25 Functional Skin Testing: the SMART Procedures
advertisement

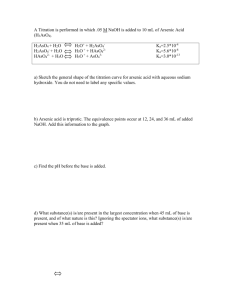
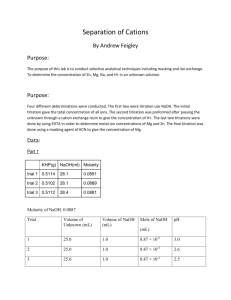
211 25 Functional Skin Testing: the SMART Procedures Swen Malte John, Hans J. Schwanitz (†) Contents 25.1 25.2 25.2.1 25.2.1.1 25.2.1.2 25.2.1.3 25.2.2 25.2.2.1 25.2.2.2 25.2.2.3 25.2.2.4 25.2.2.5 25.2.3 25.3 25.4 25.1 Irritant Patch Testing with Sodium Hydroxide . . . 211 Swift Modified Alkali Resistance Test (SMART) . . . 211 Methods and Participants . . . 211 Subjects . . . 211 Irritant Patch Testing . . . 212 Relevant Variables and Statistical Analyses . . . 213 Results . . . 214 Cohort and Medical Diagnoses . . . 214 Irritant Patch Testing . . . 215 30-Minute NaOH Challenge . . . 216 Reproducibility . . . 216 Constitutional Risks: Atopy . . . 216 Conclusions . . . 217 Applications of the SMART: Differential Irritation Test . . . 218 Outlook: Implications for Medicolegal Evaluations in Occupational Dermatology . . . 219 References . . . 220 Irritant Patch Testing with Sodium Hydroxide An archetype of chemical skin irritation tests is Burckhardt’s “alkali resistance test” which he introduced in 1947, using 0.5 M sodium hydroxide up to 8×10 min under occlusion [9]. The test procedure was later modified by Burckhardt and his colleagues [37, 29, 10; Table 1]. He and his co-workers claimed that the test was able to assess the integrity of the epidermal barrier; the test was recommended as a screening tool for chemically phenotyping the individual. There were some reports claiming that the technique was useful for pre-employment testing in risk professions [14, 23]. However, the concept was controversial from the start, findings were inconsistent, and the technique fell into oblivion in most countries [5, 6, 17, 23, 24]. In current occupational dermatology in Germany, alkali resistance tests given in numerous variations still play an important role for medicolegal evaluations. However, the use of these tests for such purposes in routine diagnostics is controversial [23]. Throughout the last five decades, many scientists have studied sodium hydroxide as an irritant and debated its value, using various test protocols (Table 1). Recent epidemiological data from the Swiss metal industry seem to confirm the use of sodium hydroxide for pre-employment screening [4]. In the United States, where “alkali resistance” never caught on, two modifications have recently been proposed, one of which only uses skin bioengineering for the assessment of test results obtained with sodium hydroxide [39], while the other employs only clinical evaluations [24]. Both groups claim high reliability of the respective test procedure. However, results were obtained in small populations, and reproducibility has been questioned [2, 22]. Unlike the popular irritant model sodium lauryl sulfate (SLS), for which the standardization process is far advanced [35, 27], no such efforts have yet been undertaken concerning NaOH. Therefore, with the special indication of standardizing diagnostics in occupational dermatology, we re-evaluated sodium hydroxide skin irritation in a large group of patients with occupational dermatoses, objectifying results using current biophysical techniques. 25.2 Swift Modified Alkali Resistance Test (SMART) 25.2.1 Methods and Participants 25.2.1.1 Subjects We tested 1,271 patients from various high-risk professions with a history of previous occupational eczema for medicolegal evaluations from January 1993 to April 1999 in the dermatology department of Os- 212 Swen Malte John, Hans J. Schwanitz Table 1. Alkali resistance test and some recommended modifications NaOH concentration in aqueous solutions: 1 normal (N) = 1 molar = 1 mol/l. FA forearm, UA upper arm, DH dorsum of hand, Th thigh, Sh shoulder Test site(s) Maximum occlusion time NaOH concentration Parameters studied Remarks References FA dorsal, upper back 8×10‘, later 3×10‘ 0.5 N Vesicles, erythema, erosions, patchy brown stains (stinging) [9, 10] Subsequent observation of reactions in test site FA volar, upper back, UA 3×10‘ 0.5 N Papules, vesicles, erosions, crusts after 24 h Parallel observation of three test sites; late reactions relevant [37] FA volar, Sh, UA 8×10‘, later 6×10‘ 0.5 N ≥10 Red spots or vesicles No glass blocks [29] Th 5×5‘ 0.5 N ≥10 Nitrazine yellow-positive erosions Introduction of nitrazine yellow [26] Sh, FA, DH 5×5‘ 0.5 N a. Erythema >1 cm If a–c not fulfilled, break up according to Locher. Late readings (24 h) [36] b. Erosion >2 mm c. Three nitrazine yellow-positive erosions div. 1 h; for 6 days 0.03 N TWL + assessment Claimed reproducof refractory period ibility + intraindivual constancy [32,33] FA 1×5‘ 0.2 N SSWL 5‘ after occlusion Biophysical assessment only, no clinical skin signs induced [39] FA, volar, dorsal 20×1‘ 1.0 N Time interval to ≥1 nitrazine yellowpositive erosion (erosion time) Clinical assessment only, erosion time not altered by petrolatum pretreatment [24] nabrueck University. Of these patients, aged 17 – 73 years (314 female, 258 male), 572 fulfilled the criteria mentioned below and were subsequently accepted for the study. History taking and detailed dermatological examination of the complete integument were performed by physicians in a specialist training programs for occupational dermatology or dermatologists. For the most part, there were abundant prior medical records available and assessments from the (former) workplace. Additionally, in most of these patients, epicutaneous patch testing was performed and prick tests as well as serologic investigations (e.g., IgE and sIgE) for assessing inhalatory atopy. 25.2.1.2 Irritant Patch Testing Irritant patch testing was conducted after informed consent was obtained. The study was approved by the Ethical Committee of the University of Osnabrueck. Measurements were only taken in clinically healthy skin. Skin lesions had to have healed at least 3 weeks 25 Functional Skin Testing: the SMART Procedures before the investigation. Participants were requested not to use soap or creams/emollients in the areas of investigation 24 h prior to each examination. NaOH Challenge Sodium hydroxide (33 µl, 0.5 M) was pipetted to the test site (mid-volar forearm) and covered by a 2.5×3×1,0-cm glass block according to Locher [26]. The glass block was fixed with nonocclusive tape under slight pressure to assure uniform spreading of the solution; 0.9% NaCl (33 µl) served as a control in an adjacent area and was covered by a glass block in the same fashion. After 10 min, the solution was gently wiped off with a swab. Clinical and biophysical readings were done in the test and control area 10 min after the end of the provocation phase. Then a second, identical 10-min provocation phase with consecutive clinical and biophysical assessment after 10 min was conducted. Another clinical and biophysical reading was done after 24 h. Clinical skin changes in the test areas were recorded using a five-grade ordinal scale: 1 = “Nil” 2 = “Soap effect” 3 = “Minimal erythema and/or minimal vesiculation and/or maximally one erosion” 4 = “Marked erythema and/or marked edema and/or marked vesiculation and/or 2 erosions” 5 = “Very marked erythema/vesiculation/edema and/ or 5 erosions or necrosis” The test was stopped immediately if after the first provocation phase there were marked clinical skin changes (grade 4 [n=51] or grade 5 [n=0]) or subjective discomfort (n=0). Skin Bioengineering In a previous pilot study with 92 similar patients, we showed that two 10-min provocation periods with 0.5 M NaOH provided significant information on individual skin sensitivity [23]. Briefly, evaporimetric measurements of SSWL/TWL were performed 2– 10 min after the end of NaOH-provocation in 2-min intervals. Transepidermal water loss (TWL) allows an estimation of water evaporation through the stratum corneum providing information on epidermal barrier function [28]. If evaporimetric measurements are performed immediately after aqueous solutions have been applied to the skin, initially the SSWL (skin surface water loss; equals excess water loss from skin surface hydration plus TWL [40]) is being measured. The experiments revealed that a 10-min interval after the end of each of the NaOH provocation phases was a suitable time period for clinical and biophysical patch test reading. At this time, excess water loss from skin surface hydration was already minimal so that roughly only TWL has been estimated. In the present study, therefore, TWL and also relative skin moisture (RSM) were routinely assessed. TWL was measured using the ServoMed evaporimeter EP1 (ServoMed, Stockholm, Sweden) in a perspex-incubator applying the ServoMed gold-plated protection cover (steel grid) and a rubber stopper as an insulating probeholder according to the ESCD guidelines [28]. Relative skin moisture was estimated by capacitance using the corneometer C 820 (Courage & Khazaka, Cologne, Germany). Measurements were conducted in triplicate, the median was then taken as the RSM value. The investigations took place in an air-conditioned laboratory in steady state conditions (ambient temperature 20–21° C, relative humidity 40%–45%). Acclimatization of participants was at least 15 min, usually 30 min. Measurements were conducted after acclimatization in the prospective test and control areas (ex-ante readings), and then 10 min after each provocation phase and finally after another 24 h. 25.2.1.3 Relevant Variables and Statistical Analyses Clinical Diagnoses and Atopy Diagnosis of clinical atopy usually had to be made retrospectively because skin lesions were either healed on investigation or reduced to minor residuals; if florid skin changes were detected on first clinical examination subjects