stroke: A Prospective Cohort Study Rebecca Ichord, Niharika Gupta, Michael Uohara, Lori Billinghurst, Daniel Licht, Lauren Beslow 3:45 p.m. S61.003 MicroRNA-29 Overexpression Delivered by Adeno-Associated Virus Suppresses Fibrosis in mdx:utrn +/Mice Eric Meadows, Janaiah Kota, Vinod Malik, Reed Clark, Zarife Sahenk, Scott Harper, Jerry Mendell 4:00 p.m. S60.004 Viral Infections during Pregnancy: a Risk Factor for the Development of Concurrent Autism and Epilepsy in the Offspring Raman Sankar, Andrey Mazarati, James Washington III, Eduardo Pineda, Don Shin 4:00 p.m. S61.004 AAV Gene Transfer Utilizing Homologous Overlap Vectors Mediates Functional Recovery of Dysferlin Deficiency Patricia Sondergaard, Eric Pozsgai, Danielle Griffin, Jerry Mendell, Louise Rodino-Klapac 4:15 p.m. S60.005 Predictors of Outcome in a Large Cohort of Infantile Spasms of Unknown Cause Christopher Yuskaitis, Maura Madou, Katherine Howell, Annapurna Poduri, Elliott Sherr 4:15 p.m. S61.005 Fhl1 W122S Knock-in Mice Manifest Late-onset Mild Myopathy Valentina Emmanuele, Akatzuki Kubota, Beatriz Garcia-Diaz, Caterina Garone, Orhan H. Akman, Kurenai Tanji, Catarina Quinzii, Michio Hirano 4:30 p.m. S60.006 Pellagra-like Syndrome Proves to be a Variant of Xeroderma PigmentosumCockayne Syndrome and Niacin Confers Clinical Benefit Mustafa Salih, Hadia Hijazi, Muddathir Hamad, Hamdy Hassan, Shinu Ansari, Fowzan Alkuraya 4:45 p.m. S60.007 Presurgical Evaluations in Children with Pathology Confirmed Focal Cortical Dysplasia Anna Mrelashvili, Katherine Nickels, Elaine Wirrell, Lily Wong-Kisiel 4:30 p.m. S61.006 Impaired Muscle Regeneration in CAPN3-KO Mice Related to MicroRNA Dysregulation Zarife Sahenk, Cilwyn Braganza, Lei Chen, Syed-Rehan Hussain, Eric Meadows, Sarah Lewis, Kevin Flanigan, K. Reed Clark, Jerry Mendell 4:45 p.m. S61.007 Mutations in Zaspopathy Cause Disruption of Actinin-Crosslinked Actin Filaments, the Core Structure of Skeletal Muscle Z-discs Xiaoyan Lin, Janelle Ruiz, Ilda Bajraktari, Rachel Ohman, Robert Griggs, Kenneth Fischbeck, Ami Mankodi S62 Cerebrovascular Disease and Interventional Neurology: Cognitive and Behavioral 3:15 p.m. S62.001 Post-Surgical Cognitive Outcomes Tania Giovannetti, Molly Fanning, Sarah Ratcliffe, Catherine Price, Steven Messe, Ola Selnes, Michael Acker, Thomas Floyd, Wilson Szeto, Joseph Bavaria 3:30 p.m. S62.002 Antiphospholipid Antibodies, Brain Infarcts, and Cognitive and Motor Decline in Aging (ABICMA): Final Cerebral Infarct Results from a Community-Based, Longitudinal, Clinical-Pathological Study Steven Levine, Zoe Arvanitakis, Robin Brey, Jacob Rand, Julie Schneider, Lei Yu, Sue Leurgans, David Bennett 3:45 p.m. S62.003 Elevated Blood Pressure and Risk of Incident Amnestic Mild Cognitive Impairment/Alzheimer’s Disease Steven Edland, Guerry Peavy, David Salmon, Douglas Galasko 4:00 p.m. S62.004 Influence of Pre-Existing Cognitive Impairment on the Outcome of Stroke Patients Treated by Thrombolytic Therapy. Results of the OPHELIECOG Study Kei Murao, Didier Leys, Solene Moulin, Yasushi Okada 4:15 p.m. S62.005 Early Depression Screening Is Feasible in Hospitalized Stroke Patients Rahul Karamchandani, Farhaan Vahidy, Suhas Bajgur, Kim Yen Thi Vu, H. Alex Choi, Adeolu Oladunjoye, Robert Hamilton, Sean Savitz 4:30 p.m. S62.006 Pre-Existing and Incident Cerebral Microbleeds Are Associated with Progression of Ischemic Vascular Lesions Saloua Akoudad, Mohammad Ikram, Peter Koudstaal, Albert Hofman, Wiro Niessen, Steven Greenberg, Aad Van Der Lugt, Meike Vernooij 4:45 p.m. S62.007 Comparing Semi-quantitative and Volumetric Measurements of MRI White Matter Hyperintensities: The Northern Manhattan Study Carly Oboudiyat, Hannah Gardener, Chensy Marquez, Mitchell Elkind, Ralph Sacco, Charles DeCarli, Clinton Wright S63 Neuromyelitis Optica and Autoimmune Encephalitis 3:15 p.m. S63.001 Revised Diagnostic Criteria for Neuromyelitis Optica Spectrum Disorders Dean Wingerchuk, Brenda Banwell, Jeffrey Bennett, Philippe Cabre, William Carroll, Tanuja Chitnis, Jerome De Seze, Kazuo Fujihara, Benjamin Greenberg, Anu Jacob, Sven Jarius, Marco Lana-Peixoto, Michael Levy, Jack Simon, Silvia Tenembaum, Anthony Traboulsee, Patrick Waters, Kay Wellik, Brian Weinshenker 3:30 p.m. S63.002 Differentiating NMO and MSassociated Optic Neuritis by MRI Maureen Mealy, Anna Whetstone, Peter Calabresi, Michael Levy 3:45 p.m. S63.003 Clinical and Demographic Features of Children with NMO: Report from the U.S. Network of Pediatric MS Centers of Excellence Tanuja Chitnis, Jayne Ness, Lauren Krupp, Emmanuelle Waubant, Tyler Hunt, Moses Rodriguez, Timothy Lotze, Mark Gorman, Anita Belman, Bianca Weinstock-Guttman, Marc Patterson, John Rose, Charlie Casper 4:00 p.m. S63.004 AQP4-IgG Assays Comparison in Laboratory Clinical Serivce James Fryer, Vanda Lennon, Sean Pittock, Sarah Jenkins, Stacey Clardy, Erika Horta, Eric Jedynak, Claudia Lucchinetti, Elizabeth Shuster, Brian Weinshenker, Dean Wingerchuk, Andrew McKeon 4:15 p.m. S63.005 Therapeutic Effect of Plasma Exchange (PLEX) in Neuromyelitis Optica (NMO): Immediate and Long Term Response Moogeh Baharnoori, Marika Hohol, Katerina Pavenski, Paul O’Connor 4:30 p.m. S63.006 Neuromyelitis Optica Spectrum with Autoantibodies Against Myelin-Oligodendrocyte Glycoprotein have Distinct Clinical Features and Prognosis from Seronegative Patients Douglas Sato, Dagoberto Callegaro, Marco Lana-Peixoto, Patrick Waters, Satoru Tanaka, Frederico Jorge, Toshiyuki Takahashi, Tatsuro Misu, Samira Apostolos-Pereira, Natalia Talim, Renata Simm, Angelina Lino, Ichiro Nakashima, Kyoichi Nomura, Masashi Aoki, Kazuo Fujihara 4:45 p.m. S63.007 From Behavior to Synapse: A Murine Model of Passive Transfer of Antibodies from Patients with Anti-NMDAR Encephalitis Mannara Francesco, Javier Gutierrez Cuesta, Frank Leypoldt, Jesús Planagumà, Elena Martín García, Ankit Jain, Francesc Graus, Rita Balice-Gordon, Rafael Maldonado Lopez, Josep Dalmau Fast, Easy Registration Online · AAN.com/view/AM14 127 Thursday May 1 S59 Epilepsy and Clinical Neurophysiology (EEG): Reproduction, Health Care Delivery, and Co-morbidities Thursday, May 1 1 Current as of 2/13/2014 Controversies in Neurology Plenary Session 5:30 p.m.–7:00 p.m. The program features experts discussing the most current and controversial issues in neurology. It is set up as a series of debates in which two speakers argue opposing sides of a single topic, followed by a rebuttal. Each round concludes with a 10-minute question and answer period. Moderators: Joseph Jankovic, MD, FAAN Member, Science Committee Walter A. Rocca, MD, MPH Member, Science Committee; Chair, Clinical Research Subcommittee Does Preventing Relapses Protect Against Progressive MS? Pro: Maria Trojano, MD University of Bari, Bari, Italy Con: Helen Tremlett, PhD, BPharm University of British Columbia, Vancouver, BC, Canada Is Intervention for Asymptomatic AVM Useful? Pro: Robert M. Friedlander, MD UPMC Presbyterian, Pittsburgh, PA Con: J. P. Mohr, MD, FAAN Columbia University, New York, NY Should Neurologists Prescribe Marijuana for Neurological Disorders? Pro: Barbara S. Koppel, MD, FAAN Metropolitan Hospital, Rye, NY Con: John C. M. Brust, MD, FAAN New York Neurological Institute, New York, NY For Full Abstracts and Bios for Plenary Speakers Visit AAN.com/view/SearchAM 128 2O14 Scientific Abstract Listing and Annual Meeting Information Friday, May 2 Integrated Neuroscience Session Proteinopathy in Neurodegenerative Disease I11 8:00 a.m.–12:00 p.m. Coordinators: Carol F. Lippa, MD, and David G. Munoz, MD Invited Speaker Session: 8:00 a.m.–10:30 a.m. 8:00 a.m.–8:15 a.m. Neurodegenerative Disease: Past, Present, and Future David G. Munoz, MD 8:15 a.m.–8:45 a.m. Bioenergetic Consequences of Protein Misfolding in Neurodegenerative Diseases M. Flint Beal, MD, FAAN 8:45 a.m.–9:15 a.m. Molecular Correlates of Alzheimer Progression Bradley T. Hyman, MD, PhD 9:15 a.m.–9:45 a.m. Alpha-Synuclein Associated Mechanisms of Neuronal Injury: The Mitochondrial Link J. Timothy Greenamyre, MD, PhD 9:45 a.m.–10:15 a.m. Prion-like Diseases: The Future is Unfolding Neil R. Cashman, MD 10:15 a.m.–10:30 a.m. Panel Discussion Poster Rounds: 10:30 a.m.–11:30 a.m. I11-1.001 An Abeta Oligomer Receptor Antagonist and Antibodies to Specific Target Receptor Epitopes Displace Abeta Oligomers in Alzheimer’s Patient Brain Tissue Sections Susan Catalano, Nicholas Izzo, Courtney Rehak, Raymond Yurko, Kelsie Mozzoni, Colleen Silky, Gary Look, Gilbert Rishton, Hank Safferstein, Tara Spires-Jones I11-1.002 Imaging Tau Pathology in Vivo in FTLD: Initial Experience with (18F) T807 PET Bradford Dickerson, Kimiko Domoto-Reilly, Daisy Hochberg, Michael Brickhouse, Michael Stepanovic, Keith Johnson I11-1.003 A CSF Signature of Frontotemporal Lobar Degeneration with C9orf72 Repeat Expansions William Hu, Jonathan Glass, Vivianna Van Deerlin, Murray Grossman, Kelly Watts, James Lah, John Trojanowski, Allan Levey I11-1.004 Progressive Supranuclear Palsy (PSP): Diagnosis Through Skin Biopsy Ildefonso Rodriguez-Leyva, Ana Calderon-Garcidueñas, Martha Santoyo, Erika Chi, Verónica Medina-Mier, Maria Jimenez-Capdeville I11-1.006 Complement Factor H Is a Biomarker for Mild Cognitive Impairment Not Due to Alzheimer’s Disease Trung Nguyen, Kelly Watts, James Lah, Jonathan Glass, Allan Levey, William Hu I11-1.007 Cytoplasmic Redistribution of Mutant TDP-43 in a BAC Based Mouse Model of Amyotrophic Lateral Sclerosis Kevin Talbot, David Gordon, Ruxandra Mutihac, Javier AlegreAbarrategui, Lucy Farrimond, Ben Davies, Richard Wade-Martins I11-1.005 Spinocerebellar Ataxias I11-1.008 Coenzyme Q10, Statin, and Spinocerebellar Ataxias Sheng-Han Kuo, Raymond Lo, Karla Figueroa, Stefan Pulst, Susan Perlman, George Wilmot, Christopher Gomez, Jeremy Schmahmann, Henry Paulson, Vikram Shakkottai, Sarah Ying, Theresa Zesiewicz, Khalaf Bushara, Michael Geschwind, Guangbin Xia, S Subramony, Tetsuo Ashizawa I11-1.009 Epigenetic Mechanisms Linking Diabetes and Synaptic Plasticity Giulio Pasinetti I11-1.010 PACAP Deficit in Alzheimer’s with Hypogonadism: Unraveling a Novel Group of Inherited Neurometabolic Disorders Charles Lourenco, Claudia Sobreira, Roberto Giugliani, Stephan Zuchner, Wilson Marques, Jr. Disease and Protection Against BetaAmyloid Toxicity PengCheng Han, Zhiwei Tang, Jun-Xiang Yin, Thomas Beach, Eric Reiman, Jiong Shi Data Blitz: 11:30 a.m.