From www.bloodjournal.org by guest on March 4, 2016. For personal use only.
Plenary paper
Platelets from patients with the Quebec platelet disorder contain and secrete
abnormal amounts of urokinase-type plasminogen activator
Walter H. A. Kahr, Shilun Zheng, Prameet M. Sheth, Menaka Pai, Alison Cowie, Madeleine Bouchard, Thomas J. Podor,
Georges E. Rivard, and Catherine P. M. Hayward
The Quebec platelet disorder (QPD) is an
autosomal dominant platelet disorder associated with delayed bleeding and
␣-granule protein degradation. The degradation of ␣-granule, but not plasma, fibrinogen in patients with the QPD led to
the investigation of their platelets for a
protease defect. Unlike normal platelets,
QPD platelets contained large amounts of
fibrinolytic serine proteases that had
properties of plasminogen activators.
Western blot analysis, zymography, and
immunodepletion experiments indicated
this was because QPD platelets contained large amounts of urokinase-type
plasminogen activator (u-PA) within a secretory compartment. u-PA antigen was
not increased in all QPD plasmas, whereas
it was increased more than 100-fold in QPD
platelets (P < .00009), which contained
increased u-PA messenger RNA. Although
QPD platelets contained 2-fold more plasminogen activator inhibitor 1 (PAI-1)
(P < .0008) and 100-fold greater u-PA–
PAI-1 complexes (P < .0002) than normal
platelets, they contained excess u-PA activity, predominantly in the form of two
chain (tcu-PA), which required additional
PAI-1 for full inhibition. There was associated proteolysis of plasminogen in QPD
platelets, to forms that comigrated with
plasmin. When similar amounts of tcu-PA
were incubated with normal platelet secretory proteins, many ␣-granule proteins
were proteolyzed to forms that resembled
degraded QPD platelet proteins. These
data implicate u-PA in the pathogenesis
of ␣-granule protein degradation in the
QPD. Although patients with the QPD
have normal to increased u-PA levels in
their plasma, without evidence of systemic fibrinogenolysis, their increased
platelet u-PA could contribute to bleeding
by accelerating fibrinolysis within the hemostatic plug. QPD is the only inherited
bleeding disorder in humans known to be
associated with increased u-PA. (Blood.
2001;98:257-265)
© 2001 by The American Society of Hematology
Introduction
Congenital platelet disorders are usually associated with defective
primary hemostasis.1-3 The Quebec platelet disorder (QPD) is an
autosomal dominant platelet disorder that has unusual clinical
features: it is associated with moderate to severe delayed bleeding,
that typically begins 12 to 24 hours after surgery or trauma, and its
hemorrhagic manifestations can be controlled with fibrinolytic
inhibitors but not with platelet transfusions.1,4-6 This disorder was
initially designated as factor V Quebec because of the abnormalities found in platelet factor V of these patients.7 Two families from
Quebec have been identified with this condition, which is now
known to be associated with other platelet abnormalities that
include reduced to low-normal platelet counts, proteolytic degradation of soluble and membrane proteins stored in platelet ␣-granules, an apparent quantitative deficiency of the ␣-granule protein
multimerin, and defective aggregation with epinephrine.1,4-6,8 Although patients with the QPD have elevated levels of fibrinogen
degradation products (FDPs) in their serum (because of platelet
fibrinogen degradation), their plasma contains normal amounts of
FDPs and D-dimers.6 Complex platelet abnormalities in these
patients led us to redesignate their bleeding disorder as the Quebec
platelet disorder.5
The cause of the QPD has been uncertain. Affected patients
of both families share a characteristic pattern of platelet
␣-granule protein degradation that is not evident in unaffected
family members or in patients with other congenital and
acquired platelet disorders1,4-6,9 This degradation affects both
plasma-derived and megakaryocyte-synthesized proteins stored
in QPD ␣-granules, but it spares external membrane, densegranular, and cytosolic platelet proteins.1,4,5 Moreover, some
proteins (eg, fibrinogen, von Willebrand factor, and factor V) are
degraded in QPD platelets but not in QPD plasma.1,4-6,8 The
observation that endogenously synthesized and plasma-derived
␣-granule proteins were degraded in QPD platelets, despite their
normal storage within ␣-granules,5 suggests some proteolysis
occurs late, after megakaryocyte-synthesized and plasmaderived ␣-granule proteins enter the same compartment. This
possibility led us to investigate QPD platelets for the presence of
abnormal protease activity. We report that QPD platelets contain
abnormal fibrinolytic activity, attributable to their stores of large
amounts of urokinase-type plasminogen activator (u-PA). Furthermore, we observed that the consequence of adding similar
amounts of exogenous u-PA to normal platelet proteins was the
From the Departments of Pathology and Molecular Medicine, and Medicine,
McMaster University, Hamilton; the Hamilton Regional Laboratory Medicine
Program, Ontario; and the Department of Hematology/Oncology, Hôpital St
Justine, Montreal, Quebec, Canada.
Foundation of Canada Post-Doctoral Fellowship Award.
Submitted November 6, 2000; accepted March 12, 2001.
The publication costs of this article were defrayed in part by page charge
payment. Therefore, and solely to indicate this fact, this article is hereby
marked ‘‘advertisement’’ in accordance with 18 U.S.C. section 1734.
Supported by grant NA 4379 from the Heart and Stroke Foundation of Ontario
(C.P.M.H.) and a grant from Aventis Behring Canada (G.E.R.). W.H.A.K. is the
recipient of a Medical Research Council of Canada/Heart and Stroke
BLOOD, 15 JULY 2001 䡠 VOLUME 98, NUMBER 2
Reprints: Catherine P. M. Hayward, Department of Pathology and Molecular
Medicine, McMaster University Medical Center, Rm 2N32, 1200 Main St West,
Hamilton, Ontario, Canada L8N 3Z5; e-mail: haywrdc@mcmaster.ca.
© 2001 by The American Society of Hematology
257
From www.bloodjournal.org by guest on March 4, 2016. For personal use only.
258
KAHR et al
proteolysis of ␣-granule proteins to forms resembling the
degraded proteins in QPD platelets.
Patients, materials, and methods
Patients
Blood was collected with informed consent and institutional, ethics board
approval from unrelated healthy controls (n ⫽ 20) and 5 affected patients with
QPD, representing both families with this disorder. Stored samples of washed
platelet lysates, pelleted platelet lysates, and plasmas, collected from patients with
QPD for previous studies,4-6 were included in some analyses.
Materials
The protease inhibitors aprotinin, E-64, AEBSF (4-(2-aminoethyl)-benzenesulfonyl fluoride), and leupeptin were from Boehringer Mannheim Canada (Laval,
QC, Canada). All other protease inhibitors, PGE1, theophylline, ionophore
A23187, adenosine 5⬘ diphosphate (ADP), and amiloride were from SigmaAldrich Canada (Oakville, ON, Canada). Fibrinogen (free of plasminogen and
von Willebrand factor), Glu-plasminogen, plasmin, and bovine thrombin were
from Enzyme Research (South Bend, IN). Polyclonal and monoclonal antibodies
to u-PA were from Monosan (Uden, The Netherlands). Recombinant, active
human plasminogen activator inhibitor 1 (PAI-1) was prepared and isolated as
described.10 Polyclonal antibody against PAI-1 was raised in rabbits as previously
described.11 Polyclonal anti–human plasminogen was from Biogenesis (Kingston, NH). Other antibodies and the procedures used for Western blotting of
fibrinogen, fibronectin, von Willebrand factor, multimerin, factor V, thrombospondin-1, and osteonectin were as previously described.4,5 Purified recombinant single chain u-PA (scu-PA), high–molecular weight two-chain u-PA
(tcu-PA), and low–molecular weight two-chain u-PA (LMW u-PA) were
generously provided by Dr Jack Henkin (Abbott Laboratories, North Chicago,
IL). Recombinant tissue-type plasminogen activator (t-PA) was from Hoffman-La Roche (Mississauga, ON, Canada). Supplies for sodium dodecyl
sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) were from Bio-Rad
(Mississauga, ON, Canada). SeeBlue prestained SDS-PAGE protein standards
were from Helixx Technologies (Scarborough, ON, Canada). Protein A Sepharose beads were from Amersham Pharmacia (Uppsala, Sweden). u-PA and t-PA
enzyme-linked immunosorbent assays (ELISA) were purchased from American
Diagnostica (AD; Greenwich, CT), and u-PA, PAI-1, and u-PA–PAI-1 complex
ELISA were purchased from Oncogene Science (OS; Cambridge, MA). Results
for u-PA ELISA were referred to by abbreviations of the assay manufacturer. 1
KB Plus DNA Ladder was from Gibco BRL (Burlington, ON, Canada).
