pain & sports injuries
advertisement

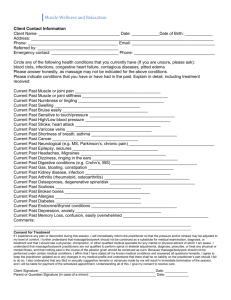
13/05/2012 Pain "an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.“ g PAIN & SPORTS INJURIES Total pain encompasses multidimensional factors It may include all of the following: Intellectual Pain Emotional Pain Interpersonal I l PPain Financial Pain Spiritual Pain Bureaucratic Pain, and Physical Pain (McCaffery, M & Beebe, A. Pain: Clinical manual for nursing practice. 1989. St Luis: CV Mosby Co.) Perception of pain can be subjectively modified (The International Association for the Study of Pain.) Subjective sensation The patient’s experience of pain is expressed within the context of the illness, and the personal, emotional, social, cultural, and spiritual orientation of the individual. Suffering, like pain, is subjective. Suffering is characterised as a person’s evaluation of the significance of an event such as pain - or the meaning of an event in relationship to self and to the quality of life. Pain has a purpose by past experiences & expectations - provoke a withdrawal response thi iis often this ft th the aim i off ttreatment t t - warning i off d danger or harm h “Pain is what the patient says it is, and exists whenever the patient says it does.” (McCaffery & Beebe, 1989) 1 13/05/2012 Components of pain Pain can persist longer than it is useful enhancing disability inhibiting effects to rehabilitate injury eg. prolonged spasm leads to; - decreases circulation - muscle atrophy - disuse habits - conscious / unconscious guarding which can lead to severe loss of function, changed biomechanics, overuse injuries, development of chronic pain and chronic injuries Chronic pain = disease state (cause??) Physical + Psychological components of pain Types of pain Acute Chronic Persistent R f Referred d Radiating Somatic Trigger Point Pain Types of Pain Persistent Pain - Continuing pain Symptom of a treatable condition Types of Pain Acute - of sudden onset - Usually short lived - occurs when tissue damage is impending or after it has occurred - Muscle M l strains, lligament sprains, contusions, surgery Chronic - pain that persists after noxious stimulus has been removed - pain lasting for more than 6 months - defies intervention Types of Pain Trigger Points - hyperirritable points within a taut band of muscle (latent or active) - may refer pain Referred Pain - pain that is perceived to be in an area that seems to have little relation to the existing pathology (either acute or chronic) - outlast causative factors because altered reflex patterns / mechanical stress on muscles, guarding habits or development of T.P.'s Therefore massage treatment must attempt to modify or control pain on all levels - modalities (massage, stretching, exercise, etc) - medication / drug therapy - coping behaviours Radiating Pain - irritation of nerves and nerve root Somatic Pain - associated deep musculature, skin, joints and bone - often a discrepancy b/w site & location of pain and disorder 2 13/05/2012 Tissue Sensitivity & Pain Response Most sensitive to noxious stimuli periosteum and joint capsule subchondral b h d l bone, b tendon, d & liligaments muscle and cortical bone synovium and articular cartilage 1. 2. 3. 4. Tissue Sensitivity & Pain Response Nerve ending: termination of nerve fibre in a peripheral structure Sensory Motor ending (receptor) ending (effector) Several types of sensory receptors Activation of some of these sense organs with therapeutic agents can decrease the perception of pain eg. avulsion # - tear periosteum A nociceptive neuron is one which transmits pain signals the cell body is in the dorsal root ganglion near the spinal cord afferent neurons conduct impulses from the periphery toward the brain efferent neurons (eg. motor neurons) conduct impulses from the brain toward the periphery p p y Nociceptors are stimulated and release a neuropeptide (substance P) this initiates an electrical impulse to be conducted along the afferent fibre to the spinal cord the electrical impulses are sensory messages of pain, warmth, or touch to sensory centres in the brain where they are integrated, interpreted, and acted upon. 2nd Order afferent fibres Carry sensory message from dorsal horn to the brain Nociceptive p specific p Exclusive to noxious stimulation Aδ and C fibres Serve smaller receptor fields From sensory receptor to the dorsal horn Four different types of 1st order neurons; Aα and Aβ Large High Aδ diameter conduction velocity and C fibres Small diameter conduction velocity (aching/ throbbing pain may continue long after stimulus is removed) Low 3rd Order Input from Aβ, Aδ and C fibres Overlapping receptor fields Wide dynamic range 1st Order (Primary Afferents) 3rd order neurons project to sensory cortex and various other centres in the CNS This allows for perception of pain and permits integration of past experiences and emotions, which form our response. All these neurons synapse with 3rd order fibres. 3 13/05/2012 Lateral spinothalamic tract Neurophysiologic Explanations of Pain Control 3 models of analgesic mechanisms response to cutaneous receptor stimulation: 1. Stimulation from ascending Aβ afferents results in blocking of impulses (pain messages) carried along Aδ and C afferent fibres. 