Quantitative Analysis of the Structure of the Human Extraocular
advertisement
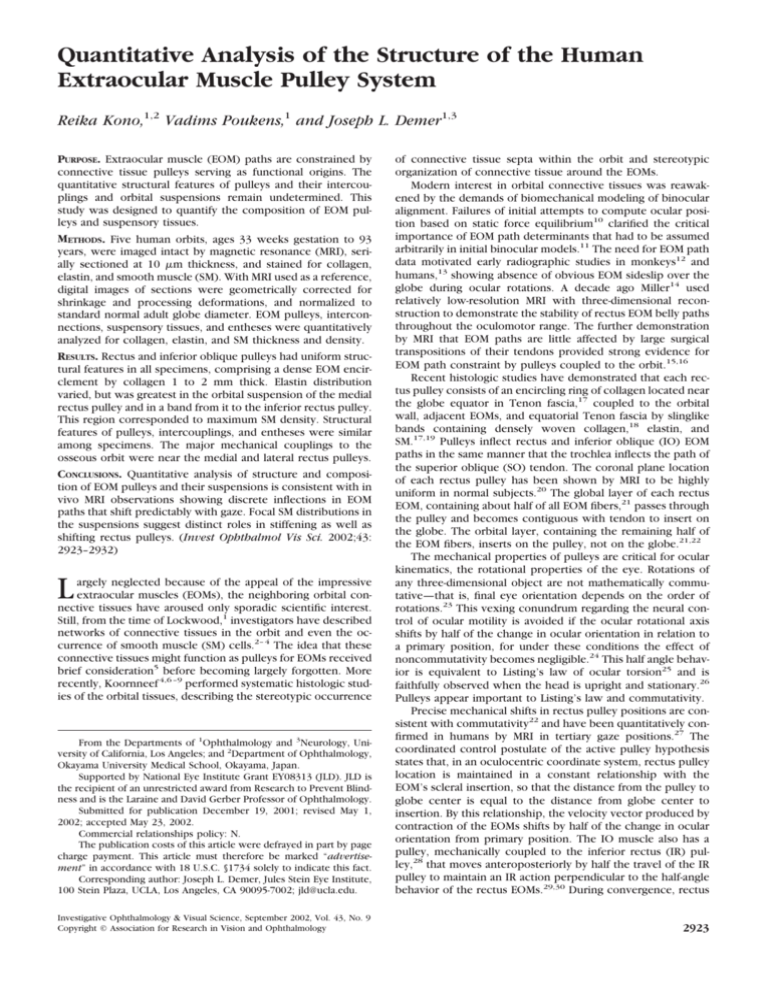
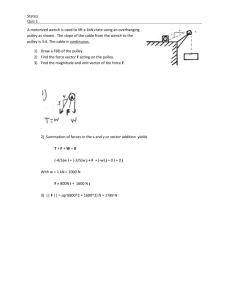
Quantitative Analysis of the Structure of the Human Extraocular Muscle Pulley System Reika Kono,1,2 Vadims Poukens,1 and Joseph L. Demer1,3 PURPOSE. Extraocular muscle (EOM) paths are constrained by connective tissue pulleys serving as functional origins. The quantitative structural features of pulleys and their intercouplings and orbital suspensions remain undetermined. This study was designed to quantify the composition of EOM pulleys and suspensory tissues. METHODS. Five human orbits, ages 33 weeks gestation to 93 years, were imaged intact by magnetic resonance (MRI), serially sectioned at 10 m thickness, and stained for collagen, elastin, and smooth muscle (SM). With MRI used as a reference, digital images of sections were geometrically corrected for shrinkage and processing deformations, and normalized to standard normal adult globe diameter. EOM pulleys, interconnections, suspensory tissues, and entheses were quantitatively analyzed for collagen, elastin, and SM thickness and density. RESULTS. Rectus and inferior oblique pulleys had uniform structural features in all specimens, comprising a dense EOM encirclement by collagen 1 to 2 mm thick. Elastin distribution varied, but was greatest in the orbital suspension of the medial rectus pulley and in a band from it to the inferior rectus pulley. This region corresponded to maximum SM density. Structural features of pulleys, intercouplings, and entheses were similar among specimens. The major mechanical couplings to the osseous orbit were near the medial and lateral rectus pulleys. CONCLUSIONS. Quantitative analysis of structure and composition of EOM pulleys and their suspensions is consistent with in vivo MRI observations showing discrete inflections in EOM paths that shift predictably with gaze. Focal SM distributions in the suspensions suggest distinct roles in stiffening as well as shifting rectus pulleys. (Invest Ophthalmol Vis Sci. 2002;43: 2923–2932) From the Departments of 1Ophthalmology and 3Neurology, University of California, Los Angeles; and 2Department of Ophthalmology, Okayama University Medical School, Okayama, Japan. Supported by National Eye Institute Grant EY08313 (JLD). JLD is the recipient of an unrestricted award from Research to Prevent Blindness and is the Laraine and David Gerber Professor of Ophthalmology. Submitted for publication December 19, 2001; revised May 1, 2002; accepted May 23, 2002. Commercial relationships policy: N. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be marked “advertisement” in accordance with 18 U.S.C. §1734 solely to indicate this fact. Corresponding author: Joseph L. Demer, Jules Stein Eye Institute, 100 Stein Plaza, UCLA, Los Angeles, CA 90095-7002; jld@ucla.edu. of connective tissue septa within the orbit and stereotypic organization of connective tissue around the EOMs. Modern interest in orbital connective tissues was reawakened by the demands of biomechanical modeling of binocular alignment. Failures of initial attempts to compute ocular position based on static force equilibrium10 clarified the critical importance of EOM path determinants that had to be assumed arbitrarily in initial binocular models.11 The need for EOM path data motivated early radiographic studies in monkeys12 and humans,13 showing absence of obvious EOM sideslip over the globe during ocular rotations. A decade ago Miller14 used relatively low-resolution MRI with three-dimensional reconstruction to demonstrate the stability of rectus EOM belly paths throughout the oculomotor range. The further demonstration by MRI that EOM paths are little affected by large surgical transpositions of their tendons provided strong evidence for EOM path constraint by pulleys coupled to the orbit.15,16 Recent histologic studies have demonstrated that each rectus pulley consists of an encircling ring of collagen located near the globe equator in Tenon fascia,17 coupled to the orbital wall, adjacent EOMs, and equatorial Tenon fascia by slinglike bands containing densely woven collagen,18 elastin, and SM.17,19 Pulleys inflect rectus and inferior oblique (IO) EOM paths in the same manner that the trochlea inflects the path of the superior oblique (SO) tendon. The coronal plane location of each rectus pulley has been shown by MRI to be highly uniform in normal subjects.20 The global layer of each rectus EOM, containing about half of all EOM fibers,21 passes through the pulley and becomes contiguous with tendon to insert on the globe. The orbital layer, containing the remaining half of the EOM fibers, inserts on the pulley, not on the globe.21,22 The mechanical properties of pulleys are critical for ocular kinematics, the rotational properties of the eye. Rotations of any three-dimensional object are not mathematically commutative—that is, final eye orientation depends on the order of rotations.23 This vexing conundrum regarding the neural control of ocular motility is avoided if the ocular rotational axis shifts by half of the change in ocular orientation in relation to a primary position, for under these conditions the effect of noncommutativity becomes negligible.24 This half angle behavior is equivalent to Listing’s law of ocular torsion25 and is faithfully observed when the head is upright and stationary.26 Pulleys appear important to Listing’s law and commutativity. Precise mechanical shifts in rectus pulley positions are consistent with commutativity22 and have been quantitatively confirmed in humans by MRI in tertiary gaze positions.27 The coordinated control postulate of the active pulley hypothesis states that, in an oculocentric coordinate system, rectus pulley location is maintained in a constant relationship with the EOM’s scleral insertion, so that the distance from the pulley to globe center is equal to the distance from globe center to insertion. By this relationship, the velocity vector produced by contraction of the EOMs shifts by half of the change in ocular orientation from primary position. The IO muscle also has a pulley, mechanically coupled to the inferior rectus (IR) pulley,28 that moves anteroposteriorly by half the travel of the IR pulley to maintain an IR action perpendicular to the half-angle behavior of the rectus EOMs.29,30 During convergence, rectus Investigative Ophthalmology & Visual Science, September 2002, Vol. 43, No. 9 Copyright © Association for Research in Vision and Ophthalmology 