Not a search in vein: novel stimulus for vascular dysfunction after
advertisement

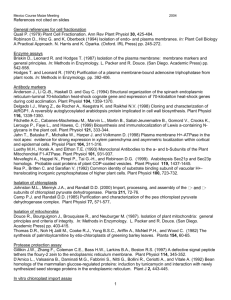
J Appl Physiol 104: 1257–1258, 2008; doi:10.1152/japplphysiol.00174.2008. Invited Editorial Not a search in vein: novel stimulus for vascular dysfunction after simulated microgravity William G. Schrage Department of Kinesiology, University of Wisconsin, Madison, Wisconsin CARDIOVASCULAR ADJUSTMENTS to real or simulated microgravity appear to be appropriate adaptations as long as the microgravity environment is maintained. It is when the subject returns to 1 G that problems with these adjustments arise. Rat models simulating microgravity use head-down tilt (HDT), where the rat ambulates on its forelimbs while suspended from its tail (see Fig. 1). This model provides two fundamental changes that occur in human spaceflight, namely a cephalic fluid shift and muscle atrophy of the locomotor muscles in the hindlimbs (3, 16, 17, 19). When these rats resume four-legged posture, they exhibit some similarities to, as well as some differences from, humans returning from spaceflight or experiencing bed rest. Rats and humans both experience reduced exercise capacity (12, 19), and rats and some humans demonstrate an inability to maintain blood pressure (BP) during an orthostatic challenge (orthostatic intolerance; OI) (2, 7, 9, 18). Do these two earthly shortcomings share a common vascular mechanism? After HDT, exercise cardiac output is reduced, and it is abnormally redistributed (10, 19). Specifically, skeletal muscle blood flow is reduced and the splanchnic bed is overperfused. Excess splanchnic blood flow can be explained by a reduced adrenergic vasoconstriction of mesenteric arteries (1, 11). Many arteries, both conduit and resistance, exhibit blunted vasoconstrictor responsiveness following HDT (3, 4, 13). A notable exception are cerebral arteries, which we will visit again later. What about the role of the venous circulation in HDT cardiovascular dysfunction? Reduced venoconstriction should effectively increase venous capacitance and limit increases in central blood volume that are critical to maintain high cardiac output with exercise (14). Similarly, a lack of venous blood redistribution during orthostatic stress will limit the body’s ability to elevate cardiac output (15). That, combined with poor vasoconstriction in mesenteric arteries (1, 5), leads us to the conclusion that the capacity of both variables in Ohm’s law (MAP ⫽ CO ⫻ TPR, where MAP is mean arterial pressure, CO is cardiac output, and TPR is total peripheral resistance) contribute to impaired orthostasis and exercise tolerance. Previous work suggests HDT does not reduce adrenergic constriction of femoral veins (13), but norepinephrine (NE) constriction is diminished in large (400 –550 m) mesenteric veins (5). What has been lacking in this field is direct evidence for poor venoconstriction, along with a viable, testable mechanism that evokes weak venoconstriction and might contribute to poor cardiac filling. In their study in the Journal of Applied Physiology, Delp’s group (1) provides with food for thought, not only with regard to new studies of veins, but also a better integrative picture of the physiological stimuli during HDT that evoke vascular dysfunction. Using classic microcirculation techniques in isolated vessels, Behnke et al. (1) study both vaso- and venoconstrictor properties in Sprague-Dawley rats following 14 days of HDT. Several key findings are of note. First, mesenteric (⬃250 m) arteries clearly show blunted vasoconstriction to NE following HDT. Second, mesenteric veins (⬃240 –250 m) from HDT rats exhibit impaired constriction to increased luminal pressures, even in a scenario with “maximal” (10⫺4 M) NE stimulation as background. Third, impaired vaso- and venoconstriction occurs without structural changes observed in many other vascular beds (smooth muscle atrophy, altered diameter). Fourth, Behnke and colleagues (1) report increased levels of atrial natriuretic and brain natriuretic peptides (ANP and BNP, respectively). Most importantly, they use ANP and BNP acutely to mimic the chronic effects of HDT on mesenteric vascular dysfunction and provide a novel mechanism for microgravity-induced vascular changes. The impaired vasoconstriction of mesenteric arteries seems to fit well with reports