2. Stimulation along descending pathways in the dorsal horn of the spinal cord results in a blocking of the impulses carried along the Aδ and C afferent fibres (central biasing). 3. The stimulation of Aδ and C afferent fibres causes the release of endogenous opioids (β-endorphin) into the central nervous system, resulting in an narcotic-like suppression of the central nervous system and a generalised analgesic response. 1. These theories or models are not necessarily mutually exclusive. Pain relief may result from combinations of dorsal horn and central nervous system activity. The "pain message" carried along the smaller diameter fibres is not transmitted to the second order neuron. The pain message never reaches the sensory centres. Balance between input to afferents determines how much pain is blocked or gated eg. Rubbing a contusion, moist heat, or massaging decreases perception of pain. This is attributed to increased stimulation of large diameter afferents Aβ Blocking the Pain Impulses with Ascending Aβ Input Pain modulation due to sensory stimulation and the resultant increases in the impulses in the large diameter Aβ afferent fibres Impulses ascending on Aβ afferent fibres stimulate the substantia gelatinosa as they enter the dorsal horn of the spinal cord. Stimulation of the substantia gelatinosa inhibits synaptic transmission in the Aδ and C fibre afferent pathways. 2. Blocking the Pain Impulses with Ascending Aβ Input Gate Control Theory: (Spinal Level Pain Modulation) Descending Pain Control Mechanisms (Supraspinal Level) The central control originating in higher centres of the CNS could affect the dorsal horn gating process. Impulses from the thalamus and brain stem (central biasing) are carried into the dorsal horn on efferent fibres in the dorsal or dorsal lateral paths. Impulses from the higher centres act to close the gate and block transmission of the pain message at the dorsal horn synapse. Through this system, previous experiences, emotional influences, sensory perception, and other factors could influence the transmission of the pain message and the perception of pain. 4 13/05/2012 Endogenous Opioids in the Descending Pathways Stimulation of the periaqueductal grey region sends impulses along the efferent fibres in the dorsal lateral tract, which synapse with encephalin interneurons. The interneurons Th i release l encephalin h li iinto the h d dorsall hhorn, inhibiting the synaptic transmission of impulses to the second order afferent neurons. Explains the analgesic response to brief, intense stimulation. ie, acupressure, TENS, Trigger Point Therapy Summary The body's pain control mechanisms are probably not mutually exclusive. Rather, analgesia is the result of overlapping processes. Also, these are only models, conceptualisations of how pain relief occurs. They give explanations that assist in understanding the effects of therapeutic modalities and form a rationale for their use or application. Managing Pain 3. β-Endorphin Electro-acupuncture and TENS can cause this release. Pain perception and the response to a painful experience may be influenced by a variety of cognitive processes, including anxiety, attention, depression, past pain experiences, and cultural influences. Mediated by higher centres in the brain. Goals in Dealing with Pain Unidentified pain may hide a serious disorder, and treatment of such pain may delay the appropriate treatment of the disorder. The therapist must match the therapeutic technique for pain control with the situation. A therapeutic agent should not be applied without first developing a clear rationale for the treatment. Prolonged (20 - 40 mins.) C fibre afferent stimulation has been thought to trigger the release of β-Endorphin from the anterior pituitary gland. Cognitive Influences The source of pain must be identified. There is not one "best" therapeutic agent for pain control. β-Endorphin is a neuroactive peptide with potent analgesic affects. Regardless of the cause of pain the aim of treatment is to decrease the pain. Once diagnosed - pain serves little purpose in relation to treatment or rehabilitation other than a guide to treatment delivery or limits of treatment Pain will inhibit massage treatment programs Therefore control acute pain and protect from further injury 5 13/05/2012 Pain and Therapeutic Massage Techniques Massage Technique the application of some form of stress to the body for the purpose of eliciting an adaptive response Therapeutic to be deemed therapeutic the stress applied to the body must be conducive to the healing process of the injury in its current state Summary - PAIN Pain is a response to an injury / noxious stimulus that is subjectively modified by past experiences and expectations. Sports Injury Pain is classified as either acute or chronic and can exhibit many different patterns. Early reduction of pain in a treatment program will facilitate return to movement, exercise an full sports participation Stimulation of sensory receptors via the application of therapeutic massage techniques can modify the athlete's perception of pain. Assessment Ongoing comprehensive assessment is the foundation of effective pain management Including interview, physical