Congenital Abnormalities - University of Texas Medical Branch
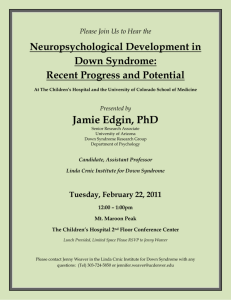
advertisement

Common Otolaryngological Congenital Abnormalities Visual Synopsis of Classic Syndromes and Features http://www.explosm.net/comics Viet Pham, M.D. Lewis Hutchinson, M.D. Harold Pine, M.D. Shraddha Mukerji, M.D. University of Texas Medical Branch Grand Rounds Presentations November 22, 2010 Foreword and Acknowledgements Special appreciation to Dr. Hutchinson for his assistance and contribution Additional gratitude to Drs. Pine and Mukerji All clinical photos are presented solely for educational purposes All other photos were obtained via a Google search http://www.explosm.net/comics unless otherwise specified and are used without permission Objective Highlight typical features of congenital abnormalities evaluated in the otolaryngology practice Visual emphasis on classical presentation of commonly encountered syndromes Down Syndrome (Trisomy 21) Extra chromosome 21 Meiotic nondisjunction in gamete formation Mosaicism (1-2%) Robertsonian translocation (2-3%) Duplication (rare) Increased risk with advanced maternal age Most common cause of intellectual disability Down Syndrome Features Brachycephaly Flat nasal bridge and occiput Small, low-set ears Macroglossia, glossoptosis Upslanting palpebral fissures Epicanthal folds Brushfield spots Simian crease Sandal gap deformity of feet Excessive nuchal folds Mental retardation (courtesy of Dr. Hutchinson via Maria Blazo, M.D.) Down Syndrome Features (Dourmishev, 2009) Brachycephaly Brushfield spots Macroglossia, glossoptosis Epicanthus Flat nasal bridge, hypoplastic maxilla (Dourmishev, 2009) Microtic, low-set ears (Dourmishev, 2009) Upslanting palpebral fissure Sandal deformity Simian crease Excessive nuchal folds Down Syndrome Other Features Muscular hypotonia Strabismus Congenital cataracts Atrial or ventricular septal defect Gastroesophageal reflux Duodenal stenosis or atresia Hirschsprung disease or celiac disease Seizures Down Syndrome Prenatal Ultrasound Absent nasal bones First trimester (60-80%) Second trimester (37-41%) Hypoplastic nasal bones Not useful as single marker in first trimester Best used with absent nasal bones in second trimester (60-100%) (Gonçalves, 2004) Down Syndrome Otolaryngological Considerations Tympanostomy tubes Esophageal atresia, tracheoesophageal fistula Atlantoaxial instability Obstructive sleep apnea Hypothyroidism Increased risk for malignancy Acute lymphoblastic leukemia Transient myeloproliferative disorder Crouzon Syndrome (Craniofacial Dysostosis) Autosomal dominant Virtually complete penetrance Mutation of fibroblast growth factor receptor II (FGFR2) on chromosome 10 Affects first pharyngeal arch Precursor maxilla and mandible Early fusion of face and skull bones (courtesy of Dr. Pine) Crouzon Syndrome (Jackson, 2009) Features Craniosynostosis Exophthalmos Hypertelorism Strabismus Psittichorhina Hypoplastic maxilla Mandibular prognathism Caused by a mutation in the fibroblast growth factor receptor II, located on chromosome 10 this syndrome affects the first branchial (or pharyngeal) arch, which is the precursor of the maxilla and mandible What occurs in the disease is that an infant's skull and facial bones, while in development, fuse early or are unable to expand. Thus, normal bone growth cannot occur. Fusion of different sutures leads to different patterns of growth of the skull. hypoplastic maxilla: insufficient growth of the midface mandibular prognathism: chin appears to protrude despite normal growth of mandible and gives the effect of the patient having a concave face Mental retardation possible if premature closure of the cranial suture lines Psittichorhina: beak-like nose Crouzon Syndrome Features Strabismus Exophthalmos Hypertelorism (Jackson, 2009) Cranial synostosis Mandibular prognathism Psittichorhina Hypoplastic maxilla Crouzon Syndrome Otolaryngological Considerations Hearing loss in 1/3 of cases Auricular misalignment Ossicular fixation Serous otitis media Sensorineural and mixed hearing losses Surgical craniofacial reconstruction (http://candar.wordpress.com) Crouzon Syndrome Otolaryngological Considerations Surgical craniofacial reconstruction (Jackson, 2009) Apert Syndrome (Acrocephalosyndactyly) Autosomal dominant Craniofacial abnormalities by FGFR2 mutations Syndactyly by keratinocyte growth factor receptor (KGFR) mutations Parents pass on to offspring 50% of the time Sporadic mutation in 98% Affects first pharyngeal arch (Shah AR, Danahey DG. Distraction Osteogenesis of the Maxilla. eMedicine 11 Feb 2009.) Apert Syndrome Craniofacial dysostosis Hypoplastic maxilla Frontal prominence Syndactyly Exophthalmos Hypertelorism Saddle nose, depressed nasal bridge Oral cavity High-arched palate, cleft palate Dental abnormalities (courtesy of Dr. Hutchinson) Features Apert Syndrome (Chen, 2009) Features Craniofacial dysostosis Syndactyly Frontal prominence Malocclusion Ectopic eruption Depressed nasal bridge Hypoplastic maxilla Hypertelorism Apert Syndrome Dr. Hutchinson’s mnemonic Apert = Crouzon + Syndactyly Apert Syndrome Otolaryngological Considerations Conductive hearing loss Chronic otitis media Stapes fixation Patent cochlear aqueduct Surgical craniofacial reconstruction (Jackson, 2009) Treacher Collins Syndrome (Mandibulofacial Dysostosis) Also known as Franceschetti-Zwahlen-Klein syndrome Autosomal dominant TCOF1 gene on chromosome 5q New mutation in up to 60% Complete penetrance, variable expression First and second pharyngeal arches, grooves, and pouches Treacher Collins Syndrome Features Characteristic facial dysmorphia Downward slanting palpebral fissures Hypoplastic supraorbital rims Malar hypoplasia Mandibular hypoplasia Auricular and middle ear malformations Lower eyelid coloboma May have cleft palate Normal intelligence (Tolarova, 2009) Treacher Collins Syndrome Features Malar hypoplasia Lower eyelid colobomas Hypoplastic supraorbital rims (courtesy of Dr. Hutchinson) Downward slanting palpebral fissures Mandibular hypoplasia Auricular malformation Treacher Collins Syndrome Features Malar hypoplasia Lower eyelid colobomas Hypoplastic supraorbital rims Scant lower eyelashes Mandibular hypoplasia Auricular malformation (courtesy of Dr. Hutchinson) Downward slanting palpebral fissures Treacher Collins Syndrome Otolaryngological Considerations Hearing Conductive hearing loss in 30% Ossicular malformation Microtia and/or canal atresia Mastoid hypoplasia Some sensorineural hearing loss and vestibular dysfunction Upper airway obstruction (Tolarova, 2009) Treacher Collins Syndrome Otolaryngological Considerations Surgical craniofacial reconstruction (Jackson, 2009) Goldenhar Syndrome Oculoauriculovertebral Dysplasia Diverse etiologies In utero vascular disruption with hematoma Disturbed neural crest cells at 30-45 days gestation No single genetic locus First and second branchial arch Hemifacial microsomia when no internal organ or vertebral disruption Goldenhar Syndrome Features Hemifacial microsomia Mandibular hypoplasia Microstomia Epibulbar lipodermoids Upper eyelid coloboma Vertebral anomalies (Bailey, 2006) Goldenhar Syndrome Features Mandibular hypoplasia Hemifacial microsomia Microtia and preauricular tags/pits Upper eyelid coloboma Epibulbar dermoid Goldenhar Syndrome Classification Scheme OMENS Orbital distortion Mandibular hypoplasia Ear anomaly Nerve (facial) involvement Soft-tissue deficiency “Plus” to include additional anomalies Cardiac Skeletal, limb Pulmonary Renal Gastrointestinal Anderson PJ, David DJ. Spinal anomalies in Goldenhar syndrome. Cleft