JAG/jme/Papers/Cervical ManagementGuidelines/updated 14
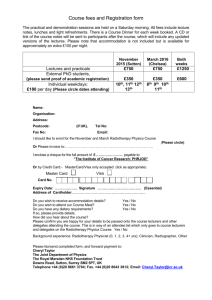
advertisement

Agreed 2009 Review in 2012 MEDICAL PROTOCOL ONCOLOGICAL MANAGEMENT OF CERVICAL CANCER These guidelines have been developed by members of the Gynaecological Oncology Guidelines Group, for approval by the Merseyside and Cheshire Gynaecological Cancer Network Group. 1. Background ........................................................................................................................................ 3 2. General Information .......................................................................................................................... 3 3. Prevention – Cervical Screening and Colposcopy .............................................................................. 4 4. Referral............................................................................................................................................... 5 Histological Types and Incidence ........................................................................................................ 5 5. Stage Information .............................................................................................................................. 6 6. Pre-Treatment Assessment ............................................................................................................... 6 Clinical Staging..................................................................................................................................... 6 Pre-operative imaging ......................................................................................................................... 7 7. Treatment overview .......................................................................................................................... 7 8. Management of Invasive Disease ...................................................................................................... 8 I. Superficially invasive cervical carcinoma (microinvasive carcinoma).............................................. 8 II. Stage IBI and stage 2A less than 4 cms ........................................................................................... 8 III. More advanced stage (1B2, bulky 2a and higher) and patients unsuitable for surgery irrespective of stage ............................................................................................................................ 9 9. Cervical adenocarcinomas ........................................................................................................... 9 10. Small cell cervical carcinomas (neurendocrine tumours, malignant carcinoids) ............................. 9 11. Incidental finding of invasive cancer of the cervix found after Simple Hysterectomy .................... 9 12. Radical Trachelectomy ................................................................................................................... 10 13. Relapse ........................................................................................................................................... 10 14. Adjuvant Surgery............................................................................................................................ 10 15. Radiotherapy or Surgery for Carcinoma of the Cervix ................................................................... 11 I. Stage 1a disease ............................................................................................................................. 11 II. Stage 1b1 and 2a disease (non bulky) ........................................................................................... 11 III. Bulky stage 1B and 2A disease and stages IIb – IVa ..................................................................... 12 1|P age Agreed 2009 Review in 2012 Squamous cell carcinoma (SCC) versus adenocarcinoma (ACC) ....................................................... 12 16. Chemotherapy and radiotherapy for cervical cancer ..................................................................... 12 I. Neoadjuvant chemotherapy .......................................................................................................... 12 II. Concurrent Chemoradiation ......................................................................................................... 12 III. Integrated chemotherapy ............................................................................................................ 13 17. Postoperative radiotherapy ........................................................................................................... 13 I. Patients with involved pelvic lymph nodes:................................................................................... 13 II. Postoperative radiotherapy for patients with involved resection margins after RH: .................. 13 III. Postoperative radiotherapy for high-risk node negative patients: ............................................. 14 IV. Postoperative radiotherapy for patients treated inadvertently with simple hysterectomy: ..... 14 Morbidity of combined treatment with RH and radiotherapy. ........................................................ 14 18. Extended field radiotherapy .......................................................................................................... 15 I. Prophylactic extended field radiotherapy: .................................................................................... 15 II. Irradiation of patients with known para-aortic nodal metastases: .............................................. 15 19. Radiotherapy for patients with isolated local failure in the pelvis after RH .................................. 16 20. Palliative radiotherapy ................................................................................................................... 16 21. Improving Effectiveness of Radiotherapy: Hb Levels .................................................................... 16 22. Chemotherapy for advanced or recurrent cervical cancer ............................................................ 17 23. Follow-Up ....................................................................................................................................... 20 24. Maintenance of Quality ................................................................................................................. 20 25. Audit and Clinical Outcome ....................................................................................................... 20 26. Clinical Trials ................................................................................................................................... 20 27. Palliative Care and Nursing care ..................................................................................................... 