Function of Bones
• They function in providing:
Bone Tissue and Bones
Bones form the framework of the skeleton.
Anatomy and Physiology Text and Laboratory Workbook, Stephen G.
Davenport, Copyright 2006, All Rights Reserved, no part of this publication can
be used for any commercial purpose. Permission requests should be
addressed to Stephen G. Davenport, Link Publishing, P.O. Box 15562, San
Antonio, TX, 78212
– (1) structural support,
– (2) attachment sites for tissues and organs,
– (3) protection - especially for the brain and organs of
the chest,
– (4) a mineral storage site - especially for calcium and
phosphorus,
– (5) a site (red bone marrow) for the production of the
formed elements of blood, and
– (6) providing a site for fat deposit (yellow bone
marrow).
BONE CLASSIFICATION
A general classification of bones
is by their external shape.
• Long bones
Long Bones
Gross Anatomy
– Long bones are longer than
they are wide.
• Short bones
– Short bones are boxy in
shape.
Long bones are longer than they are wide.
• Flat bones
– Flat bones are thin and
flattened.
• Irregular bones
– Irregular bones are irregular in
shape, often with curved,
pointed, and ridged surfaces.
Fig 10.1
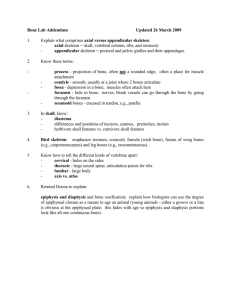
Lab Activity 1 Gross Anatomy of a Long Bone
Observe a longitudinally sectioned femur.
Know the following:
• Articular cartilage (removed; identify as to
its placement)
• Compact bone
• Diaphysis (shaft).
• Endosteum (removed; identify placement)
• Epiphyseal line
• Epiphyses
• Medullary (marrow) cavity
• Periosteum (removed; identify placement)
• Spongy bone
• Red bone marrow
• Trabeculae
• Yellow bone marrow
Fig 10.2
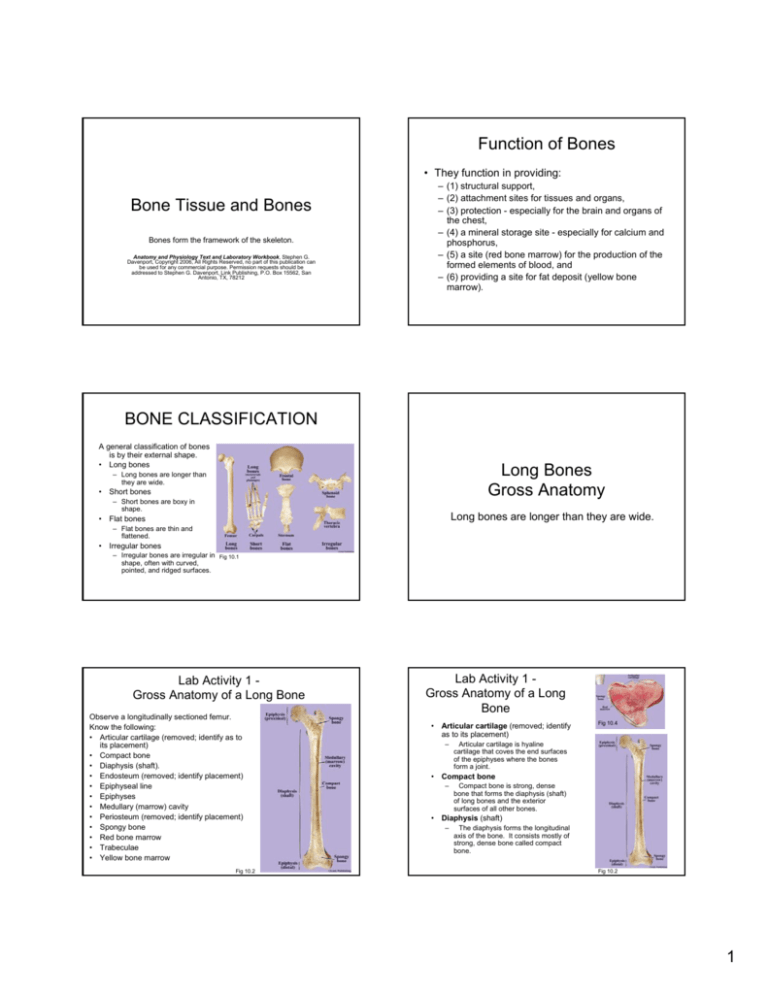
Lab Activity 1 Gross Anatomy of a Long
Bone
• Articular cartilage (removed; identify
as to its placement)
–
Fig 10.4
Articular cartilage is hyaline
cartilage that coves the end surfaces
of the epiphyses where the bones
form a joint.
