RESPIRATORY SYSTEM Necessities: 1. Large surface area 2. Moist
advertisement
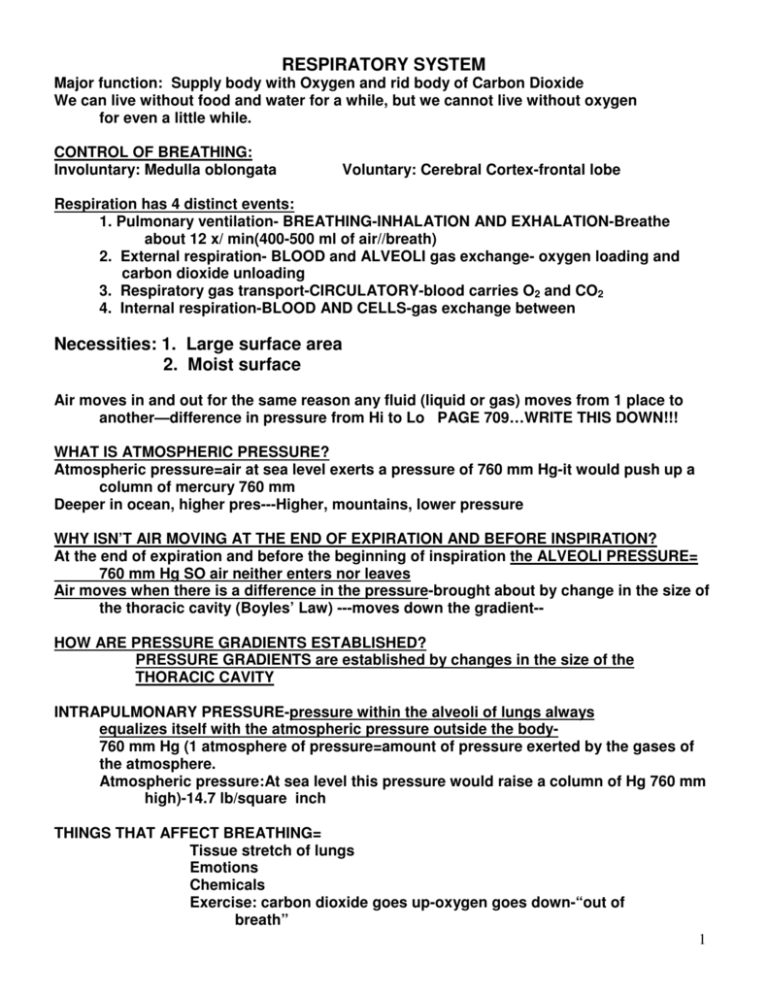
RESPIRATORY SYSTEM
Major function: Supply body with Oxygen and rid body of Carbon Dioxide
We can live without food and water for a while, but we cannot live without oxygen
for even a little while.
CONTROL OF BREATHING:
Involuntary: Medulla oblongata
Voluntary: Cerebral Cortex-frontal lobe
Respiration has 4 distinct events:
1. Pulmonary ventilation- BREATHING-INHALATION AND EXHALATION-Breathe
about 12 x/ min(400-500 ml of air//breath)
2. External respiration- BLOOD and ALVEOLI gas exchange- oxygen loading and
carbon dioxide unloading
3. Respiratory gas transport-CIRCULATORY-blood carries O2 and CO2
4. Internal respiration-BLOOD AND CELLS-gas exchange between
Necessities: 1. Large surface area
2. Moist surface
Air moves in and out for the same reason any fluid (liquid or gas) moves from 1 place to
another—difference in pressure from Hi to Lo PAGE 709…WRITE THIS DOWN!!!
WHAT IS ATMOSPHERIC PRESSURE?
Atmospheric pressure=air at sea level exerts a pressure of 760 mm Hg-it would push up a
column of mercury 760 mm
Deeper in ocean, higher pres---Higher, mountains, lower pressure
WHY ISN’T AIR MOVING AT THE END OF EXPIRATION AND BEFORE INSPIRATION?
At the end of expiration and before the beginning of inspiration the ALVEOLI PRESSURE=
760 mm Hg SO air neither enters nor leaves
Air moves when there is a difference in the pressure-brought about by change in the size of
the thoracic cavity (Boyles’ Law) ---moves down the gradient-HOW ARE PRESSURE GRADIENTS ESTABLISHED?