h i l assessment,t medications, medical and surgical history, psychosocial measures Pain and Therapeutic Massage Techniques Therapeutic massage techniques do not actually hasten the healing process but attempt to provide the optimal environment for healing to take place The application of thermal, mechanical, electrical or chemical energy to the body. Goal of Pain Assessment to capture the individual’s pain experience in a standardised way to help determine type of pain and possible aetiology to determine d i the h effect ff and d impact i the h pain i experience i has on the individual and their ability to function. basis on which to develop treatment plan to manage pain to aid communication between interdisciplinary team members. Re-Assessment A comprehensive pain assessment should be re-done if there is: a significant change in the pain, any modification difi ti to t the th pain i managementt plan, l or if a new pain has been identified Assessment must determine the cause of pain, effectiveness of treatments and impact on sporting participation for the athlete 6 13/05/2012 Establish a Plan includes physical, psychological, and behavioural interventions includes treatments and selection of analgesia/adjuvants which are individualised and consistent with the athlete’s goals for pain relief. These goals may also relate to: o maintenance of training / sporting involvement o acceptable competitive involvement o quality of sporting / competitive life o capacity for adequate rest and sleep o medication side effects minimal or at least tolerable Assess and document the effectiveness of the plan on an ongoing basis Education Some athletes may under report pain Have not been taken seriously in the past Fear being labelled a “wimp” Want to appear stoic, an important characteristic in most sports Expect pain with training / competition (pain should be viewed as common but not a normal) Choose to avoid medications (especially if banned as part of competition) Education for athlete should occur regarding these concerns to ensure they report their pain in a trusting and caring environment. Include the athlete, trainer and coaches and family in decision making to determine a treatment plan that meets the athlete’s wishes, emphasising the shared goals of care. Pain Severity Scales Assessment of pain severity on a scale of 0-10 using a pain scale would be the minimum assessment to be completed to monitor effectiveness of treatment in decreasing patient’s pain Use of a standard pain scale matched to the patient’s cognitive and communication abilities Visual Analogue Scale (VAS) Numeric Rating Scale (NRS 0-10) Faces Scale Body maps Pain Charts Verbal Scale ALL Pain assessments should be documented It is important to explain to the athlete that pain may get worse as the injury and treatment progresses Discuss the concept of pain management with the athlete in an effort to lessen the p pain experience p before pain becomes difficult to manage. Teach athlete to report changes in pain, pain that is new, and pain that does not improve after treatment Pain Assessment Scales Pain is a complex phenomenon that is difficult to evaluate and quantify because of its subjective nature and it is influenced by the attitudes and beliefs of the therapist and the athlete Visual Analogue Scales Quick and simple Client required to mark the line at the point corresponding to the severity of the pain. A similar scale can be used to assess treatment effectiveness. Scales can be completed daily or used as pre and post treatment assessments 7 13/05/2012 VAS Numeric Pain Scale Client asked to rate his/her pain on a scale from 1 to 10 with 10 representing the worst pain s/he has experienced or could imagine. Asked before and after treatment When the treatment offers pain relief the client is asked about the h extent and d duration d off pain relief. l f Also could ask - portion of the day that they experience pain relief - specific activities that offer relief - sleep patterns in the last 24 hours - medication required (amount) NRS Therefore can assess pain and any changes to pain with regard to treatment. Faces / Numeric scale Athlete circles which one is appropriate Body Map Place a number (eg 1, 2, 3 on the body indicating the locations of pain / discomfort Use 1 for worst pain and 2 for next pain etc. In the order of how distressing each pain is 8 13/05/2012 Pain Charts Can be used to determine spatial properties of pain. Used to assess location and number of subjective components. Different colours or patterns can be used to define different types of pain or pain sensations Descriptions can be added to enhance the communication. Pain Words Words the athlete uses to describe pain / discomfort Discomfort Pins & needles Shooting Constant Dull ache Stabbing Electric like Occasional Sharp Cramping p g Surface Burning Throbbing Deep Other The McGill Pain Questionnaire (MPQ) A tool with words to describe pain. 20 sets of 4 categories of words representing the pain experience. 