Sample preparation
Double-centrifuged plasma (from blood collected in 9:1 vol/vol 3.2%
buffered sodium citrate), washed platelet lysates, and platelet releasates
were collected from patients and controls as previously described,4,5 with
the following modifications. Resting platelets were prepared using anticoagulant and wash buffers supplemented with 2 M PGE1 and 1 mM
theophylline (final concentrations). Cell counts confirmed the washed
platelets contained minimal leukocyte contamination. Washed platelets
were solubilized (1 ⫻ 109 platelets/mL final)5 using buffer containing 0.5%
Triton X-100 and multiple protease inhibitors (0.3 M aprotinin, 2.8 M
E-64, 10 mM EDTA, 1 M leupeptin, 5 mM N-ethyl-maleimide, 4 mM
AEBSF, 1 M pepstatin, 100 M 1,10-phenanthrolene monohydrate, and
100 g/mL soybean trypsin inhibitor [STI]). For some studies, platelet
lysates were prepared without the serine protease inhibitors AEBSF,
aprotinin, STI, and leupeptin. Platelet releasates4,5 were prepared from
washed platelets, resuspended in albumin-free Tyrode buffer (pH 7.4 with 2
mM Ca⫹⫹, 1 mM Mg⫹⫹, and 5 mM HEPES; 1 ⫻ 109 platelets/mL) and
activated (20 minutes, 37°C) using 50 M ADP or 2 M calcium ionophore
A23187 (samples centrifuged 2000g for 10 minutes, followed by 14 000g
for 15 minutes before freezing). All samples were frozen and stored at
⫺70°C until analyzed. K562 cells stimulated with 12-O-tetradecanoylphorbol-13-acetate (TPA, 3 nM final; Sigma-Aldrich Canada) were used as
a source of PAI-1 protein and u-PA messenger RNA (mRNA).12
BLOOD, 15 JULY 2001 䡠 VOLUME 98, NUMBER 2
Protein and protease analyses
Zymography was performed using 3% agarose substrate gels (SeaPlaque
agarose; BioWhittaker Molecular Applications, Rockland, MD; in phosphatebuffered saline [PBS], pH 7.4) containing plasminogen-free fibrin or casein
(1% wt/vol; Carnation Instant Skim Milk Powder, Nestle Canada, Toronto,
ON), with or without added plasminogen (5 g/mL final), similar to
methods previously described.13,14 Protease activities were tested by
spotting samples directly onto substrate gels, or after proteins were
separated by nonreduced SDS-PAGE and renatured with 2% Triton X-100
in PBS, pH 7.4, for 1 hour. Casein gels with or without 1 mM amiloride
were used for some determinations. Substrate gels were incubated with
samples (37°C, 18 hours) and were photographed wet. Some samples were
preincubated with protease inhibitors (same final concentrations as lysates;
20 minutes on ice) or recombinant PAI-1 (0-4000 ng/mL final after 1:1
dilution in a releasate pool, prepared from 5 QPD ionophore releasates; 1 hour,
22°C) before testing their proteolytic activity. Others were tested after immunodepletion with rabbit anti–human u-PA or control normal rabbit immunoglobulin G (IgG) bound to protein A Sepharose, similar to methods described.15
Plasma samples were assayed at 1:5 to 1:100 dilutions in the u-PA
ELISA. Platelet lysates were tested at 1:2.5 and larger dilutions. Data for
stored, washed, and pelleted platelet lysates were pooled because they
contained similar amounts of u-PA at the dilutions tested. Data for new and
stored lysates were analyzed separately because the stored samples were
prepared with different protease inhibitors.4,5 All samples were tested
undiluted in the t-PA ELISA, which was modified to include a lower
concentration (2 ng/mL) standard. Some normal samples contained less
u-PA or t-PA than the lowest standard of the AD ELISA when tested at
recommended and lower dilutions. These amounts were reported as “less
than” values when ranges for controls were determined, and they were
rounded up to the nearest measurable value to calculate means and standard
deviations for controls.
Active PAI-1 in platelet ionophore releasate and lysate (without added
serine protease inhibitors) was assessed by measuring u-PA–PAI-1 complex
generation, similar to methods previously described.16 Briefly, pooled
samples of releasate and lysate, prepared from 5 control and 5 QPD donors,
respectively, were incubated (30 minutes, 22°C) with or without added
recombinant tcu-PA (200 ng/mL final in 20 L sample) before measuring
u-PA–PAI-1 complexes by ELISA (values expressed as an average of
duplicate determinations).
For studies of ␣-granule protein degradation in vitro, recombinant tcu-PA
(0-400 ng u-PA/mL) was incubated overnight (37°C) with releasate from control
ionophore-stimulated platelets or with control platelet lysate, prepared without
serine protease inhibitors (multimerin digests only) (0.4% Triton X-100, final; all
reactions stopped with 4 mM AEBSF). Degraded proteins in these digests were
compared to QPD platelet proteins by Western blotting after separation on
SDS-PAGE or SDS-multimer gels.4-6 To determine whether u-PA formed
high–molecular weight complexes when incubated with secreted platelet proteins, 10 ng recombinant u-PA was incubated with 10 to 60 L control ionophore
releasate for 1 to 18 hours.
Analyses of platelet mRNA
Total RNA was extracted from platelets and from K562 cells, as previously
described.17 Complementary DNA (cDNA) synthesis was carried out on 1
g total RNA (20 L final volume) using oligo dT as a primer and
Thermoscript (Life Technologies, Burlington, ON, Canada) reverse transcriptase (RT), as recommended by the manufacturer. Polymerase chain reaction
(PCR) was performed on 2 L cDNA reaction in a final volume of 50 L
using Platinum Taq DNA polymerase (Life Technologies). Primers (synthesized by the Central Facility, McMaster University), expected products
sizes, and cycle sequences for u-PA and -actin reverse transcription–-PCR
were u-PA forward, 5⬘-GGAATGGTCACTTTTACCG-3⬘, u-PA reverse,
5⬘-CTGCCCTGAAGTCGTTAG-3⬘, expected product 1.55 kb, 94°C at 30
seconds, 50°C at 30 seconds, 72°C at 2 minutes for 30 cycles; -actin
forward, 5⬘-CCTCGCCTTTGCCGATCC-3⬘, -actin reverse, 5⬘-GGATCTTCATGAGGTAGTCAGTC-3⬘, expected product 620 bp, 94°C at 30
seconds, 55°C at 30 seconds, 72°C at 1 minute for 25 cycles. Products were
analyzed on 1% agarose gels and visualized with ethidium bromide.