–12:00 p.m. 11:30 a.m. 1II-2.001 11:35 a.m. 1II-2.002 RER1: A Novel Regulator of AlphaSynuclein Nikolaus McFarland, Hyo-Jin Park, Lauren Ricchiuti HuR Is Essential for TDP-43 Expression Through Posttranscriptional Mechanisms: Implications for Motor Neuron Toxicity and ALS Liang Lu, Lei Zheng, Ying Si, Shin Oh, Peter King 11:40 a.m. 1II-2.003 α-Synuclein in Red Blood Cells Is a potential Diagnostic Biomarker for Parkinson’s Disease Rodolfo Savica, Roy Dyer, Michelle Mielke, Bryan Klassen, Bradley Boeve, George Klee, J. Ahlskog, Walter Rocca, Marina Ramirez-Alvarado 11:45 a.m. 1II-2.004 Isradipine Rescues Alpha-synuclein Toxicity in a Zebrafish Model of Parkinson’s Disease by Upregulating Autophagy Mark Stahl, Shubhangi Prabhudesai, Aaron Lulla, Jeff Bronstein 11:50 a.m. Education Program Syllabi Full text syllabi and program slides will be available electronically only—online or via the Annual Meeting mobile app. All registered attendees will receive an email notification once syllabi are available. 130 2O14 Scientific Abstract Listing and Annual Meeting Information 1II-2.005 GGGGCC Repeat Expansion of C9ORF72 Is Toxic Via Sequestration of RNA Binding Proteins and Consequent Disruption of RNA Splicing Johnathan Cooper-Knock, Matthew Walsh, Adrian Higginbottom, J Robin Highley, Joanna Bury, Mark Dickman, Magnus Rattray, Paul Heath, Matthew Wyles, Paul Ince, Stephen Wharton, Stuart Wilson, Janine Kirby, Guillaume Hautbergue, Pamela Shaw Plenary Session Current as of 2/13/2014 Clinical Trials Plenary Session 12:00 p.m.–1:30 p.m. This mid-day session covers important clinical topics that affect patient care identified from other society meetings. The latest updates within several clinical trials conducted over the course of the last year will be presented with an open panel discussion at the conclusion. Moderators: Natalia Sana Rost, MD, FAAN Vice-Chair, Science Committee The Idiopathic Intracranial Hypertension Treatment Trial: A Multicenter, DoubleBlind, Randomized Clinical Trial Comparing Acetazolamide and Placebo on Visual Outcome Michael Wall, MD, FAAN University of Iowa, Iowa City, IA Anti-angiogenic Therapy for Glioblastoma: A Randomized, DoubleBlinded Phase III Trial of Bevacizumab in Newly Diagnosed Patients Mark R. Gilbert, MD The University of Texas MD Anderson Cancer Center, Houston, TX TOPIC: Efficacy and Safety of Once-daily Oral Teriflunomide in Patients with First Clinical Episode Consistent With Multiple Sclerosis Petra Kaufmann, MD Member/Federal Liaison, Clinical Research Subcommittee FAST-MAG Trial in Acute Ischemic Stroke Jeffrey L. Saver, MD, FAAN UCLA School of Medicine, Los Angeles, CA CGRP Monoclonal Antibody LY2951742 for the Prevention of Migraine: A Phase 2, Randomized, Double-Blind, Placebo-Controlled Study avid Dodick, MD D Mayo Clinic, Phoenix, AZ Randomized, Double-blind, Placebo-controlled Trial of ALD403: An Anti-CGRP Peptide Antibody in the Prevention of Frequent Episodic Migraine Peter Goadsby, MD, PhD University of California, San Francisco, CA Aaron E. Miller, MD, FAAN Mt. Sinai School of Medicine, New York, NY For Full Abstracts and Bios for Plenary Speakers Visit AAN.com/view/SearchAM Fast, Easy Registration Online · AAN.com/view/AM14 131 Section Topic Controversies/ Integrated Neuroscience Friday, May 2 S64 Section Topic Controversies: Pain: Methods of Treatment 1:00 p.m.–2:30 p.m. 1:00 p.m.–1:05 p.m.Introduction Guy Burrows, MD 1:50 p.m.–2:05 p.m. Headache: Classification Morris Levin, MD 1:05 p.m.–1:20 p.m. Interventional Pain Procedures for Headache and Facial Pain Syndromes Charles Brock, MD 2:05 p.m.–2:25 p.m. Panel Discussion 2:25 p.m.–2:30 p.m.Conclusion Guy Burrows, MD 1:20 p.m.–1:35 p.m. Pain Connection with Sleep Disorders lon Avidan, MD, MPH A 1:35 p.m.–1:50 p.m. Opioids in Neurology Practice C hristopher Gibbons, MD Concussion in Sports and the Military I12 1:00 p.m.–5:00 p.m. Coordinators: Anthony G. Alessi, MD, FAAN, and Jack W. Tsao, MD, DPhil, FAAN Invited Speaker Session: 1:00 p.m.–3:30 p.m. 1:00 p.m.–1:10 p.m.Introduction 1:10 p.m.–1:40 p.m. Headaches Following Concussion Tad Seifert, MD 1:40 p.m.–2:10 p.m. Imaging Following Concussion Gary Small, MD, PhD 2:10 p.m.–2:40 p.m. Sleep Disturbances Following Concussion Joseph Krainin, MD 2:40 p.m.–3:10 p.m. Blast Effects Causing TBI and Role of Blast Sensors Geoffrey Ling, MD, PhD, FAAN 3:10 p.m.–3:30 p.m. Questions and Answers Poster Rounds: 3:30 p.m.–4:30 p.m. I12-1.001 fMRI Neuropsychological I12-1.004 Alterations in Network I12-1.002 Etiology and Epidemiology of I12-1.005 Structural Imaging Battery for Athletes with Concussion David Hubbard, Adam Hampshire, Adrian Owen Traumatic Brain Injury in Relation to Gender Differences Among African American Patients Lien Diep, Robert Farney, Stacy Cary-Thompson, Jean Belcourt, Robert Farney, Janaki Kalyanam, Annapurni JayamTrouth I12-1.003 Is There Chronic Brain Damage in Retired NFL Players? Neuroradiology, Neuropsychology and Neurology of 45 Retired Players Ira Casson, David Viano, E. Mark Haacke, Zhifeng Kou, Danielle LeStrange Dynamics Following Blast-Induced Mild Traumatic Brain Injury Andrei Vakhtin, Paul Taylor, Corey Ford Correlations with Memory Assessment and Concussion in Retired NFL Athletes Kyle Womack, Jeremy Strain, Nyaz Didehbani, Heather Conover, Michael Kraut, Munro Cullum, John Hart I12-1.006 Progressive Return to Activity Following Acute mTBI: A Standardized Approach Robert Labutta, Therese West, Helen Coronel, Katherine Helmick I12-1.007 Axonal Injury, Neuroinflammation and Amyloid Pathology After Traumatic Brain Injury: Making Connections to Neurodegeneration David Sharp, Gregory Scott, Ramlackasingh Anil, Hellyer Peter, Leech Robert, Federico Turkheimer, Paul Matthews, David Brooks I12-1.008 Neural Correlates of Cognitive Anosognosia in Veterans with Mild Traumatic Brain Injury (mTBI) Mohammed Ahmed, Ihtsham Haq, Robin Hurley, Katherine Taber, Jared Rowland, Ruth Yoash-Gantz, Stephen Kramer I12-1.009 Comparison of Headache in OEF/OIF Veterans with Traumatic Brain Injury (TBI) Against Controls Matched for Age, Sex, Race, and Deployment Time James Couch, Kenneth Stewart I12-1.010 The King-Devick Test Is Vastly Superior to the Symbol Digit Modalities Test as a Sideline Determinant of Concussion in Mixed Martial Arts Fighters Daniel Kantor Data Blitz Session: 4:30 p.m.–5:00 p.m. 4:30 p.m. I12-2.001 Effect of Concussion and Blast Exposure on Clinical Symptoms Following Deployment of U.S. Military Personnel Mikias Wolde, Briana Perry, Jay Haran, Justin Campbell, Alia Creason, Catalina Sher, Lauren Stentz, Jack Tsao 132 4:35 p.m. I12-2.002 The Natural History of Acute Recovery of Blast-induced Mild Traumatic Brain Injury: A Case Series During War Jason Hawley, David Larres, Elizandro Gonzales, Walter Carr 4:40 p.m. I12-2.003 4:45 p.m. I12-2.004 Field Utilization of the Cleveland Clinic Concussion iPad Assessment Tool Jay Alberts, Joshua Hirsch, Susan Linder, David Schindler Development of a Medical Device for the Rapid Assessment of Concussion Donald Weaver, Ying Tam, Christopher Barden, Ryan D’Arcy, Love Kalra, Lauren Petley, Chen Wei 2O14 Scientific Abstract Listing and Annual Meeting Information 4:50 p.m. I12-2.005 Vision Testing Is Additive to the Sideline Assessment of Sports-Related Concussion Rachel Ventura, Zoe Marinides, Steven Galetta, James Clugston, Laura Balcer Plenary Session Current as of 2/13/2014 Neurology Year in Review Plenary Session 5:30 p.m.–7:00 p.m. This plenary session will feature six speakers, each focusing on the latest research that has happened in the last year within a specific subspecialty topic. Moderator: Lisa M. DeAngelis, MD, FAAN Chair, Science Committee Multiple Sclerosis Movement Disorders Anne H. Cross, MD Washington University School of Medicine, St. Louis, MO Kathleen M. Shannon, MD Rush University Medical Center, Chicago, IL Headache/Pain Neurocritical Care Peter Goadsby, MD, PhD UCSF, San Francisco, CA David M. Greer, MD Yale University School of Medicine, New Haven, CT Neuromuscular Alzheimer’s Disease Robert C. Griggs, MD, FAAN University of Rochester, Rochester, NY Todd E. Golde, MD, PhD University of Florida, Gainesville, FL For Full Abstracts and Bios for Plenary Speakers Visit AAN.com/view/SearchAM Fast, Easy Registration Online · AAN.com/view/AM14 133 AANonDemand.com/premeeting 2O14 Annual Meeting On Demand AAN is pleased to offer three educational products to enhance your experience at this year’s Annual Meeting. 1. Best Value: AAN Annual Meeting On Demand— is the comprehensive digital library of content with more than 500 hours* of presentations from the 2014 AAN Annual Meeting educational programs (including the Syllabi on CD and Neurology Update On Demand library). Watch presenters’ slides while listening to fully synchronized audio as if you were actually attending each session. Features of AAN Annual Meeting On Demand include: ¡¡ Online access to content within 24 hours of live presentations ¡¡ Streaming content for viewing on iPad® and most mobile devices ¡¡ Companion portable hard drive for offline access (shipped after the meeting) ¡¡ Downloadable MP3 files for convenient on-the-go audio (listen in the car, or on your MP3 player) ¡¡ Advanced Search: Search any word on the slides and immediately jump to that part of the presentation 2. Neurology Update On Demand— offers a paired-down library of approximately 70 hours* of presentations focused on the latest updates in the field of neurology. Sessions in this online only catalog will be available within 24 hours of the live presentation. Save $100 or more off the list price (savings depend on membership status and registration category). 3. Syllabi on CD— serves as a quick reference tool with syllabi summaries of more than 160 programs presented during the 2014 Annual Meeting for only $299. * T otal hours of presentations available subject to speaker permissions. Pre-order now to save with deep discounts. AAN Annual Meeting On Demand + Syllabi Online, Portable Hard Drive, Mobile Streaming $1,599 (List Price) $599 (save $1,000) $699 (save $900) $399 (save $1,200) $899 (save $700) Member Attendee before May 3, 2014 Nonmember Attendee before May 3, 2014 Junior Attendee before May 3, 2014 Non Attendee before May 3, 2014 Syllabi CD CD Neurology Update Online, Mobile Streaming $299 (List Price) $249 (save $50) $299 $99 (save $200) $299 $599 (List Price) $399 (save $200) $499 (save $100) $249 (save $250) $499 (save $100) To lock in the best prices, purchase the AAN Annual Meeting on Demand when you register for the 2014 Annual Meeting at AAN.com/view/register Order one of three ways: 1. When you register for the Annual Meeting online you are able to conveniently add the on demand products you wish to purchase. Register for the Annual Meeting and purchase these on demand products at AAN.com/view/register. 2. If you are not attending this year’s Annual Meeting, you are still able to purchase on demand products to see what you missed! Visit AANonDemand.com/PreMeeting to learn more and purchase. 3. Or call us at (800) 501-2303 or (818) 844-3299. Monday–Friday, 6:00 a.m.–5:00 p.m. PST. Fast, Easy Registration Online · AAN.com/view/AM14 135 Connect at Social Events There’s no better way to combine an evening of great fun and entertainment with unparalleled networking than to attend the Opening Party, Closing Party—or both. Whether you attend the Annual Meeting at the beginning of the week, or the end, the events are not-to-be-missed. Comedy Show: The Water Coolers 8:30 p.m.