Blood pressure regulation in neurally intact human vs. acutely
advertisement

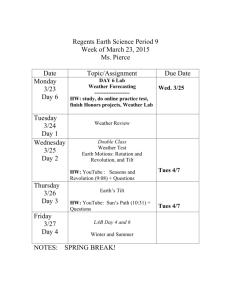
Am J Physiol Regul Integr Comp Physiol 292: R1146 –R1157, 2007. First published November 2, 2006; doi:10.1152/ajpregu.00225.2006. Blood pressure regulation in neurally intact human vs. acutely injured paraplegic and tetraplegic patients during passive tilt Sevda C. Aslan,1 David C. Randall,1,3 Kevin D. Donohue,2 Charles F. Knapp,1 Abhijit R. Patwardhan,1 Susan M. McDowell,4 Robert F. Taylor,5 and Joyce M. Evans1 1 Center for Biomedical Engineering, Wenner-Gren Research Laboratory, University of Kentucky, Lexington; Electrical and Computer Engineering, University of Kentucky, Lexington; 3Department of Physiology, University of Kentucky College of Medicine, Lexington; 4Department of Physical Medicine and Rehabilitation, University of Kentucky, Lexington; and 5Cardinal Hill Rehabilitation Hospital, Lexington, Kentucky 2 Submitted 30 March 2006; accepted in final form 12 October 2006 Aslan SC, Randall DC, Donohue KD, Knapp CF, Patwardhan AR, McDowell SM, Taylor RF, Evans JM. Blood pressure regulation in neurally intact human vs. acutely injured paraplegic and tetraplegic patients during passive tilt. Am J Physiol Regul Integr Comp Physiol 292: R1146 –R1157, 2007. First published November 2, 2006; doi:10.1152/ajpregu.00225.2006.—We investigated autonomic control of cardiovascular function in able-bodied (AB), paraplegic (PARA), and tetraplegic (TETRA) subjects in response to head-up tilt following spinal cord injury. We evaluated spectral power of blood pressure (BP), baroreflex sensitivity (BRS), baroreflex effectiveness index (BEI), occurrence of systolic blood pressure (SBP) ramps, baroreflex sequences, and cross-correlation of SBP with heart rate (HR) in low (0.04 – 0.15 Hz)- and high (0.15– 0.4 Hz)-frequency regions. During tilt, AB and PARA effectively regulated BP and HR, but TETRA did not. The numbers of SBP ramps and percentages of heartbeats involved in SBP ramps and baroreflex sequences increased in AB, were unchanged in PARA, and declined in TETRA. BRS was lowest in PARA and declined with tilt in all groups. BEI was greatest in AB and declined with tilt in all groups. Low-frequency power of BP and the peak of the SBP/HR cross-correlation magnitude were greatest in AB, increased during tilt in AB, remained unchanged in PARA, and declined in TETRA. The peak cross-correlation magnitude in HF decreased with tilt in all groups. Our data indicate that spinal cord injury results in decreased stimulation of arterial baroreceptors and less engagement of feedback control as demonstrated by lower 1) spectral power of BP, 2) number (and percentages) of SBP ramps and barosequences, 3) cross-correlation magnitude of SBP/HR, 4) BEI, and 5) changes in delay between SBP/HR. Diminished vasomotion and impaired baroreflex regulation may be major contributors to decreased orthostatic tolerance following injury. 12,000 spinal cord injuries (SCI) occur yearly in North America. Most SCI involve the cervical spine region, and patients who sustain cervical spine injuries have lasting, often devastating, neurological deficits and disabilities. Although the most visible effects of SCI are a loss of motor and sensory function below the lesion, acute SCI, especially those occurring in the cervical region, are often associated with hemodynamic instability. Cardiovascular problems known to arise from sympathetic nervous system dysfunction include low resting arterial blood pressure (BP), orthostatic hypotension, autonomic dysreflexia, reflex bradycardia, and cardiac arrest (2, 5, 8, 28, 49, 50). These cardiovascular conditions severely limit a patient’s participation in rehabilitation, thus extending hospital stay, increasing the cost of rehabilitation, and possibly limiting the effectiveness of other treatment. Orthostatic hypotension is a common problem, particularly in the acute phase of recovery (26, 32, 49). Short-term stability of arterial BP is achieved in large part by appropriate adjustments in sympathetic and parasympathetic outflow from the central nervous system to cardiovascular effector mechanisms (6, 35, 40, 42) It is generally assumed that fluctuations in cardiovascular parameters originate from interactions between sympathetic and parasympathetic neural branches and other low-frequency sources (22, 45, 47). Spontaneous oscillations of heart rate (HR) and BP can be analyzed to extract frequencyrelated information. In particular, two rhythms are generally observed in short-term heart rate recordings: a respiratory or high-frequency (HF) rhythm (peak ⬃0.2– 0.3 Hz in humans), considered a marker of vagal activity, and a low-frequency (LF) rhythm (peak ⬃0.1 Hz in human), a marker of sympathetic activity or combined vagal and sympathetic influence. Both LF and HF components of HR are influenced by the gain of the baroreflex (14, 33, 46). The baroreflex provides negative (i.e., closed loop) feedback regulation that minimizes the short-term fluctuations in arterial pressure (29). Although there has been a long-standing interest in assessing baroreflex characteristics and the importance of determining baroreflex sensitivity (BRS) is widely recognized, there is no “gold standard” among techniques for spontaneous baroreflex assessment (40). One of the most frequently employed approaches is the sequence technique. Sequences of three or more consecutive heartbeats in which a monotonic increase (or decrease) of systolic blood pressure (SBP) is followed, usually after a delay of one beat, by a monotonic lengthening (or shortening) of the R-R interval, are accepted as baroreflex sequences (7). Recently, the baroreflex effectiveness index (ratio between the total number of baroreflex sequences and the total number of SBP ramps) was proposed to quantify the number of times that the baroreflex is effective in driving the sinus node (15). In addition to assessment of the sensitivity of the baroreflex, the number of baroreflex sequences that occur provides information concerning overall activity of this reflex (9, 11, 15, 20, 21, 31). To find an absolute value, the occurrence number can be normalized by time (15, 31), by mean HR (11), by the Address for reprint requests and other correspondence: J. M. Evans, Center for Biomedical Engineering, Wenner-Gren Research Laboratory, Univ. of Kentucky, Lexington, KY 40506-0070 (e-mail: jevans1@pop.uky.edu). The costs of publication of this article were defrayed in part by the payment of page charges. The article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. orthostatic hypotension; baroreflex sensitivity; baroreflex effectiveness index; cross correlation; feedback APPROXIMATELY R1146 0363-6119/07 $8.00 Copyright © 2007 the American Physiological Society http://www.ajpregu.org R1147 BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY number of validated sequences (20), or by the number of heartbeats (9, 20). The number of baroreflex sequences depends on the number of analyzed heartbeats, and the number of heartbeats varies among subjects and within a subject according to activity. In addition, each baroreflex sequence can have various numbers of involved heartbeats, usually ranging from three to six. Therefore, normalization of the heartbeats involved in baroreflex sequences by the total number of heartbeats in a data segment yields more realistic information on the occurrence of baroreflex sequences. Assessing vagal and sympathetic contributions to baroreflex actions includes decomposition of BP and HR variabilities into LF and HF periodic components (4, 13, 44). In addition to the information provided by LF and HF components of BP and HR, the cross correlation between BP and HR, when considered in the same LF and HF regions, provides both magnitude and time lag (between the BP and HR variability) information to quantitatively characterize vagal and sympathetic influences on autonomic regulation (4). This study investigates short-term cardiac