PRESSURE GRADIENTS are established by changes in the size of the
THORACIC CAVITY
INTRAPULMONARY PRESSURE-pressure within the alveoli of lungs always
equalizes itself with the atmospheric pressure outside the body760 mm Hg (1 atmosphere of pressure=amount of pressure exerted by the gases of
the atmosphere.
Atmospheric pressure:At sea level this pressure would raise a column of Hg 760 mm
high)-14.7 lb/square inch
THINGS THAT AFFECT BREATHING=
Tissue stretch of lungs
Emotions
Chemicals
Exercise: carbon dioxide goes up-oxygen goes down-“out of
breath”
1
4 IDEAL GAS LAWS----WHY “IDEAL”?
Ideal-gas whose molecules are so far apart they rarely collide with each other
Gas pressure-molecules collide with walls of container and exert force (pressure—
FACTORS THAT AFFECT GASES???? (1) PRESSURE (2) TEMPERATURE
(3) IF THE GAS IS A MIXTURE=SUM OF PRESSURE OF ALL GASES
(4) SOLUBILITY OF GASES
THE CHEST IS THE CONTAINER FOR THE RESPIRATORY SYSTEM
1. BOYLE’S LAW
Gas’ volume is INVERSELY proportional to its pressure when held at a
constant temperature P1V1=P2V2
When the volume of a container (the chest) goes up, pressure goes down,
When the volume of a container (the chest) goes down, pressure goes up
APPLICATION:
When the volume of the thorax increases, (diaphragm-Phrenic Nerve,
intercostals-Intercostal nerve),
the pressure decreases and is lower than atmospheric pres=
(760 mm Hg) so air from outside->into the airways (inspiration)
expiration–opposite occurs
2. CHARLES’ LAW
Gas volume is DIRECTLY proportional to temperature when pressure is held
constant-also, pressure is directly proportional to temperature when
volume is held constant SO Pressure and Volume Directly Proportional
to Temp when the other is held constant
APPLICATION:
During INSPIRATION air expands in volume as it is warmed by respiratory
mucosa
3. DALTON’S LAW (LAW OF PARTIAL PRESSURES)
The total pressure exerted by a mixture of gases (such as air) is equal to the
sum of the pressures of each individual gas
Partial pressure=pressure each gas in a mixture exerts is directly
proportional to its % in the total gas mixture—
Air
N2 =78.6 %
O2=20.9 %
CO2=.04 %
H2O=.046 %
X 760=P…
So multiply these % X 760 mm Hg to get PO2 etc of each
Partial pressure of oxygen is directly proportional to its percentage in the total
gas mixture-Oxygen makes up about 21% of the atmosphere-has a
PO2=0.21 x 760 = 159 mm Hg
At high altitudes where atmosphere is less influenced by gravitational
pull, all partial pressures decline in direct proportion to the decline
in atmospheric pressure
Below sea level atmospheric pressure increases by 1 atmosphere for
each 33 feet of descent so at 99 feet below sea level, the total
pressure on the body is = to 4 atmospheres or 3040 mm Hg-so
partial pressure of each gas is also multiplied
2
PO2 PCO2=partial pressure
Determined by its concentration or % of the mixture—O2=21% so
atmospheric PO2=.21 X 760=159.6 mm Hg
APPLICATION:
Used for determining direction of diffusion if know Partial Pressure of each gas
Also, used for determining the pressure of oxygen in air we breathe
4. HENRY’S LAW
The concentration of a gas in a solution depends on the PARTIAL PRESSURE
of the gas and its SOLUBILITY as long as the temp remains constant
when a mixture of gases is in contact with a liquid each gas will dissolve
in the liquid in proportion to its partial pressure and its solubility in the
liquid
CO2 is most soluble in plasma
O2 is relatively insoluble-so needs pigment to carry-Hb
N2 is least soluble
APPLICATION:
The amount of gas dissolved in the PLASMA relates to Henry’s Law
Oxygen Toxicity
Although breathing oxygen at 2 atmospheres presents no problems for short
periods of time, oxygen toxicity develops rapidly when the PO2 is
greater than 2.5-3 atmospheres-excessive oxygen concentrations
