Here Follows Background Information to the DRIs
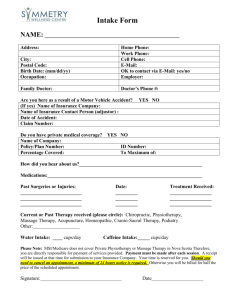
advertisement

MACRONUTRIENTS Macronutrients, particularly fats and carbohydrate, are known to play a role in the risk of chronic diseases. People can consume moderate levels of these nutrients without risk of adverse health effects. However, increased risk of disease may occur with the chronic consumption of diets that are too low or too high in these macronutrients. This is based on evidence, which relates to clinical endpoints e.g. risk of coronary heart disease, diabetes, cancer and obesity. Nevertheless, these are thought to be associations rather than distinct endpoints, since there may be factors other than diet that may contribute to chronic disease. It was not, therefore, possible to determine a defined level of intake at which chronic disease may be prevented or may develop. Acceptable Macronutrient Distribution Ranges (AMDR) Based on the evidence to suggest a role in chronic diseases as well as information to ensure sufficient intakes of essential nutrients, AMDRs have been estimated. An AMDR was defined as a range of intake for a particular energy source that is associated with reduced risk of chronic disease while providing adequate intakes of essential nutrients. A key feature of each AMDR is that it has a lower and upper boundary, some determined mainly by the lowest or highest value for the other, judged to have an expected impact on health. If an individual consumes below or above this range, there is potential for increasing the risk of chronic diseases shown to affect long-term health as well as increasing the risk of inadequate intake of essential nutrients. The AMDR for fat and carbohydrate was estimated to be 20-35 and 45-65% of energy, respectively for all adults (see Summary DRI Tables). These AMDRs were estimated based on evidence indicating a risk for coronary heart disease (CHD) at low intakes of fat and high intake of carbohydrate and based on evidence for increased risk of obesity and its complications, including CHD, with high fat intake. Although the evidence suggesting that a low or high fat intake during childhood can lead to increased risk of chronic diseases later in life is less clear, the AMDRs for fat have been estimated for children who are primarily based on a transition from a high fat intakes that occurs during infancy to the adult AMDR for fat. The AMDR for fat has been set at 30–40% of energy for children 1–3 years and 25– 35% of energy for children 4–18 years, while the AMDR for carbohydrate is 45–65% of energy. The AMDR for protein is 10–35%, 5–20% and 10–30% of energy for adults, young and older children, respectively. Based on usual median intakes of energy, it is estimated that a lower boundary level of 5% of energy will meet the AI for linoleic acid. An upper boundary for linoleic acid is set at 10% of the energy for 3 reasons: • Individual dietary intake of linoleic acid in the North American population rarely exceeds 10% of energy • Epidemiological evidence for safety of intakes greater than 10% of energy are generally lacking • Higher intakes of linoleic acid can create a pro-oxidant state that may predispose to several chronic diseases such as CHD and cancer • Therefore, an AMDR of 5-10% of energy is suggested for n-6 polyunsaturated fatty acids The AMDR for α-linolenic acid was set at 0.6-1.2 percent of energy. The lower boundary of the range meets the AI for α-linolenic acid. The upper boundary corresponds to the highest intakes from foods consumed by individuals in the US and Canada. A growing body of literature suggests that diets higher in α-linolenic acid, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) may afford some degree of protection against CHD. Because the physiological potency of EPA and DHA is much greater than that for α-linolenic acid, it was not possible to estimate one AMDR for all n-3 fatty acids. Up to 10% of the AMDR can be consumed as EPA and/or DHA. Due to the limited available data, an AMDR for n-9 polyunsaturated fatty acids was not set. Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 13 A maximal intake of 25% or less of energy from added sugars has been recommended. This maximal intake was set so as to ensure an adequate intake of micronutrients that are not present in foods and beverages that contain added sugars. A UL was not set for saturated fatty acids, trans fatty acids and cholesterol. Caution Although a specific UL was not set for any of the macronutrients, the absence of definitive data does not signify that people can tolerate chronic intakes of these substances at high levels. Like all chemical agents, nutrients and other food components can produce adverse effects, if intakes are excessive. Therefore, when data are extremely limited or conflicting, extra caution may be warranted in consuming levels significantly above that found in typical food-based diets. Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 14 Energy The basis on which energy requirements were established The Estimated Energy Requirement (EER), a new term, which is similar to the EAR, was defined as the average dietary energy intake that is predicted to maintain energy balance in a healthy adult of a given age, gender, weight, height and level of physical activity, consistent with good health (Table 3; see also Summary of DRI Tables). In children and pregnant and lactating women, the EER includes the needs associated with the deposition of tissues or the secretion of milk at rates consistent with good health. To calculate the EER, prediction equations for normal weight individuals [Body Mass Index (BMI) 18.5–25kg/m2] aged 0–100 years were developed from data on total daily energy expenditure measured by the doubly labelled water technique (DLW). A DLW database was also developed for overweight/obese children and adults. There were insufficient data to develop a similar database for overweight/obese pregnant or lactating women. Physical Activity Level (PAL) categories were defined as follows: • Sedentary : (PAL ≥ 1.0 - < 1.4) • Low active : (PAL ≥ 1.4 - < 1.6) • Active : (PAL ≥ 1.6 - < 1.9) • Very active : (PAL ≥ 1.9 - < 2.5) There are no RDAs for energy, since energy intakes above the EER would be conducive to weight gain. Additionally, the UL concept does not apply to energy because any energy intake above the EER would lead to undesirable and potentially hazardous gain in weight. Other indicators considered, but not used, for estimating energy requirements • • Reported Energy Intake: It is now widely recognised that reported energy intake in dietary surveys underestimates usual energy intake. Convincing evidence of