baroreflex regulation in able-bodied, paraplegic, and tetraplegic subjects within the first 2 mo following injury. The provocative stimulus was head-up tilt. We compared results from 1) mean values, 2) spectral power (LF and HF regions), 3) baroreflex sequence analysis, and 4) the cross correlation between SBP and HR for their potential to assess cardiovascular deficits resulting from SCI. METHODS Subjects Eleven healthy, drug-free, able-bodied volunteers (age: 25 ⫾ 4 yr, means ⫾ SE; 8 men and 3 women) were recruited as a control group. Five paraplegics (with lesions between T6 and T11; age: 34 ⫾ 15 yr; 4 men and 1 woman), and five tetraplegics (with lesions between C3 and T5; age: 26 ⫾ 9 yr; 5 men) were recruited from patients admitted to Cardinal Hill Rehabilitation Hospital (CHRH, Lexington, KY) and studied in their first 8 wk postinjury (Table 1). The following conditions excluded subjects: any orthopedic, neurological, or dermatological disorder that would contraindicate a head-up tilt, as well as deep vein thrombosis or a psychological disorder. Most SCI subjects were in some degree of deconditioning secondary to extended bed rest and immobility, causing some degree of orthostatic intolerance during the rehabilitation phase. Demographic information of the spinal cordinjured patients is given in Table 1. Subjects 2 and 7 relocated from the area before their second studies, and subject 10 did not choose to participate in a second session. Testing Schedules Able-bodied subjects were studied once, and spinal cord-injured subjects were studied twice within 8 wk postinjury. For each SCI patient, experiments were conducted while they were undergoing rehabilitation at CHRH. Studies of able-bodied subjects were performed at the General Clinical Research Center (GCRC) at the University of Kentucky. The able-bodied subjects were admitted on the day before the data collection session, to provide dietary and behavioral conditions similar to those at CHRH. Tilt Protocol All participants were familiarized with the study and gave informed consent to a protocol approved by the University of Kentucky Institutional Review Board and the Cardinal Hill Rehabilitation Hospital. All subjects were studied at least 1 h postprandial and refrained from AJP-Regul Integr Comp Physiol • VOL Table 1. Demographic characteristics of spinal cord-injured patients Postinjury Time Subject No. Age, yr Sex 1 2 3 4 5 31 20 60 23 38 M M M F M T11 ASIA A L1–L3 ASIA A T10 ASIA A T5–T10 ASIA A T10 ASIA A 6 7* 8 9 10 19 30 41 24 19 M M M M M C3 ASIA B T5 ASIA A C3 ASIA A C4 ASIA B C5 ASIA B Level of Injury First session Second session 1w, 9w, 4w, 2w, 1w, 2d 4d 1d 3d 2d 2w, 5d 1w, 8w, 1w, 3w, 2w, 5d 3d 5d 6d 3d Paraplegics 7w, 2d 3w, 2d 2w, 5d Tetraplegics 3w, 5d 3w, 5d 5w, 4d The American Spinal Injury Association (ASIA) classifications of spinal cord injury (SCI) were assessed via the sensitivity of 28 dermatomes and 10 mytomes to pin prick and light touch, and were graded by strength from 0 to 5: ASIA A, complete cord transection: no preserved motor or sensory function in S4 –S5; ASIA B, sensory incomplete: preserved sensory but not motor function below the level of injury including S4 –S5; ASIA C, motor incomplete: motor function preserved in more than half of key muscles below the level of injury, with muscle strength grade less than 3, and sensory function present below the neurological level including sacral segments S4 –S5; ASIA D, motor incomplete: preserved motor function in more than half of key muscles below the level of injury, with muscle strength grade of 3 or greater, and sensory function preserved below the neurological level including segments S4 –S5; ASIA E, normal: motor and sensory function are normal. Tetraplegia refers to an injury to the cervical section of the spinal cord. Paraplegia refers to an injury in the thoracic, lumbar, or sacral section of the spinal cord. *Behavioral characteristics (difficulty using upper extremities) of this subject led us to characterize him as tetraplegic rather than paraplegic. w, Weeks; d, days. alcohol and caffeine 24 h before the study. All subjects consumed a fat-free breakfast. Spinal cord-injured subjects wore abdominal binders and support hose. Thirty minutes before study, able-bodied subjects emptied their bladder, and SCI subjects had bladder catheterization. An intravenous cannula (Quick Cath, Baxter) was inserted into an antecubital vein to obtain blood (six 11-ml samples) for fluid volume and hormonal analyses for use in another project. Noninvasive instrumentation, described below, was applied while the subject lay supine on the tilt table. These preparations took ⬃30 min. All subjects were fixed to the tilt table by straps at the chest and pelvis. The study lasted ⬃1 h, beginning with a 10-min period of supine control, followed by four levels of head-up tilt (20°, 40°, 60°, 80°), each lasting 7–10 min (rate of tilt ⫽ 2°/s during transition). The recovery period consisted of 1 min at 20° tilt followed by 7 min supine. During tilt, members of the research and clinical team continuously monitored the alertness of the subject and hemodynamic variables. If subjects developed presyncopal symptoms (signs of fainting) during any part of the study, they were brought to supine position and the recovery phase began. Measurement Variables Beat-to-beat continuous BP was acquired from a finger cuff placed around the left middle or index finger (Portapres model-2; Finapres Medical Systems, Amsterdam, The Netherlands). Manual arterial BP measurements were taken at the beginning of supine control and at the end of the recovery period from an arm cuff blood pressure measurement device. Eight thoracic impedance (Z) leads were placed on the neck and thorax to obtain analog ECG, dZ/dt, respiration (from dZ/dt), cardiac output, and stroke volume (EXT-TEBCO; Hemo Sapiens, 292 • MARCH 2007 • www.ajpregu.org R1148 BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY Sedona, AZ). Calf circumference was acquired via a mercury-inrubber strain gauge placed around the largest part of the left calf (EC-4 plethysmograph; Hokanson, Bellevue, WA). Tilt angle was acquired from an accelerometer mounted on the tilt table. Data presented in this study include only those parameters that provide insight into reflex regulation of BP through autonomic efferent activity. Other results have been presented in abstract form (3, 19, 23). Data Acquisition the filtered sequence was then reversed and run back through the filter. The resultant series has precisely zero phase distortion. Each signal was divided into 30-s segments (150 data points) for LF and HF analysis. Data segments overlapped by 50% and were linearly detrended. Finally, cross-correlation coefficients were calculated, where the SBP segment was used as the reference signal and the HR segment was delayed with respect to the reference signal to create the time-lag axis. All coefficient values were normalized by the product of the root mean square values of HR and SBP. All data were acquired at 250 Hz and saved as a Labview file to a Dell Inspiron 4100. Before analyses, data abnormalities were removed with the Browser C⫹⫹ program written by Dr. David Brown (Biomedical Engineering, University of Kentucky). For the baroreflex sequence technique, a Matlab (The MathWorks) program was written to identify the location of the R wave in the ECG and construct a beat-to-beat R-R interval time series. The maximum value of arterial BP between the two R-R intervals (in ms) was computed and resulted in beat-by-beat sampled SBP. For the cross-correlation technique, HR was computed from ECG, SBP was computed from continuous BP, and both variables were then down-sampled to 5 Hz, all using Browser. All analyses were done using Matlab. Mean values from the two studies on the SCI subjects were used for statistical analysis. Differences within and between the three groups (able bodied, paraplegic, and tetraplegic subjects) during supine control, the four