were asked to return after healing for patch testing. If in the medical records previous atopic dermatitis (n=92), palmar or plantar eczema [31] in its various manifestations (n=93), or previous flexural eczema (n=208) was documented, the respective subjects were grouped as “atopic skin disposition” (n=248; it should be noted that there were frequent combinations of the above-mentioned skin manifestations). The other main groups of diagnoses were pure “irritant contact dermatitis” (without atopic skin manifestations in the history, n=138) or pure “allergic contact dermatitis” (n=130). Biophysical Parameters ∆-TWL and ∆-RSM, respectively, were calculated in regard to the ex-ante-values and the values in the NaCL controls using the following mathematical term: ∆-TWLNaOH, 10 or 20 min = (TWLNaOH, 10 or 20 min – TWLNaOH, 0 min) – |TWLNaCl, 10 or 20 min – TWLNaCl, 0 min|. 213 214 Swen Malte John, Hans J. Schwanitz Fig. 2. Time course of biophysical parameters with respect to the result of visual scoring (negative/positive) after 2×10 min NaOH challenge. The medians of ∆−TWL and ∆−RSM measurements are shown (Pos TWL10’ NaOH n=287, Neg TWL10’ NaOH n=285; Pos TWL20’ NaOH n=238, Neg TWL20’ NaOH n=283; Pos TWL24 h n=212, Neg TWL24 h n=199; identical n for RSM values) Fig. 1. Age and sex distribution of cohort (n=572) For the second difference (|TWLNaCl, 10 or 20 min – TWLNaCl, 0 min |), only the total positive amount was used; this is of relevance when the second difference is negative. In these 176 cases (TWLNaCl, 10 min), and 102 cases (TWLNaCl, 20 min), respectively, the ex-ante value in the control area was slightly higher then after 10 or 20 min of NaCl application. ∆-TWL and ∆-RSM will be negative if the difference of values in the NaOH areas (TWLNaOH, 10 min – TWLNaOH, 0 min) is smaller than the respective difference in the control areas. This was only rarely the case in robust skin without skin changes, due to the variance of measurements (∆TWLNaOH, 10 min: n=37; ∆-TWLNaOH, 20 min: n=46). Statistical Analyses Besides descriptive statistical analysis, data evaluation focused on the estimation of a predictive (critical) value of the investigated biophysical parameters; for this purpose, receiver operating characteristic (ROC) curves were developed, as described in detail by Green and Swets [20], and Lange and Weinstock [25]. For ROC curves and other investigations, the clinical score (five-point ordinal scale) was dichotomized (clinical grades 1, 2 vs grades 3–5). Differences in TWL, RSM between NaOH, and controls were tested using bivariate two-tailed nonparametric tests (Mann-Whitney U or Kruskal-Wallis test). In crosstabulations, the chi-square statistics or the McNemar-test (linked samples), respectively, were used to analyze the differences between the observed and the expected values. Using the Cohens Kappa index [11], the degree of agreement of clinical and biophysical parameters and reproducibility were calculated. Correlations between the various clinical, demographical, and biophysical parameters were analyzed using the two-tailed Spearman rank correlation test. The size of estimated effects was judged with Cohen’s classification [12]. An error probability of <5% was considered statistically significant. For statistical analyses, the statistical software package SPSS (version 9.0 D, SPSS Inc., Munic, Germany) was employed. 25.2.2 Results 25.2.2.1 Cohort and Medical Diagnoses The age and sex distribution of the study population is given in Fig. 1. The most frequent profession was “hairdresser” (22.6%), followed by various “professions in the health sector” (16.9%), mainly nursing. This explains the dominance of women in the young age groups. Male-dominated jobs followed in third and fourth positions: “metal worker” (7.0%) and “brick layer” (6.4%). In 84.6%, the result of medicolegal evaluation was that skin disease was considered to have been induced by the job; overall the most relevant single factor for the elicitation of the dermatoses was wet work. As pointed out above, diagnosis had to be made in retrospect because skin lesions were either healed on investigation or reduced to minor residuals. The most frequent primary diagnosis was allergic contact dermatitis (n=165; 28.9%), followed by irritant dermatitis (n=158; 27.6%) and various atopic skin manifestations (e.g., atopic dermatitis; atopic palmar or plantar eczema). Due to the frequent overlap in the pathogenesis of occupational skin diseases in 205 cases, more than one diagnosis was made; most frequently atopic manifestations were diagnosed together with allergic or irritant contact dermatitis. If all cases in which atopic skin manifestations were diagnosed alone or in combination are taken together, 248 patients (43.4%) were considered atopic (“atopic skin disposition”). 