Volume 9 Issue 1
Winter 2015
Aspiration Pneumonia
See page 4
Local Regional Anesthesia in the ER
See page 8
Case Study: Lameness in a Greyhound
See page 12
Message from the Chief Executive Officer
Thank You
In the past couple months we released our 2014 Annual Report announcing a 7% increase in
total patients from the previous year to 13,369 and were recognized with several awards and
commendations. We are proud and know that we simply couldn't have accomplished this without
you. We were recognized as one of the Top 10 Most Admired Companies in nonprofit category by
the Portland Business Journal for the eighth year, recognized as one of the Top Animal Non Profits
by the Portland Business Journal, awarded the NW Wild Heritage Award in recognition of our
support for the relationship between wildlife and humans by the Wild Artist Guild, and ranked the
#1 Emergency Veterinary Hospital by Spot Magazine. As an extension of your practice, we share
each of these honors with our referring partners.
CEO Ron Morgan
The reality of our industry consolidating with increasing competition continues to materialize.
We understand you have more options now than ever before for your emergency needs and we are
thankful each time you refer your patients to DoveLewis. Your referrals allow us to maintain a fully staffed, state-of-the-art facility
available to the community 24 hours per day, every single day of the year.
As our annual report illustrated, we put $1,396,735 over the year into our community programs. Our community programs make
us a truly unique organization and include one of the region’s largest volunteer-based animal blood banks, a nationally recognized
pet loss support program, animal-assisted therapy made possible through a partnership with Guide Dogs for the Blind, stabilizing
care for lost, stray, wild and abused animals, education and outreach for veterinary professionals as well as the animal loving
community, and financial assistance for qualifying low-income families facing pet emergencies. It is only with your referral support
and generous donors that we are able to continue and expand these programs.
We are grateful the veterinary community keeps supporting DoveLewis with
referrals and recommendations, because without your continued support our
community may not have access to our many programs. We rely on referring
veterinarians and community supporters to help us keep our doors open. Thank you
for trusting us with your patients’ care during animal emergencies. Your confidence
and support allows us to continue providing our many unique programs to our
community.
Message from the Chief Medical Officer
Think Positive
Lee Herold, DVM,
DACVECC
Chief Medical Officer
Daily affirmations were not invented by the Saturday Night Live character Stuart Smalley; however, this
character played by comedian Al Franken popularized - though undoubtedly also mocked - the idea of
affirmations. Even if you may not know the origin, I’m sure that most people can recite Stuart’s mantra
“I’m good enough, I’m smart enough, and doggone it, people like me.” Did this affirmation play a role in
jettisoning this comedian to becoming a two term United States senator? Maybe, though we probably
shouldn’t discount his Harvard education. But in all seriousness I do believe the daily intentions that we
set, whether that is by way of a positive affirmation or a general positive attitude can greatly direct the
course of our day and our life.
I have used affirmation as a tool to set a positive intention for myself at times when I felt very bleak about an obstacle. My first
experience with affirmation was in the summer of 2006. I was daunted by the task of preparing for my critical care specialty board
exams. A trusted advisor, my husband, suggested I use an affirmation. I was skeptical, but what harm could it do? I wrote and
recited an affirmation daily, along with a lot of studying for 3 months in preparation for boards. The great news is that I passed
boards, but when I look back a more important lesson learned that summer was how to create a positive attitude.
Though I will never be an outwardly joyful person, I recognize, admire, and enjoy working with people who are positive and upbeat.
Fortunately veterinary medicine draws an abundance of truly joyful people so I have the pleasure to work with many of them. Not
being a naturally optimistic person, remaining positive is something that I work on daily - it is a goal that is worth the effort it takes.
If you are finding yourself despairing at times, I would suggest emulating the positive people around you, but also maybe letting go
of the mocking stereotype of Stuart Smalley and try reciting a daily positive affirmation.
2 VetWrap Volume 9 Issue 1
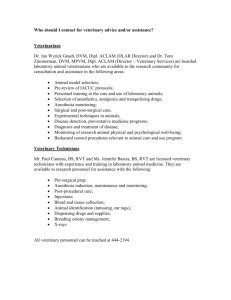
DVM Outreach Corner
One of the best parts of my outreach duties is making
personal visits to veterinary clinics. Sometimes I
make unannounced, drop-in visits with tasty treats
and a referral binder because I know you all have
busy schedules. Even when I arrive unannounced I
always find there is a team member who is gracious
enough to give me a tour of the clinic and go through
Ladan Mohammadthe highlights of our information binder. The services
Zadeh, DVM,
I receive the most positive feedback on are the
DACVECC
overnight monitoring package and the shuttle service
– both the routine transport and the critical transport. If you have not utilized
either of these services yet, you may be wondering “are they commonly used?”
Well I have answers for you!
In 2014 we had a total of 279 patients that stayed with DoveLewis under the
overnight monitoring package. 37 of those patients stayed multiple nights
after being with their primary care veterinarian during the day. The overnight
monitoring package was designed to offer continued overnight care for your
stable patients for the affordable price of $220. Common examples of cases
that stay here under the overnight monitoring package include stable renal
failure patients undergoing fluid diuresis, uncomplicated post operative cases,
uncomplicated urinary obstruction cases that have an indwelling urinary
catheter in place, and patients with gastroenteritis. Disqualifications include
the need for EKG monitoring, oxygen therapy, imaging, frequent blood sugar
or blood pressure monitoring, fluid boluses or vasopressor support. The cost
does include replacement IV catheter if needed, fluid therapy, routine injectable
and oral medications, 12 hours of hospitalization and up to two blood panels
performed on our Nova machine which provides electrolytes, BUN, creatinine,
blood glucose, ionized calcium, lactate and PCV/TS. As with other referrals, you
would call to speak to a staff doctor prior to transfer. You might be surprised
which cases can fit into the overnight monitoring package.
The van transport is another service we offer that has increased in popularity
over the last few years. In 2014 we performed 96 routine shuttle transports and
49 critical transports. A routine shuttle is one where a technician assistant only
drives the van to transport a stable patient. One way shuttle cost is $35, round
trip is $55. A great way to take advantage of this service is in combination with
the overnight monitoring. For $275, we can provide round trip shuttle transport
and overnight monitoring. Critical transport utilizes the same van, but a doctor
accompanies the patients. This enables us to provide fluids, monitoring, oxygen
therapy, and even blood transfusions during the transport. The cost of the
critical transport is $225. With both the routine shuttle and critical transport, we
do require the owners contact information and permission prior to performing
the transport. The van services the greater Portland area. You can find the
service area map on our website.
As you can see, the overnight monitoring and shuttle service are well utilized.
But we always have room for more requests. So if you think you have a stable
patient that needs affordable overnight care, or an unstable patient that requires
oxygen during transport, please call us to see our services will fit your needs.