From www.bloodjournal.org by guest on March 4, 2016. For personal use only.
BLOOD, 15 JULY 2001 䡠 VOLUME 98, NUMBER 2
u-PA ABNORMALITIES IN QUEBEC PLATELET DISORDER
259
Results
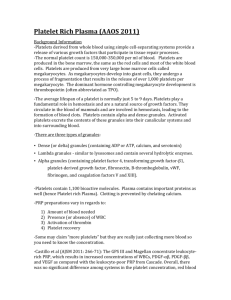
Because platelet fibrinogen was degraded in patients with the QPD,
their platelet releasates and lysates were screened for proteolytic
activity using fibrin substrate gels (Figure 1). Fibrinolytic activity
was evident in all QPD platelet releasates tested, but it was not
detected in the same amounts of control releasates (Figure 1A; data
representative of 5 patients and 12 controls). Fibrinolytic activity in
QPD platelet releasates was inhibited by the serine protease
inhibitor AEBSF (Figure 1A), but it was not blocked by EDTA,
leupeptin, the cysteine protease inhibitor E64, the aspartic protease
inhibitor pepstatin, or the metalloproteinase inhibitor phenanthrolene (not shown). Similar fibrinolytic serine protease activity was
present in lysates of QPD resting platelets, whereas it was
undetectable in the same volume of control sample (Figure 1A).
Fibrinolytic activity released by QPD platelets was not blocked in
1:2 mixtures with normal platelet releasate or lysate (Figure 1B),
suggesting the defect was not due to an inhibitor deficiency.
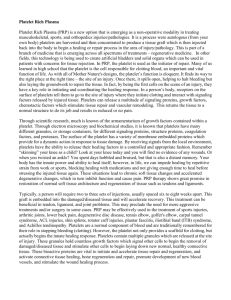
Zymograms indicated there were secretable 50-kd (major band)
and 100-kd (minor band) (Mr nonreduced) fibrinolytic enzymes in
QPD platelets that were not detectable in similar amounts of
normal platelets (Figure 2A-B shows data representative of 5
patients and 12 controls). The activities of these fibrinolytic
enzymes were destroyed by reduction (not shown). Comparisons of
their activities on fibrin substrate gels, with and without added
plasminogen (Figure 2B), indicated the 50- and 100-kd QPD
platelet proteases had properties of plasminogen activators. QPD
Figure 2. Fibrin gel zymograms of proteases in QPD platelets. Samples of QPD
(Q1 and Q2 indicate patients from families 1 and 2, respectively) and control (C)
platelet lysates (lys; A, 12.5 L; B, 2 L) and ADP releasates (ADP rel; A, 50 L; B, 2
L) were analyzed on fibrin substrate gels after 9% (A) or 5% to 15% (B) nonreduced
SDS-PAGE. (A) Analyses using gels without added plasminogen indicated QPD
platelets contained 50-kd (major band) and 100-kd (minor component) secretable,
fibrinolytic proteases (arrows) that were not evident in the same amount of control
samples. (B) Comparative analyses, using substrate gels with (⫹) or without (⫺)
added plasminogen, indicated the 100- and 50-kd QPD platelet proteases had
properties of plasminogen activators. A 33-kd plasminogen activator was also
detected in QPD (but not in control) platelets and releasates (Mr based on 5%-15%
nonreduced SDS-PAGE).
Figure 1. Fibrinolytic proteases in QPD platelets. Platelet lysates (lys; 3 L) and
releasates (rel; 3 L) from patients with QPD (Q) and control subjects (C) were
spotted onto fibrin substrate gels. (A) There was abnormal fibrinolytic activity in QPD
platelet lysates and releasates that was blocked by the serine protease inhibitor
AEBSF. The secretagogue ionophore A23187 (iono) released more of this activity
from QPD platelets than ADP. (B) The fibrinolytic enzymes released by QPD platelets
were not inhibited in 1:2 mixtures with normal platelet lysates or releasates (tested
ratios of patient ionophore releasate–control samples are shown). Protein rings,
without evidence of fibrinolysis, were seen in the tests of control lysates.
platelets also contained and secreted a 33-kd plasminogen activator
that was not detected in the normal samples (Figure 2B).
ELISA and Western blots were used to determine whether the
plasminogen activators in QPD platelets were either t-PA or u-PA.
Although QPD and control plasmas contained similar amounts of
t-PA, neither QPD nor control platelets contained detectable t-PA
(Table 1). Both the OS and AD u-PA ELISA indicated there was
more than 100-fold more u-PA in QPD platelets than in normal
platelets (Table 1). Furthermore, comparisons of platelet u-PA
levels in unaffected family members and family members with the
QPD indicated that only the affected patients had increased platelet
u-PA levels (Table 1; data for stored platelet samples). The OS u-PA
ELISA detected approximately 4-fold more u-PA in QPD platelets
than the AD u-PA ELISA (Table 1), suggesting these assays
differed in their ability to detect some forms of u-PA. The amounts
of u-PA in normal plasma, measured by both OS and AD u-PA
ELISA (Table 1), were similar to previously reported values.18-21
Each ELISA indicated patients with the QPD had larger increases
in u-PA in their platelets than their plasmas because many patients
had normal plasma u-PA levels (Table 1). u-PA ELISA confirmed
From www.bloodjournal.org by guest on March 4, 2016. For personal use only.
260
BLOOD, 15 JULY 2001 䡠 VOLUME 98, NUMBER 2
KAHR et al
Table 1. Tissue-type plasminogen activator, urokinase-type plasminogen activator, plasminogen activator inhibitor 1, and u-PA–PAI-1 complexes in patients and
controls measured by enzyme-linked immunosorbent assays
ng/mL plasma or ng/109 platelets
Protein
t-PA
t-PA
u-PA, AD
u-PA, OS
u-PA, AD
u-PA, AD
u-PA, OS
PAI-1
u-PA–PAI-1 complexes
n
Mean ⫾ SD
Q
8
6.3 ⫾ 2.7
3.7-11.2
C
8
6.1 ⫾ 2.0
4.3-9.8
Q
5
All values ⬍ 2
All values ⬍ 2
C
20
All values ⬍ 2
All values ⬍ 2
Q
12
2.3 ⫾ 1.2
0.8-4.6
C
20
0.7 ⫾ 0.3
⬍ 0.5-1.9‡
Q
12
7.0 ⫾ 6.7
1.9-22.6
C
20
1.2 ⫾ 0.6
0.6-2.7
Q
5
123 ⫾ 16
106-143
C
20
0.4 ⫾ 0.2
⬍ 0.25-0.75†
Q
9
76 ⫾ 28
C*
5
All values ⬍ 5
All values ⬍ 5
Q
5
505 ⫾ 70
409-603
C
20
0.8 ⫾ 0.2
0.4-1.3
Q
5
954 ⫾ 162
816-1161
C
20
407 ⫾ 96
286-660
Sample
Plasma
Platelets
Plasma
Plasma
Platelets
Stored platelets
Platelets
Platelets
Platelets
Range
45-122
Q
5
95 ⫾ 14
82-115
C
20
0.9 ⫾ 0.2
0.6-1.3
P
.87
—
⬍ .0009
⬍ .02
⬍ .00008
⬍ .00006
⬍ .00009
⬍ .0008
⬍ .0002
Data for patients and controls were compared using two-tailed, Student t tests. Results for AD and OD u-PA ELISA are shown separately.
t-PA indicates tissue-type plasminogen activator; u-PA, urokinase-type plasminogen activator; PAI-1, plasminogen activator inhibitor 1; ELISA, enzyme-linked
immunosorbent assays; AD, American Diagnostica; OS, Oncogene Science; Q, patients; C, controls.
