Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
SHOCK
Objectives:
At the completion of this section, the learner will be able to:
Define shock
Differentiate the signs of compensatory shock fro m deco mpensatory shock
List the three forms of distributive shock
The CEN exam contains nine questions on shock which invol ve the following topics:
Card iogenic shock
Distributive shock (e.g. anaphylactic, septic, neurogenic shock)
Hypovolemic
Obstructive (e.g. pericardial tamponade, tension pneumothorax)
Shock (not specific)
Shock (lack of oxygen to the tissues)
o Hypovolemic shock – Decreased cellular perfusion secondary to lack of circulating volu me
o Card iogenic shock – Decreased cellular perfusion secondary to failure of the central pu mp
o Distributive shock – Decreased cellular perfusion secondary to maldistribution of the o xygen to the periphery
o Obstructive shock – Decreased cellu lar perfusion secondary to obstruction of blood into or out of the ventricles (e.g.
pulmonary embolis m, pericard ial tamponade, tension pneumothorax)
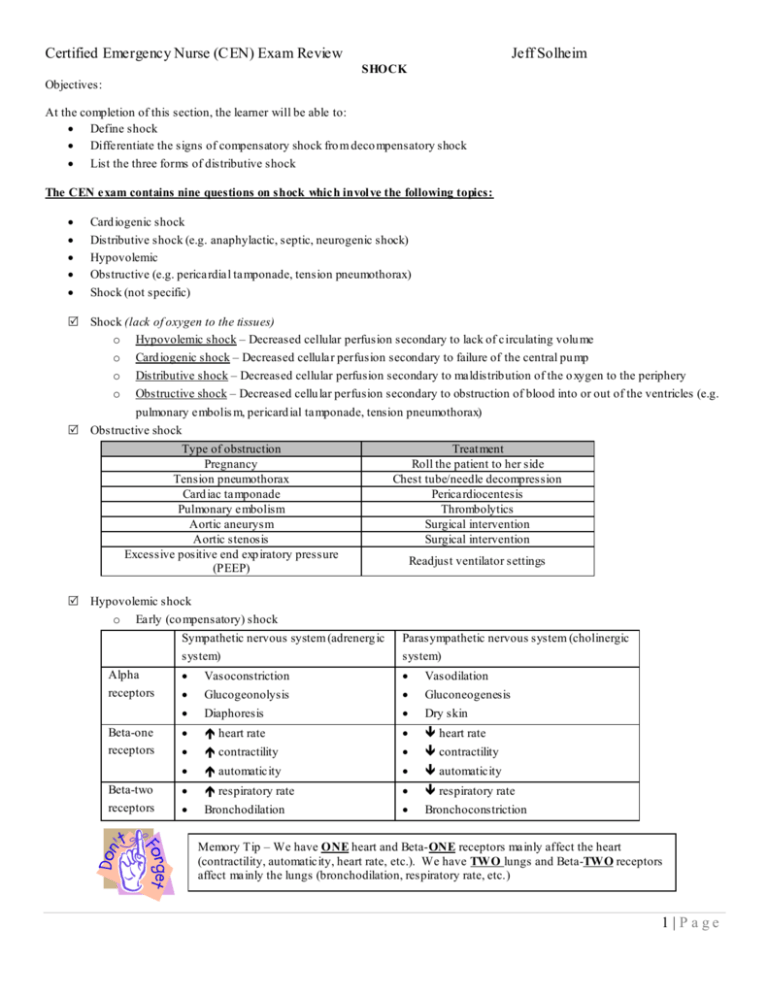
Obstructive shock
Type of obstruction
Pregnancy
Tension pneumothorax
Card iac tamponade
Pulmonary embolism
Aortic aneurysm
Aortic stenosis
Excessive positive end exp iratory pressure
(PEEP)
Treat ment
Roll the patient to her side
Chest tube/needle decompression
Pericardiocentesis
Thrombolytics
Surgical intervention
Surgical intervention
Readjust ventilator settings
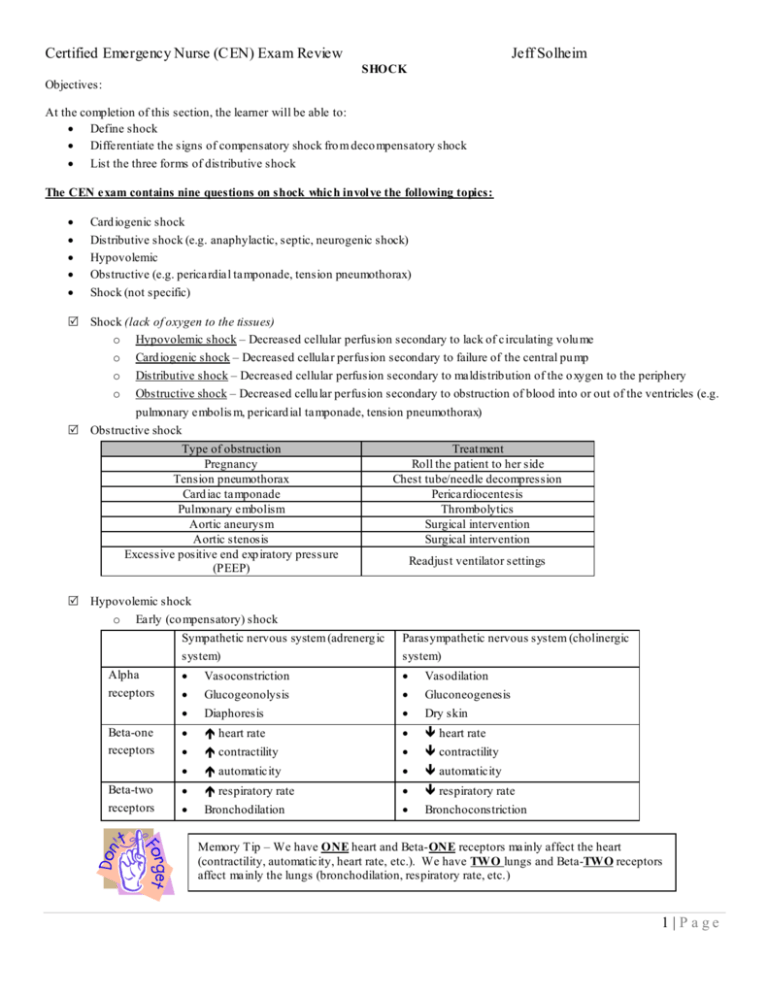
Hypovolemic shock
o Early (co mpensatory) shock
Alpha
receptors
Beta-one
receptors
Beta-two
receptors
Sympathetic nervous system (adrenerg ic