“The overnight monitoring package provided by Dove Lewis has been a
life-saver in more ways than one, for our doctors, clients, and patients
of St. Johns Veterinary Clinic. It removes the worry over maintaining the
recently unblocked cat, the post-op foreign body dog, or the pancreatitis
patient that needs more than 8 hours of IV fluid therapy. What a relief
to know that our patients will be monitored and cared for in such good
fashion, and return to us with updated progress reports. We value this
service greatly, with the peace of mind it has offered over the years.
Thank you, Dove!”
-Mary Blankevoort, DVM
Board of Directors
CEO
Ron Morgan
DoveLewis Emergency Animal Hospital
President
Katherine Wilson, DVM
Forest Heights Veterinary Clinic
Immediate Past President
Adrianne Fairbanks, DVM
Mountain View Veterinary Hospital
Vice President
Governance & Nominating Chair
Carol Opfel, DVM
PDX Visiting Vet LLC
Secretary
Andrew Franklin
member at large
Finance Chair
Sang Ahn, CPA
McDonald Jacobs
PVMA Representative
Lori Gibson, DVM
Compassionate Care Home Pet
Euthanasia Service, P.C.
Medical Advisory Chair
Elizabeth Altermatt Herman, DVM
Murrayhill Veterinary Hospital
Human Resources Chair
Scott Bontempo
Welsh, Carson, Anderson & Stowe
Board Personnel
Courtney Anders, DVM
Pearl Animal Hospital
Julie Poduch
Marketing Consultant
Michael Remsing
Dignified Pet Services
Steven Skinner, DVM, DACVIM
Oregon Vet Specialty Hospital
Kelly Zusman
U.S. Department of Justice
Thomas Mackowiak, DVM
Heartfelt Veterinary Hospital
DoveLewis Emergency Animal
Hospital is recognized as a charitable
organization under Internal Revenue
Code, Section 501(c)(3). All donations
are tax deductible as allowable by law. Federal
Tax ID No. 93–0621534.
St. Johns Veterinary Clinic, Portland OR
Volume 9 Issue 1 VetWrap 3
CRITICALIST
Aspiration Pneumonia
Erika Loftin, DVM, DACVECC
Aspiration pneumonia is,
unfortunately, a frequent
occurrence in veterinary patients,
and is recognized far more
commonly in dogs than in cats.
The initial injury (aspiration
pneumonitis) actually occurs
due to chemical irritation from
stomach acid with a high risk for
subsequent bacterial infection
due to altered microenvironment and potentially
aspiration of contaminated liquid and/or pathogenic bacteria in
the oropharynx. While minor aspiration events probably occur
relatively frequently, normal defense mechanisms (coughing,
mucociliary clearance, and the immune system) protect against
the development of clinical pneumonia. When these systems
are impaired or overwhelmed infection occurs. In some cases,
acute respiratory distress syndrome (ARDS) can develop, with a
worsening prognosis and often a need for ventilator support.
should also be evaluated for the cause of the aspiration event,
including megaesophagus, gastrointestinal obstruction or
pancreatitis. Figure 1 shows the typical radiographic findings
of right cranial lung lobe alveolar infiltrate in a patient with
aspiration pneumonia, and Figure 2 shows the same patient 24
hours later. Due to progression of his disease despite aggressive
initial therapy and suspected ARDS, this patient required
mechanical ventilation and 13 days of ICU hospitalization prior
to discharge.
A complete blood count (CBC) and chemistry panel are
recommended in patients with aspiration pneumonia, but
findings are often non-specific. CBC may reveal neutrophilia
with a left shift or less commonly neutropenia. A chemistry
panel is primarily useful for identifying concurrent or underlying
diseases. Additional diagnostic testing should be recommended
as indicated based on the specific patient.
Tracheal wash with cytology and culture is useful to confirm
the diagnosis and identify the organism(s) responsible, which
allows for targeted antibiotic therapy. Samples can be obtained
via bronchoscopy (with bronchoalveolar lavage) or more
commonly via endotracheal or trans-tracheal wash. The use of
a deep oral swab (DOS) as a surrogate for tracheal wash (TW)
to obtain bacterial cultures was recently investigated (Sumner
2011), and the authors concluded that in adult dogs with
aspiration pneumonia, there was partial agreement between
tracheal wash culture and deep oral swab culture, and that DOS
may represent a reasonable alternative sample in patients that
are too unstable for TW. Antibiotic administration can decrease
Factors shown to predispose to aspiration pneumonia in
veterinary patients include gastrointestinal disease, esophageal
disease, neurologic disease, upper airway disease, and recent
anesthesia. Male large-breed dogs appear to be predisposed. A
recent retrospective multicenter study showed a post-anesthetic
aspiration pneumonia incidence of ~0.17%, with significant
association with patients that had a regurgitation
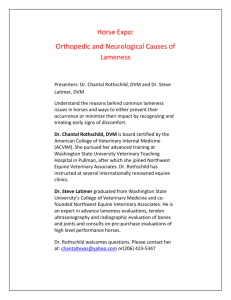
Figure 1a, 1b - Typical ventrodorsal and left lateral radiographic findings of right
episode, and those that received hydromorphone at
cranial lung lobe alveolar infiltrate in a patient with aspiration pneumonia.
induction (Ovbey 2014). The aspiration event is often
unwitnessed and initial clinical signs can be delayed
for hours to days. Physical examination findings
can include fever, weakness, lethargy, increased
respiratory rate and effort, coughing, abnormal lung
sounds on auscultation (including crackles and/or
dull regions), and nasal discharge. Interestingly, in
a recent retrospective study, only about 50% of the
patients presented with signs of aspiration pneumonia
and 26% actually had normal lung sounds on thoracic
auscultation (Tart 2010), so it is important to keep
aspiration pneumonia in mind for patients even without
specific signs of this disease.
The diagnosis of aspiration pneumonia is usually
made on the basis of radiographic findings, most
commonly a dependent alveolar lung pattern. Other
differentials to consider should include infectious
bronchopneumonia, hemorrhage, neoplasia,
atelectasis, and lung lobe torsion. The right middle
lung lobe is the most frequently affected, although
the cranial lung lobes are also commonly implicated.
When aspiration is suspected, it may be helpful to
obtain a left lateral radiograph as this will increase
the ability to detect right-sided infiltrates. It is not
uncommon for radiographic changes to correlate poorly
with the stage and/or severity of disease. Radiographs
4 VetWrap Volume 9 Issue 1
Figure 2a, 2b – Recheck ventrodorsal and right lateral radiographs taken 24 hours
later document significant progression in pulmonary pathology, which necessitated mechanical ventilation. Note the changes are far less obvious on the right
lateral film than on the left lateral film shown in Figure 1.
the yield of bacterial culture, and culture samples should ideally
be obtained prior to initiation of antibiotic therapy.
A variety of bacteria can be found in respiratory cultures, with
Escherichia coli and Pasturella typically the most common.
