Fluoroscopic Swallowing Study in Elderly Patients Admitted to a
advertisement

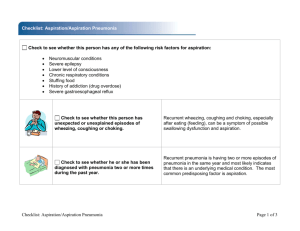
Original Article DOI:10.4235/jkgs.2009.13.4.195 Fluoroscopic Swallowing Study in Elderly Patients Admitted to a Geriatric Hospital and a Long-Term Care Facility Sang Jun Kim, MD, Tai Ryoon Han, MD Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul, Korea Background: No study has been done to detect the aspiration using the videofluoroscopic swallowing study in the elderly patients. Elderly patients admitted to hospitals or long-term care facilities may intake the food orally without any evaluation of swallowing function and may be exposed to aspiration risk, which can be eliminated by some diet modification based on the fluoroscopic findings. Methods: Sixty-three elderly patients who had an oral-feeding status were recruited in this study. They swallowed diverse food textures twice in the following order; liquid, Yoplait yogurt, pudding, soft-bland diet, and a regular diet. Swallowing parameters were checked as subglottic aspiration, supraglottic penetration, delayed pharyngeal reflex, and vallecular and pyriform sinus residues. Results: Only 2 patients showed both aspiration signs and the subglottic aspiration in the fluoroscopic study. Six patients showed the subglottic aspiration in the fluoroscopic study without any clinical sign. Seven patients who complained of aspiration signs did not show the subglottic aspiration, but all of them presented the supraglottic penetration. Multivariate logistic regression analysis showed that no covariate was correlated with the subglottic aspiration whereas delayed pharyngeal reflex during liquid (p<0.001) or Yoplait (p=0.010) swallowing were correlated with aspiration plus penetration. Conclusion: This study demonstrates that a fluoroscopic swallowing study is important for the dysphagia diagnosis in elderly patients because of no significant correlation between the aspiration signs assessed clinically and the subglottic aspiration detected by the fluoroscopic swallowing study. Diet modifications, such as, liquid thickening will be necessary when patients demonstrate the evidence of subglottic aspiration during swallowing. Key Words: Deglutition, Fluoroscopy, Geriatrics piecemeal deglutition, premature loss of liquid, oral and phar- INTRODUCTION yngeal residues, and laryngeal penetration are significantly Dysphagia is a common problem in geriatric medicine. pose the elderly to develop dysphagia, especially in the phar- Swallowing in the elderly is characterized by slow hyoid move- yngeal phase, a condition in which a young patient will not greater in dentate elderly persons3). These characteristics dis- 1) ment, delayed pharyngeal reflex , and vallecular and pyriform 2) sinus residues caused by muscular weakness . Frequencies of show dysphagia. Common diseases among the elderly, such as small vessel, Alzheimer’s and Parkinson’s disease, also in- ▸Received: Jul 16, 2009 ▸Revised: Set 15, 2009 ▸Accepted: Set 25, 2009 Address for correspondence: Tai Ryoon Han, MD, PhD Department of Rehabilitation Medicine, Seoul National University College of Medicine, 28 Yeongun-dong, Jongro-gu, Seoul 110-744, Korea Tel: +82-2-2072-1358, Fax: +82-2-743-7473, E-mail: guitar1@snu.ac.kr *This study was supported by a research fund from the Korean Geriatric Society in 2005. J Korean Geriatr Soc 13(4) Dec 2009 195 Sang Jun Kim: Fluoroscopic Swallowing Study in Elderly Patients 4) 12) crease the risk of dysphagia . Moreover, the decreased de- amount . Thus, increasing viscosity is not always a safe op- fense systems (e.g., decreased immunity and reduced pulmo- tion in dysphagic patients. 5) nary clearance), increase the risk of aspiration pneumonia . With age, elderly patients show decreased swallowing ca- Therefore, pharyngeal dysphagia is an important health issue pacity, delayed triggering of the pharyngeal swallow, and sig- in the elderly. nificant vallecular and pyriform sinus residue2). Thus, it is im6) In a chart review, Lin et al. found that the prevalence of portant to know the effects of swallowing parameters, includ- impaired swallowing was 31.9% among non tube-fed subjects ing pharyngeal reflex delay and residue amount, on the risk of in nursing and intermediate care facilities in Taiwan. Kawa- aspiration in elderly patients by using a fluoroscopic study. 