20 minutes to complete - can be frustrating from a language point of view. Commonly used for clients with low back pain. Can demonstrate changes in status quite clearly (when administered every 2-4 weeks) Activity Pattern Indicators Profile 64 question, self-report tool that may be used to assess functional impairment associated with pain. The instrument measures the frequency of certain behaviours such as work,, housework,, recreation and social activities. Non-Verbal Pain Indicators Verbally excessive Moans / sighs Weeps /cries C i outt when Cries h moved Grimaces / grunts Rubs body part Restless Rocks Guards Retracts H ld body Holds b d partt Fidgets Resistive to touch Lethargic 9 13/05/2012 Other symptoms General Has the pain / discomfort or treatment produced any other symptoms Nausea Drowsiness Change in mood Loss of appetite Dizziness Disturbed sleep Diarrheoa Unclear thinking Constipation Anxiety Other Often in a long recovery clients lose sight of the progress made in terms of functional activities. A review of the pain scales can reassure the client and foster a more positive outlook, or reinforce the commitment to the plan of treatment. Role of massage treatment in sports injuries The therapist employs massage techniques to create an optimum environment for tissue healing minimising i i i i th the symptoms t associated i t d with ith neuromuscular pain while hil THE HEALING PROCESS – SPORTS INJURIES Understanding the Healing Process Pain and the healing process Recognition of signs and symptoms Awareness of timeframes associated with the healing process of various types of tissue. Knowing as much as you can about the healing process is important in developing a safe and effective massage treatment Performing a massage technique before the injured area is ready to tolerate that level of stress can impede healing and cause additional injury You have a duty to understand healing and realise the impact of therapeutic massage 10 13/05/2012 Repair vs Regeneration Most healing results in scar tissue formation Primary and Secondary Healing Dependent on the extent of injury of the wound site’s ends approximation Tissues in the body can regenerate themselves? Healing by Primary Intention If separation is small, a bridge of cells binds the ends together eg. Minor wounds, surgical incisions Understanding the Healing Process Healing by Secondary Intention severe wounds where stump ends are further apart and cannot be bridged Wound W d hheals l by b producing d i scar tissue ti Heals from the bottom and sides of the wound to fill in the space created by the wound eg. 2° ligament sprain Tissue is torn but not surgically repaired Takes longer and results in a larger scar More Primary Injury Described as either chronic or acute Macrotraumatic injuries Result of acute trauma Produce immediate pain and disability Fractures, dislocations, sprains, strains Programs must be based on healing process framework Phases Inflammatory Fibroblastic-repair Maturation-remodelling No definitive beginning or end Inflammatory Response Phase Injury results in altered cellular metabolism and chemical mediators Macroscopic characteristics Microtraumatic injuries Swelling S lli Overuse injuries, resulting from repetitive overload, incorrect mechanics Tendinitis, tenosynovitis bursitis Tenderness Secondary injury Redness Increased temperature Initial response is critical in healing process Inflammatory or hypoxia response 11 13/05/2012 Fibroblastic-Repair Phase Chronic Inflammatory Response Chronic inflammation Fibroplasia Active scar formation last 4-6 weeks Signs and symptoms will subside b d Endothelial capillary buds develop allowing for aerobic healing Increased blood flow for nutrient delivery Occurs when acute inflammation does not eliminate injuring agents and restore normal physiological state Leucocytes are replaced with macrophages, lymphocytes and plasma cells Specific mechanism is unknown May Overuse and overload related No specific time frame in which acute becomes chronic inflammation Resistant to physical and pharmacological agents Introduction of non-steroidal anti-inflammatory drugs (NSAID’s) Maturation-Remodelling Phase Role of Massage Realignment of collagen Bone and soft tissue will respond to physical demands placed upon them Remodelling and realignment Continued breakdown and synthesis of collagen Increased stress and strain results in increased collagen realignment Nonvascular, contracted, strong, firm scar present after 3 weeks Scar formation Revascularisation Muscle regeneration and fibre reorientation Tensile properties Corticosteroids Keloids and hypertrophic scars Infection Humidity, climate, and oxygen tension Health, age, and nutrition Progressive and controlled massage techniques allows for gradual return to normal levels of function Sports Injury to Various Tissues Factors that Impede Healing Extent of Injury Oedema Haemorrhage P Poor V Vascular l SSupply l Separation of tissue Muscle spasm Atrophy Initial immobilisation is necessary y Controlled mobilisation enhances Maturation may require several years to complete Wolff’s Law Ligament Sprains Sprains involve damage to a ligament Li Ligaments Inelastic band of tissue Provides joint stability, controls bone position during joint motion, provides proprioceptive input 12 13/05/2012 Ligament Healing Sports Injury to Various Tissues Grades of Ligament Sprains Grade I - some pain, minimal loss of function, no abnormal motion, and