Functional abdominal wall reconstruction improves core

Functional abdominal wall reconstruction improves core physiology and quality-of-life
Cory N. Criss, MD, a
Nicola Lai, PhD, b,c
Clayton C. Petro, MD,
Justin Fiutem, MS, c a
David M. Krpata, MD,
Yuri W. Novitsky, MD, a and a
Christina M. Seafler, RN,
Michael J. Rosen, MD, a a
Cleveland, OH
Introduction.
One of the goals of modern ventral hernia repair (VHR) is restoring the linea alba by returning the rectus muscles to the midline. Although this practice presumably restores native abdominal wall function, improvement of abdominal wall function has never been measured in a scientific fashion.
We hypothesized that a dynamometer could be used to demonstrate an improvement in rectus muscle function after open VHR with restoration of the midline, and that this improvement would be associated with a better quality-of-life.
Methods.
Thirteen patients agreed to dynamometric analysis before and 6 months after an open posterior component separation (Rives-Stoppa technique complimented with a transversus abdominis muscle release) and mesh sublay. Analysis done using a dynamometer (Biodex 3, Corp, Shirley, NY) included measurement of peak torque (PT; N*m) and PT per bodyweight (BW; %) generated during abdominal flexion in 5 settings: Isokinetic analysis at 45
8
/s and 60
8
/s as well as isometric analysis at 0
8
, 15
8
, and +15
8
. Power (W) was calculated during isokinetic settings. Quality-of-life was measured using our validated HerQles survey at the time of each dynamometric analysis.
Results.
Thirteen patients (mean age, 54 ± 9 years; mean body mass index, 31 ± 7 kg/m
2
) underwent repair with restoration of the midline using the aforementioned technique. Mean hernia width was
12.5 cm (range, 5–19). Improvements in PT and PT/BW were significant in all 5 settings ( P
<
.05).
Improvement in power during isokinetic analyses at 45
8
/s and 60
8
/s was also significant ( P
<
.05). All patients reported an improvement in quality-of-life, which was associated positively with each dynamometric parameter.
Conclusion.
Restoration of the linea alba during VHR is associated with improved abdominal wall functionality. Analysis of rectus muscle function using a dynamometer showed statistical improvement by isokinetic and isometric measurements, all of which were associated with an improvement in qualityof-life. (Surgery 2014;156:176-82.)
From the University Hospitals Case Medical Center, Case Comprehensive Hernia Center, a
Biomedical Engineering, b
Case Western Reserve, and the Department of Pediatrics, c
Department of
Rainbow Babies and
Children’s Hospital, Cleveland, OH
H
ERNIATION OF THE VENTRAL ABDOMINAL WALL causes lateralization of the rectus muscles, as well as a loss of the medial tendonous insertion point for core abdominal musculature, resulting in atrophy.
Understandably, a goal of modern ventral hernia repair (VHR) is to reestablish native abdominal wall anatomy by restoring the linea alba at the
Accepted for publication April 14, 2014.
Reprint requests: Clayton C. Petro, MD, University Hospitals
Case Medical Center, Case Comprehensive Hernia Center,
Cleveland, OH 44106. E-mail: Clayton.Petro@UHhospitals.org
.
0039-6060/$ - see front matter
Ó
2014 Mosby, Inc. All rights reserved.
http://dx.doi.org/10.1016/j.surg.2014.04.010
176 SURGERY midline. Although restoring native anatomy after
VHR presumably restores its native function, this relationship has never been fully elucidated. One way to assess abdominal muscle functionality is the use of dynamometry, a measurement of muscle power or force popularized in physical therapy
A Biodex dynamometer
(Biodex Medical Systems, Shirley, NY) specifically allows an evaluation of trunk flexion/extension by isokinetic and isometric
Recently, some authors have demonstrated that using a dynamometer is a reliable and valid method of measuring abdominal muscular impairment in ventral hernia patients.
Although dynamometric measurements have been shown to assess rectus muscle function adequately, its use
Surgery
Volume 156, Number 1
Criss et al 177 measuring the effect of VHR has not yet been clar-
The initial objective of this investigation was to determine the effect of reconstructing the linea alba during VHR on core abdominal wall muscle function utilizing dynamometry.
