Anosmia after Intranasal Zinc Gluconate Use
advertisement

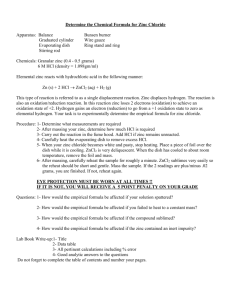
Anosmia after Intranasal Zinc Gluconate Use Bruce W. Jafek, M.D., Miriam R. Linschoten, Ph.D., and Bruce W. Murrow, M.D., Ph.D. ABSTRACT Background: Zinc is an essential mineral. Beneficial zinc absorption takes place via enteral, parenteral, or cutaneous routes. However, direct application to the olfactory epithelium has been reported to cause loss of smell. Recently, intranasal zinc gluconate has been recommended as a treatment for the common cold. Severe posttreatment hyposmia and anosmia have been observed. Methods: The case report of a typical patient is presented and analyzed in detail, followed by a series of patients with severe hyposmia or anosmia after the use of intranasal zinc gluconate. Results: Although interindividual variation in drug response and drug effect is apparent, the severe hyposmia or anosmia appears to be long lasting or permanent in some cases. The mechanism of olfactory loss is thought to be the direct action of the divalent zinc ion on the olfactory receptor cell. Conclusions: Zinc ions are toxic to olfactory epithelium. Reports of severe hyposmia with parosmia or anosmia have occurred after intranasal use of zinc gluconate. (American Journal of Rhinology 18, 137–141, 2004) Z inc is an essential element found in almost every cell. It is involved in a number of areas of human physiology, including the activity of ⬃100 enzymes,1 the immune system,2,3 wound healing,4,5 the senses of taste and smell,4,5 and DNA synthesis.6 Zinc also supports normal growth and development during pregnancy, childhood, and adolescence.7,8 The deleterious effects of both deficiency2,5,6,9–11 and toxicity (acute and chronic)2,12,13 are described. From the Department of Otolaryngology—Head and Neck Surgery, University of Colorado School of Medicine, Denver, Colorado Address correspondence and reprint requests to Bruce W. Jafek, M.D., F.A.C.S., UCHSC (B-205) Otolaryngology, 4200 E. Ninth Ave., Denver, CO 80262 Copyright © 2004, OceanSide Publications, Inc., U.S.A. Beneficial zinc absorption takes place via enteral, parenteral, or cutaneous routes.5,13 However, direct application to the olfactory epithelium was known to be toxic over 60 years ago.14–16 This toxicity is thought to be caused by the direct effects of the divalent zinc ion on the olfactory receptor cell.17–19 Otherwise beneficial divalent ions (e.g., copper, cadmium, and barium) also have been shown to be toxic when applied directly to the olfactory epithelium.17–19 Recently, intranasal zinc gluconate has been recommended as a treatment for the common cold.20 We present a series of patients with severe hyposmia or anosmia after the use of intranasal zinc gluconate. METHODS/OBSERVATIONS Case Reports 55-year-old man with previously normal taste and smell developed clear rhinorrhea and congestion and treated himself with over-the-counter (OTC) zinc gluconate* for a self-diagnosed cold. He noted immediate burning in his nose and did not use the spray again. He noted immediate anosmia, which was persistent. He also noted a “slightly salty” taste, which was intermittent. He did not smoke. He had rheumatoid arthritis, for which he took Remicade (Imfliximab, CENTOCOR, Inc., Malvern, PA) and regular bursts of prednisone (which did not subsequently improve his anosmia). He also took Arava (Leflunomide, Aventis Pharmaceuticals, Inc., Kansas City, MO) until 8 weeks before the incident and methotrexate (for the arthritis) until 10 weeks before the incident. His other medications included Prilosec (Omeprazole, AstraZeneca PLC, London, U.K.), Allegra, (Fexofenadine HCl, AstraZeneca PLC), and Flonase (Fluticasone Propionate, Glaxo Welcome, Inc., Research Triangle Park, NC). He had some indications of lupus and his liver function tests were “borderline normal.” He was otherwise in excellent health. He was seen by an otolaryngologist, and the otolaryngo- A *Zicam, Mattrixx Initiatives, Phoenix, AZ American Journal of Rhinology 137 logical examination was normal. A magnetic resonance image, with and without contrast, was normal. No evidence of sinus disease was seen. Detailed chemosensory evaluation was done. Absolute monorhinal butanol sensitivity was determined with a twoalternative forced-choice method using a maximum-likelihood adaptive staircase procedure.21 This procedure continuously estimates the sensory threshold while keeping track of the pattern of responses, as well as response bias. The