• Compact bone
–
Compact bone is strong, dense
bone that forms the diaphysis (shaft)
of long bones and the exterior
surfaces of all other bones.
• Diaphysis (shaft)
–
The diaphysis forms the longitudinal
axis of the bone. It consists mostly of
strong, dense bone called compact
bone.
Fig 10.2
1
Lab Activity 1 Gross Anatomy of a Long Bone
• Epiphyses
• Endosteum (removed; identify as
to its placement)
–
–
The endosteum is a membrane that
lines the medullary cavity, the
trabeculae of spongy bone (mostly in
the epiphyses), and extends into the
central canals of the osteons
(Haversian systems). The endosteum
is composed mostly of osteoprogenitor
cells, osteoblasts, and osteoclasts.
An epiphyseal line is a line of bone
formed by trabeculae at the site where
a cartilage growth area, the epiphyseal
plate, was located. The epiphyseal
line in the distal epiphysis of the femur
is the easiest to observe.
Epiphyses are the expanded ends of
the long bone. The epiphyses are
described as proximal or distal according
to their respective closer or farther
placement from the body. Their external
surface is composed of thin, compact
bone. Internally, they are composed of
spongy bone.
• Medullary (marrow) cavity
• Epiphyseal line
–
Lab Activity 1 Gross Anatomy of a Long Bone
–
The medullary cavity is a large cavity
within the diaphysis of a long bone and
partially extends into the epiphyses. In
adults, it contains mostly fatty (yellow)
bone marrow.
Fig 10.2
Fig 10.2
Lab Activity 1 Gross Anatomy of a Long Bone
Lab Activity 1 Gross Anatomy of a Long Bone
• Periosteum (removed; identify
placement)
–
• Red bone marrow
The periosteum is a membrane that
covers the outer surface of the diaphysis
and the epiphyses, except at their articular
cartilage surfaces. The periosteum
consists of an inner cellular layer and an
outer fibrous layer. The cellular layer is
composed mostly of osteoprogenitor cells
(stem cells), bone-producing cells
(osteoblasts), and bone-removing cells
(osteoclasts.) The fibrous layer is mostly
dense irregular connective tissue that
provides attachment sites for tendons,
ligaments, and into the bone itself by
perforating fibers (Sharpey’s fibers) which
penetrate the cellular layer into the matrix
of compact bone.
–
Red bone marrow is
located in the spongy bone
tissue of the epiphyses of
long bones and within the
spongy bone tissue of all
other bones.
– Red bone marrow is the
tissue where the formed
The formed elements enter
into blood capillaries in the
marrow.
• Spongy bone
–
Spongy bone is composed of thin plates
of bone called trabeculae. Spongy bone is
located in the epiphyses of long bones and
forms the internal framework in all other
bones.
Fig 10.4
Fig 10.2
Fig 21.6
Lab Activity 1 Gross Anatomy of a Long Bone
• Trabeculae
–
Trabeculae are thin plates of bone
that form the internal framework of
the epiphyses of long bones and
most other bones. Trabeculae form
an inner framework that is strong,
light, and contains red bone marrow.
Flat Bones
Gross Anatomy
A flat bone is characterized by being
thin and flat, with an internal framework
of spongy (trabecular) bone.
• Yellow bone marrow
–
Yellow bone marrow is found within
the medullary (marrow) cavity of long
bones. It consists mostly of
adipocytes and functions as a
nutrient (fat) storage site.
Fig 10.2
2
Flat Bone
• A flat bone is
characterized by
being thin and flat,
with an internal
framework of spongy
(trabecular) bone.
The surfaces of flat
bones consist of
compact bone.
MEMBRANES OF BONE
Two membranes are associated with
bone, the
1. outer periosteum and the
2. inner endosteum.
Fig 10.5
Periosteum
• The periosteum is the
outer covering of all
bones except at their
sites of articulations.
• The periosteum functions
to
– (1) provide attachment
sites for tendons and
ligaments,
– (2) house the cells of bone,
the osteoprogenitor cells,
osteoblasts, and
osteoclasts, and
– (3) serve as a site for the
supply of nerves and blood
vessels to the bone.
Layers of the Periosteum
• The periosteum consists of two layers:
• Fibrous Layer
– The outer fibrous layer of the periosteum is a dense
regular connective tissue membrane consisting
mostly of collagen fibers and fibroblasts.