2923 L argely neglected because of the appeal of the impressive extraocular muscles (EOMs), the neighboring orbital connective tissues have aroused only sporadic scientific interest. Still, from the time of Lockwood,1 investigators have described networks of connective tissues in the orbit and even the occurrence of smooth muscle (SM) cells.2– 4 The idea that these connective tissues might function as pulleys for EOMs received brief consideration5 before becoming largely forgotten. More recently, Koornneef 4,6 –9 performed systematic histologic studies of the orbital tissues, describing the stereotypic occurrence 2924 Kono et al. pulleys may systematically shift in the coronal plane to meet visual demands, probably under the influence of the orbital layers of the oblique EOMs31,32 and SM in the medial orbit.19 These observations indicate a far greater degree of complexity in EOM function than previously suspected, with mutual mechanical interactions among EOMs in the periphery replacing the notion of a neural final common pathway.33 Interpretation of neural control of binocular coordination will require an accurate computational simulation of the mechanics of the EOMs and associated connective tissues. Although existing computational models of orbital biomechanics now incorporate pulleys,34,35 these are nonphysiologic regarding their essentially fixed orbital suspensions and absence of realistic gazerelated movements. Physiologic models of EOM action must incorporate a quantitative description of pulley structure. The present study was performed to determine quantitatively the composition and relative abundance of connective tissue components in the human EOM pulley system. METHODS En Bloc Tissue Preparation All human specimens were obtained from cadavers in conformity with legal requirements and in compliance with the tenets of the Declaration of Helsinki. Three human orbits (17 months, 4 years, and 57 years) were obtained from a tissue bank (IIAM, Scranton, PA), in heads fresh frozen shortly after death. The frozen heads were slowly thawed in 10% neutral buffered formalin. The head of a 33-week stillborn fetus was obtained at autopsy and fixed by immersion in formalin. These orbits were fixed in situ within the cranial bones. One additional human orbit (93 years old) was exenterated en bloc at autopsy through an intracranial approach within 24 hours of death and fixed for at least 5 days in 10% neutral buffered formalin with the periorbita intact but separated from bony support. Magnetic Resonance Imaging The four fixed heads and the 93-year-old orbit were imaged by MRI, with dual 3-in. phased array surface coils in a 1.5-T scanner (Signa; General Electric, Milwaukee, WI). Multiple contiguous quasicoronal MRIs, 2 or 3 mm in thickness, were then obtained with a T1 pulse sequence encompassing a 256 ⫻ 256 matrix over a 4- or 5-cm2 field of view, providing a pixel resolution of 156 or 195 m, respectively. To improve the signal-to-noise ratio at these high resolutions, four to nine excitations were performed. Digital MRIs were transferred to computers (Macintosh; Apple Computer, Cupertino, CA), converted into eightbit tagged image file format (TIFF) by locally developed software, and quantified by NIH Image (W. Rasband, National Institutes of Health; available by file transfer protocol from zippy.nimh.nih.gov or on floppy disc from NTIS Springfield, VA; part number PB95500195GEI). Histologic Processing The four orbits fixed in situ were then removed in continuity with the eyelids and orbital bones. The orbital rims and walls were carefully thinned under magnification by using a high-speed drill and rongeurs before decalcification for 24 hours at room temperature in 0.003 M EDTA and 1.35 N HCl.22 Formalin-fixed tissues were dehydrated in graded solutions of alcohol and chloroform or xylenes, embedded in paraffin, and serially sectioned in the coronal plane at 10-m thickness by disposable metal blades on a microtome (HM325; Carl Zeiss, Thornwood, NY), as previously described.17,19,22 This produced 2800 to 4800 sections per orbit, depending on the orbit’s size. Alternate sets of five contiguous sections were saved and mounted on 50 ⫻ 75 mm gelatin-coated glass slides. Masson trichrome stain was used to show muscle and collagen, and van Gieson stain to show elastin.36 As previously described,19 SM was confirmed using a monoclonal mouse antibody to human SM IOVS, September 2002, Vol. 43, No. 9 ␣-actin, which was visualized with an avidin-biotin complex (ABC) kit with blue chromogen (Alkaline Phosphatase Kit 3; Vector Laboratories, Burlingame, CA). To maximize chromatic uniformity, sections were stained with Masson trichrome and van Gieson stains in batches of 25 to 50 slides, and, for human SM ␣-actin, in batches of five slides, with fresh reagents used for each specimen. Analysis Whole stained histologic sections were imaged in color with one of two digital cameras equipped with a 50-mm fixed or variable macro lens (Nikon, Tokyo, Japan). One camera (Leaf Lumina; ScyTech, Bedford, MA) had a resolution of 3400 ⫻ 2800 pixels, and the other (D1X; Nikon) had a resolution of 3008 ⫻ 1960 pixels in 24-bit color. Images were spatially calibrated by imaging a 1-mm rectilinear grid affixed to a glass slide before and after each session of histologic imaging. Higherpower images were obtained by mounting either digital camera on a microscope (BH-2; Olympus, Lake Success, NY). Coronal MRIs of each specimen were used as the spatial standard to correct histologic images for shrinkage and nonuniform distortions introduced by later processing. For this purpose, one coronal plane MRI was selected for each specimen from the level of the globe equator, so that it included the rectus EOMs and pulleys (Fig. 1, top left).17 A more anterior MRI plane would have better intersected the densest pulley regions, but the flatness of EOM tendons and the density of connective tissue make it difficult to distinguish contours required to judge EOM or pulley position in the image plane.16 First, MRIs in NIH Image were absolutely scaled, based on the calibrated MRI field of view. Then, the MRI and histologic images (Fig. 1, center left) were superimposed at partial transparency in image management software (Photoshop, ver. 5.5; Adobe Systems, San Jose, CA) and rotated to identical orientations (Fig. 1, bottom left). To correct for shrinkage, the histologic images were then differentially scaled in the horizontal and vertical directions so that the orbital walls superimposed