underreporting is supported by the DLW technique. There is also no objective evidence for the existence of “small eaters”, individuals who can survive long-term on the low energy intake that they report in dietary survey. It is no longer tenable to base energy intake on self-reported food consumption data. Factorial Approach: The factorial approach used in setting the RDA for energy in the past on the basis of Total Energy Expenditure (TEE) was deemed inappropriate, because of the wide range of physical activities performed during normal life which cannot be accurately measured, the constraints imposed on the subjects while performing a given physical activity, which can be measured, increased energy expenditure, and the energy expenditure of spontaneous activity, e.g. fidgeting, which may amount to significant energy expenditure. Special considerations • Overweight and Obesity: EERs were not defined for overweight/obese individuals, since EERs are values appropriate for the maintenance of long-term good heath. Instead, weight maintenance TEE values are given, adjusted for age, height, gender and various PALs, which were derived from the combined DLW database of normal and overweight/obese individuals. Equations were generated to predict TEE in overweight/obese adult men and women BMI ≥ 25). PAL categorisation (PAL >1.0 and < 2.5) was determined using the adults’ observed Basal Energy Expenditure (BEE). The TEE for overweight/obese individuals is higher than normal-weight adult men and women which implies that overweight/obese individuals, who do not wish to lose weight, need to consume more energy in order to maintain their weight, i.e. the overweight/obese weight, than individuals within the normal weight range. Equations for TEE during underfeeding have been used to predict the anticipated reduction in energy to achieve a given level of weight loss, in the absence of any change in energy expenditure for physical activity. For example, a weight loss of 0.45 – Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 15 0.90 kg/week (65–130g/day) is equivalent to a body energy loss of 468–936kcal/day, because the energy content of weight loss averages 7.2kcal/day (i.e. 75% fat containing 9.25kcal/g and 25% fat fee mass containing 1kcal/g). Taking into account the decrease in TEE due to weight loss (16.6kcal/Kg) and due to negative energy balance (8.4% of the initial TEE), the total expected reduction of TEE after 10 weeks of dieting is predicted to be 376–542 kcal/day for an individual with an initial weight maintenance TEE of 2500kcal/day. • • The CDC definition of “risk of overweight” and “overweight” above the 85th and 95th percentile for children has been accepted in the report. In addition, children under the age of two years should not be placed on energy-restricted diets. Separate equations for TEE were developed for children, in a manner similar to that for adults, who need to loose weight. A weight reduction of 0.45kg/month would be considered small enough to be achievable either by energy restriction or increased physical activity or, preferably, both. Undernutrition: In an underweight adult (BMI<18.5) the additional energy intake to normalise body weight will depend on the initial deficit and the desired rate of recovery. The average energy cost of tissue synthesis and deposition for catch-up-growth are reported to amount to 5kcal/g tissue. Median weight for height should be used as a target for recovery. These estimates apply to children with a weight deficit relative to height. In stunted children, weight may be adequate for height and unless an increased energy intake elicits both gains in weight and height, the child may become overweight without correcting the height. Physical Activity: With minor exceptions, dietary recommendations for athletes were not distinguished from those of the general population and vice versa. The amount of dietary energy from the recommended nutrient mix should be adjusted to achieve and maintain optimal body weight for competitive athletes and others engaged in similarly demanding activities. Relationship of energy intake to chronic disease EERs can be estimated for four levels of activity from the equations provided. The active PAL is recommended to maintain health and decrease risk of chronic disease and disability (Table 3). Adverse effects of energy overconsumption Safety Weight changes invariably occur with increased or decreased energy intake. It is likely that, for most individuals, the principal mechanism for maintaining body weight is by controlling food intake rather than physical activity. Since it would be expected that energy intake in excess of EER results in weight gain and the associated increased in morbidity, the UL method is not applicable to energy. The LOAEL would be any intake in excess of the EER that results in weight gain. Caution Weight gain to a BMI in excess of 25 is associated with an increased risk of premature mortality, and morbidity risk for type II diabetes, hypertension, coronary heart disease, stroke, gallbladder disease, osteoarthritis, and some types of cancer. Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 16 Table 3. The DRIs for energy by active individuals* [kcal (kJ)]: Gender ♂ ♀ Pregnancy Lactation Age Years 0 – 0.5 0.5 - 1 1–2 3–8 9 – 13 14 – 18 19 – 30 31 – 50 51 – 70 > 70 0 – 0.5 0.5 - 1 1–2 3–8 9 – 13 14 – 18 19 – 30 31 – 50 51 – 70 > 70 ≤ 18 1st trimester ≤ 18 2nd trimester ≤ 18 3rd trimester 19 – 50 1st trimester 19 – 50 2nd trimester 19 – 50 3rd trimester ≤ 18 1st 6 months ≤ 18 2nd 6 months 19 – 50 1st 6 months 19 – 50 2nd 6 months Active PALa EER kcal/day (kJ) 570 (2 394) 743 (3 121) 1 046 (4 393) 1 742 (7 316) 2 279 (9 572) 3 152 (13 238) 3 067b (12 881) 3 067b (12 881) 3 067b (12 881) 3 067b (12 881) 520 (2 184) 676 (2 839) 992 (4 166) 1 642 (6 896) 2 071(8 698) 2 368 (9 946) 2 403c (10 093) 2 403c (10 093) 2 403c (10 093) 2 403c (10 093) 2 368d (9 946) 2 708d (11 374) 2 820d (11 844) 2 403ce (10 093) 2 743ce (11 521) 2 855ce (11 991) 2 698f (11 332) 2 768f (11 626) 2 733cg(11 479) 2 803cg(11 773) ♀ female ♂ male * for healthy moderately active Americans and Canadians a PAL= Physical Activity Level b Subtract 10kcal/day for males for each year of age above 19 years c Subtract 7kcal/day for females for each year of age above 19 years d Adolescent female EER plus change in TEE (total energy expenditure) plus pregnancy energy deposition e Adult female EER plus change in TEE plus pregnancy energy deposition f Adolescent female EER plus milk energy output minus weight loss g Adult female EER plus milk energy output minus weight loss Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 