mild point tenderness Grade II - pain, moderate loss of function, swelling, and instability Grade III - extremely painful, inevitable loss of function, severe instability and swelling, and may also represent subluxation Factors Affecting Ligament Healing Surgically repaired extra-articular ligaments Intra-articular ligament damage Injuries to Musculo-tendinous Structures Results in synovial fluid presence, diluting haematoma, disrupting clot and healing Strains occur when the musculo-tendinous unit is: Overstretched Forced to contract against too great a resistance Muscle Strain Classifications Skeletal muscle exhibits 4 traits Elasticity Extensibility Irritability Contractility Muscle size and architecture often contribute to type and magnitude of motion (gross vs. fine, powerful vs. coordinated) Ligament healing and immobilisation Muscle strength training can enhance joint stability Muscle Strains Ligaments sprained extra-articularly result in bleeding in the subcutaneous space p Intra-articular ligament sprains result in bleeding within the capsule Vascular proliferation, fibroblastic activity and clot formation occur during the initial 6 weeks of recovery Collagen and ground substance work to bridge torn ends of ligaments via scarring Scar maturation will gradually occur and collagen tensile strength will increase Heal with less scarring Stronger than un-repaired ligaments Heal via fibrous scarring resulting in ligament lengthening and increased joint instability Follows same course of repair events as with other vascular tissues Non-surgically repaired ligaments Damage occurs Muscle Tendon Musculo-tendinous junction Tendon-bone interface Grade I : G d II: Grade II some fibres have been stretched or actually torn resulting in tenderness and pain on active ROM, movement painful but full range present number of fibres have been torn and active contraction is painful, usually a depression or divot is palpable, some swelling and discoloration result Grade III: Complete rupture of muscle or musculotendinous junction, significant impairment, with initially a great deal of pain that diminishes due to nerve damage 13 13/05/2012 Muscle Healing Similar healing to other soft tissues Haemorrhaging and oedema lead to phagocytosis Fibroblasts and ground substance produce a gel-like matrix leading to fibrosis and scarring Myoblastic cells infiltrate the region promoting myofibril regeneration Collagen undergoes maturation – with active contractions being critical to apply tensile stress Lengthy recovery for each grade Patience is a must Chronic Tendinitis Tendon degeneration Loss of normal collagen and cellularity No inflammatory cellular response Signs and symptoms Tendinitis Pain with movement Swelling Crepitus Large amounts of collagen are required for adequate healing However, collagen synthesis can become excessive resulting in fibrosis and interfering with tendon sliding action Scar tissue will gradually elongate allowing for appropriate tendon motion If a synovial sheath surrounds an injured tendon the injury could be devastating Typical tendon healing may require 4-5 weeks before strong contractions can be imparted on tendon Due to friction and decreased space for sliding synovial sheaths are necessary in tendons Overuse results in inflammation and development of sticky ti k adhesions dh i within ithi th the sheath h th Signs and symptoms Similar to tendinitis Movement may be more limited with tenosynovitis Treatment is the same as if treating tendinitis NSAID’s and modalities Alternative activities Tendon Healing Degenerative tendon changes with no clinical or histological signs of inflammation Tenosynovitis Key treatment = rest Additional treatment options Inflammation of tendon outer layer Friction injury Tendinosis Inflammation of tendon, with no involvement of paratenon Paratenonitis Term used to describe multiple pathological tendon conditions Injury to Nerve Tissue Generally involve contusion or inflammation More severe injuries involve crushing or severing Causes life-long disability Paraplegia p g or quadriplegia q p g 14 13/05/2012 Injury to Nerve Tissue Peripheral nerves can regenerate if injury does not impact cell body Injury to Nerve Tissue New axon buds will develop on the proximal axon One sprout will form new axon Contact with Schwann cells will allow for Schwann cell proliferation = new myelin Slower regeneration with proximity to cell body Regeneration g requires q an optimal p environment Degenerative changes occur Increased metabolism and protein production for regeneration While cell body contains genetic material necessary to maintain axon it does not transmit to distal segments of axon Schwann cells Regeneration is slow Additional Musculoskeletal Injuries Bursitis Dislocations and Subluxations Dislocations present with total disunion of bone apposition between articular surfaces- requiring manual or surgical realignment High level of incidence in fingers and shoulder Subluxations are partial dislocations causing incomplete separation of two bones Reduction should not occur without an X-ray (necessary to rule out fractures) Inappropriate reduction may complicate the injury Return to play is largely governed by the degree of soft