on the MRI (Fig. 1, bottom left). This procedure assumes that dimensional distortion produced by shrinkage or stretching affects the entire section similarly in the same direction, but allows this distortion to be different in orthogonal directions. For example, sections tended to stretch in the dimension parallel to the motion of the microtome knife, but did not do so perpendicular to this direction. Specimens were not uniformly oriented in relation to the direction of knife travel, and shrinkage was therefore represented for the two arbitrary orthogonal directions required for superimposition of histologic images on MRIs. Shrinkage in orthogonal directions ranged from 30% ⫻ 40% (smaller ⫻ larger dimension) in the exenterated specimen to 10% ⫻ 15% in specimens processed with orbital bones intact, with mean (⫾SD) shrinkage of 20% ⫾ 9% ⫻ 27% ⫾ 7%. All dimensional measurements reported herein were performed with images individually corrected for bidirectional shrinkage distortions. Two high-quality sections, corresponding to vicinity of the MRI plane, were selected for measurement of pulleys and connective tissues defined as in Figure 1. It must be noted that the quasicoronal plane perpendicular to the orbital axis, although optimal for all the rectus EOMs in aggregate, is not exactly perpendicular to any rectus EOM or parallel to the planes of the rectus pulleys. To measure the thickness of the orbital and global aspects of the rectus pulleys, it was necessary to identify the thickest regions using different sections. Thicknesses of pulleys and connective tissue and SM bands were measured from the digital images using the measurement tool. Orbital and global thickness of each of the six EOM pulleys, the band connecting the medial rectus (MR) and superior rectus (SR) pulleys (MR–SR band), the band connecting the MR and inferior rectus (IR) pulleys (MR–IR band), and the band connecting the lateral rectus (LR) and SR pulleys (LR–SR band) were determined in duplicate in two sections for each specimen. Each thickness determination consisted of the mean (⫾SE) of seven measurements distributed in representative fashion over the extent of the structure. Sections stained with Masson trichrome were used to measure collagen density and pulley thickness. Densitometry was performed IOVS, September 2002, Vol. 43, No. 9 Human Pulley Structure 2925 FIGURE 1. Correction of stretching distortions produced by histologic handling using preprocessing MRI. Sample coronal section at level of pulleys from 17-month-old human right orbit. Left: coronal MRI of the sample with bony orbit intact (top); low-power coronal micrograph stained with Masson trichrome (middle); dimensions and shape of the micrograph were digitally corrected to superimpose with the comparable coronal MRI as shown at partial transparency (bottom). Enlarged and labeled view of corrected micrograph at right. Rectangles A, B, and C are magnified in Figure 3. digitally using the color range command in the image management software (Photoshop; Adobe). Collagen, constituting the most abundant and anatomically defining constituent of pulleys, stains blue with Masson trichrome. Most pulleys and connective tissue bands consist of laminae of collagen separated by voids that probably contain adipose tissue. The relative proportion of pulley or band thickness that contained collagen, as opposed to void, was considered to be collagen density. Collagen density was measured in the same sections stained with Masson trichrome and at the same low magnification used for measurement of pulley thickness. Density of the less-abundant microscopic elastin fibrils, which stain dark black with van Gieson elastin FIGURE 2. Adjacent 10-m coronal sections of 17-month-old human. (A) Masson trichrome stain showing dense collagen (dark blue) of MR pulley ring. (B) Van Gieson elastin stains appears black in region of dense deposition of elastin. Elastin fibrils, with larger aggregates denoted by arrows, are not individually resolvable at this low magnification, but are seen at higher power in Figure 3E. (C) Immunostaining for human SM ␣-actin (blue). stain (Fig. 2B), was determined from high-power digital micrographs of adjacent sections. SM density was determined from high-power digital micrographs of adjacent sections immunostained with a blue chromogen for human SM ␣-actin, which is highly specific for SM (Fig. 2C). For each connective tissue constituent, the selected color was converted to grayscale. Grayscale images of specific tissue constituents were imported into NIH Image, and the density function was applied with the use of a consistent threshold. Density (percentage) was calculated as pixels exceeding threshold divided by grayscale pixels. Use of a threshold is unavoidable for quantitative analysis, because chromatic variation among specimens is inevitable, even with large-scale histo- 2926 Kono et al. IOVS, September 2002, Vol. 43, No. 9 FIGURE 3. Magnified views from field in Figure 1 showing adjacent 10-m coronal sections of 17-monthold human orbit with columns illustrating the MR–SR band (Fig. 1A), the MR pulley (Fig. 1B), and the MR–IR band (Fig. 1C). (A–C) Masson trichrome stain demonstrating dense collagen (dark blue) in all regions. (D–F) van Gieson elastin stain demonstrating elastin fibers (black) richer in the orbital aspects of the MR pulley and MR–IR band, than in MR–SR band. (G–I) Immunoreactivity (blue) for human SM ␣-actin showing small and large SM bundles at the MR pulley and MR–IR band, but only small bundles in the MR–SR band. logic processing techniques such as those used in the current study. Use of a threshold that appears reasonable in comparison with the original color images and is qualitatively consistent among specimens minimizes the effects of threshold selection. Identifiable blood vessels were excluded from areas of SM measurement, because vascular SM is not relevant to mechanical measurements. We estimated total connective tissue content to be the average density multiplied by average thickness of the structure under consideration. A distinct band of connective tissue with an insertion on orbital bone was considered to constitute an enthesis. Total collagen and elastin content at the level of each enthesis was also measured using the same methods. The dense connective tissue extending from the MR pulley to the medial orbital periosteum was considered the medial enthesis. The dense connective tissue band extending from the LR pulley to the lateral periosteum was considered