To provide the appropriate physiologic tension during abdominal wall reconstruction, a myofascial release is often performed. Originally, Ramirez et al
proposed an external oblique release to advance the midline. Given the high wound complications associated with the large lipocutaneous flaps required to access the external oblique muscle, our group has developed alternative methods to gain advancement of the midline. Currently, we typically utilize a posterior component separa-
This approach borrows from the concept of a Rives and Stoppa’s retromuscular repair, but their approach is supplemented with a transversus abdominus muscle release when necessary. We have shown that the posterior component separation technique provides similar advancement of the midline as a standard anterior external oblique release
; however, the potential donor morbidity on abdominal muscle core physiology from transecting the transversus abdominus muscle during this repair has not been evaluated.
The second objective of the current study was to determine the effect on core muscular physiology after division of the transversus abdominus muscle during VHR. Herein we report the effect of abdominal wall function on patients undergoing abdominal wall reconstruction with restoration of the linea alba utilizing a posterior component separation and transversus abdominis muscle release.
METHODS
After approval by our institutional review board, patients undergoing open VHR at University Hospitals Case Medical Center, Cleveland, Ohio, by 2 surgeons (M.J.R., Y.W.N.), were recruited under a volunteer basis for prospective analysis. Thirteen adult patients (7 males; 6 females) agreed to participate. All subjects gave written informed consent to take part in this study. Baseline demographics including age, sex, body mass index, comorbidities, smoking status, number of previous abdominal surgeries, number of previous hernia surgeries, and previous wound infections were reviewed. In our practice, we mandate smoking cessation
$
1 month before complex abdominal wall reconstruction.
Despite this, patients were defined as being active smokers if occurring within a 3-month period before operation. Perioperative data included American Society of Anesthesiologists score, operative repair technique, defect dimensions, mesh type, and mesh area. The primary outcome variables for this study were abdominal wall functionality as measured using dynamometry
(see below), and quality-of-life as measured by the
HerQLes questionnaire.
Statistical analysis was performed using Graphpad Prism (V 6.0c). Descriptive statistics were used where appropriate, with standard deviations used to describe variance. Groups were compared with a
2-tailed t -test and Fisher’s or Chi-square statistics.
Linear regression was performed to identify an association between dynamometric improvement and quality-of-life.
Open ventral hernia operative technique.
Our technique for VHR has been presented extensively elsewhere.
In brief, we perform a full abdominal adhesiolysis. The dissection begins in the retrorectus space, and it is carried out to the lateral border of the rectus muscle carefully preserving the segmental intercostal nerves. The medial aspect of the transversus abdominus muscle is transected, and the preperitoneal/retroperitoneal plane is continued laterally. A large prosthetic mesh is placed in the retromuscular space and secured with transfascial sutures. The linea alba is then re-
Dynamometric measurements.
Trunk flexion exercise protocols were used to assess abdominal muscle performance before and 6 months after operative
Abdominal muscle function was assessed using an isokinetic dynamometer (Biodex System 3 Pro) with the dual position back extension/flexion attachment. The protocols were performed in the human performance exercise and metabolism laboratory at University Hospitals
Case Medical Center in Cleveland, Ohio.
The duration of the test was approximately
20 minutes. Before the trunk flexion exercise, participants were instructed to breathe properly during testing to avoid a Valsalva maneuver. The anatomic components of the machine were adjusted according to the individual’s anthropometric characteristics with the axis of rotation positioned at the iliac crest. The device chair was positioned parallel to the floor. The chest and upper legs were fixed to the device with straps, and the lower legs were suspended at the knee joint at a 90
8 angle. The individual anatomic component adjustments used for the preoperative intervention testing were the same of those used for postoperative testing to ensure that protocols are performed under similar conditions. Patients were instructed to keep their arms crossed over the chest during the test to minimize muscle forces from other body parts.
178 Criss et al Surgery
July 2014
The abdominal musculature exercise was performed using 2 different protocols: Isokinetic and isometric exercise of the trunk flexors. The differences between isokinetic and isometric testing modalities were described and patients were familiarized with both protocols as well as with the device by performing a series of fifteen trunk flexion/extensions with moderate efforts at the speed of 45
8
/s as a warm up. After 3 minutes of rest, the subject performed the isokinetic and isometric exercise tests.
Throughout both isokinetic and isometric testing, subjects were verbally encouraged to give a maximal effort during each test.
During isokinetic exercises, the dynamometer imposes a fixed movement speed while varying the resistance based on the subject’s effort. The device matches the force generated by the participant throughout the range of motion while keeping the speed constant. Therefore, this test allows the device to determine the maximal muscular force changes of the subject throughout the entire range of motion. Two separate series of 6 trunk flexion/ extension were performed at a speed of 45
8
/s and
60
8
/s. The subject rested in an upright fixed position for one minute between the 2 series.