system)
Parasympathetic nervous system (cholinergic
system)
Vasoconstriction
Vasodilation
Glucogeonolysis
Gluconeogenesis
Diaphoresis
Dry skin
heart rate
heart rate
contractility
contractility
automaticity
automaticity
respiratory rate
respiratory rate
Bronchodilation
Bronchoconstriction
Memory Tip – We have ONE heart and Beta-ONE receptors mainly affect the heart
(contractility, automaticity, heart rate, etc.). We have TWO lungs and Beta-TWO receptors
affect mainly the lungs (bronchodilation, respiratory rate, etc.)
1 |P age
Certified Emergency Nurse (CEN) Exam Review
Definiti on:
Agonist – St imu lates a system
Antag onist – Diminishes the response of a system
Jeff Solheim
How would an alpha-adrenergic agonist affect the blood pressure?
How would an anticholinergic affect the pulse rate?
How would a beta-blocker affect the respiratory rate?
Late (deco mpensatory shock
Inflammatory mediators are released in response to either foreign invasion of tissue or tissue damage. They
have three main courses of action:
Vasodilation
Increased capillary permeability
Increased coagulation
Clinical manifestations of shock
Early (co mpensatory) shock
Late (deco mpensatory) shock
Blood pressure
Pulse
Respiratory rate
Arterial blood gases
Skin condition
CNS
Urinary output
o
Treat ment
Flu id replacement
Crystallo ids
Isotonic
solutions
0.9% normal saline (NS)
Lactated Ringers solution (LR)
Hypotonic
solutions
0.45% NS
0.2% NS
Dextrose 5% and water (D5 W)
Hypertonic
solutions
Dextrose 5% in NS
Dextrose 10% in NS
Dextrose 10% in water
Dextrose 5% in 0.45 NS
Dextrose 20% in water
o
o
o
Isotonic crystalloids given at a 3:1 replacement ratio.
