RENAL PHYSIOLOGY AND FUNCTION Objectives: Upon
advertisement

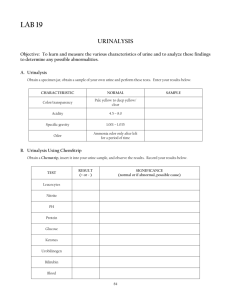
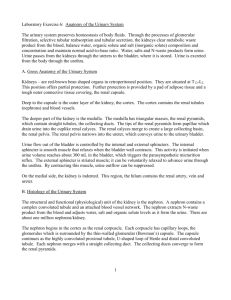
RENAL PHYSIOLOGY AND FUNCTION Objectives: Upon completion of this CLS 426 module, the Clinical Laboratory Science student will be able to: 1. Define the following terms: a. Cystitis b. Nephritis c. Urethritis 2. Describe the gross anatomy of the urinary tract system. 3. Name the functional unit of the kidneys. 4. Describe the components of the nephron, in sequence, as related to urine formation. 5. Discuss the formation of urine, involving the following physiologic mechanisms: a. Renal blood flow b. Glomerular filtration c. Tubular reabsorption 1) Active 2) Passive d. Tubular secretion 1) Active 2) Passive 6. Discuss the following functions of the kidneys: a. Maintenance of acid-base balance b. Regulation of water and electrolyte balance, including the effects of: 1) ADH 2) Aldosterone c. Excretion of waste products d. Maintenance of blood pressure 7. Explain the term “renal threshold”, using glucose as an example. 8. Discuss the factors that influence the concentration of substances in urine. 9. Discuss the following as they relate to urine output in 24 hours, including possible causes of any abnormal conditions: a. Normal urine output d. Anuria b. Polyuria e. Nocturia c. Oliguria 10. Evaluate the use of the creatinine clearance test for the assessment of glomerular function. 11. Evaluate the use of specific gravity and osmolality for the assessment of renal concentrating ability CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 1 RENAL PHYSIOLOGY AND FUNCTION I II. Renal Function A. Urine formation is the primary excretory function of the kidneys B. The kidneys function to regulate the body's internal environment, maintaining homeostasis: 1. Maintains acid-base balance of the body 2. Regulates body fluids and water balance 3. Aids in maintenance of blood pressure 4. Maintains electrolyte balance 5. Excretes potentially toxic waste products 6. Reabsorbs essential substances 7. Hormonal function a. Serves as target organ for certain hormones (aldosterone, ADH) b. Influences the metabolism of certain hormones (Vitamin D) c. Secretes regulatory hormones (erythropoietin) d. Secretes the enzyme Renin (Renin-Angiotensin-Aldosterone Axis) C. Kidney function is dependent upon proper: 1. Renal blood flow (~20-25% of cardiac output circulates to renal artery) 2. Glomerular filtration 3. Tubular reabsorption 4. Tubular secretion Components of the Urinary Tract System (gross, macro level) A. Kidneys (textbook, pg 54, fig 4-1 1. Bean-shaped paired organs located in the small of the back 2. Each kidney: ~ 12 cm long, 5-7 cm wide, 2.5 cm thick, weigh 150 grams 3. Two distinct areas apparent on cross section a. Outer cortex layer (granular in appearance) b. Inner medulla layer (renal tissue shaped into pyramids) 4. Inflammation/infection of kidney: __________________________ B. Renal Pelvis: Funnel-shaped, receives urine from the major calyces; funnels urine into the ureter C. Ureter: Fibromuscular tube approx 25 cm long; one ureter extends down from each kidney and connects to the bladder D. Bladder: Muscular sac, shaped like a pyramid; acts as a ‘holding tank’ for temporary urine storage until voided; Inflammation/infection of the bladder wall: _______________ E. Urethra: Canal connecting the bladder to the exterior of body Length: males = 24 cm, women = 4 cm; Inflammation/infection of urethra: _________________ CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 2 III. Components of the Nephron (micro level) (textbook, pg 55, fig 4-2; pg 57, fig 4-3) A. The nephron is the functional unit of the kidney B. C. IV. Component parts of the nephron include 1. Glomerulus (renal corpuscle, cortex only) 2. Tubules a. Proximal convoluted tubule b. Loop of henle c. Distal convoluted tubule d. Collecting tubule (duct) Function of the nephron 1. Urine formation 2. Three distinct processes a. Filtration b. Reabsorption c. Secretion Glomerulus A. Component parts 1. Consists of a capillary network (or tuft) surrounded by a thin layer of cells known as Bowman's capsule (Bowman’s