generate large amounts of harmful free radicals causing profound
central nervous system disturbance resulting in coma and death
Even though 80% of air is N2 it has little affect on the body because nitrogen is very
insoluble in blood, HOWEVER when a deep sea diver breathes under
HYPERBARIC (high pressure) conditions more nitrogen gas (80% of gases in air)
dissolves in the blood and causes nitrogen narcosis->dizziness, drowsiness,
giddiness, and other symptoms similar to alcohol intoxication (“RAPTURE OF THE
DEEP”)
If a diver ascends to surface gradually the dissolved nitrogen gas can be eliminated
by the lungs without problems but if ascent is rapid, the nitrogen forms large
gas bubbles in blood causing an embolus (can be moving clot or in this case a gas)
If bubbles occur in the tissue, it causes excruciating pain-commonly called the
BENDS–more accurate: DECOMPRESSION SICKNESS
Like gas boiling out of solution in body fluids (not very soluble in body fluids so eager to
get out)-and can damage the brain
3
INSPIRATION-breathe in
Quiet inspiration:Diaphragm (Phrenic nerve) and external intercostal muscles
(Intercostal/vagus nerve)cause thorax volume to increase
Forceful inspiration: Diaphragm, external intercostals, sternocleidomastoid,
pectoralis minor, and serratus anterior muscles cause thorax volume to
increase
As the size of the thorax increases, intrapleural /intrathoracic/intraalveolar pressure
decreases and inspiration occurs
Just before inspiration is beginning the intrathoracic pressure is about 4 mm Hg less
than atmospheric pressure
As the thorax enlarges it pulls the lungs along with it because of the COHESION
between the moist pleura covering the lungs and the moist pleura lining the
thorax
When all of this occurs, the air pressure inside the lungs is less than atmospheric
pressure and the air rushes in
Then the tendency of the thorax and lungs to return to their preinspiration volume is
a physical phenomenon called ELASTIC RECOIL
(REPEAT:::::During inspiration COHESION occurs between moist pleura covering
lungs and moist pleura lining the thorax and pulls the lungs along with it as
it moves out
During expiration ELASTIC RECOIL-natural tendency of lungs to contract
GO TO PICTURE AT TOP OF 711
Explain inspiration and expiration using these numbers for intraalveolar pressure
(Pressure=757 and 763)
EXPIRATION-breathe out—passive process
Inspiratory muscles relax-size of thorax decreases so intrathoracic/intrapleural pres
goes up
NEGATIVE PRESSURE BREATHING:
NEGATIVE PRESSURE-less than atmospheric
ALWAYS NEGATIVE BETWEEN PARIETAL AND VISCERAL PLEURA TO PREVENT
COLLAPSE OF LUNGS:
NEGATIVE PRESSURE-Super important to understand!!!
The intrapleural pressure in the intrapleural space is always about
4 mm Hg less than the pressure in the alveoli and is said to be
negative relative to both the intrapulmonary and atmospheric
pressures
NEGATIVE PRESSURE results from 2 groups of factors:
those factors acting to hold the lungs to the thorax wall -Cohesion
1. those factors acting to pull the lungs away from the thorax wallRecoil/surface tension of the alveoli
The negative pressure is required to overcome 2 factors that would cause collapse of
lungs
NEGATIVE PRESSURE MUST:
(1) Overcome collapse tendency of lungs caused by surface tension of fluid
lining of alveoli (bugs walk on water-mol attracted to each other)
(2) Overcome tendency of elastic fibers constantly attempting to recoil
4
COMPLIANCE-ability of lungs and thorax to stretch-essential to normal respiration
THE IMPORTANCE OF THE NEGATIVE PRESSURE IN THE INTRAPLEURAL
SPACE AND THE TIGHT COUPLING OF THE LUNGS TO THE THORAX
WALL CANNOT BE OVEREMPHASIZED......
ANY CONDITION THAT EQUALIZES THE INTRAPLEURAL PRESSURE WITH
THE INTRAPULMONARY OR ATMOSPHERIC PRESSURE CAUSES
IMMEDIATE LUNG COLLAPSE!!!!!
