When is solution filtration necessary?
advertisement

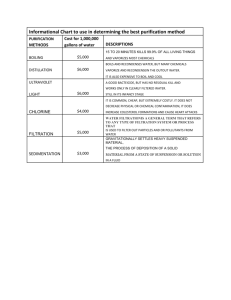
When is solution filtration necessary? Why are we still talking about this? Filters and phlebitis were hot topics 20 years ago, culminating in the trial published by Falchuck et al in NEJM 1985 that found phlebitis was caused by microparticulates and could be prevented by inline filtration.. or did it? In the subsequent 20 years, increasing numbers of infusion providers – hospitals, long term care, home infusion – stopped using routine filtration both inline and in pharmacy compounding. And all who kept data found no significant change in the frequency of phlebitis. Was the decision based on cost or cost/benefit? Does a filter prevent something from happening, reduce morbidity, and reduce the associated costs of infusion therapy? Is it that phlebitis is the consequence of many more things than microparticulate contamination? The 1991 trial by Dr Maki listed the risk factors for phlebitis as: Antibiotics: relative risk = 2 Female: relative risk =1.9 Catheterization > 48 hrs: relative risk = 1.8 Catheter material: relative risk = 0.7 Catheter related infection: relative risk = 6 Phlebitis with previous catheter: relative risk = 1.5 Anatomic site hand/wrist: relative risk = 0.7/0.6 Within the antibiotic category (and other drugs) one must consider the pH, osmolarity, and infusion rate along with particulate contamination. It is known that certain disease states, trauma, and stress predispose to vascular sensitivity and a phlebitic response to irritants, and clinical trials have clearly demonstrated that significant intrapatient and interpatient variability exists. So what is the role of filters in infusion therapies? • Reduce phlebitis? • Prevent infection? • Prevent air emboli? • Sterilize the solution? • Reduce particulate contamination? • Prevent endotoxin contamination? • Extend the expiration dating of the infusate? What is a filter, how does it work, describe the types and purposes of filters Filters are loosely classified by the size or nature of the particles they remove from the solution being purified. The general classifications are macrofiltration, microfiltration, ultrafiltration, nanofiltration, and reverse osmosis. The key to classifying a filter is determining what the filter is capable of retaining. The pore size (e.g., 0.2, 1.2 micron) has nothing to do with physical measurement of the pore sizes. The size designation is actually tied to the ability of the filter to retain types and quantities of organisms. A 0.2 micron filter is capable of retaining 1 X 107 colony forming units of Brevundimonas diminuta per square centimeter of filter, bacteria commonly of a 0.3 micron size. Many factors influence the ability of a filter to retain micro-organisms – the pressure at which the solution passes through the filter, the solution flow rate, the duration of the filtration, the throughput (volume filtered), and the characteristics of the microorganisms – starved and water borne (due to osmotic changes) can pass through filters that would retain their properly nourished and diluted cohorts. Because no filter is guaranteed to work under all conditions, it is important to select the right filter for each use based on these characteristics. The only way to know the filter worked is to test the effluent or the filter itself (filter integrity test/bubble point Marc Stranz Page 1 AVA 18th Annual Conference September 2004 When is solution filtration necessary? test). That is not done in clinical situations, but is routine in drug manufacturing and is expected in high risk (nonsterile to sterile) pharmacy compounding. Macrofiltration is the coarsest category. These filters remove particles > 15 micron in size. The most common clinical application is in IVIG filtration and is of more historical than clinical relevance. Microfiltration includes the 0.1 to 10 micron filter sizes. The 0.2 micron filter retains most bacteria, fungus, and particulate matter, but no viruses. The 1.2 micron filter is used for fat emulsion filtration (captures inappropriately large fat globules and some unintentional precipitates. The 5 micron filter is used in filter needles and straws for