Coeliac disease Malabsorption Maldigestion
advertisement

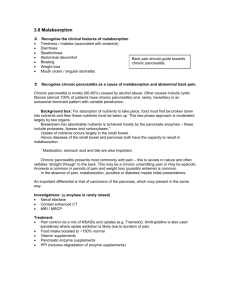
Coeliac disease Malabsorption Maldigestion Krisztina Gecse, MD, PhD First Department of Medicine Semmelweis University Budapest, Hungary Coeliac disease, malabsorption, maldigestion Overview Coeliac disease • Patomechanism • Classification • Signs and symptoms • Diagnosis • Treatment • Complications Malabsorption, maldigestion • Definitions • Etiology • Signs and Symptoms • Diagnosis Coeliac disease (gluten-sensitive enteropathy/nontropical sprue) Patomechanism • Loss of immune tolerance • • • • http://bestpractice.bmj.com; Plenge RM Nature Genetics 2010 to gliadin peptide antigens derived from wheat, rye, barley, and related grains High-affinity binding to HLA peptides (DQ2 or DQ8) found on APCs Activation of Th cells Th1: cell death and tissue remodelling (villous atrophy and crypt hyperplasia) Th2: plasma cell maturation and anti-gliadin and antitTG antibody production Coeliac disease Classification • Classic • diarrhea, • symptoms of malabsorption such as steatorrhea, • weight loss, or other signs of nutrient or vitamin deficiency • possess antibodies against gliadin and tissue transglutaminase (tTG) • typical histology features • Atypical • minor gastrointestinal complaints • osteoporosis, arthritis, increased transaminases, neurological symptoms, or infertility • typical mucosal damage and celiac specific antibody pattern Coeliac disease Classification • Asymptomatic (Silent) • incidental diagnosis (no or only mild clinical symptoms) • based upon screenings for antibodies against gliadin or tissue transglutaminase • typical architectural remodelling on histology • Latent • minor or no symptoms • , positive serology, but normal jejunal mucosa • eg.: childhood disease Coeliac disease Signs and symptoms • Presents between the ages of 10 and 40 years • GI manifestations: diarrhea, steatorrhea, flatulence • Consequences of malabsorption: • iron-deficiency anaemia, • weight loss, • neurologic disorders (vitamin B deficiency), • osteopenia (deficiency of vitamin D and calcium) • Associated diseases: • Type 1 DM • Sjögren-sy • Allopecia areata • Dermatitis herpetiformis Duhring • Autoimmune hepatitis • Autoimmune thyreoiditis Coeliac disease Diagnosis • Clinical signs and symptoms • Serology • anti-tissue transglutaminase (TTG) antibody IgA, IgG • Anti-endomysial antibody IgA • Anti-deamidated gliadin peptides (DGPs) IgG N.b.: serology may turn negative on gluten-free diet • Gluten challenge • HLA DQ2/DQ8 testing • Endoscopy: • scalloping of the small bowel folds • mucosal mosaic pattern or "cracked-mud” Coeliac disease Diagnosis • Histology: Marsh classification Rubio-Tapia A Am J Gastroenterol 2013, http://openi.nlm.nih.gov Coeliac disease Treatment • Lifelong adherence to a gluten-free diet - consultation with a dietitian: • foods containing wheat, rye, and barley should be avoided • soybean, rice, corn and potatoes are safe • stabilizers or emulsifiers may contain gluten • distilled alcoholic beverages and wine are gluten free; beers, ales, lagers, and malt vinegars should be avoided • dairy products not be well tolerated initially, due to secondary lactose intolerance • oats can be introduced with caution • Education about the disease • Identify and treat nutritional deficiencies • Continuous long-term follow-up Coeliac disease Complications • • • • • consequences of malabsorption malnutrition enteropathy-associated T-cell lymphoma (EATL) adenocarcinoma collagenous sprue (rare) Maldigestion and malabsorption Definition and etiology • Maldigestion: abnormal digestion – nutrient break-down due to insufficiency of gastric, pancreatic or bile function • Gastrectomy • Exocrine pancreatic insufficiency: chr. pancreatitis, CF, resection • Cholestasis, bile loosing sy: eg.: ileum resection in CD • Malabsorption: abnormal absorption of the broken-down nutrients due to mucosal, vascular or lymphatic abnormalities digestion • Mucosal injury/lack of absorptive surface: coeliac disease, M. Crohn, lactase intolerance, amyloidosis, radiation enteritis, short bowel sy. • Vascular: mesenteric ischemia, right sided congestive heart failure • Lymphatic: M. Whipple Maldigestion and malabsorption Signs and Symptoms • Diarrhoea (watery: carbs and bile acids; steatorrhea: lipids) • Weight loss • Nutrient deficiencies (both qualitative and quantitative) • protein malabsorption --> hypoproteinaemiac oedema • Fe • Folic acid --> anaemia • B12 • Ca • Vitamin D --> osteoporosis, osteopenia • Vitamin K • Vitamin B • Vitamin A --> coagulopathy --> neuropsychiatric --> hairloss, breaking nails, vision Maldigestion and malabsorption Diagnosis: A. Morphological imaging of the small bowel - endoscopy 1. Push enteroscopy 2. Double-balloon enteroscopy 200cm enteroscope + 140cm overtube balloon on the enteroscope and the overtube 3. Single-balloon enteroscopy Yamamoto et al. Gastrointest Endosc 2001; Tsujikawa et al. Endoscopy 2008 Maldigestion and malabsorption Diagnosis: A. Morphological imaging of the small bowel Maldigestion and malabsorption Diagnosis: A. Morphological imaging of the small bowel 4. Capsule endoscopy https://www.youtube.com/watch?v=9qnvSrqV6Lw Maldigestion and malabsorption Diagnosis: A. Morphological imaging of the small bowel - radiology 1. X-ray: native, mono- or double contrast 2. CT-enterography or enteroclysis 3. MR enterography Maldigestion and malabsorption Diagnosis: B. Functional imaging of the small bowel 1. D-xilose test: 5g D-xilose in 300ml water Background: D-xilose is absorbed and not metabolised excretion in the urine can be measured Use: differentiates between malabsoption and maldigestion 2. Schilling test: radio-labelled B12 per oral Background: absorbed in the terminal ileum, urine excretion can be measured Use: renal excretion is low if malabsorption in the terminal ileum (even after addition of IF) 3. Oral iron challenge: Background: iron absorbs in the proximal small bowel Use: no increase in serum iron level in case of malabsorption 4. Lactose H2 breath test 5. Lactulose H2 breath test