• Cellular Layer
– The inner cellular layer of the periosteum mostly
functions as an osteogenic layer. Its cells are mostly
osteoprogenitor cells, osteoblasts and osteoclasts,
active in bone growth and remodeling.
Fig 10.6
Layers of the Periosteum
Endosteum
• The inner membranous covering associated with
bone is the endosteum.
• The endosteum, a single cellular layer, is found
lining
– (1) the medullary (marrow) cavity,
– (2) the trabeculae, and
– (3) the surfaces of the central canals.
•
Fig 10.7 A cross-section of compact bone (diaphysis) and its associated
periosteum (100x). The fibrous layer of the periosteum is interwoven into the
collagen fibers of a tendon. Collagen fibers called perforating fibers (not shown)
extend from the fibrous periosteum into the matrix of bone. This collagenous
organization makes an extremely strong attachment.
• The cells of the endosteum are osteoprogenitor
cells, osteoblasts, and osteoclasts. The
endosteum is active in bone growth and
remodeling.
3
Endosteum
BONE TISSUE AND
STRUCTURE
Figure 10.8
• A cross-section of compact bone (diaphysis) and its associated
membranes, the periosteum and endosteum. The endosteum is a
single cellular layer found lining the medullary cavity, the trabeculae,
and the central canals. The endosteum consists mostly of
osteoblasts and osteoclasts.
Two types of bone tissue are found in bones:
1. compact and
2. Spongy.
Both types have an extracellular framework, the matrix,
which exhibits considerable hardness and tensile
strength.
Matrix – Inorganic Component
Matrix of Bone Tissue
The extracellular framework of bone,
the matrix, consists of both inorganic
and organic components.
Matrix – Inorganic Component
Figure 10.10
• A photograph of a
bone that was heated
to remove its organic
constituents. The
loss of the strong
collagen fibers
produced a brittle
bone containing
calcium salts.
• The inorganic component of bone tissue
(about two-thirds) is mineral salts, mostly
the calcium salt hydroxyapatite, a crystal
form of calcium phosphate.
– Mineral salts make the matrix hard and
noncompressible.
Matrix – Organic Component
• The organic components of the matrix
(about one-third) are mostly collagenous
fibers produced by bone-forming cells, the
osteoblasts.
– Collagen fibers provide a framework for the
deposition of hydoxyapatite crystals and give
the matrix great tensile strength.
4
Matrix – Organic Component
• Figure 10.9
A photograph of a fibula
(leg bone) which was
demineralized by a weak
acid, then tied into a knot.
The acid dissolved the
mineral salts leaving the
rubbery, flexible collagen
framework of the bone.
Compact Bone
Compact bone is dense and is
found where strength is needed.
Compact Bone
• Compact bone is dense
and is found where
strength is needed. It
makes up the external
surfaces of all bones and
forms the diaphysis
(shaft) of long bones.
• The structural units of
compact bone are
osteons (Haversian
systems).
Fig
10.13
Osteon
An osteon is the
structural unit of compact
bone. Each osteon
consists of concentric
layers of matrix (lamellae)
around a central canal
lined with endosteum.
Each central canal
houses blood vessels and
sometimes a nerve.
Fig 10.12
Osteon
• The osteons are usually parallel, and when shown in
cross section, each system is seen as a region of
concentric layers (lamellae) of matrix surrounding a
central canal.
• Osteocytes, each in a small cavity called a lacuna, are
scattered between the lamellae of each osteon.
• Filling the spaces between adjacent osteons are regions
called interstitial lamellae. Interstitial lamellae are
remnants of older osteons that were destroyed during
bone remodeling.
• Lamellae called circumferential lamellae encircle the
outer and inner regions of the bone.
Lamellae
• A layer of lamellae,
the inner
circumferential
lamellae, encircle the
inner portion of a
bone.
Figure 10.11
5
Perforating and Central Canals
• Perforating canals
– Small canals called
perforating canals
(canals of Volkmann)
extend inward, deep
into the bone. The
perforating canals
bring blood vessels
into the central canals
and to the bone
marrow.
Fig 10.13
• Central Canals
– Each central canal
contains one or more
blood vessels and
occasionally a nerve.
Lab Activity 2
Bone - Ground
• Observe a tissue
preparation of
compact bone labeled
“Bone, ground.”
• Ground bone tissue in
cross-section (43x)
shows many osteons.
Each osteon has a
centrally located
Haversian (central)
canal.
Fig 10.14
Canaliculi
•
Small interconnecting
canals called canaliculi
pierce the matrix.
• The canaliculi
interconnect the lacunae
and the central canals.
• Canaliculi are pathways
for branches of the
osteocytes and their
surrounding interstitial
fluid.