threshold results indicated severely limited detection ability bilaterally. Odor identification was absent on the right side and severely limited on the left. The composite score indicated severe hyposmia. Using Vicks VapoRub (Proctor & Gamble, Cincinnati, OH) as a trigeminal stimulant, bilateral normal trigeminal activity was determined. Taste testing was normal except for the salty taste, which was partially extinguished by 0.5% Diclone (Antra, Astra Pharmaceutical Products, Inc., Westborough, MA) application. The severe hyposmia has persisted, unchanged, 10 months posttesting and 23 months postincident. Patient Series Data ur taste and smell center (Department of Otolaryngology, University of Colorado School of Medicine, Denver, CO) receives numerous inquiries from patients with chemosensory dysfunction. By reviewing these, a number of patients with loss of smell after the use of intranasal zinc gluconate have been identified. Seven men and three women, aged 31–55 years comprised the study series. The distinguishing characteristics were immediate, severe burning of the nose (similar to that reported previously in the zinc literature16) after the use of intranasal zinc gluconate, followed by severe hyposmia with parosmia or anosmia in patients who reported previously normal taste and smell and no other causative history to account for the loss. Through the use of the Colorado Chemosensory Questionnaire, the possibility of other causes of chemosensory loss (e.g., previous sinus surgery or chronic sinusitis, nasal polyposis, or other pathology or use of potentially toxic medications) was ruled out. We assume that additional patients did not contact us and that additional cases still have not been diagnosed, raising the apparent incidence of the smell loss. O DISCUSSION n 1934, investigations of the local effect of chemicals in controlling viral disease (polio) in experimental animals had shown the apparent beneficial effects of intranasal alum in preventing polio in exposed monkeys.14 Intranasal picric acid then was tried with apparent greater success. Schultz methodically began testing a long list of chemicals in the hope of finding the ideal one that offered the most protection and could be used safely on humans.22 He found what he thought was the “golden chemical,” zinc sulfate.22,23 The theory was that zinc ions “coagulated natural proteins in the olfactory epithelium, forming a protective coating around I 138 the nerves, which prevented them from absorbing the polio virus.”14 At that time, the hypothesis of the pathogenesis of polio was that the virus was inhaled into the olfactory cleft and then attacked the olfactory nerves to travel “along these tiny nerves to the spinal cord where large motor bodies are located.”14 Supporting this theory, the virus had been recovered from the nasal discharge of polio patients as well as from monkeys artificially infected with the disease. Invariably, the olfactory mucosa showed the marks of the virus and microscopic pathological changes were found along the olfactory nerves extending to the motor nerve cells of the spinal cord.14 When the olfactory nerves were cut, uptake of the virus in exposed monkeys appeared to be blocked, while the disease occurred in control animals (monkeys with intact olfactory nerves). The watchword became, “protect the nose and prevent polio.”24 Schultz initially tried the alum-picric acid on humans as an intranasal spray during the summer of 1936 when an epidemic of polio struck the southern states.14 The results of the experiment in ⬎4600 children and adults treated were “most discouraging,” but the failure was attributed to the haphazard manner in which the solution was administered and the study was termed “unscientific” and “confidence in chemically induced prevention of the dread disease was unabated.”14 Schultz argued that the Alabama experiment had failed for two reasons: the alum-picric acid solution was intrinsically inferior to his own zinc sulfate compound and protection could only be gained by erecting an impenetrable barrier around the olfactory nerves. The success of the treatment would be judged by making the nerves “inactive for a period of time,” the criterion for success being “loss of the sense of smell.”14 “Protection against the virus” could not be gained “unless the protective spray had temporarily (authors’ emphasis) destroyed the sense of smell.”14 Several authors debated the proper technique and cautioned that only “trained experts” could