–10:00 p.m. Opening Party Sunday, April 27 6:00 p.m.–10:00 p.m. Join your friends and colleagues for an exciting evening filled with delicious food, beverages, and entertainment. Each registered meeting attendee will receive one free ticket to these events. Guest tickets are available through registration for $50. Neurobowl® 6:00 p.m.–8:00 p.m. This popular event hosted by AAN former president Thomas R. Swift, MD, FAAN, is one of the Annual Meeting’s premier happenings. Neurobowl showcases the best and brightest in neurology competing for the coveted Neurobowl trophy in an entertaining game-show format. Ever start your day with 300 meetings scheduled, 700 emails in your inbox, and a soccer game at 3:00? Join the Water Coolers, the music and comedy act E Entertainment calls “the hottest ticket in town,” for a hilarious evening of laughout-loud song and sketch comedy that answers the question “does this stuff happen to anyone else?” Closing Party Friday, May 2 7:30 p.m.–9:00 p.m. Celebrate the end of a great meeting with the Closing Party! Each registered meeting attendee will receive one free ticket to this event. Guest tickets are available through registration for $50. Musical Entertainment 7:30 p.m.–9:00 p.m. NFL star-turned-singer—and Public Leadership in Neurology Awardwinner—Ben Utecht will enchant you with his inimitable vocal stylings. After winning a Super Bowl ring in 2007, his career ended unexpectedly after a traumatic brain injury in 2009. Many saw this as an ending, but Ben saw an opportunity to pursue another lifelong passion—singing. Exhibit Hall Opening Reception Main Stage: JellyRoll 8:30 p.m.–10:00 p.m. Don’t miss this high-energy, 11-piece band that will get your feet moving with a repertoire including material from the classics to the newest top 40 hits. Fronted by the JellyRoll vocalists, driven by The JellyRoll Horns and Philadelphia’s tightest rhythm section, the awardwinning JellyRoll has won over audiences from Madison Square Garden in New York City to the White House in Washington, DC, with their unique blend of dance music. 136 Monday, April 28 4:30 p.m.–6:30 p.m. Attend the opening reception to mingle with fellow attendees and preview the latest products and services available in the neurologic industry. Light hors d’oeuvres and beverages will be served. The exhibits will be open at this time. 2O14 Scientific Abstract Listing and Annual Meeting Information Current as of 1/31/2014 –Programs and dates are subject to change American Academy of Neurology and American Brain Foundation Awards Luncheon Wednesday, April 30 12:00 p.m.–1:30 p.m. Public Leadership in Neurology Award Winner Ben Utecht Run/Walk For Brain Research Tuesday, April 29 6:30 a.m.–8:30 a.m. Support research in neurology and join us for a 5k run or onemile walk along the Philadelphia waterfront. Both occasional and seasoned runners—and walkers—will enjoy this beautiful trek for a good cause. All proceeds will go to the American Brain Foundation to help support research. The race is open to all meeting attendees and their families. Water and refreshments will be available following the race. The registration fee is $25. More information about this event will be posted as it becomes available on AAN.com/view/AMEvents. Bus service to and from the race site will be provided. For registration and details, visit AAN.com/view/RunWalk or contact Andrew Halverson at ahalverson@aan.com or (612) 928-6117. Reunion/Alumni Meetings Reconnect with your peers and program directors, and network with your fellow alumni at various department reunion meetings occurring throughout the Annual Meeting. If your department is interested in hosting its alumni meeting during the 2014 Annual Meeting, reserve your meeting today at AAN.com/view/alumni or by contacting Tammi Sand at tsand@aan.com or (612) 928-6136. NFL star-turned-singer Ben Utecht will receive the American Brain Foundation’s 2014 Public Leadership in Neurology Award for his commitment to spreading the word about how concussions and traumatic brain injury have affected his life. After winning a Super Bowl ring in 2007, his career ended unexpectedly after a traumatic brain injury in 2009. Many saw this as an ending, but Ben saw an opportunity to pursue another lifelong passion—singing. Join AAN leaders as they honor the recipients of the 2014 AAN and American Brain Foundation Awards. From enterprising high school students to world-renowned researchers, this program recognizes some of the top accomplishments in neuroscience research. Past keynote speakers on the importance of neurologic diseases include Billy McLaughlin, Tedy Bruschi, Dame Julie Andrews, Cuba Gooding Jr., Leeza Gibbons, and Michael J. Fox. Tickets are available for $60 through registration. Students and Junior members of the AAN may attend this event at no cost by requesting a ticket. Buy a ticket and show your support for award recipients. Reserve a Department Table and Be Recognized Bring your department together and gain exposure for your team at the Awards Luncheon by reserving a department table. Give your residents and fellows the chance to sit together with department faculty and chairs in a place of honor among the top minds in the neurology/neuroscience academic community. For questions, contact Laurie Dixon at ldixon@aan.com or (612) 928-6154. Yoga Sessions Need to relax before a day filled with the latestbreaking science and the best in education? Yoga sessions will be offered Sunday and Monday from 6:30 a.m.-7:30 a.m. If you need to unwind after the day we will be offering a Wednesday evening Yoga session from 5:00 p.m.-6:00 p.m. The registration fee is $10 per session. For registration and details please visit AAN.com/view/AMEvents. Fast, Easy Registration Online · AAN.com/view/AM14 137 Highlights for Students, Residents, and Fellows The AAN Annual Meeting is an ideal setting for students, residents, and fellows to gain exposure to a variety of interests and career disciplines, as well as network with leading neurologists and neurology professionals from around the world. Registration FREE for Medical Students Annual Meeting registration is FREE to medical students, graduate students, and PhD candidates who present a student ID card or are AAN members. Only $100 for Junior Residents and Junior Fellows 2014 Medical Students, Residents, and Fellows Guide Annual Meeting registration is only $100 (a $740 savings from nonmember neurologist registration!) before the April 3, 2014, early registration deadline. Opportunities to Save Money Rush Line Tickets Check in at the Registration Booth located in the Convention Center each morning for FREE tickets to Education Programs for that day. A minimum of two tickets will be held for each program available on a first-come, first-served basis. nts, ical Stude 2014 Med llows Guide , and Fe Residents Co nn ec tin uro log g All of Ne y 3, 2014 26 – Ma y • Ap ril hia , PA Phi lad elp Get 50% Off Education Program Registration Junior members who register for two Education Programs at full price will receive 50% off the cost of a third Education Program of equal or lesser value. Volunteer Opportunities Serve as a program monitor or a workshop volunteer to gain free access to the specific program (see page 142). A detailed guide highlighting all events and opportunities of interest to Students, Residents, and Fellows is available at AAN.com/view/resident. “[The Annual Meeting Science Programs give me] a lot of exposure to different researchers and to different work that people do in the field of neurology. When you come to this place, you are exposed to everything: the cutting-edge science, the new techniques, the basically new science, the new indications, the new guidelines.” Mohamed El Hag, MD (Resident) Cleveland, OH 138 2O14 Scientific Abstract Listing and Annual Meeting Information There’s no better way to combine an evening of great fun and entertainment with unparalleled networking than to attend the Opening Party, Closing Party—or both! Whether you attend the Annual Meeting at the beginning of the week, or the end, these parties are not-to-be-missed. Opening Party Sunday, April 27 6:OO p.m.–1O:OO p.m. Join your friends and colleagues for an exciting evening filled with entertainment, including: Neurobowl® 6:OO p.m.–8:OO p.m. This popular event is one of the Annual Meeting’s premier happenings. Neurobowl® showcases the best and brightest in neurology competing for the coveted Neurobowl® trophy in an entertaining game-show format. Main Stage Music: JellyRoll 8:3O p.m.–1O:OO p.m. Don’t miss this high-energy, 11-piece band that will get your feet moving with a repertoire including material from the classics to the newest top 40 hits. Fronted by the JellyRoll vocalists, driven by The JellyRoll Horns and Philadelphia’s tightest rhythm section, the award-winning JellyRoll has won over audiences from Madison Square Garden in New York City to the White House in Washington, DC, with their unique blend of dance music. Comedy Show: The Water Coolers 8:3O p.m.–1O:OO p.m. Ever start your day with 300 meetings scheduled, 700 emails in your inbox, and a soccer game at 3:00? Join The Water Coolers, the music and comedy act E Entertainment calls “the hottest ticket in town,” for a hilarious evening of laugh-out-loud song and sketch comedy that answers the question “does this stuff happen to anyone else?” Closing Party Friday, May 2 7:3O p.m.