– Through interstitial fluid
and the interconnection of
their branches (gap
junctions), the osteocytes
maintain communication
with the blood vessels
located in the central canal.
Fig 10.12
Lab Activity 2
Bone - Ground
• Each osteon
(Haversian system)
contains a centrally
located central canal.
In the matrix are
concentric rows of
osteocytes. Small
canals, the canaliculi,
contain branches of
the osteocytes.
Figure 10.15
Lab Activity 3
Bone - Demineralized
• Observe a tissue
preparation labeled
“Bone, demineralized.”
• Demineralized bone
tissue (100x) shows
numerous osteocytes
surrounded by collagen
fibers. The central canal
is lined with the
endosteum and contains
blood vessels.
Spongy Bone
Figure 10.16
Spongy (trabecular) bone is located in
the epiphyses of long bones and forms
the internal framework of all other
bones.
6
Spongy bone
• Spongy (trabecular) bone
is located in the
epiphyses of long bones
and forms the internal
framework of all other
bones.
Cells of Bone Tissue
– Spongy bone is made up of
numerous interconnecting
bony plates called
trabeculae. The trabeculae
are organized in an open
framework that provides
Figure 10.17
considerable strength with
reduced weight. Their
open framework provides a
site for red bone marrow.
Types of bone cells are
(1) osteoprogenitor,
(2) osteoblasts,
(3) osteocytes, and
(4) osteoclasts.
Osteoblasts
Osteoprogenitor cells
• Osteoprogenitor cells are bone stem cells that
undergo mitosis. Some of the daughter cells
remain as osteoprogenitor cells, and the
remaining daughter cells differentiate into
osteoblasts.
• Osteoprogenitor cells are found in the cellular
layer of the periosteum and in the endosteum.
• Osteoprogenitor are important in maintaining a
population of osteoblasts for bone growth and
repair.
Osteocytes
• Osteocytes, the mature
maintenance cells of
bone tissue, are the most
abundant of the bone
cells.
• Osteocytes are not
mitotically active and are
located within the bone
matrix within small
cavities called lacunae.
– Small canals, the
canaliculi, extend from and
interconnect the lacunae.
Figure 10.19
Figure 10.18
• Osteoblasts are the building cells of bone matrix and are
located in the cellular layer of the periosteum and in the
endosteum.
• They are actively involved in the production of the organic
portion of the matrix, the osteoid, which consists mostly of
collagenous fibers.
• Additionally, the activity of osteoblasts promotes the
calcification of the osteoid to form bone tissue.
Osteoblasts may become completely surrounded by
matrix and differentiate into osteocytes.
Osteocytes
• Osteocytes (430x) are
found within the matrix of
bone. Cell branches
interconnect the
osteocytes by gap
junctions and along with
the interstitial fluid, which
surrounds the osteocytes
and their branches,
permits exchange of
nutrients, gases, etc.
among the cells.
Figure 10.20
7
Osteoclasts
• Osteoclasts are cells that
breakdown bone matrix.
Osteoclasts are large
multinucleate cells found
in the cellular layer of the
periosteum and in the
endosteum.
• They function in the
breakdown of bone matrix
(osteolysis) mostly to
BONE DEVELOPMENT and
GROWTH
Figure 10.21
– remodel bone and to
– maintain blood calcium ion
levels.
The skeleton begins as an embryonic
framework composed of hyaline
cartilage and fibrous membranes.
Ossification
Ossification
Ossification is the formation and
development of bone tissue.
Ossification
• Calcification is the deposition of calcium
salts and occurs in a wide variety of
tissues including bone. In bone formation,
calcification occurs with the deposit of
hydroxyapatite (mostly calcium phosphate)
in the organic portion of the matrix, the
osteoid, and produces a calcified matrix. In
other tissues, calcification produces
calcified tissues.
• The formation and development of bone
tissue, ossification, eventually form the
mature bones of the skeleton.
• Osteogenesis, the production of bone
forming tissue, begins about six weeks
after fertilization with the differentiation of
stem cells into osteoprogenitor cells.
Two Types of Ossification
The embryonic skeleton undergoes ossification by
two processes:
1. Intramembranous ossification
– Intramembranous ossification occurs within fibrous
membranes and produces flat bones. Flat bones,
such as the bones of the roof of the skull, are
produced by intramembranous ossification.
2. Endochondral ossification
– Endochondral ossification replaces a hyaline
cartilage framework. Most bones of the skeleton are
produced by this method. Long bones, such as the
femur, humerus, tibia, etc., are excellent examples of
endochondral ossification.