21 Appendix I ............................................................................................................................................. 23 Appendix II ............................................................................................................................................ 25 References ............................................................................................................................................ 27 2|P age Agreed 2009 Review in 2012 1. Background 1897: Ernest Wertheim in Vienna embarked on a remarkable series of radical hysterectomies and limited pelvic node resections – eventually performing over 1300 procedures with no patient lost to follow-up. Operative mortality of 30% in the first hundred cases was later reduced to 10%. 1903: Margaret Cleaves, a New York physician first applied radium to carcinoma of the cervix. 1911: the first “clinical cure” of cervical cancer by radium reported from the Radiumhemmet at Stockholm which had been established in 1910. 1940s: Meigs of Boston revised and extended the Wertheim operation, claiming 75% survival among his first hundred cases and a survival of stage I of 81.8%. 1948: Brunschwig of New York published on adjacent pelvic organs with diversion of urine and the faecal stream through conduits leading to the abdominal wall for advanced and recurrent cervical cancer. 2. General Information Carcinoma of the cervix is the third most common gynaecological malignancy in women, accounting for 2740 new cases and 1,225 deaths in England and Wales in 1997(1). World-wide, cervical cancer is second only to breast cancer as the most common malignancy in both incidence and mortality. More than 420,000 new cases are diagnosed each year (2), predominantly among the lower socio-economic classes in both developing and industrialised nations (3) There is a very strong aetiological link with human papilloma virus (HPV) infection and cervical cancer (4). Indeed HPV has recently been identified in 99.7% of all cervical cancers tested by Walboomers et al (5). Apart from smoking all other risk groups are merely co-factors for the risk of high risk HPV infection eg age at first intercourse and number of sexual partners. 3|P age Agreed 2009 Review in 2012 The Health of the Nation set a target to reduce the incidence of cervical cancer by 20% before the year 2000 (6). This was achieved in 1993, in part as a consequence of an effective cervical screening programme (5). Among the major factors that influence prognosis are stage, tumour volume and grade of tumour, histological type, lymphatic spread, and vascular invasion, depth of stromal invasion with the latter being most important and reproducible. ( 7,8,9). A multivariate analysis of prognostic variables in 626 patients with locally advanced disease (II, III, and IV) studied by the GOG revealed that para-aortic and pelvic lymph node status, tumour size, patient age, and performance status were significant for progression-free interval and survival. Adenocarcinoma of the cervix over recent years has increased both in proportion and true incidence compared to squamous tumours ( 10). Immunocompromised women have more aggressive and advanced disease and a poorer prognosis. 3. Prevention – Cervical Screening and Colposcopy Compelling evidence exists that large numbers of cervical cancers can be prevented by a well-organised cervical screening programme (11). These programmes combine cervical cytology as a primary screen with colposcopy, and treatment where appropriate, for those who are screen positive. In the United Kingdom, “Health of the Nation” targets for the reduction of cervical carcinoma incidence have been reached many years ahead of target. A consistent fall in incidence at all ages follows improvements in the NHS Cervical Screening Programme (NHSCSP) and the introduction of computerised “call and recall” systems in the late 1980’s. This success reflects the huge rise in the percentage of the target population who are now being screened (eg this rose from 44 – 83% between 1988 and 1993). The NHSCSP has produced a number of publications which outline the standards that are expected from those who participate in all aspects of the screening process ( 12). The main role of the cervical screening programme is to lower the incidence and mortality of cervical carcinoma. However, there will be occasional referrals where it is felt that an invasive lesion may be present, and these patients should receive urgent management on the grounds of clinical suspicion. 4|P age Agreed 2009 Review in 2012 The North West presently has the highest regional incidence and lowest screening cover for cervical cancer in the country. The regional quality assurance team is coordinating initiatives to correct this. 4. Referral Any woman with either post-coital or inter-menstrual bleeding, persistent vaginal discharge or whose cervix looks abnormal should be referred by a rapid access referral to a gynaecologist or colposcopy clinic. If the patient appears to have superficial invasion a loop or cold knife cone biopsy should be performed by the lead clinician locally. The specimens should be reported by a pathologist with special interest in gynaecological malignancies and reviewed by the MDT. When the disease is higher than stage IaI, and for all non-squamous invasive lesions, referral of the patient to the specialist gynaecological team is indicated. All patients with biopsy proven invasive disease should be considered for pathological review. Our aim is to achieve clinical management of all patients within the target cancer waiting times of the Dept of Health. Histological Types and Incidence As a result of screening, rates per 100,000 for all invasive cervical cancers decreased by 36.9% over 24 years [12.35 (1973–1977) vs 7.79 (1993–1996)]. Similarly, the age-adjusted incidence rates for squamous cell carcinoma declined by 41.9%. In contrast, the age-adjusted incidence rates for adenocarcinoma increased by 29.1%. The proportion of adenocarcinoma increased 95.2% relative to squamous cell carcinoma. Observed survival rates for adenocarcinoma vs squamous cell carcinoma were poorer for regional but not localized or distant disease (13). Adenosquamous, small cell carcinomas and primary sarcomas of the cervix have been described occasionally, and malignant lymphomas of the cervix, both primary and secondary, have also been reported. 