levels of head-up tilt, and recovery were tested for significance using a two-factor ANOVA. The group factor was used to indicate differences among the three groups. The tilt factor was used to indicate tilt effects for all groups. The group ⫻ tilt factor was used to determine the significance of differences in tilt effects among groups. A P value ⱕ 0.05 was accepted as indicating statistical significance. Results are presented as means ⫾ SE. Data Analysis RESULTS Spectral power. Data from the last 10 min of supine control and the last 5 min at each level of tilt (20°, 40°, 60°, 80°) and recovery were used to calculate spectral power, based on Welch’s averaged periodogram technique. Power spectral density estimates were made from 500-point windows with 50% overlapping segments using Matlab. Total spectral power was calculated for LF (0.04 – 0.15 Hz) and HF (0.15– 0.4 Hz) regions (40, 47). Baroreflex sequences. A computer program similar to those of Blaber et al. (9) and Di Rienzo et al. (15) was written to scan the beat-to-beat time series of SBP and R-R intervals using 1 mmHg (SBP) and 4 ms (R-R interval) as minimum thresholds. The last 5 min of data acquired from each tilt position were used for analysis. Three or more consecutive beats that independently contained increasing and decreasing pressure (SBP⫹, SBP⫺) and R-R interval (RR⫹, RR⫺) sequences were identified. Any SBP beats that fell within Portapres servo adjustments were excluded. The total number of excluded beats was ⬍1% of the total number of analyzed beats. If an identified SBP sequence was followed by an identified RR sequence with delays of zero, one, or two beats, these SBP and RR sequences were assigned as coupled. Only coupled sequences with regression coefficients r ⬎ 0.90 were accepted as baroreflex sequences: a positive baroreflex sequence included coupled SBP⫹ and RR⫹, and a negative baroreflex sequence included coupled SBP⫺ and RR⫺ sequences. The mean slope of the baroreflex sequence was calculated and taken as an estimation of the BRS (ms/mmHg). The numbers of beats involved in SBP ramps and baroreflex sequences were determined at each tilt position. Since the mean R-R interval varied among subjects and from supine to head-up tilt positions within the same subject, the number of beats involved in SBP ramps and baroreflex sequences are reported as the percentage of the overall number of analyzed heartbeats in the defined segment. The program gave acceptable results when tested on the Eurobavar data set (30). The baroreflex effectiveness index (BEI) was evaluated as the ratio between the total number of baroreflex sequences and the total number of SBP ramps (15). Positive BEI, the ratio between positive baroreflex sequences and SBP⫹, and negative BEI, the ratio between negative baroreflex sequences and SBP⫺, were also analyzed to determine the “selective” responsiveness of the baroreflex to rising (SBP⫹) and falling (SBP⫺) blood pressure (15). Cross-correlation analysis. The last 5 min of the HR and SBP time series from each tilt interval were filtered using fourth-order Butterworth band-pass filters to include oscillations in LF (0.04 – 0.15 Hz) or HF regions (0.15– 0.45 Hz). After filtering in the forward direction, At their first session, three able-bodied, one paraplegic, and three tetraplegic subjects demonstrated symptoms of presyncope at the end of 60° head-up tilt and were returned to the supine position immediately. The paraplegic and one of the tetraplegic subjects were able to finish the protocol at their second session. The four remaining paraplegics finished the protocol at both their first and second sessions. Illustrative data from one able-bodied (left) and one tetraplegic subject (right, C4 incomplete) are shown in Fig. 1. Blood pressure (channel 2) was well regulated in the able-bodied subject during head-up tilt, including appropriate increases in HR (channel 1) and peripheral resistance (not shown). The poor control of BP and HR during head-up tilt shown in Fig. 1 for the presyncopal tetraplegic patient was characteristic of this group. AJP-Regul Integr Comp Physiol • VOL Statistical Analysis Mean Values Average (⫾SE) SBP and HR data for able-bodied, paraplegic, and tetraplegic subjects are given in Fig. 2, A and B. Able-bodied and paraplegic subjects maintained BP throughout the tilt sequence, whereas tetraplegics exhibited a significant reduction in BP under increasing orthostatic stress (Fig. 2A). In addition, paraplegics had higher mean HR than the other groups, and tetraplegics were significantly less effective in increasing HR to accompany the tilt-induced decrease in BP (Fig. 2B). Mean breathing frequency in resting control occurred at 0.29 ⫾ 0.01 Hz for able-bodied subjects and 0.31 ⫾ 0.02 Hz for paraplegic subjects and remained fairly stable throughout the tilt. The mean breathing frequency of tetraplegic subjects ranged from 0.16 to 0.48 Hz at control with no consistent response to head-up tilt. Spectral Power The LF spectral powers of BP (LFBP) at rest and each level of head-up tilt are given in Table 2. In the LF region, ablebodied but not paraplegic or tetraplegic subjects increased LF power in response to tilt, and tetraplegic subjects had lower values than both able-bodied and paraplegic subjects. In the HF 292 • MARCH 2007 • www.ajpregu.org BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY R1149 Fig. 1. Time series for one able-bodied (AB) and one spinal cord-injured (SCI; tetraplegic) subject undergoing increasing levels of head-up tilt (HUT). After supine control, each subject was tilted to 20°, 40°, 60°, and 80° and returned to the supine position. Each tilt angle was held for 7–10 min. The SCI subject was returned to supine position upon the development of symptoms of presyncope. The AB subject used increases in heart rate (HR; bpm, beats/min) to regulate blood pressure (BP), whereas the SCI subject was much less successful in regulating BP and HR. Calf circumferences, an estimation of blood pooling to the lower extremities, were not different between subjects, probably because SCI wore support hose. region, there was a significant overall effect of tilt to decrease power, but the interaction among groups and tilt was not significant (data not shown). Baroreflex Sequences Baroreflex sensitivities (slope of the R-R interval-SBP relationship) at rest and during head-up are given in Table 3 for all groups. The lower slope of BRS in paraplegic compared with able-bodied subjects was significant only in recovery. The group ⫻ tilt interaction results apply to the tilt-induced decrease in BRS that was significant in able-bodied and tetraplegic subjects but not significant in paraplegic subjects. The average (⫾SE) percentage of heartbeats involved in SBP ramps (A) and in baroreflex sequences (B) are given for all groups in Fig. 3. The actual numbers of blood pressure ramps that occurred were also lower in both SCI groups than in the able-bodied group (data not shown). Each index increased significantly in able-bodied subjects, remained relatively unchanged in paraplegics, and declined in tetraplegics with increasing tilt angle. Both SCI groups had significantly lower values than the able-bodied group at each tilt position. Only group and tilt main effects, but not their interaction, were significant for the BEI, which was greater in able-bodied than in tetraplegic subjects and declined with increasing tilt in all groups (Fig. 4). Positive and negative BEI values were similar at each tilt level. Cross Correlation Cross correlation of BP and HR can be used to evaluate both direct and inverse relationships between BP and HR (4). Figure 5 shows simultaneous 50-s recordings of SBP (A) and HR (B) and the cross correlation between the two variables (C) for one able-bodied subject at 80° head-up tilt. The cross correlation in Fig. 5C has two main features: the magnitude of the correlation on the vertical axis and the lead/lag time between SBP and HR AJP-Regul Integr Comp Physiol • VOL