*Control subjects who were unaffected relatives.
†Tested at 1:2.5 dilutions.
‡Tested at 1:5 dilutions.
Two of 20 control platelet lysates and 5 of 20 control plasmas contained less u-PA than the lowest standard of the AD ELISA. Stored platelet lysates were tested at 1:50 and
larger dilutions in the AD u-PA ELISA only because sample volumes were limited.
QPD platelets released significant quantities of u-PA with secretagogue stimulation because their ADP releasates contained approximately 9% of their platelet u-PA, and their ionophore releasates
contained approximately 48% of their platelet u-PA (averaged data,
AD ELISA; n ⫽ 3 patients evaluated).
Western blots (probed with monoclonal and polyclonal u-PA
antibodies) confirmed that QPD platelets and platelet releasates
contained abnormally large amounts of u-PA (Figure 3A shows
data representative of 5 patients). Western blots of stored platelet
lysates, from additional affected (n ⫽ 9) and unaffected (n ⫽ 5)
members of both QPD families, confirmed this abnormality was
present only in affected patients (not shown).
Western blots were used to determine whether the u-PA in QPD
platelets comigrated, nonreduced and reduced, with purified scuPA, tcu-PA, or LMW u-PA (Figure 3). There was considerable
heterogeneity in the forms of u-PA found in QPD platelet lysates,
and their releasates contained identical forms (Figure 3). On nonreduced gels (Figure 3A; Figure 3B, left panel), the most abundant
form of u-PA in QPD platelets comigrated with scu-PA and tcu-PA,
whereas only a small proportion comigrated with LMW u-PA
(Figure 3B). After reduction (Figure 3B, right panel), the most
abundant form of u-PA in QPD platelets had the mobility of tcu-PA,
indicating most u-PA in QPD platelets had been activated. Some of
the less abundant forms of u-PA in QPD platelets were proteolyzed
and did not comigrate with scu-PA, tcu-PA, or LMW u-PA (Figure
3A-B and longer exposures, not shown). A small proportion of their
total u-PA was larger than scu-PA and tcu-PA and resembled
high–molecular weight complexes generated by incubating exogenous scu-PA (Figure 3A, right panel) or tcu-PA (not shown) with
normal platelet releasate proteins.
Zymograms indicated none of the QPD platelet plasminogen
activators comigrated with t-PA or plasmin, and they confirmed the
50- and 33-kd plasminogen activators in QPD platelets comigrated
with tcu-PA and LMW u-PA, respectively (Figure 4A). The
activities of the 100-, 50-, and 33-kd QPD platelet plasminogen
activators were blocked by 1 mM amiloride, which inhibited
tcu-PA but not t-PA activity, as previously reported22 (Figure 4B).
All the plasminogen activators in QPD releasates were neutralized
when recombinant PAI-1 was added to final concentrations of 3000
ng/mL or more (Figure 4C), which was more than the concentration
of PAI-1 in normal and QPD platelet lysates (Table 1). Furthermore, antibodies to u-PA selectively removed all detectable plasminogen activators (Figure 4D) and fibrinolytic proteases (not shown)
from QPD releasates. These observations indicated that the fibrinolytic, plasminogen-activating proteases detected in QPD platelets
were different forms of the enzyme u-PA.
RT-PCR analyses were performed to determine whether the
u-PA abnormalities in the QPD platelets were associated with
increased u-PA mRNA levels in platelets. Although platelets from
patients and controls contained similar amounts of -actin mRNA,
only QPD platelets contained detectable u-PA mRNA (Figure 5).
Unregulated u-PA activity in QPD platelets was further investigated
by measuring platelet PAI-1 antigen and u-PA–PAI-1 complexes using
ELISA. QPD platelets contained approximately 2-fold more PAI-1
antigen and more than 100-fold more u-PA–PAI-1 complexes than
normal platelets (Table 1). Western blots confirmed some of the PAI-1 in
QPD platelets had formed complexes with u-PA, though the proportions
of complexed PAI-1 varied slightly between patients (Figure 6A; Pt 3
indicates the patient with the highest concentrations of platelet u-PA–
PAI-1 complexes by ELISA). Increased u-PA–PAI-1 complexes were
also detected in QPD platelet releasates using ELISA (Figure 6B), but
they were difficult to detect by Western blotting (Figure 6A and analyses
of larger sample volumes, not shown). The high–molecular weight
PAI-1 complexes stored in QPD platelets expressed epitopes recognized
by u-PA antibodies (Figure 6A, lane *), and they comigrated with PAI-1
complexes generated in vitro by adding tcu-PA to normal platelet
releasate (Figure 6A, right panel). All the QPD platelets tested contained
proteolyzed forms of PAI-1 (Figure 6A, arrow) that were not evident in
From www.bloodjournal.org by guest on March 4, 2016. For personal use only.
BLOOD, 15 JULY 2001 䡠 VOLUME 98, NUMBER 2
u-PA ABNORMALITIES IN QUEBEC PLATELET DISORDER
261
plasminogen was proteolyzed (Figure 7), and there was a form that
comigrated with plasmin on reduced (Figure 7) and nonreduced
(not shown) gels. When normal platelet releasate was incubated
with exogenous tcu-PA, there was loss of detectable intact plasminogen; however, the extent of plasminogen proteolysis was not as
complete as in QPD platelets and the tcu-PA digests of purified
plasminogen (Figure 7).
Next, we investigated whether exogenous tcu-PA (in concentrations similar to the increased u-PA in QPD platelets) could trigger
the proteolysis of other stored platelet proteins to forms that
comigrated with degraded proteins in QPD platelets (Figures 8, 9,
10). Adding tcu-PA to normal platelet releasate resulted in the
Figure 3. Western blots of u-PA in platelets. u-PA in platelet lysates (L; 5 L) and
ionophore releasates (R; 5 L) from patients with QPD (Q) and healthy control
subjects (C) was visualized with monoclonal or polyclonal antisera after 10%
SDS-PAGE. (A) Nonreduced analyses indicated QPD platelet lysates and releasates
contained abnormally large amounts of u-PA. The predominant form of u-PA in QPD
platelets comigrated, nonreduced, with recombinant scu-PA (scuPA, 10 ng), though
larger and smaller forms were also detected. When control platelet releasate was
incubated (lanes *) with recombinant scu-PA (lane CR ⫹ scuPA*), high–molecular
weight u-PA complexes were generated that resembled large forms of u-PA in QPD
releasates (arrow indicates the most abundant large form). (B) QPD platelet
releasates and lysates (R and L, 5 L nonreduced, 20 L reduced) contained forms
of u-PA with the characteristic nonreduced/reduced mobility of purified tcu-PA (tcuPA;
4.4 ng nonreduced, 17.6 ng reduced) and LMW u-PA (LMWuPA; 3.2 ng nonreduced,
12.8 ng reduced). Arrows indicate the A chain (A*) of reduced tcu-PA, the B chain (B*)
common to reduced tcu-PA and LMW u-PA, and the nonreduced form of LMW u-PA
(LMW). A reduced protein with the mobility of the A chain of tcu-PA was seen in
prolonged exposures of the QR and QL lanes (not shown).
normal platelets, but only traces of similar proteolyzed forms were
detected in control releasates incubated with tcu-PA (Figure 6A and
longer exposures, not shown).
Assays of active PAI-1 indicated that although pooled QPD
platelet lysates and releasates contained abnormally large amounts
of u-PA–PAI-1 complexes before exogenous u-PA was added, they
were unable to generate additional complexes with exogenous
u-PA (Figure 6B). Furthermore, the amounts of u-PA–PAI-1
complexes generated when u-PA was added to pooled normal
releasates and lysates were similar to the amounts contained in
pooled QPD releasates and lysates (Figure 6B). These data
indicated the active forms of PAI-1 had been depleted in QPD
platelets, likely because they had formed complexes with u-PA
in vivo.