5|P age Agreed 2009 Review in 2012 5. Stage Information The precursor lesion is dysplasia or cervical intraepithelial neoplasia [CIN], which can subsequently become invasive cancer. This process can be quite slow. Longitudinal studies have shown that in untreated patients with CIN 3, 18% will develop invasive carcinoma over a period of 10 years (13). As it becomes invasive, the tumour breaks through the basement membrane and invades the cervical stroma. Extension of the tumour in the cervix may ultimately manifest as an exophytic growth (70%), ulceration (20%) endocervical barrel shaped cervix or with extensive infiltration of underlying tissue including bladder or rectum. In addition to local invasion, carcinoma of the cervix can spread via the regional lymphatics or blood stream. Tumour dissemination is generally a function of the extent and invasiveness of the local lesion. While cancer of the cervix generally progresses in an orderly manner, one occasionally sees a small tumour with distant metastasis. For this reason, patients must be carefully evaluated for metastatic disease. Treatment is very dependent on stage and can therefore affect management and outcome (14). FIGO Staging System (See Appendix I) 6. Pre-Treatment Assessment Examination under anaesthetic, cystoscopy and biopsy of the cervix for histology Sigmoidoscopy may be performed if clinically indicated Other investigations should include: FBC, Biochemical Profile Chest X-Ray IVP or MRI Clinical Staging The staging should be performed by an experienced examiner under GA, including a cystoscopy. There are occasions where outpatient clinical assessment and imaging may be sufficient. The clinical staging should not be changed on the basis of subsequent findings, thus allowing more accurate comparison to other treatment regimes. There are however limitations to clinical staging. 6|P age Agreed 2009 Review in 2012 Pre-operative imaging Magnetic Resonance Imaging (MRI) is accurate in evaluating cervical disease, early parametrial extension and lymph node status which translates into prognosis and survival predictions. MRI, in terms of determining extent of tumour, is generally superior to CT (15) and ultrasound (16,17), but in many cases clinical examination will be the overriding factor. MRI may be superfluous and delay treatment if clinical examination confidently indicates a stage of 1b1 or less, when a traditional IVP may be sufficient. Ultrasound (US) is commonly used to predict hydroureter and hydronephrosis and has replaced IVP in many centres. There is some evidence to suggest that the use of internal coils for high resolution MRI of the cervix for greater detailed cervical anatomy and pathology (18). Advances in radiology mean that cancer of the cervix can be evaluated pre-operatively allowing for more informed discussion regarding the optimum treatment, either radiotherapy or surgery. PET-CT scanning is being evaluated and my prove to be useful for selected patients. It may help reduce inappropriate surgery for women with parametrial extension. 7. Treatment overview Radiotherapy and surgery are equally effective in terms of survival for the majority of women with early cervical cancer. Surgical treatment should be offered to women with early stage cancer for whom a cone biopsy is inadequate. This should be carried out by a sub-specialist gynaecological oncologist working within a Cancer Centre. Radical radiotherapy should be offered when surgery is unlikely to remove the tumour completely. The effects of radiotherapy can cause long term damage to other organs; bowel, bladder and ovary, and this is worst when combined with surgery. Two meta-analyses have shown convincing evidence of survival benefit for chemoradiation over radiotherapy alone in locally advanced disease, at a cost of greater short term toxicity and an uncertain increase in late effects. The survival and disease free benefit may be greater in Stage I and II disease. (2, 19) During pregnancy, no therapy is warranted for lesions of the cervix which can be confidently assessed colposcopically as being preinvasive. One third of these lesions will regress during pregnancy so colposcopic assessment and treatment as 7|P age Agreed 2009 Review in 2012 required should be arranged at a suitable interval after delivery. Treatment of invasive cervical cancer during pregnancy depends on the stage of the cancer and gestational age at diagnosis. The traditional approach is to recommend immediate therapy appropriate for the disease stage when the cancer is diagnosed before fetal maturity, and to delay therapy only if the cancer is detected in the final trimester (20,21). However, other reports suggest that deliberate delay to allow improved fetal outcome may be a reasonable strategy. Published evidence regarding this problem is largely anecdotal but there is no published work suggesting that such delay results in a large reduction in survival. 8. Management of Invasive Disease All patients with a diagnosis of invasive cervical cancer are referred for MDT opinion and almost all will be subsequently managed by the specialist team at the gynaecological oncology centre. I. Superficially invasive cervical carcinoma (microinvasive carcinoma). Early stromal invasion with unmeasurable invasive component is diagnosed and treated by cone biopsy, normally at the referring unit. Stage IA2 disease within the current staging definition is treated at the centre by modified radical hysterectomy (Meigs 2), with pelvic node dissection up to the iliac bifurcation. Intermediate cases of superficially invasive disease are reviewed on an individual basis at the central diagnostic MDT meeting and the individual management thereby determined. In premenopausal patients, the ovaries are normally conserved. II. Stage IBI and stage 2A less than 4 cms Treatment of choice is Meigs 3 radical hysterectomy with pelvic lymphadenectomy up to the aortic bifurcation. We usually aim to conserve the ovaries in patients under the age of 45 (squamous) or age of 40 (adeno). 8|P age Agreed 2009 Review in 2012 III. More advanced stage (1B2, bulky 2a and higher) and patients unsuitable for surgery irrespective of stage Patients are normally referred for radiotherapy +/- chemotherapy. See sections 15.3 and 16.3. 9. Cervical adenocarcinomas They are treated the same as invasive squamous carcinomas stage for stage. Microinvasive adenocarcinomas are more difficult to diagnose than their squamous counterparts, but when diagnosed with confidence may be amenable to local treatment. High grade glandular intraepithelial neoplasia (adenocarcinoma in-situ), is diagnosed and treated by cone biopsy but radical treatment tends to be recommended for most invasive lesions. Villoglandular carcinomas should be treated similarly to other adenocarcinomas, though following definitive histology a more favourable prognosis may be assigned for true villoglandular lesions. (22) 10. Small cell cervical carcinomas (neurendocrine tumours, malignant carcinoids) Combined modality treatment is recommended with chemotherapy and radiotherapy in patients with good performance status. The standard regimen in Clatterbridge Centre for Oncology for small cell tumours is : Carboplatin AUC 6 and Etoposide 100mg/m2 daily X 4 cycles, followed by radiotherapy for localised disease. 