8
Two Types of Ossification
Intramembranous Ossification
Figure 10.22
• This specially prepared and stained animal
demonstrates the early stages of bone development.
Intramembranous ossification
occurs within fibrous membranes
and produces flat bones.
– Intramembranous ossification produces flat bones replaces
fibrous membranes and produces flat bones.
– Endochondral ossification replaces the hyaline cartilage
framework that forms most bones of the body.
Intramembranous Ossification
Intramembranous ossification occurs within and replaces
fibrous membranes to form flat bones.
• The process:
1. Mesenchymal cells (undifferentiated cells of mesodermal
origin) within the fibrous membrane differentiate into
osteoprogenitor cells.
2. Osteoprogenitor cells undergo mitosis to maintain a
stem cell population.
3. Some of the daughter cells differentiate into osteoblasts,
which begin the process of ossification.
4. Ossification sites, called centers of ossification, develop
as the osteoblasts secrete the organic portion, the
osteoid, of the bone matrix.
5. The osteoblasts that become completely surrounded
(entrapped) by osteoid promote the process of
calcification and differentiate into osteocytes.
• Osteoprogenitor cells remain in a cellular layer at the
surface of the matrix where they function as stem cells.
Intramembranous Ossification
• Intramembranous
ossification (100x)
continues with the
production of spongy
bone tissue with the
formation of bony plates
called trabeculae.
Trabeculae are produced
from the continued
activity of osteoblasts.
Intramembranous Ossification
• The formation of
ossification centers in
intramembranous
ossification (430x)
occurs with the
entrapment of
osteoblasts in the
osteoid.
Figure 10.23
Intramembranous Ossification
Mature Flat Bone
• Cross section of the
sternum, a flat bone.
• A flat bone is
characterized by
parallel surfaces of
compact bone
separated by a layer
of spongy bone.
Figure 10.25
•Figure 10.24
9
Lab Activity 5
Fetal Skull
Lab Activity 4
Intramembranous Ossification
• Observe a microscope
slide preparation labeled
“Intramembranous
Ossification.”
• Intramembranous
ossification (100x) occurs
within a fibrous
(mesenchyme)
membrane. Plates of
bone, the trabeculae, are
produced by the activity
of osteoblasts.
• Intramembranous ossification
can be observed in the fetal
skull.
• Initially, intramembranous
ossification of the flat bones
(such as the parietals)
produces
Figure 10.27
– (1) a thick region of bone at
the ossification centers,
– (2) areas of large, fibrous
membranes, the fontanels,
between the developing
bones, and
– (3) developing sutures,
regions of fibrous membrane
between the articulating
bones.
Figure 10.26
Figure 10.27
Fontanels
• Anterior (frontal) fontanel
– The anterior fontanel (frontal fontanel) is located midline
between the two segments of the frontal bone and the paired
parietals.
ENDOCHONDRAL
OSSIFICATION
• Posterior (occipital) fontanel
– The posterior (occipital) fontanel is located midline between the
paired parietals and the occipital bone.
• Sphenoid (anterolateral) fontanels
– The sphenoid (anterolateral) fontanels are located anteriorly and
laterally, one on each side of the skull, and formed at the
junction of the parietal, frontal, temporal, and sphenoid bones.
Most bones of the body are formed by
endochondral ossification.
• Mastoid (posterolateral) fontanels
– The mastoid (posterolateral) fontanels are located posteriorly
and laterally, one on each side of the skull, and formed at the
junction of the parietal, occipital, and temporal bones.
Primary Ossification Center and
Bony Diaphysis
Endochondral Ossification
• Endochondral ossification begins with the
replacement of hyaline cartilage of the
embryonic skeleton. Throughout the
process of endochondral ossification,
hyaline cartilage continues to serve as the
site and the model for the formation of
bone tissue.
•
•
•
In early development, endochondral ossification begins in an area
in the diaphysis of the hyaline cartilage model called the primary
ossification center.
Before endochondral ossification begins the perichondrium (a
fibrous membrane that surrounds the cartilage) is converted into
the periosteum and forms a bony collar.
As the bony collar develops, the cartilage cells (chondrocytes) in
the center of the shaft
1. enlarge (hypertrophy), and
2. their surrounding matrix calcifies. The calcification of the cartilage
matrix results in the inability of nutrients to diffuse to the chondrocytes.
3. The chondrocytes die, and their surrounding
4. matrix begins to degenerate and form cavities.
10
Deterioration of Hyaline Cartilage
• A collar of bone forms
around the diaphysis of
the hyaline cartilage
model.