153 (26.7%) had a history of inha- 25 Functional Skin Testing: the SMART Procedures Fig. 3. Association of ∆-TWL after 2×10 min NaOH challenge and clinical grading (n=572; in 51 cases test was stopped after 10 min in accordance with break-up criteria; then 10-min readings were used]) latory atopy (rhinitis or asthma), which was mostly associated with a history of some kind of atopic skin manifestations. Pure “irritant contact dermatitis” – without atopic skin manifestations in the history – was found in 138, and pure “allergic contact dermatitis” manifested in 130 subjects. 25.2.2.2 Irritant Patch Testing During the test period and within a follow-up of at least 24 h, patients felt no relevant discomfort or pain by the test. Clinical grade 5 (“very marked erythema/ vesiculation/edema and/or 5 erosions or necrosis”) was never observed. If reactions were positive after 20 min then after 24 h sometimes minimal erythema or solitary, small superficial erosions were detected, but no necrosis, scarring, infection, or discoloration. Healing was uneventful: in 43.6% of test-positive individuals skin reactions were completely reversed after 24 h. Thus, as expected, agreement between 2×10min- and 24-h observation concerning identifiable skin changes was poor (Cohens κ=0.38). Therefore test reading after the second 10-min NaOH-provocation phase was considered relevant for clinical outcome. The time course of the biophysical parameters within the observation period (24 h) with respect to the results of visual scoring after 2×10 min NaOH challenge is shown in Fig. 2 (clinical observations dichotomized). The differences were statistically significant for ∆−TWL after 10 min (z=–7.3; p<0.001), Fig. 4. ROC curve for ∆-TWL after 2×10 min NaOH and clinical outcome after 20 min (n=572). X-axis: inverse specificity (equals false-positive classifications) 20 min (z=–12.0; p< 0.001), 24 h (z=–7.6; p<0.001) and for ∆−RSM (10 min: z=–4.6; p<0.01; 20 min z=–2.5; p<0.01; 24 h: z=–3.0; p<0.01); (Mann-Whitney U test). In the group of patients who reacted clinically after NaOH challenge, there was an increase of TWL after 20 min, which was still detectable after 24 h, whereas ∆−RSM showed after an initial increase a decline 24 h after NaOH provocation, most likely due the exsiccation following the barrier impairment. Differences in measurements in the test (NaOH) and control areas (NaCl) were for both biophysical parameters significant at all observation intervals (p<0.05; Wilcoxon test). If the result of visual scoring is examined in detail, a good correlation between the degree of clinical reactivity and ∆−TWL can be demonstrated. Correlation was best after 20 min NaOH provocation (rs=0.587; p<0.01 [Spearman rank correlation]; Fig. 3). Correlation was poor at all measurment intervals for ∆−RSM (20 min: rs=0.106). No significant correlations could be detected between age or sex and clinical or biophysical findings, nor any job-specific effects. A relevant question is whether biophysical parameters can predict clinical outcome. In order to answer this question, a ROC analysis was conducted. For the parameter ∆-TWL after 2×10 min NaOH, the ROC curve is shown in Fig. 4. As a cut-off point, a ∆-TWL of 2 g/m2h was determined; for this cut-off point (“critical value”) TWL has a sensitivity of 76.7% and a specificity of 74.7% (C=0.83) for prediction of the target variable (“clinical outcome after 2×10 min NaOH”). ROC analysis for ∆-TWL after 10 min 215 216 Swen Malte John, Hans J. Schwanitz Fig. 5a, b. Clinical (a) and biophysical (b) response with respect to the three main clinical diagnoses (n=516). a Percent of positive clinical reactions after 2×10 min NaOH. b Boxplot of ∆−TWL after 2×10 min NaOH; (o) extremes, (*) outliers NaOH for the target variable was not significant (C=0.67). Also for ∆-RSM at all measuring intervals, there was no relevant ability to significantly discriminate between positive and negative clinical test results. 25.2.2.3 30-Minute NaOH Challenge At the beginning of the study, in 18 patients in whom there were no or only minor clinical reactions and only a small increase of TWL after 2×10 min NaOH challenge, another 10-min NaOH provocation phase was added; this approach corresponds to Burckhardt's most recent modification of his original method [37, 10]. Thus it could be shown that in the investigated subgroup it was not possible to gain relevant additional information; the agreement of clinical outcome after 20 and 30 min was high, reflected by a Cohens kappa-coefficient κ=0.87. Significant agreement was also demonstrated for the parameter TWL (κ=0.88; ∆-TWL dichotomized at cut-off point [2 g/m2h]). 25.2.2.4 Reproducibility Fourteen patients were examined twice in the recruitment-phase; the median of the interval between the two separate investigations was 2 years (range, 1–3 years). In the NaOH challenge, there were similar clinical findings after 2×10 min NaOH (κ=0.66). However, agreement of TWL values was below the significance level (κ=0.43; ∆-TWL dichotomized at cut-off point [2 g/m2h]). 