Western blots were used to determine whether the changes in
u-PA in the QPD were associated with plasminogen proteolysis.
QPD plasmas contained forms and amounts of plasminogen that
were indistinguishable from normal controls (not shown). Although the plasminogen in normal, washed platelets comigrated
with purified Glu-plasminogen, in QPD platelets much of the
Figure 4. Plasminogen activators in QPD platelets. Plasminogen activators were
analyzed on casein substrate gels containing plasminogen. (A, D) Samples tested
after 10% nonreduced SDS-PAGE. (B, C) Samples spotted directly onto substrate
gels. (A) QPD releasate (QR, 6 L; QR*, 10 L) contained plasminogen activators
that comigrated with tcu-PA (tcuPA, 8.8 ng) and LMW u-PA (LMWuPA, 3.2 ng), but not
with purified plasmin (10 ng) or t-PA (tPA, 1 IU). (B) Unlike t-PA (0.5 IU), tcu-PA (5 ng)
and the plasminogen activators in 1 L QR and QL (QPD lysate) were inhibited on gels with
added (⫹) 1 mM amiloride. (C) Large amounts of recombinant PAI-1 (final concentrations
shown) were required to fully neutralize the plasminogen activators in pooled QR. (D)
Zymograms indicated that the 100-, 50-, and 33-kd proteases in QR (5 L/lane) were
removed by rabbit antibodies to human u-PA (depl), but not by normal rabbit IgG
(sham). The 33-kd protease in lanes sham and QR was evident on the original gel.
From www.bloodjournal.org by guest on March 4, 2016. For personal use only.
262
KAHR et al
Figure 5. Platelet u-PA and -actin mRNA, analyzed by RT-PCR. u-PA and -actin
transcripts were amplified separately before running the products in lanes of the gel.
Lanes compare transcripts amplified from platelets of 2 controls (C) and 3 patients
with the QPD (Q), with transcripts from TPA-stimulated K562 cells. QPD platelets
contained normal amounts of -actin mRNA and increased u-PA mRNA, which was
not detectable in control platelets.
BLOOD, 15 JULY 2001 䡠 VOLUME 98, NUMBER 2
Figure 7. Plasminogen in control and QPD platelets. Proteins were analyzed by
Western blotting with rabbit anti–human plasminogen after 10% reduced SDS-PAGE.
Lanes compare 12 L control (C) and QPD (Q) lysates (L) and ionophore releasates
(R) and control ionophore releasate, incubated overnight with 0 to 400 ng/mL tcu-PA
(CR ⫹ tcuPA), as indicated. As references, Glu-plasminogen (plg; 20 ng/lane) and the
plasmin generated by digesting Glu-plasminogen (60 ng) with 100 ng/mL tcu-PA
(plg ⫹ tcuPA) are shown. QPD platelets contained proteolyzed plasminogen that
comigrated with the heavy chain of plasmin (arrow; the light chain of plasmin was not
visualized by the antisera). They also contained correspondingly reduced proportions
of intact plasminogen and some smaller proteolyzed components, not evident in
normal platelets. When control platelet releasate was incubated with exogenous
tcu-PA, there was a similar loss of intact plasminogen, but the extent of plasminogen
proteolysis was not as complete as in QPD platelets.
degradation of ␣-granule fibrinogen to FDPs that comigrated with
QPD platelet FDPs (Figure 8A). ␣-Granule fibronectin was also
degraded when tcu-PA was added to normal platelet releasate
(Figure 8B). Although the fibronectin degradation in vitro was not
as extensive as in QPD platelets, there were many similarities in the
sizes of degradation products (Figure 8B, arrows). When tcu-PA
was incubated with normal platelet releasate, thrombospondin-1
was converted to a form that comigrated with the larger thrombospondin-1 degradation product in QPD platelets (Figure 9A,
arrow). Osteonectin and von Willebrand factor were degraded
when normal platelet releasate was incubated with tcu-PA to forms
Figure 6. PAI-1 in control and QPD platelets. (A) PAI-1 in control (C) and QPD (Q; 3
patients [Pt] are shown) samples was analyzed by Western blotting with rabbit
anti–human PAI-1 after 10% nonreduced SDS-PAGE. Lanes compare 5 L lysate (L)
and ionophore releasates (R), 20 L K562 media, and 5 L control ionophore
releasate, incubated with 0 to 400 ng/mL tcu-PA (CR ⫹ tcuPA), as indicated. Lane *
shows the PAI-1 affinity purified from QL using monoclonal anti–u-PA. QPD platelet
lysates contained PAI-1 in high–molecular weight complexes (bands near the 98-kd
marker) that comigrated with the complexes generated by adding tcu-PA to control
releasates. Proteolyzed PAI-1 (arrow) was detected in QPD platelet lysates and in
long exposures (not shown) of control releasates incubated with tcu-PA. (B)
u-PA–PAI-1 complex ELISA indicated that, unlike control samples, QPD platelet
lysates and releasates were unable to generate additional u-PA–PAI-1 complexes in
vitro with added (⫹) tcu-PA (data representative of 2 separate experiments with
pooled samples).
Figure 8. ␣-granule fibrinogen and fibronectin degradation. Western blots
compare nonreduced fibrinogen (A; 5%-8% SDS-PAGE) and fibronectin (B; 4%-8%
SDS-PAGE) in QPD (Q) and control (C) platelet lysates with the degradation products
generated by incubating normal platelet ionophore releasate (CR) with 0, 25, 50, or
100 ng/mL tcu-PA (tcuPA), as indicated (volumes of releasate and lysates: A, 3.6
L/lane; B, 15 L/lane). When tcu-PA was incubated with normal platelet secretory
proteins, ␣-granule fibrinogen and fibronectin were proteolyzed to forms that
comigrated (arrows) with their degraded forms in QPD platelets.
From www.bloodjournal.org by guest on March 4, 2016. For personal use only.
BLOOD, 15 JULY 2001 䡠 VOLUME 98, NUMBER 2
u-PA ABNORMALITIES IN QUEBEC PLATELET DISORDER
263
Figure 9. ␣-granule thrombospondin-1, von Willebrand factor, and osteonectin degradation. Western blots compare thrombospondin-1 (A), von Willebrand factor (vWF)
(B), and osteonectin (C) in QPD platelet lysates with degraded forms generated by incubating normal platelet ionophore releasate with tcu-PA (lanes and samples as in Figure
8; ng/mL tcu-PA are indicated). (A) When tcu-PA was incubated with normal platelet releasate, ␣-granule thrombospondin-1 was partially proteolyzed to a form that comigrated
with the larger thrombospondin-1 degradation product in QPD platelets (arrow) (lanes compare 24 L releasate and lysate, after reduced 4%-8% SDS-PAGE). (B) tcu-PA
induced the degradation of von Willebrand factor to a form that comigrated with degraded von Willebrand factor in QPD platelets (arrow) (lanes compare 6 L of releasate and
lysate, after reduced 7% SDS-PAGE). (C) tcu-PA also induced the proteolysis of ␣-granule osteonectin, generating a form that comigrated with degraded osteonectin in QPD
platelets (arrow) (lanes compare 9 L releasate and lysate, after reduced 12% SDS-PAGE).
that comigrated with degraded osteonectin and von Willebrand
factor in QPD platelets (Figure 9B-C, arrows). Platelet factor V was
degraded when normal platelet releasate was incubated with tcu-PA
(Figure 10A), resulting in a loss of factor V detectable by Western
blotting, as in QPD platelets.4,5 Because the amount of multimerin
in platelet releasates was limiting, multimerin proteolysis was
investigated by adding tcu-PA to normal platelet lysate, prepared
without serine protease inhibitors (Figure 10B). tcu-PA induced a
striking loss of multimerin detected by Western blotting in these
experiments, as in QPD platelets (Figure 10B shows multimerin
multimers; findings in samples analyzed by reduced SDS-PAGE
were similar [not shown]).