• Cartilage cells undergo
hypertrophy and the
surrounding matrix
calcifies.
• Calcification blocks
nutrient delivery and
cartilage cells deteriorate
producing cavities.
Figure 10.29
Primary Ossification Center
• Blood vessels from the periosteum
of the bony collar invade the
cavities and form capillary
networks.
• Blood brings in osteoprogenitor
cells, which divide to produce
osteoblasts.
• Osteoblasts begin to secrete
bone matrix (osteoid) and
ossification begins with the
formation of bone trabeculae.
• This area, the primary
ossification center, is the first
place where bone matrix is formed
and consists of spongy bone
tissue.
Figure 10.30
Formation of Bony Diaphysis
Lab Activity 6
Early Endochondrial Ossification
• Observe a microscope slide preparation labeled “Early
Endochondral Ossification.”
• Within a short time, a
bony diaphysis is formed
with two distinctive areas
of hyaline cartilage, one
at each end of the
diaphysis, the cartilage
epiphyses.
• Two metaphyses,
regions of transformation
of cartilage into bone,
develop at the proximal
and distal regions
between each epiphysis
and the diaphysis.
Figure 10.31
Typical preparations (15x) used in the study of the primary ossification
center.
Figure 10.30
Lab Activity 6
Early Endochondrial Ossification
• A hyaline cartilage
model will serve as
the site for
endochondral
ossification. In this
specimen, no
ossification has
occurred.
Lab Activity 7
Endochondrial Ossification
• Observe a
microscope slide
preparation labeled
“Endochondral
Ossification.”
• Figure 10.33
– The formation of
bone tissue (43x)
begins at the primary
ossification center.
Figure 10.33
Figure 10.32
11
Lab Activity 7
Endochondrial Ossification
Secondary Ossification Center
•
• The primary ossification
center has developed into
a bony diaphysis (15x).
• Hyaline cartilage remains
at the ends in the regions
called the epiphyses.
• The metaphyses are
regions of tissue
transformation. The
metaphysis is located
between the diaphysis
and each epiphysis.
•
In the center of the hyaline
cartilage epiphyses, sites
called secondary
ossification centers begin to
develop.
A secondary ossification
center is formed when
1. blood vessels from the
periosteum bud into the
hyaline cartilage of the
epiphyses.
2. Osteoprogenitor cells and
osteoblasts arrive.
3. The deposition of osteoid by
osteoblasts activity begins the
formation of trabeculae and
produce a central region of
spongy bone.
Figure 10.35
Figure 10.34
Secondary Ossification Center
• At the secondary
ossification centers, blood
vessels from the
periosteum invade the
cavities in the hyaline
cartilage and form
capillary networks.
• Osteoclasts and
osteoblasts arrive and
begin to modify the area
into spongy bone.
Articular Cartilage and Epiphyseal Plate
At each epiphysis, the
spongy bone continues to
enlarge until two
distinctive areas of
hyaline cartilage remain.
• Articular cartilage
– The permanent outer
cartilage area is the
articular cartilage
• Epiphyseal Plate
– The inner cartilage area is
a disc-like plate, the
epiphyseal plate.
Figure 10.36
Lab Activity 8
Secondary Ossification Center
• Observe a
microscope slide
preparation labeled
“Secondary
Ossification Center.”
• In Fig. 10.38 a
secondary ossification
center (20x) is shown
in the epiphysis.
Figure 10.38
Figure 10.37
Lab Activity 8
Secondary Ossification Center
Figure 10.39
• A secondary ossification center (100x) is shown in the
epiphysis. The replacement of the epiphyseal hyaline
cartilage leaves two areas of hyaline cartilage, an outer
articular cartilage and an inner epiphyseal cartilage plate.
12
Growth of the Diaphysis
• Longitudinal growth
Growth of the Diaphysis
Bone growth occurs in two areas and produces two
types of growth:
(1) growth in length, or longitudinal growth, and
(2) growth in diameter, or appositional growth.
– Longitudinal growth, which results in an
increase in length, occurs at the metaphysis,
or the epiphyseal plate (observed in children
and adolescents).
• Appositional growth
– Appositional growth, which results in an
increase in diameter, occurs at the cellular
(osteogenic) layer of the periosteum.
Lab Activity 9
Growth of the Diaphysis
Longitudinal Growth
Longitudinal growth, which results in an
increase in length, occurs at the
metaphysis, or the epiphyseal plate
(observed in children and adolescents).
Lab Activity 9
Growth of the Diaphysis
• In the near central area of
the epiphysis, the hyaline
cartilage is described as
the area of proliferation;
the hyaline cartilage
mitotically divides.