17 Physical Activity General recommendations Some benefits of physical activity can be achieved with a minimum of 30 minutes of moderate intensity activity most days of the week. However, 30 minutes of regular daily activity is insufficient to maintain body weight in adults in the recommended BMI range (18.5–25kg/m2) and derive all the identified health benefits fully. Hence, to prevent weight gain and to accrue additional weight-independent health benefits of physical activity, 60 minutes of daily moderate intensity activity (e.g. walking/jogging at 6–8km/hour) was recommended in addition to the activities required by a sedentary lifestyle. This amount of physical activity leads to an “active” lifestyle corresponding to PAL greater than 1.6, consistent with those observed in the DLW database utilised to derive the energy requirements. For children, the physical activity recommended was also 60 minutes or more of daily activity and exercise. Increasing the Energy Expenditure of Physical Activity (EEPA) needs to be considered in determining the energy intake to achieve energy balance in weight stable individuals, and adequate growth and development in children. Body weight serves as the ultimate indicator of adequate energy intake. Increasing EEPA or maintaining an active lifestyle provides an important means for individuals to balance food energy intake with total energy expenditure. Recommendations for nutrient selection for very active people, such as athletes and labourers, were considered as generally the same as those for the population at large. With regard to the impact of activity level on energy balance, modifications in the amounts, type, and frequency of food consumption may need to be considered within the context of overall health and fitness objectives. Dietary considerations for active people need to be made with the goal of achieving optimal overall nutrition. Water, fluids containing carbohydrates and electrolytes may be consumed immediately prior to, during and after physical activity. Following competition or training for competition, athletes should rehydrate and consume a high carbohydrate meal. Relationship of physical activity to chronic disease • • • • • Cancer: It has been shown that regular exercise is negatively correlated with the risk for colon cancer. Apart from the role of exercise in the prevention of obesity, which is positively related to cancer, a plausible mechanism for the protective role of physical activity on colon cancer may be the shortening of the of intestinal transit time, thus reducing the contact time between the colonic mucosa and carcinogens. Heart Disease: An inverse relationship between physical exercise and coronary heart disease has been reported and repeatedly confirmed. Regular physical exercise increases serum HDL cholesterol, decreases serum triglycerides, decreases blood pressure, enhances fibrinolysis, lessens platelet adherence, enhances glucose tolerance and insulin sensitivity, and decreases the risk of cardiac arrhythmias. The mechanism(s) by which physical exercise ameliorates the progression of the disease include improved endothelial function and favourable changes in lipoprotein profiles. Diabetes: Obesity, physical inactivity and advancing age are recognised primary risk factors for insulin resistance and the development of type II diabetes. The short- and long-term effects of physical exercise on glucose tolerance, insulin action and muscle glucose uptake show that contracting muscle has an “insulin-like” effect on promoting glucose uptake and metabolism. Further, by decreasing total abdominal obesity, increasing muscle mass, and diverting dietary carbohydrate to muscle for oxidation and glycogen synthesis, physical activity reduces the potential for energy intake exceeding energy expenditure, and fat accumulation. Obesity: The risk factors for developing obesity are not fully understood but include genetics, food intake, some metabolic disorders and physical inactivity. The latter is known to be of fundamental importance in achieving energy balance and maintaining a weight appropriate for optimal health. Skeletal Health: Physical activity has significant beneficial effects on bone health by increasing bone mass in children and adolescents and maintaining bone mass in Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 18 adults. In the elderly, physical activity is known to improve mineral density, muscle strength, coordination, flexibility, and thus falls and fractures. Adverse effects of excessive physical activity Safety: Physical exercise, when excessive and beyond one’s established tolerance has the potential to do harm. • Overuse Injuries: Overuse injuries to muscles, bones and joints as well as injuries caused by accidents have been reported. Additionally, pre-existing conditions can be aggravated upon initiation of a physical activity programme and chronic, repetitive activities can cause injury. • Dehydration and Hyperthermia: Loss of body water as sweat can be greater than can be replaced during physical activity with resultant dehydration and heat injuries, which can be accentuated by prevailing environmental conditions at the time of the activity. People should, therefore, drink water before, during (if possible) and after exercise. Individuals who have lost more than 2% of their body weight after exercise are to be considered physiologically impaired and should not exercise, but rehydrate themselves. • Hypothermia: This can occur from water exposure, winter sports, inadequately clothed individuals in cool, damp environments as well as in physically exhausted individuals. Appropriate precautionary measures is the best means of prevention. • Cardiac Events: Heavy physical exertion can trigger the development of arrhythmias or myocardial infarction or even sudden death. While it is true that compared to the population at large, people who exercise regularly have a reduced risk of cardiovascular disease and sudden death, there is a transient increase in the risk of such people for cardiac events during and immediately after exercise. • Female Athlete Triad: Athletic women who undereat or overtrain can develop a condition or a cluster of conditions (disordered eating, amenorrhoea and osteoporosis), termed the “female athlete triad”. Caution: The prudent approach for previously sedentary individuals (men > 40 and women > 50 years of age) or individuals with pre-existing medical conditions, who wish to initiate physical activity is to seek appropriate medical advice before initiating a physical activity programme. Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 19 Carbohydrate (Sugars and Starches) The basis on which carbohydrate requirements were established The RDA for carbohydrate was established on the basis of the average amount of glucose utilized by the brain, which is the only truly carbohydrate-dependant organ. The AI for older infants is based on carbohydrate intake from human milk and complementary foods (Table 4). Special considerations • • Infant Formula: The carbohydrate content of milk-protein based formula for term infants is similar to that of human milk. Whole cow's milk contains lower concentrations of carbohydrate than human milk. In contrast to human milk, conventional infant formula contains sucrose and glucose polymers. Exercise: Individuals adapted to low carbohydrate diets can perform adequately for extended periods at exercise levels of less than 65% O2 max. For extended periods of exercise exceeding this level, the dependence on carbohydrate as a fuel increases rapidly to near total dependence. For such individuals, there must be a corresponding increase in carbohydrate derived directly from carbohydrate containing foods. Relationship of carbohydrate intake to chronic disease • • • • • • • Behaviour: The long-term effects, if any, of sugar consumption on behaviour remains unclear. A meta-analysis of 23 studies conducted over a twelve-year period concluded that sugar intake does not affect either behaviour or cognitive function in children. Dental Caries: Caries occurrence is influenced by frequency of meals and snacks, oral hygiene, water fluoridation, fluoride supplementation and fluoride toothpaste. Hence, it is difficult to rationalise the role of sugar in dental caries as a cause-andeffect relationship. Dislipidaemia: There is some evidence that increased sugar intake is positively associated with plasma triglycerides, LDL cholesterol concentrations, and an inverse relationship with HDL cholesterol concentrations. Coronary Heart Disease: Four epidemiological studies have shown no risk of coronary heart disease from consuming naturally occurring or added sugars. However, although there is some evidence for an association between high glycaemic index (GI) foods and risk for coronary disease, this relationship remains to be defined. Diabetes: Two prospective cohort studies have shown no risk of diabetes from consuming increased amounts of sugar. Furthermore, results from intervention studies evaluating the effect of sugar intake on insulin concentration and insulin resistance are contradictory. Compared to regular consumption of low GI carbohydrates, regular consumption of high GI carbohydrates results in high concentrations of circulating glucose and insulin. The extent to which consumption of high GI index diets may influence the development of diabetes as compared with other dietary variables, which also influence insulin secretion, e.g. fibre, remains to be defined. Obesity: A negative correlation between total sugar intake and BMI has been consistently reported for children and adults. The effects of an increased intake of total sugars on energy intake are contradictory (probably reflecting the limitations of dietary methodology) and the increased intake of added sugars are most often associated with increased energy intake. There is no clear and consistent association between increased energy intake of added sugars and BMI. Although some evidence indicates that in short-term studies a relationship exists between dietary GI and hunger, satiety, and energy intake at single meals, many of the studies are confounded by differences between test diets and in variables other than the GI. However, there is little data on the effect of the GI on energy intake from longer-term clinical trials. Cancer: One case control study has suggested that sugar-rich foods, total sucrose intake, sucrose to dietary fibre ratio and the GI were associated with increased risk of lung cancer. There is inconsistent and insufficient data to determine the role of sugars, if any, on breast, colon and prostate cancer. Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 20 Adverse effects of carbohydrate overconsumption Safety: Based on the available evidence on dental caries, behaviour (hyperactivity), cancer, risk of obesity, glycaemic index and risk of hyperlipidaemia, there is insufficient evidence to set a UL for total or added sugars. Caution: Although a UL is not set for sugars, a maximal intake level of 25% or less of energy from added sugars is suggested. While it is recognised that hypertriglyceridaemia can occur with increasing (added and intrinsic) sugars, total sugar intake can be limited by minimising the intake of added sugars and consuming naturally occurring sugars present in nutrient-rich foods such as milk and dairy products as well as fruits. Diets low in sugars tend to be less palatable and inadequate micronutrient intake can occur with a very low sugar intake (less that 4% of total energy) because foods abundant in micronutrients, such as fruits and dairy products, also contain naturally occurring sugars. Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 21 Table 4. The DRIs for carbohydrates Gender Age EAR RDA AI UL Years g/day g/day g/day ♀♂ 0 – 0.5 60fg 0.5 - 1 95fh a 1–3 100 130 4–8 100a 130 ♂ 9 – 13 100a 130 14 – 18 100a 130 19 – 30 100 130 31 – 50 100 130 51 – 70 100 130 > 70 100 130 ♀ 9 – 13 100a 130 14 – 18 100a 130 19 – 30 100 130 31 – 50 100 130 51 – 70 100 130 > 70 100 130 175 135 b Pregnancy ≤ 18 19 – 30 135c 175 31 – 50 135c 175 210 160d Lactation ≤ 18 19 – 30 160e 210 31 – 50 160e 210 ♀ female ♂ male a extrapolation from adult data b adolescent female EAR plus fetal brain glucose utilization c adult female EAR plus fetal brain glucose utilization d adolescent female EAR plus average human milk carbohydrate content e adult female EAR plus average human milk carbohydrate content f for healthy infants receiving human milk the AI is the mean intake g average content of human milk h average intake from human milk plus complementary foods Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). NOAEL - LOAEL - 22 Fibre The biochemical basis on which fibre requirements were established Definitions: • • • Dietary Fibre was defined as non-digestible carbohydrates and lignin that are intrinsic and intact in plants. It includes plant non-starch polysaccharides (e.g cellulose, pectin, gums, hemicellulose, β-glucans, and fibres contained in oat and wheat bran) plant carbohydrates that are not recovered by alcohol precipitation (e.g. inulin, oligosaccharides and fructans), lignin and some resistant starch. Functional Fibre is defined as isolated, non-digestible carbohydrates that have been shown to have beneficial physiological effects in humans. It