Other pathogenic respiratory bacteria include Staphylococcus,
Mycoplasma, Klebsiella, Pseudomonas, Enterococcus, and
Streptococcus species. Polymicrobial cultures are relatively
common, likely due to aspiration of oropharyngeal and/or
enteric bacteria. A recent study (Epstein 2010) demonstrated
that patients with more severe respiratory signs (respiratory
failure requiring ventilator support) had a higher incidence of
antimicrobial resistance on bacterial cultures, suggesting that
these patients should probably be started on more aggressive
antibiotic regimens pending culture results. In this patient
population, 98% of the bacteria cultured were susceptible to
amikacin and 91% were susceptible to imipenem, as compared
to only 35% susceptible to amoxicillin-clavulonate and 48%
susceptible to enrofloxacin. Another recent study (Proulx 2014)
showed that 26% of patients with bacterial pneumonia that had
a respiratory culture performed had at least 1 bacterial isolate
that was resistant to the empirically selected antimicrobials.
The incidence was even higher (57%) in patients that had
received antibiotics over the preceding 4 weeks. This suggests
that airway cultures should be routinely recommended, and that
care should be taken to select different antibiotics in patients
that have recently undergone treatment.
pneumonia. It has been suggested that movement of colloid
molecules across the damaged alveolar endothelium may lead
to increased interstitial fluid accumulation. However, it is also
possible that the more critically ill patients were more likely to
receive colloids and that there is not a causative link.
Respiratory physiotherapy 2-4 times daily is helpful to
mobilize and eliminate respiratory secretions in patients with
pneumonia. In veterinary patients, this is most commonly
provided as nebulization (instillation of very small water droplets
capable of reaching the lower airways) and coupage (rhythmic
clapping against the sides of the thorax to stimulate coughing).
While studies are equivocal on the benefits of this practice, it is
commonly recommended in veterinary patients. No benefit has
been shown to nebulization of antibiotics, and this can cause
airway irritation and inconsistent antibiotic delivery due to poor
lung penetration.
Empiric antibiotic therapy should be started pending bacterial
culture results, or when airway sampling is not feasible due
to patient stability or financial constraints. Cytology can be
evaluated quickly in hospital, and can help guide selection.
In stable patients with mild clinical signs, monotherapy
with amoxicillin-clavulanic acid may be adequate. Patients
that are more clinically compromised should be treated with
combination therapy (such as a potentiated penicillin along
with either a fluoroquinolone or an aminoglycoside). Alternative
antibiotic strategies may be necessary in patients that are
not showing a good clinical response, patients that have been
on recent antibacterial therapy, or based on known hospital
bacterial populations and resistance patterns.
The need for oxygen supplementation is determined by
both subjective and objective means. Pulse oximetry (SpO2)
measurements assess the percentage of hemoglobin saturation
with oxygen and can be obtained non-invasively, but can be
difficult to measure in non-compliant patients, those with
pigmented mucous membranes, and those with arrhythmias.
In general, patients with SpO2 <95% will benefit from
supplementation oxygen. Arterial blood gas measurement is
a more accurate assessment of oxygenation, but is also more
invasive and requires specialized equipment. Subjective
evaluation of the respiratory status of the patient can also be
useful, and includes monitoring respiratory rate and effort,
as well as observing appetite and ability to rest. Oxygen
supplementation can be provided in a variety of ways, including
an oxygen cage, oxygen mask, nasal prongs or tubes, an
oxygen “hood” constructed from a covered E-collar, and via
endotracheal tube. Oxygen supplementation is typically at
~40% initially, but can be provided at higher concentrations
depending on the method and patient requirements. Oxygen
supplementation at high concentrations (60% or above) can
cause toxicity due to free radical accumulation, and use should
ideally be limited to 24 hours or less. Patients with severe
respiratory impairment may require mechanical ventilation.
Some patients with aspiration pneumonia do not require
hospitalization, and can be managed with oral antibiotics.
Radiographs should be monitored serially to help determine
response to therapy, and duration of antibiotic treatment should
ideally continue for 2 weeks past clinical and radiographic
resolution of disease. Many patients are sick enough that they
require hospitalization for supportive care. Fluid therapy should
be used as needed to maintain hydration and perfusion, and
febrile patients in particular can have increased insensible
losses and easily become dehydrated. However, excessive
administration of intravenous fluids should be avoided as
pulmonary capillaries may have increased permeability due to
the acute inflammatory response; this can lead to interstitial
edema and worsening hypoxemia. This risk is higher in
patients with cardiac disease. Patients with sepsis may require
vasopressor support to help maintain perfusion. A recent
retrospective study (Tart 2010) identified colloid therapy as
a negative prognostic indicator in patients with aspiration
Bronchodilators such as terbutaline or theophylline are
sometimes used in patients with aspiration pneumonia, and
can theoretically be useful in ameliorating the bronchospasm
that can accompany chemical injury to the airways. However,
bronchodilators can potentially impede the cough reflex
and also worsen hypoxemia by opening airways that lead to
diseased alveoli and increasing dead-space ventilation. Recent
human ARDS trials have not shown any improvement with
bronchodilator therapy. While glucocorticoids could theoretically
be beneficial to reduce pulmonary inflammation, they are also
immunosuppressive which can be deleterious in the face of
bacterial infection. Glucocorticoids are likely only indicated in
the presence of concurrent inflammatory lung disease, with
upper airway swelling, and with hypoadrenocorticism or other
concurrent steroid-responsive conditions. Cough suppressants
are generally contraindicated in aspiration pneumonia as
they can impair clearance of respiratory secretions. In some
cases, oral or intravenous N-acetylcysteine
Continued on page 6
Volume 9 Issue 1 VetWrap 5
Continued from page 5
(mucomyst) may be useful as a mucolytic, but this
medication should not be nebulized due to airway irritation
and bronchospasm. Furosemide should not be used as it can
result in drying and trapping of infectious debris in the lower
airways.
Preventive measures are very important, especially in
patients that have known risk factors for aspiration. Rapid
induction and endotracheal intubation is critical for patients
undergoing general anesthesia, particularly those that
have not been appropriately fasted. Some references have
suggested that increasing gastric pH via administration of
H2 blockers or proton pump inhibitors can decrease risk of
airway acid injury in the event of aspiration, while others
have shown increased risk of bacterial pulmonary infection
in human patients that are on these medications. Use of
a prokinetic such as metoclopramide has been shown to
decrease risk of aspiration in humans when given 12 hours
prior as well as on the day of anesthesia. If regurgitation
occurs in an anesthetized patient, care should be taken to
swab or suction the oral cavity, and it may be indicated to
remove the endotracheal tube with the cuff still partially
inflated. These patients should also be monitored very closely
for signs of pneumonia. Patients receiving enteral nutritional
support are also considered at increased risk of aspiration
pneumonia, as well as those with decreased gag reflex,
diseases causing dysphagia, and decreased mentation.
Patients with laryngeal paralysis (with or without arytenoid
lateralization surgery) have an increased risk of aspiration
pneumonia.
With rapid recognition and treatment, the prognosis
for aspiration pneumonia is relatively good. A recent
retrospective study (Tart 2010) showed a survival rate
of approximately 82% in patients treated for aspiration
pneumonia. A statistically significant association was
documented between number of lung lobes affected
radiographically, and survival. No prognostic difference was
found among patients based on signalment, culture results or
specific treatment protocol.
