Can a moral reasoning exercise improve response quality to
advertisement

Ethics
Can a moral reasoning exercise improve response
quality to surveys of healthcare priorities?
M Johri,1 L J Damschroder,2 B J Zikmund-Fisher,3 S Y H Kim,4 P A Ubel5
c Additional data are published
online only at http://jme.bmj.
com/content/vol35/issue1
1
Department of Health
Administration, Faculté de
Médicine, Université de
Montréal, Montréal, Quebec,
Canada; 2 Veteran Affairs Ann
Arbor Healthcare System R&D
Center of Excellence; 3 Center
for Behavioral and Decision
Sciences in Medicine, Veteran
Affairs Ann Arbor Healthcare
System & University of
Michigan; 4 Bioethics Program,
Department of Psychiatry,
Center for Behavioral and
Decisions Sciences in Medicine,
Veteran Affairs Ann Arbor
Healthcare System & University
of Michigan; 5 Center for
Behavioral and Decisions
Sciences in Medicine, Veteran
Affairs Ann Arbor Healthcare
System & University of
Michigan, Ann Arbor, Michigan,
USA
Correspondence to:
Mira Johri, Associate Professor,
Department of Health
Administration, Faculté de
Médicine, Université de
Montréal, CP 6128, succ.
Centre-Ville, Montréal, Quebec,
Canada H3C 3J7; mira.johri@
umontreal.ca
Received 8 February 2008
Revised 4 June 2008
Accepted 10 June 2008
ABSTRACT
Objective: To determine whether a moral reasoning
exercise can improve response quality to surveys of
healthcare priorities
Methods: A randomised internet survey focussing on
patient age in healthcare allocation was repeated twice.
From 2574 internet panel members from the USA and
Canada, 2020 (79%) completed the baseline survey and
1247 (62%) completed the follow-up. We elicited
respondent preferences for age via five allocation
scenarios. In each scenario, a hypothetical health planner
made a decision to fund one of two programmes identical
except for average patient age (35 vs 65 years). Half of
the respondents (intervention group) were randomly
assigned to receive an additional moral reasoning
exercise. Responses were elicited again 7 weeks later.
Numerical scores ranging from –5 (strongest preference
for younger patients) to +5 (strongest preference for older
patients); 0 indicates no age preference. Response quality
was assessed by propensity to choose extreme or neutral
values, internal consistency, temporal stability and appeal
to prejudicial factors.
Results: With the exception of a scenario offering
palliative care, respondents preferred offering scarce
resources to younger patients in all clinical contexts. This
preference for younger patients was weaker in the
intervention group. Indicators of response quality favoured
the intervention group.
Conclusions: Although people generally prefer allocating
scarce resources to young patients over older ones, these
preferences are significantly reduced when participants
are encouraged to reflect carefully on a wide range of
moral principles. A moral reasoning exercise is a
promising strategy to improve response quality to surveys
of healthcare priorities.
As a complement to assessments of safety, efficacy
and economic efficiency, decision-makers seeking
to allocate healthcare resources increasingly
demand information on the values, preferences,
ethical principles and beliefs of the constituencies
they serve. In Canada, values-based decisionmaking and public engagement in the prioritysetting process were recently identified as national
priority areas for research.1 In the UK, both the
National Institute for Health and Clinical
Excellence (NICE) and the National Health
Service (NHS) now view the values of the British
public as vital to fulfilment of their democratic
mandates.2 3
But what is the best way to identify the public’s
values? This paper introduces a novel technique
to investigate social values, evaluates its
performance via a randomised experiment and
assesses its potential contribution to strengthening
J Med Ethics 2009;35:57–64. doi:10.1136/jme.2008.024810
values-based decision-making and public engagement. We evaluate our technique by exploring
people’s attitudes toward the role of patient age in
healthcare resource allocation. This topic was
chosen because it has been researched extensively
in the scientific literature4–12 and by NICE,2 13
which has assumed a leadership role in exploring
social value judgments related to priority setting.2
We first motivate the enquiry with a brief review
of current methods and findings.
Large-scale surveys have been widely used to
explore social value judgements such as the role of
age in healthcare priority setting. Despite their
ability to elicit information from a large crosssection of the public rapidly and at relatively low
cost, these approaches suffer from at least four
important shortcomings. (1) People may require
time to form a considered judgement on an issue,
while such surveys prompt responses based on
initial reactions with little time to reflect.14 15 (2)
Some responses to public surveys may reflect
prejudices unsuitable for embodiment in public
policy. For example, there is evidence of widespread age-based prejudice in society16 and in
medical practice.17–20 (3) Responses can be shaped
inappropriately by subjective factors and framing
effects.12 14 21 22 (4) The perspective of survey
designers may also unintentionally skew results.