of diminished adrenergic vasoconstriction in arteries including aorta, femoral, carotid, and some skeletal muscle arterioles (3, 4, 13). The exceptions to this rule are cerebral arteries, which show enhanced constriction after HDT (6, 18, 20). Classically, the explanations for these divergent findings are pressure and flow differences in relation to the hydrostatic indifference point. Interestingly, arteries “above the heart,” like cerebral arteries, encounter large fluid and BP stimuli during HDT and exhibit vascular wall hypertrophy and Address for reprint requests and other correspondence: W. G. Schrage, Dept. of Kinesiology, Univ. of Wisconsin, Madison, WI 53706 (e-mail: wschrage@education.wisc.edu). Fig. 1. Regional vascular consequences in head-down tilt (HDT). VSM, vascular smooth muscle; ANP, atrial natriuretic peptide; BNP, brain natriuretic peptide; 1, increase; 2, decrease; 7, no change; NA, not applicable. http://www. jap.org 8750-7587/08 $8.00 Copyright © 2008 the American Physiological Society 1257 Invited Editorial 1258 enhanced vasoconstrictor properties (6, 17, 18, 20). Conversely, many hindlimb muscles experience low blood flow (shear) (10) and low BP during HDT, and arteries exhibit reductions in diameter and smooth muscle content (and impaired constriction) (4, 13) (see Fig. 1). With no evidence of structural remodeling in mesenteric arteries or veins (1, 8), it is unlikely smooth muscle atrophy is the culprit for lack of constriction. Moreover, splanchnic blood flow is not altered during HDT (10). These observations raise the question, what are the stimuli for blunted mesenteric vaso- and venoconstriction? The novel findings of decreased venoconstriction and increased ANP and BNP in plasma of HDT rats are thought provoking. The study of Behnke et al. (1) is the first report of how HDT might alter BNP levels and tilts the literature slightly in favor of ANP influencing vascular function (2 studies show increased, 1 shows decreased, and 1 shows no change in ANP with HDT or bed rest). While these peptides are known to reduce smooth muscle contractile function by interfering with protein kinase C and inositol 1,4,5-trisphosphate, the increased peptides alone are a weak explanation for the present findings. However, Behnke et al. (1) take the next step and use acute exposure of ANP or BNP of mesenteric arteries and veins in vitro. As hypothesized, both small vessels exhibit markedly reduced constriction to NE after only a 20-min incubation with ANP or BNP. Taken together, the authors used a systemic change in two peptides to mimic the anemic constrictor responses in mesenteric arteries and veins, providing convincing support for a novel systemic HDT stimulus (1). This is the first study that does not rely on local, tissue-specific changes in blood flow or BP during HDT to evoke vascular dysfunction on return to a 1-G environment. Of course, ANP and BNP are excluded from the cerebral circulation by the blood-brain barrier. Is this further evidence why nearly all peripheral arteries exhibit impaired adrenergic constriction, while the cerebral arteries are spared (or even enhanced from increased BP stimulus)? It appears this newly discovered systemic factor is not quite systemic after all. What questions remain? First, why do vessels from HDT rats, which presumably were exposed to the peptides for up to 14 days, show impaired constriction without ANP or BNP in the bathing solution, but the peptides can impart dysfunction after only 20 min in control rat vessels? Future studies are needed to determine the acute vs. chronic effects of these peptides, as well as the signaling cascades involved. Second, do astronauts who exhibit OI show increased ANP or BNP levels, and if so, what is the time course? Third, what other hormones may be changing in microgravity that might impart vascular consequences? Can any of these systemic circulating “factors” cross the blood-brain barrier and influence the cerebral circulation, possibly exacerbating OI? Fourth, are any pharmacological interventions available to counteract the smooth muscle effects of ANP and BNP? The functional consequences of blunted venoconstriction and thus functionally increased venous capacitance are potentially large, given the related observations of OI and exercise intolerance, both of which appear to be associated