11. Incidental finding of invasive cancer of the cervix found after Simple Hysterectomy Further management is based on the above principles. Treatment options will therefore, lie between expectant management, node dissection (open or laparoscopic) with or without radical parametrectomy, or chemoradiation. 9|P age Agreed 2009 Review in 2012 12. Radical Trachelectomy Trachelectomy is becoming an accepted alternative approach to early cervical cancers in women wishing to preserve the option of fertility (23). The procedure involves removing the cervical together with the parametrial tissue whilst preserving the uterine body. Publications have suggested an equivalent survival when compared to a standard radical hysterectomy, for stage 1a2 or small (<2cm) stage 1b1 cervical tumours. Trachelectomy for 1b1 tumours of >2cm has been associated with a higher recurrence rate. The procedure is carried out in conjunction with a laparoscopic pelvic lymphadenectomy. Preoperative evaluation prior to consideration of a trachelectomy includes an EUA (and assessment of the cervical length), MRI and careful counselling regarding the risks associated with the procedure. Published figures have stated a 60-70% chance of pregnancy following trachelectomy, but a 25-75% risk of a preterm (potentially extremely preterm) delivery. (24,25,26,27). In the Liverpool Womens Hospital, all women who have undergone a radical trachelectomy have a prophylactic cervical cerclage placed at the time of the original surgery, and are followed up during any subsequent pregnancy by the recurrent miscarriage team. 13. Relapse Local relapse after primary surgery is managed in most cases by radical chemoradiation. Those patients who relapse after radiotherapy are carefully assessed for surgery. However, pelvic exenteration is technically difficult, bladder and bowel diversion are required with associated morbidity and in this centre it is considered only in very selected patients. Metastatic disease is managed with palliative chemotherapy +/- radiotherapy. 14. Adjuvant Surgery In the recent GOG series, bulky stage IB patients were followed by hysterectomy after chemoradiation.(28,29). No survival advantage ensued but pelvic control was 10 | P a g e Agreed 2009 Review in 2012 improved. A second option may be surgery following neo-adjuvant chemotherapy for Stage 1B-IIB patients, as in the proposed EORTC trial 55994. This is based on studies in Argentina and more recently Italy (30). A meta-analysis has been published in preliminary form and shows a highly significant survival benefit compared to radiation alone (31). The place of hysterectomy as a routine adjunct to pelvic radiotherapy is controversial. The increased risk of combined modality treatment is not necessarily balanced by improved outcome (32). In this centre it is considered only in exceptional cases, such as disruption of optimal dose fractionation, distortion of normal pelvic anatomy (e.g. fibroids), coincidental gynaecological pathology, or in selected cases of poor response to external beam radiotherapy. 15. Radiotherapy or Surgery for Carcinoma of the Cervix I. Stage 1a disease These patients are generally managed surgically but those unsuitable for surgery can be treated with intracavitary brachytherapy alone. . II. Stage 1b1 and 2a disease (non bulky) There is agreement that for these patients either radical chemoradiation or radical hysterectomy (RH) are equally effective treatments with approximately 85-90% of patients being cured with either modality (33,34). RH and radiotherapy are associated with different types of complications. The choice of treatment depends on the general health of the patient. Surgery is generally recommended for pre-menopausal women as preservation of ovarian function is possible and vaginal stenosis can be avoided. The risk of late bladder and bowel toxicity is also less after surgery. For less fit patients surgery with prolonged general anaesthesia is best avoided and these patients are generally treated with radiotherapy or chemoradiation. As the risk of pelvic lymph node involvement is estimated to be 15% our policy is to treat these patients with a combination of external beam radiotherapy and intracavitary treatment. For less fit patients intracavitary treatment alone can be considered accepting a higher risk for nodal failure. 11 | P a g e Agreed 2009 Review in 2012 III. Bulky stage 1B and 2A disease and stages IIb – IVa These patients are best treated with a radical course of chemoradiation. Less fit patients may be treated with radiotherapy alone. Squamous cell carcinoma (SCC) versus adenocarcinoma (ACC) These are treated similarly with either radical surgery or radiotherapy. A large series from the MDA hospital showed that with radiation therapy the control of disease in the pelvis was similar for ACC as for SCC. The survival rates were lower for ACC than for SCC due to a higher rate of distant metastases (13). 16. Chemotherapy and radiotherapy for cervical cancer I. Neoadjuvant chemotherapy This is not routinely recommended. Eight of nine randomised studies and a recent literature based meta-analysis have not shown a benefit with this approach ( 35), but a second individual patient meta-analysis is more optimistic for further development of this (36). It is not standard treatment, but patients may be considered for randomisation to EORTC 55994. II. Concurrent Chemoradiation This is now standard practice for patients with bulky or locally advanced disease who are fit for the combined approach. There have been six North American based randomised trials published since April 99, and there have been 2 meta-analyses, one of 19 studies (2), the other comprising 8 English language publications using only cisplatin based chemotherapy (19) . All except one of the US trials showed a clear benefit for this approach in terms of improved disease control in the pelvis and a 10 –15% improvement in overall survival (2,28,37,38,39,40). The overview demonstrated both an improvement in overall survival but also improved local and distant control rates (2). The acute toxicity is greater with concurrent chemotherapy and potentially higher rate of late complications. This approach is considered in all patients with locally advanced carcinoma of the cervix who have good performance status and considered suitable for radical treatment (41). 12 | P a g e Agreed 2009 Review in 2012 III. Integrated chemotherapy This is a specialised approach piloted at Clatterbridge over the last 10 years and can be considered in patients who have persistently bulky disease after external beam XRT or disease extending to the pelvic side wall and brachytherapy is not appropriate. These patients are given three cycles of chemotherapy and repeat EUA is performed in view to proceed with brachytherapy. Clatterbridge experience with this approach has been good particularly for patients with stage II disease (32). 