glass ampules. The 0.1 micron filter or redundant 0.2 micron filters is standard in pharmaceutical manufacturing because of its greater (double that of a single 0.2 micron) sterilizing and particle removing capacity. Ultrafiltration uses membranes to separate macromolecules. Membrane filtration captures all bacteria, most virus particles, and even large proteins. Nanofiltration also uses membranes to separate fluids or ions. This process pushes the solution through even smaller pores than ultrafiltration and removes almost all viruses and many proteins. Reverse osmosis uses a semi-permeable membrane and removes almost everything from the solution – not by size but by the electrical charge of the particles. If the particle is charged, it is removed, includes dissolved particles and ions. Reverse osmosis is commonly used to make sterile water for injection, one of the most pure solutions. How does filtration help the body cope with infusions? The common pathogenic microorganisms are larger in size than 0.2 microns. If the infusate were contaminated, a 0.2 micron filter would capture and retain these organisms. Pseudomonas and Klebsiella penetrate 0.45 micron filters. Although Serratia, E. coli, and other gram-negative bacteria are retained by filtration, they produce an endotoxin that is not retained by normal filters. Endotoxin production within a bacteria-contaminated filter begins within 24 hours, increases over time, and produces a constellation of symptoms including fever, chills, headache, and nausea. There are filters able to bind and retain endotoxins. The capillaries are about 8 microns in diameter. The terminal arterioles that feed the capillaries are 20-50 microns in diameter. The most common size of particulate matter in properly prepared infusates is 2 to 10 microns. Drug abusers are the extreme case of particulate and bioburden risk. They are known to suffer ophthalmic complications, tissue infarction, and severe pulmonary distress after injecting street drugs, as well as a variety of infections. In the patient receiving properly prepared solutions, microthrombi composed of platelets and neutrophils may develop from particles < 2 microns in diameter. These particles do lodge in the pulmonary microcirculation and generally result in foreign body-type granulomas. However, these reactions have not been correlated with clinical manifestations. Controlled clinical trials in humans cannot be conducted to determine the hazards associated with particulate matter contamination. Several animal models have been tested, but all failed to produce clinically significant harm beyond the formation of granulomas in these healthy animals. Marc Stranz Page 2 AVA 18th Annual Conference September 2004 When is solution filtration necessary? One trial has proposed clinical consequences to excessively particle-laden infusions. Lehr et al (2002) studied an animal model of particle contamination and microcirculation using low and high particle containing antibiotic solutions. No compromise of healthy tissue circulation occurred, despite the use of abnormally high particle count products (30 times normal). The investigators did find that postischemic tissue was adversely affected by the particles, showing loss of capillary perfusion. The authors suggest that particulate contaminants could adversely affect capillary blood flow in tissue that is already compromised by ischemia, which includes patients with trauma, major surgery, sepsis, or shock. The loss of capillary perfusion was apparently not mechanical obstruction by the particles, but could be the result of increased adhesivity of the endothelial lining, fibrogen deposition on endothelium, or activation of mononuclear cells. Reasons to use filters: Sterilization. Microbial contamination of commercial products is uncommon now. Pharmaceutical manufacturers: In 1978, the final current good manufacturing procedures (cGMP) were published. Prior to 1978, FDA inspections were cursory and sterile products were produced in unclassified areas, to inconsistent standards. The testing of sterile products was briefly mentioned in the new standards: “ For each batch purporting to be sterile, there shall be appropriate tests to