Large-scale surveys have found extensive evidence
of public preferences favouring allocation to
younger age groups6–12 but health economists may
systematically have neglected dimensions where
preferences for age-based priority setting are
neutral across age groups or where they favour
the elderly.23
Deliberation is a form of discussion focussing on
careful weighting of reasons for and against some
Proponents
of
deliberative
proposition.24 25
approaches argue that, compared with large-scale
surveys, methods such as focus groups, citizen’s
panels and citizen’s juries increase the quality of
reflection contained in individual responses and
reduce prejudicial responses.14 15 26 The most important vehicle currently used by NICE to investigate
public values is the Citizen’s Council: a 30-member
panel reflecting the age, gender, socio-economic
status and ethnicity of the people of England and
Wales. The Council’s role is to engage in deliberation to help develop the broad social values that
NICE should adopt in preparing its guidance.2 13 27
Reflections on age and priority setting in Citizen’s
Councils have proven more nuanced and less
conclusive than survey responses.13
Deliberative
approaches
have
important
strengths: chief among them is that they enhance
response quality as respondents reflect on and
57
Ethics
reweigh the criteria used to adjudicate scenarios through
conversation.14 28 Although superior in certain respects, deliberative approaches have drawbacks. For example, the number of
participants who can meaningfully deliberate at one time is
small. Deliberative debates, therefore, become exclusive processes restricted to a small group of citizens.25 This raises
concerns about issues such as (1) participant selection; (2)
adequate representation of community views;25 (3) a high cost
per respondent; (4) potential for dominance of group discussions by strong personalities; and (5) a lack of scientific
generalisability due to inherent difficulties in replicating focus
group results.14
We hypothesised that it is possible to draw upon some of the
strengths of deliberation in an affordable manner that would
enable widespread public participation. We conducted a webbased survey of social value judgments concerning healthcare
allocation among age groups and used a randomised design to
assess whether an intervention to improve moral reasoning
influences the relative value people place on age. We also
measured the impact of the moral reasoning intervention on
response quality, decision-making characteristics and quality of
moral reasoning.
METHODS
Participants
Study subjects were members of a panel of over one million
internet users (the ‘‘Survey Spot Internet panel’’) residing in the
United States or Canada who voluntarily agreed to participate
in research surveys.29 Subjects were recruited via email;
participation was encouraged via entry into a sweepstakes
upon survey completion. Web-based surveys are a cost-effective
way to reach large numbers of respondents and are increasingly
used for survey research.23 30–32 We employed a stratified
sampling strategy mirroring the age and sex composition of
the census population of the participant’s country of residence and an experimental survey design using computergenerated randomisation and blinding of participants to group
assignment.
Questionnaire design
Respondents were presented with five allocation scenarios
(Appendix 1; see online supplementary material). All were
designed from the perspective of a health system planner faced
(due to budgetary limitations) with a decision to fund one of
two programmes. Programmes were identical except for patient
age. Scenarios elicited preferences to fund a programme targeted
to younger patients (average age 35 years) versus older patients
(average age 65 years). They included three life-saving programmes (liver and lung transplants and coronary bypass
surgery), depression treatment and palliative care. Allocation
preferences were expressed on a sliding scale from –5 (target
younger patients) to +5 (target older patients), with 0 indicating
no preference between age groups. After responding to the five
scenarios, subjects were asked about emotions evoked while
responding to the survey, whether they wished to change their
responses (although they were not permitted to do so) and to
provide demographic information.
Study procedures
We randomised half of the respondents to a survey with an
embedded moral reasoning exercise (intervention group) and
half to a survey without (control group). Two survey versions
reversing scenario order (liver transplant, palliative care,
58
depression treatment, coronary bypass and lung transplant)
were created and randomly assigned within both control and
intervention groups. Liver and lung transplant scenarios were
identical except for the organ specified. At no point were
subjects able to refer to their previous responses. The
questionnaire was administered at two time points: baseline
and 7 weeks later (follow-up). Everyone received the same
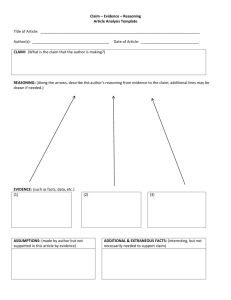
questionnaire at follow-up as at baseline (fig 1).
Intervention
For subjects in the intervention group, the questionnaire
included a moral reasoning exercise. For each of the five
scenarios, intervention group members were asked to read the
scenario description, perform a moral reasoning exercise and
provide allocation preferences. The exercise asked participants
to select which 3 of 10 possible allocation principles they
deemed most important for the scenario under study. The 10
principles appeared in random order for each participant; the
order once presented was consistent within subject across the
scenarios and the two time points. The list of 10 principles was
developed initially from accounts of allocation decisions given
by participants in a prior study on age and priority setting.24 We
coded the rationales, supplemented and refined the list through
a review of the literature in ethics and health economics, and
condensed it to produce an inventory of principles pertinent to
discussions of age and resource allocation (table 1). The
intervention aimed to remind people of principles that they
might not spontaneously have considered and to prompt them
to reflect on their applicability prior to making a decision, as
often happens in conversation with others. Moral reasoning can
be viewed as a species of practical reasoning; that is, as a type of
reasoning directed towards deciding what to do.33 The assigned
exercise aims to enhance participants’ ability to determine a
morally appropriate course of action in response to a specific
scenario. We hypothesised that this moral reasoning exercise
would improve response quality.
Participants in the control group were asked to respond to the
five choice scenarios without undertaking the moral reasoning
exercise. However, to gain insight into their moral reasoning,
control group members were presented with the moral reasoning exercise once, after the last scenario (either liver or lung
transplant, depending on the scenario order to which they were
randomised).