17. Postoperative radiotherapy This is considered for patients at high risk for disease recurrence. These include the following groups of patients. I. Patients with involved pelvic lymph nodes: There are no randomised trials looking at the benefit of postoperative XRT in this situation. Retrospective studies show that pelvic radiotherapy reduces the risk of local failure but does not impact on overall survival (42,43). One study showed that for patients with a single positive node with small primary tumours the prognosis is good without radiotherapy (29). Our current policy is to consider adjuvant radiotherapy to patients with more than one involved pelvic lymph node, or where there is extracapsular spread. II. Postoperative radiotherapy for patients with involved resection margins after RH: Patients with close margins are discussed at the multidisciplinary meeting and decisions regarding further treatment are made on an individual basis. Our policy is to consider postoperative external beam intracavitary treatment. Patients with gross residual disease after RH do badly. To optimise local control higher radiation doses may be used than for patients with residual microscopic disease. 13 | P a g e Agreed 2009 Review in 2012 III. Postoperative radiotherapy for high-risk node negative patients: A recent GOG randomised study showed that for patients with negative pelvic nodes and either large primary tumours, CLS invasion or deep stromal invasion, there was an advantage for postoperative radiotherapy in terms of reducing the risk of recurrence. No survival advantage was seen and the rate of major complications was 6% in the combined treatment group vs 2% in the patients treated with RH (29). Our current policy is not to offer radiotherapy to these patients. IV. Postoperative radiotherapy for patients treated inadvertently with simple hysterectomy: These patients can subsequently have parametrectomy, pelvic lymphadenectomy and upper vaginectomy. The complication rates with reoperation can be substantial and there are several reports suggesting very good outcome with radiotherapy (44). Our policy is to discuss the further management of these cases at our multidisciplinary meeting. For those patients treated with radiotherapy a combination of external beam and intracavitary treatment is used in combination with chemotherapy. Morbidity of combined treatment with RH and radiotherapy. There is evidence that the major complication rate is increased with combined treatment. One randomised study comparing surgery with radiotherapy described a 28% rate of major complications in the surgical arm vs 12% with radiotherapy (45). However almost two thirds of the surgical arm had postoperative radiotherapy because of bulky disease, tumour cut-through or involved pelvic lymph nodes For this reason it is important to predict patients who are likely to need postoperative radiotherapy if treated with RH, such as those with tumours >4cm. These patients are best treated with radiotherapy Our aim is to carefully select patients for surgery and to avoid postoperative radiotherapy as it is associated with much greater morbidity. 14 | P a g e Agreed 2009 Review in 2012 18. Extended field radiotherapy Extended field radiotherapy, which includes para-aortic nodes, is associated with an increased rate of acute and late toxicity. I. Prophylactic extended field radiotherapy: There is evidence from one randomised study that extended field radiotherapy offers a survival advantage compared with pelvic radiotherapy for stage I and II patients with a high risk of para-aortic nodal metastases i.e. those with either bulky disease or involved pelvic lymph nodes (46). However one of the recent Chemoradiation trials compared extended field radiotherapy with Chemoradiation and found the latter to be better in terms of overall and disease free survival (47). Prophylactic para-aortic radiotherapy can be considered for patients not fit for primary chemoradiation. II. Irradiation of patients with known para-aortic nodal metastases: Five-year survival rates for patients with para-aortic node metastases treated with extended field radiotherapy vary between 8-50% (48). The worst results are in patients with stage III and IV disease as control of pelvic disease is also an issue for these patients. The best results are seen in patients with small volume stage I and II disease who are found to have microscopic nodal disease intraoperatively. The management of patients with multiple grossly involved para-aortic nodes is generally palliative. A recently published single arm study using extended field radiotherapy and concurrent chemotherapy reported a three year overall survival rate of 39% for patients with para-aortic nodal metastases (49). Both acute and late toxicity was substantial. In highly selected patients this approach would appear to have a curative potential. 15 | P a g e Agreed 2009 Review in 2012 19. Radiotherapy for patients with isolated local failure in the pelvis after RH Up to 50% of these patients can be salvaged with radiotherapy ( 50,51). The prognosis is best for those with small volume central recurrences. Treatment includes both external beam and intracavitary radiotherapy. Patients with bulky recurrences have a poor prognosis and may be considered for neoadjuvant or concurrent chemotherapy. Decisions regarding the use of chemotherapy are made on an individual basis. 20. Palliative radiotherapy This is considered for patients with either advanced, recurrent, metastatic disease or for unfit patients with any stage of disease. Palliative local radiotherapy is particularly effective for bleeding, discharge or pain. Depending on the performance status of the patient external beam or intracavitary or combinations of both can be used. 21. Improving Effectiveness of Radiotherapy: Hb Levels The presence of oxygen has important implications in effectiveness of radiotherapy. Hypoxia plays an important role in tumour resistance in most solid tumours including carcinoma of the cervix. There is growing evidence in the literature that local control by radiotherapy is closely related with haemoglobin levels and this reflects the overall survival. Our policy at CCO is that all patients with cervical carcinoma undergoing radical radiotherapy should have weekly blood test for FBC and would require blood transfusion if Hb is <12g/dl. Selected patients may benefit from prophylactic use of growth factors (Erythropoetin) where the Hb level prior to starting chemoradiation is <12.0g/dl (52). 