determine conformance to such requirements”. Aseptic processes such as media fill and process simulation were voluntary. The FDA’s “Guidelines on Sterile Drug Products Produced by Aseptic Processing” were published in 1987 to address specific issues in the industry and included many of the current production guidelines. The United States Pharmacopeia (USP) is the official compendium of the FDA, establishing standards for drug safety, identity, strength, quality, and purity. These standards are updated annually and reflect the most current practices to achieve these goals. Within FDA approved pharmaceutical manufacturers, you can expect sterilization by both filtration and heat (where feasible). Compounding pharmacies. Until the release of USP Chapter 797 in January 2004, there were no consistent requirements for the production of sterile drugs by pharmacies. There were guidelines from USP (Chapter 1206) and the American Society of Healthcare Pharmacists (ASHP), but compliance was voluntary. The FDA has no authority to inspect pharmacies unless they are violating FDA guidelines that distinguish between compounding and manufacturing. State Boards of Pharmacy could regulate sterile compounding, but few have the skill to do so and regulations are cursory. Accrediting organizations had few enforceable standards on sterile compounding. The release of USP Chapter 797 was accelerated by the recent deaths attributed to bacterial and fungal contamination of injectable drugs. The new USP Chapter 797 addresses the following issues: • • • Responsibilities of all compounding personnel Classification of IV products into three risk levels, with quality assurance practices specific to each level Verification of compounding accuracy and sterilization Marc Stranz Page 3 AVA 18th Annual Conference September 2004 When is solution filtration necessary? • • • • • • • • • • • Personnel training and competence assessment in aseptic manipulation skills Environmental quality and control Equipment used in the preparation of compounded sterile products Verification of automated compounding devices for parenteral nutrition Finished product release checks and tests Storage and beyond-use (expiration) dating Maintaining product quality and control once the product leaves the compounding facility Packing, handling, storage, and transport of compounded sterile products Patient or caregiver training Patient monitoring and adverse events reporting A quality assurance program for compounded sterile products Relative to filtration, Chapter 797 requires that the compounding pharmacy demonstrate that injectable solutions are sterile. Sterilization through filtration (0.2 micron) is acceptable, but the pharmacy must also determine that the solution is in fact sterile. If no sterility test is performed, the chapter sets the following expiration dates for compounded products: 1. Low risk solutions (minibags, hydration, syringes) expire after 14 days refrigerated or 48 hours room temperature. 2. Medium risk solutions (parenteral nutrition, multi-day cassettes) expire after 7 days refrigerated or 30 hours room temp. 3. High risk solutions (nonsterile to sterile) expire after 3 days refrigerated or 24 hours room temperature. Infection control. There is no evidence that inline filters reduce microbial contamination of intravenous fluids. • • • • The 2002 publication of the CDC Guidelines for the Prevention of Intravascular CatheterRelated Infections says no data support inline filter efficacy in preventing infections associated with intravascular catheters and infusion systems. Newall et al. Observed hospitalized patients for septicemia for 1 year before and 1 year after 0.2 filter discontinued (19,221 iv days). No difference in septicemia. Centre for Clinical Effectiveness. Australia. Review of all published trials to 1999. No evidence found to support inline filtration to reduce line-associated bacteremia. Van Lingen et al. (Netherlands 2004) Found 0.2 micron filters significantly reduced bacteremia when the pre-existing line contamination rate was 14%. In high risk neonates receiving multiple therapies, line contamination rates may run to 30%. Particle removal. Particles are insoluble material present in