on the horizontal axis. A correlation magnitude value of ⫹1 indicates perfect direct association between these two signals; ⫺1 indicates a perfect indirect association. Just to the left of zero in Fig. 5C on the abscissa lies the principal negative cross-correlation peak. Since SBP was used as a reference signal and HR was slid backward and forward, negative lags refer to SBP leading HR. One would expect an inverse relationship between SBP and HR, with SBP leading, if the baroreflex were figuring importantly in BP regulation. Restated, the negative peak value of ⫺0.86, occurring around ⫺1.5 s, indicates that changes in SBP drive opposite (feedback) changes in HR with an ⬃1.5-s time delay. There is also, however, a positive peak of ⫹0.75 at ⬃4.5 s (i.e., to the right of zero lag), indicating that changes in HR resulted in samedirectional (i.e., direct, not inverse) changes in SBP with a 4.5-s time delay. Indexes of Sympathetic Activity Figure 6 displays the SBP/HR cross correlation developed in Fig. 5 with the added feature of tracking the correlation across time (abscissa in each box). In effect, the correlation in Fig. 5C has been rotated 90° counterclockwise (positive lags corresponding to SBP lagging HR are shown above zero) with sequential correlations across time chained together (time progressing left to right for each segment). Data are given as the group-averaged LF (0.04 – 0.15 Hz) cross correlations for ablebodied, paraplegic, and tetraplegic studies at rest (supine control), in response to tilt, and during recovery from tilt. The magnitudes of the cross-correlation values are color coded according to the color bars indicated: positive values are shown in yellow/red, whereas negative values are shown in blue/ violet. The time in minutes (i.e., progression of the experiment) is plotted along the horizontal axes for each tilt angle. The able-bodied group had strong negative and positive interactions (blue and red bands, respectively) at all tilt levels. Paraplegics 292 • MARCH 2007 • www.ajpregu.org R1150 BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY Figure 7 shows the average cross-correlation magnitude of the SBP/HR negative peak in the LF region. Although correlation magnitudes were similar for all groups during the initial supine condition, SCI patients did not exhibit increasing magnitude in response to tilt, as was the case for able-bodied subjects. In response to tilt, time lags for reaching the LF maximum negative correlation peak did not change significantly from the control value (1.7 ⫾ 0.1 to 1.8 ⫾ 0.3 s) for able-bodied subjects. In SCI, time lags were similar to those in able-bodied subjects at control but were significantly greater at 20° and 40° tilt (2.5 ⫾ 0.4 and 2.1 ⫾ 0.3 s for paraplegics, 3.1 ⫾ 0.8 and 3.2 ⫾ 0.9 s for tetraplegics). In addition, the time delays in paraplegic subjects were significantly greater than in able-bodied subjects during recovery. Although the effect was significant, time lags in tetraplegic subjects were erratic and difficult to identify at higher tilt levels, probably because the correlation was obscured by noise and other weakly correlated processes (note low correlation values). Indexes of Parasympathetic Activity Fig. 2. Averaged (⫾SE) systolic blood pressure (SBP; A) and HR (B) for AB (n ⫽ 11), paraplegic (PARA; n ⫽ 5), and tetraplegic subjects (TETRA; n ⫽ 5) in response to HUT. TETRA demonstrated decreases in mean BP and less effective increases in HR in response to increasing orthostatic stress. PARA demonstrated higher mean HR to accompany the tilt-induced orthostatic stress. P ⬍ 0.05, SBP: group, tilt, and group ⫻ tilt interaction. P ⬍ 0.05, HR: tilt and group ⫻ tilt interaction. F, Significantly different from AB (same stress level); ⌬, significantly different from PARA (same stress level); ⽤, significantly different from control (same group). maintained strong interactions between HR and SBP during increasing stress, whereas tetraplegics had weaker interactions during rest and recovery that essentially disappeared during higher levels of tilt. Figure 8 contains group-averaged HF (0.15– 0.45 Hz) cross correlation between SBP and HR for able-bodied, paraplegic, and tetraplegic subjects during supine rest, in response to tilt, and recovery from tilt. Able-bodied subjects had the strongest blue and red bands, both at rest and during head-up tilt. Paraplegics had weaker correlations than able-bodied subjects, but a discernable coordination between the two variables remained throughout the study. Both positive and negative correlations declined with progressive head-up tilt in tetraplegics. Figure 9 shows the group-averaged magnitude of the HF negative peak of the cross correlation between SBP and HR in the HF region. There was an overall tilt effect (decline in correlation magnitude with increasing tilt angle) and the magnitude of the HF negative peak was greater in able-bodied subjects than in spinal cord-injured subjects, but there was no significant interaction. Time lags in this HF region significantly increased from supine control to 80° head-up tilt in able-bodied and paraplegic subjects (from 0.2 ⫾ 0.07 to 0.6 ⫾ 0.1 s in able-bodied subjects; from 0.4 ⫾ 0.09 to 0.8 ⫾ 0.2 s in paraplegics). The time lags of paraplegic subjects were significantly greater than those of able-bodied subjects at 40° head-up tilt and recovery. Time lags of tetraplegic subjects were erratic and subject to much variability; therefore, their values were not included in the analysis. DISCUSSION The present study examined short-term cardiac baroreflex regulation in able-bodied, paraplegic, and tetraplegic subjects Table 2. Averaged (⫾SE) spectral power of blood pressure in the LF region for able-bodied, paraplegic, and tetraplegic subjects in response to head-up tilt Group Supine control 20° HUT 40° HUT 60° HUT 80° HUT Supine recovery Able bodied Paraplegic Tetraplegic 69.7⫾10.2 40.9⫾14.4* 18.3⫾4.5* 59.0⫾6.6 28.9⫾6.4* 13.3⫾4.46* 84.7⫾10.3 37.9⫾11.4* 9.9⫾3.0* 113.0⫾18.2‡ 41.1⫾9.54* 14.3⫾5.7*† 129.6⫾28.3‡ 43.0⫾9.4* 12.9⫾3.8*† 50.9⫾5.6 47.6⫾14.5 16.9⫾4.27*† Values are average (⫾SE) spectral power of blood pressure (BP) in the low-frequency region for able-bodied (AB; n ⫽ 11), paraplegic (n ⫽ 5), and tetraplegic subjects (n ⫽ 5) in response to varying degrees of head-up tilt (HUT). Spectral power of BP in the low frequency (LF) region significantly increased in AB and decreased in spinal cord-injured subjects (SCI) (group, tilt, and group ⫻ tilt interaction, P ⱕ 0.05). *Significantly different from AB (same stress level). †Significantly different from paraplegic (same stress level). ‡Significantly different from control (same group). AJP-Regul Integr Comp Physiol • VOL 292 • MARCH 2007 • www.ajpregu.org R1151 BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY Table 3. Averaged (⫾SE) baroreflex sensitivity index for AB, paraplegic, and tetraplegic subjects in response to HUT Group Supine control 20° HUT 40° HUT 60° HUT 80° HUT Supine Recovery AB Paraplegic Tetraplegic 20.7⫾4.1 9.8⫾3.2 21.9⫾7.1 18.7⫾4.8 7.6⫾2.2 12.8⫾2.8 10.1⫾2.2† 5.2⫾1.5 11.4⫾2.9† 7.2⫾2.7† 3.9⫾0.9 11.1⫾3.4† 5.5⫾2.2† 3.7⫾1.3 5.2⫾2.7† 24.5⫾4.7 7.8⫾2.3* 21.0⫾4.6 Values are average (⫾SE) baroreflex sensitivity index (ms/mmHg) for AB (n ⫽ 11), paraplegic (n ⫽ 5), and tetraplegic subjects (n ⫽ 5) in response to HUT. Tilt and group ⫻ tilt interaction, P ⱕ 0.05. *Significantly different from AB (same stress level). †Significantly different from control (same group). during the injured subjects’ acute phase of recovery. There are three major findings. First, tetraplegic subjects demonstrated a significant reduction in their ability to regulate BP and HR in response to tilt. Second, paraplegic and tetraplegic patients demonstrated significantly reduced input to baroreflexes as indicated by lower values of LF spectral power of BP, lower numbers of SBP ramps and percentages of heartbeats involved in ramps and baroreflex sequences, and a lower BEI than did able-bodied persons. Third, SCI