properly administer the zinc.24–26 To accomplish proper application, the zinc had to be administered by experts in nose anatomy to reach the critical area and had to be used often enough to produce the desired anosmia, which Schultz reiterated was only a temporary condition.14 In 1937, therefore, during an epidemic in Toronto, Canada, special clinics manned by “nose and throat specialists” sprayed a population of 5000 children twice at intervals of 10–12 days with a solution of 1% zinc sulfate and 0.5% Pontocaine.15 There were additional “off protocol” administrations of the treatment as well, estimated as over “a thousand more children,” as the public sought relief from the dreaded disease. Most of the children suffered “some discomfort” from the nasal spray. However, there were a few cases of severe nasal pain that “continued for many hours.”15 The most frequent complaints were headaches, nausea or vomiting, and some stiffness of the neck. Sometimes the child developed transient fever, but overall, “reactions were singularly few.”14,15 “It was many months later that Schultz began receiving complaints from physicians May-June 2004, Vol. 18, No. 3 that many of their patients had suffered a complete and permanent loss of the sense of smell.”14 Using relatively primitive psychophysical testing, employing oil of cloves and oil of spearmint, 10–13% of children were thought to be anosmic, apparently permanently.14 Note that because oil of cloves and oil of spearmint stimulate the trigeminal nerve, a percentage of 10–13% is most likely a gross underestimation of the actual percentage of anosmics. Unfortunately, the protective spraying with zinc sulfate did not alter the attack rate of the disease and a more critical examination of the olfactory tissues previously thought to be involved, along with additional experimentation, ruled out the olfactory epithelium as the sole portal of entry of the polio virus into humans.15 But the toxic effect of zinc on human olfactory epithelium was clearly shown. Although interindividual variation in drug response and drug toxicity is apparent, the effects appear to be dose related and long lasting or permanent in some cases. Subsequently, transient olfactory loss has been reported in some of the studies of experimental animals such as that of McBride.27 The use of intranasal zinc was abandoned. In 1976, Matulionis observed distinct patterns of degeneration and regeneration of the olfactory epithelium in mice receiving intranasal irrigation with 1% aqueous zinc sulfate.28 During the first 24 hours after treatment, three progressive manifestations of the degenerative process were seen: (1) a relatively mild condition which was characterized by surface irregularities produced by cell protrusions, highly vacuolated cytoplasm, presence of large lysosomelike bodies, and prominent intercellular spaces; (2) a more severe condition in which large areas of the epithelium were detached from the basement membrane and cellular debris was present in the nasal chamber; and (3) a condition of total or near-total denudation of the epithelium of olfactory mucosa. The basal lamina was continuous and intact in most regions and the integrity of the subadjacent connective tissue mostly was well preserved. The nerve bundles of the fila olfactoria were noted to be in varying degrees of degeneration during the course of the experiment, with the most advanced neural degeneration from 24–72 hours after treatment. In 1978, Harding, described immediate and total anosmia in mice irrigated with intranasal 0.17 M ZnSO4.17 This anosmia persisted for 6 weeks in at least 80% of the treated animals and 4 months in one-half of the treated animals. Changes were still apparent at 1 year, the limit of the experimental observation. By 1982, Cancalon attributed the “necrotic effect” of various salt solutions to the divalent “zinc cation” in irrigation experiments on the catfish olfactory mucosa, using concentrations of 6–960 mM of zinc sulfate.18 He noted that ZnSO4 and ZnCl were “equally effective in destroying the olfactory epithelium, offering proof that it was the zinc cation that produces the toxic effects. He reported that the damage was very reproducible, largely concentration independent, and almost completely specific for the olfactory American Journal of Rhinology receptor cells. The nonsensory respiratory cells were unaffected. The sustentacular cells surrounding the receptor cells were affected mainly by a loss of microvilli. The olfactory