–9:OO p.m. Musical Entertainment Former NFL star-turned-singer and Public Leadership in Neurology Award-winner Ben Utecht will enchant you with his inimitable vocal stylings. General Information CME/Accreditation/Core Competencies Accreditation The American Academy of Neurology Institute (AANI), the education subsidiary of the American Academy of Neurology, is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education (CME) for physicians. AMA Credit Designation The AANI designates this live activity for a maximum of (*) AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. *See individual program descriptions in this booklet for the maximum number of credits per program. CME/Participation Records knowledge, skills, and professional performance and relationships that a physician uses to provide services for patients, the public or the profession. The content of CME is the body of knowledge and skills generally recognized and accepted by the profession as within the basic medical sciences, the discipline of clinical medicine, and the provision of health care to the public. (HOD policy #300.988) Certified CME is defined as: 1.Nonpromotional learning activities certified for credit prior to the activity by an organization authorized by the credit system owner, or 2.Nonpromotional learning activities for which the credit system owner directly awards credit Accredited CME providers may certify nonclinical subjects (e.g., office management, patient-physician communications, faculty development) for AMA PRA Category 1 Credit™ as long as these are appropriate to a physician audience and benefit the profession, patient care, or public health. AANI has mechanisms in place to record, and when authorized by the participating physician, verify participation in the CME activity. To receive CME for the Annual Meeting live program, participants must: (1) register for the program(s); (2) attend the program(s); (3) submit the evaluation form for the program(s). CME is given only when all three steps are completed. AAN member CME and participation transcripts are available approximately four to six weeks following the close of the meeting via the AAN’s NeuroTracker AAN.com/cmeand-moc/track-and-view-transcript/ . Nonmembers’ CME credits and participation transcripts will be sent via email. CME activities may describe or explain complementary and alternative health care practices. As with any CME activity, these need to include discussion of the existing level of scientific evidence that supports the practices. However, education that advocates specific alternative therapies or teaches how to perform associated procedures, without scientific evidence or general acceptance among the profession that supports their efficacy and safety, cannot be certified for AMA PRA Category 1 Credit™. Core Competencies The AANI, as an ACCME accredited provider, is responsible for validating the clinical content of CME activities that it provides. Specifically, 1. All the recommendations involving clinical medicine in a CME activity must be based on evidence that is accepted within the profession of medicine as adequate justification for their indications and contraindications in the care of patients. 2. All scientific research referred to, reported or used in CME in support or justification of a patient care recommendation must conform to the generally accepted standards of experimental design, data collection and analysis. The AANI develops its activities/educational interventions in the context of the desirable physician attributes. Specifically, the AANI develops its educational interventions in the contents of the Accreditation Council for Graduate Medical Education (ACGME) Core Competencies which include: ¡¡ Patient Care ¡¡ Practice-Based Learning and Improvement ¡¡ Medical Knowledge ¡¡ Professionalism ¡¡ Interpersonal and Communication Skills ¡¡ Systems-Based Practice For more information on the definitions of the ACGME core competencies, please consult the following webpage: www.acgme.org Once again, this year’s Annual Meeting CME offerings, at the program and lecture level, are identified according to these competencies. Through identifying individual programs by competencies, attendees can easily identify and attend programs that meet each core competency. AMA CME Definition/ Educational Content of Certified CME The AMA HOD and the Council on Medical Education have defined continuing medical education as follows: CME consists of educational activities which serve to maintain, develop, or increase the 140 Content Validation Disclaimers/Disclosures AAN/AANI Education/Scientific Disclaimer The primary purpose of the Annual Meeting is to meet the educational needs of its members and address practice gaps by providing practice-oriented and scientifically based educational activities that will maintain and advance competence and performance in the field of neurology. A diversity of opinions exists in the medical field and the views of the Annual Meeting faculty do not represent those of the AAN/AANI or constitute endorsement by the AAN/AANI. The AAN/AANI disclaims any and all liability for the claims that may result from the use or nonuse of information, publications, therapies, and/or services discussed at the Annual Meeting. 2O14 Scientific Abstract Listing and Annual Meeting Information Relationship Disclosure and Conflict of Interest Resolution Internet Kiosks According to AANI and ACCME policies, everyone who is in a position to control the content of an education activity must disclose financial relationships with any commercial interest to the provider. An individual who refuses to disclose relevant financial relationships is disqualified from being a planning committee member, a teacher, or an author of CME, and cannot have control of, or responsibility for, the development, management, presentation or evaluation of the CME activity. In addition, the AANI must implement a mechanism to identify and resolve all conflicts of interest prior to the education activity being delivered to learners. The resolution of conflict is handled by the Education and Science Committees. Disclosures for everyone in the position to control Annual Meeting content can be found on the AAN Annual Meeting website. In addition, education and science faculty disclosures can also be found in the syllabi, slides, handouts, and/or is done verbally from the podium. Unlabeled Use Disclosure The AANI requires all Annual Meeting presenters to disclose if a therapy/product is not labeled for the use being discussed or if the therapy/product is still investigational. Unlabeled use disclosures can be found in the program materials. Education Grants Some Annual Meeting education and scientific programs are supported in part by educational grants from commercial entities. Disclosure of the educational grant is done through acknowledgement statements on the program materials, signs outside of the room, and verbally from the podium. Although educational grants are received, all programs are developed and implemented solely by the Education Committee and Science Committee. The terms, conditions, and purposes of the commercial support are documented in a written agreement between the AANI and commercial supporter. The AAN uses grant funds to support and enhance existing, as well as new, education programs. The internet kiosks provide attendees with computer workstations and Internet access. Check email, search the AAN website, or complete online evaluations to obtain CME Credit. Wireless Connection Wireless Internet hotspots will be available at the Pennsylvania Convention Center. Business Center The Pennsylvania Convention Center has a business center that offers administrative and office services, including copy machines, faxes, and shipping services. The business center is located on the lobby level of the Pennsylvania Convention Center. First Aid Station A First Aid station is located on the lobby level of the Pennsylvania Convention Center. The station is staffed by licensed medical professionals and fully equipped with supplies, including automatic external defibrillators (AED). The station is operational throughout the duration of the Annual Meeting. Brain Food During the 2014 Annual Meeting, attendees will be provided with light, brain healthy, meals throughout each day. Small break carts will be placed in an accessible area to allow attendees registered for paid Education Programs will be served a great tasting, healthy snack during the break time to keep all energized and ready to learn. Prayer Room A prayer room will be available in the Convention Center for attendees looking for a quiet space for thought, reflection, and prayer. Mother’s Room A private room will be available in the Convention Center for nursing mothers and others with sensitive personal health needs. Please note that this room will not be staffed. Services Guidelines Child Care Information Photography and Recording of Programs A variety of child care options are available in Philadelphia. Check with the concierge at your hotel on or before your arrival to make your arrangements. The AAN strictly prohibits all unauthorized photography (flash, digital, or otherwise), audio and/or video recording during the Annual Meeting. Equipment will be confiscated. Photography is allowed only in the Poster Sessions. Luggage Check No luggage check is available at the Pennsylvania Convention Center. Check with your concierge at your hotel to make your arrangements. Shuttle Service Complimentary shuttle bus service will be provided between designated official AAN hotels and the convention center. Schedules will be available at the Pennsylvania Convention Center and will also be posted in each hotel lobby. Consent to Use of Photographic Images Registration and attendance at, or participation in, AAN/AANI meetings and other related activities constitutes attendee’s authorization to AAN’s use and distribution (both now and in the future) of the attendee’s image or voice in photographs, video recordings, electronic reproductions, audio recordings and other media throughout the world and royalty free. Fast, Easy Registration Online · AAN.com/view/AM14141 General Information Cell Phones The AAN requests that attendees turn cellular phones and pagers to vibrate mode upon entering all Annual Meeting programs. Language The official language of the Annual Meeting is English. No simultaneous translation is available. No Smoking The Pennsylvania Convention Center is a nonsmoking facility. For the health and comfort of everyone, smoking is prohibited at Annual Meeting functions, which include all education and scientific activities and social functions. Press Room Only authorized media may use the Press Room at the Annual Meeting. Journalists must check in at the Press Room and provide proper credentials. For more information, contact Rachel Seroka at rseroka@aan.com or (612) 807-6968. Volunteer Opportunities Education and Scientific Program Monitors RED: 14AM RunWalk Ad MonitorsNeurology are needed for alloreducation programPractice, offerings and scientific Placed in AANnews, Journal, Neurology Clinical AMRAP 8.25"x5.4375", Full Bleed +0.125", (BWdirectors, if in NJ) faculty, session co-chairs, and platform sessions to 4C assist staff as required. The AAN will waive all monitors' Annual Meeting registration, registration fee for monitored program, as well as grant CME credit for the monitored program. Space is available on a firstcome, first-served basis. For an application form or more information, contact Laurie Dixon at ldixon@aan.com or (612) 928-6154. Skills Workshop Volunteers Volunteers are needed to participate in the Neurophysiologic Intraoperative Monitoring Skills Workshop on Sunday, April 27. Volunteers are also needed to participate in the EMG Clinical Skills Workshop Monday, April 28, and the Neuromuscular Ultrasound Skills Pavilion on Friday, May 2. Skills workshop subjects will receive a waived meeting registration and workshop fee as well as payment of $40 per noninvasive session and $60 per invasive session. Space is available on a first-come, first-served