with lack of splanchnic venoconstriction and poor maintenance of stroke volume during stress (14, 15). Delp’s laboratory is acknowledged for a rich tradition in physiological studies of vascular function from “head to tail” in the HDT rat model. Their studies are innovative and have consistently J Appl Physiol • VOL showed the complexity of changes in cerebral, skeletal muscle, and mesenteric circulations, traditionally attributed to the fact that shifts in pressure and/or flow are driving the changes in a tissuespecific manner. Behnke et al. (1) should be commended for exploring new ideas regarding mechanisms that work in HDT in a systemic manner. These new data on ANP- and BNP-mediated vascular dysfunction offer inspiration for research design in future studies examining novel ideas for the physiological stimuli during real or simulated microgravity. REFERENCES 1. Behnke BJ, Zawieja DC, Gashev AA, Ray CA, Delp MD. Diminished mesenteric vaso- and venoconstriction and elevated plasma ANP and BNP with simulated microgravity. J Appl Physiol (January 24, 2008). doi:10.1152/japplphysiol.00954.2006. 2. Buckey JC Jr, Lane LD, Levine BD, Watenpaugh DE, Wright SJ, Moore WE, Gaffney FA, Blomqvist CG. Orthostatic intolerance after spaceflight. J Appl Physiol 81: 7–18, 1996. 3. Delp MD. Myogenic and vasoconstrictor responsiveness of skeletal muscle arterioles is diminished by hindlimb unloading. J Appl Physiol 86: 1178 –1184, 1999. 4. Delp MD, Holder-Binkley T, Laughlin MH, Hasser EM. Vasoconstrictor properties of rat aorta are diminished by hindlimb unweighting. J Appl Physiol 75: 2620 –2628, 1993. 5. Dunbar SL, Berkowitz DE, Brooks-Asplund EM, Shoukas AA. The effects of hindlimb unweighting on the capacitance of rat small mesenteric veins. J Appl Physiol 89: 2073–2077, 2000. 6. Geary GG, Krause DN, Purdy RE, Duckles SP. Simulated microgravity increases myogenic tone in rat cerebral arteries. J Appl Physiol 85: 1615–1621, 1998. 7. Levine BD, Zuckerman JH, Pawelczyk JA. Cardiac atrophy after bed-rest deconditioning: a nonneural mechanism for orthostatic intolerance. Circulation 96: 517–525, 1997. 8. Looft-Wilson RC, Gisolfi CV. Rat small mesenteric artery function after hindlimb suspension. J Appl Physiol 88: 1199 –1206, 2000. 9. Maurel D, Ixart G, Barbanel G, Mekaouche M, Assenmacher I. Effects of acute tilt from orthostatic to head-down antiorthostatic restraint and of sustained restraint on the intra-cerebroventricular pressure in rats. Brain Res 736: 165–173, 1996. 10. McDonald KS, Delp MD, Fitts RH. Effect of hindlimb unweighting on tissue blood flow in the rat. J Appl Physiol 72: 2210 –2218, 1992. 11. Overton JM, Tipton CM. Effect of hindlimb suspension on cardiovascular responses to sympathomimetics and lower body negative pressure. J Appl Physiol 68: 355–362, 1990. 12. Overton JM, Woodman CR, Tipton CM. Effect of hindlimb suspension on V̇O2 max and regional blood flow responses to exercise. J Appl Physiol 66: 653– 659, 1989. 13. Purdy RE, Duckles SP, Krause DN, Rubera KM, Sara D. Effect of simulated microgravity on vascular contractility. J Appl Physiol 85: 1307–1315, 1998. 14. Rowell LB. Human Cardiovascular Control. New York: Oxford University Press, 1993. 15. Rowell LB, Detry JM, Blackmon JR, Wyss C. Importance of the splanchnic vascular bed in human blood pressure regulation. J Appl Physiol 32: 213–220, 1972. 16. Schrage WG, Woodman CR, Laughlin MH. Mechanisms of flow and ACh-induced dilation in rat soleus arterioles are altered by hindlimb unweighting. J Appl Physiol 92: 901–911, 2002. 17. Wilkerson MK, Colleran PN, Delp MD. Acute and chronic head-down tail suspension diminishes cerebral perfusion in rats. Am J Physiol Heart Circ Physiol 282: H328 –H334, 2002. 18. Wilkerson MK, Lesniewski LA, Golding EM, Bryan RM Jr, Amin A, Wilson E, Delp MD. Simulated microgravity enhances cerebral artery vasoconstriction and vascular resistance through endothelial nitric oxide mechanism. Am J Physiol Heart Circ Physiol 288: H1652–H1661, 2005. 19. Woodman CR, Sebastian LA, Tipton CM. Influence of simulated microgravity on cardiac output and blood flow distribution during exercise. J Appl Physiol 79: 1762–1768, 1995. 20. Zhang LN, Zhang LF, Ma J. Simulated microgravity enhances vasoconstrictor responsiveness of rat basilar artery. J Appl Physiol 90: 2296 –2305, 2001. 104 • MAY 2008 • www.jap.org