I. Principle Blood specimens obtained by skin puncture are
advertisement

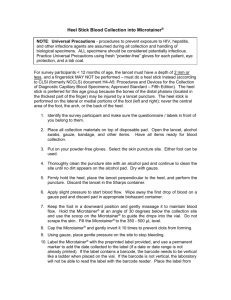
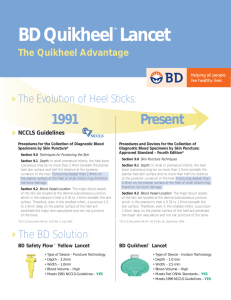
I. Principle Blood specimens obtained by skin puncture are especially important in pediatrics, because small but adequate amounts of blood for laboratory tests can be obtained with this technique. It is also the primary sample used when collecting blood for bedside testing such as whole blood glucose and hemoglobin. The quantity of blood removed and the avoidance of injury during specimen collection are important considerations. Therefore, blood collection by skin puncture is the technique of choice for collecting small amounts of blood from children, especially newborns. In children, depending on the age, skinpuncture blood may be obtained from the heel or the finger. II. Supplies Assemble the following supplies on a tray or in a drawing room: Microtainers Retractable lancets Alcohol, 78% isopropyl, or alcohol prep pads Gauze pad or cotton ball Bandages Heel warmer Lancets Various devices for skin puncture are available. Refer to the manufacturer’s directions for optimum performance. In small or premature infants, the heel bone may be no more than 2.0 mm beneath the plantar heel-skin surface. Puncturing deeper than 2.0 mm on the plantar surface of the heel of small infants may therefore risk bone damage. The major blood vessels of the skin are located at the dermal-subcutaneous junction, which in the newborn’s heel is 0.35 to 1.6 mm beneath the skin surface. Therefore, even in the smallest infant, a puncture 2.0 mm deep on the plantar surface of the heel will penetrate the major skin vasculature and not risk puncture of the bone. III. Patient Preparation A. Patient identification- Testing personnel must positively identify the patient that is being drawn. The following step ensure patient identification: 1. In an Outpatient setting: a. Ask the patient to state their full name, including the spelling of an unusual name. If the patient is very young, ask his/her parents or guardian to state the name and/or the correct spelling. b. Compare the name with that on the patient chart you have. 2. B. C. D. E. IV In an inpatient setting: c. Compare your information with the patient’s name and hospital number found on the patient’s wristband. d. If the patient is old enough, identify yourself to the patient stating that you have come to test their blood. Reassuring the Patient Testing personnel must gain the patient’s confidence and assure him that although the puncture will be slightly painful, it will be of short duration. Patients should never be told that “this will not hurt,” and they should be told when the needle enters the skin so as to avoid fright. Determine whether the patient has fasted (if necessary) Some tests require the patient to fast or to eliminate certain foods from the diet before the blood drawing. Time and diet restrictions vary according to the tests. Such restrictions are needed to ensure accurate results. Verify that the patient is free of latex allergies. Assemble the necessary supplies, wash your hands, and put on gloves. Procedure for Heelstick A. B. C. D. E. F. G. Prewarm the infant’s heel with a warm, wet towel (or other warming device) at a temperature no higher than 42C for three to five minutes (if the temperature used to warm the heel is too high, you risk burning the baby). This is essential for capillary blood gas sample collection, and it greatly increases the blood flow for collection of other specimens. Clean the chosen puncture site with alcohol and allow the site to thoroughly dry. Use the sides of the heel. Do not perform punctures on the posterior curvature of the heel. Do not puncture through previous sites which may be infected. (See training manual for details on selecting a puncture site). If possible, place the baby in a prone position (on stomach). This may not be possible in the neonatal intensive care unit. Hold the patient’s heel firmly to prevent sudden movement and to facilitate adequate puncturing. Select the appropriate retractable lancet, position it above the selected site, and activate. Discard of used lancet in approved puncture-resistant sharps container. Puncture sites should be oriented perpendicular to the skin print lines so the blood drop will well up, and should not be in the same place as a previous heel stick. After the chosen site has been prepared and punctured, the first drop of blood should be wiped away with a gauze pad, since the H. I. J. K. L. M. N. V. first drop is most likely to contain excess tissue fluid. Discard of gauze in a biohazard container. Newborns often do not bleed immediately. If the blood is not free flowing, blood flow may be enhanced by holding the puncture site downward and gently applying intermittent pressure to the surrounding tissue. Strong repetitive pressure (milking) must not be applied. Milking may cause hemolysis or tissue-fluid contamination of the specimen. Fill the testing device as needed by gently scooping up the drops of blood and allowing them to roll into the testing device. Drops of blood should be allowed to flow freely. After blood has been collected from an infant’s heel, the foot should be elevated above the body and a clean gauze pad should be pressed against the puncture site until the bleeding stops. Do not use adhesive bandages on infants. Adhesive