cells started to degenerate within a few hours and by day 4, only 20% of the original receptor population remained. Mucosal basal cell mitosis increased during days 3 and 4 and by day 7, the receptor population had reached 80% of its original value. On the other hand, when the salt solution was maintained in contact with the olfactory epithelium for several days, only very limited regeneration occurred as most of the lamellae were irreversibly destroyed. In 1997, Mayer and Rosenblatt reported that the spray application of ZnSO4 (1.74% in 0.9% saline) to the olfactory mucosa in rats produced severe nasal congestion that cleared within 24 hours, followed by, in 48 hours, anosmia in 80% of the treated animals.29 From a more basic standpoint, the transduction of odors into electrical signals takes place on the surface of the olfactory receptor cells and is necessary for olfactory function. In particular, an odorant binds to a cyclic nucleotidegated receptor that generates cyclic adenosine monophosphate, which in turn activates a nonspecific cation channel, allowing Ca2⫹ entry into the cell. This Ca2⫹ then activates a calcium-activated chloride channel that results in depolarization of the cell. The divalent cation Ba2⫹ is suggested to block the nonspecific cyclic nucleotide-gated channel in animals.30 This also appears to be the case in human olfactory receptor cells (Fig. 1). Zinc, a divalent cation, also may block this channel and interfere with olfactory function. Ongoing studies are evaluating both the short-term and long-term effects of zinc on olfactory cell function. In 2000, Hirt et al., recommended the intranasal use of an OTC zinc gluconate nasal gel formulation* to bring the medication closer to the causative organism, rhinovirus, in alleviating the symptoms of the common cold, decreasing the duration of symptoms by 75%.20 Citing the antirhinoviral activity of ionized zinc,31–33 they recommended that the “mixed benefits” of zinc gluconate lozenges dissolved in the mouth, affecting rhinovirus in the nose to prevent or alleviate the symptoms of the common cold, could be improved by “delivery of ionic zinc directly to the site of infection.”20,34,35 They noted that although 42% of “zinctreated patients” and 37% of controls described a “slight tingling or burning sensation on intranasal zinc application,” five other potential side effects (nausea, bad taste reactions, odor, dizziness, and drowsiness) were not found. It is not apparent from their publication that they tested for or considered olfactory deficits in their study group. Other studies concluded that intranasal zinc was not nearly as helpful in the treatment of the common cold. Belongia found “no effect on the duration of the common cold, but possibly mild and transient reduction in the severity of nasal symptoms, using 0.12% zinc sulfate nasal *Zicam, Mattrixx Initiatives, Phoenix, AZ 139 Figure 1. Human olfactory epithelium was isolated from fresh cadavers and EOG recording techniques used to study olfactory transduction.40 (A) Cineole (100 M) applied to the olfactory epithelium produced a response (B) that in the presence of 5 mM of Ba2⫹ was blocked. This effect was fully reversible after several minutes of exposure to Ba2⫹. The bars below each trace indicate the application time of cineole and note that there was a delay before the start of the upward-going odorant response in panel A. Saline control traces were subtracted from each trace and low pass filtering was used. spray.”36 Turner concluded that the commercially available zinc gluconate gel* was “‘ineffective’ in preventing progression of an experimentally induced rhinovirus infection 33 mM of zinc gluconate in an emulsification of benzalkonium chloride, glycerine, hydroxymethylcellulose, sodium chloride, and sodium peroxide, buffered to pH 7.2.”37 A single case report of anosmia due to inhalational zinc soon followed.38 In 2003, Mossad concluded that ionic zinc (33 mmol/L of zincum gluconium) “shortens the duration and reduces symptom severity of the common cold in healthy adults.”39 140 Adverse effects were solicited by an open-ended telephone question, the most commonly identified being “nasal stinging or burning.” Neither olfactory complaints nor evaluation were mentioned. Because patients use the intranasal zinc when they “feel a cold coming on,” postviral anosmia should be considered a cause for the chemosensory loss. Three factors argue against this conclusion. First, the admittedly modest study population had