injectable solutions. Mississippi mud – was once the nickname for vancomycin. From its introduction in the late 1950’s and through the mid-1980s, vancomycin vials also contained large amounts of fermentation broth impurities. The preparation was brown and thus was dubbed Mississippi mud because of its appearance. Before purification methods improved, vancomycin was a toxic antibiotic; however, the modern formulation has an excellent safety profile. This is indicative of how injectable drug manufacturing has changed in just the last 20 years. Marc Stranz Page 4 AVA 18th Annual Conference September 2004 When is solution filtration necessary? Pharmaceutical manufacturers: In the 1970’s, industry used 5 and 0.45 micron filters in the manufacturing process, as the particle requirements were lax, reflecting the technology available. The use of reverse osmosis for sterile water was new. Particle counters, automated filling machines, and cleanroom technology were in early development. Glass ampules were a common container, despite the knowledge that drug solutions extracted from ampules were particle laden. In the early 1990’s technology had evolved to the point that removal of particles > 10 micron in size was easy, but removal of particle of 1 micron or less was still difficult. The goal was to produce products with low levels of random particles of random size. That has evolved to current standards for processing drugs in solution that include prefiltration, redundant filtration, and use of the relatively new 0.1 micron filters. By starting with water for injection produced through reverse osmosis, the base is the most particle free solution available. The solution filtration methods for companies such as Abbott/Baxter/Braun include prefiltration with a 5 micron filter, two 0.45 micron filters, and final filtration with least one 0.2 micron filter, often more than one. When the drug solution cannot be heat sterilized, multiple filtrations with 0.2 micron filters or with a 0.1 micron filter is common. Particulate matter in drug powders for reconstitution was significantly reduced with the introduction of lyophylization. Prior to lyophylization, investigators had documented that the filterable residue from drugs like cephalothin caused a tissue reaction with venous endothelium, but not cutaneous or subcutaneous tissue. The lyophylization process uses solubilizing agents, charcoal filtration, pH adjustment, and 0.2 micron filtration in combination to yield low particle counts. Marc Stranz Page 5 AVA 18th Annual Conference September 2004 When is solution filtration necessary? Compounding in pharmacies: It is well documented that while large volume parenteral solutions have very low particle counts, additives increase that count significantly. Highly soluble additives like potassium chloride produce a negligible increase in particle counts, while antibiotics added to small volume parenteral solutions produce the highest particle counts. The particle counts have declined significantly in the last 30 years, but are highly influenced by the skill of the compounder. Compounded correctly, the drug solutions made using products from brand name manufacturers fall well within the USP allowable particle counts. Solubilized drugs (using vehicles such as lipids, polyethylene glycol deoxycholate, castor oil, etc) such as amphotericin and diazepam necessarily have higher particle counts. Particles from plastics A Swiss study (Di Paolo 1990) found that small particles (< 10 microns) were present in fluid extracted from tubing, with the drip chamber and the latex connector the primary sources. The authors noted that tubing is much less a source of particles than parenteral solutions. A Norwegian study (Roksvaag 1990) found that PVC plastic releases DEHP and EVA plastic releases vegetable oils as particles. Policy statements (Baxter/Braun/Abbott) indicate that plastic tubing and containers are screened and extruded at 300° F. QA checks include particulate matter in tubing and containers at the USP micron ranges. As technology improves, the allowable particulate matter in injectable drugs declines. The USP has gradually tightened the standards for particles in drug solutions, but