to be the lateral enthesis, distinguishable from the enthesis of the lateral canthal tendon, slightly more anterior on the periosteum of the zygomatic bone. The anteroposterior extent of the MR–IR SM band was measured in each specimen, as judged by the maintenance of the band structure in serial 10-m-thick sections. Data on thickness and extent in each specimen were normalized to that specimen’s globe diameter compared with a normal globe diameter in vivo of 24.3 mm obtained by MRI.37 Enthesis dimensions were also measured. The SO pulleys (trochleas) in two specimens (57 and 93 years old) were not measured because of damage sustained during specimen preparation. RESULTS Major histologic findings were similar in all specimens, ranging in age from fetal to 93 years. In low-power micrographs near the globe equator where the pulley ring was present, Masson trichrome stain clearly distinguished the EOMs (purple) surrounded by pulleys consisting of encirclements of collagen (Fig. 1, blue). Structural details are clearer at higher power (Fig. 2), showing adjacent 10-m coronal sections of a 17-month-old human MR stained with Masson trichrome stain (Figs. 2A, 3B) and van Gieson elastin stain (Figs. 2B, 3E) and for human SM ␣-actin (Figs. 2C, 3H). The image plane in Figure 2 intersects a dense region of the orbital aspect of the MR pulley, showing a dense encirclement by collagen laminae having only sparse voids that presumably contained fat before elution in process- ing. More posterior sections demonstrated a thicker ring on the global aspect of the MR pulley, but the global aspect was not as thick as the orbital. Black elastin fibrils were embedded in the collagen of the pulley ring and in suspensory bands running superiorly and inferiorly (Figs. 2B, 3). SM, appearing blue due to immunoreactivity for human SM ␣-actin, was abundant on the orbital surface of the MR pulley (Figs. 2C, 3). The orbital layers of the rectus EOMs inserted into the collagen of each of their respective pulleys in every specimen. The morphology of the MR pulley was identical in all specimens except the fetal one. Suspensory bands of connective tissue were also consistently identified in all specimens (Fig. 1). A dense band was present from the MR to the IR pulleys (MR–IR band, Fig. 1), and from the MR to the SR pulleys (MR–SR band, Fig. 1). Another dense band was present from the SR to the LR pulleys (LR–SR band, Fig. 1). The IO muscle was present between the IR and LR pulleys. The collagenous sheath of the IO was contiguous with the LR and IR pulleys, forming an interconnection analogous to the other interconnections of contiguous pulleys. Anterior to the pulley rings, posterior Tenon fascia formed a complete cup investing the globe analogous to a ball within a socket, and inserting most anteriorly on the orbital rim. The posterior Tenon fascia contained abundant collagen and elastin. Quantitative analysis recognized that, because of the intersection of coronal histologic sections with the three-dimensional structure of the orbital connective tissues, the coronal histologic planes would not exactly coincide with the plane of each pulley ring. Total pulley thickness for each EOM was measured separately for the orbital and global portions, in each case from the coronal section showing the most complete development of that portion. The tissue bands interconnecting the pulleys were measured from sections showing maximal development of the two pulleys under consideration. In each case, measurements included all connective tissue constituents, plus intervening spaces that had presumably contained fat (Fig. 4). The thickness, collagen, and elastin contents in the three specimens aged 17 months, 4 years, and 57 years were similar and were averaged to represent data from the predominant part of the postnatal human age range, whereas quanti- IOVS, September 2002, Vol. 43, No. 9 FIGURE 4. Connective tissue thickness normalized to standard global diameter. Data are the average of the three specimens aged 17 months, 4 years, and 57 years. *Not measured in the 57- and 93-year-old specimens, because of exenteration damage to the trochlea. tative data from the fetal and 93-year-old specimens were considered separately. Pulley thickness tended to be greater on the orbital than the global aspect (Fig. 4). For the mid–agerange specimens, mean pulley thickness of the orbital aspect ranged from 1.0 to 2.25 mm, whereas global aspect thickness ranged from 0.5 to 1.75 mm. Pulley thickness was modestly lower in the fetal and 93-year-old specimens. Interconnections among pulleys ranged in mean thickness from 1.25 mm for the MR–SR band to 2.75 mm for the MR–IR band. Similar to the thickness of the pulleys, interconnecting band thickness was generally lower in the fetal and 93-year-old specimens than in the other specimens. The SO sheaths were thinner than in the remaining EOMs. Total collagen content was taken to be the product of pulley thickness and collagen density, and its dimension was thus expressed in millimeters (Fig. 5). The orbital part of each rectus pulley had a mean collagen content of 0.5 to 0.75 mm in the three specimens aged 17 months, 4 years, and 57 years. The fetal specimen had collagen content similar to these, but the 93-year-old specimen consistently had less collagen. The global part of each rectus pulley had mean collagen content of 0.25 to 0.5 mm, again with the 93-year-old specimen having less. The MR–IR band had the greatest collagen content of any structure studied, averaging 1 mm. Total elastin content was taken to be the product of pulley thickness and elastin density and its dimension was also expressed in millimeters (Fig. 6). Elastin content was much less than collagen, ranging downward from a mean of approximately 0.075 mm in the MR pulley orbital layer and MR–IR band in the three specimens aged 17 months, 4 years, and 57 years. Unlike collagen, elastin content was often greater in the 93-year-old specimen. Elastin fibrils were qualitatively different in the oldest specimen, showing evidence of shredding and clumping. Elastin content was almost uniformly zero in the fetal specimen, except in the SO sheath where elastin was present. Because of careful preparation of whole orbits processed en bloc in continuity with orbital bones, it was possible to study the structure of each major connective tissue enthesis on the periosteum (Fig. 7). This included all except the 93-year-old specimen, which was processed by exenteration before fixation and thus had dissection