Generally, a bolus of 1 – 2 liters of crystalloid solution is ad ministered to a patient with
indications of hypovolemic shock.
Pediatric patients are given boluses at a rate of 20 mL/ kg.
2 |P age
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
Colloids (given at a 1:1 replacement ratio)
Solution
Dextran (co mes in
40, 70, and 75
mo lecular weight)
Notes
May cause anaphylaxis
Increases bleeding times
Carries a risk o f fluid overload
May increase serum amylase levels
Hetastarch
May cause coagulopathies
Carries a risk o f fluid overload
May cause hypocalcaemia
Albumin (5% or
Is a human blood product
25% solutions
Can increase intravascular volume quickly so infuse cautiously and monitor for
available)
indications of flu id overload
Pro motes rapid expansion of blood volume and pro motes retention of volume in
Hypertonic saline
the vascular space.
(7.5%) with
Frequently used to combat hypovolemia in the face of increased intracranial
Dextran 70
pressure.
Blood Products
o ABO Blood types
o
Woman with Rh antibodies may
pass those on to an Rh positive
fetus during pregnancy causing
hemolytic reactions in the fetus.
Care should be taken to prevent
exposure of wo man with Rh
negative blood who may become
pregnant to Rh positive blood to
prevent the development of Rh
antibodies.
o
Type A blood
Antibodies
B
Antigens
A
Type B Blood
A
B
Type O blood
AB
None
Type AB blood
None
AB
O-negative blood is
considered the
“universal donor”
Hemolytic reactions
Early signs
Late signs
Anxiety
Restlessness
Nausea and Vo miting
Flushing
Chest/Lumbar Pain
Tachypnea
Fever
Cyanosis
Hemoglobinemia
Hemoglobinuria
Heat along the vein receiv ing
the transfusion
Tachycardia
Chills
Shock
Rh co mpatibility
Rh positive blood is born with Rh antigens but no Rh antibodies and should
ideally receive Rh positive blood.
Rh negative indiv iduals are born without Rh antigens and Rh antibodies. If they
receive Rh positive blood, they will develop Rh antibodies which will cause a
transfusion reaction in future transfusions.
3 |P age
Certified Emergency Nurse (CEN) Exam Review
Blood component
Whole blood
Packed red blood
cells
Fresh frozen
pl asma
Platelets
Cryopreci pitate
Jeff Solheim
Types of blood components
Notes
Provides all blood components although clotting factors deteriorate if product is older
than 24 hours.
Must be ABO co mpatib le
Co mes in 500 mL volu mes
Give 20 mL/ kg in children
Elevates hemoglobin levels by 1 g/dL and hematocrit by 3% per unit
Best blood product to rapidly elevate o xygen carrying capacity
Must be ABO co mpatib le.
Co mes in 250 mL volu mes
Give 10 mL/ kg in children
The flu id portion of one unit of hu man blood that has been frozen solid within six hours
of collect ion to preserve clotting factors.
Useful for hypovolemia co mbined with hemorrhage caused by clotting deficiencies
Must be ABO co mpatib le.
Takes 20 minutes to thaw and must be used within 6 hours of thawing.
Does not need to be ABO co mpatible
Used for conditions such as hemophilia, von Willebrand disease, hypofibrinogenemia
and factor XIII deficiency.
Multiple units may be ordered (one unit fo r every 7 – 10 kg in children)
Prepared fro m plas ma and rich in Factor VIII, fibrinogen, von Willebrand factor, and
Factor XIII.
Is frequently given for bleed ing disorders such as hemophilia and disseminated
intravascular coagulation.