includes isolated, nondigestible plant (e.g. resistant starch, pectin and gums), animal (e.g. chitin and chitosan) or commercially produced (e.g. resistant starch, polydextrose, polyols, inulin and indigestible dextrins) carbohydrate. Total Fibre is the sum of Dietary Fibre and Functional Fibre. Dietary or Functional Fibre was not considered as an essential nutrient, such as calcium or folate, which when consumed in inadequate amounts results in biochemical and clinical symptoms of a deficiency. Nevertheless, lack of fibre in the diet can result in inadequate faecal bulk and may detract from optimal health in a variety of different ways depending upon other factors, including the rest of the diet, the stage of the lifecycle and the type of fibre consumed (or not). A recommended intake for fibre has been set based on the prevention of coronary heart disease, while recognising that the greatest benefit is derived from the ingestion of cereal fibres and viscous Functional Fibres, including gums and pectins (Table 5). This intake should be sufficient to also reduce constipation in most normal people assuming adequacy of hydration of the large bowel. Although high dietary fibre intake is associated with a decreased risk of several chronic diseases, there is no conclusive evidence that it is the dietary fibre rather than other components of fruits, vegetables and cereal products, which reduce the risk for these diseases. Implicit in the adopted definition of Dietary Fibre “intrinsic and intact in plants” is that the reported beneficial effects are due to the fibre source not the fibre per se. Also implicit in the definition of Functional Fibre (isolated, non-digestible, carbohydrates with beneficial physiologic effects in humans) is the need to document that the beneficial physiological effects in humans are due to the isolated or synthesised fibre itself. Physiological effects of isolated and synthetic fibres Both safety and efficacy, especially of synthetic fibres, have to be established before a product can be identified as a fibre source. Three measures of efficacy have been identified, namely, laxation, normalisation of blood lipid concentrations and attenuation of blood glucose responses. Relationship of fibre intake to chronic disease • • • Coronary Heart Disease (CHD): The available evidence indicates that Dietary Fibre (cereal foods) and certain Functional Fibres (viscous) are associated with reduced risk of CHD. In prospective population studies, there is a strong relationship between Total Fibre intake from foods and CHD. Gastrointestinal Health: The available evidence is supportive of certain Dietary and/or Functional Fibres having a beneficial effect on duodenal ulcers, constipation, laxation, faecal weight, energy source for the colon and the prevention of diverticular disease. The data were, however, insufficient on which to base a recommended intake. Colon Cancer: Marked international differences in rates of colorectal cancer, coupled with findings from migratory studies in which individuals take on the cancer demographics of the population in which they move to, have suggested a strong role of environmental factors in colon cancer incidence. A review of 48 studies on the relationship between Total Fibre intake and colon cancer found that 38 studies Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 23 • • • reported an inverse relationship, 7 reported no association and 3 reported a direct association. However, other studies and three recent clinical intervention trials do not support a protective effect of Dietary fibre intake against colon cancer. The available data on the role of Functional Fibres in the incidence of colon cancer is insufficient to make a recommendation because of lack of appropriate intake data. Breast Cancer: A growing number of studies have reported on the relationship between Dietary Fibre and breast cancer incidence, and the strongest case can be made for cereal consumption rather than Dietary Fibre per se. There are no reports on the role of Functional Fibres on the risk of breast cancer, a relationship that needs to be elucidated. Glucose Tolerance, Insulin Response and Diabetes: Epidemiological evidence supports the protective effect of Dietary Fibre intake against type II diabetes. Intervention studies with viscous Dietary and Functional Fibre, such as oat products, isolated pectin and guar gum, have reported significant reductions in glycaemic response, a relationship that is less consistently documented with non-viscous fibres. Satiety and Weight Maintenance: The strongest data supporting a relationship between fibre and weight maintenance come from epidemiological studies which show that Dietary Fibre intake is lower in obese men and women when compared with lean men and women, and that BMI is lower with higher fibre consumption for both men and women. The evidence regarding whether feeding of specific fibres increases satiety and thus results in a decreased food intake and weight maintenance has been deemed inconclusive. Adverse Effects of Dietary Fibre Safety Several animal and human studies have shown that foods or diets high in fibres may alter mineral metabolism, especially when phytate is present. Diets with a content of 10–12g of Dietary Fibre are generally considered as “safe”. In this regard, there is no consistent evidence that fibres from cereals, vegetables and fruits impair calcium absorption or balance, nor that Dietary Fibre adversely affects magnesium absorption or balance. Regarding zinc and iron absorption, cereal fibres, because of their phytate rather than their fibre content, are known to impair the absorption of these trace elements. A limited number of studies suggest that high intakes of Dietary Fibre can cause gastrointestinal distress. Flatulence has been reported to increase with an increased intake of Dietary Fibre. High Dietary Fibre intake, as part of an overall healthy diet is unlikely to produce any significant deleterious effects in healthy individuals. Caution Dietary Fibre can be a cause of gastrointestinal distress in people with the irritable bowel syndrome. Those who suffer as a result of excess gas formation should consume a low gas forming diet, which is low in Dietary Fibre. Unlike Dietary Fibre, it may be possible to concentrate large amounts of Functional Fibres (isolated or synthetic) in foods, beverages and supplements. The evaluation of the safety and efficacy of such products should be product- and fibre-specific. Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 24 Table 5. The DRIs for total fibre Age EAR RDA AI a UL NOAEL LOAEL Years g/day b ♀♂ 0 – 0.5 * 0.5 - 1 * 1–3 19 4–8 25 ♂ 9 – 13 31 14 – 18 38 19 – 30 38 31 – 50 38 51 – 70 30 > 70 30 ♀ 9 – 13 26 14 – 18 26 19 – 30 25 31 – 50 25 51 – 70 21 > 70 21 28 Pregnancy ≤ 18 19 – 30 28 31 – 50 28 29 Lactation ≤ 18 19 – 30 29 31 – 50 29 ♀ female ♂ male * not determined a intake level shown to provide the greatest protection against coronary heart disease (14g/1000 kcal) x median energy intake level (kcal/1000kcal/day) b based on 14g/1000kcal of required energy Gender Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 25 Total Fat and Fatty Acids The basis on which total fat and fatty acids requirements were established Neither an AI nor an RDA has been set for fat because there was insufficient data to determine a defined level of intake at which the risk of inadequacy or prevention of chronic disease occurs. Similarly neither an AI nor an RDA has been set for saturated or trans fatty acids because of the linear relationship between saturated fatty acids and serum LDL cholesterol and the attendant increased risk of CHD (Table 6). The AI for the n-6 polyunsaturated fatty acid, linoleic acid, and n-3 polyunsaturated fatty acid, linolenic acid, was set on the basis of the median intake of the fatty acids in the USA. Neither an AI nor an RDA was set for n-9-cis monounsaturated fatty acids because of their endogenous synthesis and lack of evidence for independent beneficial effects on health (Tables 7 and 8). AMDRs, however, have been estimated for these nutrients. There is no evidence for a biological requirement for cholesterol and, therefore, neither an AI nor an RDA was set. Special considerations • • Infant Formula: Evidence from clinical trials with term infant formula containing DHA is inconsistent. Associations between lower growth and delays in some developmental tests have been noted in pre-term and term infants fed formula containing DHA, but not arachidonic acid. n-6:n-3 Fatty Acid Ratio: The available data, although limited, indicate that a linoleic:α-linolenic acid ratio below 5:1 may be associated with impaired growth in infants. The available data was insufficient to set an upper range for this ratio. Relationship of total fat intake to chronic disease • • • • Obesity: Epidemiological evidence is not conclusive as to whether high fat (low carbohydrate) diets predispose to overweight/obesity and promote weight gain. However, it may be concluded that higher fat intakes are accompanied with increased energy intake and increased weight gain in populations, which are already predisposed to being overweight/obese. Coronary Heart Disease: Case control studies indicate an association between total fat intake and CHD. However, a detailed evaluation of these studies shows that it is not possible to separate total fat intake from saturated fatty acid intake, which is known to raise serum LDL cholesterol concentration. Nevertheless, a total fat intake, which exceeds 35% of total energy results in an unacceptably high intake of saturated fatty acids relative to polyunsaturated fats. Furthermore, there is a possibility that a higher fat intake may enhance a thrombogenic state, despite the fact that the evidence regarding this mechanism alone for enhancing CHD risk was not strong enough to make a recommendation. Hyperinsulinaemia, Glucose Intolerance, Metabolic Syndrome and Type II Diabetes: Although high fat diets can induce insulin resistance in rodents, investigations in humans fail to confirm this effect. Moreover, an association between dietary fat intake and risk for diabetes has been reported in some epidemiological studies, but this association is most likely confounded by various factors, such as obesity and glyceamic index. Cancer: A high intake of dietary fat has been implicated in the development of lung, breast, colon and prostate cancer. The totality of the currently available evidence, however, is not supportive of such an association. Clinical effects of excessive fat intake • With increasing intakes of fat and, therefore, decreasing carbohydrate intake, there is a trend towards reduced consumption of dietary fibre, folate and vitamin C. Additionally, Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 26 it is rather difficult to design a diet high in fat, which does not contain a high amount of saturated fatty acids. Clinical effects of inadequate fat intake • • • Impaired Growth: Inadequate fat intake may potentially result in lower than required total energy intake, which is of particular concern in infants and children as well as during pregnancy, when there is a relatively high energy requirement for both energy expenditure and for fetal growth. Chronic Disease: Compared with a higher fat intake, low fat–high carbohydrate diets may be considered unfavourable with respect to chronic disease, such as CHD and diabetes, because of the metabolic alterations they induce, which include a reduction in HDL cholesterol concentration, increase in serum triglycerides, and higher responses in postprandial glucose and insulin concentrations. This metabolic pattern has been associated with an increased risk for CHD and type II diabetes both in intervention and prospective studies. However, strong supportive evidence for this association does not exist. Chronic non-specific Diarrhoea: Low fat diets may have the potential to predispose to diarrhoea, which is considered to be an intestinal motility disorder that may improve with a higher fat intake by slowing gastric emptying and favourably altering intestinal motility. Adverse effects of fat overconsumption Safety A UL was not set for fat because there is no defined level of intake at or above which adverse effects occur. A UL for either saturated or trans fatty acids was not set because of the increased risk of CHD with any incremental increase in saturated fatty acid intake. There was insufficient evidence to use the model of risk assessment to set a UL for n-6 and n-3 polyunsaturated, and n-9 monounsaturated fatty acids. Caution There is some evidence to suggest that a high intake of n-3 polyunsaturated fatty acids, particularly EPA and DHA, may impair immune response (in vitro studies) and result in excessively long bleeding times in a non-dose response relationship. Caution was recommended with the consumption of EPA and DHA supplements, especially in individuals who: • Have impaired glucose tolerance and diabetic conditions • Require increased doses of oral hypoglycaemic agents • Are diagnosed with familial hypercholesterolaemia and have an increased incidence of nose bleeds while on n-3 polyunsaturated fatty acid supplements • Are on anticoagulant therapy e.g. aspirin, warfarin, coumadin. It is not advisable to attempt to reduce the intake of any of these nutrients to zero or a very low intake in the belief that one would attain the maximum possible health benefit. Such extraordinary adjustments may, more than likely, induce undesirable adverse effects (e.g. exclusion of certain foods, inadequate intake of other nutrients including micronutrients) and unknown and/or unquantifiable health risks. It is possible to follow a diet with an appropriate content of these nutrients by following the DRIs. Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 27 Table 6. The DRIs for total fat Gender Age EAR RDA AI UL NOAEL Years g/day ♀♂ 0 – 0.5 31ab 0.5 - 1 30ac 1–3 * 4–8 * ♂ 9 – 13 * 14 – 18 * 19 – 30 * 31 – 50 * 51 – 70 * > 70 * ♀ 9 – 13 * 14 – 18 * 19 – 30 * 31 – 50 * 51 – 70 * > 70 * * Pregnancy ≤ 18 19 – 30 * 31 – 50 * * Lactation ≤ 18 19 – 30 * 31 – 50 * ♀ female ♂ male * not determined a for healthy infants receiving human milk the AI is the mean intake b average consumption of total fat from human milk c average consumption of total fat from human milk and complementary foods Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). LOAEL - 28 Table 7. The DRIs for n-6 polyunsaturated fatty acids (Linoleic Acid) Gender Age EAR RDA AI UL NOAEL LOAEL Years g /day ♀♂ 0 – 0.5 4.4 ab 0.5 - 1 4.6ac 1–3 7.0d 4–8 10d ♂ 9 – 13 12d 14 – 18 16d 19 – 30 17d 31 – 50 17d 51 – 70 14d > 70 14d ♀ 9 – 13 10d 14 – 18 11d 19 – 30 12d 31 – 50 12d 51 – 70 11d > 70 11d 13d Pregnancy ≤ 18 19 – 30 13d 31 – 50 13d d 13 Lactation ≤ 18 d 19 – 30 13 31 – 50 13d ♀ female ♂ male a for healthy infants receiving human milk the AI is the mean intake b average consumption of total n-6 fatty acids from human milk c average consumption of total n-6 fatty acids from human milk and complementary food d median intake of linoleic acid from Continuing Survey of Food Intake by Individuals (CFSII) Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 29 Table 8. The DRIs for n-3 polyunsaturated fatty acids (α-Linolenic Acid) Gender Age EAR RDA AI UL NOAEL LOAEL Years g/day ♀♂ 0 – 0.5 0.5ab 0.5 - 1 0.5ac 1–3 0.7d 4–8 0.9d ♂ 9 – 13 1.2d 14 – 18 1.6d 19 – 30 1.6d 31 – 50 1.6d 51 – 70 1.6d > 70 1.6d ♀ 9 – 13 1.0d 14 – 18 1.1d 19 – 30 1.1d 31 – 50 1.1d 51 – 70 1.1d > 70 1.1d d 1.4 Pregnancy ≤ 18 d 19 – 30 1.4 31 – 50 1.4d 1.3d Lactation ≤ 18 19 – 30 1.3d 31 – 50 1.3d ♀ female ♂ male a for healthy infants receiving human milk the AI is the mean intake b average consumption of total n-3 fatty acids from human milk c average consumption of total n-3 fatty acids from human milk and complementary food d median intake of α-linolenic acid from Continuing Survey of Food Intake by Individuals (CFSII) Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 30 Protein and Amino Acids The basis on which protein and amino acid requirements were established The RDA for both men and women were based on meta-analysis of nitrogen balance studies (Table 9). For amino acids, isotopic tracer methods and linear regression analysis were used, whenever possible, to determine requirements. Special considerations • • • • • • Infant Formula: Although protein intake has been reported to be 66 - 70% higher in formula fed infants as compared with breastfed infants, there is no evidence that the lower protein intake in breastfed infants is associated with adverse clinical outcomes. It is recognised that casein and whey in cow's milk is not the same as those in human milk, and that the absorption and digestibility of amino acids from formula milk would be different from that of human milk. Estimates indicate that protein in cow's milk is 70 – 90% as efficiently utilised as the protein in human milk. In determining the level of protein to be added to infant formula based on various possible protein sources, it is important to evaluate the digestibility and comparative protein quality. Twin Pregnancies: Although no data were available on dietary protein intervention in twin pregnancies, it was recommended as prudent to provide such women with an additional protein intake of 50g from the second trimester of pregnancy together with an adequate energy intake to utilise the protein as efficiently as possible. Endurance Training: Endurance exercise is accompanied by an increase in the oxidation of branched chain amino acids, which has been suggested to imply an increased need for dietary protein. The branched chain amino acid oxidation data, however, were obtained from acute studies performed around the time of the exercise itself and did not take into account the remaining part of the day. Additionally, the reported differences were statistically significant, but small in relation to the total daily amount of oxidation. On this basis and other considerations, it was not possible to conclude that endurance exercise increases protein requirements. Resistance Training: The methodological limitations together with, at times, inappropriate interpretation of the available data do not support a conclusion that protein requirements for those who engage in resistance training are greater than normal non-exercising individuals. Vegetarians: Vegetarian diets that include complementary mixtures of plant protein can provide the same quality of protein as that from animal protein sources and, therefore, no special recommendations on the protein requirements for such individuals have been made. Protein Quality: Different sources of protein vary widely in their composition and nutritional value. The quality of a protein is an expression of its ability to provide the nitrogen and amino acid requirements for growth, maintenance and repair, and is principally determined by its digestibility (the proportion of the protein nitrogen that is absorbed) and its amino acid composition (the relative content and metabolic availability of the individual indispensable amino acids). In this regard, if the content of a single indispensable amino acid in the diet is insufficient to meet the individual’s requirements, known as the limiting amino acid, then it will limit the utilization of other amino acids and protein synthesis, even if the total nitrogen intake is adequate. The concept of the limiting amino acid has led to the practice of amino acid scoring, whereby the indispensable amino acid composition of a specific protein source is compared with that of a reference amino acid composition profile (e.g. egg). The Protein Digestibility Corrected Amino Acid Scoring (%) (PDCAAS) is the amino acid score of a protein corrected for its digestibility. The recommended PDCAAS pattern for proteins for children older than one year and all older age groups (mg/g protein) is: • Isoleucine 25 • Leucine 55 • Lysine 51 • Methionine and cysteine25 • Phenylalanine