damage to the entheses. The Human Pulley Structure 2927 FIGURE 5. Total collagen content computed as mean pulley thickness multiplied by mean collagen density, normalized by standard global diameter. Data are the average of the three specimens aged 17 months, 4 years, and 57 years. *Not measured in the 57- and 93-year-old specimens, because of exenteration damage to the trochlea. pulley suspensory system entheses corresponded to the horizontal rectus pulleys: laterally on the zygomatic bone at what is probably the zygomatic tubercle,38 medially at the lacrimal, and probably also the maxillary and frontal bones. These entheses have been described as the “check ligaments,” and it has been correctly recognized that only the MR and LR are endowed with them.38 The lateral enthesis extended directly to the LR pulley, which was then indirectly coupled to the SR through the LR–SR band, and indirectly coupled to the IR along the IO muscle and its sheath. The lateral enthesis was distinct from the lateral canthal tendon extending through the lacrimal grand and having its own enthesis on the zygoma at the orbital rim approximately 3 mm more anteriorly. The lateral enthesis FIGURE 6. Total elastin content computed as mean pulley thickness multiplied by mean elastin density, normalized by standard global diameter. Data are the average of the three specimens aged 17 months, 4 years and 57 years. *Not measured in the 57- and 93-year-old specimens because of exenteration damage to the trochlea. There was greater elastin in the orbital than the global aspect of the MR pulley and rich elastin in the MR–IR band. 2928 Kono et al. IOVS, September 2002, Vol. 43, No. 9 FIGURE 7. Coronal section of 17month-old old human right orbit at the level of the entheses, stained with Masson trichrome. Residual bone stained bright red, but was largely removed from the underlying periorbita after fixation, to enable sectioning. Dense, blue-staining collagen is visible in the connective tissues. Left: high-power view at the level of lateral canthal tendon approximately 4 to 5 mm anterior to lateral enthesis (top) and high-power view of lateral enthesis extending from the orbital rim at zygomatic bone to the LR pulley (bottom). Sheath of SO tendon unites with nasal aspect of the SR pulley. measured approximately 5 mm mediolaterally and anteroposteriorly and 6 mm dorsoventrally (Fig. 7) and often incorporated a central lobule of lacrimal gland that was unavoidably included in these dimensions. Dimensions of the lateral enthesis for each specimen are presented in Table 1. The medial enthesis extended directly to the MR pulley, which was then coupled indirectly to the SR and IR through their corresponding bands. The medial enthesis measured approximately 10 mm in mediolateral and 11 mm in dorsoventral extent, but only 4 mm in anteroposterior extent. Measured dimensions for the medial enthesis of each specimen are presented in Table 1, except for the 57-year-old specimen, in which processing damage prevented accurate determination of the anteroposterior extent. The medial enthesis band incorporated a slip of anteroposteriorly oriented striated muscle in its center (Fig. 7) that was unavoidably incorporated in its measured dimensions (Table 1). The medial canthal tendon had its enthesis at the same site as that of the band to the MR. There were no direct entheses from the vertical rectus pulleys to the immediately adjacent orbital bones. The pulley enthesis bands were composed of very dense connective tissue. Total collagen content of both the medial and lateral enthesis bands exceeded that of any other pulley suspensory structure, whereas total elastin content was comparable to that of other dense pulley suspensions. Dimensions of enthesis bands in individual specimens are reported in Table 2. Nonvascular SM was stereotypically but not uniformly distributed in the orbital connective tissues of all specimens, and was identified by immunoreactivity to human SM ␣-actin. Recognizable blood vessels were avoided in the quantitative evaluations, but a few small vessels may have been included if their lumina could not be identified. There were two types of SM distributions (Fig. 3). Large SM bundles averaged 30 to 40 m in diameter and were mainly located in a band from the superior border of the MR to the nasal border of the IR. These large bundles were apparently cut transversely by the coronal sections. Small SM bundles averaging 10 m in diameter were located on the global surface of the large cell bundles, but formed a band having greater length, extending from the nasal border of the SR to the nasal border of the IR. The small SM bundles appeared to have been cut more tangentially, so that their long axes approximated the coronal plane. Because it formed a distinct structure (Figs. 3B, 3E, 3H), the SM band at the MR pulley was not included in the pulley’s thickness, but the SM bundles at the MR–IR band were included in the pulley’s thickness, because the bundles were intrinsic within the band (Figs. 3C, 3F, 3I). For quantitative analysis, large and small SM bundle distributions were lumped together as a single structure. The normalized anteroposterior extent of the MR–IR TABLE 1. Pulley System Enthesis Band Dimensions Mediolateral Dorsoventral Anteroposterior Specimen Age Medial Enthesis Lateral Enthesis Medial Enthesis Lateral Enthesis Medial Enthesis Lateral Enthesis 33-wk fetus 17 mo 4y 57 y Mean ⫾ SE 11.03 10.42 8.18 11.29 10.23 ⫾ 0.71 3.28 3.26 5.26 6.11 4.48 ⫾ 0.72 13.12 10.20 9.47 12.02 11.20 ⫾ 0.83 8.97 4.12 3.87 7.06 6.01 ⫾ 1.23 2.36 2.35 3.16 ND 2.62 ⫾ 0.27 5.11 3.49 3.97 6.93 4.88 ⫾ 0.77 Data are expressed in millimeters. ND, not determined. Human Pulley Structure IOVS, September 2002, Vol. 43, No. 9 2929 TABLE 2. Total Collagen and Elastin Content of Pulley System Enthesis Bands Total Collagen Content (mm) Total Elastin Content (mm) Specimen Age Medial Enthesis Lateral Enthesis Medial Enthesis Lateral Enthesis 33-wk fetus 17 mo 4 mo 57 mo Mean ⫾ SE 2.50 2.59 1.55 1.35 2.00 ⫾ 0.32 1.42 1.10 0.93 1.71 1.29 ⫾ 0.17 0.080 0.158 0.087 0.057 0.095 ⫾ 0.022 0.003 0.066 0.010 0.070 0.037 ⫾ 0.018 SM band of the five specimens averaged 4.74 ⫾ 0.82 mm (⫾SE; range, 2.77– 6.68 mm). The LR–SR band, as well as other connective tissue bands, had few and widely scattered small SM cells. The MR–SR band and the LR–SR band had insufficient SM for quantitative measurement by ␣-actin immunoreactivity. The lateral levator aponeurosis (LLA) has been described to be a connective tissue