a male preponderance of more than 2:1, as opposed to the 2:1 female ratio seen in postviral anosmia; the patients in the intranasal zinc group also were younger, on average, than reported postviral patients.40 Second, postviral anosmia typically occurs with “the worst upper-respiratory infection (URI) I’ve ever had.” Our study population typically used the intranasal zinc early in the course of a mild URI, and most convincing was the immediate, acute, “burning” pain with the use of the zinc gluconate, followed immediately by persistent severe hyposmia or anosmia. Other explanations for the smell loss (e.g., post-traumatic, etc.) were ruled out by a negative history in each case. A Web site maintained by Dr. Karl L. Wuensch offers additional discussion of the issue of loss of smell after the use of intranasal zinc.41 Recent advertisements have added a pediatric applicator for intranasal zinc. This extension of the use of intranasal zinc gluconate to the pediatric age group is of concern because the use of intranasal zinc in this age group could be expected to generate anosmia although this age group is less likely to describe the symptom, resulting in repeated treatments rather than immediate discontinuation of the drug. It should be noted that only a single trademarked preparation of zinc gluconate was available at the time of this report and was used by each of the patients cited immediately before their loss of smell.* Subsequently, this brand has been extended by the manufacturer to several products. This communication only concerns the product containing zinc gluconate. CONCLUSION n conclusion, the divalent zinc ion is reported to be toxic to olfactory epithelium, the toxicity apparently being related to both concentration and interindividual sensitivity, but not the source of the ion (e.g., salt source, as shown by Cancalon18 and others). The temporal association of the use of intranasal zinc gluconate with the development of severe partial or total loss of the sense of smell raises significant concern regarding its safety for intranasal application in humans. Given the prevalence of viral URIs, the strong desire of patients for symptomatic relief and the widespread availability and marketing of OTC products for this purpose, there is the potential for a very large number of people to be exposed to intranasal zinc gluconate. Therefore, even if the frequency of loss of smell is low, the number of I *Zicam, Mattrixx Initiatives, Phoenix, AZ May-June 2004, Vol. 18, No. 3 people affected by this treatment could be alarmingly high. The public may assume that because intranasal zinc gluconate is sold as an OTC “patented, homeopathic” preparation, containing a “natural,” or even “essential” element, that it is safe. This report raises important questions about that generalization. Because the effects appear to be somewhat dose-related, use of this drug in the pediatric age group would be expected to generate an even larger incidence of anosmia in this population and is especially concerning. If history repeats itself, and the unexpected always happens, how incapable must man be of learning from experience. —George Bernard Shaw (1856–1950), Irish dramatist REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. Sandstead HH, and Alcock NW. Zinc: An essential and unheralded nutrient. J Lab Clin Med 130:116–118, 1997. Solomons NW. Mild human zinc deficiency produces an imbalance between cell-mediated and humoral immunity. Nutr Rev 56:27–28, 1998. Prasad AS. Zinc: An overview. Nutrition 11:93–99, 1995. Heyneman CA. Zinc deficiency and taste disorders. Ann Pharmacother 30:186–187, 1996. Lansdown AB. Metallothioneins: Potential therapeutic aids for wound healing in the skin. Wound Repair Regen 10:130–132, 2002. Prasad AS, Beck FW, Grabowski SM, et al. Zinc deficiency: Changes in cytokine production and T-cell subpopulations in patients with head and neck cancer and in noncancer subjects. Proc Assoc Am Physicians 109:68–77, 1997. Simmer K, and Thompson RP. Zinc in the fetus and newborn. Acta Paediatr Scand Suppl 319:158–163, 1985. Fabris N, and Mocchegiani E. Zinc, human diseases, and aging. Aging (Milano) 7:77–93, 1995. Prasad AS. Zinc deficiency in women, infants, and children. J Am Coll Nutr 15:113–120, 1996. Hambidge KM. Mild zinc deficiency in human subjects. In Zinc in Human Biology. Mills CF (Ed). New York: Springer-Verlag, 281–296, 1989. King JC, and Keen CL. Zinc. In Modern Nutrition in Health and Disease, 9th ed. Shils ME, Olson JA, Shike