7) shima et al. found a 13.8% prevalence rate of dysphagia by Elderly patients admitted to hospitals or long-term care fa- means of a questionnaire to screen community-dwelling eld- cilities have diverse diseases, and may show dysphagia from erly in the northern region of Honshu Island, Japan. Roy et underlying diseases or an unknown cause. Oral feeds may be 8) al. showed the prevalence of swallowing disorder to be 33% given without evaluating the swallowing function, exposing of the 117 seniors living independently in Utah and Kentucky them to the risk of aspiration, which can be eliminated by diet via an interview questionnaire. However, none of these au- modification based on fluoroscopic findings. thors performed a videofluoroscopic swallowing study, consid- Therefore, the aim of this study was to compare subglottic ered the gold standard for diagnosing dysphagia. This is im- aspiration detected by fluoroscopy with the aspiration signs portant because silent aspiration, which is difficult to detect by seen clinically in elderly patients being fed orally at a geriatric 9) questionnaire, occurs in up to 30% of dysphagic patients . hospital and a long‐term care facility and to find the swallow- Moreover, this topic will be of increasing concern as the num- ing parameters that correlate with aspiration and penetration. ber of geriatric hospitals and long‐term care facilities increase MATERIALS AND METHODS in many countries. Methods for managing pharyngeal dysphagia are diverse. Changing food consistency and texture (e.g., by adding food 1. Subjects thickeners) is one example. It is generally believed that food viscosity is inversely proportional to the likelihood of laryn- From the inpatients at a local geriatric hospital and resi- geal penetration or aspiration in dysphagic patients because the dents at a long-term care facility, 63 subjects were recruited in fast movement of food with low viscosity induces penetration February 2005 in Gyeonggi‐do, Korea. Selected subjects had or aspiration, whereas the slow movement with high viscosity “oral-feed” statuses, and were competent enough to understand will not do so in patients with delayed pharyngeal reflex. the purpose of this study and to agree to participate. All sub- 10) Lending support to this hypothesis is an earlier study , which jects provided informed consent for this study. The subjects revealed that increasing bolus viscosity greatly improves swal- comprised 43 women and 20 men with an average age of 76.0 lowing function in patients with neurological problems. Howe- ±7.0 years, and had various diagnoses (stroke-19; dementia-7; 11) showed that there was more pharyngeal Parkinsonism-5; low back pain-4; arthritis-3; hip joint frac- retention with ultra-thick liquids, like pudding, than with apple ture-3; others-6; no identifiable disease-16). Seven subjects juice or apricot nectar, suggesting that high viscosity increased with dementia had their orientation and judgment evaluated pharyngeal retention. Postdeglutitive overflow aspiration is through a mental status examination. All subjects, except those found frequently in patients with pharyngeal retention, and the with no identifiable disease, experienced disease onset at least risk of aspiration increases markedly with increasing residual a year prior to the beginning of this study. Time of onset was ver, another study 196 J Korean Geriatr Soc 13(4) Dec 2009 Sang Jun Kim: Fluoroscopic Swallowing Study in Elderly Patients not known in 25 patients. At the beginning of this study, 50 subjects were on a regular diet while the others were on a soft-bland diet because of dental problems. 2. Swallowing evaluation Aspiration signs were delineated as wet voice and reflex cough during meal time. Aspiration was deemed to be present clinically when aspiration signs were present more than once per meal time. 1) Fluoroscopic swallowing study One rehabilitation doctor (KSJ), one fluoroscopist (PKW), and one nutritionist (HMH) performed the fluoroscopic swallowing studies on the 63 participants. The results were immediately recorded on paper as they could not be recorded as video files for technical reasons. Subjects swallowed foods with diverse viscosities twice in the following order: 5 mL of water by syringe, then a spoonful of Yoplait yogurt, pudding, soft‐bland diet, and a regular diet. All foods were mixed with ® a 35% diluted barium solution (Solotop ; Taijoon, Seoul, Korea) without significant change to viscosity. In this study, Yoplait corresponds to the fluid-type yogurt, soft‐bland diet to the thin rice gruel, and a regular diet to the thick rice gruel of the previous study13). 