the solutions are not particle free. The USP standards apply to all large-volume injections and small-volume injections as well as for drugs in solution and drug solutions after reconstitution. Most brand name manufacturers exceed USP requirements but generic drugs, especially those from foreign countries, may exceed these parameters. As of 2004, the USP allows Air elimination. Laskey et al. Air embolism can occur when there is an open venous structure 5 cm or more above the heart or if air is delivered into the venous system under pressure, as with mishaps with infusion bags. Morbidity and mortality are related to the volume of air, rate of entrainment, the underlying patient status and the patient’s position. In animals, infusion rates of >1.8ml/kg/minute are fatal. In humans, the actual volume tolerated is unknown, but mortality has been reported with 100 to 300ml. The highest incidence of air embolism is with central venous access, with the majority occurring during catheter maintenance: disconnecting the line, fracture of the hub, and a break in the tubing. Marc Stranz Page 6 AVA 18th Annual Conference September 2004 When is solution filtration necessary? The frequency of air embolism is not known, but when it does occur it is generally due to a procedural failure. Filters do not block air passage until they become wet, so air embolism due to failure to prime the tubing is not prevented. A filter would block air passage from primed but empty tubing, but the frequency of occurrence is low enough to question the need for routine prevention. Endotoxin removal. Sterile products should be free of endotoxin, also called pyrogens and lipopolysaccharides, but the USP recognizes that is not possible and sets a maximum endotoxin concentration per product. All microbes produce pyrogen; the most potent pyrogen comes from gram-negative bacteria. Humans react to pyrogen with fever, chills, headache, increased blood pressure and a constellation of other symptoms. Pharmaceutical manufacturers and compounding pharmacies prevent pyrogen contamination through the use of pyrogen-free raw materials and depyrogenated equipment. Additionally, manufacturers and most compounding pharmacies test the final product for pyrogen (LAL tests). If a filter retains gram-negative bacteria, those bacteria can thrive on the upstream side of the filter and release endotoxin, which passes through a filter that cannot retain those endotoxins. The Posidyne® nylon filter material from Pall Medical is capable of retaining pyrogen, blocking its passage through the filter for at least 7 days (96 hours in Pall literature). This feature has value in pharmacy drug compounding where endotoxin prevention is potentially more difficult. It also has value when inline filtration is used for extended periods (96 hours). The Posidyne® material is only available as a small volume disk filter and inline tubing units (ELD & NEO). Phlebitis prevention. The Pro & Con literature review is at the end of the handout. On the surface, the volume of literature says filters reduce phlebitis, but examination shows that investigators were unable to control all the variables that influence phlebitis and many of the studies were done prior to the major improvements in pharmaceutical manufacturing. Many articles are from an era when drug solutions were clearly not to today’s standards. The 2002 publication of the CDC Guidelines for the Prevention of Intravascular CatheterRelated Infections says “In-line filters reduce the incidence of infusion-related phlebitis (79,80)”, but the second reference for this statement (80), an article by Maddox et al from 1983, says “inline filters did not affect the incidence of post-infusion phlebitis or bacterial colonization of IV catheters… their use as a means of reducing post-infusion phlebitis is unwarranted.” The first reference (79), by Rusho and Bair, published in 1979 but using years earlier data, demonstrated that a 0.45 micron filter was only as good as a 5 micron filter in reducing phlebitis, and just slightly better than no filter. Additional complicating factors include the risk factors for phlebitis from the Maki & Ringer trial of 1991. Antibiotics and other drugs were associated