condensation extending between the superior border of the LR pulley and the lateral border of the levator palpebral superioris (LPS).19 Careful examination of the our high-quality specimens suggested the need for revision of this description. More correctly, the LLA should be considered to be a lateral expansion of the LPS tendon, running inferolaterally and partially through the lacrimal gland to insert on the orbital bone at the lateral canthus. The muscular tissues of the LLA began superiorly as a lateral extension of striated muscle from the LPS in the medial half, contiguous with a particularly dense band of SM in the lateral half of the LLA. The SM in the LLA did not appear to be directly coupled to the oculorotary EOMs. However, another SM distribution, distinct from the LR–SR band, extended from a lateral expanse of striated muscle fibers from the levator and continued laterally and inferiorly to the LR pulley. This distribution, forming part of what was described by Müller as the “peribulbar muscle,”39,40 was present anterior to the equator. With both large and small bundles included, maximum SM thickness near the MR pulley or MR–IR band ranged from 0.2 FIGURE 8. SM thickness normalized by standard adult globe diameter. Only the MR pulley region and MR–IR band had sufficient SM for quantitative analysis. SM in these regions was measured in sections corresponding to those used for analysis of collagen and elastin. Maximum SM thickness was determined from examination of all sections from each specimen. There was insufficient SM for measurement in the MR–IR band in the 93-year-old specimen. Except for maxima, duplicate measurements were made in the same orbits (duplicated symbols). to 1.4 mm (Fig. 8). Total SM content was taken to be the product of band thickness and SM density, thus having the dimension of mm (Fig. 9). The SM content at the MR pulley in the region of the medial enthesis ranged from 0.01 to 0.13 mm. DISCUSSION Recent formulations of EOM biomechanics emphasize the pivotal role of EOM pulleys in ocular kinematics.22,24,32,41,42 These formulations are supported by MRIs in living humans that demonstrate the highly stereotyped locations and stability of rectus pulleys.20,27,37 Qualitative features of EOM pulleys are similar in humans, monkeys,19 rats,43 and rabbits (Demer JL, unpublished data, 2002). Further support for the importance of pulleys is provided here by the demonstration of quantitative histologic uniformity in composition and structural features of pulleys in specimens prepared en bloc to maintain critical anatomic relationships. The general arrangement of orbital connective tissues is uniform throughout the range of human age from fetal life to the tenth decade and is summarized in schematic form in Figure 10. After fetal life when it was smaller, even the normalized thickness of pulley rings and suspensory bands remained high and roughly consistent across the age range. Such uniformity supports the concept that pulleys and orbital connective tissues constitute important components of the ocular motor apparatus. Although precise timing of pulley maturation cannot be determined from the available specimens, the pulley system of even the 17-monthold specimen had adult characteristics. Only fetal pulley structure showed immaturity in development of collagen thickness and elastin content (Figs. 4, 5, 6). FIGURE 9. SM content computed as the mean thickness multiplied by mean density, both determined from SM ␣-actin immunoreactivity, and normalized by standard adult globe diameter. Sites and duplicate measurements denoted as in Figure 8. 2930 Kono et al. FIGURE 10. Frontal view of major orbital connective tissues. Globe is depicted as sectioned at approximately the coronal plane level of the pulley rings, but the illustration also includes the more anteriorly located medial and lateral entheses. LG, lacrimal gland; SOT, superior oblique tendon. Intercouplings between adjacent pulleys were also stereotypic in configuration and composition (Fig. 10). The MR–IR band was not only the thickest such intercoupling, but it also contained the most collagen, elastin, and SM. These features of the MR–IR band seem ideal to provide a stiff elastic coupling between the highly stable MR and relatively mobile IR pulleys,20 permitting the latter to move nasally and laterally, not only under passive tension but also nasally during contraction of the intrinsic band of small SM cells. This may be one mechanism underlying nasal repositioning of the IR pulley during convergence.31,32 In rat, a species without convergence, the MR–IR band is poorly developed and contains minimal SM.43 The MR–IR band forms part of the Lockwood ligament, a structure that has been described to form a kind of suspensory sling running mediolaterally inferior to the globe.38 However, the present study indicates that the connective tissue of the Lockwood ligament temporal to the IR pulley is much less substantial than that nasal to it. The MR–SR band, although thinner and containing less connective tissue and much less SM, seems also sufficiently robust to provide significant mechanical coupling between these two pulleys. The MR–SR band should be considered to have lower stiffness than the MR–IR band. Earlier studies of orbital anatomy were hampered by difficulties in removing the delicate, elastic, soft tissues from the supporting orbital bones. Removal of the soft tissues by dissection almost inevitably results in damage, particularly to the entheses, where adhesion to bone is most secure. In the current study, we used specimens that, for the most part, had been processed in continuity with the orbital bones to clarify the relationship between the pulley system and its bony support, as depicted in the schematic frontal view in Figure 10. This schematic depicts only the thick and presumably mechanically significant connective tissue structures, omitting the thinner anterior and posterior pulley slings. Figure 10 also depicts structures that generally do not all lie in the same plane. Contrary to the depiction in an earlier schematic, the IR and SR pulleys were found not to have direct mechanical coupling to an enthesis on the adjacent orbital bone. The rectus pulley system is mechanically coupled to the anterior orbital bones by heavy connective tissues nasally and temporally. The medial enthesis corresponds to the medial canthal tendon region where the lids are anchored nasally, whereas the lateral enthesis is several millimeters posterior to the lateral