Outcome measures
In order to assess respondents’ age-related allocation preferences, we compared response patterns between intervention
and control groups on the 25 to +5 numerical response scale.
We also compared the three principles selected by intervention
and control group members as most important in the moral
reasoning exercise for either liver or lung transplant (depending
on survey version received). To gain insight into moral
reasoning for the intervention group, we analysed their
responses to the moral reasoning exercise for all scenarios.
We used four criteria, defined prior to fielding the study, to
evaluate response quality:
1. Rates of ‘‘no preference’’ and ‘‘extreme’’ responses On our
response scale, a value of 0 signals neutrality between age
groups, while 25 (+5) reflects the strongest preference to
allocate resources to younger (older) patients. Based on the
responses of an earlier study, we expected that participants
would exhibit higher rates of ‘‘no preference’’ responses for
depression treatment and palliative care, but maintain
strong preferences towards younger groups for the three
J Med Ethics 2009;35:57–64. doi:10.1136/jme.2008.024810
Ethics
Figure 1 Flowchart of trial. The study
was originally designed as two identical
experiments fielded in parallel: one in
Canada and one in the USA. As analyses
showed that preferences did not differ
significantly between Canada and the
USA, we pooled data in the results and
present a consolidated design in this
flowchart. We adjusted for country as
appropriate in modelled analyses. All
respondents who completed baseline
analyses were invited to repeat the
survey 2 weeks later. Experimental group
assignments were preserved during
follow-up analyses.
J Med Ethics 2009;35:57–64. doi:10.1136/jme.2008.024810
59
Ethics
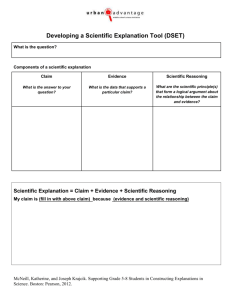
Table 1 Proportion (%) of respondents* selecting each allocation principle{ by scenario{
Scenario
Allocation principle
Equal treatment
Sample comment"
‘‘All patients deserve
the best medical care,
regardless’’
Patient need
‘‘Give it to the group
that needs it most’’
Relief from suffering
‘‘We should always
relieve pain when we
can’’
Capacity to benefit/best
‘‘Give the treatment to
outcomes
patients who will
benefit most’’
Maximise number helped ‘‘Fund the programme
that helps the most
people’’
Family responsibilities
‘‘At 35, people are
likely to be raising
families’’
Guarantee chance for
‘‘Give the younger
‘‘full life’’
patients a chance for
full life’’
Duration of benefit
‘‘Giving the treatment
to the younger group
makes sense since
they will enjoy it
longer’’
Personal responsibility for ‘‘Society shouldn’t pay
health
to treat people who
haven’t taken care of
themselves’’
Economic productivity
‘‘Help those who are
most likely to have
jobs they have to do’’
Depression
treatment
Liver transplant
Palliative care
46
55{
50
42
54{
34
Coronary bypass
Lung transplant
Overall
44
47
48
50{
47
41
47
68{
33
34
37
41
35
24{
33
35
37
33
31
34
36
28
31
32
38
17{
31{
33{
36
31
22
26{
36{
28{
23
27
24
12{
15{
21
21
19
16
7{
8{
22{
17
14
11
3{
8
9
9
8
*Analysis for intervention group at baseline only, n = 942. A similar analysis performed at follow-up is available upon request. The follow-up analysis showed no differences
compared with the baseline analysis with the exception of a statistically significant reduction in selection of ‘‘family responsibilities’’ as a relevant allocation principle; {after each
scenario was introduced, intervention group respondents were asked to perform a moral reasoning exercise asking them to select 3 of a possible 10 allocation principles
(reproduced here). They were asked to select principles relevant to the scenario under consideration, in response to the question: ‘‘How important is each principle to you for making
a decision as to which programme to fund?’’ {indicates a statistically significant difference (p,0.05) based on logistic regression models adjusting for age and male, taking liver
transplant as the reference scenario; "several sample comments were provided for each allocation principle—these are illustrative only.
2.
3.
4.
60
lifesaving scenarios (lung transplant, liver transplant,
bypass surgery).23 We expected few respondents to choose
positive extreme values for any of the scenarios.23 We
compared rates of ‘‘no preference’’ and ‘‘extreme’’
responses across experimental groups to better understand
how members of each group made decisions.
Internal consistency The liver and lung transplant scenarios
were identical except for the organ named and, thus,
preferences should be equivalent. We compared responses
to these scenarios for each participant separately by
experimental group.
Temporal stability If they are to inform public policy,
preferences for resource allocation should be relatively
stable over time. This critical dimension of response
quality is virtually unexplored. We examined consistency
in responses at baseline and follow-up for intervention and
control groups.
Assessment of ‘‘prejudicial reasons’’ We assessed the quality
of moral reasoning by examining respondents’ assessments
of prejudicial reasons. The coronary bypass surgery
scenario included the following statement, deliberately
pejorative for the younger group: ‘‘Almost 90% of the risk
of developing the severe form of CAD (coronary artery
disease) is because of lifestyle choices like smoking
cigarettes, poor diet and a lack of regular exercise. A
healthy lifestyle can substantially delay the age at which a
heart attack occurs.’’ Focus group studies report that
statements placing blame for health conditions on
individual behaviours receive less weight after group
discussion.13 15 Our aim was to see whether the moral
reasoning exercise would prompt respondents in the
intervention group to evaluate this statement differently
than did those in the control group. If the reference to
lifestyle factors appeared less salient upon reflection, this
would be associated with a higher rate of neutral
preference scores or scores favouring the younger for the
intervention (compared with the control) group.