basis. For more information, contact Elizabeth Busch at ebusch@aan.com or (612) 928-6115. Weather/Attire The climate in Philadelphia in April is generally warm and pleasant. In April, temperatures usually range from 66 degrees to 73 degrees Fahrenheit. The AAN promotes business casual attire for the duration of the Annual Meeting. Consider bringing a light jacket or sweater to Annual Meeting activities since meeting room temperatures and personal comfort levels vary. Run/Walk for Brain Research On your mark, get set…help cure BRAIN DISEASE! Join your colleagues on Tuesday, April 29, 2014, at 6:30 a.m., for a friendly run/walk. All proceeds will go to the American Brain Foundation to help support research. Sign up for the Run/Walk at AAN.com/view/RunWalk Annual Meeting App Coming Soon! The Mobile App puts all the information you need conveniently on your phone or tablet: ¡ View your itinerary ¡ Find room locations ¡ Access program slides and syllabi ¡ More A LITE version is available now, which allows you to browse programs, speakers, and convention details. Full version to be available prior to the meeting. Available for iPhone®, iPad®, or Android ® Sponsored by: Registration The field of neurology is rapidly changing, and there’s nowhere like the AAN Annual Meeting to make sure you’re up to date. The 66th AAN Annual Meeting in Philadelphia offers breakthrough research, exceptional education programs, and boundless networking opportunities. Log in to the registration site where you can: ¡¡ Register quickly and easily ¡¡ Make your hotel selection and reservation ¡¡ Create your itinerary incorporating your education programs, scientific sessions and other Annual Meeting events ¡¡ Print your schedule and not miss a thing at the meeting! Ways to Save The Annual Meeting offers a great value for the quality and quantity of programming. Try some of these savings tips: ¡¡ Renew your AAN membership or join the AAN now for maximum savings on registration and course fees at AAN.com/view/membership . ¡¡ Register now to avoid increased rates after the April 3, 2014, early registration deadline. ¡¡ Purchase education programs individually or select the new BUY ALL registration option and register for any course of interest for one flat rate.* Member Type General Registration1 Before April 3, 2014 General Registration After April 3, 2014 Students $0 $0 Senior $0 $0 Honorary Member $0 $0 Junior and Non-Neurologist Member (Junior Intern, Resident or Junior Fellow, Business Administrator, Non-Neurologist Clinician, Research Scientist, Research Coordinator) $100 $130 Member Neurologist (Active, Associate, Fellow) $305 $420 Nonmember $610 $840 * Skills Workshops and Skills Pavilions excluded from BUY ALL pricing. Attendee must identify courses to be included as part of “BUY ALL” purchase. Courses are subject to closure due to reaching maximum capacity. BUY ALL registration option is only available prior to early registration deadline of April 3, 2014. 144 Course Fees Early:$45-$350 On-Site: $45-$350 Early:$85-$460 On-Site: $105-$480 Early:$85-$460 On-Site: $105-$480 Early:$45-$350 On-Site: $45-$350 Early:$85-$460 On-Site: $105-$480 Early:$115-$615 On-Site: $135-$635 BUY ALL* Registration Option2 Before April 3, 2014 $400 $400 $400 $400 $1,000 $2,000 (includes meeting access only, education courses must be paid for individually) 2 (includes access to meeting and ability to register for courses at no additional cost) 1 2O14 Scientific Abstract Listing and Annual Meeting Information Three Easy Ways to Register Online Fast, easy online registration available at AAN.com/view/AM14 Online registration walks you step-by-step through completing your registration, reserving a hotel, and personalizing your itinerary with top-tier education courses, scientific sessions, special Annual Meeting events, and more! Fax/Mail A printable registration form is available at AAN.com/view/register Download and print a registration form to complete and mail or fax to: Deadline: April 3 Mail: AAN Registration/CMR 33 New Montgomery, Suite 1100 Registrations received after April 3, 2014, San Francisco, CA 94105 will be processed at a higher rate. Questions Online: Email: AAN.com/view/register aanreg@cmrus.com Fax: (415) 293-4071 Telephone US/Canada: (800) 676-4226 International: (415) 979-2283 Fees General Registration Fee Cancellations/Refunds of Registration The general registration fee is mandatory for all registrants and is determined by AAN member type. Attendees selecting the new BUY ALL option will have the general registration fee included in the price. Until April 3, 2014 April 4–April 18, 2014 After April 18, 2014 Education Programs Purchase programs individually or select the new BUY ALL option to register for any course of interest for one flat rate (Note: Skills Workshops and Skills Pavilions are excluded from the BUY ALL registration package.) In addition, Junior Members who register for two Education Programs at full price will receive 50% off the cost of a third education program of equal or lesser value. Changes in Education Programs Select education programs carefully. An administrative fee of $20 ($30 after April 3, 2014) will be charged for program cancellations without a replacement program. Many programs and events are included with your registration. See page 6 for details. Cancelled or Closed Programs Education programs may be closed due to reaching maximum capacity or cancelled due to insufficient enrollment. In the event of cancellation, registration for the cancelled course will be fully refunded. The AAN is not responsible for airfare, hotel, or other costs incurred by participants in the event of program or registration closure or cancellation. Refund less $50 administrative fee Refund less $100 administrative fee No refund ¡¡ All cancellations must be submitted in writing to aanreg@cmrus.com or faxed to (415) 293-4071. ¡¡ No-shows will not receive a refund. ¡¡ Name substitutions are not permitted. ¡¡ No refunds will be processed for amounts of $20 or less. Special Accommodations Deadline: April 3 The Pennsylvania Convention Center and the AAN are in compliance with the Americans with Disabilities Act or Human Rights Code and strive to accommodate all visitors. Information booths, designated parking, and assisted listening devices are available. If you require special accommodation to attend the Annual Meeting, submit your request while registering online or contact Laurie Dixon no later than April 3, 2014, at ldixon@aan.com or (612) 928-6154. Kosher meals may be provided at any breakfast or lunch, and must be arranged on or before April 3, 2014, through the registration website or by contacting AAN Registration/CMR at aanreg@cmrus.com, (800) 676-4226, or (415) 979-2283. There is a $50 surcharge per meal. On-site requests cannot be accommodated. Group Registration Deadline: March 26 Group registrations are those in which 10 or more individuals’ fees are paid for with one check or credit card. Special registration instructions are available online AAN.com/view/register or by contacting CMR’s Group Registration at (800) 676-4226 (US/Canada) or (415) 979-2283 (International). See page 114 for housing information. Fast, Easy Registration Online · AAN.com/view/AM14145 Hotel Reservations Why Book a Hotel Room Through the AAN? Booking your room through the official AAN housing company assures you are getting a room at the hotel that best fits your needs. You are also helping the AAN maintain consistent and competitive registration fees. The reason is simple. When a city is selected as the site for the AAN Annual Meeting, contracts are signed with several hotels reserving a specific number of rooms to be available for meeting attendees. If these rooms are not sold, the AAN is liable financially. Penalties incurred affect the overall costs of the Annual Meeting and what the AAN charges for registration, exhibit space, and other services. Save on Hotel Reservations Take advantage of the AAN’s special hotel rates to make your trip more affordable. Annual Meeting hotel reservations are processed by Convention Management Resources (CMR). AAN Online Hotel Reservations AAN.com/view/BookHotel The AAN makes it easy and convenient to book your hotel rooms for the 66th Annual Meeting. Booking online allows you to: ¡¡ Take advantage of the AAN’s special hotel rates ¡¡ View room descriptions, photos, and availability ¡¡ Access maps of hotel proximity to Annual Meeting locations Telephone Reservations All correspondence, questions, and inquiries should be directed to CMR at: Phone:Hours: Credit card reservations only Monday–Friday US/Canada (800) 676-4226 6:00 a.m.–6:00 p.m.(PST) International (415) 979-2283 Deposits ¡¡ All hotels require a credit card guarantee or a check deposit of $300 (US dollars) per room and $500 (US dollars) per suite. Deposits will be credited towards your first night’s room and tax. ¡¡ No hotel reservation will be processed without a credit card guarantee or a deposit. ¡¡ Deposits are refundable up to seven days prior to arrival, after which there will be no refunds. ¡¡ Credit cards will be charged for one night’s room and tax if you fail to arrive on the confirmed date of arrival or if you fail to cancel your reservation at least seven days prior to arrival. Confirmations, Changes, and Cancellations ¡¡ You will receive your hotel confirmation from CMR. This is the only confirmation you will receive. ¡¡ Please check your arrival and departure dates on the confirmation carefully. ¡¡ After March 26, 2014, contact CMR to book a room. After this date, however, rooms are subject to availability. Note: Some hotels may charge a penalty for changes made to your departure date after you have checked in. Group Accommodations Blocks of 10 or more sleeping rooms are considered a group. Fax your written request to (415) 293-4071 or email to aanhousing@cmrus.com and you will be contacted by an AAN Housing Consultant. Additional Tax/Assessments ¡¡ Rates do not include the 15.5% hotel tax. ¡¡ An $8 per night assessment fee is included to offset the expense of the meeting. 146 2O14 Scientific Abstract Listing and Annual Meeting Information Corporate Therapeutic Updates Tuesday, April 29, 2O14 and Wednesday, April 3O, 2O14 Starting at 7:00 p.m. Registration is free and open to registered Annual Meeting attendees. Representatives from the following companies invite you to an informational session on therapeutic updates. This program provides you the opportunity to learn about current therapies and projects in the corporate pipeline. Tuesday, April 29 Wednesday, April 3O Baxter Healthcare Multifocal Motor Neuropathy (MMN) Location: Loews Philadelphia Hotel Common Wealth Biogen Idec Tecfidera® (dimethyl fumarate): An Interactive, Case-Based Presentation Location: Philadelphia Marriott Downtown Grand Ballroom Salon EF Biogen Idec TYSABRI® (natalizumab) Label Update Location: Philadelphia Marriott Downtown Grand Ballroom Salon EF Eisai Inc Now Available: FYCOMPA™ (perampanel) as an Adjunctive Therapy for the Treatment of Partial-Onset Seizures in Patients 12 Years and Older Location: Loews Philadelphia Hotel Congress ABC Genzyme, A Sanofi Company The Evolving Treatment Paradigm: Individualizing MS Care Location: Sheraton Philadelphia Downtown Hotel Liberty CD Time: 7:00 p.m.