Must be ABO co mpatib le
End points to fluid resuscitation
Improvement in level of consciousness, condition of skin and capillary refill
Decreased pulse and increased blood pressure
Urinary output
o 0.5 mL/ kg/hour (adults)
o 1 – 2 mL/ kg/hour (infants)
Seru m pH and base excess levels returning to normal ranges
A stable or decreasing serum lactate level
Distributive shock
o
Neurogenic shock (loss of sympathetic tone)
Causes:
Spinal cord in juries above T4 – T6
Brain injury
Spinal o r general anesthesia
CNS depressants
Hypoxia
Lack of g lucose or excessive insulin (insulin
shock)
Vasovagal syncope
4 |P age
Certified Emergency Nurse (CEN) Exam Review
Sympto ms
Jeff Solheim
Vasodilation
Gluconeogenesis
Dry skin
Bradycardia
Decreased contractility
Decreased automaticity
Bradypnea
Bronchoconstriction
Treat ment
1 – 2 Liter flu id bolus for hypovolemia, consider vasoconstrictor such as phenylnephrine
if bo luses ineffective
Atropine for lo w heart rate
Assist respirations as needed
o Septic shock
Hyperdynamic sepsis
Hypodynamic sepsis
Malaise, not feeling well,
Mentati on
Decreasing LOC, stupor and coma
tiredness, restlessness
Cutaneous
Warm, flushed dry skin
Cold, clammy, pale, mottled skin
manifestations
Heart Rate
Tachycardia, full bounding pulses
Tachycardia, weak, thready pulse
Respiratory Rate
> 20/ minute
Shallo w and tachypneic
Urine Output
Decreased
Decreased or anuria
Co mbined metabolic and respiratory
Aci d-base values
Respiratory alkalosis
acidosis
Body
Fever/Shaking and chills
Hypothermic and mottled
Temperature
o
Treat ment
Flu id resuscitation
Crystallo id boluses
Vasopressors
Inotropes
Source control
Identify and remove potential infected sources
Wound cultures
o
Antimicrobial therapy
Consider Drotrecogin Alfa (Xigris)
Anaphylactic shock
Mil d symptoms (normal
BP, minimal respiratory
distress)
Give 0.2 – 0.3 mL
1:1,000 epinephrine SQ/IM
Repeat epinephrine
every 5 – 10 minutes
as needed
Maintai n ABC’s – oxygen,
intubation, surgical airway,
flu id boluses, positive
inotropes
Severe symptoms
(hypotensive, respiratory
distress –Give 0.1 – 0.5 mL
1:10,000 ep inephrine IV
Secondary treatments
Antihistamines (e.g.
Benadryl)
Beta-2-agonists (Albuterol)
Corticosteroids
5 |P age
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
Practice Questions
A patient sustaining mu ltip le trau matic in juries presents with a BP of 50/32 mm Hg, a pulse of 146/ minute, a capillary refill of 4
seconds, and no urinary output. Appropriate volume resuscitation is:
a)
b)
c)
d)
D5 W at a rate of 3 mL for every 1 mL o f blood loss
Hetastarch at a rate of 3 mL for every 1 mL of b lood loss
Blood replacement at a rate of 1 mL for every 1 mL of b lood loss
Lactated Ringers solution at a rate of 1 mL for every 1 mL of b lood loss
An overdose which results in profound central nervous system depression may result in :
a.
b.
c.
d.
Distributive shock
Obstructive shock
Card iogenic shock
Hypovolemic shock
Which of the follo wing assessment parameters is most consistent with early co mpensated hypovolemic shock?
a)
b)
c)
d)
Respiratory alkalosis and cool clammy skin
Hypoglycemia and decreased urinary output
Deep, rap id respirations and hyperactive bowel sounds
Near-normal systolic blood pressure and abnormally lo w diastolic blood pressure
Which of the follo wing parameters indicates that fluid resuscitation for hypovolemia has been effective in a 200 (90 kg) poun d
patient?
a)
b)
c)
d)
A declining seru m pH
A narrowing pulse pressure
A declining seru m lactate level
A urinary output of 30 milliliters per hour
ANSWERS: C, A, A, C
6 |P age
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
HEMATOLOGICAL DISORDERS
Disorders of the red blood cells
Polycythemia (elevation in red blood cell count – often secondary to hypoxia)
Co mmon causes:
Living or v isiting a high altitude
Prolonged physical activ ity associated with hypoxia (e.g. – running a marathon)
Erythrocytosis – polycythemia secondary to hypoxic diseases such as COPD
Signs and symptoms
Fatigue
Bru ising
Sensation of warmth in the limbs
Treat ment
Supportive therapy
Treat underlying causes of erythrocytosis
Polycythemia vera (A condition with an overactive bone marrow resulting in high red blood cell, high white blood cell
and high platelet counts. Is a genetic disease which typically affects middle-aged Jewish men)
Sympto ms: Elevated blood counts which may cause heart failure and hypoxia.
Treat ment
Admin istration of radiat ion phosphorus
Phlebotomy to remove who le blood and replace with normal saline.