Statistical analyses
We compared demographic characteristics across experimental
groups using Student’s t test for continuous variables (that is,
age) and x2 tests for categorical variables.
Numerical preference scores were assessed as continuous
variables on the 25 to +5 response scale. We compared mean
outcomes and frequencies of neutral and extreme responses
across experimental groups using the Student’s t test. For each
of the 10 allocation principles, we used logistic regression to
model the odds of its occurrence using dummy variables for
scenario. We assessed the impact of the intervention and survey
timing on preference scores using cross-sectional time-series
random-effects regression models adjusted for demographic
characteristics (country, health status and education level) and
J Med Ethics 2009;35:57–64. doi:10.1136/jme.2008.024810
Ethics
clustered by participant. Results were confirmed using ordered
logistic regression.
Analyses were performed using Stata (v.9) on all participants
for whom reliable information on outcome measures was
available (per protocol analysis).
Additional information on the methods can be found in the
online supplementary material.
follow-up). Overall, of the people who initially responded to the
invitation, 78% were included in the baseline analyses (1239
receiving the intervention and 1333 controls) and 48% in the
follow-up analyses (574 receiving the intervention and 671
controls).
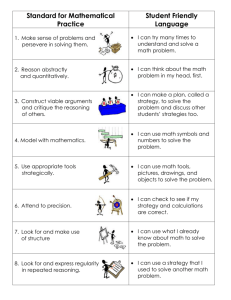
Characteristics of subjects at baseline are described in table 2.
Participants in experimental groups had similar characteristics.
RESULTS
Sample characteristics
Outcome measures
From April to June 2005, 2574 (8%) of internet users who
received an email invitation responded by clicking onto the
survey (fig 1). Of those who responded, 2020 (79%) completed
the baseline survey and were invited to return and 1247 (62%)
completed the follow-up 7 weeks later. Participants who
admitted that they gave ‘‘intentionally wrong answers’’ were
excluded from the analyses (11 individuals at baseline and 2 at
Analyses showed that preferences did not differ significantly
between Canada and the United States. As recruiting mechanisms were identical, concurrent and from the same source, we
pooled data and adjusted for country in regression analyses.
Numerical preference scores
Participants in both experimental groups preferred offering
scarce resources to young patients over older patients in all
Table 2 Respondent characteristics at baseline*
Variable
Age (years)
Male sex
Country of residence
USA
Canada
Minority?{ (US only)
Education
Secondary school or less"
Some post-secondary1
Bachelors degree
Masters degree or more**
Self-rated health{{
Excellent
Very good
Good
Fair
Poor
Employment status{{
Full-time employment
Part-time employment
Not employed
Civil status{{
Single/never married
Married
Divorced/separated/widowed
Living with partner
Annual income ($) (n = 1822){{
,20 000
20 000–49 999
50 000–74 999
75 000–99 999
100 000–150 000
.150 000
Time to complete survey (minutes)
Baseline
Follow-up
Intervention group
942 (47%)
Control group
1067 (53%)
Overall
2009{ (100%)
45 (SD 15)
457 (49)
46 (SD 15)
497 (47)
466 (49)
476 (51)
103 (22)
552 (52)
515 (48)
135 (25)
189
483
182
87
(20)
(51)
(19)
(9)
255
499
231
82
(24)
(47)
(22)
(8)
444
982
413
169
(22)
(49)
(21)
(8)
112
349
350
108
23
(12)
(37)
(37)
(11)
(2)
114
400
385
136
31
(11)
(38)
(36)
(13)
(3)
226
749
745
244
54
(11)
(37)
(37)
(12)
(3)
45 (SD 15) (14 to 95)
48 (954)
1018 (51)
991 (49)
238 (23)
470 (50)
148 (16)
324 (34)
518 (49)
179 (17)
370 (35)
216
496
152
77
(23)
(53)
(16)
(8)
212
582
203
69
(20)
(55)
(19)
(6)
428
1078
355
146
(21)
(54)
(18)
(7)
121
360
211
84
48
18
(14)
(43)
(25)
(10)
(6)
(2)
164
417
210
102
59
18
(17)
(43)
(22)
(11)
(6)
(2)
285
777
421
186
107
36
(16)
(43)
(23)
(10)
(6)
(2)
17 (SD 19)
11 (SD 10)
13 (SD 16)""
9 (SD 7)""
998 (49)
327 (16)
624 (35)
15 (SD 18)""
10 (SD 8)""
*Variables reported as frequency (per cent) unless otherwise stated. Sample size (n) is given at top of column unless otherwise indicated. Percentages may not sum to 100 due to
rounding; {the denominator is 2009 unless otherwise indicated. Numbers may not sum to 2009 due to missing values; {information on race/ethnicity was sought only for US
participants. Minority status is defined as ‘‘underrepresented minority’’ by the US Federal Office of Management and Budget (OMB) for the health professions, science and
engineering (http://www.whitehouse.gov/omb/fedreg/race.ethnicity.html (accessed 27 October 2008)) and was defined as those who self-identified as black, Hispanic, American
Indian/Alaskan Native or Pacific Islander; "denotes all those whose maximum educational attainment is successful completion of 12 years of formal schooling (high-school
diploma); 1defined as those with a high-school diploma who attended trade school or attended some college. Those who completed a 2-year degree (for example, AA, AS) are
included in this category; **‘‘masters’ degree or more’’ refers to those respondents holding a masters degree, a doctoral degree or a professional degree such as an MD; {{the
denominator for these variables is 2020. Numbers may not sum to 2020 due to missing values; {{annual household incomes reported in nominal dollars; ""difference between
intervention and control groups statistically significant at the p,0.001 level.