Palate-Craniofacial Journal 2005; 42:477-80. Goldenhar Syndrome Classification Scheme: Mandible (Horgan, 1995) Normal mandible Goldenhar Syndrome Classification Scheme: Mandible (Horgan, 1995) Type I Smaller mandible but identifiable mandible Goldenhar Syndrome Classification Scheme: Mandible (Horgan, 1995) Type II Functioning temporomandibular joint (TMJ) but abnormal shape and glenoid fossa Type IIA Glenoid fossa is in an acceptable position Goldenhar Syndrome Classification Scheme: Mandible (Horgan, 1995) Type II Functioning temporomandibular joint (TMJ) but abnormal shape and glenoid fossa Type IIB Abnormally placed TMJ cannot be incorporated into surgical reconstruction Goldenhar Syndrome Classification Scheme: Mandible (Horgan, 1995) Type III Absent ramus and nonexistent glenoid fossa Goldenhar Syndrome Classification Scheme Orbits Ear (Horgan, 1995) Goldenhar Syndrome Classification Scheme Facial Nerve Soft tissue defect (Horgan, 1995) Goldenhar Syndrome Otolaryngological Considerations Hearing loss More conductive than sensorineural Ossicular abnormalities Microtia Aberrant facial nerve course Surgical craniofacial reconstruction Pierre Robin Syndrome Sequence of micrognathia, glossoptosis, and cleft palate Syndrome reserved for multiple malformations by a single etiology Confusing classification, up to 14 definitions (Breugem 2009) Possibly due to arrested intrauterine development Mechanical Neurological Ontogenesis (Tolarova, 2009) Pierre Robin Syndrome (courtesy of Dr. Hutchinson) Features Cleft palate Glossoptosis Retrognathia Macroglossia and ankloglossia uncommon (Jackson, 2009) Micrognathia (courtesy of Dr. Hutchinson) Pierre Robin Syndrome Sequence Mandibular hypoplasia Between 7-11 weeks gestation Mandible gets temporarily “stuck” between clavicle and sternum Oligohydramnios Tongue remains high in oral cavity Cleft palate results from failed closure of palatal shelves U-shaped cleft palate (80%), can have V-shaped (20%) Typically no cleft lip Pierre Robin Syndrome Otolaryngological Considerations Airway compromise Upper airway obstruction Feeding, aspiration Subglottic stenosis Hearing loss Otitis media most common (60%) Auricular malformation Mixed hearing loss Associated syndromes Stickler (18-25%) Velocardiofacial (7-15%) Treacher Collins (5%) Hemifacial microsomia (3%) Mandibular “catch up” if isolated sequence (Tolarova, 2009) Pierre Robin Syndrome Otolaryngological Considerations Distraction osteogenesis Intubation, tracheostomy (Tolarova, 2009) Cleft palate repair (courtesy of Dr. Hutchinson) Stickler Syndrome Autosomal dominant Mutations of type II and XI collagen COL2A1 gene on chromosome 12 COL11A1 and COL11A2 genes on chromosome 6 COL9A1 is rare recessive variant Craniofacial, ocular, and arthopathic features Stickler Syndrome “Flattened” face Ocular findings Musculoskeletal abnormalities Cleft palate (courtesy of Dr. Hutchinson via Maria Blazo, M.D.) Features Stickler Syndrome Features Midfacial hypoplasia Short upturned nose Long philtrum (Tolarova, 2009) (Poulson, 2004) Micrognathia Stickler Syndrome Features Ocular Myopia Glaucoma Retinal detachment Cataracts Musculoskeletal Osteoarthritis Joint hypermobility Abnormal epiphyseal development Vertebral abnormalities Scoliosis Stickler Syndrome Otolaryngological Considerations Hearing loss Mild to moderate sensorineural hearing loss (SNHL) in 80% Significant SNHL or mixed hearing loss in 15% Conductive component secondary to eustachian tube dysfunction from cleft palate Ossicular abnormalities may be present Pierre Robin sequence Present in 25% of Stickler syndrome Cleft palate Micrognathia (courtesy of Dr. Hutchinson via Maria Blazo, M.D.) Waardenburg Syndrome Autosomal dominant Multiple genes PAX3 (Types 1 and 3) MITF, SNAI2 (Type 2) EDN3, EDNRB, SOX10 (Type 4) Autosomal