The patient then performed the isometric exercise protocol after 5 minutes of resting at the end of the isokinetic exercise protocol. In this protocol, the subject develops muscular force against the device without body movement. Therefore, peak torque (PT) is measured without any movement around the hip joint when the trunk flexors are contracting. This test was performed using 3 static positions: Extended, neutral, and flexed. In the neutral position, the subject is seated on a Biodex chair with the spine straight forming a
90
8 angle at the hip joint, whereas in the extended and flexed positions, the subject was leaning back
( 15
8
) or forward (+15
8
) beyond neutral (0
8
)
positions, respectively ( Figs 1–3 ). Subjects per-
formed 3 maximal isometric contractions of the trunk flexors for each of the 3 different static positions. There was a 10-second rest period between each repetition. At the end of each series of 3 repetitions, subject was resting for 1 minute in neutral position.
Outcome measures for all 5 settings were both
PT and PT per bodyweight (BW). For isokinetic measurements, power was also calculated.
Quality-of-life.
Quality-of-life was measured by our previously validated HerQles questionnaire.
The survey consists of twelve 0–6 Likert scale questions specifically designed to assess quality-of-life related to abdominal wall function. Scores range
Fig 1.
Neutral position (0
8
).
Fig 2.
Positioned at 15 8 .
from 0 to 72, which are then converted to a standardized 0–100 scale with larger numbers correlating with a better quality-of-life. All patients were instructed to fill out a preoperative questionnaire at the time of the exercise test, and once again at the postoperative exercise test. These values were analyzed and interpreted to provide a comparison of the quality-of-life for each included patient before and after their operation.
RESULTS
A total of 13 patients met the inclusion criteria for the study and completed the dynamometric exercises successfully before and after their VHR.
There were 7 males and 6 females, with a mean age of 54 ± 9 years (range, 36–69), and a mean preoperative body mass index of 31 ± 7 kg/m
2
(range, 20–46). Associated comorbidities included diabetes in 1 patient and smoking history in
Surgery
Volume 156, Number 1
Criss et al 179
Fig 3.
Positioned at +15
8
.
another. Our patients had a mean ASA score of 2.5
and had undergone an average of 4 (range, 1–6) prior abdominal surgeries and 2 (range, 0–6) previously attempted hernia repairs. Seven patients had a history of wound infection and 1 patient had a history of an open abdomen requiring a skin graft.
Regarding operative characteristics, the mean defect width was 13 ± 5 cm (range, 5–19), and the mean area was 267 ± 174 cm
2
(range, 50–570) with an average mesh size of 754 ± 421 cm
2
(range, 200–
1,872). All patients underwent a retrorectus repair supplemented with a TAR. Synthetic mesh was utilized in 11 cases, with Bard Soft Mesh (Davol, Cranston, RI) used in 10, and Bard Mesh (Bard, Murray
Hill, NJ) in 1. Biologic mesh (Strattice; LifeCell,
Bridgewater, NJ) was used in 2 cases owing to enterocutaneous fistula takedown and removal of infected synthetic mesh. All patients achieved full midline reconstruction with restoration of the linea alba (
Preoperative versus postoperative dynamometric assessment.
All 13 patients completed both preoperative and postoperative exercise evaluation. Two isokinetic (45
8
/s, 60
8
/s) and 3 isometric (0
8
, 15
8
, +15
8
) measurements were performed on each patient for a total of 5 separate tests. PT and PT/BW were recorded for isometric and isokinetic settings. Power was reported for isokinetic analyses only.
For isokinetic measurements at 45
8
/s, the mean
PT improved from 102 to 123 N*m ( P = .016), the mean PT/BW improved from 116 to 139 ( P = .019) and mean power improved from 39 to 50 W
( P = .006). For isokinetic measurements at 60
8
/s, the mean PT improved from 92 to 121 N*m
( P = .003), the mean PT/BW improved from 106
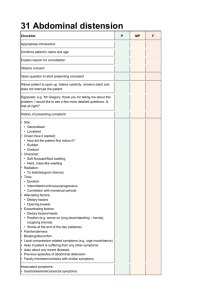
Table I.
Patient demographics and operative characteristics
Characteristic Value
Male/female
Age, y
Body mass index, kg/m
Diabetes
Chronic obstructive pulmonary disease
Smoking history
American Society of Anesthesiologists
History of wound infection
History of an open abdomen
Hernia area, cm
2
Synthetic/biologic mesh
*Mean value (range).