16 | P a g e Agreed 2009 Review in 2012 22. Chemotherapy for advanced or recurrent cervical cancer Cytotoxic chemotherapy with drugs including mitomycin C, cisplatin, 5FU and more recently ifosfamide has been employed in the management of advanced disease for several years, with response rates of the order of 30% and a duration of response of 6-9 months. The most active drug is cisplatin, which therefore restricts the eligible patient group to those without renal impairment. There is little evidence in favour of activity of carboplatin Problems such as prior radiation treatment, extensive surgical procedures and often poor general performance status in elderly patients have contributed to the low expectation of efficacy of this modality in the past. A number of trials in the 1970’s addressed first line chemotherapy (neoadjuvant) followed by radiation therapy, and these were largely negative in terms of improvement in progression free or overall survival, although response rates were higher than in the advanced disease patients (35). Two more recent series have explored neoadjuvant chemotherapy followed by surgical excision (NACT-S). (53,54), with more promising results, as a result of which an EORTC trial is being proposed for this approach with cisplatin based chemotherapy in Stage IIB patients. The regimen employed in the CCO for many years has been bleomycin, mitomycin C and cisplatin (BMC) based on the original MD Anderson publication (55) and there is experience in both advanced disease and as adjuvant therapy after external beam radiation therapy (32). A number of other regimens have been advocated including Bleomycin, Ifosfamide and Cisplatin (BIP) as published by Buxton et al (56), which is considered to be toxic, and cisplatin and 5FU regimens such as that proposed in the CE04 study. Topotecan is a topoisomerase I inhibitor. The response rates to single agent Toptecan ranges from 13% to 28% depending on whether or not patients received prior treatment. The GOG 179 confirmed significantly superior response rates, DFS and OS in patients treated with combination Cisplatin and Topotecan as compared to single agent Cisplatin (Long HJ 3rd, et al. Randomized phase III trial of cisplatin with or without topotecan in carcinoma of the uterine cervix: a Gynecologic Oncology 17 | P a g e Agreed 2009 Review in 2012 Group Study. J Clin Oncol. 2005 Jul 20;23(21):4626-33). In this study, patients had a better outcome irrespective of previous cisplatin chemotherapy. However, on multivariate analysis, the improvement in OS is statistically significant only in patients with a long duration from time of diagnosis to time of starting study treatment (16 months or more). There was a significant 17.7% rate of FN in the combination arm and the protocol recommended secondary prophylactic G-CSF if FN occurs after dose modification. When Topotecan is licensed for the use in cervical cancer we recommend selecting patients who have more chance of benefit from Topotecan and Cisplatin combination to justify administration of this potentially myelotoxic regimen as follow: Time from diagnosis to relapse >/= 12 months (Whether or not had prior radiosensitizing cisplatin) No prior radio-sensitizing cisplatin (irrespective of time from diagnosis to relapse). PS 0/1 (only 8% of patients in each arm had PS 2). The regimen will be as follows: TC Topotecan 0.75 mg/m2 IV (over 30 min) D1,2,3 Cisplatin 50 mg/m2 IV infusion D1 Body surface area capped at 2 m2 Repeated every 21 days for maximum of 6 cycles. Attention to 20% and 40% Toptecan dose reduction for grades III and IV myelotoxicity respecrively. Option 2; Cisplatin and Paclitaxel (cisplatin 50 mg/m2 plus paclitaxel 135 mg/m2) every 3 weeks for six cycles. Moore DH. J Clin Oncol. 2004 Aug 1;22(15):3113-9. Phase III study of cisplatin with or without paclitaxel in stage IVB, recurrent, or persistent squamous cell carcinoma of the cervix: a gynecologic oncology group study. Rationale is: higher RRs and longer PFS for this combination as compared to single agent Cisplatin. 18 | P a g e Agreed 2009 Review in 2012 Adenocarcinoma and Adeno.squamous carcinoma. Traditionally literature report similar or worse overall outcome for Adenocarcinoma and Adeno.squamous carcinoma as compared to Sq C Ca. However, there is substantial evidence that Adenocarcinoma and Adeno.squamous carcinoma are equally chemosensitive and in some reports more sensitive to chemotherapy. Ref (n of pts) Treatment Histology RR % Fiorica J (n=35) (no prior CTH) Dimopoulo s MA. (n=60) Routine GCSF Topotecan+ Cisplatin Sq=21 Non Sq=11 33 27 (ORR=28) Cisplatin+ Ifosfamide+Paclitax el Sq =41 36* Non Sq=19 67* Kavanagh JJ. (n=24) Cisplatin+ Doxorubicin+5FU (76h infusion / 4w) Curtin JP. Paclitaxel (n=42) pts 175mg/m2. 130 failed mg/m2 if prior RTH standard treatment) (Ad.Ca & Ad.Sq.Ca) 42 (25) Ad. Ca 27 31 pts (22) Ad.Sq 15 pts PFS G3/4 neutrope nia 26% & Thrombo cytopenia 7% DOR=7m DOR 4.8 m OS (month) Irradiation % (CR) All 10 In=33 (11) Out=30 (10) 11.5 m* 24.7 m* In=23% Out=58% GIII/IV Neut 26% NF 10/296 cycles (OS=8.3 ) = For Adeno Ca and Adeno.sq.ca Option 1: Single agent paclitaxel (Curtin JP JCO 2001. 1,19 (5).1275 (GOG). (see table) Option 2: Cisplatin and Paclitaxel Rational for option 2: (1) Curtin JP study showed RR of 31%. We know that Cisplatin is tradionally the drug of choice. Combining them is likely to improve response rates. (2) Cisplatine+ Ifosfamide+Paclitaxel yields high response RR of 67% in Non Squamous histologies (Dimopoulos MA. Gynecol Oncol. 2002 Jun;85(3):476-82). However myelotoxicity was high despite G-CSF). This toxicity is most likely to be due to Ifosfamide rather than Cisplatin. It is sensible to omit Ifosfamide from this regimen for treating these patients with an intent of palliation. (3) If we also chose Cisplatin 19 | P a g e Agreed 2009 Review in 2012 and Paclitaxel for Sq C Ca as discussed above, then this treatment will be for all histologies. Other drugs Carboplatin AUC 5 unproven Some centres employ methotrexate in place of mitomycin C CPT 11 (ironitecan) Gemcitabine promising) promising) Taxanes 23. Follow-Up Standard: Four monthly for years 1 and 2, six monthly to 3 years. Discharge with open access to CNS in the event of new symptoms or concerns. CNS holistic assessment is carried out 6 weeks after the completion of primary treatment. 24. Maintenance of Quality These guidelines conform to: Improving outcomes in Gynaecological Cancers NHS Executive 1999-10-21 RCOG recommendations on specialists in gynaecological oncology 1996 NIH Consensus Statement on Chemoradiation 1999 25. Audit and Clinical Outcome Gynaecological database is now in place which will facilitate clinical audit and research. 