Does Retrojugular Route for Carotid Endarterectomy
advertisement

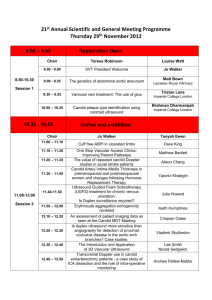
Acta chir belg, 2006, 106, 397-399 Does Retrojugular Route for Carotid Endarterectomy Increase the Risk of Internal Jugular Vein Thrombosis ? V. Scavée*, S. Theys**, J. C. Schoevaerdts** Department of Thoracic and Vascular Surgery*, Saint-Pierre Clinic, Ottignies and Department of Vascular Surgery**, University Clinic of Mont-Godinne (UCL), Yvoir, Belgium. Key words. Internal jugular vein thrombosis ; retrojugular route ; carotid endarterectomy. Abstract. Two different approaches are available to perform carotid endarterectomy : the traditional antejugular or the retrojugular route. With retrojugular route, direct access to the carotid arteries necessitates median retraction and often collapse of the internal jugular vein (IJV). Therefore, we have prospectively evaluated the potential incidence of IJV thrombosis. Introduction Recent large prospective randomized trials previously demonstrated the superiority of carotid endarterectomy (CEA) over medical management to reduce the incidence of strokes among patients, selected both symptomatic and asymptomatic, with significant extracranial internal carotid artery stenosis (1-4). Whatever the surgical technique used, carotid arteries dissection is either performed by a traditional antejugular approach or by a retrojugular route (5-6). With the retrojugular route, the internal jugular vein (IJV) is retracted medially and often collapse, by two umbilical tapes (Fig. 1), to allow direct access to the internal carotid artery (5-6). Then, the purpose of our study was to evaluate the potential occurrence of IJV thrombosis following retrojugular route for CEA. Fig. 1 With retrojugular route, direct access to the carotid arteries (ICA) necessitates median retraction and often collapse of the internal jugular vein (IJV). Material and Methods Patients demographics and risk factors Between September 2003 and November 2003, 20 patients underwent primary CEA following a standard uniform technique. There were 10 men (50%) and 10 women with a mean age of 71.8 years (range, from 44 to 82). Pertinent atherosclerotic risk factors and indications for CEA are listed in Table 1. Preoperative data The degree of internal carotid stenosis and the anatomical features were evaluated by both ultrasonography and MRA. The mean internal carotid artery degree of stenosis was 85 ± 6.3%. Preoperative duplex ultrasound scans were performed the day before procedure, including specific evaluation to bilateral IJV. Doppler with colour flow provided information about venous compression, patency and direction of flow (7) Surgical technique All patients were operated under general endotracheal anaesthesia with full cardiovascular monitoring. The CEA procedures were performed through a longitudinal neck incision with exposure of the extracranial carotid artery by a retrojugular route, as previously described (5-6). With retrojugular route, direct access to the carotid arteries necessitated median retraction and often collapse of the IJV (Fig. 1). Systemic heparin was 398 V. Scavée et al. Table 1 Risk factors and indications for surgery in 20 patients who underwent CEA through retrojugular route Variables N % 15 13 9 9 8 8 75 65 45 45 40 40 Risk factors Hypertension Smoking history Pulmonary disease Diabetes mellitus Coronary artery disease Peripheral artery disease CEA indications Asymptomatic Transient ischaemic attack Stroke 12 5 3 60 25 15 administrated (30 U/Kg body weight) prior to carotid clamping. Routine temporary shunt (Javid™, C.R. Bard®, Inc., USA) was used and the arteriotomy was closed by autologous ankle venous patching. Mean operative time was 92 minutes (range, from 75 to 104). Heparin administered was not reversed at the end of the procedure. The postoperative care was delivered in the intensive care unit for 24 h and 160 mg aspirin daily was prescribed after surgical procedure. Follow-up Postoperative clinical, neurological evaluation and all complications were assessed. Postoperative duplex ultrasound scans were performed before hospital discharge, at 3 and 6 months, with specific evaluation of the jugular veins. Only qualitative venous Doppler features were assessed (7). Results During the 30-day postoperative period, there was no neurological event or death. One patient (5%) developed