25.2.2.5 Constitutional Risks: Atopy If the degree of clinical reactivity after NaOH challenge is analyzed with respect to the presence of “atopic skin disposition” there is a significant negative association with the clinically unresponsive grades “nil” and “soap effect” and a corresponding positive association with marked clinical reactivity (X32 =12.17; p=0.007). This phenomenon is further elucidated by the post-hoc comparison of the adjusted, standardized residuals (Table 2). There was no such association with the other main clinical diagnoses “irritant dermatitis” and “allergic contact dermatitis” (Fig. 5a). Statistical analysis of the cross-tabulation showed again that distribution was unequal (X22=9.65; p<0.01). By post-hoc-comparison of the adjusted, standardised residuals it was obvious that this was only due to the parameter “atopic skin disposition” (Table 3). There was also a significant positive association of “atopic skin disposition” and the variable ∆−TWL at all measuring intervals (10 min NaOH: z=–2.69, p<0.01; 20 min NaOH z=–3.17, p<0.01; 24 h z=–2.2, p=0.02 [Mann-Whitney U test]). When the association with the other main clinical diagnoses was evaluated, again there were differences detectable for this variable; however, this was significant only after 20 min NaOH (Fig. 5b): X22=10.36, p=0.006 (Kruskal-Wallis test); in separate Mann-Whitney U tests it could be confirmed that differences in distribution were explained only by the parameter “atopic skin disposition.” For the variable ∆−RSM, a significant association with clinical diagnoses, single or in combination, was not detectable. 25 Functional Skin Testing: the SMART Procedures Table 2. Association between the clinical response after 2×10 min NaOH and the parameter “atopic skin disposition.” Clinically unresponsive grades 1 and 2 (“nil”, “soap effect”) are comprised Atopic skin disposition No Clinic 20’ count NaOH Nil/soap effect Mild erythema Count 181 104 Corrected residuals 3.3 –3.3 Count Corrected residuals 65 58 –1.0 1.0 Marked erythema/ Count 78 86 Edema/vesicle Corrected residuals –2.8 2.8 Count 324 248 total Total Yes 285 123 164 572 Table 3. Association between the clinical response after 2×10 min NaOH and the three main clinical diagnoses Clinical outcome 20“ NaOH Negative Diagnosis Atopic skin disposition Irritant contact dermatitis Allergic contact dermatitis total 25.2.3 Positive Total 248 Count 104 144 Corrected residuals –3.1 3.1 Count 76 62 Corrected residuals 1.7 –1.7 138 Count 73 57 130 Corrected residuals 1.9 –1.9 Count 253 263 Conclusions Burckhardt's alkali resistance test – even in the less rigid modifications [26] – was shown to induce colliquation necrosis in 1% [36]. The above-proposed modification with only two 10-min NaOH challenges did not produce relevant volunteer discomfort when the above-defined break-up criteria were used. This is a relevant finding, when considering that, unlike previous studies employing NaOH where small groups of healthy individuals were studied [39, 24], we examined a large cohort of patients with former occupational dermatitis. Even in these patients with a high likelihood of increased skin sensitivity, the test was well tolerated and yet revealed remarkable individual differences. Minimal clinical reactions (erythema) were taken as sufficient sign of positive skin reactivity, and clinical findings were objectified by current biophysical techniques. TWL proved the biophysical variable of relevance; whereas RSM was not equally useful. The TWL reading after the second challenge period (2×10 min NaOH) provided the most relevant re- 516 sults, longer provocations (30 min) or late readings (24 h) did not yield more information, neither clinically nor biophysically. Prediction of clinical outcome by TWL20 min NaOH was good. Thus both parameters (clinical grading and TWL) can serve as internal controls, opening up a kind of stereoscopic view of the test result. If in an individual clinical and biophysical findings are in agreement, measurements are to be considered relevant; if not, especially if there are clinical changes without a corresponding increase in TWL, the investigation may be repeated. Generally, results should be interpreted considering the complete range of anamnestic and physical findings in the individual, the test providing valuable additional information. In the investigated cohort of 572 thoroughly examined patients with a history of former occupational skin disease, the test was able to distinguish atopics from nonatopics, thus identifying constitutional risks. The detection of constitutional risks, especially atopy, by irritant patch testing is a controversial issue [3–5, 6, 10, 15, 16, 29, 34]. The discrepancies