Anemia (A decreased red blood cell count)
Treat ment
Type of
Treat ment
Deficiency
Blood Loss
Stem blood loss as well as fluid and blood replacement
Iron
• Oral iron therapy.
•
Iron is caustic to GI tract, may turn stools green or dark black
• Iron is constipating
• Take iron with acid ic substance, not with antacids
Vitamin B
This deficiency is usually secondary to lack of the intestinal en zy me needed to absorb it, therefore,
12
oral vitamin B is unlikely to be effective and subcutaneous vitamin B will be given
12
12
Folic acid
This is almost always secondary to nutritional deficits and patients should be encouraged to increased
fresh fruits and vegetables in their d iets and to take folic acid sup plements. (Note that cooking
vegetables cooks out the folic acid ).
All anemias
Maximize o xygenation of t issue via oxygen administration
Sickle Cell Disease (congenital hemolytic anemia that occurs mainly in those of West African descent)
Factors which may precipitate sickling:
Low o xygen concentrations
Infection
Acidosis
Dehydration
Exposure to cold
Clin ical manifestations
Sudden explosive abdominal, chest, back and joint pain
Splenic ischemia can lead to increased susceptibility to infection
Heart ischemia can lead to acute coronary syndromes
Priapism
Ulcers of the lower ext remities and long thin extremities
7 |P age
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
Treat ment
Treat the underlying cause (IV flu ids for dehydration, sodium bicarbonate for acidosis, antibiotics for infect ion,
etc.)
High flow o xygen (may reverse as many as 80% of sickled cells)
Pain control
Support extremit ies on pillows
Oral hydro xyurea
Discharge Instructi ons for Sickle Cell Disease:
Warm moist heat to affected areas to reduce pain and swelling
Keep well hydrated and rested
Exercise regularly
Avoid high altitudes or flying in non-pressurized aircraft
Limit exposure to the cold
Seek medical help for shortness of breath, weakness, fatigue, chest, abdominal, or back pain, or swelling of the hands
and feet.
Disorders of the white b lood cells
Neutropenia (A decrease in the white blood cells responsible for protecting the body from bacteria)
Co mmon causes:
Cancer treat ment such as chemotherapy or radiation
Immunosuppressive therapy after organ transplantation
Immunosuppressive diseases such as acquired immune deficiency syndrome
(AIDS)
Nutrit ional deficits
Clin ical manifestations
Increased susceptibility to infect ion (especially g ram-negative bacteria)
Blunted responses to infection (decreased redness, swelling, edema and pus formation.)
Treat ment considerations
Reverse Isolation
Avoid the use of indwelling catheters
Dilute IV med ications, administer slowly
Culture all potentially infected sites
Early init iation of antib iotics
Acetaminophen (Tylenol) alternated with ibuprofen (Motrin , Advil) every 2 – 3 hours to decrease fever and
drug toxicity.
Admin ister drugs to stimulate neutrophil p roduction:
The only sign of infection in a
neutropenic patient may be
fever. Therefore fever in the
neutropenic patient constitutes
a medical emergency.
Granulocyte colony-stimulat ing factor (Neupogen)
Granulocyte-macrophage colony-stimulating factor (Leukine, Prokine)
Hu man Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS) – (A retrovirus spread via
direct contact with an infected person’s blood or body secretions.)
Sympto ms:
2 – 6 weeks post exposure: Sy mptoms similar to mononucleosis.
Onset of AIDS - Changes in level o f consciousness ranging fro m withdrawn to demented, indicat ions of
wasting, volume depletion and weakness. The comp lete blood count will likely show anemia, ly mphopenia and
thrombocytopenia. Indications of infections such as oral candidiasis, herpes zoster, tinea and other skin rashes.
8 |P age
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
Diagnosis: ELISA test, Western Blot test (consider informed consent)
Treat ment: A variety of antiviral medications can significantly slow
down the progression of this disease, but it is not curable. Treat ment
is main ly symptomat ic.
Leukemia (Excessive production of abnormal, immature white blood cells.
Although the number of white blood cells increases, they do not function
normally and protection from infection diminishes.)
•
•
•
Signs and symptoms:
Fatigue
Fever
Weight loss
Bone pain
Elevated uric acid levels
Ly mph node enlargement
Hepatomegaly, and splenomegaly
•
Discharge teaching for
HIV/ AIDS
Disinfect all body fluid spills
with 10% solution of bleach
in water.
