Pelvic Inflammatory disease
advertisement

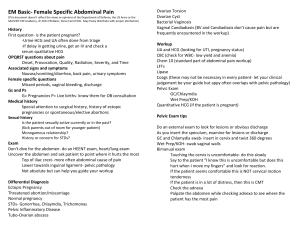
6/10/2012 Pelvic Inflammatory disease Adity Bhattacharyya, MD, FAAFP. RWJMS Family Medicine Residency at Capital Health. Disclosure • Dr. Bhattacharyya has indicated that she has nothing to disclose relative to this presentation. Pelvic inflammatory disease • Pelvic inflammatory disease is a polymicrobial disease of the upper genital tract • Primarily affects young sexually active women • Diagnosis is made clinically 1 6/10/2012 Pelvic inflammatory disease • 750,000 cases a year of PID, mostly in women under 30 yrs • It costs about $1.5 billion annually to treat PID • 80 – 90% of women with Chlamydia infection are asymptomatic • Women with PID have a 20% chance of infertility from tubal scarring Pelvic inflammatory disease • Case 1: 22 year old patient presents to your office with pain in the lower abdomen for the past week which has gotten worse over the last 2 days. Pain is constant, 8/10 in severity, does not radiate and some times gets worse on movement Pelvic inflammatory disease • Urgent conditions that should not be missed: • • • • • Ectopic pregnancy Ovarian torsion Pelvic inflammatory disease Appendicitis Ruptured ovarian cyst 2 6/10/2012 Pelvic inflammatory disease • RISK FACTORS: 1. 2. 3. 4. 5. 6. Age less than 25 Intercourse before age 15 Non Barrier contraception New or multiple sexual partners H/O PID or any STD Vaginal douching Pelvic inflammatory disease • History: • • • • • • • • Pain Relation to menstruation Relation to sexual intercourse Vaginal bleeding Vaginal discharge Urinary and bowel symptoms Past History Sexual history Case 1 • Patient’s LMP was 6 weeks ago but she usually has irregular cycles. • She has been having a yellowish vaginal discharge for the past week which is not foul smelling. • It is painful to have sex for the past week. She is sexually active with her partner for the past 4 weeks. They uses condoms off and on. • She has some mild dysuria, but no urgency. She is usually constipated. 3 6/10/2012 Pelvic inflammatory disease • Physical Examination: • • • • • Vital Signs Abdominal examination Pelvic examination: Speculum and bimanual Rectal examination if needed Musculoskeletal exam of lower back, hip Case 1 • VS: P 120/min, RR 20/min, BP 100/60. Temp 101 degree F. BMI 30. • ABDOMEN: Tenderness in lower abdomen with guarding in the RLQ. BS +, no clear mass palpable • PELVIC: Ext gen normal, copious yellow discharge from cervix which is inflamed Cultures sent • Bimanual:‐ CMT+, Right adnexa tender with some fullness, Left adnexa tender Pelvic inflammatory disease 4 6/10/2012 Pelvic inflammatory disease • LABORATORY TESTING/ IMAGING: • Vaginal wet mount • GC and Chlamydia testing • ESR/ C reactive protein • Ultrasonography • Laparoscopy/ Laparotomy • Endometrial biopsy Pelvic inflammatory disease Case 1 • • • • Urine pregnancy test : negative UA: Leukocytes present, with trace blood GC/Chlamydia Pending CBC: WBC count 12,000 • Pelvic Ultrasound: normal sized uterus and cervix. Bilateral tubal thickening, right side more than left. Large 4 cm fluid filled mass in rt adnexa, possible TO abscess. Free fluid in the cul de sac 5 6/10/2012 Pelvic inflammatory disease Pelvic inflammatory disease Pelvic inflammatory disease CDC criteria for diagnosis for PID: 1. At least one of the following must be present: Adnexal tenderness, cervical motion tenderness, uterine tenderness. 2. Additional Diagnostic criteria: Cervical mucopurulent discharge, elevated ESR /CRP, Fever, positive GC/Chlamydia, WBC on vaginal wet mount. 3. The most specific criteria: EMB, Laparoscopic evidence of PID, Classic US findings of TO abscess. 6 6/10/2012 Pelvic inflammatory disease CRITERIA FOR HOSPITALIZATION 1. Inability to follow or tolerate an outpatient oral regimen 2. No clinical response to oral therapy 3. Pregnancy 4. Severe illness 5. Surgical emergencies cannot be excluded 6. Tubo‐Ovarian abscess Pelvic inflammatory disease • Recommended Parenteral Regimen A • Cefotetan 2 g IV every 12 hours OR Cefoxitin 2 g IV every 6 hours PLUS Doxycycline 100 mg orally or IV every 12 hours • Recommended Parenteral Regimen B • Clindamycin 900 mg IV every 8 hours PLUS Gentamicin loading dose IV or IM (2 mg/kg of body weight), followed by a maintenance dose (1.5 mg/kg) every 8 hours. Single daily dosing (3–5 mg/kg) can be substituted Pelvic inflammatory disease • Alternative Parenteral Regimens • Ampicillin/Sulbactam 3 g IV every 6 hours PLUS Doxycycline 100 mg orally or IV every 12 hours 7 6/10/2012 Pelvic inflammatory disease • Ceftriaxone 250 mg IM in a single dose PLUS Doxycycline 100 mg orally twice a day for 14 days WITH or WITHOUT Metronidazole 500 mg orally twice a day for 14 days Pelvic inflammatory disease • OR Cefoxitin 2 g IM in a single dose and Probenecid, 1 g orally administered concurrently in a single dose PLUS Doxycycline 100 mg orally twice a day for 14 days WITH or WITHOUT Metronidazole 500 mg orally twice a day for 14 days Pelvic inflammatory disease • OR Other parenteral third‐generation cephalosporin (e.g., ceftizoxime or cefotaxime) PLUS Doxycycline 100 mg orally twice a day for 14 days WITH or WITHOUT Metronidazole 500 mg orally twice a day for 14 days 8 6/10/2012 Pelvic inflammatory disease • Clinical recommendations for practice: • No Clinical or Laboratory test is sensitive or specific enough to definitely diagnose PID: C • Empiric antibiotics should be initiated at the time of presentation in patients with symptoms suspicious of PID, even if the diagnosis has not been confirmed: B Pelvic inflammatory disease • Women with mild to moderate PID may receive out patient oral treatment without increased risk of long term sequelae: B • Screening for lower genital tract Chlamydial infection in younger and high risk population is recommended to educe the incidence of PID: A • Asymptomatic disease should be treated: A Pelvic inflammatory disease • Unless there is proven sensitivity, fluoroquinolones should not be used in women with PID because of widespread resistance in Neisseria gonorrhoeae: C 9 6/10/2012 Pelvic inflammatory disease • Questions 10