Discussion
Patients with Quebec platelet disorder have an unusual biochemical
defect that causes their ␣-granule proteins to be degraded. Unlike
patients with severe ␣-granule protein deficiencies, they suffer from
Figure 10. ␣-granule factor V and multimerin degradation. Western blots compare proteins in QPD (Q) and
control (C) platelet lysates (samples with all inhibitors) with
the forms generated by incubating normal platelet ionophore releasate (CR; A) or lysate (CL; B, lysate without
serine protease inhibitors) with 0, 25, 50, or 100 ng/mL
tcu-PA (tcuPA), as indicated. (A) When u-PA was incubated
with normal platelet secretory proteins, ␣-granule factor V
was degraded, resulting in a loss of factor V detectable by
Western blotting with polyclonal antisera, as in QPD
platelets (lanes compare 18 L lysate and releasate, after
reduced 4%-8% SDS-PAGE). (B) Although there was
some loss of detectable multimerin in lysates incubated
without tcu-PA, tcu-PA reduced the detectable multimerin,
as in QPD platelets (lanes compare 15 L lysates, separated on nonreduced multimer gels and probed with a
mixture of monoclonal and polyclonal antimultimerin).
Traces of degraded multimerin (bands below the smallest
multimerin polymer in normal platelets) were evident in the
u-PA digests (B) and in QPD platelets, with longer exposures (not shown).
bleeding that is paradoxically delayed and cannot be controlled with
platelet transfusions.1 The purpose of our current study was to determine
whether patients with QPD had a protease abnormality in their
circulating platelets. We found that unlike normal platelets, QPD
platelets contained large amounts of fibrinolytic, plasminogen-activating
proteases. Moreover, we determined this was because QPD platelets
contained markedly increased amounts of the enzyme u-PA, within a
secretory compartment. These observations suggest u-PA could be
involved in the pathogenesis of this unique storage pool disorder and its
hemorrhagic complications.
Like normal platelets, QPD platelets store plasma-derived and
megakaryocyte-synthesized proteins within their ␣-granules.5 Some
u-PA has been reported to be associated with normal platelets and their
external membranes when large quantities of platelet proteins have been
analyzed.23-26 We observed that QPD platelets contained more than
100-fold more u-PA than normal platelets, which contained up to 1.3 ng
u-PA/109 platelets. Furthermore, unlike normal platelets, QPD platelets
released u-PA and high concentrations of u-PA–PAI-1 complexes in
response to secretagogue stimulation. QPD platelet lysates, prepared
From www.bloodjournal.org by guest on March 4, 2016. For personal use only.
264
KAHR et al
with (Table 1) or without (Figure 6B) high concentrations of serine
protease inhibitors, also contained high concentrations of u-PA–PAI-1
complexes, suggesting QPD platelets costore u-PA with PAI-1 in
␣-granules.27 We suspect the increased u-PA in QPD platelets is
synthesized by their megakaryocytes because only some patients had
increased u-PA in plasma, and, unlike normal platelets, QPD platelets
contained u-PA mRNA.
u-PA has a number of different forms, and its tcu-PA form has much
greater plasminogen-activating activity than uncleaved scu-PA.28-31
These forms can be distinguished from each other and from LMW u-PA
using nonreduced and reduced SDS-PAGE.28-31 Whereas normal platelets have been reported to contain mostly scu-PA,23,24 we found QPD
platelets contained predominantly active tcu-PA, minimal scu-PA, some
LMW u-PA, and a small amount of u-PA in high–molecular weight
complexes. Moreover, unlike normal platelets, QPD platelets contained
plasminogen that was proteolyzed and that comigrated with plasmin.
The high–molecular weight u-PA complexes in QPD platelets resembled the complexes generated by incubating exogenous u-PA with
normal releasate, and they included forms recognized by PAI-1
antibodies. These data suggest the very large forms of u-PA in QPD
platelets, like the large forms in normal platelets,23,24 represent
u-PA complexed to soluble platelet protease inhibitors, such as
PAI-132-36 and protease nexin 1.37
The unregulated u-PA activity in QPD platelets indicates they do not
contain sufficient protease inhibitors to fully neutralize their stored u-PA.
Normal platelets contain large amounts of the u-PA inhibitor PAI-1
within their ␣-granules; however, most are functionally inactive, or
latent, and incapable of neutralizing plasminogen activators.27,35,38-40 We
observed that some of the u-PA in QPD platelets had been neutralized by
PAI-1. However, the amount of exogenous, recombinant PAI-1 required
to completely neutralize the u-PA secreted by QPD platelets exceeded
the amount of PAI-1 in normal and QPD platelets. Because we found
QPD platelets contained more than 100-fold more u-PA–PAI-1 complexes and 2-fold more total PAI-1 antigen than normal platelets, our
data exclude a functional or quantitative PAI-1 deficiency as the cause of
their unregulated u-PA activity. Although only a minority of the total
PAI-1 in QPD platelets was contained in high–molecular weight
complexes, we were unable to generate any further u-PA–PAI-1
complexes by adding u-PA to QPD platelet lysates or releasates in vitro.
This suggests the increased u-PA in QPD platelets depletes their stores
of active PAI-1. The relative proportions of total PAI-1, u-PA, and
u-PA–PAI-1 complexes detected in QPD platelets by ELISA (954 ng
PAI-1, 505 ng u-PA [OS assay], and 95 ng u-PA–PAI-1 complexes/109
platelets) and the similar molecular masses of PAI-1 and u-PA41 infer
that only a limited amount (approximately 5%) of the total PAI-1 in
QPD platelets was active in neutralizing u-PA in vivo. Interestingly, this
estimate corroborates previous reports that normal platelets contain less
than 10% active PAI-1.27,35,38,39 The large amounts of u-PA in QPD
platelets, and the relatively limited supply of u-PA inhibitors in platelets,
could be part of the reason patients with QPD experience delayed
bleeding that cannot be controlled with platelet transfusions.
The diversity of proteins degraded in QPD platelets has suggested
that fairly broad-specificity protease(s) are involved. The FDPs secreted
by QPD platelets are not recognized by a monoclonal antibody specific
for plasmin-degraded fibrinogen.6 Using sensitive Western blots, we
observed that QPD platelets contained proteolyzed forms of plasminogen with the mobility of plasmin, but we were unable to detect plasmin
activity in QPD platelet releasates by zymography, even after u-PA was
immunodepleted. tcu-PA and LMW u-PA are known to proteolyze
fibrinogen in addition to plasminogen,42 but where they cleave fibrinogen has not been determined. Moreover, it is not yet known whether
BLOOD, 15 JULY 2001 䡠 VOLUME 98, NUMBER 2
tcu-PA and LMW u-PA can cleave other potential substrates within
platelets. We observed that the net effects of adding exogenous tcu-PA to
normal platelet secretory proteins (in concentrations similar to the
increased u-PA in QPD platelets) were a loss of intact plasminogen and
the proteolysis of many ␣-granule proteins. There were phenotypic
similarities in the sizes of the fibrinogen, fibronectin, von Willebrand
factor, thrombospondin-1, and osteonectin degradation products generated to degraded proteins in QPD platelets. Furthermore, platelet
multimerin and factor V were proteolyzed after adding tcu-PA, resulting
in a loss of the forms detectable by Western blotting, as in QPD platelets.