• Older cartilage cells
(toward the diaphysis)
undergo hypertrophy
(enlargement) and the
matrix of the cartilage
calcifies.
Figure 10.40
• Observe a slide
preparation labeled
“Endochondral
Ossification.”
• Figure 10.40 shows
longitudinal growth of
the diaphysis (100x).
– Longitudinal growth
occurs at the region of
transformation, the
metaphysis.
Figure 10.40
Metaphysis
The metaphysis is the
region where bone
replaces hyaline cartilage
and results in an
increased length of the
diaphysis, longitudinal
growth.
• At the epiphyseal region
of the metaphysis,
– (1) the cartilage cells die,
– (2) most of the matrix
degenerates, and
– (3) cavities are formed.
Figure 10.40
13
Metaphysis
Metaphysis / Early Epiphyseal Plate
• At the diaphysis surface
of the metaphysis,
– (1) osteoblasts secrete
bone matrix on remaining
cartilage spicules and
– (2) a network of bony
trabeculae forms the
diaphysis.
• In this manner, the bone
continues to increase in
length by forming bony
trabeculae as the
cartilage is removed.
Figure 10.41
Figure 10.40
Epiphyseal Line
• The epiphyseal plates
are completely
removed (longitudinal
growth is terminated),
and a line of bone,
called the epiphyseal
line, marks their prior
location.
• A secondary ossification center (100x) is shown in the
epiphysis. The replacement of the epiphyseal hyaline
cartilage leaves two areas of hyaline cartilage, an outer
articular cartilage and an inner epiphyseal cartilage plate.
Lab Activity 10
Epiphyseal Plates
Observe an x-ray of a long
bone from an adolescent
for the identification of
epiphyseal plates.
• Epiphyseal plates are
shown in this x-ray (Fig.
10.43) of an adolescent.
Individual bones have
specific times when their
epiphyseal plates are
replaced by bone tissue.
Figure 10.42
Figure 10.43
Lab Activity 11
Epiphyseal Lines
• Under the influence of hormones, especially the
sex hormones produced in increasing amounts
at puberty, the bony tissue at the epiphyseal
plates begins rapid production. The increased
rate of bone growth eventually replaces the
hyaline cartilage epiphyseal plates.
• Marking the prior location of an epiphyseal plate
is a unique area of bone tissue, the epiphyseal
line.
Lab Activity 11
Epiphyseal Lines
• The distal end of the
femur in frontal
section shows an
epiphyseal line. The
epiphyseal line is
formed by bone
production at the site
where the epiphyseal
plate was located.
Figure 10.44
14
Appositional Growth of the
Diaphysis
Appositional Growth of the
Diaphysis
Appositional growth produces an
increase in bone diameter.
• Growth that increases the diameter, or
thickness, of the bone occurs at the inner
cellular (osteogenic) layer of the periosteum.
• The bone diameter of the bone is increased by
osteoblasts secreting bone matrix onto existing
bone.
• Osteoblast activity encircles periosteal blood
vessels with matrix and forms layers of matrix
(lamellae) to produce osteons (Haversian
systems).
Lab Activity 12
Appositional Growth
Appositional
Growth
• Sequence of
appositional growth at
the cellular
(osteogenic) layer of
the periosteum.
Figure 10.46
Figure 10.45
Lab Activity 12
Appositional Growth
• Observe a microscope slide preparation labeled
“Decalcified Bone; cross section.”
• A cross section of the diaphysis of the developing
femur (Fig. 10.46, @ 20x) shows the periosteum,
compact bone of the diaphysis, medullary cavity, and
bone marrow. The thin inner layer, the endosteum, is
not seen at this magnification.
Lab Activity 12
Appositional Growth - Endosteum
Figure 10.47
• A cross section of the diaphysis (100x) of the femur
showing the detail of its wall. The diaphysis grows
thicker (appositional growth) by the formation of new
osteons (Haversian systems) under the fibrous layer of
the periosteum.
Figure 10.48
• A cross section of the diaphysis (100x) of the femur showing the
detail of its wall. The diaphysis grows thicker (appositional growth)
by the formation of new osteons (Haversian systems) under the
periosteum. Osteoclasts of the endosteum erode the inner wall and
form the medullary (marrow) cavity.
15
Nutrients for Bone Growth,
Development, and Remodeling
BONE DYNAMICS
(growth, remodeling, and
maintenance)
Bone remodeling is a life long process that is
necessary for the body’s skeleton to
accommodate for changes mostly due to
growth, lifestyles, and aging.