PULMONARY VOLUME-very important
SPIROMETER-used to measure-PICTURE SHOWN ON 714
Tidal Volume/TV=typical in and out---+500 ml x 12/min
Expiratory Reserve Volume/ERV=amount you can force out after normal exp +1000 ml
Inspiratory Reserve Volume/IRV= amount you can force into lungs after TV-force in—
+3000 ml
Residual Volume/RV=Can not force all air out of lungs-this is the amount always left
in lungs —+1200 ml
“Wind knocked out”=ERV and some RV knocked out and even a few alveoli collapse
SO must re-inflate lungs--- requires EFFORT…still spongy and will float even
after RV forced out because of the trapped air called minimal volume 40%RV
PNEUMOTHORAX-RV eliminated and lung collapses
Vital Capacity/VC=IRV + ERV + TV 4500-5000 ml {largest volume of air that can be
moved in and out of lungs-measures largest possible EXPIRATION after
largest possible INSPIRATION): Depends on:
(1) Size of thoracic cavity
(2) Posture
(3) Volume of blood in the lungs-if more blood than normal
encroaches on alveolar air space-Important in congestive
heart failure
(4) Excess fluid in pleural or abdom cavities decreases VC and
so does Emphysema-walls stretched-lose elasticity and
can’t recoil so increases the RV-Also walls break down}
TLC= IRV + ERV + TV + RV 5700-6200 ml
TLC=VC + RV
ANATOMICAL DEAD SPACE-volume of air in nose, pharynx, larynx, trachea, and
bronchi since it does not reach alveoli SO “dead air”
Rule of thumb=AD Space=Same # in mls as weight in lbs (110 lbs=110 ml AD space)
Volume of inspired air that actually reaches alveoli is ALVEOLAR VENTILATION=70% of
TV (350 ml)
PHYSIOLOGICAL DEAD SPACE =ALVEOLAR DEAD SPACE (some alveoli can’t
exchange gases as in COPD) + ANATOMICAL DEAD SPACE
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
5
TERMS: 717
1. EUPNEA-normal breathing
HYPERPNEA-increased breathing-need for O2
2.
HYPERVENTILATION-increased breathing-in excess of need for O2
3.
Conscious effort or hysteria
4. HYPOVENTILATION-decrease in breathing that results in CO2 build up in blood
5. DYSPNEA-labored/difficult breathing-uncomfortable or in distress-hypoventilation
6. ***ORTHOPNEA-dyspnea while lying down-so sit or stand-heart disease
7. APNEA-temporary cessation of breathing-during sleep or after swallowing-at end of
a normal expiration
8. ***APNEUSIS-cessation of breathing in inspiratory position
9. RESPIRATORY ARREST-failure to resume breathing after #7 and #8
10. CHEYNE STOKES RESPIRATION-periodic type of abnormal breathing-often seen in
terminally ill or in brain damaged patients-Cycles of increased TV for several breaths
followed by several breaths with decreased TV
11. ***BIOT’S BREATHING-repeated sequences of deep gasps and apnea-usually from
increased intracranial pressure
Back to page 716
Review Dalton’s Law-the partial pressure of each gas is directly related to the concentration
in the total mixture
Atmospheric pressure is 760 mm Hg—
Oxygen is about 21% of that so can calculate the pressure of oxygen in the
atmosphere-----.21 X 760 =159.6 mm Hg
The symbol used to designate partial pressure is capital P followed by the chemical
symbol for the gas so PO2
TENSION means the same as partial pressure so oxygen tension is same as PO2
The PO2 in the atmosphere is not the same as it is when it is in the body—
This compares the partial pressures of oxygen and carbon dioxide at 4 sites
LOOK AT TABLE 24-2
Atm
Alveolar Air
Arterial Blood
Venous Blood
osp
her
e
PO2
160 mm Hg
100 mm Hg
100 mm Hg
40 mm Hg
PCO2
0.2mm Hg
40 mm Hg
40 mm Hg
46 mm Hg
Look at Figure 24.8—Notice that alveolar oxygen and carbon dioxide remain constant
This is because the alveoli are constantly ventilated-air is constantly moving in
ALVEOLAR PO2 constant=100 mm PO2
BLOOD PO2 NOT constant=40mm PO2->70mm PO2->100mm PO2
6
The amount of oxygen that diffuses into blood per minute depends on several factors: 719
1. O2 pressure gradient between alveolar air and incoming pulmonary
blood (Alveolar PO2-Blood PO2)
Application:Alveolar air PO2 decreases as altitude increases, and therefore
less oxygen enters the blood at high altitudes. At a certain high altitude
Alveolar PO2= PO2 of blood entering the pulmonary capillaries and then no