7/6
54 (36–69)
31 (20–46)
1/13
0/13
1/13
2.5 (2–3)
4 (1–6)
2 (0–6)
7/13
1/13
12.5 (5–19)
267 (50–570)
11/2 to 137 N*m/kg ( P
<
.0001) and the mean power improved from 44 to 59 W ( P = .013).
Isometric analysis at a neutral (0
8
) position resulted in an improvement in mean PT from 92 to 111 N*m ( P = .04) and improvement in mean
PT/BW from 96 to 120 N*m/kg ( P = .015). Isometric analysis in an extended ( 15
8
) position resulted in an improvement in mean PT from 102 to 123 N*m ( P = .002) and improvement in mean PT/BW from 103 to 125 N*m/kg
( P = .023). Isometric analysis at a flexed (+15
8
) position resulted in an improvement in mean PT from 83 to 104 N*m ( P = .037) and improvement in mean PT/BW from 91 to 115 N*m/kg
( P = .003;
).
Quality-of-life assessment.
All patients reported improvement in quality-of-life. The mean preoperative score was 50 and mean postoperative score was 75 ( P = .0016;
). Using ‘‘percent change’’ as the measured outcome, the mean change of the
HerQLes assessment was determined to be 50
(range, 18–67).
DISCUSSION
A well-established goal of modern VHR is to achieve midline reapproximation of the rectus muscles to restore native abdominal wall anatomy.
When necessary, component separations are utilized to achieve medial advancement of the fascial edges to allow for closure under physiologic tension. Presumably, medialization of the rectus muscles and restoration of the linea alba improves abdominal core function, but this hypothesis has never been tested objectively. Herein we have presented a series of patients who underwent
180 Criss et al Surgery
July 2014
Table II.
Dynamometric assessments
Test
Pre
PT (N*m)
Post
P value
Pre Post
Isokinetic
45
8
/s
60 8 /s
Isometric
0 8
15
8
+15
8
102 ± 67
92 ± 50
92 ± 41
102 ± 49
83 ± 35
123 ± 61
121 ± 58
111 ± 40
123 ± 58
104 ± 41
.016
.003
.040
.002
.037
116 ± 68
106 ± 52
96 ± 42
103 ± 45
91 ± 43
120 ± 47
125 ± 56
115 ± 50
*Mean preoperative body weight (BW), 89.7 kg; mean postoperative BW, 90.8 kg.
NA , Not applicable.
139 ± 59
137 ± 55
P value
Pre
Power (W)
Post
.019
< .0001
.015
.023
.003
39 ± 30
44 ± 32
NA
NA
NA
50 ± 29
59 ± 29
NA
NA
NA
P value
.006
.013
dynamometric analysis before and after VHR utilizing a posterior component separation technique.
We found improvements in all measurements of core abdominal physiology and patient reported quality-of-life metrics. This study demonstrates the benefits of a functional abdominal wall reconstruction with restoration of the midline by objective measures.
One of the major barriers to studying muscle functionality is choosing the optimal method and parameter to represent it. Dynamometry, or the study of muscular force and power measured by the Biodex dynamometer, has been established as a reliable and effective method to assess muscular function.
In several studies regarding abdominal wall function after transverse rectus abdominis myocutaneous flap reconstructions, abdominal wall function was successfully evaluated preoperatively and postoperatively using dyna-
Hernias have been shown to affect abdominal muscular function as evidenced by a study from Gunnarsson et al,
who demonstrated a decrease in functionality in patients with hernias
>
10 cm wide.
A postoperative analysis by den
Hartog et al
concluded that open incisions repaired with rectus muscular reapproximation ascertained a greater isokinetic strength than laparoscopically repaired hernias where the fascia was not restored, but these results did not attain significance. The significance of midline reapproximation is also evident in a study by Johannason et al, who showed that mesh placement had little to no effect on abdominal functionality, theorizing that restoring the linea alba was the primary
Only 1 study of 2 patients critically evaluated rectus muscle function before and after abdominal wall repair with external oblique release.
Although this study showed a similar improvement in Biodex results, the very small sample size and absence of qualityof-life metrics limit its application. Using a similar method of measurement for functionality, our prospective dynamometric analysis of a VHR demonstrated an overall improvement of functionality in all 5 isokinetic and isometric parameters.