Nutrients for Bone Growth,
Development, and Remodeling
• Vitamins
– Vitamin C
• Vitamin C is especially important in the synthesis of collagen
fibers.
– Vitamin D
• Vitamin D, of dietary origin or synthesized in the skin, is
necessary for the intestinal absorption of calcium and
phosphate from the intestine.
• The kidneys convert vitamin D3, cholecalficerol, to calcitriol.
Calcitriol targets the intestines and promotes the absorption
of calcium and phosphate.
Exercise
(mechanical stress)
• Protein
– Adequate dietary protein is required for the
construction of the organic matrix, the osteoid.
• Inorganic Matrix
– The inorganic matrix requires two major
components, the salts of calcium and
phosphate, both of which are also of dietary
origin.
Growth of Bone
• The growth of bones begins at about six weeks after
fertilization.
• The two processes, intramembranous and endochondral
ossification begin to produce bone tissue.
• As the bone tissues are produced, they are continually
remodeled as to shape, internal design, and mineral
content. The ages at which bones stop growing vary with
the bones. However, around age 25 all of the bones
have reached maturity.
• Even though the bones have reached their mature size,
bone remodeling continues as surface marking and their
internal framework continues to be modified throughout
life.
Exercise
(mechanical stress)
• A major force in promoting bone
remodeling is exercise.
• Exercise results in mechanical stresses
that generate small electrical currents
within the bone. These small electrical
currents stimulate osteoblasts.
Figure 10.49
•
The plates of spongy bone, the trabeculae, are position to supply
the greatest structural strength. Changes if life style, such as weight
lifting, change the structure of the trabeculae to accommodate for
increased mechanical stress. The femur, shown in this figure, is
continually remodeled to fit one’s lifestyle.
16
Hormonal Regulation
Hormonal Regulation
Two hormones involved with tissue growth and metabolism
of the body’s cells are growth hormone and thyroxine.
• Growth Hormone
• Additionally, two hormones that directly affect
bone are calcitonin and parathyroid hormone.
• The hormones, parathyroid hormone and
calcitonin, are involved in the maintenance of
blood calcium levels; thus, directly influencing
the homeostasis of the skeleton. Bone may be
demineralized when the body needs calcium or
mineralized when calcium supplies are plentiful.
– Growth hormone, also called somatotropic hormone, is produced
by the anterior pituitary gland. Growth hormone influences
protein, carbohydrate, and lipid synthesis. Growth hormone
plays a continual role in cartilage and bone growth, especially in
children.
• Thyroxine
– Thyroxine is a hormone produced by the thyroid gland that
regulates cell metabolism, especially involving proteins and
carbohydrates.
• The coordinated effects of both hormones are necessary
to produce normal skeletal growth and maturation.
Lab Activity 13
Hormonal Regulation
Calcitonin – Parafollicular Cells
• The parafollicular cells of the thyroid produce calcitonin.
• Calcitonin is released when blood ionic calcium levels
increase.
• The primary function of calcitonin is to decrease the
blood’s level of ionic calcium when blood ionic calcium
levels are high.
• Calcitonin targets:
• Observe a slide
preparation labeled
“Thyroid and
Parathyroid glands,”
or “Thyroid gland,”
and “Parathyroid
gland.”
Figure 10.50
– (1) osteoblasts which promote the deposition of calcium into
bone matrix, and the
– (2) kidneys to increase excretion of calcium in the urine.
Intestinal absorption of calcium is low due to a low level of
parathyroid hormone.
Parathyroid Hormone
Calcitonin
• (PTH) is released when blood ionic calcium
levels decline.
• Its primary function is to increase the blood’s
level of ionic calcium.
• Parathyroid hormone targets:
• The function of the
thyroid hormone,
calcitonin, in
regulation of blood
ionic calcium.
– (1) osteoclasts to increase the destruction of bone
matrix,
– (2) the intestines to increase absorption of calcium
and phosphate ions,
– (3) the kidneys to increase reabsorption of calcium
and to increase the production of calcitriol to
additionally promote intestinal absorption of calcium.
Figure 10.51
17
Lab Activity 14 Bone Remodeling
Parathyroid Hormone
• The function of
parathyroid
hormone in
regulation of blood
ionic calcium.
Figure
10.53
• Observe a slide preparation labeled “Ground Bone;
cross section.”
Bone remodeling involves the processes of
– (1) reabsorption and
– (2) deposit.
Figure 10.52
• Bone remodeling occurs at the cellular layer of the
periosteum and at the endosteum.
Lab Activity 14 Bone Remodeling
• Bone remodeling
produced the repair of
the fractured leg
bones, the tibia and
fibula.
Figure 10.54
18