bandages can cause irritation to an infant’s skin, and an older infant might remove the bandage, put it in its mouth, and aspirate it. Continue with the testing at the bedside (see individual testing procedures for specific instructions). If sample is to be taken to another location for testing, properly label the specimen with patient’s name and/or MR#. Remove gloves and wash hands. Discard of gloves, lancets, and other used materials in their appropriate containers. Procedure for Fingerstick NOTE: A. B. C. D. E. Fingersticks should not be performed on infants younger than 6 months of age due to the short distance between the finger bone and the skin surface. Clean the chosen puncture site with alcohol and allow the site to thoroughly dry. Perform the puncture on the center of the palmer surface the finger- not at the side or tip of the finger, because the tissue on the side and tip of the finger is about half as thick as the tissue in the center of the finger. The middle finger and ring finger are the preferred site, because the thumb has a pulse and the index finger may be more sensitive or callused. The fifth finger must not be puncture, because the skin is too thin. (See training manual for details on selecting a puncture site). Avoid a finger that is cold, cyanotic (blue), swollen, or inflamed. The patient should be positioned so that the finger is steady and supported in a comfortable position. With your thumb and index finger, grasp the patient’s finger about three inches from the tip of the finger. With your other hand, hold the sides of the patient’s finger. F. G. H. I. J. K. L. M. N. O. P. Q. R. S. T. VI. Moving your supporting hand toward the tip of the patient’s finger. Applying a massaging motion to the fleshy portion of the finger. Repeat this massaging process five or six times. Clean the chosen puncture site with alcohol and allow the site to thoroughly dry. Select the appropriate retractable lancet, position it above the selected site, and activate. Discard of used lancet in approved puncture-resistant sharps container. Puncture sites should be oriented perpendicular to the lines of the fingerprint (across the fingerprint). If the cut is made across the fingerprints and the area has been wiped dry, the blood should well up into a large rounded drop. (If the cut has been made along the lines of the fingerprint, the blood will stream down the finger). After the chosen site has been prepared and punctured, the first drop of blood should be wiped away with a gauze pad, since the first drop is most likely to contain excess tissue fluid. Discard of gauze in a biohazard container. If blood does not flow freely, increase blood flow by holding the finger downward and applying gentle continuous pressure above the puncture site. Do not massage the area since this may contaminate the blood sample with tissue fluid. If blood does not flow easily after gentle pressure, make another puncture using a new sterile lancet. Fill the testing device as needed by gently scooping up the drops of blood and allowing them to roll into the container. Drops of blood should be allowed to flow freely. After blood has been collected from the patient’s finger, place a piece of gauze on the site and apply gentle pressure to stop the blood flow. Apply bandage to puncture site after bleeding has stopped. Continue with the testing at the bedside (see individual testing procedures for specific instructions). If sample is to be taken to another location for testing, properly label the specimen with patient’s name and/or MR#. Remove gloves and wash hands. Discard of gloves, lancets, and other used materials in their appropriate containers. Additional Considerations Blood must not be obtained from the: Earlobe. Central area of an infant’s heel. Fingers of a newborn. Swollen or previously punctured site, because accumulated tissue fluid will contaminate the blood specimen. VII. References NCCLS Procedures and Devices for the Collection of Diagnostic Blood Specimens by Skin Puncture; Approved Standard- Fourth Edition, September 1999 NCCLS Specimen Collection 1989. 6.14-3. Blumenfeld, TA: Clinical Application of Microchemistry. In Werner M(ed): MicroTechniques for the Clinical Laboratory: Concept and Application, pp 1-15. New York, John Wiley & Sons, 1976. Blumenfeld, TA, Turi GK, Blanc WA: Recommended Sites and Dept. of Newborn Heel Skin-Punctures Based on Anatomic Measurements and Histopathology, Lancet 1: 213, 1979. Meites, S, Levitt MS, Blumenfeld, TA, Hammond KB, Hicks JM, Jill GJ, Sherwin JE, Smith EK: Skin Puncture and Blood Collecting Technique for Infants, Clinical Chemistry 25: 183-189, 1979. Blumenfeld TA, Hertelendy WG, Ford SH: Simultaneously Obtained Skin Puncture Serum, Kin Puncture Plasma and Venous Serum compared and Effects of Warming the Skin Before Puncture. Clinical Chemistry 23: 1705, 1977. Michealsson M, Sjolin S: Hemolysis in Blood Samples from Newborn Infants. Acta Pedatric Scand 54: 325-330, 1965. Hicks JR, Rowland GL, Buffone GJ: Evaluation of a New Blood Collection Device (microtainer) That is Suited for Pediatric Use. Clinical Chemistry 22: 2034-2036, 1976. Sell EJ, Hansen RC, Struck-Pierce S: Calcified Nodules on the Heel: A Complication of Neonatal Intensive Care. J Pediatr 96: 473-475, 1980. Feusner JH, Behrens JH, Detter JC, Cullen TC: Platelet Counts in Capillary Blood. AM J Clin Pathol 72: 410-414, 1979.