As mentioned, it is standard practice at our institution to perform a posterior components separation when needed, which involves incising the insertion point of the transversus abdominis muscle. Although it has been theorized that incising an oblique muscle may affect abdominal functionality, our results in addition to recently published data supports otherwise. A recently reported study at our institution reviewed the findings on computed tomography of patients who received a TAR, with those who did not.
The results demonstrated a compensatory hypertrophic response of the rectus muscles, external oblique muscles, and internal oblique muscles in the TAR group. Interestingly, this response was only noted in groups where the linea alba was reapproximated, and not demonstrated in laparoscopic
VHR group where a bridge of synthetic mesh was utilized. It is conceivable that, despite the disruption of the insertion point of the TA muscle in a
TAR, there exists a compensatory improvement in function by reapproximating the linea alba.
Our results demonstrated a marked improvement in quality-of-life. The HerQles quality-of-life assessment tool asks disease-specific questions related to abdominal wall function, particularly in regards to activities of daily living.
Several studies indicate the important role of the abdominal muscles in providing trunk stability and
postural support during limb movement.
Specifically, electromyographic studies have reported that abdominal and multifidus muscle contractions precede the muscle activity of the lower limb during locomotion.
Therefore, improvement of trunk muscle function and thereby
Surgery
Volume 156, Number 1
Criss et al 181 postural support and limb movement likely contributes to enhanced ability to perform activities of daily living. Supporting this hypothesis, we found a positive relationship between improvement in quality-of-life and improvement in core abdominal function as measured by dynamometry.
Evaluating novel abdominal wall reconstructive approaches with both validated subjective and objective parameters to establish their merit is critically.
Established as one of the main effectors of abdominal wall muscular function, rectus muscle flexion was the main focus of our analysis. Even so, the abdominal wall muscular function is multifactorial, affected by the intrinsic back muscles and oblique abdominal musculature as well.
Although no standard measurement exists for oblique muscle function, dynamometric measurements are unique in that they demonstrate a comprehensive representation of muscles exerted at a given angle or speed. This approach means that, despite patients performing a flexion motion, it is likely that the results reported are a representation of multiple other muscular groups, including the oblique muscles. Even so, our laboratory is currently in the process of validating a method to measure the functionality of the abdominal oblique muscles with the anticipation to further develop a comprehensive study model.
One limitation of our analysis is the absence of a control group in which the midline fascia was not reconstructed and a bridge repair of synthetic mesh was performed. In our practice, we attempt routinely to reapproximate the midline and are successful typically in
>
95% of cases. The remaining 5% of patients represent an extreme cohort of massive defects that likely would not serve the purpose as an adequate control. There is, however, other evidence that could serve as an acceptable control group. The study by den Hartog et al found that laparoscopic bridge repairs were able to generate only 71 Nm/kg of PT per body weight at
60
8
/s. Interestingly, in our study patients that had their abdominal wall fascia reapproximated they were able to generate almost twice that PT (137
Nm/kg). These findings suggest a potential advantage of improving core muscle function by reapproximating the midline fascia. It is not our practice to perform a laparoscopic bridge for patients with hernias
>
8 cm. Therefore, had we used these patients as a control, they would not have been comparable with the open repairs with a mean width of 13 cm.
Finally, it is possible that these results can be extrapolated to other techniques of component separation that achieve rectus medialization, but we currently do not have data to support this assumption. Future studies can use this data as a platform for comparisons with other techniques that wish to demonstrate improvement in functionality.
In conclusion, our results support the notion that a VHR with restoration of the midline utilizing a posterior component separation technique with transversus abdominus muscle release can improve abdominal wall functionality by medialization of the rectus muscles and reconstitution of the linea alba. Utilizing dynamometry as a method of measuring functional outcomes after VHR serves as a promising adjunct to current postoperative protocols.
REFERENCES
1.
DuBay DA, Choi W, Urbanchek MG, Wang X, Adamson B,
Dennis RG, et al. Incisional herniation induces decreased abdominal wall compliance via oblique muscle atrophy and fibrosis. Ann Surg 2007;245:40-6 .
2.
Newton M, Waddell G. Trunk strength testing with isomachines. Part 1: review of a decade of scientific evidence.
Spine (Phila Pa 1976) 1993;18:801-11 .
3.
Newton M, Thow M, Somerville D, Henderson I, Waddell G.
Trunk strength testing with iso-machines. Part 2: experimental evaluation of the Cybex II Back Testing System in normal subjects and patients with chronic low back pain.
Spine (Phila Pa 1976) 1993;18:812-24 .
4.