26. Clinical Trials 1- EORTC 55994 – Stage Ia2- IIB Ca Cervix : Cisplatin based chemotherapy followed by surgery compared to chemoradiation therapy 20 | P a g e Agreed 2009 Review in 2012 27. Palliative Care and Nursing care Palliative care input is appropriate to consider at all stages of the patient’s cancer journey. Please refer to the separate palliative care guideline for detailed advice. All women with a diagnosis of a Gynaecological Cancer should be offered the support of, and have access to a Clinical Nurse Specialist (CNS), in order to facilitate the woman’s needs throughout the Cancer Journey, including those of her partner or carer. The skills of the C.N.S. as a consultant, practitioner and educator can be drawn upon at all stages throughout their illness, from the pre-diagnosis to the terminal stage – incorporating the Specialist Palliative Care Services provided in the hospital and the community setting. Bereavement Support will also be available, if appropriate. Important aspects of the role are to provide advice, support, information and to effectively incorporate appropriate resources. The C.N.S. will be receptive to the social, physical, psychological, cultural, sexual and spiritual needs of the patient. The aim of the patient support is to assist with the improvement in the quality of their lives, allowing them to become more empowered; to help take control and enhance their self esteem. The C.N.S. works closely with Surgeons, Oncologists, Radiotherapists, Consultants in Palliative Medicine and others (Nurses & P.A.M.s). 21 | P a g e Agreed 2009 Review in 2012 They will undertake a number of key responsibilities including: Linking with other professionals who can help the patients throughout the system A resource for information and support to the patient carer and other H.C.P.s Liaison point for other health care professionals in primary and secondary care Teacher and Educator Researcher Standards and Audit Co-ordinator Co-ordinate Care Services 22 | P a g e Agreed 2009 Review in 2012 Appendix I FIGO Staging System Stage I IA Clinical lesions strictly confined to cervix Preclinical carcinomas of cervix diagnosed only by microscopy. All gross lesions even with superficial invasion are stage IB cancers. Invasion is limited to measured stromal invasion with maximum depth of 5.0 mm and no wider than 7.0 mm (1) IAI Stromal invasion no greater than 3.0 mm and no wider than 7.00 mm IA2 Maximum depth of invasion of stroma greater than 3 mm and no greater than 5 mm taken from base of epithelium, either surface or glandular, from which it originates; horizontal invasion not more than 7 mm IB Clinical lesions confined to the cervix or preclinical lesions greater than stage IA IBI Clinical lesion no greater than 4.0 cm in size IB2 Clinical lesion greater than 4.0 cm in size Stage II Extension beyond cervix but not to pelvic wall. Involves vagina, but not the lower third IIA Involves vagina, but not lower third. No obvious extension to parametria IIB Obvious parametrial involvement but not extending to pelvic sidewall Stage III Extension to pelvic wall. On rectal examination, no cancer-free space between tumour and pelvic wall. Involves lower third of vagina 23 | P a g e Agreed 2009 Review in 2012 IIIA Involves lower third of vagina IIIB Extension to pelvic side wall and/or hydronephrosis or non-functioning kidney Stage IV Extension beyond true pelvis or involvement of bladder or rectal mucosa. Bullous oedema does not permit a case to be assigned to Stage IV (IVa = local spread; IVb = distant mets) Notes: Diagnosis of both Stages IA1 and IA2 is based on microscopic examination of biopsy specimens, preferably a cone, which must include the entire lesion. 24 | P a g e Agreed 2009 Review in 2012 Appendix II Radiotherapy Details External Beam radiotherapy: Patient Position: Patient should be lying supine. Vaginal examination performed and a vaginal marker is placed if required. These patients now have a planning CT scan to outline the gross tumour clinical target volume. Field Size: Upper Border: L4/L5 disc space ( half way through L-5 if increased risk of morbidity) Lower Border: Bottom of Obturator foramen. In case of vaginal involvement, 2-3 Cm below the lower extent of disease. Lateral Border: 1 Cm lateral to the pelvic brim Posterior Border: Junction of S2 and S3 vertebrae or 2 Cm anterior to the most concave part of anterior sacrum. Take into account the sagital view of MRI scan films. Treat with parallel opposed field if Uterosacral ligament involved. Consider appropriate lead shielding. 25 | P a g e Agreed 2009 Review in 2012 Dose Fractionation: Stage I B1and non-bulky IIa: XRT: 45 Gy in 25 fractions over 35 days Brachytherapy: HDR: 7Gy x 2 to point “A”: 1 week apart Stage I B2, IIB, III and IVA: XRT: 50.4 Gy in 28 Fractions over 38 days Brachytherapy: HDR: 7Gy x 2 to point “A” 1 week apart. Consider Parametrial Boost if the disease is extending to Parametriem at the end of XRT 5.4 Gy in 3 fractions over 3 days Palliative XRT: 30 Gy in 10 fractions over 14 days or 20 Gy in 5 Fractions over 7 days 26 | P a g e Agreed 2009 Review in 2012 References 1 Cervical screening programme, England: 1997-98. Government Statistics service 2 Green JA et al. Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: a systemic review and metaanalysis. The Lancet. 358: 781-786. 2001 3 Pisani P, Parkin DM, Bray F, Ferlay J. Estimates of the worldwide mortality from 25 cancers in 1990. Int J Cancer 1999; 83: 18-29 4 Schiffman MH, Bauer HM, Hoover RN et al. Epidemiological evidence showing that human papilloma virus causes most cervical intraepithelial neoplasia. J Natl Cancer Inst 1993; 85: 958-964 5 Walboomers JMM, Jacobs MV, Manos MM et al. Human papillomavirus is a necessary cause of invasive cervical cancer world wide. J Pathol 1999;189: 431-438 6 Health of the Nation, London, Department of Health, 1992 7 Delgado G, Bundy B, Zaino R, et al. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecologic Oncology 1990; 38(3): 352-357 8 Zaino RJ, Ward S, Delgado G, et al. Histopathologic predictors of the behaviour of surgically treated stage IB squamous cell carcinoma of the cervix. Cancer 1992; 69(7): 1750-1758 9 Steren A, Nguyen HN, Averette HE et al. Radical hysterectomy for stage IB adenocarcinoma of the cervix: the University of Miami experience. Gynecologic Oncology 1993; 48(3): 355-359 10 Stockton D, Cooper P, Lonsdale RN. Changing incidence of invasive adenocarcinoma of the uterine cervix in East Anglia. J Med Screen 1997; 4: 40-3 11 Niemenen P, Kallio M, Hakama M. The effect of mass screening on incidence and mortality of squamous and adenocarcinoma of the cervix uteri. Obstet Gynecol 1995; 85: 1017-21 12 Duncan ID. Revised guidelines for clinical practice and programme management NHSCSP Publication No.8. April 1997 27 | P a g e Agreed 2009 Review in 2012 13 Smith HO, Tiffany MF, Qualls CR. Key CR. The Rising Incidence of Adenocarcinoma Relative to Squamous Cell Carcinoma of the Uterine Cervix in the United States—A 24-Year Population-Based Study. Gynecol Oncol 2000;78:97-105 14 Guidance on commissioning Cancer Services. Improving Outcomes in Gynaecological Cancers: the Research Evidence. Department of Health 1999. 