with phlebitis in several trials, but most trial did not segregate the drugs infused by their ability to induce phlebitis through pH, osmolarity and other factors. Have organizations that stopped using filters routinely noticed an increase in complications? Anecdotally, no. Providers have not returned to filters after discontinuing them. Marc Stranz Page 7 AVA 18th Annual Conference September 2004 When is solution filtration necessary? When can filter cause problems? Drug binding. Diazepam and digoxin do bind to some filters. Charged biotech proteins may also, but data are limited. Residuals. Filters that have a large priming volume relative to the dose and dose volume can retain clinically significant amounts of drug. Literature found issues with push meds and pediatric dosing. Pediatric gentamicin and small dose chemotherapy were most often indicated. When are filters required? By drug type • Parenteral nutrition • Some IVIG. Siegel J. Intravenous Immune Globulins. Pharmacy Practice News January 2004 www.pharmacypracticenews.com > archives (not functioning now) • Other drugs: ß eFacts Subscription service found in many pharmacies. Search by filtration produces a list of drugs whose monographs mention filtration in preparation/administration. http://www.efactsonline.com/Fac/servlet/MainPage ß Micromedex Subscription service found in many pharmacies. Search filtration and filter for a list of drugs requiring filtration http://www.thomsonhc.com/home/dispatch ß University Texas Medical Branch. http://www.utmb.edu/rxhome/Operations/Filtrations.htm ß Medical University South Carolina. www.musc.edu/pharmacyservices/ ß Johns Hopkins Hospital pharmacy ß www.hopkinspharmacy.org.pharmacists/References/Inline%20filter%20for%20IV%20medicat ions.pdf University Kentucky Medical Center www.mc.uky.edu/pharmacy/dic/criteria/Ivfiltration.pdf ß Many other hospitals are found by searching drugs/filtration on search engines By infusion site – epidural infusions are often inline filtered. By situation – critical care, multiple line entry versus limited entry, areas of know infectious contamination risk. By severity of disease – immunosuppressed patients? Filtration is not substantiated unless there is a pre-existing trend. To extend drug expiration dating under USP Chapter 797. Summary – When is solution filtration necessary? • Filters are necessary for particle removal from certain infusions: parenteral nutrition, other drugs. • Particles will always be present in infusions, but are not clinically significant in large volume solutions. There are more particles in compounded small volume parenterals, but in general particles remain small and within an acceptable number. No clinical complications have been demonstrated in humans. • Pharmaceutical manufacturers provide effective sterilization. Compounding pharmacies generally provide sterile compounds and should improve further with implementation of USP Chapter 797. • Infection is not impacted by filtration except in a situation with abnormally high contamination rates and still may not be the most effective preventative measure. • Phlebitis is minimally impacted by filtration. • Air elimination from administration systems is not often required and filters do not affect the most common causes. Marc Stranz Page 8 AVA 18th Annual Conference September 2004 When is solution filtration necessary? Favors filtration for phlebitis DeLuca et al 1975. Double blind, randomized, prospective 146 pts randomized to • Unfiltered; caused elevated WBC and Sed Rate • filtered (0.45); greatest benefit • solution buffered; no value • solution unbuffered • frequent tubing changes; no value • antibiotic therapy; no value Most benefit from combination of unbuffered solutions, 0.45 filtration and no set changes over 72 hrs. Evans et al AJHP 1976. Double blind, randomized, prospective 5 micron filter 49 pts No filter 49 pts Phlebitis less with filter. Rusho Bair AJHP 1979. Blinded, randomized, prospective. Identical solutions 0.45 micron filter; 50 pts Phlebitis 6% 5 micron filter; 50 pts Phlebitis 22% No filter; 50 pts Phlebitis 27% Filtration (0.45) reduces phlebitis in patient postoperatively Bivins et al Surgery 1979. Double blind, randomized, prospective 