–8:30 p.m. Genzyme, A Sanofi Company Challenging Cases in Neuromuscular Disorders: Shortening the Diagnostic Odyssey Location: Sheraton Philadelphia Downtown Hotel Liberty AB Time: 8:45 p.m.–10:00 p.m. Medtronic, Inc. DBS Therapy Innovation Reception Location: Philadelphia Marriott Downtown Liberty ABC Mylan Mylan Neurology: Patient-Focused, High Quality Medicines Location: Philadelphia Marriott Downtown Grand Ballroom Salon GH Teva CNS The Evolution of COPAXONE ® Location: Loews Philadelphia Hotel Regency Ballroom B *Commitments as of February 3, 2014 Novartis Pharma AG Basel, Switzerland Time for Change: Evolution of Outcome Measures in MS Location: Philadelphia Marriott Downtown Grand Ballroom Salon GH RSVP is recommended for these events. Please visit www.AAN.com/view/CTU for more information. No CME will be given by any accredited organization for the Corporate Therapeutic Updates, and the AAN cannot affirm claims pertaining to FDA off-label medication, research use of pre-FDA drugs, or other research information that might be discussed. Corporate Therapeutic Updates are corporate events. Hotel Map and Amenities Rate Smoke Free Hotel Distance to Convention Center $251–$271 Y 2.0 Blocks Y No Charge 1 No Charge $159 N 1.0 Blocks Y No Charge 0 N/A $229 N 6.0 Blocks Y $9.95 1 No Charge $242 N 4.0 Blocks Y $9.95 1 No Charge $189 Y Adjacent Y No Charge 1 No Charge $289 Y 4.5 Blocks Y $18.00 1 No Charge $159–$169 Y 1.0 Block Y No Charge 0 No Charge $239 Y 1.0 Block Y No Charge 1 No Charge $184 Y 4.0 Blocks Y No Charge 0 N/A $239 Y 1.0 Block Y No Charge 0 No Charge $219 N 2.7 Miles Y No Charge 0 No Charge $259 Y 8.0 Blocks Y $10.00 1 No Charge $259 Y 9.0 Blocks Y $11.99 1 No Charge $275 Y 6.0 Blocks Y $9.99 2 No Charge $239–$264 Y 1.6 Miles Y $9.95 1 No Charge $269 Y 2.3 Miles Y No Charge 1 No Charge Hotel Name & Address 1100 Arch Street Holiday Inn Express Midtown 1305 Walnut Street Home2 Suites 1200 Arch Street Homewood Suites University City 4109 Walnut Street Hotel Monaco 433 Chestnut Street Hotel Palomar 117 South 17th Street Hyatt at the Bellevue 200 South Broad Street Hyatt Regency at Penn’s Landing 201 South Columbus Blvd Inn at Penn Filber t 3600 Sansom St. Street S St N 21st N 22nd St. St. St. N 23rd K A MT R A Chestnu t St. St. t. S 21st S S 20 th Spruce St. St. St t. Blvd. erce St. Market S 22nd Walnut S St. St. St. Kennedy Comm S 23rd 16 Ludlow St. Sansom t St. John F S 24th Chestnu Blvd. ress way t. 26 St. Kennedy St. Exp St. Ludlow John F Market Sch uyl kill Spruce St. t St. St. Locust St. St. S 30 th . S 41st St St. Walnut S S 42nd S 43rd St. Sansom Winter 76 Filber t . 11 Chestnu 32 St. S 31st St Ludlow St. Market S 32nd 16 Hilton Garden Inn Center City St. 15 1301 Race Street S 33 th 14 Hampton Inn City Center St. 13 1 Logan Square S 34th 12 Four Seasons St. 11 1201 Race Street S 36 th 10 Four Points City Center St. 9 1776 Benjamin Franklin Pkwy S 37th 8 Embassy Suites Center City . 7 237 Broad Street rsit y Ave 6 Doubletree Center City S Unive 5 1227 Race Street St. 4 Days Inn Philadelphia Convention Center Hotel S 39 th 3 21 North Juniper Street St. 2 Courtyard Downtown S 40 th 1 High Speed Business Number of On-Site Internet Cost Center Restaurants Fitness Center per Day Current as of 1/31/2014 –Subject to change Rate Smoke Free Hotel Distance to Convention Center $259 N 9.0 Blocks Y No Charge 0 No Charge $299 Y 3.0 Blocks Y No Charge 4 No Charge $249–$279 Y 1.0 Block Y $12.95 1 No Charge Hotel Name & Address Latham Hotel 17 135 South 17th Street Le Meridien 18 1421 Arch Street Loews 19 1200 Market Street 20 Omni Hotel at Independence Park $259–$279 Y 1.0 Mile Y No Charge 1 No Charge 21 Philadelphia Marriott Downtown Headquarter Hotel $279–$299 Y 1.0 Block Y No Charge 1 No Charge $218 Y 10.0 Blocks Y No Charge 3 No Charge $251 Y 2.0 Blocks Y No Charge 0 No Charge $279 Y 4.5 Blocks Y $9.95 1 No Charge $219 Y 10.0 Blocks Y $12.95 1 No Charge $209 Y 2.2 Miles Y No Charge 1 No Charge $199 Y 9.0 Blocks Y $9.95 1 No Charge $259 Y 8.0 Blocks Y $5.95 1 No Charge $209 Y 5.0 Blocks Y No Charge 2 No Charge $299 Y 5.0 Blocks Y $12.95 1 No Charge $199 Y 1.0 Mile Y No Charge 1 No Charge arlton S 99 South 17thWCStreet t. t. N 8th S t. t. N 9th S t. N 6th S N Colu Market Chestnu St. 12 t St. Chestnu 95 20 t St. t. S 6th S t. 31 t. St. t. r St. 3 N 7th S 19 Walnut S St. Broad St. S 15th S 16 th St. 22 Pine St. Junipe 14 Market Arch S St. S 7th S St 9 Filber t t. 17 t. 23 Square 24 8 t. 10 21 S 13 th St. Walnut S Locust 13 S 17th St. S 18 th St. S 19 th 28 Arch S S 8th S 1 30 S Penn St. Pennsylv Conventi ania on Cente r t. 29 t. 676 St. ay Race S 18 St. N 16 th w 5 S 10 th rk 2 St. Pa Rt. 676 Vine St. S 11th St. in St. Cherr y kl N 17th N 18 th N 19 th an St. Fr St. in 7 t. St. am S 12 th Race S nj St. St. St. Be N 20 th 25 4 N 15th 6 N 13 th e St. St. Carlton St. Wood S t. Pearl S t. 400 Arch Street Vin N 10 th Wyndham Historic District Vine St. 31 S 9th S ood St. Blvd. hillSt. Westin Philadelphia 30 mb u s Callow t. 1800 Market Street N 2nd S Sonesta 29 t. 120 South 17th Street Walnut S t. t. Sofitel 28 N 3rd S 1 Dock Street S 2nd S Sheraton Society Hill 27 t. 3549 Chestnut Street N 4th S Sheraton University City 26 t. 201 North 17th Street S 3rd S Sheraton Downtown 25 t. 10 Avenue of the Arts N 5th S Ritz Carlton 24 t. 1 East Penn Square S 4th S Residence Inn Center City 23 t. 1701 South Locust Street S 5th S Radisson Blu Warwick St. 1201 Market Street N 11th 401 Chestnut Street 22 St High Speed Business Number of On-Site Internet Cost Center Restaurants Fitness Center per Day 27 15 Travel Information Reservations and Discounts The official travel agency for the Annual Meeting is Association Travel Pros. For 2%–10% discounted airline tickets to the Annual Meeting, contact them at: Phone: (877) 309-4330 Email: mytravelagent@innovativetvl.com Hours: Monday–Friday, 8:30 a.m.–5:30 p.m. CST Closed weekends and holidays A $25 service fee will be assessed per ticket for reservations made via phone. You may also book online with all airline meeting discounts applied at www.aantvlmeetings.com . A $10 service fee will apply to online bookings. Direct Through Airlines You may also contact your preferred airline directly. You must reference the AAN Annual Meeting and provide the appropriate airline discount codes listed below. Airline Discount Codes Phone Number Website American A7544AG* Delta NMGW2 United ZQVV245289 (800) 433-1790 (800) 328-1111 (800) 521-4041 www.aa.com www.delta.com www.united.com Discounts are subject to availability, so book well in advance. Normal mileage and status upgrades apply for all airline programs. A service fee will be charged for reservations made via phone. Travel Website For travel forms and information updates, visit the AAN Annual Meeting website at AAN.com/view/AM14. * Please use discount code 7544AG for travel direct through www.aa.com. Travel Tips Travel Documents/Passports and Entry Requirements Non-US visitors must have valid travel documents/passports to enter Philadelphia to provide proof of their citizenship. Document requirements vary depending on your country of origin, citizenship, the reason for your visit, and the length of your stay, and may include passport or a birth certificate, photo ID, and/or a visa. For more information, or to request a Letter of Announcement for the 2014 Annual Meeting, visit AAN.com/view/AMinfo. Currency Philadelphia’s currency is the US dollar; currency exchange is available at banks and kiosks throughout the city and at the airport. Cash machines/ATMs are available in most banks, hotels, and shopping centers. For denominations under one dollar, the currency is coins. Customs and Immigration From an international point of arrival, upon arriving in Philadelphia, you will be required to go through a US Customs and Border Protection (CBP) inspection. Before you land, your flight crew will distribute an Immigration and Customs Declaration Form for you to complete; forms are also available at the airport upon your arrival. You will need to present this form, along with your passport, visa (if any), and return tickets to the CBP officer. 150 Measurements Philadelphia uses the United States customary system for weights and measurements. If you choose to drive in Philadelphia, be aware the speed limits are posted in miles per hour. Medication If you are entering Philadelphia with prescription drugs and syringes: keep the medication in its original, labeled container; include medical certificate with syringes showing they are for medical use and have them declared to US Customs officials; bring an extra prescription in case your medication is lost and/or to attest to your need to take such prescriptions; and carry the generic name of prescription medicines. Time Zone Philadelphia is in the Eastern Standard Time Zone. In April it will be the same time as New York, one hour ahead of Chicago, three hours ahead of Los Angeles, five hours behind London, and 13 hours behind Tokyo. For more information, visit AAN.com/view/AMinfo. 