oxygen diffuses into the blood
2. Total functional surface area of respiratory membrane
Application: In EMPHYSEMA -surface area and recoil are decreased so poor
blood oxygenation ..PNEUMOTHORAX decreases functional area by collapsing
alveoli
3. Respiratory minute volume=Respiratory rate/min X vol of air
inspired/respiration
Application: Morphine slows resp rate so decreases the respiratory minute
volume and lessens the amount of oxygen entering the blood
4. Alveolar ventilation=the volume of air that actually reaches the alveoli-only
part that exchanges with blood
Application: Some air does not reach the alveoli-mucus in airways, etc
FORM AND FUNCTION:
Structural factors that facilitate oxygen diffusion into blood:
1. Walls of alveoli and capillaries are extremely thin
2. Alveolar and capillary surfaces are huge
3. Lung capillaries contain a great amount of blood
4. Every RBC comes close to alveolar air
Box 24. 3 PNEUMOTHORAX
PNEUMOTHORAX=presence of air in thoracic cavity causes lung/s to
collapse use chest tube to draw out air and allow lungs to reinflate
HOW BLOOD TRANSPORTS GASES
Immediately upon entering blood, CO2 and O2 dissolve in plasma, but because liquids can
hold only a small amt of gas in sol’n, CO2 and O2 combine with other molecules to
form a chemical union—such as hemoglobin, a plasma protein and water, SO once
bound to others, their concentration in plasma decreases and more CO2 and O2 can
diffuse into blood
HEMOGLOBIN-reddish protein pigment only in RBCs
4 polypeptide chains-2 alpha + 2 beta each with an iron containing
HEME in the middle
1 O2 molecule combines with each Heme..1 molecule of Hb holds 4 O2
*******Also CO2 can combine with the amino acids of the alpha and beta chains
So hemoglobin can be a SPONGE for both O2 and CO2
Hemoglobin also has ability to UNLOAD these 2 gases!!!
7
TRANSPORT OF OXYGEN:
At PO2 of 100 mm Hg only 0.3 ml of oxygen is dissolved in 100 ml blood
Many XXX more than that carried as OXYHEMOGLOBIN
Normal Hb level=15 gm/100 ml blood
1.34 ml O2 per gm Hb--Then 1.34 X 15 = 20.1 ml oxygen/100 ml of
blood=oxyhemoglobin
Hgb deficiciency decreases amt oxygen carried-HYPOXIA
To combine with hemoglobin oxygen must diffuse from plasma into the RBCs
where millions of hemoglobin molecules are located
Several factors affect the rate at which Hgb combines with oxygen in lung
capillaries:
oxygen-hemoglobin dissociation curve=
Hb + O2 -
Increasing PO2HbO2
And just the opposite with a decrease in PO2
HbO2-
decreasing PO2 Hb + O2
Inc PO2 accelerates Hb O2 association
Dec PO2 release of O2 from Hb--Dissociation
Association happens so quickly that -97% of blood’s hemoglobin is saturated
with O2 by time blood leaves lung capillaries to return to heart
SO oxygen travels in 2 forms:
(1) O2 ---dissolved in plasma..0.3 ml/100 ml
(2) O2 + Hb **Majority-oxyhemoglobin 20.1 ml/100 ml
Box 24. 4 CARBON MONOXIDE POISONING—Hb has 200 X the affinity for CO
than it does for O2
HbCO replaces Hb O2
Hyperbaric Oxygen Chambers-(high pressure chambers)
Application of Henry’s Law-Contain oxygen at higher pressure than
1 atmosphere-used to force greater than normal amounts of oxygen
into a patient’s blood in cases of:
Carbon monoxide poisoning
Circulatory shock
Asphyxiation
Gas gangrene or tetanus: the anaerobic bacteria causing these
infections cannot live in the presence of high levels of oxygenBox 24.5 OTHER OXYGEN BINDING PROTEINS
(1) FETAL HEMOGLOBIN
Dif structure (2 alpha and 2 gamma)-in the placenta fetal Hb can load up with
more oxygen at a low partial pressure than adult Hb can(PO2 in maternal
blood->placenta is 32mm Hg) So this is of vital importance
(2) MYOGLOBIN
Found in muscles-made up of only an alpha chain so 1 Heme group so it can
hold only 1 O2
However!! It attracts and holds oxygen much more strongly than Hb
Helps move oxygen out of blood (unloading) into muscle cells->release during
increased cell respiration/exercise—reduces intracellular PO2
8
TRANSPORT OF CO2
1. Dissolved in plasma—10%
2. Carbaminohemoblobin in RBCs-20%--united with the amine groups of Hgb
(and other plasma proteins-not included here) HCO2(Amount is governed by RATE LAW of chemistry—CO2 association with Hgb is
