Physical signs of pulmonary syndromes
advertisement

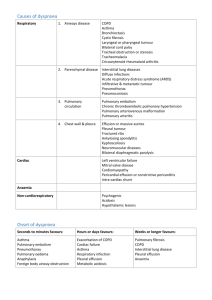
2. Physical signs of pulmonary syndromes Dr. Nebenfü Nebenführer Zsuzsa Infiltration Pneumonia Pulmonary embolism Atelectasis Pleural effusion Pneumothorax Mediastinal mass Pulmonary infiltration causes Exsudate, tumor, blood in the alveoli. Pneumonia lobar viral bronchopneumonia Pulmonay embolism Tumor Tbc Pulmonary infiltration history Shaking chill, sputum: pneumonia Operation, immobilisation, chest pain, bloody sputum: infarction after PE Weight loss, smoking, bloody sputum: tumor Pulmonary infiltration physical examination 1. Inspection: chest excursion decreased Tactile fremitus: increased Percussion: dullness Pulmonary infiltration physical examination 2. Auscultation: Crackles at the beginning (crepitatio indux) Bronchial breath sounds Crackles at the end (crepitatio redux) Bronchophony increased Pneumonia Def: inflammation of the parenchyma, alveoli, connective tissue, bronchioli of the lung Causes: bacteria, virus, Mycoplasma, fungi, chemical of physical effects Pneumonia clinical picture Symptoms: high fever, dyspnoe, cyanosis , chest pain, cough: dry → pus / bloody Exsudative pleuritis (possible) Lab: leukocytosis, left shift, ESR ↑, CRP ↑ X-ray: infiltration Atypical infiltation Massive: also the bronchi filled with exsudation or tumor Central: in the hilar region Pulmonary embolism Pulmonary embolism = embolia pulmonum = thrombus in the arteries of the lung Source: veins of the lower extremities / pelvis Anamnesis !!!! Pulmonary embolism symptoms Short of breath = dyspnea Pleural chest pain Bloody sputum = haemoptysis Collapse = syncope Palpitation Fatigue Cough Pulmonary embolism physical signs Tachypnea Cyanosis Bronchospasm Pleural friction rub Hypotension Tachycardia Fever DVT Pulmonary embolism other exams ECG: right deviation, P pulmonale, PSVT, AF Lab: D-dimer, LDH, sebi Blood gases: hypoxia, hypocapnia + alcalosis Scintigraphy Angio-CT Atelectasis Atelectasis Airless alveoli, air absorbed Causes: Insufficient breathing (weak patient, long bed rest, after abdominal operation) Bronchial obstruction or stenosis by foreign body / tumor / mucus Obstruction of the lung by pleural fluid X-ray Atelectasis Bronchostenosis tactile fremitus: decreased percussion: dullness auscultation: diminished breath sounds bronchophony: decreased Insufficient breathing or compression: air in the bronchi = similar than infiltration : bronchial breath sounds, crackles Pleural effusion Def: fluid accumulation between layers of the pleura Transsudate Exsudate Increased intrathoracic pressure (heart failure) Decreased oncotic pressure: hypoproteinaemia (liver cirrhosis, nephrosis sy) Permeability of the pleura increased + Lymphatic absorption decreased (occlusion or narrowing) Blood Pus Chyle Pleural effusion causes Transsudate Heart failure Liver cirrhosis Pulmonary embolism Nephrotic syndrome Meigs-syndrome, ovarian hyperstimulation Peritoneal dialysis Myxoedema Exsudate Tumor Infection Pulmonary embolism Lung infarction Abdominal diseases Autoimmun diseases Eosinophilic pneumonia Asbest Irradiation Eosophageal perforation Haemothorax Chylothorax Empyema thoracis Pleural effusion Anamnesis: pleuritis sicca (possible) Symptoms: cough dyspnea chest pain Pleural effusion physical signs Inspection: bulging of the affected side, excursion decreased Tactile fremitus: decreased Percussion: dullness Auscultation: breath sounds decreased or absent Bronchophony: decreased Pleural effusion percussion Upper border: Ellis-Damoiseau-line: highest point in the posterior axillary scapular line, going down on both sides Korányi-triangle: fluid dislocates the mediastinum = triangle of dullness on the other side, bordered by the diaphragm and the midline Pleural effusion punction Transsudate Exsudate protein g/l 1-2 3 specific weight < 1015 1018 albumin gradient > 1,1 < 1,1 LDH gradient < 0,6 > 0,6 sediment mesothelial cells lymphocyte leukocyte (pneumonia) malignant cells (tumor) blood tbc, PE tumor Thickening of the pleura Causes: callus or tumor Inspection: retraction of the affected side, chest excursion decreased Percussion: dullness Auscultation: decreased or absent X-ray: shadow, calcification Pleuritis sicca Severe, sharp pain, friction rub at in- and exspiration Patient lies on the affected side Shallow breath If only the diaphragmal pleura affected: pain only at breathing can cause defense in the abdominal muscles at deep inspiration can radiate to the apex, neck Pneumothorax Air in the pleural cavity Causes: from the lung (bulla, bleb) through visceral pleura injury of the chest wall Collapse of the lung = atelectasis + mediastinal shift toward the healthy side Pneumothorax clinics Symptoms: sharp pain at the moment Signs: collaps dyspnea tachycadia Pneumothorax physical exam Inspection: the affected side is bulging, chest excursion decreased Tactile fremitus: decreased or absent Percussion : small: almost no difference large: tympanic dullness of the heart shifted towards the healthy side Auscultation: decreased or absent Bronchophony: decreased or absent Seropneumothorax Fluid at the bottom of the chest X-ray: the border always horizontal Hyppocrat: shake ! Acut tracheo-bronchitis Fever, sore throat Cough (dry → sputum mucouspurulent) Louder breath sounds, prolonged exspiration, adventitious sounds (wheezes, crackles) COPD = chronic aspecific pulmonary disease Chronic bronchitis Emphysema Chronic bronchitis Cough Sputum Dyspnea No change on X-ray ! Symptoms for at least 2 years, for 3 mo /year No other underlying disease Bronchial asthma Sudden onset dyspnea caused by reversible airway obstruction Prolonged exspiration, wheezesrhonchi, use of accessory muscles, tachypnea Emphysema Def: abnormal, permanent enlargement of air spaces distal to bronchioli accompanied by the destruction of its walls Horizontal ribs, lower aperture of the thorax wide, lung borders lower Chest expansion decreased, absolute dullness of the heart decreased or missing Exspiration obstructed, air trapping Percussion: hyperresonance Auscultation: decreased vesicular sound Syndrome of mediastinal tumor Mediastinal lymph nodes: lymphoma, metastasis, Boeck sarcoidosis Aortic aneurysm Substernal goiter Extreme dilatation of left atrium Pericardial fluid Signs of compression caused by mediastinal masses Veins Superior vena cava syndrome Thrombosis Portal hypertension Trachea Cough Asphyxia Tracheomalatia Esophagus Dysphagia Bleeding from dilated veins Cerebrovascular Ischaemia Nerves Recurrent laryngeal nerve palsy → hoarsness Phrenical nerve palsy Horner-triad Chyle Chylothorax Superior vena cava syndrome Venous congestion in the head, neck and upper extremities = Stokes-collar Causes: stenosis, occlusion, thrombosis of mediastinal veins manipulation on veins or PM implantation substernal goiter