J Med Ethics 2009;35:57–64. doi:10.1136/jme.2008.024810
61
Ethics
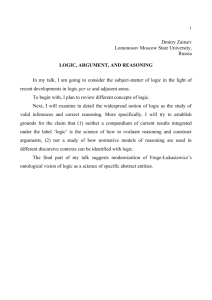
Table 3 Mean preference scores* for intervention and control groups at baseline and follow-up{
Baseline
Follow-up
Scenario
Intervention group n = 942
Control group n = 1067
Intervention group n = 574
Control group n = 671
Liver transplant
Palliative care
Depression treatment
Coronary bypass
Lung transplant
21.35
0.01
20.71
20.83
21.24
21.89{
0.15
21.04{
21.22{
21.86{
21.191
20.05
20.67
20.85
21.10
21.48"**
0.011
20.92*
21.07
21.57{1
*Scores range from –5 (preference for programme serving 35-year-olds) to +5 (preference for programme serving 65-year-olds); 0 indicates no preference between age groups; {all
comparisons based on unadjusted scores using the t test to assess the equality of means for independent populations with equal variances; {difference between experimental
groups (intervention baseline vs control baseline; intervention follow-up vs control follow-up) statistically significant at the p,0.001 level; "difference between experimental groups
(intervention baseline vs control baseline; intervention follow-up vs control follow-up) statistically significant at the p,0.05 level; 1difference within experimental groups
(intervention baseline vs intervention follow-up; control baseline vs control follow-up) statistically significant at the p,0.05 level; **difference within experimental groups
(intervention baseline vs intervention follow-up; control baseline vs control follow-up) statistically significant at the p,0.001 level.
clinical contexts except palliative care. However, participants in
the intervention group showed weaker preferences for treating
younger patients than did those in the control group (table 3).
At baseline, differences between experimental groups were
significant (p,0.001) for all scenarios except palliative care. In
the follow-up survey, differences between experimental groups
were significant for three of five scenarios (lung transplant
(p,0.001), liver transplant and depression treatment (p,0.05)).
Regression models adjusting for demographic factors largely
confirmed the effects of the moral reasoning exercise and survey
timing. For palliative care, only timing was significant in the
model (p,0.05). For the depression and bypass surgery
scenarios, the moral reasoning exercise (p,0.01) significantly
reduced preferences but timing did not (p.0.72). For the liver
and lung transplant scenarios, the moral reasoning exercise
(p,0.001) and giving preferences at follow-up (p,0.01) both
reduced preferences significantly through independent effects.
We found no interaction between survey timing and the
intervention (p.0.17).
Assessment of ‘‘prejudicial reasons’’
The coronary bypass scenario deliberately included a prejudicial
factor stressing the importance of maintaining a healthy
lifestyle. Intervention group members identified lifestyle as an
important consideration more frequently in the bypass scenario
than in any other scenario (table 1; 22% vs 16–17% for liver and
lung and 7–8% for palliative care and depression), suggesting
that our scenario description was effective at prompting people
to think about this factor.
As predicted, however, the moral reasoning intervention
reduced the weight people placed on this lifestyle factor. For the
bypass scenario, the mean preference score for those in the
intervention group is closer to 0 than for controls (table 1;
p,0.001).
Internal consistency
Liver and lung scenarios were identical except for organ;
individual respondents’ preference scores for these two scenarios
should therefore agree. We found that differences in preferences
for these two scenarios were close to zero regardless of
experimental group (p.0.15).
Analysis of moral reasoning
Overall, the most important allocation principles identified by
respondents who received the moral reasoning intervention
(table 1) were equal treatment for all, meeting patient needs and
promoting relief from pain and suffering. Considerable variation
was observed in response patterns across scenarios; however, no
significant differences in response patterns for the (identical)
lung and liver transplant scenarios were found either within the
intervention group or between experimental groups. For the
transplant scenarios, members of the intervention and control
groups selected the same moral considerations as most
important: equal treatment, relief of pain and suffering, and
meeting patient needs.
Evaluation of response quality
Rates of ‘‘no preference’’ and ‘‘extreme’’ responses
The baseline rate of ‘‘no preference’’ responses was higher for
the intervention group (p,0.001) for all scenarios. Rates of
extreme responses are also influenced by experimental group
membership. Intervention group participants showed less
tendency to choose extreme values favouring the young
(p,0.001) for all scenarios and to choose extreme values
favouring the old (p,0.001) for palliative care and bypass
scenarios. Other scenarios had very low rates of people selecting
the older population.