M, et al. (Eds). Chap. 11. Baltimore: Williams & Wilkins, 223–239, 1999. Hooper PL, Visconti L, Garry PJ, et al. Zinc lowers high-density lipoprotein-cholesterol levels. J Am Med Assoc 244:1960–1961, 1980. Shenkin A. Trace elements and inflammatory response: Implications for nutritional support. Nutrition 11(1 suppl):100–105, 1995. Berg RH. I can stop the virus. In Polio and Its Problems, Ch. 5. Berg RH (Ed). Philadelphia: Lippincott, 34–47, 1948. Rutty CJ. The middle-class plague: Epidemic polio and the Canadian state, 1–36-1937. Can Bull Med Hist 13:277–314, 1996. Tisdall FF, Brown A, and Defries RD. Persistent anosmia following zinc sulphate nasal spraying. J Pediatr 13:60–62, 1938. Harding JW, Getchell TV, and Margolis FL. Denervation of the primary olfactory pathway in mice. V. Long-term effects of intranasal ZnSO4 irrigation on behavior, biochemistry, and morphology. Brain Res 140:271–285, 1978. Cancalon P. Degeneration and regeneration of olfactory cells induced by ZnSO4 and other chemicals. Tissue Cell 14:717–733, 1982. American Journal of Rhinology 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. Moran DT, Rowley JC III, Aiken GR, and Jafek BW. Ultrastructural neurobiology of the olfactory mucosa of the brown trout, Salmo trutta. Microsc Res Tech 23:28–48, 1992. Hirt M, Nobel S, and Barron E. Zinc nasal gel for the treatment of common cold symptoms: A double-blind, placebo-controlled trial. Ear Nose Throat J 79:778–780, 782, 2000. Linschoten M, Harvey LO Jr, Eller PM, and Jafek B. Fast and accurate measurement of taste and smell thresholds using a maximum-likelihood adaptive staircase procedure. Percept Psychophys 63:1330–1347, 2001. Schultz EW. Immunity and prophylaxis in poliomyelitis. JAMA 107:2102–2104, 1936. Schultz EW, and Gebhardt LP. Zinc sulfate prophylaxis in poliomyelitis. JAMA 108:2182–2184, 1937. Peet MM, Echols DH, and Richter HJ. The chemical prophylaxis for poliomyelitis. The technique of applying zinc sulfate intranasally. JAMA 108:2184–2187, 1937. Shahinian L, Bacher JA, McNaught RC, and Newell RR. Chemoprophylaxis in poliomyelitis. JAMA 110:1254–1257, 1938. Ashley RE. Chemoprophylaxis against impending poliomyelitis. Arch Otol 29:104–114, 1939. McBride K, Slotnick B, and Margolis FL. Does intranasal application of zinc sulfate produce anosmia in the mouse? An olfactometric and anatomical study. Chem Senses 28:659–670, 2003. Matulionis DH. Light and microscopic study of the degeneration and early regeneration of olfactory epithelium in the mouse. Am J Anat 145:79–99, 1976. Mayer AD, and Rosenblatt JS. Peripheral olfactory deafferentation of the primary olfactory system in rats using ZnSO4 nasal spray with special reference to maternal behavior. Physiol Behav 53:587–592, 1997. Miyamoto T, Restrepo D, and Teeter J. Voltage-dependent and odorant-regulated currents in isolated oflactory receptor neurons of the channel catfish. J Gen Physiol 99:505–529, 1992. Korant BD, Kauer JC, and Butterworth BE. Zinc ions inhibit replication of rhinoviruses. Nature 248:588–590, 1874. Korant BD, and Butterworth BE. Inhibition by zinc of rhinovirus protein cleavage: Interaction of zinc with capsid polypeptides. J Virol 18:298–306, 1976. Kelly RW, and Abel MH. Copper and zinc inhibit the metabolism of prostaglandin by the human uterus. Biol Reprod 28:883–889, 1983. Novick SG, Godfrey JC, Godfrey NJ, and Wilder HR. How does zinc modify the common cold? Clinical observation and implications regarding mechanisms of action. Med Hypotheses 46:295–302, 1996. Godfrey JC, Godfrey NJ, and Novick SG. Zinc for treating the common cold: Review of all clinical trials since 1984. Altern Ther Health Med 2:63–72, 1996. Belongia EA, Berg R, and Liu K. A randomized trial of zinc nasal spray for the treatment of upper respiratory illness in adults. Am J Med 111:103–108, 2001. Turner RB. Ineffectiveness of intranasal zinc gluconate for the prevention of experimental rhinovirus colds. Clin Inf Dis 33: 1865–1870, 2001. DeCook CA, and Hirsch AR. Anosmia due to inhalational zinc: A case report. Chem Senses 25:659, 2000 (Abs). Mossad SB. Effects of zincum gluconium nasal gel on the duration and symptom severity of the common cold in otherwise healthy adults. QJM 96:35–43, 2003. Duncan HJ. Postviral olfactory loss. In Taste and Smell Disorders, Ch. 6. Seiden AM (Ed). New York: Thieme, 72–78, 1997. Murrow BW, Jafek BW, and Restrepo D. The use of fresh cadaveric human olfactory epithelium for physiologic study. AChemS, Sarasota, FL, April, 2001. e 141