2) Swallowing parameters Fig. 1. Delayed pharyngeal reflexes were graded as none, mild, moderate, and severe. Below figures were captured at time of hyoid elevation (beginning of pharyngeal stage). Starting at the left upper corner (clockwise direction), figures show normal and mildly, moderately, and severely delayed pharyngeal reflex. curred when the bolus passed the laryngeal vestibule along the groove to the pyriform sinus), or severe (hyoid elevation occurred when more than half of the pyriform sinus was filled with the bolus) (Fig. 1). This classification is similar to that used 12) in an earlier study . Residue amounts were graded as none, scant (the vallecula or pyriform sinus was only coated with residue), little (the height of the residue was less than half the total height of the vallecula or pyriform sinus), or much (the height of residue was more than half the total height of the vallecula or pyriform sinus). Subglottic aspiration, supraglottic penetration, delayed phar- In recording the grades, all three investigators were re- yngeal reflex, and vallecular and pyriform sinus residues were quired to agree on the readings. If an investigator disagreed, assessed using fluoroscopy with patients in the lateral position. swallowing trials were repeated (with subject approval) until Subglottic aspiration and supraglottic penetration were differ- agreement was reached. entiated based on whether the bolus entered the true vocal fold. Delayed pharyngeal reflex was graded as none (hyoid el- 3. Statistics evation occurred before the head of the bolus passed the mandibular angle), mild (hyoid elevation occurred after the head of Fisher’s exact test was done to compare the coincidence of the bolus passed the mandibular angle but most of the bolus the subglottic aspiration detected by fluoroscopy to the aspira- remained in the vallecular area), moderate (hyoid elevation oc- tion signs found clinically. Multivariate logistic regression J Korean Geriatr Soc 13(4) Dec 2009 197 Sang Jun Kim: Fluoroscopic Swallowing Study in Elderly Patients analysis was performed to determine the aspiration risk ac- soft-bland diet, and the regular diet. Three of 48 patients (6.3 cording to swallowing parameters (residues and pharyngeal re- %) showed supraglottic penetration during Yoplait swallo- flex delay). All alpha‐errors were determined to be 0.05. The wing. Of 59 patients, two (3.4%) and one (1.7%) showed sura- SPSS program version 12.0 program (SPSS Inc., Chicago, IL, glottic penetration of the soft-bland and regular diets, respe- USA) was used to perform the statistical analysis. ctively. Only two patients showed both aspiration signs and sub- RESULTS glottic aspiration in the fluoroscopic study. Six patients showed subglottic aspiration in the fluoroscopic study without any Nine patients (14.3%) showed clinical signs of aspiration clinical sign. Seven patients who complained of aspiration but did not have aspiration pneumonia since admission. signs did not show subglottic aspiration, but they all presented All 63 patients successfully swallowed the liquid, but 15 with supraglottic penetration (Table 1). Fisher’s exact test did patients refused to swallow the Yoplait, two refused the pud- not reveal a significant correlation between the signs of aspira- ding, and four the soft-bland and regular diet. Fluoroscopic tion and subglottic aspiration (odds ratio [OR], 2.286; 95% findings revealed that 31 patients showed neither subglottic as- confidence interval [CI], [0.383, 13.635]). piration nor supraglottic penetration, but eight patients (12.7%) Vallecular and pyriform sinus residues for foods are pre- showed subglottic aspiration, and 24 patients (38.1%) supra- sented in Table 2. Most patients showed little or no pyriform glottic penetration during liquid swallowing. No patient sho- sinus residue after swallowing liquid, with the exception of wed subglottic aspiration while swallowing Yoplait, pudding, one patient who showed a substantial amount of residue. Much vallecular residue was found in some patients only during swallowing of the regular diet. However, little pyriform si- Table 1. Cross table of the aspiration signs detected clinically and the subglottic aspiration by fluoroscopic swallowing study in 63 elderly subjects Aspiration sign nus residue was observed during the swallowing of all foods. Pharyngeal reflex delays for the various foods are shown in No aspiration sign Table 3. Delayed pharyngeal reflex occurred in some patients during the swallowing of liquid, soft-bland diet, and regular Aspiration by fluoroscopy 2 6 diet. Multivariate logistic regression analysis with backward No aspiration by fluoroscopy 7 48 elimination approach showed that no covariate correlated with Values are numbers of patients. subglottic aspiration whereas delayed pharyngeal reflex during Table 2. Vallecular and pyriform sinus residues after swallowing of diverse food textures in 63 elderly subjects Vallecular residue Pyriform sinus residue L Y P S N L Y P S N None 44 41 38 34 20 57 47 57 56 49 Scant 14 4 11 14 10 4 0 3 3 5 Few 5 3 11 11 15 1 1 1 0 5 Much 0 0 1 0 14 1 0 0 0 0 N/A 0 15 2 4 4 0 15 2 4 4 Values are number of patients. L, liquid; Y, yoplait; P, pudding; S, soft‐bland diet; N, normal regular diet, N/A, not applicable. 