Practice safe sex
Do not share drug
paraphernalia, razors, and
toothbrushes.
Avoid individuals who are ill.
The same precautions that were introduced for neutropenia should be
maintained for leukemia.
Disorders of the clotting functions
Idiopathic thrombocytopenia purpura (ITP) – (An autoimmune disorder that occurs most commonly in chidren between the
ages of 2 to 4 resulting in a decreased platelet count. The disease often occurs several weeks after a viral in fection or
immun izat ions.)
Signs and symptoms: Indicat ions of bleeding such as bruising, petechiae, purpura, epistaxis, b leeding gums,
gastrointestinal bleeding, and hematuria.
Treat ment:
Many patients need nothing more than careful observation
Severe cases may require glucocorticoids and immune globulins to elevate platelet co unts
Thrombocytosis (abnormally elevated platele count which leads to an increased risk of spontaneous clot formation)
Signs and symptoms
May be asymptomat ic
Burning sensation or redness in the extremities that may be relieved by aspirin
Treat ment
Monitor for pulmonary embolus, myocardial infarct ion, stroke and deep vein thrombosis.
Aspirin
Disseminated intravascular coagulation (DIC) - (DIC is not a disease, but rather an abnormal activation of the body’s
clotting system that signals severe underlying problems. It involves both abnormal clotting and abnormal bleeding).
Abnormal clotting with signs such as metabolic acidosis, mottling, gangrene and organ failure.
Abnormal anticoagulation with bleed ing such as bruising, petechiae, purpura, epistaxis, bleeding gums, gastrointestinal
bleeding, and hematuria.
Laboratory values with DIC:
Platelet count
Prothromb in time
Partial thro mboplastin time
Fibrinogen levels
D-Dimer
Hemoglobin
Hematocrit
9 |P age
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
Treat ment
Treat the underlying cause
Control bleed ing
Limit venipuncture
Apply pressure dressings or sandbags to active bleeding sites
Handle patient gently
Pharmacological interventions
Heparin
Reco mbinant human activated protein C (rhAPC)
Aminocaproic acid (A micar)
Hemophilia
Name of disorder
Alternate name
Cause of disorder
Notes
Clin ical
man ifestations
Hemophilia A
Hemophilia B
Hemophilia C
Classic hemophilia
Christmas disease
Rosenthal’s syndrome
Variant form of Factor VIII Variant form of Factor IX
Variant form of Factor XI
Congenital sex-linked disorders that affect males
• Most commonly b leed into soft tissues, muscles or weight bearing joints (knees,
elbows and ankles)
• Can also bleed into oral/nasal mucosa, urinary system, GI tract and CNS (usually
following trauma)
Treat ment
Hemoarthrosis or hemato ma
Ice
Co mpression dressing
Immobilization
Elevation
Lacerat ions
Topical thro mbin
Observe for 4 hours post suturing
Venipuncture - Ho ld pressure for a minimu m of 5 minutes
Never give an IM in jection
Purified factor VII, IX or XI
Fresh frozen p lasma and cryoprecip itate
Practice Question
Which of the follo wing patients is at highest risk for developing idiopathic thrombocytopenia purpura (ITP)?
a)
b)
c)
d)
A 3-year-o ld whose last chicken po x has just disappeared
A 52-year-o ld patient who is on daily aspirin fo r heart disease
A 17-year-o ld with an infected laceration to the dorsum of the right hand
An 80-year-old with a fractured hu merus after falling down a flight of stairs
Which of the follo wing statements, made by a patient being discharged home with leukemia, indicates they have understood their
discharge instructions?
a)
b)
c)
d)
“I will avoid exercising to decrease stress on my body.”
“I will change my tampons at least hourly to prevent infection.”
“I will call the doctor if my temperature exceeds 100°F (38°C).”
“I will avoid taking aspirin or nonsteroidal anti-inflammatory drugs to decrease the risk of bleeding.”
Answers: A C
10 | P a g e
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
REFERENCES
American Heart Association. (2010, November). Adult Advanced Cardiovascular Life Support: 2010 A merican Heart Association
Gu idelines for Card iopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation , pp. S729 - S767.
Baird, M . S., Hicks-Keen, J., & Swearingen, P. L. (2005). Manual to critial care nursing: Nursing interventions and collaborative
management. St. Louis MO: Mosby.