canthal tendon IOVS, September 2002, Vol. 43, No. 9 at the zygomatic tubercle. The absence of direct enthesis of the vertical rectus pulleys to the bone of the adjacent orbital rim regions is a necessary consequence of the mobility of the superior and inferior eyelids, which move through these regions within only loose connective tissues. The vertical rectus pulleys are thus indirectly coupled to the medial and lateral entheses by the intercouplings between the rectus pulleys. Further stability is provided by the SO tendon emerging from its rigid trochlea and by the sheath and belly of the IO muscle, which originates from anterior orbital bone. Past descriptions suggested correctly that the orbital connective tissue system supports and protects the globe, but such descriptions emphasized a major role for the “check ligaments” in limiting and dampening ocular movements.38 The elasticity of the check ligaments was believed to be important in graduating the action of EOM contraction to ensure smooth ocular rotations without jolting the globe.38 The active-pulley hypothesis,22,32 as well as the current quantitative anatomic findings, support quite a different interpretation of the check ligaments— elastic suspensions of the pulley system that actively regulates the direction of EOM force to control ocular kinematics. In view of the misleading functional connotation, the term check ligament should probably be abandoned. The current report also makes a novel distinction between the LLA and the LR–SR band. The LLA, connecting the lateral expansion of the LPS to the anterior bony orbit while partially traversing the lacrimal gland, appears to be mainly a suspension for the LPS in relationship to the Whitnall ligament. The LLA would only indirectly stabilize the SR pulley by mechanical coupling of the LPS and SR. The lateral half of the LLA contains abundant SM, whereas the medial half contains striated muscle contiguous with the LPS. In contrast, the LR–SR band extends directly between the involved pulleys and contains only a small amount of SM in small bundles. The LR–SR band is equivalent to the MR–SR band in thickness and collagen content, but probably has lower stiffness, because the elastin content of the LR–SR band is about one fourth of the MR–SR band. Elastin has the property of reversible extensibility44 that probably confers elastic stiffness on pulley suspensory tissues. The orbital aspect of each rectus pulley had more and thicker collagen than the global aspect. Elastin content in the orbital aspect was also richer than in the global aspect of each pulley. The more extensive and presumably stiffer structure of orbital aspects of rectus pulleys is likely to be related to concentration at those sites of stress associated with sharp EOM path inflections in secondary and tertiary gaze positions.27,37 Such inflections, which move in the anteroposterior direction during contraction of orbital layer fibers inserting on the pulleys,22 require support from pulley suspensions to the entheses to maintain their considerable resistance to sideslip in the coronal direction. Although general features of pulleys were preserved in the 93-year-old specimen, there was also qualitative evidence of age-related degeneration. Elastin fibers in pulley showed clumping and shredding. The change may account for the observation that total elastin thickness in the 93-year-old specimen exceeded that of the other specimens (Fig. 6). There also was obvious qualitative atrophy of collagen fibers in the 93year-old specimen, associated with reduced total collagen thickness (Fig. 5). Degenerative connective tissue changes in aging correlate with limited ocular ductions in the elderly,45 and with MRI evidence of downward displacement of horizontal rectus pulley positions.46 Asymmetrical occurrence of such changes in the two orbits may be expected to cause strabismus.46 SM has long been recognized in the orbital connective tissues,5,19,39 but its role has been unclear. Demer et al.19 described an intricate innervation pattern, including rich sym- IOVS, September 2002, Vol. 43, No. 9 pathetic, parasympathetic, and nitroxidergic innervation to pulley SM, suggesting the following possible roles for pulley SM: to maintain uniform stiffness in the pulley suspensions; to accomplish slow, adaptive adjustments in pulley locations as are necessary to maintain binocular alignment over a lifetime; and to fulfill a possible dynamic role in eye movements. The latter suggestion is consistent with new observations of excyclorotation of the four-rectus pulley array during convergence.31 The especially dense peribulbar SM between the IR and MR pulleys seems anatomically suited to accomplish the observed nasal shifting of the IR pulley in convergence. Mathematical models of EOMs have led to much insight into EOM function, and have motivated significant new lines of inquiry.47 However, even the most comprehensive currently available models34 fail to account for important features such as large gaze-related shifts in rectus pulley positions.27 Quantitative data are now available for each of the four rectus EOMs, showing the number of global layer fibers inserting on the scleral tendon and the number of orbital layer fibers inserting on the pulley.21 More complete models may incorporate this and the current quantitative data on pulley structure and interconnections in computational implementations of these critical structures. The values for collagen and elastin content reported here provide a basis for reasonable estimates of relative stiffness of pulley suspensions and interconnections. Potential for pulley shift due to the actions of striated EOMs may be estimated from connective tissue and SM content in the specific structures described herein. A realistic computational model of EOM and orbital connective tissue mechanics would be of general value in understanding normal and pathologic behavior of ocular movements and binocular alignment. Acknowledgments The authors thank Nicolasa de Salles and Frank Henriquez for technical assistance. References 1. Lockwood CB. The anatomy of the muscles, ligaments, and fasciae, etc. J Anat Physiol. 1886;20:1–25. 2. Bergen MP. Some histological aspects of the structure of the connective tissue system and its relationships with the blood vessels in the human orbit. Acta Morphol Neerl Scand. 1982;20: 293–308. 3. Jones LT. A new concept of the orbital fascia and rectus muscle sheaths and its surgical implications. Trans Am Acad Ophthalmol Otolaryngol. 