2O14 Scientific Abstract Listing and Annual Meeting Information 2O14 Annual Meeting Supporters The American Academy of Neurology and the American Brain Foundation thank the following companies, foundations, and organizations for their demonstrated vision, commitment, and strong support of programs which find answers and improve lives through neurologic education and research. ACTRIMS ¡ Exhibit Guide The Allergan Foundation ¡ Minority Scholars Program & Visiting Professor Program Allergan, Inc. ¡ ¡ ¡ ¡ ¡ ¡ ¡ C18 Therapy of Headache C81 Chronic Migraine Education Program AANextra Brain Health Fair – Gold Event Sponsor Exhibit Guide Presentation Stage Residents and Fellows Career Forum and Reception Athena Diagnostics ¡ Exhibit Hall Passport Baxter ¡ Corporate Therapeutic Update (4/29) ¡ Exhibit Hall Passport Biogen Idec ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ 5K Run/1K Walk for Brain Research Annual Meeting Mobile App Brain Health Fair – Gold Event Sponsor Corporate Therapeutic Update (4/29 and 4/30) Emerging Leaders Forum Exhibit Hall Coffee Break (5/1) Exhibit Hall Opening Reception Footprints Residents and Fellows Career Forum and Reception Eisai Inc. ¡ Corporate Therapeutic Update (4/29) ¡ Exhibit Hall Passport ElectroCore ¡ Exhibit Hall Passport Eli Lilly and Company ¡ Emerging Leaders Forum EMD Serono, Inc. ¡ Exhibit Hall Passport ¡ Resident Scholarship Fund Geisinger Health System ¡ Exhibit Hall Passport Genzyme, a Sanofi Company ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ 5K Run/1K Walk for Brain Research AANextra Brain Health Fair – Silver Event Sponsor Buy A Brain® campaign Carpet Marketing Corporate Therapeutic Update (2) (4/29) Door Drop Insert (4/28) Exhibit Guide Fellow Scholarship Fund Pillar Wrap Posters Online Presentation Stage Resident Scholarship Fund The HCA Earn While You Learn Stipend Program ¡ Resident and Fellow Scholarship Fund Ipsen Biopharmaceuticals, Inc. ¡ C28 Botulinum Toxins: Practical Issues and Clinical Uses for Neurologists ¡ C53 Clinical Usefulness of Botulinum Toxin and Treatment of Dystonia Skills Pavilion Kronus, Inc. ¡ Exhibit Guide Lundbeck LLC ¡ ¡ ¡ ¡ AANextra Door Drop Insert (4/28) Exhibit Hall Cell Phone Charging Station Exhibit Hall Passport Medtronic, Inc. ¡ ¡ ¡ ¡ C95 Deep Brain Stimulation Management Corporate Therapeutic Update (4/29) Door Drop Insert (4/28) Presentation Stage Merck & Co., Inc. Brain Food Station (4/30) Door Drop Insert (4/28 and 4/29) Exhibit Guide Exhibit Hall Cell Phone Charging Stations (2) Exhibit Hall Coffee Breaks (4/29 and 4/30) Exhibit Hall Internet Center (2) Exhibit Hall Footprints Exhibit Hall Pillar Wrap Exhibit Hall Passport Presentation Stage Supernus Pharmaceuticals, Inc. ¡ Door Drop Insert (4/28) ¡ Exhibit Guide ¡ Exhibit Hall Passport Teva CNS ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ Merz Pharmaceuticals LLC ¡ Women in Leadership Program 5K Run/1K Walk for Brain Research Brain Health Fair – Gold Event Sponsor Corporate Therapeutic Update (4/29) Emerging Leaders Forum Hotel Key Cards C99 Epilepsy Skills Pavilion C157 Therapy of Epilepsy Brain Health Fair – Silver Event Sponsor Exhibit Hall Passport Walgreens Infusion Services Mylan Corporate Therapeutic Update (4/29) Exhibit Guide Exhibit Hall Passport Presentation Stage The Resident Experience Novartis Pharmaceuticals Corporation ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ Upsher-Smith Laboratories, Inc. ¡ C10 Approach to Sleep Symptoms: Sleepy or Sleepless ¡ C147 Dementia Update ¡ ¡ ¡ ¡ ¡ Sunovion Pharmaceuticals Inc. Airport Dioramas Corporate Therapeutic Update (4/30) Exhibit Guide Taxi Tops Wayfinding Kiosk Wi-Fi Access PSAV - Presentation Services ¡ Neuro Film Festival® Questcor Pharmaceuticals, Inc. ¡ Exhibit Hall Passport ¡ Exhibit Hall Passport Wolters Kluwer Health/Lippincott Williams & Wilkins, publisher of the AAN publications Neurology ®, Neurology ®Clinical Practice, Neurology ®Neuroimmunology & Neuroinflammation, Continuum: Lifelong Learning in Neurology ®, Neurology Today ®, and Neurology Now ® ¡ ¡ ¡ ¡ ¡ ¡ ¡ Book Bags Brain Health Fair—Silver Event Sponsor Exhibit Hall Cell Phone Charging Station Exhibit Hall Internet Center Resident Scholarship Fund Shuttle Buses Transit Shelters XenoPort, Inc. ¡ Door Drop Insert (4/28) Regency Therapeutics, a Division of Luitpold Pharmaceuticals ¡ Door Drop Insert (4/29) * Commitments received as of January 31, 2014 Exhibitor Listing AbbVie ABCN/ABRET Acorda Therapeutics, Inc. ACRM/American Congress of Rehabilitation Medicine ACTRIMS Akorn Pharmaceuticals Allergan, Inc. Alzheimer’s Association American Association of Neuromuscular and Electrodiagnostic Medicine American Board of Psychiatry & Neurology American Headache Society American Neurological Association American Physician Institute American Society for Apheresis (ASFA) Athena Diagnostics, Inc. Aurora Health Care Avanir Medical Affairs Avanir Pharmaceuticals, Inc. AxelaCare Health Solutions Balanceback Banner Health Baxter Healthcare Bayer HealthCare Benign Essential Blepharospasm Research Foundation, Inc. Biogen Idec Biomed Pharmaceuticals Blackrock NeuroMed Cadwell Cambridge University Press Captureproof, Inc. Carle Physician Group Catalyst Pharmaceutical Partners, Inc. Charleston Area Medical Center Child Neurology Foundation Cleveland Clinic CNS Vital Signs Community Health Systems Compumedics USA CRC Press / Taylor & Francis Group Critical Care Assessment Cytokinetics Dementia Society of America 152 Current as of 1/31/2014 –Programs and dates are subject to change Demos Medical Publishing DENT Neurologic Institute Depomed, Inc. DigiTrace EEG Services DynaMed/EBSCO Dysautonomia International Dystonia Medical Research Foundation EFNS-ENS Eisai Inc. Electrical Geodesics, Inc. (EGI) Electro-Cap International, Inc. ElectroCore Elsevier, Inc. EMD Serono, Inc. Forest Pharmaceuticals, Inc. FR Carrick Research Institute GBS/CIDP Foundation International GE Healthcare Geisinger Health System GeneDx Genentech,INC Genzyme Genzyme Corporation Global Neuro-Diagnostics Great Lakes NeuroTechnologies Grifols USA Hayes Locums Hospital Corporation of America (HCA) IcoMetrix Impeto Medical Interacoustics International Essential Tremor Foundation (IETF) International Parkinson and Movement Disorder Society (MD) Intrafusion IPSEN Biopharmaceuticals, Inc. Jackson & Coker Jari Electrode Supply Jari Electrode Supply KabaFusion Kadlec Health System Karger Publishers KEGO FMI Kennedy Krieger Institute Kronus, Inc. La Lettre Du Neurologue LocumTenens. com Lundbeck Magstim Mallinckrodt Pharmaceuticals Max Neuro Supply Inc. Mayo Medical Laboratories McGraw-Hill Medical Neurogenetics MedLink Corporation Medtronic, Inc. Merz Neurosciences Ministry Health Care MotherToBabystudies Conducted By the Organization of Teratology Information Spec MS Coalition Multigon Industries, Inc. Multiple Sclerosis Association of America Multiple Sclerosis Foundation Mylan Inc. National Ataxia Foundation National Institute of Neurological Disorders and Stroke (NINDS) National Multiple Sclerosis Society Natus Neurology Incorporated Nervline-NeurologicDx Neurology Reviews Neurovirtual USA, Inc. Nihon Kohden America, Inc. Norton Healthcare Physician Services Novartis Pharma AG Novartis Pharmaceuticals Corporation Ochsner Health System Opexa Therapeutics Otometrics Oxford University Press Parkinson’s Action Network Pfizer Inc. Physicians Committee for Responsible Medicine Pikeville Medical Center, Inc. Piramal Imaging Polar Products Inc. Practical Neurology PracticeLink. com 2O14 Scientific Abstract Listing and Annual Meeting Information PracticeMatch Services LLC PRC Clinical ProtoKinetics, LLC Providence Health & Services Questcor Pharmaceuticals, Inc. Regency Therapeutics, a Division of Luitpold Pharmaceuticals Rochester Electro-Medical, Inc. RosmanSearch, Inc. RRS Salem Health Sensonics Int’l Soothe Personalized Medicine Rx Southeast Health Spastic Paraplegia Foundation SpecialtyCare Spectrum Health Medical Group Springer St. Luke’s University Health Network Sunovion Pharmaceuticals Inc. Supernus Pharmaceuticals, Inc. Synapse Biomedical, Inc Tenet South Florida—Advanced Neuroscience Network TEVA Neuroscience, Inc. The Electrode Store The Guthy-Jackson Charitable Foundation The JAMA Network Tourette Syndrome Association Transgenomic, Inc UCB, Inc. United Council for Neurologic Subspecialties (UCNS) Upsher-Smith Laboratories, Inc. US WorldMeds Vanda Pharmaceuticals Inc. VISTA Staffing Solutions Walgreens Infusion Services Wiley Wolters Kluwer Health World Association of Sleep Medicine (WASM) WR Medical Electronics XenoPort, Inc. 2O14 Corporate Roundtable Members* Corporate Roundtable support enables the American Academy of Neurology and the American Brain Foundation to improve patient care through their support of neuroscience research, education, and patient outreach. $40,000 $30,000 Supernus Pharmaceuticals, Inc. $20,000 Acorda Therapeutics, Inc. Medtronic, Inc. Amgen, Inc. Piramal Imaging Baxter Healthcare Corporation Questcor Pharmaceuticals, Inc. Eisai Inc. Sunovion Pharmaceuticals Inc. EMD Serono, Inc. Upsher-Smith Laboratories, Inc. *Commitments as of January 31, 2014 July 11–13 • Chicago, IL Shining the Spotlight on Concussion Research Chicago, IL • July 11–13, 2014 Register Now! AAN.com/view/ConcussionConference 66th Annual Meeting Committee Members Meeting Management Committee Stefan M. Pulst, MD, FAAN, Chair Timothy A. Pedley, MD, FAAN, AAN President Terrence L. Cascino, MD, FAAN, AAN President Elect Brenda Banwell, MD Neil A. Busis, MD, FAAN Cynthia L. Comella, MD, FAAN John Corboy, MD, FAAN Lisa M. DeAngelis, MD, FAAN Mill Etienne, MD, MPH, CPH Jonathan P. Hosey, MD, FAAN Carlayne E. Jackson, MD, FAAN Ralph F. Józefowicz, MD, FAAN Jennifer R. Molano, MD John C. Morris, MD, FAAN Ronald C. Petersen, PhD, MD Michael Pursel, Bpharm, MBA, FASCP Maisha T. Robinson, MD Stephen M. Sergay, MB BCh, FAAN Bruce Sigsbee, MD, FAAN Thomas R. Swift, MD, FAAN Education Committee Cynthia L. Comella, MD, FAAN, Chair Steven L. Lewis, MD, FAAN, Vice Chair Allen J. Aksamit Jr., MD, FAAN Imran I. Ali, MD, FAAN Allison Brashear, MD, FAAN Bruce A. C. Cree, MD, PhD, MCR Barry M. Czeisler, MD John W. Engstrom, MD, FAAN Charles C. Flippen II, MD, FAAN Blair Ford, MD, FAAN J. Clay Goodman, MD, FAAN Laurie Gutmann, MD, FAAN Jonathan P. Hosey, MD, FAAN Jaffar Khan, MD, FAAN Rebecca K. Lehman, MD Janis Miyasaki, MD, FAAN Mark L. Moster, MD, FAAN Bruce I. Ovbiagele, MD, MSc, FAAN Lori Ann Schuh, MD, FAAN Joseph I. Sirven, MD, FAAN A. Gordon Smith, MD, FAAN Science Committee Practice Committee Lisa M. DeAngelis, MD, FAAN, Chair Natalia Sana Rost, MD, Vice Chair Gregory K. Bergey, MD, FAAN Edward H. Bertram, MD David Q. Beversdorf, MD Paul M. George, MD, PhD, MSE Neill R. Graff-Radford, MD, FAAN Joseph Jankovic, MD, FAAN Eric Klawiter, MD Walter J. Koroshetz, MD, FAAN Catherine Lomen-Hoerth, MD, PhD Randolph S. Marshall, MD, FAAN Mark F. Mehler, MD, FAAN Jose G. Merino, MD, M.Phil Massimo Pandolfo, MD Rosebud Roberts, MD Walter A. Rocca, MD, MPH Nina F. Schor, MD, PhD Ericka P. Simpson, MD Mark H. Tuszynski, MD, PhD Barbara G. Vickrey, MD, MPH, FAAN Aleksandar Videnovic, MD, MSc Ryan Walsh, MD, PhD Jonathan P. Hosey, MD, FAAN, Chair Heidi B. Schwarz, MD, FAAN, Vice-Chair Wayne E. Anderson, MD Carmel Armon, MD, FAAN Sarah M. Benish, MD Bruce H. Cohen, MD, FAAN Richard M. Dubinsky, MD, MPH, FAAN Miriam L. Freimer, MD Joseph V. Fritz, PhD Larry B. Goldstein, MD, FAAN, FAHA Raghav Govindarajan, MD Cynthia L. Harden, MD Anna D. Hohler, MD, FAAN Donald J. Iverson, MD, FAAN Michael J. Kaminski, MD, FAAN David J. Likosky, MD, SFHM Pushpa Narayanaswami, MBBS, MD, FAAN Marilyn M. Rymer, MD Don B. Smith, MD, FAAN James C. Stevens, MD, FAAN Jack W. Tsao, MD, DPhil, FAAN Raissa Villanueva, MD David Z. Wang, DO, FAHA, FAAN Medical Economics and Management Committee Abstract Reviewers Orly Avitzur, MD, MBA, FAAN, Chair Gregory J. Esper, MD, MBA, Vice-Chair Neil A. Busis, MD, FAAN Allison Brashear, MD, FAAN Bruce H. Cohen, MD, FAAN Peter D. Donofrio, MD, FAAN David A. Evans, MBA Terry D. Fife, MD, FAAN William S. Henderson, FACMPE Jonathan P. Hosey, MD, FAAN Lyell K. Jones, MD Joel M. Kaufman, MD, FAAN Constantine Moschonas, MD John Ney, MD Marianna