recurrent laryngeal nerve dysfunction without recovery after 6 months. No wound infection or haematoma formation required surgical evacuation. The mean follow-up was 12 months and no signs or symptoms of IJV occlusion were recorded during the postoperative course. At 3, 6 and 12 months after the procedure, all carotid arteries evaluated by duplex remained patent, without thrombosis or recurrent stenosis. In addition, there was no dilation or aneurismal degeneration of the patch. With regards to preoperative venous imaging, both IJV of 20 patients were patent and no hypoplasia, agenesis or thrombosis vein were observed. On the first postoperative Doppler, two patients presented turbulent flow in IJV. However, all IJV were easily compressible, with thin walls and spontaneous flow toward the heart. The blood flow was normally modulated with cardiac, respiratory cycles and valsalva manoeuvre. No defect of venous filling and thrombosis was reported. During further Doppler (3, 6 and 12 months), IJV remained patent without direct or indirect signs of thrombosis or stenosis. Discussion Retrojugular approach for carotid endarterectomy presented several potential advantages (5-6). First, the exposition of the carotid artery is performed without division of any major branch of the IJV and lymphatic tissues are preserved. Furthermore, the simplicity of the anatomical dissection significantly reduces the operating time. Finally, recent trials reported no cranial nerve dysfunction (5-6). However, with retrojugular approach, direct access to the carotid arteries necessitates median retraction and often collapse of the internal jugular vein, especially in the higher cervical segment. Although the operative time in our study is relatively long, mainly due to routine temporary shunt use and saphenous vein patch angioplasty, we did not find any direct or indirect evidence of IJV stenosis or thrombosis. Only two patients presented turbulent flow without neither clinical consequence nor thrombosis on further Doppler evaluation. With respect to the quantitative Doppler parameters, PRIM et al. (8) reported a high disparity of area, expiratory and jugular flow speed between right and left IJV for patients with head and neck cancer. But, no statistically significant differences were found between sides. The venous flow is normally affected by both the respiratory and cardiac cycles (7), and thus prevents any objective conclusions about potential preoperative and postoperative measurements. Consequently, in our study, in addition to the qualitative parameters, we only registered as quantitative Doppler features the presence and the direction of venous flow. In order to confirm the absence of IJV thrombosis after CEA through retrojugular route, greater clinical experience and long-term follow-up are required. References 1. HOBSON I. I., WEISS D., FIELDS W. et al. Efficacy of carotid endarterectomy for asymptomatic carotid stenosis. N Engl J Med, 1993, 328 : 221-7. 2. North American Symptomatic Carotid Endarterectomy Trial Collaborators, Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med, 1991, 325 : 445-53. 3. Executive Committee for the Asymptomatic Carotid Atherosclerotic Study, endarterectomy for asymptomatic carotid artery stenosis. JAMA, 1995, 273 : 1421-8. Retro Jugular Carotid Exposure 4. European Carotid Surgery Trial : interim results for symptomatic patients with severe (70-99%) or with mild (0-29%) carotid stenosis. Lancet, 1991, 337 : 1235-43. 5. SAFAR H. A., DOOBAY B., EVANS G., KAZEMI K., JAHROMI A., CINA C. S. Retrojugular approach for carotid endarterectomy : a prospective cohort study. J Vasc Surg, 2002, 35 : 737-40. 6. NERI E., GIUBBOLINI M., SETACCI F., BALDI I., SETACCI C. The retrojugular route : the ideal exposure for carotid endarterectomy performed under locoregional anesthesia. Eur J Vasc Endovasc Surg, 2003, 26 : 250-5. 7. DAUZAT M. Ultrasonographie vasculaire diagnostique, théorie et pratique. Editions Vigot, 1991. 8. PRIM M., DE DIEGO J., MORENO P., GARCIA J., GAVILAN J. Implications of ultrasonographic measurements of internal jugular 399 veins in the placement of central venous catheters in ENT cancer patients. ORL Nova, 2002, 12 : 145-8. V. Scavée Department of Thoracic and Vascular Surgery Saint-Pierre Clinic Avenue Reine Fabiola B-1340 Ottignies, Belgium Tel. : +32 10 43 72 35 E-mail : vincent.scavee@skynet.be