62
Temporal stability
While both groups modified their responses over time to reflect
less age preference, control group responses were less stable
(table 3). Responses for the control group showed a significant
shift towards neutrality in preferences between age groups from
baseline to follow-up for three of the five scenarios (liver
transplant (p,0.001), lung transplant (p,0.05) and palliative
care (p,0.05)). Responses for the intervention group showed a
significant shift toward neutrality from baseline to follow-up
for only one of the five scenarios (liver transplant; p,0.05).
DISCUSSION
Principal finding
Can a moral reasoning exercise improve response quality to
surveys of healthcare priorities? We used an experimental design
and elicited preferences for patient age via choice scenarios to
study this question. Consistent with previous work, for both
experimental groups, we found that age preferences favour
younger patients6–12 23 34–36 and differ in strength according to the
clinical context.23 36 People displayed the strongest preference for
the younger group in lifesaving scenarios when resources are
especially scarce, such as transplants, but showed no age
preference in the palliative care scenario.
The principal finding of this study is that age preferences
were modified by the moral reasoning exercise. Specifically, for
J Med Ethics 2009;35:57–64. doi:10.1136/jme.2008.024810
Ethics
all scenarios except palliative care, the strength of preferences
favouring the young was significantly diminished among those
receiving the moral reasoning intervention, although it was not
eliminated. This change was accompanied by an improvement
in response quality.
Strengths and weaknesses
This study has several important strengths, including a
randomised design and a large and heterogeneous pool of
respondents drawn from two countries. Among social value
surveys of age, it is unique in assessing response quality and
innovates by seeking insight into patterns of moral reasoning. It
is, to our knowledge, the first social value survey to assess the
temporal stability of responses in this context.
Three issues merit close consideration:
1. Although we stratified the invitation list to mirror the
United States and Canadian populations with respect to age
and gender, concerns can be raised regarding the sample
composition. Our strong 79% completion rate notwithstanding, given the initial 8% response rate for the baseline
survey overall, only 6% of people in the United States and
15% in Canada invited to participate in the baseline survey
actually completed it. Moreover, the sample is self-selected
to include a predominance of internet users with higher
income and higher educational attainment. These problems
are common to internet surveys based on opt-in panels.31 36
In a review of internet surveys, Couper cites response rates
ranging from 8–60% and notes the potential for response
bias.37 Our intent was to conduct a randomised study to
elicit responses from a heterogeneous sample of subjects so
as to assess the potential of a novel intervention to improve
response quality. We succeeded in recruiting a large and
diverse pool of subjects to this task and do not intend to
generalise the specific age preference values obtained to the
general population. Given our objectives, issues of sample
selection are of lesser concern. However, future research
studies might usefully consider departing from opt-in panels
by employing methods designed to represent general
populations such as proportional sampling based on
random digit dialling.
2. Although intention-to-treat (ITT) analysis is considered an
ideal for randomised clinical trials, our study took a perprotocol approach. An ITT approach, which analyses all
participants according to original experimental group
assignment regardless of subsequent events, would have
required us to impute missing age preference scores for all
participants who failed to complete the survey.38 We judged
this task inappropriate to the goals of the study. ITT
analysis is legitimately defended as the gold standard when
the goal is to assess the effect of a treatment or policy in a
general population that will include deviations from
protocol and non-compliant individuals. The question we
are asking is a distinct one, oriented towards establishing
the potential for an intervention effect in a large and
heterogeneous population. As specified in the original
protocol, our analyses included all participants who
completed a survey and reported giving truthful answers.
We feel that this approach is fully suited to our study
question.
3. While the intervention serves to modify response patterns,
does it improve response quality? Our study traced the
impact of the moral reasoning intervention on response
quality in four dimensions of which two were selected to
permit comparison with findings from focus groups.
Although there is no gold standard for the public’s age
preferences, focus groups are commonly acknowledged to
J Med Ethics 2009;35:57–64. doi:10.1136/jme.2008.024810
yield better-quality responses than standard large-scale
surveys. In keeping with focus groups results suggesting
that participants become more nuanced in their judgments
and attenuate the strength of their age preferences through
deliberation, we found that rates of no preference responses
were greater and rates of extreme responses favouring the
young were lower for the intervention group for all
scenarios.14 15 26 Results from the bypass scenario are
consistent with the intervention group giving less weight
to a prejudicial statement, as documented in focus
groups.13 15 However, these results are also consistent with
the overall pattern of attenuation of age preferences. The
remaining two criteria, internal consistency and temporal
stability, are formal criteria of good response quality.
Experimental groups were found to be equally consistent
but the intervention group generally gave more stable
responses over time. Temporal stability was assessed by
comparing consistency in numerical responses between
experimental groups at baseline and follow-up. While both
groups modified their responses over time to reflect less age
preference, control group responses were considerably less
stable than those from the intervention group, showing
significant shifts toward neutrality for three of five
scenarios (vs one of five for the intervention group).
Together, these results provide plausible evidence of
improved response quality for the intervention group.