266 post surgical patients receiving solutions were randomized to: • 0.2 filter • solution buffering • heparin • hydrocortisone • heparin/hydrocortisone • frequent tubing changes Only filtration and heparin/hydrocortisone reduced phlebitis Allcutt et al Br J Surg 1983. Double blind, randomized, prospective 0.2 filter 101 pts No filter 93 pts Filtration delayed phlebitis in antibiotic patients, but did not extend catheter duration. Falchuk et al NEJM 1985. Double blind, randomized, prospective 0.2 filter; 277 pts Phlebitis Day 1 7%; Day 2 10%; Day 3 11% No filter; 264 pts Phlebitis Day 1 14%; Day 2 31%; Day 3 27% Stated phlebitis caused by microparticulate contamination. Roberts et al Ann Pharmacother 1994. Prospective, randomized 0.2 filter versus heparin/hydrocortisone in prolonged antibiotic therapy in CF Filtration equal to heparin/hydrocortisone. Chee Tan J Infus Nurs 2002. Retrospective and prospective 0.2 filter Phlebitis 1997 5%; 2000 8% No filter Phlebitis 1997 31%; 2000 35% Stated filtration reduces phlebitis Marc Stranz Page 9 AVA 18th Annual Conference September 2004 When is solution filtration necessary? Does not favor filtration for phlebitis Chamberland et al AJHP 1977. Prospective. 0.45 filter; 49 pts Phlebitis 86% No filter; 40 pts Phlebitis 75% Filtration (0.45) of no value in postsurgical phlebitis. Use of cephalothin and KCl common. Maddox et al Clin Pharm 1983. Double blind, randomized, prospective. 0.2 filter; 95 pts Phlebitis 40% No filter; 100 pts Phlebitis 39% Filtration did not reduce phlebitis. Variables such as age, flow rate, catheter, KCl did not influence outcome. Richards et al J Clin Pharm Ther 1995. Historical controls, CF, extended therapy 0.2 filter; 12 pts. Each patient own control 7 patients had no benefit; 4 patients had 50% increase in time to phlebitis Marc Stranz Page 10 AVA 18th Annual Conference September 2004 When is solution filtration necessary? References: • • • • • • • • • • • • • • • • • • • • • • • • Akers M. 25 years of change in the parenteral technology field 1976 – 2001. Pharmaceut Technol 2001; 78-79. Akers MJ, Larrimore DS, Guazzo DM. Parenteral Quality Control: Sterility, Pyrogen, Particulate, and Package Integrity Testing. 3rd Edition. Marcel Dekker, New York. 2003 Alcutt DA, Lort D, McCollum CN. Final inline filtration for intravenous infusions: a prospective hospital study. Br J Surg 1983; 70: 111-113. Bach A, Bottiger BW. Microfilters within the scope of infusion therapy. Zentralblatt Chir 1994; 119:268-275. Backhouse CM Ball PR, Booth S et al. Particulate contaminants of intravenous medications and infusions. J Pharm Pharmacol 1987; 39: 241-245. Ball PA. Intravenous inline filters: filtering the evidence. Curr Opin Clin Nutr Metab Care 2003; 6: 319-325. Bivins BA, Rapp RP, DeLuca PP, et al. Final inline filtration: a means of decreasing the incidence of infusion phlebitis. Surgery 1979; 85:388-394. Borchert SJ, Aldrich DS, Fox LE et al. Particulate matter in parenteral products. J Parenter Sci Technol 1986; 40: 212-241. Bottiger BW, Bach A. Use of microfilters within the scope of infusion therapy. Infusionther Transfusion Med 1994; 21:42-51. Chamberland ME, Lyons RW, Brock SM. Effect of inline filtration of intravenous infusions on the incidence of thrombophlebitis. AJHP 1977; 34:1068-1070. Chee S, Tan W. Reducing infusion phlebitis in Singapore hospitals using extended life endline filters. J Infus Nurs 2002; 25:95-104. DeLuca PP, Rapp RP, Bivins B et al. Filtration and infusion phlebitis: a double blind prospective clinical study. AJHP 1975; 32:1001-1007. DeMuynck C, DeVroe C, Remon JP, Colardyn F. Binding of drugs to end-line filters. J Clin Pharm Ther 1988; 13:335-340. Di Paolo ER, Hirschi B, Pannatier A. Quantitative determination of particulate contamination in intravenous administration sets. Pharm Weekbl Sci 1990; 12: 190-195. Dorris GG, Bivins BA, Rapp RP, et al. Inflammatory potential of foreign particulates in parenteral drugs. Anesth Analg 1977; 56: 422-428. Ennis CE, Merritt RJ, Neff DN. In vitro study of in line filtration of medications commonly administered to pediatric patients. JPEN 1983; 7:156-158. Evans WE, Barker LF, Simone JV. Double blind evaluation of 5 micron