resulted in a significant reduction in the negative cross-correlation peak and changed the Fig. 3. Averaged (⫾SE) percentage of heartbeats involved in SBP ramps (A) and in baroreflex (BR) sequences (B) for AB (n ⫽ 11), PARA (n ⫽ 5), and TETRA (n ⫽ 5) at rest and in response to HUT. AB significantly increased both indexes with HUT. Both indexes were significantly lower in PARA and TETRA than in AB during HUT. P ⬍ 0.05, group, tilt, and group ⫻ tilt interaction. F, Significantly different from AB (same stress level); ⽤, significantly different from control (same group). AJP-Regul Integr Comp Physiol • VOL time delay (between fluctuations in SBP and HR) in response to increasing levels of head-up tilt. The reduced correlation occurred in both LF (index of sympathetic activity) and HF (index of parasympathetic activity) regions, with the major impact of SCI occurring in the LF region. Mean Values HR increased significantly during tilt in able-bodied subjects and paraplegics and enabled these individuals to maintain BP during the orthostatic challenge; conversely, the tilt-induced rise in HR in tetraplegics was not significant and (in combination with small increases in total peripheral resistance) was not sufficient to maintain stable blood pressure. We hypothesize that the limited, tilt-induced rise in HR in tetraplegics is a direct result of disruption of the normal sympathetic innervation of the heart. That is, withdrawal of cardiac parasympathetic nervous activity is the surviving autonomic nervous mechanism to control HR in these patients; if so, HR can increase only up to the “intrinsic” rate of the sinoatrial (SA) node (18). This intrinsic rate, however, is modulated by circulating catecholamines. This latter effect should be substantial in these SCI subjects, since circulating levels of catecholamines were more than double that in able-bodied subjects both at rest and during tilt (19). We addressed the role of sympathetic versus parasympathetic denervation in a previous study in dogs where we demonstrated that intrinsic HR was significantly reduced after 3 wk of total denervation of the heart (19). In those animals, selective parasympathectomy of the SA node accounted for only some of the decline in intrinsic Fig. 4. Averaged (⫾SE) baroreflex effectiveness index for AB (n ⫽ 11), PARA (n ⫽ 5), and TETRA (n ⫽ 5) at rest and in response to HUT. The index was greatest in AB and declined with increasing tilt level in all groups. P ⬍ 0.05, group (TETRA ⬍ AB) and tilt effects. 292 • MARCH 2007 • www.ajpregu.org R1152 BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY resulting vaso- and venomotor tone strongly influence results reported. Baroreflex Fig. 5. Fifty seconds of SBP (A) and HR (B) from 1 AB subject at 80° HUT. The cross correlation between these variables is shown in C, where the magnitude of the correlation is given on the vertical axis and the lead/lag between signals is given on the horizontal axis. A negative magnitude denotes negative feedback (i.e., an inverse relationship between changes in BP and HR); a positive magnitude denotes a direct relation between signals (i.e., HR and BP increasing concurrently). Negative lags indicate that SBP led HR, and positive lags indicate that SBP lagged HR. rate. We therefore hypothesize that the inability of tetraplegics to achieve HR comparable to those of able-bodied subjects and paraplegics was most likely due to injury-related decline in intrinsic HR, secondary to “denervation” of sympathetic HR control. As has been previously reported (51), paraplegics had higher HR, significant at supine control and recovery, than did able-bodied controls. Hormonal activity for a subset of these subjects was reported previously and indicated that, this early after injury, spinal cord-injured subjects exhibited significantly higher resting and tilt values of plasma renin activity and catecholamines (particularly epinephrine) than able-bodied subjects (23). In addition, able-bodied subjects responded to head-up tilt with increasing values of these substances, whereas levels in spinal cordinjured subjects were tonically elevated. Cardiovascular effects of chronically elevated vasoactive hormones probably play a very significant role in setting mean BP and HR. Effects of these hormones on the other variables measured or calculated in the present study are not as clear, but we hypothesize that AJP-Regul Integr Comp Physiol • VOL Our able-bodied BRS values fell in the range previously reported for similar subjects in both supine and head-up tilt positions (16, 20, 25, 30, 36, 52). The BRS did not differ significantly between able-bodied and tetraplegic subjects (Table 3), an effect previously observed for tetraplegics studied 12 mo post injury (25). The lower BRS in paraplegics that was significant in recovery can probably be accounted for by the higher HR of paraplegics. BRS is strongly dependent on the prevailing HR, an effect that was used to explain the lower BRS of paraplegic compared with able-bodied subjects of a previous study (1). In fact, when we plotted the natural logarithm of BRS against HR, we found that able-bodied and tetraplegic subjects had equivalent BRS values at HR ⬍ 70 beats/min, whereas able-bodied and paraplegic subjects demonstrated similar BRS values at HR ⬎ 75 beats/min (data not shown). These findings are consistent with the probability that baroreflex responses to tilt were highly influenced by the prevailing HR. If so, with BRS strongly being a function of parasympathetic outflow and vagal control of HR remaining relatively intact after SCI, our results are in agreement with prevailing wisdom. The occurrence of baroreflex sequences has been reported previously to increase in able-bodied subjects as they were moved from supine to head-up tilt position (11, 20, 31). Our able-bodied group demonstrated a tilt-induced increase in the percentage of heartbeats involved in baroreflex sequences (from 32 ⫾ 0.02% at rest to 41.3 ⫾ 0.03% at 60° head-up tilt), within the same range reported by one of these groups (11). In addition, able-bodied subjects demonstrated increased LFBP power as well as an increased number and percentage of SBP ramps during tilt. The situation in paraplegics and particularly in tetraplegics was quite different. Although control values were not different from those of able-bodied subjects, neither paraplegic nor tetraplegic subjects increased the number of BP ramps or the percentage of heartbeats involved in either baroreflex sequences or SBP ramps during head-up tilt. The smaller percentages of SBP ramps and baroreflex sequences in response to head-up tilt relative to able-bodied subjects were significant for both paraplegics and tetraplegics. In addition, these same paraplegic and tetrapletic subjects exhibited significantly lower LF spectral power of lower body skin perfusion, an independent measure of vasomotion (23). We interpret this diminution within the LF range as a direct result of SCI-induced dysfunction of sympathetic control of vascular dynamics. Conversely, the similar HF performance of all three groups probably results from the relatively intact parasympathetic control of HR in all groups. The combination of lower values of LFBP, the lower number of SBP ramps, and, consequently, a lower number of baroreflex sequences, leads us to conclude that higher levels of SCI resulted in reduced stimulation to baroreceptors. These results are supported by spectral power of BP, which was significantly lower in tetraplegics, probably a result of diminished vasomotion following SCI. Finally, reduced afferent baroreflex stimulation was not completely responsible for the loss of regulatory capability in 292 • MARCH 2007 • www.ajpregu.org BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY R1153 Fig. 6. Group-averaged low-frequency (0.04 – 0.15 Hz) cross correlation between SBP and HR for AB (top, n ⫽ 11), PARA (middle, n ⫽ 5), and TETRA (bottom, n ⫽ 5) at rest (supine control), in response to