V. Spanaki, MD, PhD Alex Abou-Chebl, MD Andrew H. Ahn, MD, PhD Yama Akbari, MD,PhD Roger L. Albin, MD Phillip J. Albrecht, PhD Roy Alcalay, MD Jason Lamar Aldred, MD Beau M. Ances, MD, PhD, MS Liana Apostolova, MD Charles E. Argoff, MD Misha-Miroslav Backonja, MD Alison Baird, FRACP, PhD, MBBS,MPH Laura J. Balcer, MD, MSCE, FAAN Brenda Banwell, MD Sergio Baranzini, PhD Amit Bar-Or, MD, FRCPC Kevin M. Barrett, MD A. M. Barrett, MD Tracy T. Batchelor, MD, MPH E Martina Bebin, MD Fast, Easy Registration Online · AAN.com/view/AM14155 66th Annual Meeting Committee Members Joseph R. Berger, MD, FAAN Bibiana Bielekova, MD Kevin M. Biglan, MD Arnaud Biraben, MD Gretchen L. Birbeck, MD, MPH, DTMH, FAAN Karen Ann Blindauer, MD Christopher J. Boes, MD James H. Bower, MD, MSc K.C. Brennan, MD Jeffrey W. Britton, MD Matthew A. Brodsky, MD Amy Brodtmann, MD, PhD, FRACP Krzysztof Bujarski, MD Rami Burstein, PhD Cheryl Bushnell, MD, MHS Peter A. Calabresi, MD, FAAN Patrizia Casaccia, MD, PhD Sydney Cash, MD John N. Caviness, MD, FAAN Antonia Ceccarelli, MD Marc Chamberlain, MD, FAAN Seemant Chaturvedi, MD, FAAN, FAHA Tanuja Chitnis, MD Tracey Cho, MD Emma Ciafaloni, MD, FAAN Adam B. Cohen, MD Amy Colcher, MD Greg Cole, PhD Giacomo Pietro Comi, MD Francis X. Conidi, MD, DO Wayne T. Cornblath, MD, FAAN Fiona Evann Costello, MD Patricia K. Coyle, MD, FAAN Claire Creutzfeldt, MD Ricardo Cruciani, MD Kevin E. Crutchfield, MD Nabila Dahodwala, MD Debra G. Davis, MD Philip De Jager, MD, PhD Stephanie Debette, MD, PhD Suhayl S. Dhib-Jalbut, MD, FAAN Alan Lee Diamond, DO Bradford Dickerson, MD Mazen M. Dimachkie, MD, FAAN Barbara A. Dworetzky, MD 156 P. James B. Dyck, MD, FAAN Eric R. Eggenberger, DO, FAAN Deniz Erten-Lyons, MD Amelia Evoli, MD Stewart A. Factor, DO, FAAN Samuel A. Frank, MD Johanna Therese Fifi, MD Elizabeth Fisher, PhD Kevin M. Flanigan, MD, FAAN Roy L. Freeman, MD Deborah I. Friedman, MD, FAAN Jennifer A. Frontera, MD Jessica Gautreaux, MD Frank G. Gilliam, MD, MPH Darren R. Gitelman, MD Christopher Glisson, DO Alica M. Goldman, MD Jennifer G. Goldman, MD Myla Goldman, MD Pedro Gonzalez-Alegre, MD Ari Green, MD Robert S. Greenwood, MD, FAAN David M. Greer, MD Rishi Gupta, MD Roop Gursahani, MD Amy K. Guzik, MD Katrina A. Gwinn, MD Karen Gylys, PhD, RN Atticus Hainsworth, MD E. Clarke Haley, Jr., MD, FAAN Rashmi B. Halker, MD Roy H. Hamilton, MD, MS John Hart, MD Anhar Hassan, MBBCH Michael K. Hehir, II, MD Victor W. Henderson, MD, FAAN David N. Herrmann, MD, FAAN Michio Hirano, MD, FAAN Timea M. Hodics, MD Yolanda Holler, MD Julia Holtmann, MD Muhammad Shazam Hussain, MD Matilde Inglese, MD, PhD Kurt A. Jaeckle, MD, FAAN Alan C. Jackson, MD, FAAN 2O14 Scientific Abstract Listing and Annual Meeting Information Carlayne E. Jackson, MD, FAAN Michael S. Jaffee, MD, FAAN Nathalie Jette, MD, MSc, FRCPC Glen Jickling, MD Barbara C. Jobst, MD, FAAN Nicholas Elwood Johnson, MD S. Andrew Josephson, MD Tudor G. Jovin, MD Vern C. Juel, MD, FAAN Larry Junck, MD Andres M. Kanner, MD Orhun H. Kantarci, MD Jonathan S. Katz, MD Daniel Kaufer, MD, FAAN Claudia Kawas, MD Mark Keegan, MD Omar A. Khan, MD, PhD Babar Khokhar, MD Eric Klawiter, MD Peter J. Koehler, MD, PhD, FAAN Matthew A. Koenig, MD Martin Kohrmann, MD Mohamad Koubeissi, MD, FAAN Jeff Kraakevik, MD Fred A. Lado, MD Annette M. Langer-Gould, MD Maarten G. Lansberg, MD Douglas J. Lanska, MD, FAAN Suzette M. LaRoche, MD, FAAN Alan D. Legatt, MD, PhD, FAAN Richard A. Lewis, MD, FAAN David S. Liebeskind, MD, FAAN Arne Lindgren, MD Italo Linfante, MD Carol F. Lippa, MD Eric L. Logigian, MD, FAAN Zachary N. London, MD Jau-Shin Lou, MD, PhD, FAAN Fred D. Lublin, MD, FAAN Jennifer Lyons, MD Jennifer J. Majersik, MD Andrew Mammen, MD, PhD Ruth-Ann Marrie, MD Randolph S. Marshall, MD, FAAN Warren P. Mason, MD Katherine D. Mathews, MD Farrah J. Mateen, MD Kimford J. Meador, MD, FAAN Matthew N. Meriggioli, MD, FAAN Tom Mikkelsen, MD Martha Morrell, MD, FAAN Ellen M. Mowry, MD Tahseen Mozaffar, MD, FAAN Susanne Muehlschlegel, MD Nils Hendrik Mueller, MD Louis Burt Nabors, III, MD Abraham J. Nagy, MD Sandra Narayanan, MD Avindra Nath, MBBS, FAAN Mohit Neema, MD Lawrence C. Newman, MD, FAAN David E. Newman-Toker, MD, PhD, FAAN Thanh Ngoc Nguyen, MD Paul Alan Nyquist, MD, MPH Darin T. Okuda, MD Adriana Elena Palade, MD Mamatha Pasnoor, MD Neepa J. Patel, MD Steven G. Pavlakis, MD, FAAN Aimee Lucinda Pierce, MD Istvan Pirko, MD, FAAN Sean J. Pittock, MD Ela B. Plow, PhD Ann N. Poncelet, MD Shyam Prabhakaran, MD J. Javier Provencio, MD, FAAN Vinaykumar Puduvalli, MD John Pula, MD Svetlana Pundik, MD Mark S. Quigg, MD Goran Rakocevic, MD Anthony Reder, MD Daniel Reich, MD,PhD Awais Riaz, MD, PhD, FAAN John Ringman, MD Ramon L. Rodriguez, MD Michael R. Rose, MD Yelena Roshchina, MD Natalia Sana Rost, MD, FAAN Janet C. Rucker, MD Robert L. Ruff, MD, PhD, FAAN Seward B. Rutkove, MD Ned C. Sacktor, MD Joseph E. Safdieh, MD Juan R. Sanchez-Ramos, MD, PhD Valeria Sansone, MD Sean I. Savitz, MD Michael Joel Schneck, MD, FAAN Todd J. Schwedt, MD Lauren Seeberger, MD Benjamin M. Segal, MD Duygu Selcen, MD, FAAN Linda M. Selwa, MD, FAAN Kathleen M. Shannon, MD William R. Shapiro, MD, FAAN Kazim Ali Sheikh, MD Kevin N. Sheth, MD Holly A. Shill, MD Joshua M. Shulman, MD Nancy L. Sicotte, MD, FAAN Lisa C. Silbert, MD, FAAN David K. Simon, MD, PhD Joseph I. Sirven, MD, FAAN Jeffrey Statland, MD Israel Steiner, MD Victor W. Sung, MD Firas A. Taha, MD Nilufer Taner, MD, PhD Alrabi Tawil, MD, FAAN Edmond Teng, MD, PhD Claudia M. Testa, MD, PhD William H. Theodore, MD, FAAN Parthasarathy Thirumala, MD Matthew J. Thurtell, MD Michel T. Torbey, MD, MPH Helen Tremlett, PhD, BPharm Jay A. Van Gerpen, MD Panayiotis N. Varelas, MD, PhD Kathryn Rae Wagner, MD, PhD David Walk, MD Michael Mei-Hwa Wang, MD Michael F. Waters, MD, PhD Nathaniel F. Watson, MD Emmanuelle Waubant, MD, FAAN Thomas W. Weber, MD Bianca Weinstock-Guttman, MD Patrick Y. Wen, MD, FAAN Norman S. Werdiger, MD, FAAN Dean M. Wingerchuk, MD, FAAN Elaine C. Wirrell, MD George F. Wittenberg, MD, PhD Bradford B. Worrall, MD, MSc, FAAN James P. Wymer, MD, PhD, FAAN Dileep R. Yavagal, MD Manuel S. Yepes, MD Scott S. Zamvil, MD, PhD, FAAN Wendy C. Ziai, MD Charles Zollinger, MD Fast, Easy Registration Online · AAN.com/view/AM14 157 Meeting Information and Contacts Hotel Reservation Deadline: March 26, 2014 Meeting Registration Deadline: April 3, 2014 Registration, Hotel, and Travel Reservations: Meeting Registration and Housing Phone: Credit card reservations only US/Canada (800) 676-4226 International (415) 979-2283 Travel Reservation Services Airline Reservations: Association Travel Pros Phone: (877) 309-4330 www.aantvlmeetings.com Hours: Monday–Friday 6:00 a.m.–6:00 p.m. PST Hours: Monday–Friday, 8:30 a.m.–5:30 p.m. CST Closed weekends and holidays Email: Email: mytravelagent@innovativetvl.com AAN.com/view/AM14 Registration: aanreg@cmrus.com Housing: aanhousing@cmrus.com Annual Meeting Oversight Science Program Corporate Relations Catherine M. Rydell, CAE Chief Executive Officer/Executive Director, AAN, AAN Institute, and American Brain Foundation science@aan.com Alberta Zais Director, Corporate Relations Christine E. Phelps Deputy Executive Director, AANI and American Brain Foundation Erin Jackson Senior Manager, Scientific Programs Nate Kosher Senior Administrator, Scientific Programs Registration Kris Fridgen Senior Director, Research, Education, and Development AANReg@cmrus.com Kevin Heinz Associate Director, Education and Science Housing Deb Stender Senior Manager, Meetings and Conference Management Education Program education@aan.com Amy Nostdahl Senior Manager, Education Programs Heather Lundgren Administrator, Education Programs 158 Laurie Dixon Administrator, Registration and Logistics Bridget Farley Senior Manager, Corporate Relations Compliance Issues Susan Rodmyre Senior Director, Education Resident and Student Activities Lucy Persaud Samaroo Manager, Education Julie Ratzloff Manager, Conference Management Cheryl Alementi Senior Administrator, Education Programs Affiliate Events Practice and Advocacy Related Issues Tammi Sand Senior Manager, Meetings and Conference Management Exhibits Franziska Schwarz Manager, Exhibits and Services 2O14 Scientific Abstract Listing and Annual Meeting Information advocacy@aan.com Rod Larson Chief Health Policy Officer For direct email and phone contacts, please contact Member Services at: memberservices@aan.com (800) 879-1960 or International (612) 928-6000 Take Your Commitment to Your Profession to the Next Level 2O14 AAN Physician Leadership Programs Whether you want to be a mentor or an advocate, to guide or inspire others, you need to cultivate the skills to be an effective leader. NEW for 2O14! Monday, April 28, 9:OO a.m.-5:OO p.m. Women in Leadership The AAN is seeking talented, highly motivated AAN member women with a commitment to neurology who are interested in learning from successful female members in the field of neurology, including members of the AAN Board of Directors, about how to lead at senior levels. If this is you, apply today for the new Women in Leadership course during the 2014 AAN Annual Meeting in Philadelphia! Selected recipients will receive complimentary registration for this course. Directors: Allison Brashear, MD, MBA, FAAN, Winston Salem, NC Barbara Hoese, Principal President, The Inventure Group, Minneapolis, MN Space is limited and the application deadline is April 4, 2014. Apply now at AAN.com/view/WomenLead. Sunday, April 27, 8:OO a.m.-12:OO p.m. Life Reimagined Are you at a point in your life where you are asking “What’s next?” You’ve finished one chapter and have not written the next. Many of us face these transitions at midlife, but they can happen at any point. It’s a time of enormous potential and it defines a whole new phase of life. It’s called a Life Reimagined. Director: Richard Leider, Founder, The Inventure Group, Minneapolis, MN Other Leadership Development Opportunity Monday, April 28, 1:OO p.m.-5:OO p.m. Improving Your Leadership Skills: A Practical Approach Leadership has been defined as “having a sound vision and convincing others to follow you.” This course will assist you in implementing the vision and offer practical tips and case examples on how to persuade others to follow. Directors: Terrence L. Cascino, MD, FAAN, Rochester, MN Ralph L. Sacco, MD, MS, FAHA, FAAN, Miami, FL PAID 201 Chicago Avenue Minneapolis, MN 55415 Permit No. 3840 Twin Cities, MN 2O14 Scientific Abstract Listing and Annual Meeting Information Non-Profit Org. US Postage Register Today for the 66th AAN Annual Meeting April 26–May 3, 2O14 Philadelphia, PA ¡¡ Hotel Reservation Deadline: March 26, 2014 ¡¡ Early Registration Deadline: April 3, 2014 ¡ AAN Member Services: (800) 879-1960 Use #AANAM and follow the AAN AMERICAN ACADEMY OF NEUROLOGY AAN.com/view/AM14