tissue injury Muscle Soreness Overexertion in strenuous exercise resulting in muscular pain Two types of soreness pain that occurs 24-48 hours following activity that gradually subsides Caused by slight microtrauma to muscle or connective tissue structures Gradual build-up of intensity Some form of stretching May y continue to become inflamed with repeat p irritation with increasingly more pain Commonly impacted bursa Pre-patellar Olecranon Subacromial Contusions Result of sudden blow to body Can be both deep and superficial Haematoma results from blood and lymph flow into surrounding tissue Localisation of extravasated blood into clot, encapsulated by connective tissue Speed of healing dependent on the extent of damage accompanies fatigue, muscle pain experienced immediately after exercise Prevention and treatment Delayed-onset muscle soreness (DOMS) Result of excessive movement or trauma to bursa Causes irritation, inflammation and increased synovial fluid production Acute-onset Acute onset muscle soreness CNS nerves regenerate poorly due to lack of connective tissue support If cut contacts Schwann cells re-innervation of distal segments is more likely Occurs at a rate of 3-4 mm per day Can be obstructed by scar formation If muscle damage occurs ROM will be impacted Incidents of repeated blows may result in myositis ossificans development Prevention = rest and protection Allow for calcium re-absorption 15 13/05/2012 Classification of injury Considerations of the Healing Stage Classification of an injury should be made according to the existing signs and symptoms that include the various stages of the healing process and not according g to time frames or mechanisms of injury. j y Phase 1: Acute Injury Phase Phase 1: Acute Injury Phase SSx includes the classic symptoms of tenderness, swelling, redness, increased temperature, loss of function and p pain. Goals Control but not eliminate the amount of active inflammation Contain the original injury by reducing the secondary hypoxic reaction Control oedema and spasm Control pain If active inflammation is present , even after several months, the injury should be considered acute and must be treated accordingly. Phase 1: Acute Injury Phase Phase 1: Acute Injury Phase Modalities R.I.C.E Cold modalities are used to reduce the amount of secondary hypoxic injury, reduce pain and eliminate spasm. Compression devices and elevation are used to encourage venous and lymphatic return. Immobilisation devices are used to limit ROM. Electrical stimulation may assist in decreasing vascular permeability, limiting the amount of oedema formed and help reduce pain. Use of NSAID’s Exercise in the form of gentle pain-free ROM and possibly isometric exercises within the patient's pain tolerance Based on this definition of acute and chronic injury the massage treatmnet progression may be determined by the three phases of healing and may show h extreme variation between individuals If the therapist is too aggressive during the first 48 hours the inflammatory process may not have time to accomplish what it needs to Immobilisation for 24-48 hours is a must. By days 3-4 the patient should be engaged in some form of mobilising massage and should be encouraged to gradually bear weight if it is a lower extremity injury 16 13/05/2012 Massage Treatment Phase 2: Repair Phase Goals Assist the body in delivering nutrients and materials necessary to repair the injured tissues Assist in removing the inflammatory debris Increasing blood flow to and from the injured tissues As the inflammatory process has subsided and pain decreases massage should be added with an aim to; Restore full ROM Realign scar tissue to increase strength Re-establish neuromuscular control Phase 2: Repair Phase Massage Treatment Modalities Continued massage use for pain modulation and swelling control Cryotherapy / ? Heat ? Longitundinal pressure to stretch the tissues, prevent shortening of the fibres and encourage the alignment of collagen along the lines of stress. Low-intensity tension is placed on the structures to slowly increase their tensile strength and to assist in the formation of proprioceptive nerves. Proprioceptive activities and muscle re-education movements to help protect the scar. Newly formed capillary buds are fragile so care must be taken not to damage them through excessive pressure, movement or increased tension. Phase 3: Maturation/ Remodelling Phase Goals Modalities Longest phase with the ultimate goal being return to playy p Continued Pain Phase 3: Maturation/ Remodelling Phase collagen realignment continues to decrease with activity Regain sports-specific, ADLs, workplace skills Functional testing Determine specific skill weakness Heating Massage therapy Increase circulation in deeper tissue Reduce guarding, spasm, pain Enhanced blood and lymphatic flow will deliver essential nutrients and increase breakdown/removal of waste, respectively Dynamic sports activities Sports - directed strengthening activities 17 13/05/2012 Massage Treatment Approach to the Healing Process Assist the natural process of the body while doing no harm Primary goals Have a positive influence on inflammation and repair process Expediate recovery of function Minimise early