Beall, B. D. (2005). Salicylate overdose. In E. L. Mitchell, & R. Medzon (Eds.), Introduction to Emergency Medicine (pp. 469 - 473).
Philadelphia, Pennsylvania: Lippincott, Williams and Wilkins.
Carter, J. S. (2004, November 2). Atoms, molecules, water and pH. Retrieved July 27, 2008, fro m File atom H2O:
http://biology.clc.uc.edu/courses/bio104/atom-h 2o.htm
Center for disease control and prevention. (2008, February 22). Bacterial vaginosis. Retrieved September 29, 2008, fro m Center for
disease control and prevention: http://www.cdc.gov/STD/BV/ STDFact -Bacterial-Vag inosis.htm#Treatment
Center for disease control and prevention. (2007). Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents
in Healthcare Settings 2007 . Retrieved April 15, 2008, fro m Center for d isease control and prevention:
http://www.cdc.gov/ncidod/dhqp/gl_isolation.html
Center for Disease Control. (2007, September 21). Traumatic Brain Injury. Ret rieved June 2, 2008, fro m National Center for in jury
prevention and control: http://www.cdc.gov/ncipc/factsheets/tbi.htm
Corbett, J. V. (2004). Laboratory tests and diagnostic procedures (6 ed.). Upper Saddle River: Pearson Prentice Hall.
Danis, D., Blansfield, J., & Gervasini, A. (2007). Handbook of clinical trauma: the first hour (4 ed.). St. Lou is: Mosby Elsevier.
Emergency Nurses Association. (2004). Emergency Nursing Pediatric Course Provider Manual (3 ed.). Des Plaines: Emergency
Nurses Association.
Emergency Nurses Association. (2007). Trauma Nursing Core Course Provider Manual (6 ed.). Des Plaines Il: Emergency Nu rses
Association.
Ferrell, J. J. (2007). Forensic aspects of emergency nursing. In K. S. Hoyt, & J. Selfridge-Thomas (Eds.), Emergency Nursing Core
Curriculum (6 ed., pp. 1025 - 1032). Philiadelphia: Saunders - Elsevier.
Gray, R. O. (2009). Hypertension. In J. A. Marx, R. S. Hockberger, & R. M. Walls (Eds.), Rosen's Emergency Medicine (7 ed.). St.
Louis: Mosby-Elsevier.
Hebra, A. (2006, May 5). Intestinal volvulus. Retrieved Ju ly 28, 2008, fro m eMedicine: http://www.emedicine.co m/ped/topic1205.htm
Hoek, T. L., Morrison, L. J., Shuster, M., Donnino, M., Sinz, E., Lavonas, E. J., et al. (2010). Part 12: Cardiac Arrest in Special
Situations: 2010 A merican Heart Association Gu idelines for Cardiopulmonary Resuscitation and Emergency Card iovascular Care.
Circulation , S829 - S 861.
Honig man, B. K. (2005). Emergency Medicine (2 ed.). (mitchell, & e. L. Mitchell, Eds.) balt imore: Lippincott, Williams, Wilkins.
Hospital Incident Command System. (2008, Ju ly 28). Retrieved August 11, 2008, fro m Western Safety Products:
http://images.google.com/img res?imgurl=http://www.westernsafety.com/HICS new/hics_color2.jpg&imgrefu rl=http://www.westernsafety.com/HICSnew/hics2006pg1.ht ml&h=1315&w=720&sz=134&hl=en&start=1&u m=1&tbnid=uZww2DkgFtensM:&tbnh=150&tbnw=82&prev=/
images%3Fq%3D
Hoyt, K. S., & Selfridge-Tho mas, J. (Eds.). (2007). Emergency Nursing Core Curriculum (6 ed.). St. Lou is: Saunders Elsevier.
11 | P a g e
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
International Critical Incident Stress Foundation Inc. (2004). Related articles and resources. Retrieved August 11, 2008, fro m
International Critical Incident Stress Foundation Inc.: http://www.icisf.org/articles/
Kaplow, R., & Hardin, S. R. (2007). Critical Care Nursing. Boston: Jones and Bartlett Publishers.
Klein man, M. E., Chameides, L, Schexnayder, S. M ., Samson, R. A., Hazinski, M . F. Atkins, K. L.. et al.. (2010, November).
