diagnosis of multiple pregnancy
advertisement
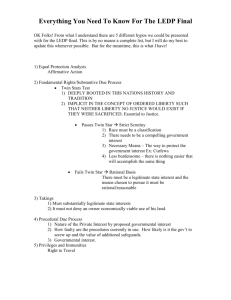
Dr. Sharifa Al Sibiani MULTIPLE PREGNANCY Introduction: Multiple pregnancy is a complicated pregnancy associated with high risk of mortality and morbidity for both mother and fetus. Types: 1. Twins Monozygotic Diazygotic 2. Triplets 3. Quadruplets 4. Etc. TWIN PREGNANCY TYPES: 1. Monozygotic 2. Diazygotic INCIDENCE: Twin Diazygotic 1.80 in UK Higher multiples follow Hellin’s Law Triplets = 802 Quadruplet = 803 Monozygotic : relatively constant world wide 1.250 birth independent of associated factors. Incidence of diazygotic twin is influenced largely by: Race (Negro > White) Hereditary (maternal side) Maternal age (> 35 years) Maternal size of length (large and tall > small and short) Parity (mulliparous > nulliparous) Fertility drugs (injection > oral) Soon after stop long term OCP (Rebound birth secretion) Blood group A & O ? unknown 1 Dr. Sharifa Al Sibiani Genesis of Twinning 1. Diazygotic (biovulular, fraternal, non-identical) twin Two separate ova fertilized by two different sperms 2. Monozygotic (monovular, indentical) twin One ovum fertilized by one sperm If division occurs within 5 days i.e. at two cell stage (before the inner mass formation) Two embryo, two amnions and two chorions Diamniotic dichorionic (30% of twins) Between (5 – 10 days) after fertilization i.e. at blastocyst stage (after the inner mass formation) Two embryo, two amnion and one chorion Diamniotic monochorionic Monochorionic (70% of twins) About (10 to 14th day) after fertilization (After amnion and chorion formation) Two embryo, one amnion and one chorion Monoamniotic monochorionic (1% of twins) Later (? 14 days) after embryonic disk formation, cleavage is incomplete (conjoined twins) (1% of monozygotic twins) 2 Dr. Sharifa Al Sibiani DIAGNOSIS OF MULTIPLE PREGNANCY I – History FH + ve Past History Fertility drugs Excessive vomiting in early pregnancy II – Examination Bigger uterus Two separate fetal heart at 18-20 weeks After 30 – 32 weeks 3 fetal pole may be identified (two head and one breech) III – Investigations 1. Ultrasound - > 80% of twins are diagnosed before labour (10% of multiple pregnancy are missed) 2 x gestational sac 6 – 7 weeks scan 2 x embryos 7 – 8 weeks scan A definitive diagnosis at 16 weeks scan As commonly one pair twin diagnosed early doesn’t develop and observed later (vanishing twin) AS number of fetuses ↑ → ↑ accuracy of diagnosis of number of fetuses. 2. Biochemical test Higher hormones of pregnancy HCP, PL, α FP, PP But there is no biochemical test will differentiate clearly between one and more than one fetus. 3 Dr. Sharifa Al Sibiani COMPLICATIONS Most pregnancy related problems are common and more severe. These cause high morbidity and mortality to both mother and fetus. I - FETAL COMPLICATIONS I – ANTEPARTUM 1. Risk of spontaneous abortion 2x as singleton pregnancy Vanishing twin Only 50 % of twins diagnosed by early ultrasound continue to delivery 2. Preterm Labour Over all twins account for about 10% of all prematurity 20 – 50% of multiple pregnancies don’t reach 37th week In general as the number of fetuses ↑ -> the duration of pregnancy ↓ (singleton 280 days (40 weeks), twin 260 days (37 weeks) triplet 247 days (35 weeks) Prematurity is the most important factor in increasing prenatal mortality and morbidity. 3. Growth retardation 50% of all twins weight < 2500 grams In general, the larger number of fetuses the greater degree of growth retardation More in monozygotic Discordant twins - IUGR of one of fetuses - > 25 % difference in weight Weight difference = 250 grams U/S difference BPD = 5 mm, HC = 5%, AC = 20 mm - 15 – 30% of twin pregnancy - Cause higher perinatal mortality - Cause by placental insufficiency Twin – twin transfusion 4. Congenital anomalies - Major and minor malformation x 2 as singleton (major = 1% in singleton 2% in twin) - More in monozygotic twins 5. Increased Perinatal Mortality - 2 x more than singletons (10 – 15% most report) - More neonatal mortality > still birth (due to prematurity) - Monozygotic > diazygotic 4 Dr. Sharifa Al Sibiani - More in monozygotic (intertwining of cord) - Causes – Mainly prematurity Other - Congenital malformation - IUGR - Twin – twin transfusion - Birth trauma or hypexia 6. Twin – twin transfusion Syndrome (Fetal – fetal haemorrhage) - Limited to those with monochorial placenta - 15% of monozygotic twin Results when one placental cotyledon is fed by artery from the first twin and drained by a vein that lead to the second twin . - C/F varies (mild-moderate-severe) - Full blown picture Hyperfused Twin ----→ Polycylthemic, ↑ BP, Cardiac hypertrophied, Oedema, polyhydramnios Hypoperfused Twin ---→Anaemic, ↓BP, IUGR, Oligohydraminase The hallmark is rapid polyhydraminase and discordant fetal growth. PMR close to100% if develop before 26 weeks. If one fetus dies, usually the recipient from CHF & hydrops. This can cause a consumption coagulopathy or emboli to the remaining twin. Management: “Depend as gestational