recessive for Type 4 Variable penetrance Hearing loss Dystopia canthorum Pigmentary abnormalities (courtesy of Dr. Hutchinson) Waardenburg Syndrome Features Dystopia canthorum Flat nasal root Hypoplastic nasal alae Synophyrs Heterochromia irides Isohypochromia irides White forelock Vitiligo Cleft lip and palate (10%) (Schwartz, 2010) Waardenburg Syndrome (courtesy of Dr. Hutchinson) Features White forelock Synophyrs Hypoplastic alae Short philtrum Heterochromia irides Flat nasal root Dystopia canthorum Isohypochromia irides (Schwartz, 2010) Waardenburg Syndrome Features Major Heterochromia irides White forelock Dystopia canthorum Congenital sensorineural hearing loss Affected first-degree relative Minor Congenital leucoderma Synophyrs Broad high nasal root Hypoplastic nasal alae Premature graying hair Waardenburg Syndrome Diagnosis Major Heterochromia irides White forelock Dystopia canthorum Diagnosis Congenital sensorineural 2 major features hearing loss 1 major features + Affected first-degree relative Minor Congenital leucoderma Synophyrs Broad high nasal root Hypoplastic nasal alae Premature graying hair 2 minor features Waardenburg Syndrome Subtypes Type 1 Type 2 No dystopia canthorum, white forelock less common Sensorineural hearing loss, heterochomia irides Type 3 (Klein-Waardenburg syndrome) Full symptomatology Facial asymmetry, dysmorphic facies Similar to Type 1 but with skeletal anomalies and mental retardation Rib aplasia, cystic sacrum, cutaneous syndactyly Type 4 (Shah-Waardenburg syndrome) Association with Hirschsprung disease (courtesy of Dr. Hutchinson) (Schwartz, 2010) Waardenburg Syndrome Subtypes Type 1 Type 2 No dystopia canthorum, white forelock less common Sensorineural hearing loss, heterochomia irides Type 3 (Klein-Waardenburg syndrome) Full symptomatology Facial asymmetry, abnormal facies Similar to Type 1 but with skeletal anomalies and mental retardation Rib aplasia, cystic sacrum, cutaneous syndactyly Type 4 (Shah-Waardenburg syndrome) Association with Hirschsprung disease (courtesy of Dr. Hutchinson) Waardenburg Syndrome Subtypes Type 1 Type 2 No dystopia canthorum, white forelock less common Sensorineural hearing loss, heterochomia irides Type 3 (Klein-Waardenburg syndrome) Full symptomatology Facial asymmetry, abnormal facies Similar to Type 1 but with skeletal anomalies and mental retardation Rib aplasia, amyoplasia, cystic sacrum, cutaneous syndactyly Type 4 (Shah-Waardenburg syndrome) Association with Hirschsprung disease Waardenburg Syndrome Subtypes Type 1 Type 2 No dystopia canthorum, white forelock less common Sensorineural hearing loss, heterochomia irides Type 3 (Klein-Waardenburg syndrome) Full symptomatology Facial asymmetry, abnormal facies Similar to Type 1 but with skeletal anomalies and mental retardation Rib aplasia, cystic sacrum, cutaneous syndactyly Type 4 (Shah-Waardenburg syndrome) Association with Hirschsprung disease Waardenburg Syndrome Otolaryngological Considerations Congenital sensorineural deafness Typically not progressive Hearing amplification Cochlear implantation Cleft lip or palate repair Cosmetic considerations Beckwith-Wiedemann Syndrome Imprinting defect at chromosome 11p15 Most cases are sporadic Autosomal dominant familial inheritance in 15% Most common overgrowth syndrome in infancy Five common features Macroglossia Macrosomia Midline abdominal wall defect Ear pits/creases Neonatal hypoglycemia (courtesy of Dr. Hutchinson) Beckwith-Wiedemann Syndrome Imprinting defect at chromosome 11p15 Most cases are sporadic Autosomal dominant familial inheritance in 15% Most common overgrowth syndrome in infancy Five common features Macroglossia Macrosomia Midline abdominal wall defect Ear pits/creases Neonatal hypoglycemia Beckwith-Wiedemann Features Macrosomia Midline abdominal defect (courtesy of Dr. Hutchinson via Maria Blazo, M.D.) Macroglossia Ear pits/creases Beckwith-Wiedemann Features Major Midline abdominal defect Macroglossia Macrosomia Ear pits/creases Adrenocortical cytomegaly Renal abnormalities Embryonal tumors Cleft palate (rare) Hemihyperplasia Beckwith-Wiedemann Features Major Midline abdominal defect Macroglossia Macrosomia Ear pits/creases Adrenocortical cytomegaly Renal abnormalities Embryonal tumors Cleft palate (rare) Hemihyperplasia Minor Neonatal hypoglycemia Polyhydramnios Prematurity Facial nevus flammeus Hemangioma Characteristic facies (i.e. midface hypoplasia) Cardiac anomalies Diastasis recti Advanced bone age Beckwith-Wiedemann Diagnosis Major Minor Midline abdominal defect Neonatal hypoglycemia Macroglossia Polyhydramnios Macrosomia Prematurity Diagnosis Ear pits/creases Facial nevus flammeus At least 2 common features Adrenocortical cytomegaly Hemangioma 3 major features Renal abnormalities Characteristic facies (i.e. 2 major features midface hypoplasia) Embryonal tumorsfeatures + 3 minor Cardiac anomalies Cleft palate (rare) Diastasis recti Hemihyperplasia Advanced bone age Beckwith-Wiedemann Otolaryngological Considerations Macroglossia Airway obstruction, feeding difficulty Less noticeable with age Increased risk of malignancy Wilms’ tumor Hepatoblastoma Surveillance Abdominal ultrasound every 3 months until 8 years Alpha-fetoprotein every 6 weeks until 4 years Neurofibromatosis Type 1 (von Recklinghausen) Peripheral neurofibromatosis Autosomal dominant Neurofibromin gene (NF1) on chromosome 17 Half result from de novo mutation Variable expression Better prognosis than Neurofibromatosis Type 2 (courtesy of Dr. Hutchinson via Maria Blazo, M.D.) (Dahl, 2010) Neurofibromatosis, Type 1 Features Café au lait spots Cutaneous neurofibromas Plexiform neuromas Lisch nodules Axillary or perineum freckling (Crowe sign) Optic gliomas Bone abnormalities Neurofibromatosis, Type 1 Features Café au lait spots Plexiform neuroma Axillary freckling (Dahl, 2010) (courtesy of Dr. Hutchinson via Maria Blazo, M.D.) Cutaneous neurofibomas Optic glioma Lisch nodules Long bone bowing Neurofibromatosis, Type 1 Diagnosis Six or more café au lait macules Diameter larger than 5mm in prepubescent Diameter larger than 15mm in adults Two or more neurofibromas or one plexiform neurofibroma Axillary or inguinal freckling Optic glioma Two or more Lisch nodules Distinctive osseous lesion First-degree relative with condition (Nazareth, 2010) Neurofibromatosis Type 2 Central neurofibromatosis Autosomal dominant NF2 (Merlin) gene on chromosome 22 Approximately 10% of all individuals with neurofibromatosis Significant morbidity, decreased lifespan Paucity of café au lait spots and Crowe sign (Pletcher, 2010) Café au lait spots Schwannomas Bilateral acoustic neuromas Spinal cord Nonvestibular Subcapsular cataracts Meningiomas Kutz JW Jr, Roland PS, Isaacson B. Skull base, acoustic neuroma (vestibular schwannoma): multimedia. eMedicine 24 Sep 2009. Accessed 5 Nov 2010 <http://emedicine.medscape.com/article/882876-media>. Neurofibromatosis, Type 2 Features Neurofibromatosis, Type 2 Diagnosis Bilateral vestibular schwannomas Presumptive Suggestive Affected first-degree relative Unilateral vestibular schwannoma Or two of the following: Meningioma Glioma Schwannoma Juvenile posterior subcapsular or cortical cataract Unilateral vestibular schwannoma Two of the following: Meningioma Glioma Schwannoma Juvenile posterior subcapsular or cortical cataract Or multiple meningiomas Klippel-Feil Syndrome (Brevicollis, Wildervanck) Cervical vertebral fusion Type I – single level Type II – multiple, noncontiguous segments Type III – multiple, contiguous segments Short, webbed neck and low hairline Unclear etiology Associated abnormalities Sprengel deformity