effects of inflammatory process Prevent recurrence of injury ROM, strength, cardiorespiratory fitness, neuromuscular control Pain, spasm, oedema accumulation, decreased motion Resist future periods of tissue overload through strengthening PAIN AND SPORTS INJURIES ASSESSMENT & TREATMENT The efficacy of many of the treatments used by sports/rehabilitation therapists has not been fully substantiated. These scales are one source of data that can help the therapist identify the most effective approaches to managing common injuries. Deborah A. Pascoe These assessment tools can also be useful when reviewing a client’s progress with their doctor or third party payers. Workshop Aim This workshop will explore techniques to measure pain during the assessment and treatment of some of the more common sports injuries PhD scholar, MA Grad Dip Ex Rehab, B App Sc (PE) Cert Hydro Dip Rem Mass Cert Sports Cert Relax. Overview Assessment of the pain associated with different sports injuries Discussion and practice of the most appropriate treatment strategies for the respective tissue(s) and stage(s) of healing Contractile Tissue - Muscle and tendon Non-contractile Tissue (inert structures) Ligament, fascia, joint capsule, cartilage, nerve, skin, blood vessels, bone. Use of pain measures to monitor healing and effects of treatment Massage and other soft tissue techniques in the treatment of sports injuries 18 13/05/2012 Assessment of tissues affected by sports injuries Assessment of Sports Injuries Contractile Tissue Muscle and tendon Observation AROM RROM PROM Special Tests Functional Testing – sports specific skills Palpation Non-contractile Tissue (inert structures) Ligament, fascia, joint capsule, cartilage, nerve, skin, blood vessels, bone. Active ROM Pain /NO Pain End-feel Radiating / defining Compare passive ROM to AROM. Describe the end-feel Soft, firm, hard, or empty. Springy, Springy muscle guarding guarding, muscle spasm spasm, muscle spasticity, abnormal. Determine the stage of pathology by observing when the pain is experienced relative to the ROM. Is the pain or muscle guarding experienced Passive ROM Record using the following grades: Ankylosed Hypomobile / Considerable limitation Slight limitation Normal Hypermobile / Slight increase Considerable increase Unstable before the end feel (acute) concurrent with the end feel (sub-acute) after application of over-pressure (chronic)? Resisted Tests Determine the stability and mobility of the joint. Assessment Plan Passive ROM Because both contractile and inert structures are influenced by active ROM, specific pain response(s) will not be limited or isolated to one tissue Note: abnormal movement any experience of pain any changes in sensation Subjective Objective 0 1 2 3 4 5 6 Note whether there is a painful arc in either active or passive ROM A painful arc indicates some sensitive structure is being pinched at that part of the ROM. Resist the related muscles so that they contract isometrically in the mid-range to determine whether there is pain or decreased strength Mid-range g isometric contractions are used for minimal movement or stress on non-contractile structures around the joint or if pain is severe Initially tests performed on groups of muscles then if a problem is noted each muscle potentially involved is isolated and tested Note individual pain response to determine extent of injury 19 13/05/2012 Assessment of Muscles & Tendons Assessment of Inert Structures Muscle & tendon - Active ROM Resisted ROM Passive ROM Shorten = contract Shorten = contract Lengthen = stretch Non-contractile Tissue (inert structures) Ligament, fascia, joint capsule, cartilage, Pain and / or weakness AROM - pain/weakness mid-range RROM - increase pain/weakness response PROM - only at end ROM (stretch / tightness) Assessment of Inert Structures PROM - stability & mobility - compression - distraction - gliding Special Test - stability & mobility Functional / Sports Specific Tests End Feels for passive ROM Normal End-points End Feels for passive ROM Abnormal End-points Loose Occurs in extreme hypermobility. Capsular p feel An abrupt, hard, firm end-point where two hard surfaces come in contact with one another. Bone to Bone A distinct and abrupt end-point where two hard surfaces come in contact with one another. Muscular Springy feel with some associated discomfort. Nerve Injuries & pain Injury indicated by Muscular Empty feel Movement is definitely beyond the anatomical limit, and pain occurs before end of range or not at all. Spasm Involuntary muscle contraction that prevents motion because of pain; should also be called guarding. Soft Tissue Approximation Soft and spongy, a gradual painless stop. Changes weakness (AROM & RROM) in sensation (palpation, sensation testing) Reflexes Percussion Stretch / elongation Compression Springy Block A rebound at the end-point. 