These observations provide indirect evidence that the changes to
␣-granule proteins, including multimerin, in the QPD likely reflect a
complex process of proteolysis that may be initiated by increased
platelet u-PA. The less extensive proteolysis of plasminogen—and some
of the other ␣-granule proteins—in the in vitro digests compared to
QPD platelets could reflect differences in the duration of substrate
protein exposure to u-PA, or it could reflect contributions of factors, such
as the environment within platelets, that enhance ␣-granule protein
proteolysis in vivo. Although platelets have receptors on their external
membranes for scu-PA and tcu-PA43,44 that could modulate some aspects
of u-PA proteolysis in the QPD, we observed that membrane-tethered
proteins were not required to degrade ␣-granule proteins to forms found
in QPD platelets.
u-PA is normally expressed in many different tissues,45 and it is
thought to play a role in diverse physiological and pathological
processes.31 In mice, u-PA deficiency causes problems with excess
fibrin deposition, whereas its overexpression in the liver results in
bleeding, marked hypofibrinogenemia, and systemic fibrinogenolysis.46,47 The QPD has biochemical abnormalities distinct from other
platelet storage pool disorders1 and from congenital bleeding
disorders associated with increased t-PA levels or t-PA–related
proteins in plasma.48,49 Like ␣2-antiplasmin deficiency,50 the QPD
is not associated with systemic fibrinogenolysis.6 This may be
because plasma u-PA inhibitors effectively regulate the normal to
increased u-PA levels in the plasma of patients with QPD. Our
observations indicate patients with the QPD have an inherited,
autosomal dominant defect that increases u-PA expression and
storage in their megakaryocytes and platelets. Fibrinolytic inhibitors (such as tranexamic acid and epsilon amino caproic acid)
rapidly and effectively control bleeding in patients with the QPD,
yet they do not measurably improve QPD ␣-granule protein
degradation, even when they are given for several weeks of
therapy.6 This observation suggests that the moderate to severe
bleeding in patients with the QPD could result from accelerated
fibrinolysis within the hemostatic plug, where the concentrations of
released u-PA may overwhelm protease inhibitors.
The QPD is the only inherited bleeding disorder in humans
associated with increased levels of u-PA in blood. Unraveling its
genetic cause is likely to provide further insights into this unusual
and sometimes fatal bleeding disorder.
Acknowledgments
C.P.M.H. is the recipient of a Career Investigator Award from the
Heart and Stroke Foundation of Ontario, and a Canada Research
Chair in Molecular Hemostasis from the Government of Canada
and a Premier’s Research Excellence Award from the Ontario
Government. We thank Dr Jack Henkin at Abbott Laboratories
(North Chicago, IL) for the gift of recombinant u-PA.
From www.bloodjournal.org by guest on March 4, 2016. For personal use only.
BLOOD, 15 JULY 2001 䡠 VOLUME 98, NUMBER 2
u-PA ABNORMALITIES IN QUEBEC PLATELET DISORDER
265
References
1. Hayward CPM. Inherited disorders of platelet
␣-granules. Platelets. 1997;8:197-209.
2. Rao AK. Congenital disorders of platelet function:
disorders of signal transduction and secretion.
Am J Med Sci. 1998;316:69-76.
3. Nurden AT. Inherited abnormalities of platelets.
Thromb Haemost. 1999;82:468-480.
4. Hayward CPM, Rivard GE, Kane WH, et al. An
autosomal dominant, qualitative platelet disorder
associated with multimerin deficiency, abnormalities in platelet factor V, thrombospondin, von Willebrand factor, and fibrinogen and an epinephrine
aggregation defect. Blood. 1996;87:4967-4978.
5. Hayward CPM, Cramer EM, Kane WH, et al.
Studies of a second family with the Quebec platelet disorder: evidence that the degradation of the
alpha-granule membrane and its soluble contents
are not secondary to a defect in targeting proteins
to alpha-granules. Blood. 1997;89:1243-1253.
6. Hayward CPM, Welch B, Bouchard M, Zheng S,
Rivard GE. Fibrinogen degradation products in
patients with the Quebec platelet disorder. Br J
Haematol. 1997;97:497-503.
7. Tracey PB, Giles AR, Mann KG, Eide LL,
Hoogendoorn H, Rivard GE. Factor V (Quebec):
a bleeding diathesis associated with a qualitative
platelet factor V deficiency. J Clin Invest. 1984;74:
1221-1228.
8. Janeway CM, Rivard GE, Tracy PB, Mann KG.
Factor V Quebec revisited. Blood. 1996;87:35713578.
9. Weiss HJ, Lages B, Zheng S, Hayward CPM.
Platelet factor V New York: a defect in factor V
distinct from that in factor V Quebec resulting in
impaired prothrombinase generation. Am J Hematol. 2001;66:130-139.
10. Stefansson S, Muhammad S, Cheng X-F, Battey
FD, Strickland DK, Lawrence DA. Plasminogen
activator inhibitor-1 contains a cryptic high-affinity
binding site for low-density lipoprotein receptorrelated protein. J Biol Chem. 1998;273:63586366.
11. Kassis J, Hirsh J, Podor TJ. Evidence that postoperative fibrinolytic shutdown is mediated by
plasma factors that stimulate endothelial cell type
1 plasminogen activator inhibitor biosynthesis.
Blood. 1992;80:1758-1764.
12. Alitalo R, Andersson LC, Tapiovaara H, Sistonen
L, Vaheri A, Stephens R. Down-regulation of proteolytic activity in 12-O-tetradecanoyl-phorbol-13acetate-induced K562 leukemia cell cultures:
depletion of active urokinase by excess type 1
plasminogen activator inhibitor. J Cell Phys.
1989;140:119-130.
13. Granelli-Piperno A, Reich E. A study of proteases
and protease-inhibitor complexes in biological
fluids. J Exp Med. 1978;148:223-234.
14. Vassalli JD, Dayer JM, Wohlwend A, Belin D.
Concomitant secretion of prourokinase and of a
plasminogen activator-specific inhibitor by cultured human monocytes/macrophages. J Exp
Med. 1984;159:1653-1668.
15. Hayward CPM, Smith JW, Horsewood P, Warkentin TE, Kelton JG. p-155, A multimeric platelet
protein that is expressed on activated platelets.
J Biol Chem. 1991;266:7114-7120.
16. Philips M, Juul A-G, Selmer J, Lind B, Thorsen S.
A specific immunologic assay for functional plasminogen activator inhibitor 1 in plasma: standardized measurements of the inhibitor and related
parameters in patients with venous thromboembolic disease. Thromb Haemost. 1992;68:486494.
17. Hayward CPM, Hassell JA, Denomme GA, Ra-
chubinski RA, Brown C, Kelton JG. The cDNA
sequence of human endothelial cell multimerin: a
unique protein with RGDS, coiled-coil, and epidermal growth factor-like domains and a carboxyl
terminus similar to the globular domain of
complement C1q and collagens type VIII and X.
J Biol Chem. 1995;270:18246-18251.
18. Darras V, Thienpont M, Stump DC, Collen D.
Measurement of urokinase-type plasminogen activator (u-PA) with an enzyme-linked immunosorbent assay (ELISA) based on three murine monoclonal antibodies. Thromb Haemost. 1986;56:
411-414.
19. Grondahl-Hansen J, Agerlin N, Munkholm-Larsen
P, et al. Sensitive and specific enzyme-linked immunosorbent assay for urokinase-type plasminogen activator and its application to plasma from
patients with breast cancer. J Lab Clin Med.