Balogh B, Zauner-Dung A, Nicolakis P, Armbruster C, Kriwanek S, Piza-Katzer H. Functional impairment of the abdominal wall following laparoscopic and open cholecystectomy.
Surg Endosc 2002;16:481-6 .
5.
Feiring DC, Ellenbecker TS, Derscheid GL. Test-retest reliability of the biodex isokinetic dynamometer. J Orthop
Sports Phys Ther 1990;11:298-300 .
6.
Rothstein JM, Lamb RL, Mayhew TP. Clinical uses of isokinetic measurements. Critical issues. Phys Ther 1987;67:
1840-4 .
7.
Atisha D, Alderman AK. A systematic review of abdominal wall function following abdominal flaps for postmastectomy breast reconstruction. Ann Plast Surg 2009;63:222-30 .
8.
Zauner-Dungl A, Resch KL, Herczeg E, Piza-Katzer H.
Quantification of functional deficits associated with rectus abdominis muscle flaps. Plast Reconstr Surg 1995;96:
1623-8 .
9.
Kannus P. Isokinetic evaluation of muscular performance: implications for muscle testing and rehabilitation. Int J
Sports Med 1994;15(Suppl 1):S11-8 .
10.
Stark B, Emanuelsson P, Gunnarsson U, Strig ard K. Validation of Biodex system 4 for measuring the strength of muscles in patients with rectus diastasis. J Plast Surg Hand Surg
2012;46:102-5 .
11.
Baltzopoulos V, Brodie DA. Isokinetic dynamometry. Applications and limitations. Sports Med 1989;8:101-16 .
12.
Gunnarsson U, Johansson M, Strigard K. Assessment of abdominal muscle function using the Biodex System-4.
Validity and reliability in healthy volunteers and patients with giant ventral hernia. Hernia 2011;15:417-21 .
13.
den Hartog D, Eker HH, Tuinebreijer WE, Kleinrensink GJ,
Stam HJ, Lange JF. Isokinetic strength of the trunk flexor
182 Criss et al Surgery
July 2014 muscles after surgical repair for incisional hernia. Hernia
2010;14:243-7 .
14.
Grabiner MD, Jeziorowski JJ, Divekar AD. Isokinetic measurements of trunk extension and flexion performance collected with the biodex clinical data station. J Orthop
Sports Phys Ther 1990;11:590-8 .
15.
Ramirez OM, Ruas E, Dellon AL. ‘‘Components separation’’ method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 1990;86:519-26 .
16.
Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ. Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg 2012;204:709-16 .
17.
Krpata DM, Blatnik JA, Novitsky YW, Rosen MJ. Posterior and open anterior components separations: a comparative analysis. Am J Surg 2012;203:318-22 .
18.
Krpata DM, Schmotzer BJ, Flocke S, Jin J, Blatnik JA, Ermlich B, et al. Design and initial implementation of HerQLes: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 2012;215:635-42 .
19.
Rosen MJ, Fatima J, Sarr MG. Repair of abdominal wall hernias with restoration of abdominal wall function.
J Gastrointest Surg 2010;14:175-85 .
20.
Kind GM, Rademaker AW, Mustoe TA. Abdominal-wall recovery following TRAM flap: a functional outcome study.
Plast Reconstr Surg 1997;99:417-28 .
21.
Dulin WA, Avila RA, Verheyden CN, Grossman L. Evaluation of abdominal wall strength after TRAM flap surgery.
Plast Reconstr Surg 2004;113:1662-5 .
22.
Saberski ER, Orenstein SB, Novitsky YW. Anisotropic evaluation of synthetic surgical meshes. Hernia 2011;
15:47-52 .
23.
Shestak KC, Edington HJ, Johnson RR. The separation of anatomic components technique for the reconstruction of massive midline abdominal wall defects: anatomy, surgical technique, applications, and limitations revisited. Plast
Reconstr Surg 2000;105:731-8 .
24.
De Silva GS, Krpata DM, Hicks CW, Criss CN, Gao Y,
Rosen MJ, et al. Comparative radiographic analysis of changes in the abdominal wall musculature morphology after open posterior component separation or bridging laparoscopic ventral hernia repair. J Am Coll Surg
2014;218:353-7 .
25.
Hodges PW, Richardson CA. Contraction of the abdominal muscles associated with movement of the lower limb. Phys
Ther 1997;77:132-42 .
26.
Leetun DT, Ireland ML, Willson JD, Ballantyne BT, Davis
IM. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc 2004;36:
926-34 .
27.
Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med 2006;36:189-98 .