and tyrosine 47 Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 31 • • • • Threonine Tryptophan Valine Histidine 27 7 32 18 Because high quality protein is typically derived from animal products, which are also the primary sources of certain micronutrients, such as calcium, vitamin B12 and bioavailable iron and zinc, low protein intakes may result in an inadequate intake of these micronutrients. Relationship of protein intake to chronic disease • • • • • Osteoporosis: Increased calcium excretion with increasing protein intake is reasonably well documented. One of the potential consequences of increased calcium excretion is bone resorption, which, although documented with increased protein intake, remains controversial in terms of clinical significance. Poor protein status in itself leads to bone resorption, whereas increased protein intake may lead to increased calcium intake, and bone loss does not occur when calcium intake is adequate. Renal Stones: The only long-term (4.5 years) prospective trial on the effect of animal protein restriction on stone formation in newly diagnosed patients with calcium stones reported a negative effect. The relative risk for recurrent stone formation was 5.6 (confidence interval 1.2 – 26.1), which strongly suggests that the dietary advice given was detrimental. However, as the protein restriction was not the only variable that changed in the trial, the relationship, if any, remains to be defined. Renal Failure: The available evidence does support the concept that the protein content of the diet is responsible for the progressive decline in kidney function with age. Coronary Heart Disease: An inverse relationship has been documented between protein intake and risk of hypertension and CVD. Cancer: Reviews of the literature have concluded that high meat intake may be associated with increased risk of colon cancer, but that high total protein intake is not. For other types of tumours, there is no clear indication of greater risk with higher protein intakes. Clinical Effects of Inadequate Protein Intake Protein is a fundamental component for organ function and must not only be provided in adequate amount, but also together with sufficient non-protein energy so that the carbon skeleton of the amino acids is not used to meet energy requirements. Protein Energy Malnutrition (PEM) is not only common in children with an estimated 6 million deaths annually, but also in adults, especially in association with disease. The hypoalbuminaemic malnutrition seen in hospitalised adults has also been called adult kwashiorkor. In infants and young children PEM impairs brain function and development, impairs immune function with attendant increase in the risk of infections, alters gastrointestinal mucosa function and permeability, and adversely affects glomerular and tubular function of the kidney. In children, diets low in protein and energy are most frequently associated with a deficit in weight and height (wasting) and height for age (stunting). Adverse effects of protein overconsumption Safety There were insufficient data to provide dose response relationships in order to set the UL for total protein or any of the amino acids. The absence of a UL implies that caution should be exercised when using any amino acid at levels significantly higher than those normally found in food. Because of the current widespread use of protein supplements more research is needed to assess their safety. A number of adverse effects have been reported, especially with the very high intakes that can be achieved with supplements, but also at more modest levels of intake. Oral intakes of oral arginine aspartate (5 – 10g/day for 80 days) resulted in weight gain, digestive disturbances, nausea, diarrhoea and somnolence. Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 32 In humans, there is a direct relationship between serum glutamate levels and nausea. The possible involvement of glutamate in the “Chinese Restaurant Syndrome” has not been firmly established. Conflicting evidence is available on the association between glutamate and bronchospasm. In some individuals glutamate may exacerbate urticaria. High doses of methionine have been associated with decreased folate and increased homocysteine serum concentrations. High doses of tryptophan have been associated with appetite suppression, nausea and drowsiness. The role of chronic high dose tryptophan supplements in the development of eosinophilic fasciitis remains uncertain. Caution In view of the lack of compelling evidence to the contrary, no additional dietary protein was suggested for healthy adults engaging in endurance or resistance exercise. Vegetarians who restrict their diet to plant foods, in the absence of complementary mixtures of plant protein, may have an inadequate intake of certain indispensable amino acids because the concentration of lysine, sulphur amino acids and threonine are sometimes lower in plant food proteins than in proteins derived from animal foods. Some naturally occurring proteins are allergenic to susceptible individuals. In this regard, it should be borne in mind that relatively few protein foods cause most allergic reactions and include milk, eggs, peanuts and soy in children, and fish, shellfish, peanuts and tree nuts in adults. Individuals with idiopathic hypercalciuria should not be encouraged to consume more protein than the RDA. Aspartic acid dietary supplements are not advisable for infants and pregnant women. Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 33 Table 9. The DRIs for protein Gender Age EAR RDA AI UL NOAEL Years g/kg/day g/kg/day g/day g/kg/day ♀♂ 0 – 0.5 9.1* 1.52e 0.5 - 1 1.1a 1.52 13.5 1–3 0.88a 1.10 13 4–8 0.76a 0.95 19 ♂ 9 – 13 0.76a 0.95 34 14 – 18 0.73a 0.85 52 19 – 30 0.66b 0.80 56 31 – 50 0.66b 0.80 56 51 – 70 0.66b 0.80 56 > 70 0.66b 0.80 56 ♀ 9 – 13 0.76a 0.95 34 14 – 18 0.71a 0.85 46 19 – 30 0.66b 0.80 46 31 – 50 0.66b 0.80 46 51 – 70 0.66b 0.80 46 > 70 0.66b 0.80 46 1.10 71 0.88c Pregnancy ≤ 18 19 – 30 0.88c 1.10 71 31 – 50 0.88c 1.10 71 d 1.10 71 1.05 Lactation ≤ 18 d 19 – 30 1.05 1.10 71 31 – 50 1.05d 1.10 71 ♀ female ♂ male * This is an AI value a Nitrogen equilibrium + protein deposition b Nitrogen equilibrium c the EAR and RDA are only for the 2nd half of pregnancy. For the 1st half of pregnancy, the protein requirements are the same as those for non-pregnant woman d In addition to the EAR and RDA of the non-lactating adolescents or woman e for healthy infants receiving human milk the AI is the mean intake Reproduction requires the permission of NICUS (www.sun.ac.za/nicus) and copyright exemption from the National Academy Press (www.nap.edu). 34 LOAEL -