Suggested Reading
RADLAB
Radiology Case Study
Alan Lipman, DVM, DACVR
An 8 year old Springer Spaniel
presented with a 48 hour history
of lethargy and vomiting. Physical
examination determined the patient
had a distended, tense abdomen and
was mildly dehydrated. Abdominal
radiographs were performed and a
lateral view of the abdomen is included
for evaluation. Describe significant
radiographic findings and list possible
differential diagnoses. Please determine what additional
diagnostic imaging may be useful. Continued on page 11
Radiology Services
OUTPATIENT SERVICES & FEES
Radiographs (two views and interpretation; no exam). .......................$235.00
Radiograph Interpretation (per case).................................................$37.00
Interpretation of digital or plain films by Dr. Lipman
Abdominal Ultrasound.......................................................................$330.00
Second Cavity Ultrasound (same patient)........................................$170.00
Dear JD. Bacterial pneumonia in dogs and cats. Vet Clin North Am Small Anim Pract.
2014;44(1):143-159.
Echo / Single Organ Ultrasound.......................................................$265.00
Epstein SE, Mellema MS, Hopper K. Airway microbial culture and susceptibility
patterns in dogs and cats with respiratory disease of varying severity. J Vet Emerg Crit
Care 2010;20(6):587-594.
Ultrasound–guided Fluid Drainage*................................................$240.00
Kogan DA, Johnson LR, Sturges BK, Jandrey KE, and Pollard RE. Etiology and clinical
outcome in dogs with aspiration pneumonia: 88 cases (2004-2006). J Am Vet Med
Assoc 2008;233:1748-1755.
Ultrasound–guided FNA*..................................................................$100.00
Ultrasound–guided Fluid Aspirate*................................................. $50.00
Ultrasound–guided Cystocentesis*................................................. $40.00
*All Ultrasound-guided procedure pricing does not include sedation if necessary
CT of Chest, Abdomen, Nasal or Brain............................................$ 879.00
Ovbey DH, Wilson DV, Bednarski RM, Hauptman JG, Stanley BJ, Radlinsky MG,
Larenza MP, Pypendop BH, Rezende ML. Prevalence and risk factors for canine postanesthetic aspiration pneumonia (1999-2009): a multicenter study. Vet Anaesth Analg
2014;41(2):127-136.
(includes contrast, anesthesia & exam fee)
Proulx A, Hume DZ, Drobatz KJ, Reineke EL. In vitro bacterial isolate susceptibility to
empirically selected antimicrobials in 111 dogs with bacterial pneumonia. J Vet Emerg
Crit Care 2014;24(2):194-200.
CT Ortho additional study (same visit). ............................................$ 625.00
CT Lung Met Check (includes anesthesia and exam). .......................$379.00
Sumner CM, Rozanski EA, Sharp CR, Shaw SP. The use of deep oral swabs as a
surrogate for transoral tracheal wash to obtain bacterial cultures in dogs with
pneumonia. J Vet Emerg Crit Care 2011;21(5):515-520.
Dr. Alan Lipman, DVM, DACVR Phone: 971.255.5964
Diagnostic Imaging Coordinator:
Katie Olsen, CVT
Phone: 971.255.5964
Tart KM, Babski DM, Lee JA. Potential risks, prognostic indicators, and diagnostic
and treatment modalities affecting survival in dogs with presumptive aspiration
pneumonia: 125 cases (2005-2008). J Vet Emerg Crit Care 2010;20(3):319-329.
6 VetWrap Volume 9 Issue 1
CT additional study (same visit).........................................................$325.00
CT Orthopedic (includes contrast, anesthesia & exam fee)................$914.00
Phone consultations are welcomed!
DoveLewis Education
& Outreach Program
Third Thursday Rounds Continuing Education
We invite all doctors and support staff in the
community to attend our free Third Thursday
Rounds. Rounds cover all topics in veterinary
medicine.
For more information on topics and registration
visit dovelewis.org/third-thursday-rounds.
Focused on business.
Passionate about
community.
Pacific Continental Bank
proudly supports DoveLewis
Emergency Animal Hospital.
503-350-1205
therightbank.com
Experience you can
trust to care for your
patients overnight.
TECHNICIAN LECTURES BROUGHT
TO YOU IN PARTNERSHIP WITH
s
“Thank you for alway
zed,
emphasizing organi
ning,
consistent staff trai
development and
skills acquisition.”
d.,
-Liz Hughston, ME
VTS (SAIM, ECC)
RV T, CV T,
Dove overnight monitoring includes exam,
ER or ICU monitoring as determined by
a DoveLewis veterinarian with fluids,
pain management—antibiotics, or oral
medications as prescribed by the referring
veterinarian (if indicated) and patient
status lab work (if necessary).
The medical team at Frontier Veterinary Hospital is so
thankful and appreciative of Dove’s overnight monitoring
package and their shuttle service. We have utilized
both services many times. It is such a relief to be able
to send over our stable post-operative/milder medical
patients and know that we don’t have to worry about
them at home overnight – essentially the overnight
monitoring package is an extension of our hospital’s
continued care... Thank you, Dove!
-Lisa Yung, DVM
main 503.228.7281 • backline 971.255.5990 • fax 503.228.0464
Volume 9 Issue 1 VetWrap 7
DVM
Block Party: Local Regional Anesthesia in the ER
Josh Cruz, DVM
If pain control was a party, the opioids,
NSAIDs, and neuromodulating therapies
would be the most glamorous and
gregarious attendees. But sometimes a
very effective member of the party is the
often forgot wallflower, the local regional
block. Local regional anesthesia, or
local blocks, is an essential component
to managing pain in a wide variety
of our patients in the emergency and
critical care setting. Of course, the primary goal of these blocks
is to provide relief from current painful stimuli, or to prevent
the sensation of pain caused by our own intervention. A local
block’s use, however, extends beyond this simple classification.
Allowing for the minimization of other analgesics and sedatives,
ease of administration with minimal risk, and overall cost
effectiveness, make local anesthesia one of the more interesting
and useful characters at this party.
Understanding basic nerve anatomy and physiology is essential
for understanding how local anesthesia works. Rapid changes
to an electrical gradient across nerve membranes allows for
transmission of various signals (pain, sensation, motor) through
nerve fibers. These action potentials of electrical energy are
typically managed by sodium gated channels. Local blocks
utilize these channels to inhibit propagation of nerve signals,
hence, anesthesia. At greater doses of blockade, not only pain
sensation but motor function may be inhibited. While the basic
function is similar among local anesthetics, there are many
local anesthetics that vary in duration and strength of action,
positive/negative side effects, and motor and sensory blockade.
Lidocaine and bupivacaine are the most notable and widely
used sodium channel blockers in the ER/ICU setting, and will
be the focus of this article.