space) B. 2. Afferent arteriole feeds into the glomerulus from renal artery 3. Efferent arteriole exits the glomerulus and extends into a network of peritubular capillaries and finally into the renal vein 4. Ultrafiltrate empties into the proximal convoluted tubule (PCT) Function: FILTRATION of plasma 1. Serves as a non-selective filter of plasma substances a. Allows free passage of water, electrolytes and plasma substances with low molecular weight (<70,000) b. `Selectivity' of the filtration process is based on the solute's molecular size and charge. Glomerular ‘shield of negativity’ essentially repels most plasma proteins 2. Difference between glomerular filtrate and plasma is the absence of a. Large plasma proteins (>70,000) b. Protein-bound substances (bilirubin, drugs, etc) c. Cells (RBC, WBC) 3. Glomerular filtrate (filtered urine) is referred to as an ‘ultrafiltrate’ of plasma with specific gravity = 1.010 4. Ultrafiltrate volume = 120 ml/minute CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 3 5. V. Filtration of plasma is dependent upon a. Normal cellular structure of glomerulus (basement membrane) b. Hydrostatic pressure: due to size difference of afferent and efferent arterioles c. Oncotic pressure: due to unfiltered plasma proteins d. Feedback mechanisms: Aldosterone-Renin-Angiotensin system (textbook, pg 74, fig 4-15) 1) Responds to changes in blood pressure and plasma sodium Decreased BP; decreased plasma sodium 2) Monitored by juxtaglomerular apparatus: specialized cells in the afferent arteriole and distal convoluted tubule 3) Renin: enzyme produced by the juxtaglomerular cells Aldosterone: hormone produced by adrenal cortex Angiotensinogen: protein substrate produced by liver Renal Tubules A Component parts (textbook, pg 55, fig 4-2) 1. Proximal Convoluted Tubule (PCT) B. 2. Loop of Henle: consists of descending and ascending limbs 3. Distal Convoluted Tubule (DCT) (textbook, pg 71-73, fig 4-13, 4-14, 4-15, 4-16) a. Antidiuretic Hormone (ADH) controls water permeability of DCT b. Aldosterone controls sodium reabsorption by DCT 4. Collecting Tubule or Ducts a. ADH controls water permeability of collecting ducts Function 1. REABSORPTION of substances needed by the body, from tubules back into the bloodstream (glucose, amino acids, water, electrolytes) 2. SECRETION of substances not needed by the body, from the bloodstream into the tubules/urine for excretion (toxins, drugs, metabolic waste products) 3. Final urine output: a. 1 ml/minute (recall glomeruli produce 120 ml/min of filtrate) b. Dependent on hydration status: can range from 0.3 ml/min (dehydrated) to 15 ml/min (excessive hydration) CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 4 C. Tubular transport mechanisms 1. Active transport a. Substance to be reabsorbed must combine with a carrier protein located in the membrane of the renal tubular cells b. This interaction creates electrochemical energy c. Energy is used to transfer substance across cell membrane back into bloodstream 2. Passive transport a. Simple diffusion b. Molecules move across cell membranes due to concentration differences on opposite sides of membrane c. No energy is involved in this process 3. Renal threshold a. Plasma concentration of a substance at which reabsorption stops b. Active and passive transport can be influenced by the plasma concentration of the substance c. Maximal reabsorptive capacity is reached d. Example: glucose = 160-180 mg/dl Tubular Reabsorption Mechanism Substance Location Active transport glucose, amino acids, HCO3, salts chloride sodium PCT Ascending loop of Henle PCT, DCT Passive transport Water urea sodium PCT, descending loop of Henle, collecting tubules PCT, ascending loop of Henle Ascending loop of Henle (carried with chloride) VI. Normal Urine Composition (textbook, pg 81, table 5-1) A. Water (94%) B. Solutes (6%) 1. Chemical (organic) substances: metabolic waste a. Urea b. Creatinine c. Uric acid 2. Electrolytes and ions a. Salt as NaCl (sodium and chloride) b. Potassium c. NH4 d. Inorganic phosphates (PO4) e. Inorganic sulfates (SO4) f. Hormones, vitamins, medications g. Threshold substances (ex: glucose) CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 5 C. VII. Factors which influence the 'concentration of substances' found in the urine: 1. Dietary intake 2. Physical activity 3. Body metabolism 4. Endocrine function (ADH, Aldosterone) 5. Body position (orthostatic proteinuria) Urine Output A. Average 24 hour output 1. Normal: _________________________ 2. Extreme: _________________________ B. Factors influencing urine volume 1. Fluid intake 2. Non-renal fluid loss (vomiting, diarrhea, sweating) 3. Secretion of ADH (too much, too little) 4. Body’s need to excrete solutes such as glucose, salt or urea C. Abnormal Urine Output 1. Polyuria a. Increased urine output (>2500 ml/24 hr) b. Causes of polyuria 1) Artificially induced by suppression of ADH (diuretics, caffeine, alcohol) 2) Diabetes mellitus: condition of abnormal carbohydrate metabolism; plasma glucose levels rise, exceeding renal threshold, causing glucose to be excreted into the urine resulting in polyuria 3) Diabetes insipidus: abnormality in ADH secretion or tubular response to ADH, resulting in polyuria a) b) ;4) ;2. Neurogenic diabetes insipidus: pituitary gland does not produce ADH Nephrogenic diabetes insipidus: renal tubules do not respond to ADH Diabetes mellitus and diabetes insipidus are completely unrelated conditions. Explain why these two different conditions share the term ‘diabetes’; explain the meaning of ‘mellitus’ and ‘insipidus’ (textbook, pg 108) Oliguria a. Defined as: b. Occurs when: CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 6 ;3. Anuria a. Defined as: b. ;4. Nocturia a. Defined as: b. VIII. Occurs when: Occurs when: Renal Function Tests A. Assessment of Tubular Reabsorption 1. Used to assess the kidney's ability to concentrate the urine 2. Good test to detect early renal disease 3. Collectively termed CONCENTRATION TESTS. Urine concentration is largely determined by the body’s state of hydration, and the normal kidney will reabsorb only the amount of water necessary to preserve an adequate supply of body water. Thus, control of fluid intake must be incorporated into test protocol a. Fluid Deprivation Test b. Free Water Clearance Test 4. Laboratory measurements: a. Specific gravity and osmolality measurements indicate how concentrated a urine sample is and therefore reflect the kidneys ability to concentrate urine (recall these tests determine the density of the urine) b. Specific gravity (by refractometry) 1) Dependent on the number and density of particles in soln 2) Presence of high molecular weight substances (glucose, protein) affect density of urine 3) Not ideal test to determine concentrating ability of kidney because presence of glucose and protein in urine is due to disease process, not due to a change in the tubules’ ability to concentrate urine (determining specific gravity by reagent strip method eliminates this problem) 4) Normal: SG >1.025 (indicates concentrated urine specimen) CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 7 c. Osmolality 1) Dependent on number of particles in solution and is expressed as: osmoles of solute present kilogram of solvent (urine) 2) An osmole is defined as the amount of a substance that dissociates in solution to produce one mole of particles If 1 osmol dissociates into 1 mole of particles in solution, then 1 milliosmole = 1 millimole mOsmol is the term used most frequently (mOsm) when referring to solute composition in body fluids 3) Presence of high molecular weight substances (glucose, protein) do not affect osmolality measurements Example: Glucose does NOT dissociate in solution; 1 mmol of glucose equals 1 mOsm NaCl dissociates into 2 particles: 1 Na+ and 1 Cl- ion; 1 mmol of NaCl equals 2 mOsm The osmolality of 1 mmol/L of NaCl is ~ 2 times greater than the osmolality of 1 mmol/L glucose B. 4) Osmolality is preferred over specific gravity for determining concentrating ability of renal tubules because it provides a more accurate evaluation of the kidney’s concentrating ability 5) Normal: >800 mOsm/L (indicates concentrated urine) Assessment of Glomerular Filtration 1. The standard test used to measure the filtering capacity of the glomeruli is the CLEARANCE TEST. a. A clearance test measures the RATE at which the kidneys can clear a ‘filterable’ substance from the blood b. Glomerular filtration rate (GFR): to ensure that only glomerular filtration is measured, the substance must not be reabsorbed or secreted by the tubules CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 8 c. 2. Sample requirements: 1) Timed urine specimen, usually 24hr collection. 