198 J Korean Geriatr Soc 13(4) Dec 2009 Sang Jun Kim: Fluoroscopic Swallowing Study in Elderly Patients Table 3. Degree of pharyngeal reflex delay during swallowing of diverse food textures in 63 elderly subjects signs assessed clinically and the subglottic aspiration detected by the fluoroscopic swallowing study. Vallecular residues were significantly greater during swallowing of the regular diet, Delayed pharyngeal reflex L Y P S N whereas the pyriform sinus residues were not. Subglottic aspi- None 23 38 43 27 20 ration was not correlated with residues and delayed pharyngeal Mild 13 10 13 20 17 reflex. However, delayed pharyngeal reflex during liquid or Moderate 21 0 4 12 16 Yoplait swallowing correlated with aspiration plus penetration. Severe 6 0 1 0 6 The prevalence of aspiration in this study was 12.7% on N/A 0 15 2 4 4 the fluoroscopic swallowing study, in line with the findings of Values are number of patients. L, liquid; Y, yoplait; P, pudding; S, soft-bland diet; N, normal regular diet, N/A, not applicable 7) Kawashima et al. ; however, it was lower than that of Lin et al.’s study6), although the number of patients was too small to represent the prevalence in elderly patients. From this study, it was expected that the prevalence rate would be similar to Lin liquid (p<0.001) or Yoplait (p=0.010) swallowing correlated with et al.’s study6) because subjects admitted to a hospital or a fa- aspiration plus penetration. cility were enrolled. In view of the findings of a previous When the subjects were divided into stroke (n=19) and non- study 14) which stated that deep laryngeal penetration often pro- stroke (n=44) groups, four patients (21.1%) in the stroke group gressed to aspiration, it is possible that patients showing su- showed supraglottic penetration, and four (21.1%) experienced praglottic penetration without subglottic aspiration might also subglottic aspiration. The non-stroke group revealed supra- be at risk of aspiration. If penetration cases were included, the glottic penetration in 20 subjects (45.5%) and subglottic aspi- prevalence rate of aspiration plus penetration would increase ration in four patients (9.1%). The incidences of aspiration in to 50.8%. the two groups were not significantly different by Fisher’s ex- The six patients who showed subglottic aspiration on the act test (OR, 0.375; 95% CI, [0.083, 1.693]). When subjects fluoroscopic study without any aspiration sign (silent aspira- were dichotomized by diseases that might cause dysphagia tion) emphasize the importance of this study. Seven patients (stroke, dementia, and Parkinsonism) and those unlikely to do who showed supraglottic penetration with clinical aspiration so, the incidences of aspiration were not significantly different signs suggest that supraglottic penetration also must not be between the two groups by Fisher’s exact test (OR, 0.538; 95 overlooked in the detection of aspiration as only few swallow- % CI, [0.117, 2.475]). ing trials are performed in most fluoroscopic swallowing studies. However, Daggett et al.15) found that 16.8% of swal- DISCUSSION lows showed penetration in normal subjects aged 50 and above in a videofluoroscopic swallowing study. Therefore, the diag- This is the first study on the swallowing characteristics of nosis of aspiration must be considered in a comprehensive elderly patients admitted to a geriatric hospital or a long‐term manner. It will be necessary to classify penetration cases accor- care facility using fluoroscopic swallowing study. Subglottic ding to several steps using the penetration‐aspiration scale , aspiration was observed in 12.7% of patients and supraglottic which was not done in this study. 