Many local regional anesthesia dose variations and recipes
involving lidocaine/bupivacaine have been described in
8 VetWrap Volume 9 Issue 1
veterinary medicine. Combining both shorter acting lidocaine
with longer acting bupivacaine is often used. Mixing local
blocks with sodium bicarbonate, in an attempt to minimize
patient discomfort and increase onset of anesthesia is still
controversial. Mixing with a vasoconstrictor (epinephrine)
has also been used to prolong duration of analgesia, but may
alter regional pH limiting clinical benefit. Opioids, alpha-2
agonists, and NMDA antagonists (ketamine) have also been
used in conjunction with sodium channel blockade to achieve
regional anesthesia. Ultimately it is difficult to determine the
effectiveness and benefit of adjunctive mixtures to the primary
sodium channel blockage anesthetics. Often in the emergency
setting, keeping it simple is often the best. Patient selection and
reason for anesthesia should help guide your choice but there is
nothing wrong with one drug selection for local blocks.
Various complications exist with performing local blocks.
These complications are usually rare. With appropriate dose,
technique, and patient selection, complications become
insignificant. Systemic absorption and subsequent side
effects to the cardiovascular and central nervous systems
are definitely possible, but using appropriate drug volumes
and understanding species difference should help prevent
this complication. Injection at any site that may already be
compromised from severe trauma or infection should not be
performed. Moving the injection site further up the neurologic
pathway, or increasing the circumference of the block, may be
reasonable options assuming safety of injection and dosage
is still appropriate. Hemorrhage is always a concern, but
understanding landmarks, knowing rough location of major
vessels, and aspirating back prior to injection will help prevent
this complication. Also having a good understanding of patient
systemic health is essential (eg. coagulation parameters,
drug sensitivities, and concurrent medications). Reconsider
performing local anesthesia on patients with coagulopathies
and thrombocytopathies. Nerve trauma is of course possible,
but less likely in the majority of blocks performed in the ER.
Local Block Techniques
The following are four of my favorite, and most commonly used local blocks. This is meant to be a quick guideline, for a more in
depth anatomy and description, other resources should be consulted. The techniques described below are by no means meant to
be all inclusive. Dental, topical, intraarticular, testicular, ring, epidural, and brachial plexus (all-time favorite) blocks are all useful,
but usually used preemptively prior to more advanced surgery or painful stimuli, and not as practical in the ER setting. As with
all blocks, calculating total doses prior to injection, site preparation (clip/scrub), aseptic technique (sterile gloves, needles), and
aspirating prior to injection is essential.
Incisional Line Block
Sacrococcygeal Block
Retrobulbar Block
The most commonly used
block in the ER. One of the
biggest perceived failures of
this block is its failure to work
adequately. Ensuring accurate
dosage and allowing time to
pass (>5 minutes) is essential.
Most traumatic wounds
requiring local regional
anesthesia typically also
require thorough hair clipping,
cleaning, and flushing. Usually
by performing a local block
prior to final wound cleaning,
but well before induced
injury, you are able to give
enough time to allow complete
anesthesia to occur. Also
remember to block those areas
not near the wound site but
near areas of future pain (i.e.
drain placement).
While typically associated with
male feline urinary catheter
placement, any procedure in
which caudal pudendal and tail
anesthesia is required could make
use of this block. This block is only
recently described and further
investigation into its effectiveness
is warranted. However, it has
been used effectively, and for
some cases, allowing urinary
catheterization without use of
general anesthesia. Because
of this, assuming the patient
already has systemic analgesia
and sedation, a sacrococcygeal
block is attempted on the
majority of my patients in which
a urinary catheter needs to be
placed. Depending on block’s
effectiveness, you can either move
on towards catheterization or
general anesthesia if needed.
In the ER setting, the
retrobulbar block is typically
performed prior to enucleation
post traumatic proptosis.
Patient selection is essential in
deciding whether to perform
this block, and controversy still
exists regarding the preferred
technique and overall
effectiveness. Traumatized
anatomy, increased vagal
tone, and unseen bacterial
contamination may lead to
increased procedural risks.
Also due to its location, the
risk for injury and systemic/
CNS absorption is higher.
Regardless, this block can still
be used to good effect and
should be considered.
Intrapleural/
Intercostal Block
An easy, often
underutilized option
for analgesia in critical
patients suffering from
pancreatitis, painful
pleural space disease, or
diaphragmatic disease is
the intrapleural/intercostal
block. Many patients
already on systemic
multimodal analgesia that
still exhibit refractory pain
may see dramatic benefit
from these blocks. For
most of the pain expected
in these patients,
initial administration of
lidocaine, followed by
bupivacaine should be
performed.
Hopefully after reading this, if you are new to local blocks you will be more comfortable performing these various techniques. If
you are already well versed in local blocks, let this be a gentle reminder. I like to think that if it is painful, and I can get close to or
around the nerves responsible for the pain with a needle, local regional anesthesia should be considered. Remember, sometimes
even the wallflower has something to add. After all, everyone is invited to a block party.
Technique
Dosage
Description
Comments
Incisional Line
Lidocaine 2%
2-4 mg/kg
Bupivacaine 0.5%:
1-2 mg/kg
25 or 22 gauge needle.
Dilute with saline as needed
for volume, or 0.3mls of
sodium bicarbonate per 10
mls.
Sacrococcygeal
Lidocaine 2%: 0.25-0.5 mls
25 gauge needle inserted
30-45 degrees into most
mobile joint caudal to
sacrum.
Sacrococcygeal joint, or
first 2 coccygeal joints are
acceptable. Feel for “pop”.
Retrobulbar
Lidocaine 2%: 1-2mls
22 gauge 1.5 inch needle.
Bent at middle 20 degrees,
inserted at midline or just
lateral to midline under
inferior eyelid.
Aim slightly dorsally and
nasally after initial insertion
about 1-2 cm. Feel for “pop”.
Intrapleural
Lidocaine 2%: 1.5mls/kg,
followed by bupivacaine
0.5%: 1.5mls/kg
Injected at middle of 9th rib
space. 25 to 22 gauge needle
in small patients. 22 gauge
1.5 inch needle for larger
patients.
Block can be instilled into
chest tubes, but will likely
need saline as flush down
tube.
Volume 9 Issue 1 VetWrap 9
COMMUNITY
PROGRAM
When to Say ‘Goodbye’
A discussion with Ron Morgan & Enid Traisman, M.S.W., CT
With so many great community programs at DoveLewis, it was hard to choose just
one to write about. But it was my recent experience saying goodbye to our pug,
Lucy, which led me to our Pet Loss Support Program. I asked our Director of the
program, Enid Traisman, certified grief counselor, to help co-write this article.
Lucy Morgan
Ron: I work in a building where end of life for animals is, unfortunately,
sometimes a reality. We see pet parents struggle with the decision to
euthanize their beloved companion animals. Whether their pet has been
battling a disease for years or suffered a recent injury, it is never easy. But
when is it time to say ‘goodbye’? Medically, we can discuss all the statistics,
survival rates, treatment options and pain the pet is experiencing. But the
decision is ultimately in the pet parents’ hands, and what it really comes
down to is the human-animal bond and quality of life. Enid, many of us have
experienced having to make this decision, sometimes more than once - what is
it that makes it so difficult for us to decide when to say ‘goodbye’?