final filtration to reduce postinfusion phlebitis. AJHP 1976; 33:1160-1163. Falchuk KH, Peterson L, McNeil BJ. Microparticulate-induced phlebitis. Its prevention by inline filtration. NEJM 1985; 312:78-82. Fennessy PA, Antonis P, Anderson J. What is the efficacy of inline filters in reducing microbiological contamination of intravenous fluids. Centre for Clinical Effectiveness, Monash Medical Centre Australia www.monash.edu.au/healthsciences/cce/evidence/pdf/c/old008.pdf Groell R, Schaffler GJ, Rienmueller R. The peripheral intravenous cannula: a cuase of venous air embolism. Am J Med Sci 1997; 314: 300-302. Groves MJ Particulate contamination in parenterals: current issues. Boll Chim Farm 1991; 130: 347-354. Gupta PK, Porembski E, Williams NA. Approaches to reducing subvisible particle counts in lyophilized parenteral formulations. J Pharm Sci Technol 1994; 48: 30-37. Hecker JF. Failure of intravenous infusions from extravasations and phlebitis. Aneasth Intensive Care 1989; 17:433-439. Hirakawa M, Makino K, Nakashima K et al. Evaluation of the inline filters for the intravenous infusion of amphotericin B fluid. J Clin Pharm Ther 1999; 24:387-392. Marc Stranz Page 11 AVA 18th Annual Conference September 2004 When is solution filtration necessary? • • • • • • • • • • • • • • • • • • • • Holmes CJ, Kundsin RB, Ausman RK, Walter CW. Potential hazards associated with microbial contamination of in-line filters during intravenous therapy J Clin Microbiol 1980; 12: 725-731. Johns T. Intravenous filters; panacea or placebo? J Clin Nurs 1996; 5:3-6. Laskey AL, Dyer C, Tobias JD. Venous air embolism during home infusion therapy. Pediatrics 2002; 109(1) e15 Lehr HA, Brunner J, Rangoonwala R, Kirkpatrick CJ. Particulate matter contamination of intravenous antibiotics aggregates loss of functional capillary density in postischemic striated muscle. Am J Resp Crit Care Med 2002; 165: 514-520. Longe RL. Particulate contamination in selected parenteral drugs. Can Anaesth Soc J 1980; 27: 62-64. Maddox RR, John JF, Brown LL, Smith CE. Effect of inline filtration on postinfusion phlebitis. Clin Pharm 1983; 2: 58-61. Maki DG, Ringer M. Risk factors for infusion-related phlebitis with small peripheral venous catheters. Ann Intern Med 1991; 114: 845-854. Newall F, Ranson K, Robertson J. Use of inline filters in pediatric intravenous therapy. J Intraven Nurs 1998; 21:166-170 Rapp RP, Bivins BA. Final in-line filtration: removal of contaminants from IV fluids and drugs. Hosp Formul 1983; 18:1124-1128. Richards C, Millar-Jones L, Alfaham M. Assessment of inline filters to prolong the life of intravenous cannulae in cystic fibrosis patients. J Clin Pharm Ther 1995; 20:165-166. Roberts GW, Holmes MD, Staugas RE et al. Peripheral intravenous line survival and phlebitis prevention in patients receiving intravenous antibiotics: heparin/hydrocortisone versus in-line filters. Ann Pharmacother 1994; 28: 11-16. Roksvaag PO, RydstromP, Smistad G, Waaler T. The mechanism of particulate contamination in soft polyvinyl chloride infusion fluid bags. Acta Pharma Nord 1990; 2: 319326. Rusho WJ, Bair JN. Effects of filtration on complications of postoperative intravenous therapy. AJHP 1979; 36:1355-1356. Satoh Y, Isohata E, Iwata S, et al. Effects of inline filtration on delivery of gentamicin at various flow rates. Keio J Med 1992; 41:16-20. Schroeder HG, DeLuca PP. Particulate matter assessment of a clinical investigation on filtration and infusion phlebitis. AJHP 1976; 33: 543-546. Scott J, Bond C, Kennedy E, Winfield A. Investigation into the effectiveness of filters for use by intravenous drug abusers. The Scientist 1998; 12: 18-23. Stinavage P. Filtration issues in pharmaceutical manufacturing: bacterial and viral retention. USP 27 Chapter 788. Particulate matter in injections. United State Pharmacopeial Convention 2004. Van Lingen RA, Baerts W, Marquering ACM, Ruijs GJHM. The use of in-line intravenous filters in sick newborn infants. Acta Paediatr 2004; 93: 658-662. Walpot H, Franke RP, Burchard WG et al. Filtering effectiveness of conventional 15 micron filtrs and newly developed 5 micron filters. Infusionstherapie 1989; 16:77-80. Marc Stranz Page 12 AVA 18th Annual Conference September 2004