tilt (20 – 80° HUT), and recovery from tilt (supine recovery). The lead/lag times in seconds are given on the vertical axes; time in minutes (i.e., during each phase of the study) is plotted along the horizontal axes. The negative lags refer to SBP leading HR; positive lags refer to SBP lagging HR. The magnitude of the correlation is indicated by the color density: blue represents negative (i.e., inverse cross correlation between BP and HR changes), whereas red represents positive (direct) correlations. Bar at right shows the magnitude of the correlation. The last 5 min of data from each tilt position are plotted. The strong blue band around ⫺2 s in AB represents responses characteristic of baroreflex function (e.g., BP increase preceding reflex HR decrease). This band also is visible in PARA, but with less strength during some orthostatic stress levels. The diminishment in the strength of the feedback magnitude with increasing orthostatic stress is clearly visible in TETRA. The direct relationship between HR and BP represented by the red band located around 3.5 s remained in AB and PARA but decreased in TETRA under increasing orthostatic stress. tetraplegics. In able-bodied subjects, the BEI decreased from 65.0 ⫾ 0.03 to 48.7 ⫾ 0.06% between supine and 80° head-up tilt, whereas BRS decreased from 20.7 to 5.5 ms/mmHg. Supine control BEI values and parallel decreases in BEI and BRS in response to orthostatic stress, similar to those of the present study, have been reported previously (16, 42). Overall tilt effects were also present for all groups for both BEI and BRS. In tetraplegics, however, BEI was lower than in ablebodied subjects, an effect that was not significant for BRS. Therefore, although the BRS index for tetraplegics was similar to that for able-bodied subjects at each tilt position, their BEI was significantly lower than that of able-bodied subjects, indicating a loss of baroreflex effectiveness in driving the SA node. Together, our data support the concept that although the parasympathetically dominated baroreflex lost some capability to regulate HR in tetraplegics, the principal affect appeared to be attenuation of (primarily) LF hydrostatic input to the baroreceptors. The mixed sympathetic and parasympathetic innervations of paraplegics and the decreased stimulation to baroreAJP-Regul Integr Comp Physiol • VOL ceptors probably all contribute to the significant decrease in BRS in that injury; however, the higher HR of paraplegics also may contribute. LF Cross Correlation As an Index of Sympathetic Activity The tilt-induced increase in the magnitude of the negative peak of the cross correlation between SBP and HR in the LF range may index a progressive increase in sympathetic dominance in able-bodied subjects at higher levels of orthostatic challenge. However, parasympathetic withdrawal is a wellestablished response to increasing orthostatic stress, so we hypothesize that the amplitude of the negative peak of the cross correlation actually assesses the balance between the two divisions of the autonomic nervous system (36). With peripheral vascular and cardiac spinal pathways impaired, paraplegics did not increase their cross-correlation magnitude during tilt. Tetraplegics steadily lost correlation during tilt, probably because of damaged sympathetic outflow to the heart in addition to the loss of peripheral pathways suffered by the para292 • MARCH 2007 • www.ajpregu.org R1154 BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY sympathetic activity (27). The time delay in our able-bodied group increased significantly from 0.2 ⫾ 0.07 to 0.6 ⫾ 0.1 s when subjects moved from supine position to 80° head-up tilt. The time delay in paraplegic subjects also increased significantly from 0.4 ⫾ 0.09 to 0.8 ⫾ 0.2 s in response to tilt, indicating typical vagal baroreflex control. The group-averaged time delay in tetraplegic subjects occurred near 0 s at each tilt level; however, the variance around the mean ranged from 0.2 to 1.3 s. This high variance, coupled with the low coherence, led us to exclude the tetraplegic group from time delay results Limitations of the Study Fig. 7. Group-averaged magnitude of the low-frequency (0.04 – 0.15Hz) negative peak of the cross correlation between SBP and HR at rest and in response to tilt is shown for AB (n ⫽ 11), PARA (n ⫽ 5), and TETRA (n ⫽ 5). With HUT, the strength of the correlation significantly increased in AB, persisted at a weaker level in PARA, and declined in TETRA (P ⬍ 0.05, group, tilt, and group ⫻ tilt interaction). F, Significantly different from AB (same stress level); ⌬, significantly different from PARA (same stress level); ⽤ significantly different from control (same group). plegic patients. All able-bodied subjects demonstrated strong, constant blue bands at each tilt position, indicating strong, active feedback control. Although characterized by lower magnitude and longer time delay, the blue band was also consistent in all paraplegic subjects, except in the 60-yr-old subject who lost consistant correlation at higher stress levels. Besides demonstrating very low magnitude and erratic time delays, negative correlations in tetraplegic subjects occurred only sporadically, indicating that a demonstrable coupling between changes in BP and HR occurred in less than one of the 5-min data segments. Since patients with poor othostatic tolerance had an increased phase shift between SBP and HR fluctuations, as well as lower magnitude correlations (20), an increase in time delay might also contribute to the orthostatic hypotension problems that occur following SCI. HF Cross Correlation As an Index of Parasympathetic Activity The tilt-induced decrease in the magnitude of the negative peak of the cross correlation between SBP and HR represents, we believe, a progressive withdrawal of parasympathetic outflow that was present in all three groups but was more pronounced in SCI subjects. Although both paraplegic and tetraplegic subjects had lower magnitude responses compared with able-bodied subjects, paraplegics did maintain feedback control at each tilt level, whereas tetraplegics increasingly lost control as tilt angle increased. The strong correlation at lower tilt angles in tetraplegics may be due in part to respiratory coupling, since our tetraplegic subjects demonstrated greater breathing fluctuation effects on HR and SBP (3). Previous studies in able-bodied subjects reported baroreflex latencies of 0.5– 0.6 s (10, 41) and significantly shorter latencies (17) in response to different types of stimuli. In addition, the time delay between baroreceptor stimulation and oscillations of R-R interval have been reported to increase with decreasing paraAJP-Regul Integr Comp Physiol • VOL One particular challenge we encountered was recruiting SCI subjects immediately following injury. In addition, the complexity of classifying the injury contributed to large variability among subjects within the same group, such as complete or incomplete injury and different levels of injury. Other factors include variability in SCI tolerance, medications, rehabilitation progress, and recovery from spinal shock. Able-bodied subjects were studied only one time. We made this decision based on previous studies in our laboratory, as well as results published by others, indicating that tolerance to a presyncopal orthostatic stress is reproducible even within a 72- to 120-h time frame, (24). The mean negative peak magnitudes and time delays in tetraplegics may not accurately represent the correlation between HR and SBP in some segments, since inconsistent structure of feedback control was common in that group. Although we did our best to identify the negative peak magnitude and time delay values to represent each 5-min correlation, the inconsistencies lead us to conclude that it is more instructive to view the feedback structure of whole segments (Figs. 6 and 8). The positive cross correlation between HR and SBP was not addressed in this report. A direct relation