Enid: It is unfortunate that our companion animal life spans are not as long as ours, thus many of us who share that special bond
are faced with very difficult end-of-life issues. Judging whether or not to euthanize a beloved pet can be among life’s most difficult
decisions. When faced with this, people often feel that they have been put unfairly in a God-like position, having to decide between
life and death for someone they love and for whom they are responsible. As compassionate guardians we are also very concerned
about whether our animal is suffering or has lost quality of life.
Ron: With more than a decade as the CEO of an emergency veterinary hospital, I still struggle just as others do when facing my
pet’s life coming to a close. Our dearest Lucy, whom many of you saw in the last issue of VetWrap and on Twitter if you are following
me, had been living with diabetes for almost 5 years. The reality is DoveLewis was able to give us so much more time with her than
we imagined after learning of her diabetes and we are grateful for that. But as a family, we started talking about euthanasia after
many hospital visits and even more so after diabetes took her vision. The dialogue that each person will have with themselves and
their family will likely center around quality of life, as did my own. What guidance can you provide for pet parents having to make
this decision?
Enid: Many people ask me how they will know if it is time to choose euthanasia for their beloved companion animal. The term
“euthanasia” means “the good death,” a death without pain or suffering. To choose this for a pet is both an honor and a burden. I tell
them to first consult with their veterinary professional about prognosis and then to trust their hearts and intuition which is based
on the bond they share and the unspoken communication they have with their pet. I tell them to talk about it with themselves, their
family and friends. And as difficult as it is, it’s important for them to express their feelings, observations and philosophies about
quality of life. Continuing to do this until they come to a decision or identify a “signal’ from their pet letting them know it is time
can be helpful in making this tough decision.
It is important to note that quality of life is interpreted uniquely by each individual. For some folks, any life is life. For others, if their
pet can no longer enjoy his or her normal activities, quality of life has been lost. There is no right or wrong answer; everyone has a
unique perspective.
Ron: When we came to the hard decision in December to let Lucy go run somewhere that she could see again and feel no pain for
the first time in a long time, we knew it was the right thing to do, the selfless thing to do. Just as my family did, there are so many
emotions that people will go through. Tell us about the emotional response and what people can do after you have made this tough
decision to say goodbye.
Enid: In pet loss groups, we often discuss the ‘5 stages of grief’. Specifically, when euthanasia was involved, we often discuss
feelings of guilt, which I describe as anger turned inward. This is a normal part of the grieving process. We do this because in
loving and grieving our pets, we wish we could have done more, or wish we did not have to choose euthanasia. Working toward
forgiving ourselves is essential. Releasing the guilt doesn’t mean that we don’t/didn’t care for our pet; instead it will allow us to
freely tap into all the wonderful memories of a lifetime shared.
But please know that whenever your clients make this tough decision, we are here for them. The Pet Loss Support Program offers
guidance and healing opportunities to those who have said ‘goodbye’ to their beloved pets.
10 VetWrap Volume 9 Issue 1
Reward Theory
{ Education rewards everyone it touches }
CE should reward not only you, but also your patients, clients and practice. So the IDEXX Learning Center provides a
comprehensive curriculum. And learning options that’ll have every member of your team wagging their tail: the veterinarian
who wants to learn from experts face-to-face, techs who love the convenience of online courses, and the practice manager
who’s eager to have protocols communicated consistently across the practice—and with clients.
To turn theory into reality, visit idexxlearningcenter.com.
Knowledge you can put into practice™
IDEXX Learning Center
© 2011 IDEXX Laboratories, Inc. All rights reserved. • 9304-00 • All ®/TM marks are owned by IDEXX Laboratories, Inc. or its affiliates in the United States and/or other countries. The IDEXX Privacy Policy is available at idexx.com.
RADLAB
Radiology Diagnosis Continued from page 6
There is increased soft tissue opacity within the dorsal to mid
abdomen which is displacing the colon ventrally adjacent to
the urinary bladder. There is a loss of serosal margin detail
within the retroperitoneal space with a lack of visualization
of the kidneys and normal retroperitoneal fat. The increased
opacity within this portion of the abdomen has a wispy,
streaking appearance. These findings are consistent with
retroperitoneal effusion. No gross evidence of peritoneal
effusion is identified. Differential diagnoses for retroperitoneal
effusion include retroperitoneal hemorrhage secondary to a
bleeding mass, trauma or coagulopathy, urinary tract leakage,
or less likely a purulent exudate. Abdominal ultrasound may
be useful to evaluate for a neoplastic process involving the
retroperitoneal space (most likely involving kidneys or adrenal
glands). Definitive diagnosis of urinary tract rupture would
require excretory urography or surgical exploratory. Abdominal
ultrasound was performed which demonstrated retroperitoneal
effusion, large bilateral adrenal masses with invasion of the right
adrenal mass into the caudal vena cava (image included) as well
as suspected metastatic nodules involving the cortices of both
kidneys. Differential diagnoses for the adrenal tumors included
adenocarcinoma, pheochromocytoma and hemangiosarcoma
given the large size of the masses and aggressive vascular
invasion of the caudal vena cava.
Volume 9 Issue 1 VetWrap 11
SURGICAL
Lameness in a
Greyhound
Coby Richter, DVM, DACVS
Zoe, a 6 year old female spayed
greyhound presented on
emergency following a witnessed
accident earlier that day. While
exercising at a park, the dog
tripped going down concrete
stairs resulting in laceration and
abrasions to both rear limbs.
She was otherwise in good
health, current on vaccination
and preventive veterinary care, and had no history of lameness.
Zoe is a retired racing dog with an unknown history of injury or
reason for retirement.
At the initial outpatient visit, Zoe’s laceration and abrasions
(over both left and right metatarsals) were treated with standard
wound care and bandaging. The dog was most sensitive to
palpation of the left rear limb but did not show lameness at
a walk or trot in the hospital. She was discharged on oral
antibiotics and pain medications with a plan for a recheck
evaluation with her primary care DVM.
Two weeks following the initial trauma, the owner noticed
a consistent lameness in the left forelimb. Zoe had been on
exercise restriction since the first tripping incident and the
owner was not aware of any trauma that could have resulted
in front limb lameness. At the primary care veterinary clinic, a
lameness exam showed a consistent left front lameness but no
soft tissue swelling or joint effusion. The only pain localization
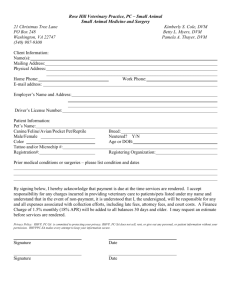
was upon squeezing the nail of the 4th digit. Radiographs were
taken of the forelimb (Figure 1) with the primary significant
finding being an absence of the distal end of P3 of the 4th
digit. Full bloodwork was collected at that time showing mild
elevation in HCT 64%, lipase 759 (138-755), albumin 4.0 (2.7-3.9),
glucose 118 (63-114), phosphorus 2.4 (2.5-6.1), creatinine 1.6 (0.51.5) and BUN of 19 (9-31).
acute-on-chronic injury to the digit was also possible. Infection
was considered less likely with the total lack of soft tissue
involvement, normal white cell count and normothermia. Injury
at the time of the park stair incident is also possible, potentially
obscured by the more obvious and painful soft tissue trauma
to both rear limbs. Options discussed at that time included
toe amputation, survey radiographs of thorax and longbones,
oncology referral and continued medical management. The
owner elected to try nonsteroidal anti-inflammatory medication
and continue monitoring. Zoe was started on carprofen (0.9mg/
kg PO BID) and continued exercise restriction.