age and severity” Daily F.M. chart and CTG Weekly ultrasound + BPD ↓ Polyhydramnios by : Therapeutic amniocentesis : PG synthetase inhibitors (indomethacin) Abnormal CTG stop Rx delivery : C/S if fetal hydrops develops Laser photocoagulation of the placental vessels 7. The antepartum death of one twin (single fetal demise in uterus) Can occur at any trimester (1st, 2nd, 3rd) Frequency : varies Monozygotic at highest risk Theoretically maternal coagulopathy could be trigged (> 5 weeks after fetal death) Hypofibronogenema, DIC (rare) Neonatal morbidity or mortality higher in the remaining twin (from emboli) 5 Dr. Sharifa Al Sibiani Management” “ Conservative with frequent antenatal surveillance of the living fetus” Maternal coagulation check up weekly Serial ultrasound – to evaluate growth . A.F., placental grade CTG + BPD Delivery for the usual obstetric indication II - MATERNAL COMPLICATIONS 1. PIH - 3-5 singleton - earlier and more severe as compared with singleton - equal frequency in mono and diazygotic twin 2. G.D.M. 3. Anemia – especially iron deficiency anemia (because of ↑ fetal iron requirement) Rarely megaloblastic anemia 4. Polyhydramnios 10 – 12% Can occur in one or both sacs More common un monozygotic (usually from twin – twin transfusion) 5. Risk of APH Placenta previa ? due to large placental surface Abruptio placentae may occur with sudden decompression of the uterus immediately after delivery of the first twin 6. Cord accidents (cord prolapse, entwinement, vasa previa) Cord prolapse may occur with malpresentation especially with 2nd twin at time when its membrane rupture. Cord entwining especially in monozygotic monoamniotic 7. In effective labour due to: Over distended uterus Malpresentation 8. Malpresentation Main factor leading to more frequent use of C/S in twin Cephalic – cephalic ---- 45 % Cephalic – breech ----- 24% 1st twin (leading twin) is cephalic in 80% Cephalic trans - ------ 10% Breech – cephalic ------ 10% Breech – breech ------ 10% 9. PPH Uterine atony (owing to inability of over distended uterus to contracted well) Operating delivery (instrumental or C/S) Placental accident (previa or abruption) 6 Dr. Sharifa Al Sibiani 10. High rate of operative delivery (instrumental or C/S) 11. Delay in delivery of twin II 12. Locked twins Very rare complication of twin delivery (1/800) May occur when first twin present as breech and second as cephalic Usually managed by C/S or decapitation head of first twin 13. High risk of birth asphyxia and neonatal depression, due to : Prematurity Malpresentation and cord accident Complicated delivery Operative delivery A.P.H. Management of multiple Pregnancy I. In pregnancy Proper antenatal care should be included: 1. Early diagnosis 2. Frequent antenatal visits At least every 2 weeks from 20 –30 weeks then weekly To allow prevention of possible or early detection and treatment of complication 3. Serial ultrasound for fetal growth to detect IUGR 4. Prevention (if possible) early detection and aggressive of preterm labour Bed rest Prophylactic beta symphathomometric drugs? Prophylactic cervical cerclage? 5. Screening 6. Additional calories (another 300 kcal / day) 7. Iron supplementation 60 – 100 mg / day + 1 mg folic acid 8. Regular B.P. monitoring 9. Hospitalization – routine admission at 26 – 30 weeks ? now not common If * any complication * CX is effused or dilated * The mother is tired 10. Watching and Rx of less complications as twin – twin transfusion II – Labour Twin Should be in well equipped hospital o Two obstetricians (one should be skilled in intrauterine manipulation) o Two Pediatricians (one should be expert in neonatal resuscitation) o Anesthesiology 7 Dr. Sharifa Al Sibiani The first stage Managed in the ordinary way with special care include. o NPO o IVF o Cross match at least two units of blood Continuous fetal monitoring o Ensure twin I is longitudinal o If twin I is transverse C/S o Check for cord prolapse when membrane rupture (Often early in labour) Insert internal fetal electrode o Progress is usually uneventful with monitor both externally after ROM one internal and other external Fetal hearts o If woman wants, an epidural anesthetic is useful for it allows any maneuvers that may be required for twin in the second stage. NB: Ceph I – ceph II – SVD Ceph I – breech II – SVD or CS Breech I – breech II – CS ?? SVD Second Stage o Episiotomy o Make sure that nobody give syntometrine after the delivery of the twin I o Clamp cord I and hand baby to Paediatrician o Immediately check lie of twin II abdominally and check presenting part vaginally If obligue or transverse make longitudinal external version or internal version NB: Twin II delivered within 20 minutes, usually start contracting again 5 minutes first delivery. If not IV oxytocin augmentation 3rd Stage o Give Syntometrine with delivery of twin II and continue Oxytocin infusion for another hour o Deliver placentae after delivery of twin II NB: PPH due to atony uterus or trained placenta is common II - Triplets or more CS 8