1988;111:42-51.
20. Wojta J, Binder BR, Huber K, Hoover RL. Evaluation of fibrinolytic capacity in plasma during
thrombolytic therapy with single (scu-PA) or twochain urokinase-type plasminogen activator (tcuPA) by a combined assay system for urokinase
type plasminogen activator antigen and function.
Thromb Haemost. 1989;61:289-293.
21. Declerck PJ, Van Keer L, Verstreken M, Collen D.
An enzyme-linked immunosorbent assay for
urokinase-type plasminogen activator (u-PA) and
mutants and chimeras containing the serine protease domain of u-PA. Thromb Haemost. 1992;
67:95-100.
22. Vassalli J-D, Belin D. Amiloride selectively inhibits
the urokinase-type plasminogen activator. FEBS
Lett. 1987;214:187-191.
33. Kruithof EKO, Tran-Thang C, Bachmann F. Studies on the release of a plasminogen activator inhibitor by human platelets. Thromb Haemost.
1986;55:201-205.
34. Sprengers ED, Akkerman JW, Jansen BG. Blood
platelet plasminogen activator inhibitor: two different pools of endothelial cell type plasminogen
activator inhibitor in human blood. Thromb Haemost. 1986;55:325-329.
35. Booth NA, Croll A, Bennett B. The activity of plasminogen activator inhibitor-1 (PAI-1) of human
platelet. Fibrinolysis. 1990;4(suppl 2):138-140.
36. van Meijer M, Pannekoek H. Structure of plasminogen activator inhibitor 1 (PAI-1) and its function in fibrinolysis: an update. Fibrinolysis. 1995;
9:263-276.
37. Gronke RS, Knauer DJ, Veeraraghavan S, Baker
JB. A form of protease nexin I is expressed on the
platelet surface during platelet activation. Blood.
1989;73:472-478.
38. Booth NA, Simpson AJ, Croll A, Bennett B,
MacGregor IR. Plasminogen activator inhibitor
(PAI-1) in plasma and platelets. Br J Haematol.
1988;70:327-333.
39. Declerck PJ, Alessi M-C, Verstreken M, Kruithof
EKO, Juhan-Vague I, Collen D. Measurement of
plasminogen activator inhibitor 1 in biologic fluids
with a murine monoclonal antibody-based enzyme-linked immunosorbent assay. Blood. 1988;
71:220-225.
40. Lang IM, Marsh JJ, Moser KM, Schleef RR. Presence of active and latent type 1 plasminogen activator inhibitor associated with porcine platelets.
Blood. 1992;80:2269-2274.
23. Park S, Harker LA, Marzec UM, Levin EG. Demonstration of single chain urokinase-type plasminogen activator on human platelet membrane.
Blood. 1989;73:1421-1425.
41. Bachmann F. Plasminogen-plasmin enzyme system. In: Colman RW, Hirsh J, Marder VJ, Clowes
AW, George JN, eds. Hemostasis and Thrombosis. Philadelphia, PA: Lippincott Williams &
Wilkins; 2001:275-320.
24. Gurewich V, Johnstone M, Loza J-P, Pannell R.
Pro-urokinase and prekallikrein are both associated with platelets: implications for intrinsic pathway of fibrinolysis and for therapeutic thrombolysis. FEBS Lett. 1993;318:317-321.
42. Weitz JI, Leslie B. Urokinase has direct catalytic
activity against fibrinogen and renders it less clottable by thrombin. J Clin Invest. 1990;86:203212.
25. Gurewich V, Johnstone MT, Pannell R. The selective uptake of high molecular weight urokinasetype plasminogen activator by human platelets.
Fibrinolysis. 1995;9:188-195.
26. Lenich C, Liu J-N, Gurewich V. Thrombin stimulation of platelets induces plasminogen activation
mediated by endogenous urokinase-type plasminogen activator. Blood. 1997;90:3579-3586.
43. Vaughan DE, Van Houtte E, Collen D. Urokinase
binds to platelets through a specific saturable,
low-affinity mechanism. Fibrinolysis. 1990;4:141146.
44. Jiang Y, Pannell R, Liu J-N, Gurewich V. Evidence for a novel binding protein to urokinasetype plasminogen activator in platelet membranes. Blood. 1996;87:2775-2781.
27. Lang IM, Schleef RR. Calcium-dependent stabilization of type 1 plasminogen activator inhibitor
within platelet ␣-granules. J Biol Chem. 1996;
271:2754-2761.
45. Larsson L-I, Skriver L, Nielsen LS, GrondahlHansen J, Kristensen P, Dano K. Distribution of
urokinase-type plasminogen activator immunoreactivity in the mouse. J Cell Biol. 1984;98:894903.
28. Dano K, Andreasen PA, Grondahl-Hansen J,
Kristensen P, Nielsen LS, Skriver L. Plasminogen
activators, tissue degradation, and cancer. Adv
Cancer Res. 1985;44:139-166.
46. Carmeliet P, Schoonjans L, Kieckens L, et al.
Physiological consequences of loss of plasminogen activator gene function in mice. Nature.
1994;368:419-424.
29. Henkin J, Marcotte P, Yang HC. The plasminogen-plasmin system. Prog Cardiovasc Dis. 1991;
34:135-164.
47. Heckel JL, Sandgren EP, Degen JL, Palmiter RD,
Brinster RL. Neonatal bleeding in transgenic mice
expressing urokinase-type plasminogen activator.
Cell. 1990;62:447-456.
30. Collen D, Lijnen HR. Basic and clinical aspects of
fibrinolysis and thrombolysis. Blood. 1991;78:
3114-3124.
31. Andreasen PA, Kjoller L, Christensen L, Duffy MJ.
The urokinase-type plasminogen activator system in cancer metastasis: a review. Int J Cancer.
1997;72:1-22.
32. Erickson LA, Ginsberg MH, Loskutoff DJ. Detection and partial characterization of an inhibitor of
plasminogen activator in human platelets. J Clin
Invest. 1984;74:1465-1472.
48. Booth NA, Bennett B, Wijngaards G, Grieve JHK.
A new life-long hemorrhagic disorder due to excess plasminogen activator. Blood. 1983;61:267275.
49. Aznar J, Estelles A, Vila V, Reganon E, Espana F,
Villa P. Inherited fibrinolytic disorder due to an
enhanced plasminogen activator level. Thromb
Haemost. 1984;52:196-200.
50. Saito H. Alpha 2-plasmin inhibitor and its deficiency states. J Lab Clin Med. 1988;112:671-678.
From www.bloodjournal.org by guest on March 4, 2016. For personal use only.
2001 98: 257-265
doi:10.1182/blood.V98.2.257
Platelets from patients with the Quebec platelet disorder contain and secrete
abnormal amounts of urokinase-type plasminogen activator
Walter H. A. Kahr, Shilun Zheng, Prameet M. Sheth, Menaka Pai, Alison Cowie, Madeleine Bouchard,
Thomas J. Podor, Georges E. Rivard and Catherine P. M. Hayward
Updated information and services can be found at:
http://www.bloodjournal.org/content/98/2/257.full.html
Articles on similar topics can be found in the following Blood collections
Hemostasis, Thrombosis, and Vascular Biology (2494 articles)
Plenary Papers (474 articles)
Information about reproducing this article in parts or in its entirety may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests
Information about ordering reprints may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#reprints
Information about subscriptions and ASH membership may be found online at:
http://www.bloodjournal.org/site/subscriptions/index.xhtml
Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of
Hematology, 2021 L St, NW, Suite 900, Washington DC 20036.
Copyright 2011 by The American Society of Hematology; all rights reserved.