20 13/05/2012 Nerve Tests for Sports Injuries Slump Test – sciatic nerve ULTT / quick test – thoracic outlet Tinel’s sign – ulna, median Piriformis syndrome Median nerve entrapment Ulna nerve palsy Subluxed ulna nerve Peroneal nerve palsy Disc related radiating pain Vascular Injuries Generally caused by compression Decreased pulse (rate and volume) Discolouration Pain associated with changes in sensation Pain associated with Swelling Thoracic outlet syndrome Compartment syndromes Palpation Usually performed following tests of provocation in order not to increase the irritability of the structures prior to testing. Massage Treatment of pain caused by sports injuries Skin and subcutaneous tissue (temperature, texture and crepitus) p ) Muscles, tendons and attachments (tenderness, trigger points and contractures) Tendon sheaths and bursae (tenderness, temperature and crepitus) Joints (effusion, tenderness, changes in position or shape, ligaments) Nerves and blood vessels (neuroma and pulse) Treatment of pain caused by sports injuries Role of Massage and choice of therapeutic technique Treatment of tissues affected by sports injuries Contractile Tissue - Muscle and tendon Non-contractile Tissue (inert structures) Ligament, fascia, joint capsule, cartilage, nerve, skin, blood vessels, bone. Muscles Ligaments Fascia Joint capsule Skin & adipose Bone Nerve = progressive deep muscle massage = deep transverse frictions = myofascial release = deep transverse frictions = rolling & wringing = mechanical stress and pressure = positioning / fascial stretching The therapist employs Massage and other soft tissue techniques to Decrease pain symptoms an optimum environment for tissue healing Minimising the symptoms associated with treatment of soft tissue / neuromuscular pain Create 21 13/05/2012 Pain Symptoms of Sports Injuries Swelling Inflammation (chemical release) M l SSpasm Muscle Muscle and/or joint dysfunction / injury Soft Tissue Oedema – arterial effusion Clinical Decision Making Phases of Injury Healing Continuum Acute Injury / Inflammatory Response Phase Fibroblastic Repair Phase M t ti – Remodelling Maturation R d lli Ph Phase What are massage and other soft tissue technique’s biophysical effects? Pain symptoms and testing indicates what structures are injured? Contractile Non-contractile (inert) What structures are affected? What Phase of Injury – Healing? Depth of Penetration Ti Tissue Affinity Affi it Resources available – your knowledge, skill and confidence? What are the parameters which guide massage and other soft tissue technique’s application Direct Effects Indirect Effects What are the massage and other soft tissue technique’s Indications? What are the massage and other soft tissue technique’s Contraindications? Choice of massage and other soft tissue technique’s Dosage, Duration, Frequency 22 13/05/2012 Massage Techniques for Pain Positioning Pain Relieving and Superficial to deep In accordance with the phase of healing (as needed) Balance Techniques for each area / muscle General Massage Techniques (Effleurage, Petrissage, Longitudinal, Cross-fibre, Attachments) Deep p Tissue Techniques q – including g on stretch Trigger Points – with movement Myofascial release – with movement Frictions – longitudinal & transverse Stretching – static, PNF Exercise prescription Any movement or massage technique that causes the pain to radiate or spread over a large area should not be included during treatment Principles of Massage Treatment General Massage Treatment Developing a strategy - Strong and weak - Long and short Stretch – to maintain and enhance effects of treatment Exercises – to help balance strength and length Sports – advice on sports movements to enhance injury healing and movements to avoid Contraindications / Precautions of Treatment GOALS of ALL TREATMENT A useful strategy for all treatments is to identify the involved section, treat it and then treat the sections above and below it. Myositis ossificans Inflammation (unresolved or worsening) Increasing or Unrelieved Pain Continued restriction in soft tissues Identified restrictions in other tissues Minimise Inflammation Promote Healing Prevent Re-injury Maintain Fitness M i i SStrengthh Maintain Restore Muscle Balance Restore Proprioception Decrease Pain Reduce Swelling Restore ROM (active, resisted & passive) Return to full training and sports competition 23 13/05/2012 Ongoing Treatment Teach management of injury to avoid recurrences of problems Educate client in preventive stretches and exercises for relief of musculoskeletal stress in sports p activities Help client recognise sports techniques that influence risk of injury Sport Injuries & Massage Therapy Injuries which occur during sports participation include injuries from both internal and external trauma. Massage therapists must be able to identify and assess the extent and severity of the injury, tissue(s) which have been damaged, and stage of healing and select an appropriate treatment protocol to enhance recovery and return to sport. Complementary Treatment Techniques Cold Heat Other Massage Techniques St t hi Stretching Strengthening Exercises Pilates Feldenkrais TREATMENT OF SPECIFIC SPORTS INJURIES Deborah A. Pascoe PhD scholar, MA Grad Dip Ex Rehab, B App Sc (PE) Cert Hydro Dip Rem Mass Cert Sports Cert Relax. Sports Injury Pain – Specific Treatments Delayed onset muscle soreness (DOMS) / (EIMS) Quadriceps contusion Knee ligament sprains Achilles tendinosis Rotator cuff (impingement) ITBFS / fascial tightness Hamstring strain Muscle cramps Plantar fasciitis Shin Splints / MTSS Lateral epicondylitis 24