of the investigators’ results may be explained by the kind and size of 217 218 Swen Malte John, Hans J. Schwanitz cohorts tested, choice of irritants, dose, method, and body site as irritant reactivity is a complex phenomenon, which is multifactorially influenced, depending on barrier function, inflammatory reactivity, and restitutional capacity [1, 17]. The absence of a gold standard for the assessment of skin hyper-reactivity is closely related to the fact that there is still no uniform pathogenic concept of this phenomenon. However, there is no doubt that an individual genetic predisposition is of relevance. Recent results from a large questionnaire investigation in Denmark show that the concordance rate of hand eczema was almost twice as high in homozygotic compared to heterozygotic twins in both sexes [8]. Also, reactivity to various irritants such as SLS, benzalkonium chloride and sapo kalinus showed a significantly higher concordance rate in identical twins than in fraternal twins [21]; similar findings were obtained with NaOH [19]. The above-proposed NaOH test is based on existing procedures, but is less time-consuming, less harmful, and has a proven efficacy. The test was found to be reproducible, though further experience has to be gained for confirmation. We call our up-dated version of Burckhardt’s test “swift modified alkali resistance test (SMART)”. Figure 6 gives an overview on the recommended test protocol based on the obtained findings. Fig. 6 Flow chart of the SMART. Clinical and biophysical readings are to be conducted 10 min after each provocation phase 25.3 Applications of the SMART: Differential Irritation Test It is beyond dispute that individuals with hyperirritable skin do exist [1, 17, 18, 24]. Using a test battery of various irritants, including sodium hydroxide, Frosch identified patterns (cluster) of individual skin susceptibility; in a group of 44 healthy volunteers 25% were deemed hypoirritable, 61% were normal, and 14% were hyperirritable [18]. Frosch also dem- onstrated that the functional integrity of the stratum corneum is critical for the degree of individual irritability. The phenomenon of hyperirritability is related to a genetic predisposition, but not necessarily identical with atopy. Besides this primary hyperirritability, it is also widely accepted that there may develop secondary hyperirritability after former dermatitis. In occupational dermatology, some patients with former, healed dermatitis complain of experiencing ongoing increased skin sensitivity. However, the clinician frequently in these cases cannot detect any skin impairment. With the aim of objectifying secondary hyperirritability we conducted a pilot study. For this purpose, the SMART was applied simultaneously to two different body areas in a comparative fashion: – One area that was previously exposed to irritants at the workplace: the back of the hand – while the other was not: the ventral forearm Forty-eight patients with completely healed, former occupational eczema (aged 19–68 years; 22 female, 26 male) were investigated, 31 healthy volunteers (aged 21–58; 21 female, 10 male) who were not previously exposed to relevant private or occupational skin hazards served as controls. The SMART was performed as described above in parallel in the two test sites; furthermore, late readings were performed after 24 and 48 h. In addition to the SMART an SLS test (1%, 24 h occlusion) was conducted in the two test sites, both tests were clinically and biophysically monitored. The study is described in detail elsewhere [23]. In summary, the test revealed that in the control group there was reactivity only in the forearm in a minority of (sensitive) individuals, as an indication of constitutionally impaired barrier function. However, there was no reactivity in the dorsum of the hands in any of the controls. Moreover, in the test group with former (healed) dermatitis a subgroup of four persons (8.3%) was detected where relevant clinical (and biophysical) reactivity to the SMART occurred only in the dorsum of the hands; these patients claimed to have observed a remaining increased skin sensitivity. It has long been known that there are marked regional variations of skin reactivity; they are attributed to differences in keratinization and in the density of epidermal shunts such as hair follicles and sweat ducts [17]. Various studies, using different irritants, have convincingly demonstrated that the back of the hand is a relatively robust area, even in skin-sensitive individuals [1, 13, 17, 30]. This is confirmed by our data, comparing skin reactivity to the SMART in the 25 Functional Skin Testing: the SMART Procedures Table 4. Interpretation of the differential irritation test (DIT), the SMART being applied to the forearm and back of hands simultaneously for objectifying secondary hyperirritability