2) Plasma sample, collected during the 24hr urine collection Clearance calculation: C=U xV P 3. = mL/min C = clearance U = urine concentration of substance P = plasma concentration of substance V = volume of urine per total minutes of collection period (ex: 1200 ml/1440 min) Endogenous procedure: measures a substance that is normally found in the patient's blood. example: creatinine, B2-microglobulin. Exogenous procedure: measures a substance which has been given to the patient (substance comes from outside the body) example: inulin. Inulin Clearance is considered the reference method for the determination of GFR. 4. Creatinine Clearance (CrCl) a. Most common test performed to evaluate GFR b. Creatinine is an endogenous substance and is a by-product of muscle metabolism c. Creatinine is produced at a steady rate, resulting in constant plasma concentration and constant urinary excretion rate. d. Creatinine production is directly dependent on muscle mass, thus values will vary with patient’s sex, age, muscle mass. e. Creatinine clearance values often are ‘normalized’ to the external body surface area (BSA) for an average person (1.73 m2) to account for variations in muscle mass (pediatric, obese) CrCl x 1.73 m2 BSA (textbook, appendix A) f. Normal CrCl: (textbook, pg 89, table 5-3) g. Calculate the CrCl and corrected CrCl given the following data: Urine creatinine (U) Plasma creatinine (P) Urine volume (V) Patient height: Patient weight: CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 185 mg/dl 0.9 mg/dl 1250 ml/24 hr 6’0” 260 lb Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 9 5. C. Measurement of GFR is not a useful indicator of early renal disease. a. Large margin of reserve in renal function b. Over two thirds of the GFR may be lost before clinical symptoms and biochemical abnormalities appear Renal Blood Flow (RBF) and Tubular Secretion Tests 1. Abnormal renal function may be caused by a. Impaired secretory ability of the tubules b. Decreased renal blood flow (RBF) 2. Tubular secretory function must be normal to provide valid renal plasma flow (RPF) test results RPF must be normal to validly evaluate tubular secretory function. 3. Standard test used is the CLEARANCE TEST. Ideal clearance substance to be measured must: a. Reside exclusively in plasma portion of blood b. Not be filtered by the glomerulus c. Be completely removed from the plasma on the first pass through the kidney, resulting in zero concentration in the venous renal blood 4. Clearance tests using p-aminohippurate (PAH) and phenolsulfonphthalein (PSP) are used to assess renal tubular secretory function. PAH and PSP are exogenous substances that must be infused into the patient and therefore these techniques are not routinely performed. 5. The most common test used to measure renal plasma flow (RPF) is the p-aminohippurate (PAH) clearance test. CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 10 URINE FORMATION IN THE NEPHRON PORTION OF THE NEPHRON ACTIVITY Glomerulus ultrafiltration Proximal Convoluted Tubule (PCT) reabsorption: sodium, chloride, H2O, amino acids, bicarbonate, glucose, uric acid, potassium, urea secretion: hydrogen ions, ammonia, protein-bound drugs, sulfates Loop of Henle reabsorption: sodium, chloride, H2O secretion: hydrogen ion Counter-current mechanism establishes hypertonic interstitium of medulla and papillae Distal Convoluted Tubule (DCT) reabsorption: sodium, chloride, H2O, bicarbonate, potassium secretion: potassium, ammonia, hydrogen ions, bicarbonate Requires ADH Collecting Ducts reabsorption: sodium, H2O, urea secretion: hydrogen ions Requires ADH CLS 426 Urine and Body Fluid Analysis UNMC: Student Lab Rotation 2006-2007 Unit: Urinalysis Module: Renal Physiology and Function (Lecture) 11