Pediatric Advanced Life support. Circulat ion 122 , pp. S876 - S908.
Kowalak, J. P., & Welsh, W. (Eds.). (2003). Handbook of diagnostic tests (3 ed.). Baltimore: Lippincott Williams and Wilkins.
Life Source. (2008). Organ and Tissue Donation Manual. St. Paul: Life Source.
Link, M. S., Atkins, D. L., Passman, R. S., Halperin, H. R., Samson, R. A., White, R. D., et al. (2010). 2010 A merican Heart
Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care: Part 6: Electrical Therapies.
Circulation , 122, S706 - S719.
Marino, P. L. (2007). ICU book (3 ed.). Philidelphia: Lippincott Williams and Wilkins.
Marx J. A., R. S. Hockberger, & R. M. Walls (Eds.) (2009), Rosen's Emergency Medicine (7 ed.). St. Louis: Mosby-Elsevier.
McCance, K. L., & Heuther, S. E. (2002). Pathophysiology: The biologic basis for disease in adults and children. St. Louis: M osby.
Mitchell, E. L., & Medzon, R. (2005). Introduction to emergency medicine. Baltimo re : Lippincott Williams and Wilkins.
National institutes of health. (2007, May 25). Preterm labor and birth. Retrieved October 2, 2008, fro m National Institute of child
health and human development: http://www.n ichd.nih.gov/health/topics/Preterm_ Labor_and_Birth.cfm
Neu mar, R. W., Otto, C. W., Lin k, M. S., Kronick, S. L., Shuster, M., Callaway, C. W., et al. (2010). Part 8; Adult Advanced
Card iovascular Life Support: 2010 A merican Heart Association Guidelines for Card iopulmonary Resuscit ation and Emergency
Card iovascular Care. Circulation 122 , S729-767S.
Niemann, J. T., & Squire, B. (2009). Imp lantable Cardiac Devices. In J. A. Marx, R. S. Hockberger, & R. M. Walls (Eds.), Rosen's
Emergency Medicine (7 ed.). St. Louis: Mosby-Elsevier.
Newberry, L. (Ed.). (2003). Sheehy's Emergency Nursing (5 ed.). St . Louis: Mosby.
Newberry, L., & Criddle, L. (Eds.). (2005). Sheehy's manual of emergency care (6 ed.). St. Louis: Elsevier Mosby.
Niemann, J. T., & Squire, B. (2009). Imp lantable Cardiac Devices. In J. A. Marx, R. S. Hockberger, & R. M. Walls (Eds.), Rosen's
Emergency Medicine (7 ed.). St. Louis: Mosby-Elsevier.
O'Toole, M. T. (Ed.). (2003). Encyclopedia and dictionary of medicine, nursing and allied health (7 ed.). St. Louis: Saunders Elsevier.
Peit zman, A. B., Rhodes, M., Sch wab, C. W., Yealy, D. M., & Fabian, T. C. (2007). The trauma manual: trauma and acute care
surgery. Philadelphia : Lippincott Williams and Wilkins.
Peberdy, M. A., Callaway, C. W., Neu mar, R. W., Geocadin, R. G., Zimmerman, J. L., Donnino, M., et al. (2010). Post -Cardiac Arrest
Care. Circulation , 122, 768-786.
United Net work for Organ Sharing. (2008, Ju ly 16). Membership. Ret rieved July 16, 2008, fro m United Netwo rk for Organ Sharing:
http://www.unos.org/whoWeAre/membership.asp
United States Depart ment of Health and Hu man Serv ices. (2003, May). OCR Privacy Brief. Retrieved May 17, 2008, fro m Su mmary
of the HIPAA privacy rule: http://www.hhs.gov/ocr/privacysummary.pdf
Urden, L. D., Stacy, K. M., & Lough, M. E. (2002). Critical Care Nursing (4 ed.). St. Louis: Mosby.
12 | P a g e
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
ValueOpt ions New Jersey. (n.d.). What is HIPAA? Retrieved May 17, 2008, fro m ValueOptions New Jersey:
http://www.vonewjersey.com/ VONJDocu ments/WhatIsHIPAA.pdf
13 | P a g e



![Electrical Safety[]](http://s2.studylib.net/store/data/005402709_1-78da758a33a77d446a45dc5dd76faacd-300x300.png)