forearm and the dorsum of the hand. In the minority of cases, where the normal hierarchy of skin sensitivity is absent (isolated reactivity in the hands), we claim that this is strong evidence for remaining acquired hyperirritability. Table 4 outlines the rationale of the above-described concept of comparative (differential) irritation testing in separate body locations. Assessment of remaining subclinical hyperirritability and differentiating between primary and secondary hyperirritability is of great importance for medicolegal evaluations in occupational dermatology (i.e., claims, prognosis). Thus far, the differential irritation test (DIT) is the first systematic methodical approach to objectify secondary, subclinical skin hyperirritability for these purposes. 25.4 Outlook: Implications for Medicolegal Evaluations in Occupational Dermatology Since 1994 in Germany, approximately 20,000 cases of assumed occupational dermatoses are reported annually, which makes skin disorders by far the most frequent occupational illnesses. Medical treatment and job rehabilitation of occupational illnesses lies in the hands of the public employers’ liability insurance, which is a specific branch of the social welfare system. In dermatology, about 12,000 medicolegal evaluations are done every year in order to distinguish between occupational and nonoccupational skin diseases. Legal requirements for accepting oc- cupational skin disease (BK 5101 [7]) are complex. In the context of medicolegal evaluations, the diagnostics routinely performed are epicutaneous allergy patch testing. While this latter method is well standardized [38], irritant patch testing is not. Nevertheless, various irritation tests are regularly conducted in such evaluations; currently, in the majority of these tests a great spectrum of modifications of the original Burckhardt alkali resistance test is employed. A recent survey among German occupational dermatologists frequently involved in medicolegal evaluations showed very heterogeneous opinions concerning the relevance of irritant patch testing in such evaluations: one-third strongly opposed such tests, one-third was strongly in favor of them, the remaining third was undecided [23]. It is likely, and could be proven by an analysis of court cases, that the outcome of evaluations may be strongly influenced by the attitude of the dermatologists as to whether irritant patch testing is considered relevant or not. We believe that this validates our claim that there is a need to reach an agreement regarding a common irritation test in occupational dermatology to ensure comparability and equal management of patients in medical opinions. Therefore, with the special indication of standardizing diagnostics, we regard the swift modified alkali resistance test (SMART) as a serious candidate for routine use in occupational dermatology. The SMART-procedures (Table 5) – as tools for assessing functional integrity of skin barrier properties – could be another step on the long road to developing a benchmark irritant patch test in occupational dermatology. 219 220 Swen Malte John, Hans J. Schwanitz Table 5. A potential role for sodium hydroxide irritant patch testing in occupational dermatology 1. SMART (forearm) Identification of constitutional risks Standard for medicolegal evaluations? 2. DIT (forearm vs dorsum of hand) Distinguishing primary from secondary hyperirritability Objectifying „acquired subclinical hyperirritability“ for medicolegal purposes (i.e., claims, prognosis) References 1. Agner T. Noninvasive measuring methods for the investigation of irritant patch test reactions. Acta Derm Venereol, Suppl 1992; 173:1–26 2. Bangha E, Hinnen U, Elsner P. Irritancy testing in occupational dermatology: comparison between two quick tests and the acute irritation induced by sodium lauryl sulphate. Acta Derm Venereol (Stockh) 1996; 76:450–452 3. Basketter DA, Miettinen J, Lahti A. Acute irritant reactivity in atopics and non-atopics. Contact Derm 1998; 38:253– 256 4. Berndt U, Hinnen U, Iliev D, Elsner P. Is occupational irritant contact dermatitis predictable by cutaneous bioengineering methods? Results of the Swiss metalworkers eczema study (PROMETES). Dermatology 1999; 198:351– 354 5. Björnberg A (1968) Skin reactions to primary irritants in patients with hand eczema. Göteburg, Isaacsons 6. Björnberg A (1974) Low alkali resistance and slow alkali neutralization. Characteristics of the eczematous subject? Dermatol 149:90–100 7. Brandenburg S, Schwanitz HJ, John SM (1999) Empfehlungen für die Begutachtung von Berufskrankheiten nach BK 5101. Dermatosen 47:109–114 8. Bryld LE, Agner T, Kyvik KO, Brondsted L, Hindsberger C, Menné T. Hand eczema in twins: a questionnaire investigation. Br J Dermatol 2000; 142:298–305 9. Burckhardt W. Neue Untersuchungen über die Alkaliempfindlichkeit der Haut. Dermatologica 1947; 94:8–96 10. Burckhardt W. Praktische und theoretische Bedeutung der Alkalineutralisations- und Alkaliresistenzproben. Arch Klin Derm 1964; 219:600–603 11. Cohen J. A coefficient of agreement for nominal scales. Educational and Psychological Measurement 1960; 20:37–46 12. Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, Erlbaum, 1988 13. Cua AB, Wilhelm KP, Maibach HI. Cutaneous sodium lauryl sulphate irritation potential: age and regional variability. Br J Dermatol 1990; 123:607–613 14. Czernielewski A. L’importance pratique du test de résistance de la peau à l’action des alcalis. In: Symp Dermatol Pragae cum participatione internationali de morbis cutaneis professionalibus, Prag 1960. 1962; Exerpta Lectionum, pp 84–85 15. Den Arend JA, de Haan AFJ, Malten KE. Seasonal transepidermal water loss and impedance of forearm skin in atopics and non-atopics. Contact Derm 1988; 19:376–390 16. Frosch PJ. Hautirritation und empfindliche Haut. Grosse Verlag, Berlin, 1985 17. Frosch PJ. Clinical Aspects of Irritant Contact Dermatitis. In: Rycroft RJG, Menné T, Frosch PJ (eds) Textbook of contact dermatitis, 3rd edn. Springer Verlag, Berlin Heidelberg New York, 2001; pp 313–354 18. Frosch PJ, Pilz B. Irritant patch test techniques. In: Serup J, Jemec GBE (eds) Handbook of non-invasive methods and the skin. CRC press, Boca Raton, 1995; pp 587–591 19. Gloor M, Schnyder UW. Vererbung funktioneller Eigenschaften der Haut. Hautarzt 1977; 28:231–234 20. Green DM, Swets JA. Signal detection theory and psychophysics, revised edn. Huntington, New York, 1974 21. Holst R, Möller H. One hundred twin pairs patch tested with primary irritants. Br J Dermatol 1975; 93:145–149 22. Iliev D, Hinnen U, Elsner P. Reproducibility of a non-invasive skin irritancy test in a cohort of metalworker trainees. Contact Derm 1997; 36:101–103 23. John SM. Klinische und experimentelle Untersuchungen zur Diagnostik in der Berufsdermatologie. Konzeption einer wissenschaftlich begründeten Qualitätssicherung in der sozialmedizinischen Begutachtung. In: Schwanitz HJ (ed) Studien zur Prävention in Allergologie, Berufs- und Umweltdermatologie (ABU 4). Universitätsverlag Rasch, Osnabrück, 2001 24. Kolbe L, Kligman AM, Stoudemayer T. The sodium hydroxide erosion assay: a revision of the alkali resistance test. Arch Derm Res 1998; 290:382–387 25. Lange N, Weinstock MA. Statistical analysis of sensitivity, specificity, and predictive value of a diagnostic test. In: Serup J, Jemec GBE (eds) Handbook of non-invasive methods and the skin. CRC press, Boca Raton, 1995; pp 33–41 26. Locher G. Permeabilitätsprüfung der Haut Ekzemkranker und Hautgesunder für den neuen Indikator Nitrazingelb “Geigy”, Modizifierung der Alkaliresistenzprobe, pH-Verlauf in der Tiefe des stratum corneum. Dermatologica 1962; 124:159–182 27. Löffler H, Effendy I, Happle R. Epikutane Testung mit Natriumlaurylsulfat. Nutzen und Grenzen in Forschung und Praxis. Hautarzt 1999; 50:769–778 28. Pinnagoda J, Tupker RA, Agner T, Serup J. Guidelines for transepidermal water loss (TEWL) measurement. Contact Dermatitis 1990; 22:164–178 29. Schultheiss E. Eigenuntersuchungen und Alkaliresistenzprobe. Arch Klin Exp Dermatol 1964; 219:638–648 30. Schulz D, Korting GW. Zur weiteren Kenntnis der Alkaliresistenz-Probe. Dermatosen 1987; 35:91–94 25 Functional Skin Testing: the SMART Procedures 31. Schwanitz HJ. Atopic palmoplantar eczema. Springer Verlag, Berlin Heidelberg New York, 1988 32. Spruit D, Malten KE. Injury to the skin by alkali and its regeneration. Dermatologica 1966; 132:124–130 33. Spruit D, Malten KE. Estimation of the injury of human skin by alkaline liquids. Berufsdermatosen 1968; 16:11–24 34. Tupker RA, Pinnagoda J, Coenraads PJ, Nater JP. Susceptibility to irritants: role of barrier function, skin dryness and history of atopic dermatitis. Br J Dermatol 1990; 123:199– 205 35. Tupker RA, Willis C, Berardesca E, Lee CH, Fartasch M, Agner T, Serup J. Guidelines on sodium lauryl sulfate (SLS) exposure tests. A report from the standardization group of the European Society of Contact Dermatitis. Contact Derm 1997; 37:53–69 36. Ummenhofer B. Zur Methodik der Alkaliresistenzprüfung. Dermatosen 1980; 28:104–109 37. Wacek A. Weitere Untersuchungen aus dem Gebiet der Alkali- und Säureabwehr der Haut, Dermatologica 1953; 107:369–417 38. Wahlberg JE. Patch testing. In: Rycroft RJG, Menné T, Frosch PJ (eds) Textbook of contact dermatitis, 3rd edn. Springer, Berlin Heidelberg New York, 2001; pp 435–468 39. Wilhelm KP, Pasche F, Surber C, Maibach HI. Sodium hydroxide-induced subclinical irritation. A test for evaluating stratum corneum barrier function. Acta Derm Venereol (Stockh) 1990; 70:463–467 40. Wilson D, Berardesca E, Maibach HI. In vivo transepidermal water loss and skin surface hydration in association of moisturization and soap effects. Int J Cosm Sci 1988; 10:201–211 221