Scoliosis Facial asymmetry Renal abnormalities (Sullivan, 2009) Other Syndromes Without Craniofacial Features Usher Hearing loss with defective inner ear Type I – deafness and vestibular dysfunction Type II – nonprogressive hearing loss and normal vestibular function Type III – progressive hearing loss and half vestibular function Progressive vision loss from retinitis pigmentosa Pendred Yeah Yeah Yeah Sensorineural hearing loss Thyroid goiter Jervell and Lange-Neilsen Defective potassium channel from KCNQ1 and KCNE1 mutations Sensorineural hearing loss and palpitations (long QT syndrome) Conclusion Many syndromes will present to the otolaryngologist Warrant otolaryngological intervention Attention to coexisting conditions Many affected individuals are aware of the social stigma related to their condition http://www.explosm.net/comics References Admiraal RJ, et al. Hearing impairment in Stickler syndrome. Adv Otorhinolaryngol 2002; 61:216-23. Bailey BJ, Johnson JT, Newlands SD, eds. Head and Neck Surgery – Otolaryngology, 4th Ed. Philadelphia: Lippincott, 2006. pp 1311-2,1380-6,2794. Breugem CC, Courtemanche DJ. Robin sequence: clearing nosologic confusion. Cleft Palate Craniofac J 2010; 47:197-200. Chen H. Apert syndrome. eMedicine 2 Sep 2009. Accessed 12 Oct 2010 <http://emedicine.medscape.com/article/941723-overview>. Chen H. Crouzon syndrome. eMedicine 10 Sep 2009. Accessed 12 Oct 2010 <http://emedicine.medscape.com/article/942989-overview>. Chen H. Down syndrome. eMedicine 22 Mar 2010. Accessed 31 Oct 2010 <http://emedicine.medscape.com/article/943216-overview>. Crawford AH, Schorry EK. Neurofibromatosis update. J Pediatr Orthop 2006; 26:413-23. Dahl AA, Grostern RJ. Neurofibromatosis-1. eMedicine 21 May 2010. Accessed 5 Nov 2010 <http://emedicine.medscape.com/article/1219222-overview>. DeBaun MR, et al. Epigenetic alterations of H19 and LIT1 distinguish patients with Beckwith-Wiedemann syndrome with cancer and birth defects. Am J Hum Genet 2002; 70:604-11. DeBaun MR, Tucker MA. Risk of cancer during the first four years of life in children from The Beckwith Wiedemann Syndrome Registry. J Pediatr 1998; 132:398-400. DeBella K, Szudek J, Friedman JM. Use of the national institutes of health criteria for diagnosis of neurofibromatosis 1 in children. Pediatrics 2000; 105(3 Pt 1):608-14. References Dourmishev AL, Janniger CK. Down syndrome. eMedicine 1 Jul 2009. Accessed 4 Nov 2010 <http://emedicine.medscape.com/article/1113071-overview>. Dourmishev LA, Janniger CK. Waardenburg syndrome. eMedicine 2 Jun 2009. Accessed 30 Oct 2010 <http://emedicine.medscape.com/article/1113314-overview>. Elliott M, et al. Clinical features and natural history of Beckwith-Wiedemann syndrome: presentation of 74 new cases. Clinical Genetics 1994; 46:168-74. Farrer LA, et al. Waardenburg syndrome (WS) type I is caused by defects at multiple loci, one of which is near ALPP on chromosome 2: first report of the WS consortium. Am J Hum Genet 1992; 50:902-13. Ferry RJ. Beckwith-Wiedemann syndrome. eMedicine 15 Apr 2010. Accessed 23 Oct 2010 <http://emedicine.medscape.com/article/919477-overview>. Flint PW, et al, eds. Cummings Otolaryngology: Head and Neck Surgery, 5th Ed. Philadelphia: Mosby Elsevier, 2010. ch 147, 184. Gould HJ, Caldarelli DD. Hearing and otopathology in Apert syndrome. Archives of Otolaryngology 1982; 108:347-9. Gonçalves LF, Espinoza J, Lee W, et al. Phenotypic characteristics of absent and hypoplastic nasal bones in fetuses with Down syndrome: description by 3-dimensional ultrasonography and clinical significance. J Ultrasound Med 2004; 23:1619-27. Handzic J, et al. Hearing levels in Pierre Robin syndrome. Cleft Palate Craniofac J 1995; 32:30-6. Hata T, Todd MM. Cervical spine considerationswhen anesthesizing patients with Down syndrome. Anesthesiology 