such as this has been attributed in rats to an open-loop control mechanism (4), which must be considered in a subsequent publication. Impedance measures of cardiac output and stroke volume, upper and lower body skin perfusions, intra/ extravascular fluid shifts, and vasoactive hormone information should provide further insight into cardiovascular regulation in these subjects. These data are not presented in the present report because of the lengthy nature of their inclusion; however, results of those analyses, reported in abstract form (3, 19, 23), support the present results. Finally, although there is controversy concerning the relationship between muscle sympathetic nerve activity and LFBP (48), the controversy does not extend to the use of this measure of Mayer wave activity as an index of vasomotion (37). Perspectives Consistent and reproducible assessment scales are necessary to define acutely injured patient deficits and to facilitate communication with caregivers regarding the patient’s status (1). The American Spinal Injury Association scale for neurological status and the Functional Independence Measure for functional outcome are the most commonly used scales. Besides the deficit of motor and sensory functioning following SCI, cardiovascular problems known to arise from sympathetic nervous system dysfunction also are common in acute SCI, especially those occurring in the cervical region. Despite these problems, there is no assessment test available to identify patients’ 292 • MARCH 2007 • www.ajpregu.org BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY R1155 Fig. 8. Group-averaged, high-frequency (0.15– 0.45 Hz) cross correlation between SBP and HR for AB (top, n ⫽ 11), PARA (middle, n ⫽ 5), and TETRA (bottom, n ⫽ 5) at rest (supine control), in response to tilt (20 – 80 HUT), and recovery from tilt (supine recovery). The lead/lag times in seconds are given on the vertical axes, and time in minutes (i.e., progression of the experiment) is plotted along the horizontal axes. The negative lags refer to SBP leading HR, and positive lags refer to SBP lagging HR. The magnitude of the correlation is indicated by the color density: blue represents an inverse relationship, whereas red represents a positive (direct) correlation. Bar at right shows the magnitude of the correlation; the darker the color, the stronger the correlation. The last five min of data from each tilt position are plotted. The strong blue band around ⫺1 s in AB represents negative feedback control, which also appears in PARA but with less strength. The diminishment in the strength of the feedback magnitude with increasing orthostatic stress is clearly visible in TETRA. The red band around 1.5 s remained in AB and PARA but diminished in TETRA during HUT. cardiovascular deficits following SCI. In this study, we attempted to discriminate able-bodied from spinal cord-injured subjects, and paraplegics from tetraplegics, by using cardiovascular variables measured at rest and in response to tilt. In that regard, the magnitude of the cross correlation between HR and SBP in the LF region, LFBP, percentage of heartbeats involved in BP ramps, and baroreflex sequences all appear to be viable diagnostic indicators of the level of autonomic injury and subsequent recovery. In summary, able-bodied subjects responded to head-up tilt with increased LFBP (Table 2), increased number of ramps and percentage of heartbeats involved in SBP ramps and baroreflex sequences (Fig. 3), and increased cross correlation between HR and SBP in the LF region (Fig. 7). That these variables were diminished in paraplegics and absent in tetraplegics supports the concept that each is dependent on intact, peripheral sympathetic pathways to the lower body. Together, our data provide evidence that tilt-induced, sympathetically mediated reflex vasomotion and modulation of HR are major components of BP regulation of orthostatic stress. In the HF region, declines in BEI (Fig. 4) and the HF cross correlation of BP and AJP-Regul Integr Comp Physiol • VOL Fig. 9. Group-averaged magnitude of the high-frequency (HF; 0.15– 0.45 Hz) negative peak of the cross correlation between SBP and HR at rest and in response to tilt is shown for AB (n ⬎ 11), PARA (n ⫽ 5), and TETRA (n ⫽ 5). Overall tilt and group effects were observed with AB ⬎ SCI and magnitude decreasing with increasing tilt (P ⬍ 0.05, group and tilt). F, Significantly different from AB (same stress level); ⽤ significantly different from control (same group). 292 • MARCH 2007 • www.ajpregu.org R1156 BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY HR (Fig. 9) characterized the response to head-up tilt in all groups. This decline probably reflects overall withdrawal of parasympathetic activity in response to tilt. However, lower values of BEI (Fig. 4) and magnitude of the HF SBP/HR cross correlation (Fig. 9) in tetraplegics compared with able-bodied subjects indicate a deficit in parasympathetic regulation of HR regulation resulting from spinal cord injury in the cervical region of the spine. ACKNOWLEDGMENTS Dr. Helena Truszczynska from the University of Kentucky assisted with the repeated-measures ANOVA statistical design and analysis. Dr. David Brown, UK Center for Biomedical Engineering, kindly provided his BROWSER program for cleaning and aligning data and constructing beat-by-beat HR, SBP, DBP, and MBP traces for subsequent analysis in Matlab. The team at Wenner-Gren Research Laboratory, Chaz Hogencamp, Adam Vogt, Will DeVries, and Evan Baxter, were invaluable in the conduct of studies. Eric Hartman and customKYnetics developed and assembled the data acquisition system. Andrea Hartman, RN, coordinated studies with the staff of both Cardinal Hill Rehabilitation Hospital and the UK General Research Center. GRANTS This work was supported by the Kentucky Spinal Cord and Head Injury Research Trust, UK General Clinical Research Center Grant MM01R022602, and Cardinal Hill Rehabilitation Hospital. REFERENCES 1. Abrahamsson C, Ahlund C, Nordlander M, Lind L. A method for heart rate-corrected estimation of baroreflex sensitivity. J Hypertens 21: 2133– 2140, 2003. 2. Aito S. Complications during the acute phase of traumatic spinal cord lesion. Spinal Cord 41: 629 – 635, 2003. 3. Aslan S, Evans JM, Knapp CK, Patwardhan AR, Hartman EJ, Donohue K, McDowell S. Neural control of cardiovascular variables following spinal cord injury (Abstract). FASEB J 442: A662, 2004. 4. Baldridge BR, Burgess DE, Zimmerman EE, Carroll JJ, Sprinkle AG, Speakman RO, Li SG, Brown DR, Taylor RF, Dworkin S, Randall D. Heart rate-arterial blood pressure relationship in conscious rat before vs. after spinal cord transaction. Am J Physiol Regul Integr Comp Physiol 283: R748 –R756, 2002. 5. Ball PA. Critical care of spinal cord injury. Spine 26: S27–S30, 2001. 6. Baselli G, Cerutti S, Civardi S, Malliani A, Pagani M. Cardiovascular variability signals: towards the identification of a closed-loop model of the neural control mechanisms. IEEE Trans Biomed Eng 35: 1033–1046, 1988. 7. Bertinieri G, DiRienzo M, Cavallazzi A, Ferrari AU, Pedotti A, Mancia G. A new approach to analysis of the arterial baroreflex. J Hypertens Suppl 3: S79 –S81, 1985. 8. Bilello JF, Davis JW, Cunningham MA, Groom TF, Lemaster D, Sue LP. Cervical spinal injury and the need for cardiovascular intervention. Arch Surg 138: 1127–1129, 2003. 9. Blaber AP, Yamamoto Y, Hughson RL. Methodology of spontaneous baroreflex relationship assessed by surrogate date analysis. Am J Physiol Heart Circ Physiol 268: H1682–H1687, 1995. 10. Borst C, Karemaker JM. Time delays in the human baroreceptor reflex. J Auton Nerv Syst 9: 399 – 409, 1993. 11. Bouhaddi MB, Henriet MT, Cappelle S, Dumoulin G, Regnard J. Active standing and passive tilting similarly reduce the slope of spontaneous baroreflex in healthy subjects. Physiol Res 47: 227–235, 1998. 12. Carlson GD, Gorden C. Current development in spinal cord injury research. Spine J 2: 116 –128, 2002. 