A recheck evaluation three weeks later showed a left forelimb
lameness of 2-3/5 in the left forelimb with soft tissue swelling
centered at the distal interphalangeal joint (Figure 2). The
owner reported that lameness improved on carprofen, but never
completely resolved. The dog was doing well otherwise. Biopsy
(incisional or needle) was discussed but was not felt to be likely
to produce a diagnosis with less than an excision procedure
(amputation). Furthermore, amputation was considered likely
to be central to the treatment plan regardless of diagnosis.
The owner elected digit amputation at that time. Zoe was
anesthetized in a routine manner and the 4th digit amputated at
the proximal interphalangeal joint. The entire resected segment
was placed in formalin for submission. Zoe was recovered in a
spoon splint to protect the surgical site. She was managed in a
splint for one week, then a simple foot bandage for an additional
two weeks. At the two week recheck and suture removal, Zoe
showed no lameness in the left forelimb. The foot was bandaged
to protect the delicate skin for a final week.
The initial histopathology of the soft tissues indicated mild
reactive fibroplasia with mild mastocytic and neutrophilic
inflammation. Decalcification and histopathology of the digit
followed revealing an expansile mass that arose from the
nailbed epithelium and was compressing the underlying third
phalanx. The final diagnosis was a nailbed keratoacanthoma;
completely excised.
Zoe was started on tramadol and referred to DoveLewis
for surgical consult. The owner reported that there was no
perceptible change in lameness over the four days on tramadol
(3mg/kg PO TID). Upon presentation, Zoe was grade 3/5 lame
in the left forelimb. There was no palpable or visible soft tissue
swelling, joint effusion or crepitus. Full range of motion was
possible in all joints (including digits) without evidence of pain.
Similar to the referring DVM visit of the previous week, the
only pain localization was when the nail of the 4th digit was
squeezed. All toenails were long but otherwise unremarkable.
The abrasions and laceration from the original trauma 2.5 weeks
earlier had healed well.
Subungual (nailbed) neoplasia is relatively common in the dog,
however keratoacanthoma is one of the more rare diagnoses
in this group. Squamous cell carcinomas represent 30-50%
of subungual tumors, followed by malignant melanoma,
osteosarcoma, soft tissue sarcomas and mast cell tumors.
Subungual SCC is locally invasive and has a low metastatic
potential. Regional lymph node or distant metastasis after
excision to the level of P1 has been reported in 10-30% of cases.
Subungual melanomas develop distant metastasis (lymph
nodes, lungs, other systemic sites) in approximately 30-50% of
cases. Prognosis following complete excision of a subungual
melanoma is fair to guarded. Soft tissue sarcomas of the nailbed
are typically locally aggressive. Approximately 75% of nailbed
tumors result in osteolysis that is appreciable on standard foot
radiographs. Other potential causes for local bone lysis would be
infection, trauma and previous surgery.
The differentials at this point included a)neoplasia, b)trauma
and c)infection. Zoe’s age and breed make osteosarcoma one of
the top cancers to consider. However, with her racing history, an
Keratoacanthoma is a benign proliferation that arises from the
superficial epithelium. When a keratoacanthoma forms beneath
the nail, the tumor’s growth is directed instead at the space
12 VetWrap Volume 9 Issue 1
The experience
you trust for
emergencies,
available for
scheduled critical
procedures too!
Consultation & Referral Scheduling Available 24/7, 365
• P
hone consultations
• C
onsultations
• Same-day surgery referrals
(Please speak to a surgeon or staff DVM prior to patient’s arrival.)
main 503.228.7281 • backline 971.255.5990 • fax 503.228.0464
Figure 1
Figure 2
occupied by the third phalanx. Gradual expansion results in pressure necrosis
and resorption of P3 such as that seen in Figure 1. Treatment for solitary tumors is
excision and prognosis is excellent. In Zoe’s case, the toe involved was a weightbearing digit, thus amputation was expected to have a permanent effect upon her
gait. At 3 months post-surgery, the owner reported that Zoe was sound in most of her
activities, although occasionally she would stumble or take one or two lame steps.
DoveLewis would like to thank the Pearl Animal Hospital and Zoe’s owner for
allowing her case to be used for teaching purposes.
Selected References:
Canine digital tumors: a Veterinary Comparative Oncology Group retrospective study of 64 dogs. Henry CJ et al. JVIM
10:720-724, 2005.
Radiographic changes associated with digital, metacarpal and metatarsal tumors and pododermatitis in the dog. Vet
Radiol Ultrasound. 37:327-335, 1996.
Volume 9 Issue 1 VetWrap 13
TECHNICIAN
End Tidal C02: Worth the Investment?
Megan Brashear,
BS, CVT, VTS (ECC)
If I were
to take
away all of
your fancy
anesthesia
monitoring
equipment
and you
could
save ONE
monitoring parameter, which would you
choose to keep? Between heart rate/
ECG, ETC02, Sp02, blood pressure (noninvasive but you can choose Doppler
unit or oscillometric), and temperature
which would you choose? Thankfully
many of us have the luxury of using all of
these parameters plus our own eyeballs
and fingers to monitor our anesthetized
patients, but if I were down to just one,
I do not want to monitor anesthesia
without capnometry to measure end tidal
C02.
End tidal C02 is the measurement of
carbon dioxide in each exhaled breath.
Before getting into everything we can
gain by monitoring this value, let’s think
about why it is important to monitor.
Carbon dioxide is the gas that drives
respiration. We (and our patients) inhale
because the respiratory center in our
brain detects higher than normal levels
of carbon dioxide in the blood. We inhale
oxygen, and then exhale that carbon
dioxide every minute of every day of our
lives. If carbon dioxide levels get too high,
our respiratory rate will increase so that
we are exhaling more C02. If levels get
too low, our respiratory rate decreases
so that we hang on to more C02. In our
normal patients without lung disease
or metabolic disease, this process
is sufficient to keep their C02 levels
perfectly normal. When we anesthetize
that patient, the drugs we use can
decrease the ventilatory drive in the brain
and relax the intercostal muscles which
can cause changes in ETC02. Changes
that, because they are anesthetized, the
patient cannot correct on their own.
Do we really need to monitor ETC02?