16) penetration in 38.1% in the fluoroscopic swallowing study The prevalence of aspiration between stroke and non‐stroke whereas 14.3% of patients showed aspiration signs clinically. groups did not show any difference. This suggests that aspira- No significant correlation was found between the aspiration tion in this study originated from multiple factors including J Korean Geriatr Soc 13(4) Dec 2009 199 Sang Jun Kim: Fluoroscopic Swallowing Study in Elderly Patients poor general condition and the aging process, rather than the to show the differences between foods. disease itself. Four patients from the non‐stroke group with as- The pyriform sinus residue amounts for pudding, soft-bland piration had additional diagnoses of herniated intervertebral diet, and regular diet were found to be unrelated to aspiration disc, asthma, dementia, and poor oral intake without a disease or penetration, unlike the initial hypothesis that high vis- cause. Their average age was 76.3 ± 5.3 years. This did not cosities are likely to increase aspiration risk as a result of differ significantly from that of the other patients (p=0.921). pharyngeal retention. This result differs from that of Eisen- They all showed a worse than moderately delayed pharyngeal huber et al.’s study , which may be because Eisenhuber et reflex. They had no definite abnormal signs suggestive of al.’s study12) recruited more patients with moderate to severe stroke or other diseases that could cause dysphagia. However, pharyngeal retention. In the present study, the pyriform sinus none of them could ambulate without assist and tended to be residue was insufficient (residues were scant or few, not much) bed‐bound. Deconditioning due to decreased activity might lead to evoke overflow aspiration with all food textures. 12) to dysphagia. Although cervical imaging was not performed, The present study has a few limitations, one of which is cervical osteophytes related to old age might be a cause of that images could not be recorded (the fluoroscopic device did 17) dysphagia in this study . not have an image storing function). Thus, this study could The results of this study showed that delayed pharyngeal only use semiquantitative data, rather than quantitative data, reflex during liquid or Yoplait swallowing had an effect on as- such as pharyngeal delay time. Further quantitative studies piration plus penetration. This finding is somewhat similar to should be done to overcome this shortcoming. Intra- and inter- 18) which showed that delayed triggering of ater reliability was not evaluated. However, all the swallowing pharyngeal swallowing is related to penetration/aspiration, with parameters were easily divided into four grades and there were an odds ratio of 2.98 during the drinking of 5 mL of water in no contradictions between the three investigators. This study is 103 stroke patients using polychotomous logistic linear regre- also limited because the precise characteristics of the patients ssion. When the dependent variable was restricted to subglottic were not known, for example, onset and lesion location (in aspiration, no covariates, including delayed pharyngeal reflex, cases of stroke). Nevertheless, the authors believe that the were correlated with aspiration. This result coincides with findings in this study can be useful to accurately detect aspira- Han et al.’s study 19) Martin-Harris’ study , which concluded that a delay in phar- tion through fluoroscopic study. yngeal swallowing per se cannot be assumed to indicate dis- Having completed this study, the diets of patients who ordered swallowing in the absence of coexisting impairments showed subglottic aspiration were changed to the better-tol- 20) observed that erated thickened liquids, and their aspiration symptoms and pharyngeal swallowing is delayed in healthy elderly subjects, fluoroscopic findings improved. An attempt was made to fol- and that elderly subjects frequently require multiple swallows low up on these patients one year later by telephone or direct to effectively clear a bolus from the pharynx. This coincides contact. Although only 14 of the 63 patients (22.2%) respon- with our results although they did not comment on vallecular ded, responders, including patients who underwent diet mod- of swallowing physiology. Schindler et al. 21) revealed that the bo- ification, had no symptoms of aspiration or events of aspira- lus type had a significant effect on residue scores, which dif- tion pneumonia. However, to confirm this, another study is re- fered from our results. This mismatch might be due to the dif- quired to evaluate improvement in general condition and re- ferences in residue scoring and the bolus amount. The Kelly duced rates of aspiration pneumonia after diet modification. or pyriform sinus residues. Kelly et al. 21) used 10 mL of foods, while we used 5 mL of liquid Though