2005; 102:680-5. References Heike CL, Hing AV. Craniofacial microsomia review. Gene Review. Eds. Pagon RA, et al. 19 Mar 2009. Accessed 23 Oct 2010 <http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=m-hfm-ov>. Horgan JE, et al. OMENS-plus: analysis of craniofacial and extracraniofacial anomalies in hemifacial microsomia. Cleft Palate Craniofac J 1995; 32:405-12. Jackson IT, Malhotra G. Congenital syndromes. eMedicine 2 Jul 2009. Accessed 12 Oct 2010 <http://emedicine.medscape.com/article/1280034-overview>. Jakobsen LP, et al. The genetic basis of the Pierre Robin Sequence. Cleft Palate Craniofac J 2006; 43:155-9. Lee KJ, ed. Essential Otolaryngology – Head and Neck Surgery, 9th Ed. New York: McGraw Hill, 2008. pp 139-59. Liu XZ, Newton VE, Read AP. Waardenburg syndrome type II: phenotypic findings and diagnostic criteria. Am J Med Genet 1995; 55:95-100. Nazareth MR, Helm TN. Neurofibromatosis. eMedicine 16 Jun 2010. Accessed 5 Nov 2010 <http://emedicine.medscape.com/article/1112001-overview>. Nowak CB. Genetics and hearing loss: a review of Stickler syndrome. J Commun Disord 1998; 31:437-54. Orvidas LJ, et al. Hearing and otopathology in Crouzon syndrome. Layrngoscope 1999; 109:1372-5. Peterson-Falzone SJ, Hardin-Jones MA, Karnell MP. Cleft Palate Speech, 4th Ed. St. Louis: Mosby, 2010. Pletcher BA. Neurofibromatosis, type 2. eMedicine 3 Mar 2010. Accessed 5 Nov 2010 <http://emedicine.medscape.com/article/1178283-overview>. Poulson AV, et al. Clinical features of type 2 Stickler syndrome. J Med Genet 2004; 41:e107. References Pron G, et al. Ear malformation and hearing loss in patients with Treacher Collins syndrome. Cleft Palate Craniofac J 1993; 30:97-103. Robin NH, Falk MJ, Haldeman-Englert CR. FGFR-related craniosynostosis syndromes. Gene Review. Eds. Pagon RA, et al. 27 Sept 2007. Accessed 19 Oct 2010 <http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=craniosynostosis>. Saenz RB. Primary care of infants and young children with Down syndrome. Am Fam Physician 1999; 59:38190,392,395-6. Samartzis DD, Herman J, Lubicky JP. Classification of congenitally fused cervical patterns in Klippel-Feil patients: epidemiology and role in the development of cervical spine-related symptoms. Spine 2006; 31:F798-804. Samartzis D, Lubicky JP, Herman J. Symptomatic cervical disc herniation in a pediatric Klippel-Feil patient: the risk of neural injury associated with extensive congenitally fused vertebrae and a hypermobile segment. Spine 2006; 31:F335-8. Sangkhathat S, et al. Novel mutation of Endothelin-B receptor gene in Waardenburg-Hirschsprung disease. Pediatr Surg Int 2005; 21:960-3. Schwartz RA, Jozwiak S, Krantz I. Waardenburg syndrome. eMedicine 4 Jun 2010. Accessed 24 Oct 2010 <http://emedicine.medscape.com/article/950277-overview>. Spivey PS, Bradshaw WT. Recognition and management of the infant with Beckwith-Wiedemann syndrome. Adv Neonatal Care 2009; 9:279-84. Sullivan AJ. Klippel-Feil syndrome. eMedicine 23 Jun 2009. Accessed 5 Nov 2010 <http://emedicine.medscape.net/article/1264848-diagnosis>. References Tewfik TL, Trinh N, Teebi AS. Pierre Robin Syndrome. eMedicine 4 Mar 2010. Accessed 21 Oct 2010 <http://emedicine.medscape.com/article/844143-overview>. Tolarova MM. Pierre Robin Malformation. eMedicine 25 Mar 2009. Accessed 21 Oct 2010 <http://emedicine.medscape.com/article/995706-overview>. Tolarova MM, Wong GB, Varma S. Mandibulofacial dysostosis. eMedicine 24 Nov 2009. Accessed 17 Oct 2010 <http://emedicine.medscape.com/article/946143-overview>. Verheij JB, et al. Shah-Waardenburg syndrome and PCWH associated with SOX10 mutations: a case report and review of the literature. Eur J Paediatr Neurol 2006; 10:11-7. Watanabe A, et al. Epistatic relationship between Waardenburg syndrome genes MITF and PAX3. Nat Genet 1998; 18:283-6.