Interpretation of findings
The internal validity of the study is high: the fundamental
finding that the moral reasoning exercise attenuated age
preferences is unlikely to be due to bias in the design and
conduct of this randomised study. In fact, four of the ten
allocation principles presented in the moral reasoning exercise
gave explicit rationales favouring younger patients; the rest
made no reference to age. Due to issues of sample selection,
specific age preference values from our study should not be
attributed to the general populations of Canada and the United
States. This caution notwithstanding, the qualitative insights
generated from these results have a remarkable convergence
with findings from other studies on age in priority settings
conducted using different study designs, populations and
methodologies.6–13 15 23 34–36
The moral reasoning exercise generated valuable insights in
its own right. Despite the diversity of scenarios, and although
several principles explicitly favoured younger patients for all
scenarios, the three principles selected as most important were
equality of treatment, meeting patient needs and relief of pain
and suffering. These social values do not reflect age preferences
and are not aligned with the allocation principles (namely.
maximisation of best outcomes, duration of benefit, maximisation of the number helped) privileged in cost-effectiveness
analysis (CEA).
CONCLUSIONS
Age preferences favouring the young exist, vary with clinical
context and are significantly reduced when participants are
encouraged to reflect on a wide range of moral principles in a
moral reasoning exercise. These findings have several implications. Concerning the debate on the relevance of patient age for
healthcare priority setting, they show that claims that the
public favours age-based rationing on equity grounds5–12 have a
much weaker empirical basis than previously thought, undercutting calls for age weighting of health benefits in CEA.
Findings from standard surveys using choice scenarios to elicit
age preferences should be interpreted with caution. In the
63
Ethics
absence of a moral reasoning exercise similar to our own, they
are likely to overstate age preferences.39
Results from the moral reasoning exercise showed that the
values held by the general public are in tension with those
privileged in economic evaluations. Participants favoured
allocation principles that supported procedural justice and
humanitarian response to suffering over the consequentialist
approach privileged in CEA methods and welfare economics.14 23 36 40 Since public values and CEA values are demonstrably
distinct, public consultation is essential for democratic, responsive setting of health priorities. The results of CEA should be
interpreted and contextualised in light of broader public values
related to equity and social justice.
Large-scale surveys have a unique contribution to make to the
process of public consultation. In contrast to face-to-face
deliberative methods, surveys extend the possibility of engaging
a large and diverse population of respondents at a relatively low
cost, enhancing external validity and replication of results.
Incorporation of a moral reasoning exercise into large-scale
surveys of social values is a promising new strategy for engaging
the public in the process of priority setting. It should be
investigated as a tool for policy setting bodies seeking to
incorporate social values in decisions concerning allocation of
health resources.
Acknowledgements: We thank Drs Howard Bergman and François Béland of the
Solidage Research Group for invaluable guidance.
Funding: The study was supported by the Department of Veterans Affairs, Veterans
Health Administration, Ann Arbor Veteran Affairs Healthcare System R&D Center of
Excellence, and by grants from the Canadian Institutes of Health Research (CIHR),
(Project number 43817) and the US National Institutes of Health (NIH) (R01-HD40789
and R01-HD38963). Dr Johri is a recipient of a New Investigator Award from the CIHR.
Dr Zikmund-Fisher is supported by a career development award from the American
Cancer Society (MRSG-06-130-01-CPPB). The funding agreements ensured the
authors’ full independence in designing the study, interpreting the data, and writing
and publishing the report.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
Competing interests: None.
29.
Ethics approval: Exemption from ethics approval was granted by the Institutional
Review Boards of the University of Michigan Medical School (IRBMED).
30.
REFERENCES
31.
1.
2.
3.
4.
5.
6.
7.
8.
9.
64
Canadian Institutes for Health Research (CIHR), Canadian Health Services
Research Foundation (CHSRF). Listening for Direction III: A National Consultation on
Health Services and Policy Issues (2007). 2007. http://www.cihr-irsc.gc.ca/e/20461.
html (accessed 23 October 2008).
National Institute for Clinical Excellence (NICE). Social value judgments:
Principles for the Development of NICE Guidance. NICE 2008. http://www.nice.org.
uk/media/CI8/30/SVJPublication2008.pdf (accessed 27 October 2008).
Department of Health. Our health, our care, our say: a new direction for community
services. London; Department of Health, 2006:1–236. http://www.dh.gov.uk/en/
publicationsandstatistics/publications/publicationspolicyandguidance/dh_4127453
(accessed 27 October 2008).
Williams A. Intergenerational equity: an exploration of the ‘fair innings’ argument.
Health Econ 1997;6:117–32.
Tsuchiya A. QALYs and ageism: philosophical theories and age weighting. Health
Econ 2000;9:57–68.
Lewis PA, Charny M. Which of two individuals do you treat when only their ages are
different and you can’t treat both? J Med Ethics 1989;15:28–34.
Busschbach JJ, Hessing DJ, de Charro FT. The utility of health at different stages in
life: a quantitative approach. Soc Sci Med 1993;37:153–8.
Cropper ML, Ayede SK, Portney PR. Preferences for life-saving programs: How the
public discounts time and age. J Risk Uncertain 1994;8:243–65.
Johannesson M, Johansson PO. Is the valuation of a QALY gained independent of
age? Some empirical evidence. J Health Econ 1997;16:589–99.