this study has several limitations, it demonstrates and one spoonful of other textures, which might be too small that a fluoroscopic swallowing study is important for diagnos- study 200 J Korean Geriatr Soc 13(4) Dec 2009 Sang Jun Kim: Fluoroscopic Swallowing Study in Elderly Patients ing dysphagia. Moreover, it reveals that diet modification, such 5. Kikawada M, Iwamoto T, Takasaki M. Aspiration and in- as thickening liquids, is necessary when patients show evidence fection in the elderly: epidemiology, diagnosis and mana- of subglottic aspiration during swallowing. Additional studies gement. Drugs Aging 2005;22:115-30. are required to confirm the clinical usefulness of diet modification. 6. Lin LC, Wu SC, Chen HS, Wang TG, Chen MY. Prevalence of impaired swallowing in institutionalized older people in Taiwan. J Am Geriatr Soc 2002;50:1118-23. CONCLUSION 7. Kawashima K, Motohashi Y, Fujishima I. Prevalence of dysphagia among community-dwelling elderly individuals This study demonstrates that a fluoroscopic swallowing study is important for diagnosing dysphagia in elderly patients be- as estimated using a questionnaire for dysphagia screening. Dysphagia 2004;19:266-71. cause of no significant correlation between the aspiration signs 8. Roy N, Stemple J, Merrill RM, Thomas L. Dysphagia in assessed clinically and the subglottic aspiration detected by a the elderly: preliminary evidence of prevalence, risk fac- fluoroscopic swallowing study. Diet modification, such as thi- tors, and socioemotional effects. Ann Otol Rhinol Laryn- ckening liquids, is necessary when patients demonstrate evi- gol 2007;116:858-65. dence of subglottic aspiration during swallowing. 9. Ramsey D, Smithard D, Kalra L. Silent aspiration: what do we know? Dysphagia 2005;20:218-25. ACKNOWLEDGEMENTS 10. Clavé P, de Kraa M, Arreola V, Girvent M, Farré R, Palomera E, et al. The effect of bolus viscosity on swallowing I especially thank Park Kun Woong for performing the fluoroscopic swallowing studies and interpreting their results, Hy- function in neurogenic dysphagia. Aliment Pharmacol Ther 2006;24:1385-94. eong Mi Hyeong for preparing the textured foods and interpre- 11. Kuhlemeier KV, Palmer JB, Rosenberg D. Effect of liquid ting the results, and Janette Villagonzalo (Customer Service bolus consistency and delivery method on aspiration and Manager of Professional Editing Services) for helping with the pharyngeal retention in dysphagia patients. Dysphagia 2001; English writing. 16:119-22. 12. Eisenhuber E, Schima W, Schober E, Pokieser P, Stadler REFERENCES A, Scharitzer M, et al. Videofluoroscopic assessment of patients with dysphagia: pharyngeal retention is a predictive 1. Robbins J, Hamilton JW, Lof GL, Kempster GB. Oro- factor for aspiration. AJR Am J Roentgenol 2002;178:393-8. pharyngeal swallowing in normal adults of different ages. 13. Paik NJ, Han TR, Park JW, Lee EK, Park MS, Hwang Gastroenterology 1992;103:823-9. 2. Logemann JA. Evaluation and treatment of swallowing disorders. Austin: PRO-ED; 1998. 3. Yoshikawa M, Yoshida M, Nagasaki T, Tanimoto K, IK. Categorization of dysphagia diets with the line spread test. Arch Phys Med Rehabil 2004;85:857-61. 14. Friedman B, Frazier JB. Deep laryngeal penetration as a predictor of aspiration. Dysphagia 2000;15:153-8. Tsuga K, Akagawa Y, et al. Aspects of swallowing in 15. Daggett A, Logemann J, Rademaker A, Pauloski B. Laryn- healthy dentate elderly persons older than 80 years. J Ge- geal penetration during deglutition in normal subjects of rontol A Biol Sci Med Sci 2005;60:506-9. various ages. Dysphagia 2006;21:270-4. 4. Rumeau P, Vellas B. Dysphagia, a geriatric point of view. Rev Laryngol Oto Rinol (Bord) 2003;124:331-3. 16. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration‐aspiration scale. Dysphagia 1996;11:93-8. J Korean Geriatr Soc 13(4) Dec 2009 201 Sang Jun Kim: Fluoroscopic Swallowing Study in Elderly Patients 17. Ladenheim SE, Marlowe FI. Dysphagia secondary to cervical osteophytes. Am J Otolaryngol 1999;20:184-9. 18. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil 2001; 82:677-82. 19. Martin‐Harris B, Brodsky MB, Michel Y, Lee FS, Walters B. Delayed initiation of the pharyngeal swallow: normal 202 J Korean Geriatr Soc 13(4) Dec 2009 variability in adult swallows. J Speech Lang Hear Res 2007; 50:585-94. 20. Schindler JS, Kelly JH. Swallowing disorders in the elderly. Laryngoscope 2002;112:589-602. 21. Kelly AM, Macfarlane K, Ghufoor K, Drinnan MJ, Lew‐ Gor S. Pharyngeal residue across the lifespan: a first look at what’s normal. Clin Otolaryngol 2008;33:348-51.