accelerated by an increased PCO2 and slowed by a decrease in PCO2
3. Bicarbonate ions 70% HCO3Equations on page 724—some of the dissolved CO2 enters RBCs and combines with
Hb to form carbaminohemoglobin and some combines with water to form
H2CO3 --CARBONIC ANHYDRASE found in RBCs-catalyzes the reaction
As this unstable compound splits, HCO3 - exits the RBC, then another negative
ion moves in to take its place-CHLORIDE SHIFT
H2O + CO2--->H2CO3 -->H+ + HCO3LOOK AT FIG 24.14 and 15
Carbon Dioxide and pH
When carbon dioxide enters blood, most becomes carbaminohemoglobin and H+
or bicarbonate and H+ so when CO2 increases-increasing H+ makes pH go
down
THIS IS A VERY IMPORTANT PRINCIPLE TO UNDERSTANDING HOW AND WHY
RESPIRATION IS REGULATED IN THE MANNER THAT IT IS
SYSTEMIC GAS EXCHANGE
Diffusion down a gas pressure gradient
Alveoli Hi in O2 and low in CO2->Pul capillaries low in O2 and high in CO2 so diffusion
Opposite at cells and as more activity PO2 decreases and so more O2 unloaded
because pressure gradient INCREASES
As dissolved oxygen diffuses out of arterial blood, blood PO2 decreases and this
accelerates oxyhemoglobin dissociation to release more oxygen into the
plasma for diffusion out to cells
When you exercise the PCO2 goes up and the PO2 goes down in cells so the
pressure gradient between cell and tissue capillaries goes up for each and
CO2 moves into capillaries and pressure goes from 40->46
Increasing PCO2 and decreasing PO2 produce 2 effects:
(1) Favors oxygen dissociation from oxyhemoglobin
(2) Favors carbon dioxide association with hemoglobin to form
carbamiohemoglobin
9
In cells PCO2 goes up as PO2 goes down SO this favors oxyhemoglobin
dissociation and more carbaminohemoglobin formation=”right shift”=
BOHR EFFECT
BOHR EFFECT=increased PCO2 decreases affinity between Hb and O2
therefore, more O2 will be released
Plasma pH becoming more acidic-normally occurs as plasma PCO2 level risehas the same effect of decreasing the affinity between Hb and O2 –more
O2 will be released
pH
PCO2
HbO2 Hb + O2 ALSO HbO2 Hb + O2
HALDANE EFFECT-increased CO2 loading caused by a decrease in PO2
PO2
Hb + CO2--------- HbCO2
********Page 727 Table 24.3
CONTROL CENTERS:REGULATION OF BREATHING
Homeostasis of blood gases (oxygen and carbon dioxide) is maintained primarily by
means of changes in VENTILATION-rate and depth of breathing
Regulators found in the brain stem=RESPIRATORY CENTERS
BASIC RHYTHM of respiratory cycle (inspiration/expiration) generated by the MEDULLARY
RHYTHMICITY AREA—has 2 interconnected control centers:MEDULLA OBLONGATA
1. INSPIRATORY CENTER-stimulates inspiratory muscles/primary respiratory
pacemaker-because normal quiet breathing involves stimulation of inspiratory
muscles (mainly diaphragm) alternating with relaxation of the same muscles
2. EXPIRATORY CENTER- stimulates expiratory muscles—active only when
FORCED expiration is needed
CHANGE BASIC BREATHING by different inputs to Medullary Rhythmicity Area for example
1. APNEUSTIC CENTER in PONS-stims inspiratory-longer/deeper breathing=
Apneustic breathing-abnormally long and deep inspirations
2. PNEUMOTAXIC CENTER in PONS-inhibits inspiratory center and apneustic centerprevents overinflation of lungs and permits normal rhythm
10
****DIVING REFLEX BOX 24.6
****BOX 24.7
FACTORS THAT INFLUENCE BREATHING
INVOLUNTARY: BRAIN STEM
Changes in the PCO2, PO2 and pH –influence Medullary Rhythmicity Area
PCO2 and pH act on chemoreceptors in medulla-sensitive to both –if PCO2
gets above 38-40 in arterial blood, it stimulates chemoreceptors to cause faster
breathing with greater volume of air moving in and out per minute
Chemoreceptors in medulla, carotid bodies, and aorta
Large decreases in CO2 content cause the opposite (BREATHE IN SACK WHEN
HYPERVENTILATING)
At PCO2 35 mm=Apnea
Role of PO2 not clear-hypoxic-send fewer impulses to respiraory muscles
Increase breathing:
(1) Rising PCO2
(2) Decreasing PO2 (Emergency only)
(3) Decreasing Ph
(4) Decreasing Arterial BP
BP acts on baroreceptors in carotid bodies and aorta
Decrease breathing: Opposite of above!!!