32.
33.
34.
35.
36.
37.
38.
39.
40.
Rodriguez E, Pinto JL. The social value of health programmes: is age a relevant
factor? Health Econ 2000;9:611–21.
Ratcliffe J. Public preferences for the allocation of donor liver grafts for
transplantation. Health Econ 2000;9:137–48.
Tsuchiya A, Dolan P, Shaw R. Measuring people’s preferences regarding ageism in
health: some methodological issues and some fresh evidence. Soc Sci Med
2003;57:687–96.
National Institute for Clinical Excellence (NICE). NICE Citizens Council Report
on Age. NICE, 2004. http://www.nice.org.uk/page.aspx?o = 101368 (accessed 23
October 2008).
Cookson R, Dolan P. Public views on health care rationing: a group discussion study.
Health Policy 1999;49:63–74.
Dolan P, Cookson R, Ferguson B. Effect of discussion and deliberation on the public’s
views of priority setting in health care: focus group study. BMJ 1999;318:916–19.
Palmore E. The ageism survey: first findings. Gerontologist 2001;41:572–5.
Rathore SS, Mehta RH, Wang Y, et al. Effects of age on the quality of care provided
to older patients with acute myocardial infarction. Am J Med 2003;114:307–15.
Alter DA, Manuel DG, Gunraj N, et al. Age, risk-benefit trade-offs, and the projected
effects of evidence-based therapies. Am J Med 2004;116:540–5.
Krumholz HM, Radford MJ, Wang Y, et al. Early beta-blocker therapy for acute
myocardial infarction in elderly patients. Ann Intern Med 1999;131:648–54.
Soumerai SB, McLaughlin TJ, Spiegelman D, et al. Adverse outcomes of underuse
of beta-blockers in elderly survivors of acute myocardial infarction. JAMA
1997;277:115–21.
Ubel PA. How stable are people’s preferences for giving priority to severely ill
patients? Soc Sci Med 1999;49:895–903.
Ubel PA, Baron J, Asch DA. Social responsibility, personal responsibility, and
prognosis in public judgments about transplant allocation. Bioethics 1999;13:57–68.
Johri M, Damschroder LJ, Zikmund-Fisher BJ, et al. The importance of age in
allocating health care resources: does intervention-type matter? Health Econ
2005;14:669–78.
Fearon JD. Deliberation as discussion. In: Elster J, ed. Deliberative Democracy.
Cambridge: Cambridge University Press, 1998:44–68.
Abelson J, Forest PG, Eyles J, et al. Deliberations about deliberative methods: issues
in the design and evaluation of public participation processes. Soc Sci Med
2003;57:239–51.
Abelson J, Eyles J, McLeod CB, et al. Does deliberation make a difference? Results
from a citizens panel study of health goals priority setting. Health Policy
2003;66:95–106.
National Institute for Clinical Excellence (NICE). Citizens Council Meeting
Report on Inequalities in Health. NICE 2006:1–32. http://www.nice.org.uk/page.
aspx?o = 384319 (accessed 23 October 2008).
Dolan P. Drawing a veil over the measurement of social welfare–a reply to
Johannesson. J Health Econ 1999;18:387–90.
Survey Sampling International (SSI). http://www.surveysampling.com (accessed
27 October 2008).
Damschroder LJ, Baron J, Jepson C, et al. The validity of person tradeoff with
computer elicitation versus face-to-face interview. Med Decis Making
2004;24:170–80.
Damschroder LJ, Zikmund-Fisher BJ, Ubel PA. The impact of considering adaptation
in health state valuation. Soc Sci Med 2005;61:267–77.
Damschroder LJ, Ubel PA, Riis J, et al. An alternative approach for eliciting
willingness-to-pay: A randomized Internet trial. Judgment and Decision Making
2007;22:96–106.
Richardson HS. Moral Reasoning. In: Zalta EN, ed. The Stanford Encyclopedia of
Philosophy. California: Stanford University, 2007. http://plato.stanford.edu/archives/
fall2007/entries/reasoning-moral (accessed 23 October 2008)
Tsuchiya A. Age-related preferences and age weighting health benefits. Soc Sci
Med 1999;48:267–76.
Nord E, Street A, Richardson J, et al. The significance of age and duration of effect in
social evaluation of health care. Health Care Anal 1996;4:103–11.
Nord E, Richardson J, Street A, et al. Maximizing health benefits vs egalitarianism:
an Australian survey of health issues. Soc Sci Med 1995;41:1429–37.
Couper MP. Internet Surveys. In: Lewis-Beck M, Bryman AE, Liao TF, eds. The SAGE
Encyclopedia of Social Science Research Methods. Thousand Oaks, California: Sage,
2003.
Consort Group. The Consort (Consolidated Standards of Reporting Trials) Statement.
http://www.consort-statement.org/index.aspx?o = 1089 (accessed 23 October
2008).
Eisenberg D, Freed GL. Reassessing how society prioritizes the health of young
people. Health Aff (Millwood) 2007;26:345–54.
Damschroder LJ, Roberts TR, Goldstein CC, et al. Trading people versus trading
time: what is the difference? Popul Health Metr 2005;3:10.
J Med Ethics 2009;35:57–64. doi:10.1136/jme.2008.024810