1968;72:755–764. 4. Koornneef L. Details of the orbital connective tissue system in the adult. Acta Morphol Neerl Scand. 1977;15:1–34. 5. Sappey PC. Traite D’Anatomie Desccriptive Avec Figures Intercalees Dans Le Texte. Paris: Delahaye et Lecrosnier; 1888. 6. Koornneef L. Spatial Aspects of Orbital Musculo-fibrous Tissue in Man. Amsterdam: Swets & Zeitlinger; 1977. 7. Koornneef L. The architecture of the musculo-fibrous apparatus in the human orbit. Acta Morphol Neerl Scand. 1977;15:35– 64. 8. Koornneef L. New insights in the human orbital connective tissue: result of a new anatomical approach. Arch Ophthalmol. 1977;95: 1269 –1273. 9. Koornneef L. Orbital septa: anatomy and function. Ophthalmology. 1979;86:876 – 880. 10. Robinson DA. A quantitative analysis of extraocular muscle cooperation and squint. Invest Ophthalmol. 1975;14:801– 825. 11. Miller JM, Robinson DA. A model of the mechanics of binocular alignment. Comput Biomed Res. 1984;17:436 – 470. 12. Miller JM, Robins D. Extraocular muscle sideslip and orbital geometry in monkeys. Vision Res. 1987;27:381–392. 13. Simonsz HJ, Harting F, de Waal BJ, Verbeeten BWJM. Sideways displacement and curved path of recti eye muscles. Arch Ophthalmol. 1985;103:124 –128. Human Pulley Structure 2931 14. Miller JM. Functional anatomy of normal human rectus muscles. Vision Res. 1989;29:223–240. 15. Miller JM, Demer JL, Rosenbaum AL. Effect of transposition surgery on rectus muscle paths by magnetic resonance imaging. Ophthalmology. 1993;100:475– 487. 16. Clark RA, Rosenbaum AL, Demer JL. Magnetic resonance imaging after surgical transposition defines the anteroposterior location of the rectus muscle pulleys. J Am Acad Pediatr Ophthalmol Strabismus. 1999;3:9 –14. 17. Demer JL, Miller JM, Poukens V, Vinters HV, Glasgow BJ. Evidence for fibromuscular pulleys of the recti extraocular muscles. Invest Ophthalmol Vis Sci. 1995;36:1125–1136. 18. Porter JD, Poukens V, Baker RS, Demer JL. Structure-function correlations in the human medial rectus extraocular muscle pulleys. Invest Ophthalmol Vis Sci. 1996;37:468 – 472. 19. Demer JL, Poukens V, Miller JM, Micevych P. Innervation of extraocular pulley smooth muscle in monkeys and humans. Invest Ophthalmol Vis Sci. 1997;38:1774 –1785. 20. Clark RA, Miller JM, Demer JL. Location and stability of rectus muscle pulleys inferred from muscle paths. Invest Ophthalmol Vis Sci. 1997;38:227–240. 21. Oh SY, Poukens V, Demer JL. Quantitative analysis of extraocular muscle global and orbital layers in monkey and human. Invest Ophthalmol Vis Sci. 2001;42:10 –16. 22. Demer JL, Oh SY, Poukens V. Evidence for active control of rectus extraocular muscle pulleys. Invest Ophthalmol Vis Sci. 2000;41: 1280 –1290. 23. Haslwanter T. Mathematics of three-dimensional eye rotations. Vision Res. 1995;35:1727–1739. 24. Quaia C, Optican LM. Commutative saccadic generator is sufficient to control a 3-D ocular plant with pulleys. J Neurophysiol. 1998; 79:3197–3215. 25. Tweed D, Vilis T. Geometric relations of eye position and velocity vectors during saccades. Vision Res. 1990;30:111–127. 26. Ruete CGT. Ocular physiology. Strabismus. 1999;7:43– 60. 27. Kono R, Clark RA, Demer JL. Active pulleys: magnetic resonance imaging of rectus muscle paths in tertiary gazes. Invest Ophthalmol Vis Sci. 2002;43:2179 –2188. 28. Demer JL, Clark RA, Miller JL. Magnetic resonance imaging (MRI) of the functional anatomy of the inferior oblique (IO) muscle [ARVO Abstract]. Invest Ophthalmol Vis Sci. 1999;40(4):S772. Abstract nr 4073. 29. Demer JL, Oh SY, Poukens V. The orbital layers of human and monkey oblique extraocular muscles (EOMs) insert on the orbital connective tissue system [ARVO Abstract]. Invest Ophthalmol Vis Sci 2001;42(4):S517. Abstract nr 2781. 30. Demer JL. Mechanical interactions of oblique extraocular muscles (EOMs) with actively controlled rectus pulleys maintain kinematics of linear oculomotor plant. Soc Neurosci Abstr. 2001;27:2071. 31. Demer JL, Kono R, Wright W. Magnetic resonance imaging (MRI) of human extraocular muscles (EOMs) during asymmetrical convergence [abstract]. 2002 Annual Meeting Abstract and Program Planner accessed at www.arvo.org. Association for Research in Vision and Ophthalmology. Abstract 1915. 32. Demer JL. The orbital pulley system: a revolution in concepts of orbital anatomy. Ann NY Acad Sci. 2002;956:17–32. 33. Miller JM, Bockisch CJ, Pavlovski DS. Missing lateral rectus force and absence of medial rectus co-contraction in ocular convergence. J Neurophysiol. 2002;87:2421–2433. 34. Miller JM, Pavlovski DS, Shaemeva I. Orbit 1.8 Gaze Mechanics Simulation. San Francisco: Eidactics; 1999. 35. Porrill J, Warren PA, Dean P. A simple control laws generates Listing’s positions in a detailed model of the extraocular muscle system. Vision Res. 2000;40:3743–3758. 36. Sheehan DC, Hrapchak BB. Theory and Practice of Histotechnology. St. Louis: Mosby; 1973:95–116. 37. Clark RA, Miller JM, Demer JL. Three-dimensional location of human rectus pulleys by path inflections in secondary gaze positions. Invest Ophthalmol Vis Sci. 2000;41:3787–3797. 38. von Noorden GK. Binocular Vision and Ocular Motility: Theory and Management of Strabismus. St. Louis: Mosby; 1996:45–50. 2932 Kono et al. 39. Müller H. Uber einen glatten Muskel in der Augenhohle des Menschen and dur Saugethiere. Zwiss Zool. 1858;9:541. 40. Page RE. The distribution and innervation of the extraocular smooth muscle in the orbit of the rat. Acta Anat. 1973;85:10 –18. 41. Demer JL. Extraocular muscles. In: Jaeger EA, Tasman PR, ed. Clinical Ophthalmology. Vol. 1. Philadelphia: Lippincott; 2000: chap 1. 42. Raphan T. Modeling control of eye orientation in three dimensions. I: role of muscle pulleys in determining saccadic trajectory. J Neurophysiol. 1998;79:2653–2667. 43. Khanna S, Porter JD. Evidence for rectus extraocular muscle pulleys in rodents. Invest Ophthalmol Vis Sci. 2001;42:1986 –1992. IOVS, September 2002, Vol. 43, No. 9 44. Christiano AM, Uitto J. Molecular pathology of the elastic fibers. J Invest Dermatol. 1994;103:53S–57S. 45. Clark RA, Isenberg SJ. The range of ocular movements decreases with aging. J Am Acad Pediatr Ophthalmol Strabismus. 2001;5: 26 –30. 46. Clark RA, Demer JL. Effect of aging on human rectus extraocular muscle paths demonstrated by magnetic resonance imaging. Am J Ophthalmol. In press. 47. Miller JM, Demer JL. Biomechanical modeling in strabismus surgery. In: Rosenbaum AL, Santiago P, eds. Clinical Strabismus Management: Principles and Techniques. St. Louis: Mosby; 1999: 99 –113.