Arterial blood pressure increase
Hering-Breuer reflex—stretch receptors in lungs
(prevents overinflation of lungs-inhibits Inspiratory Centerhelps control normal depth of breathing)
Miscellaneous Factors that Affect Breathing:
Sudden painful stimulation---reflex apnea, but if continued
pain then faster and deeper breathing
Sudden cold stimuli-reflex apnea
Simulation of pharynx or larynx by irritating/touch->apneaChoking reflex to prevent aspiration of food or liquids
VOLUNTARY: CEREBRAL CORTEX
Certain limitations---hold breath->PCO2 goes up so start breathing
KIDS CAN’T HOLD BREATH AND DIE!!!
DISORDERS
RESTRICTIVE PULMONARY DISORDERS --Decreased lung volumes and
capacities
Alveolar fibrosis
Rheumatoid lung
Obesity
Metabolic disorders
Pleurisy pain
Injury
Asbestos/toxic fumes/coal dust
OBSTRUCTIVE PULMONARY DISORDERS
CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD)
Bronchitis
Emphysema (less surface area-walls of alveoli rupture)
Asthma (Inflammation of mucous membranes/spasms of bronchi)
11
OTHER PROBLEMS: Look on p 721
CARBON MONOXIDE POISONING-CO binds 200X more strongly than O2
So it knocks out O2 from HbO2 and forms HbCO-hard to remove it
Because it binds so strongly—Person turns CHERRY RED rather than cyanotic
so doesn’t appear to have a problem superficially –But serious---One strategy
is to place a person in a HYPERBARIC OXYGEN CHAMBER
CYANOSIS-respiratory distress-person turns blue
HEIMLICH MANEUVER-if choking-make fist and place thumb side of fist against victim’s
upper abdomen-below ribcage, above navel-press with quick upward thrustrepeat until object expelled—DON’T SLAP ON BACK!!
SUDDEN INFANT DEATH SYNDROME—SIDS- crib death-usually 1 mo->1 yr--now baby’s
sleep on backs—cut down number of instances—maybe if baby on stomach
press on jaw and narrows airway
EXTERNAL RESPIRATION (Exchange of gases in the lungs)
3 Factors influence diffusion of CO2 and O2
(1) Partial pressure gradients and gas solubilities:
Steep oxygen gradient (PO2 40 mm Hg in pulmonary blood-104 mm Hg in alveoli)
O2 equilibrium occurs in .25 second-1/3 of time RBC is in a pulmonary capillary
(in other words, blood flow in pulmonary capillaries could be reduced by
2/3 and still provide adequate oxygenation)
CO2 gradient less steep (45 mmHg comp to 40 mmHg)but carbon dioxide is
20 X more soluble in the plasma and fluids than is oxygen so equal amount of
it and O2 can be exchanged
(2) Thickness and Surface Area of Respiratory Membrane
(1) About 0.5-1 micro meter thick-if fluid buildup HYPOXIA can result
(2) SA=70-80 M2 size of racquetball court-Emphysema=alveolar walls break
and bigger alveoli so less SA
(3) Alveolar airflow and pulmonary capillary circulation
These are always synchronized
If low oxygen and high carbon dioxide levels in alveoli, pulmonary capillaries
constrict and airways dilate
CONVERSELY:
If high oxygen and low carbon dioxide, alveolar partial pressures cause
constriction of bronchioles and flushing of blood into pulmonary
capillaries HOMEOSTASIS
12