We can see our patient breathing, we
14 VetWrap Volume 9 Issue 1
have the Sp02 giving us good numbers,
why bother? First of all, our trusty pulse
oximeter is only giving us part of the
picture. With some fancy new models,
we can get some impressive perfusion
information from our pulse oximeter,
but it is still only giving us oxygenation
status of our patient. It is measuring
the percentage of hemoglobin that is
saturated with oxygen. This number
tells us that the patient is receiving
enough oxygen. When that patient is
anesthetized and breathing 100% oxygen,
a low patient Sp02 may be masked by the
increase in inhaled oxygen. And the Sp02
monitor has its limitations – ambient
light, probe placement, movement, and
decreased peripheral perfusion can all
alter the reading. By monitoring ETC02
we are able to determine our patient’s
ventilation status. This is the physical
movement of air in and out of the lungs
and upper respiratory system. By using
both ETC02 and Sp02 we are getting
a more complete picture of our patient
under anesthesia.
Depending on who you read and where
you work, the normal range for ETC02
may differ slightly, but I prefer to use
35mmHg-45mmHg as my ideal range for
an anesthetized patient. Not only are we
monitoring ventilation and respiratory
drive with that normal range, we are
also protecting the patient from acid/
base changes. Elevated levels of carbon
dioxide can lead to acidosis which
can bring additional problems to our
anesthetized patient. By monitoring, we
can intervene to keep the ETC02 within
that normal range.
An elevated ETC02 (>45mmHg), or
hypercapnia, signifies that the patient is
hypoventilating. Common causes for this
include: too deep a plane of anesthesia,
an airway obstruction, pneumothorax,
body position of the patient, and disease
process (remember that obesity is a
disease, especially when we place
those patients in dorsal recumbency).
To correct hypercapnia, increase the
patient’s respiratory rate until the ETC02
reaches a normal level, and adjust
anesthesia as needed. Troubleshooting
the patient may be necessary if a
pneumothorax is present or the patient is
not responding as anticipated.
A decreased ETC02 (<35mmHG) or
hypocapnia, signifies that the patient
is hyperventilating. Common causes
for this include: too light a plane of
anesthesia, pain resulting in tachypnea,
panting, pronounced hypothermia,
decreased cardiac output, or excessive
dead space in the anesthetic circuit. To
correct hypocapnia, pain management
or deeper anesthesia may be required
to allow a lower respiratory rate, as well
as monitoring other vital signs (such as
temperature). Further troubleshooting
may be necessary if the patient is not
responding as anticipated.
In addition to exhaled carbon dioxide, a
capnometer will also display the inhaled
C02 with each breath. This number is
ideally zero, but it is acceptable for a
patient to be rebreathing a small amount
of C02, so a value of 1mmHg or 2mmHg
is tolerable. Higher inhaled C02 numbers
can indicate exhaustion of C02 granules
or a malfunction with the anesthetic
machine or circuit. In very small or
debilitated patients, increased inhaled
C02 numbers may signify a need for
mechanical ventilation or switching to a
non-rebreathing circuit.
Many capnometers will also display
each breath as a waveform, called a
capnograph. Interpreting capnography
is outside the scope of this article, but
can give valuable information about
breathing patterns, the presence of an
airway obstruction, an airway leak, and
breathing over a ventilator.
As mentioned, an end tidal C02 monitor
reads the amount of C02 exhaled with
each breath. Whether a mainstream or
side stream machine, you are looking
at the result of not only ventilation, but
also blood flow, cellular metabolism,
and alveolar ventilation. In order for
C02 to make it out of the lungs and into
your capnometer, your patient must be
perfusing cells and transporting C02
back to the lungs to be exhaled. ETC02
is reliant on ventilation and perfusion. It
is also an instantaneous result, giving
you up to the minute results of what is
happening with your patient. We have
discussed the respiratory monitoring, but
ETC02 numbers are also a clue to the patient’s perfusion and
circulation. Decreased cardiac output can lead to decreased
ETC02. The patient continues to ventilate, exhaling C02, and if
perfusion decreases there is less C02 being brought back to the
lungs to be exhaled. A rapid drop in ETC02 is cause for alarm,
as this can signify impending arrest.
Watching ETC02 in relation to other vital signs under
anesthesia will help you as the anesthetist gain a better overall
understanding of your patient. For instance, you gather the
following vitals on a 5 year old MN Doberman who is undergoing
an elective procedure. He has been under anesthesia for 30
minutes when you record the following:
• Heart rate – 52bpm (ECG normal)
• Respiratory rate – 10bpm (on an anesthesia ventilator)
• Mucous membranes – pink, CRT 1-2 seconds
• SP02 – 99%
• Temperature – 97.6°F
• Blood pressure – 112/78 (MAP 84)
• ETC02 – 33mmHg
This is a young, healthy dog, and looking at his vitals you might
be concerned about his bradycardia, but his blood pressure
looks good, his gums are pink, he is doing fine, right? His ETC02
of 33mmHg is pretty close to normal - does his bradycardia
really need to be addressed? Remember that ETC02 is also
a measurement of metabolism and perfusion. The dog is
hypothermic but not severe, the respiratory rate is not increased,
but this patient may be hypoperfused due to his bradycardia.
After treatment for his bradycardia with glycopyrrolate, this
same patient then had the following vital signs:
• Heart rate – 104bpm
• Respiratory rate – 10bpm
• Mucous membranes – pink, CRT 1-2 seconds
• Sp02 – 99%
• Temperature – 97.6°F
• Blood pressure – 119/81 (MAP 89)
• ETC02 – 41mmHg
By increasing the heart rate we were able to see a slight
increase in blood pressure, but the ETC02 came up to normal.
As we improved perfusion, we improved ETC02.
As mentioned previously, watch ETC02 for sudden changes,
especially dropping. A level that is normal and suddenly
decreases can signal impending arrest. As the animal stops
perfusing, they exhale their C02 and blood flow is too poor to
bring any new C02 to the lungs to be exhaled. That patient is
in danger and needs help immediately. Using that same logic,
monitoring ETC02 on a patient undergoing CPR can let you
know when that patient has a return of spontaneous circulation.
ETC02 readings in a patient that has arrested will be low, into
the low teens or maybe even single digits, but as that animal
begins perfusing their cells again the number will begin to
slowly rise.
Even if you are not convinced enough to say that ETC02 is your
one and only monitoring parameter if you are forced to pick only
one, hopefully you are convinced that monitoring ventilation and
perfusion is a good idea, and worth the investment in an end
tidal C02 monitor for your multi-parameter anesthesia monitor.
A Big Heart
USI works with many Northwest
organizations and we understand
the varied and complex issues
you face in growing your business
and protecting your assets.
We specialize in providing:
·
·
·
·
·
Health & Wellness Benefits
Retirement Plan Services
Commercial Insurance
Risk Management
Private Client Wealth Management
Elizabeth Templeton
Vice President
Employee Benefits
503.417.9231
Elizabeth.Templeton@usi.biz
Volume 9 Issue 1 VetWrap 15
Connect with DoveLewis
<<firstname>> <<lastname>>, <<title>>
<<clinicname>>
<<address>>
<<city>>, <<state>> <<zip>>
Volume 9 Issue 1
Winter 2015
Address changed?
Want to switch to email?
Contact James Gabrio
jgabrio@dovelewis.org or 971.255.5937