13. Cerutti S, Barres C, Paultre CZ. Baroreflex modulation of blood pressure and heart rate variabilities in rats: assessment by spectral power analysis. Am J Physiol Heart Circ Physiol 266: H1993–H2000, 1994. 14. DeBoer RW, Karemaker JW, Stracke J. Hemodynamic fluctuation and baroreflex sensitivity in humans: a beat-to-beat model. Am J Physiol Heart Circ Physiol 253: H680 –H689, 1987. 15. Di Rienzo M, Parati G, Castiglioni P, Tordi R, Mancia G, Pedotti A. Baroreflex effectiveness index: an additional measure of baroreflex control of heart rate in daily life. Am J Physiol Regul Integr Comp Physiol 280: R744 –R751, 2001. AJP-Regul Integr Comp Physiol • VOL 16. Di Rienzo M, Castiglioni P, Mancia G, Pedotti A, Parati G. Advancements in estimating baroreflex function. IEEE Eng Med Biol Mag 20: 25–32, 2001. 17. Eckberg DL. Temporal response patterns of the human sinus node to brief carotid baroreceptor stimuli. J Physiol 258: 769 –782, 1976. 18. Evans JM, Funk JN, Randall DC, Knapp CF. Influence of cardiac innervation on intrinsic heart rate in dogs. Am J Physiol Heart Circ Physiol 258: H1132–H1137, 1990. 19. Evans JM, Aslan SC, Hogancamp C, Vogt AP, Randall DC, McDowell SM, Hartman EA, Taylor RF, Ziegler MG, and Knapp CF. Autonomic damage and blood pressure regulation in spinal cord injured patients compared to able bodied subjects (Abstract). FASEB J 20: A1429, 2006. 20. Gulli G, Claydon VE, Cooper VL, Hainsworth R. R-R interval-blood pressure interaction in subjects with different tolerances to orthostatic stress. Exp Physiol 90: 367–375, 2005. 21. Hadley MN. Clinical assessment after acute cervical spinal cord injury. Neurosurgery 50: S21–S29, 2002. 22. Halàmek J, Kàra T, Juràk P, Souček M, Francis DP, Davies LC, Shen WK, Coats AJS, Novàk M, Novàkovà Z, Panovský R, Toman J, Šumbera J, Somers VK. Variability of phase shift between blood pressure and heart rate fluctuations. Circulation 108: 292–297, 2003. 23. Hogencamp CE, Knapp CF, Aslan S, Hartman A, Evans JM. Role of skin perfusion and fluid volume shifts in regulating blood pressure following spinal cord injury (Abstract). FASEB J 18: A662, 2004. 24. Howden R, Tranfield PA, Lightfoot JT, BrownSJ, Swaine IL. The reproducibility of tolerance to lower-body negative pressure and its quantification. Eur J Appl Physiol 84: 462– 468, 2001. 25. Iellamo F, Legramante JM, Massaro M, Galante A, Pigozzi F, Claudio Nardozi Santilli V. Spontaneous baroreflex modulation of heart rate and heart rate variability during orthostatic stress in tetraplegics and healthy subjects. J Hypertens 19: 2231–2240, 2001. 26. Illman A, Stiller K, Williams M. The prevalence of orthostatic hypotension during physiotherapy treatment in patients with an acute spinal cord injury. Spinal Cord 3: 741–747, 2000. 27. Keyl C, Schneider A, Dambacher M, Bernardi L. Time delay of vagally mediated cardiac baroreflex response varies with autonomic cardiovascular control. J Appl Physiol 91: 283–289, 2001. 28. Krassioukov AV, Fehlings MG. Effects of graded spinal cord compression on cardiovascular neurons in the rostra-ventro-lateral medulla. Neuroscience 88: 959 –973, 1999. 29. Lanfranchi PA, Somers VK. Arterial baroreflex function and cardiovascular variability: interactions and implications. Am J Physiol Regul Integr Comp Physiol 283: R815–R826, 2002. 30. Laude D, Elghozi JL, Girard A, Bellard E, Bouhaddi M, Castiglioni P, Cerutti C, Cividjian A, Di Rienzo M, Fortrat JO, Janssen B, Karemaker JM, Leftheriotis G, Parati G, Persson PB, Porta A, Quintin L, Regnard J, Rudiger H, Stauss HM. Comparison of various techniques used to estimate spontaneous baroreflex sensitivity (the EuroBaVar study). Am J Physiol Regul Integr Comp Physiol 286: R226 –R231, 2004. 31. Legramante JM, Raimondi G, Massaro M, Iellamo F. Positive and negative feedback mechanisms in the neural regulation of cardiovascular function in healthy and spinal cord-injured humans. Circulation 103: 1250 –1255, 2001. 32. Lehmann KG, Lane JG, Piepmeier JM. Cardiovascular abnormalities accompanying acute spinal cord injury in humans: incidence time course and severity. J Am Coll Cardiol 10: 46 –52, 1987. 33. Lucini D, Guzzetti S, Casiraghi S, Pagani M. Correlation between baroreflex gain an 24-h indices of heart rate variability. J Hypertens 20: 1625–1631, 2002. 34. McDonald JW, Sadowsky C. Spinal-cord injury. Lancet 359: 417– 425, 2002. 35. Mullen TJ, Appel ML, Mukkamala R, Mathias JM, Cohen RJ. System identification of closed-loop cardiovascular control: effects of posture and autonomic blockade. Am J Physiol Heart Circ Physiol 272: H448 –H461, 1997. 36. O’Leary DD, Kimmerly DS, Cechetto AD, Shoemaker K. Differential effect of head-up tilt on cardiovagal and sympathetic baroreflex sensitivity in humans. Exp Physiol 88.6: 769 –774, 2004. 37. Pagani M, Montano N, Porta A, Malliani A, Abboud FM, Birkett C, Sommers VK. Relationship between spectral components of cardiovascular variabilities and direct measures of muscle sympathetic nerve activity in humans. Circulation 95: 1441–1448, 1997. 38. Parati G, Saul JP, Castiglioni P. Assessing arterial baroreflex control of heart rate: new perspectives. J Hypertens 22: 1259 –1263, 2004. 292 • MARCH 2007 • www.ajpregu.org BLOOD PRESSURE REGULATION FOLLOWING SPINAL CORD INJURY 39. Parlow J, Viale JP, Hughson AG, Quintin L. Spontaneous cardiac baroreflex in human; comparison with drugs-induced responses. Hypertension 225: 1058 –1068, 1995. 40. Persson PB, DiRienzo M, Castiglioni P, Cerutti C, Pagani M, Honzikova N, Akselrod S, Parati G. Time versus frequency domain techniques for assessing baroreflex sensitivity. J Hypertens 19: 1699 – 1705, 2001. 41. Pickering TG, Davies J. Estimating of the conduction time of baroreceptors-cardiac reflex in man. Cardiovasc Res 7: 213–219, 1973. 42. Randall DC, Brown DR, Raisch RM, Randall WC. SA-nodal parasympathectomy delineates autonomic contributions to heart rate power spectrum. Am J Physiol Heart Circ Physiol 260: H985–H988, 1991. 43. Reyes del Paso G, Gonzàlez I, Hernàndez JA. Baroreceptor sensitivity and effectiveness varies differentially as a function of cognitive-attentional demands. Biol Psychol 67: 385–395, 2004. 44. Robbe HWJ, Mulder LJM, Ruddel H, Langewitz WA, Veldman JBP, Mulder G. Assessment of baroreceptor reflex sensitivity by mean of spectral analysis. Hypertension 10: 538 –543, 1987. 45. Saul JP, Berger RD, Albrecht P, Stein SP, Chen MH, Cohen RJ. Transfer function analysis of the circulation: unique insight into cardiovascular regulation. Am J Physiol Heart Circ Physiol 261: H1231–H1245, 1991. 46. Sleight P, La Rovere MT, Mortara A, Pinna G, Maestri R, Leuzzi S, Bianchini B, Tavazzi L, Bernardi L. Physiology and pathophysiology of AJP-Regul Integr Comp Physiol • VOL 47. 48. 49. 50. 51. 52. R1157 heart rate and blood pressure variability in humans: is power spectral analysis largely an index of baroreflex gain? Clin Sci (Colch) 88: 103–109, 1995. Task Force of the European Society of Cardiology, and the North American Society of Pacing and Electrophysiology. Heart rate variability standards of measurement, physiological interpretation, and clinical use. Circulation 93: 1043–1065, 1996. Taylor JA, Williams TD, Seals DR, Davy KP. Low frequency arterial pressure fluctuations do not reflect sympathetic outflow: gender and age differenced. Am J Physiol Heart Circ Physiol 274: H1194 –H1201, 1998. Teasell RW, Malcolm OA, Krassioukov A, Delaney GA. Cardiovascular consequences of loss of supraspinal control of the sympathetic nervous system after spinal cord injury. Arch Phys Med Rehabil 81: 506 –516, 2000. Ter Host GJ. The Nervous System and the Heart. Clifton, NJ: Humana, 2000. Wecht JM, De Meersman RE, Weir JP, Spungen AM, Bauman WA. Cardiac autonomic response to progressive head up tilt in individuals with paraplegia. Clin Auton Res 13: 433– 438, 2003. Westerhof BE, Gisolf J, Stok WJ, Wesseling KH, Karemaker JM. Time-domain cross correlation baroreflex sensitivity: performance the EuroBaVar data set. J Hypertens 22: 1371–1380, 2004. 292 • MARCH 2007 • www.ajpregu.org