15 Kim SH, Choi BI, Lee HP et al. Comparison of CT and MR findings. Radiology 1990; 175: 45-51 16 Innocenti P, Pulli F, Savino L et al. Staging of cervical cancer: reliability of transrectal US. Radiology 1992; 185: 201-5 17 Hawnaur JM, Johnson RJ, Carrington BM et al. Predictive value of clinical examination, transrectal ultrasound and magnetic resonance imaging prior to radiotherapy in carcinoma of the cervix. British Journal of Radiology 1998; 71: 81927 18 de Souza NM, Scooner DJ, Krauz T et al. Am J Radiol 1996; 166: 553-559 19 Lukka H, Hirte H, Fyles A et al Concurrent cisplatin-based chemotherapy plus radiotherapy for cervical cancer – a meta-analysis Clin Oncol 2002 14: 203-212 20 Greer BE, Easterling TR, McLennan DA et al. Fetal and maternal considerations in the management of stage IB cervical cancer during pregnancy. Gynecological Oncology 1989; 34(1): 61-65 21 Duggan B, Muderspach LI, Roman LD et al. Cervical cancer in pregnancy: reporting on planned delay in therapy. Obstetrics and Gynecology 1993 82 (4): 598602 22 Macdonald RD, Kirwan J, Hayat K, Herrington CS, Shawki H. Villoglandular adenocarcinoma of the cervix: Clarity is needed on the histological definition for this difficult diagnosis. Gynecol Oncol 2006;100:192-194 23 Shepherd JH, Crawford RAF, Oram DH. Radical trachelectomy: a way to preserve fertility in the treatment of early cervical cancer. Br J Obstet Gynecol 1998; 105: 9126 24 Hertel H, Köhler C, Grund D, Hillemanns P, Possover M, Michels W, Schneider A; German Association of Gynecologic Oncologists (AGO). Radical vaginal trachelectomy (RVT) combined with laparoscopic pelvic lymphadenectomy: prospective multicenter study of 100 patients with early cervical cancer. Gynecol Oncol 2006. 103: 506-11 28 | P a g e Agreed 2009 Review in 2012 25 Dursun P, LeBlanc E, Nogueira MC. Radical vaginal trachelectomy (Dargent's operation): a critical review of the literature. Eur J Surg Oncol. 2007; 33: 933-41 26 Schlaerth JB, Spirtos NM, Schlaerth AC. Radical trachelectomy and pelvic lymphadenectomy with uterine preservation in the treatment of cervical cancer. Am J Obstet Gynecol 2003; 188: 29-34 27 Plante M, Renaud MC, Hoskins IA, Roy M.Vaginal radical trachelectomy: a valuable fertility-preserving option in the management of early-stage cervical cancer. A series of 50 pregnancies and review of the literature. Gynecol Oncol 2005; 98: 310 28 Keys et al. Cisplatin,radiation and adjuvant hysterectomy compared with radiation and ajuvant hysterectomy for bulky stage 1B cervical carcinoma. NEJM. 340: No 15. 1154-1153. 1999 29 Sedlis et al. A randomised Trial of pelvic radiation therapy versus no further therapy in selected patients with stage 1B carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy. A Gynecological Oncology Group study. Gyn. Oncol. 73: 177-183, 1999 30 Benedetti-Panici P, Greggi S, Colombo A, et al. Neoadjuvant chemotherapy and radical surgery versus exclusive radiotherapy in locally advanced squamous cell cervical cancer: results from the Italian multicenter randomised study. J Clin Oncol 2002; 20: 179-188 31 Stewart L, Tierney J. Neoadjuvant chemotherapy followed by surgery for locally advanced cervix cancer : a meta-analysis using individual patient data from randomised controlled trials. Proceedings of ASCO 2002; 20:966-972 32 Tan LT, Jones B, Green JA, Kingston RE, Clark PI. Treatment of carcinomas of the uterine cervix which remain bulky after initial external beam radiotherapy: a pilot study using integrated cytotoxic chemotherapy prior to brachytherapy. Br J Radiology 1996; 69: 165-171 33 Hopkins et al. Radical hysterectomy versus radiation therapy for stage Ib squamous cell cancer of the cervix. Cancer 1991; 68: 272-277 34 Piver et al. Radical Hysterectomy and pelvic lymphadenectomy versus radiation therapy for small (<3cm) stage Ib cervical carcinoma. Am J Clin Oncol. 1988; 11: 2124 29 | P a g e Agreed 2009 Review in 2012 35 Tierney JF et al. Can the published data tell us about the effectiveness of neoadjuvant chemotherapy for locally advanced cancer of the uterine cervix? Eur. J.Cancer. 35: 406-409. 1999 36 Stewart L, Tierney J. Neoadjuvant chemotherapy followed by surgery for locally advanced cervical cancer: a meta-analysis using individual patient data from randomised controlled trials (RCTs) . Proceedings of ASCO 2002; 21: 207a 37 Morris et al. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high risk cervical cancer. NEJM. 340: No 15. 11371143. 1999 38 Rose et al. Concurrent cisplatin based radiotherapy and chemotherapy for locally advanced cervical cancer. NEJM. 340: No 15. 1144-1152. 1999 39 Whitney et al. Randomised comparison of Fluorourracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage 11B-1V carcinoma of the cervix with negative para-aortic lymph nodes: A Gynecologi Oncology Group and Southwest Oncology Group study. Journal of Clinical Oncology. 17: 1339-1348. 1999 40 Pearcey R, Brundage M, Drouin P, et al. Phase III trial comparing radical radiotherapy with and without cisplatin chemotherapy in patients with advanced squamous cell cancer of the cervix. .J Clin Oncol 2002; 20: 966-972 41 Symonds P Chemoradiation: the new gold standard for non-surgical treatment of cervical cancer Clin Oncol 2002 14 201-202 42 Kinney et al. Value of adjuvant whole pelvis irradiation for early stage squamous cell carcinoma of the cervix with pelvic node metastases; a matched controlled study. Gynecol. Oncology 43 Alvarez et al. Identification of prognostic factors and risk groups in patients found to have nodal metastases at the time of radical hysterectomy for early stage squamous carcinoma of the cervix. Gynecol Oncology 1989; 35: 130-135 44 Crane et al. Occult carcinoma discovered after simple hysterectomy treated with postoperative radiotherapy. Int. J Radiation. Oncology. Biol. Phys. 43: No. 5. 10491053, 1999 45 Landoni F, Maneo A, Colombo A, et al. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet. 1997 Oct 18;350(9085): 535-40 30 | P a g e Agreed 2009 Review in 2012 46 Rotman et al. Prophylactic extended field irradiation of para-aortic lymph nodes in stages 11b and bulky 1B and 11A cervical carcinomas. Ten year treatment results of RTOG 7920. JAMA. 274: 387-393. 1995 47 Morris et al. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high risk cervical cancer. NEJM 340 No. 15, 1137-1143, 1999 48 Rotman et al. Irradiation of pelvic and para-aortic nodes in carcinoma of the cervix. Seminars in Radiation Oncology. 4: No 1. 23-29. 1994 49 Varia et al. Cervical carcinoma metastatic to para-aortic nodes:extended field therapy with concomitant 5-Fluorouracil and cisplatin chemotherapy: Agynecologic oncology Group study. Int.J. Radiation. Oncology. Biol. Phys. 42:No 5 1015-1023. 1998 50 Deutch et al. Radiotherapy for carcinoma of the cervix recurrent after surgery. Cancer. 34: 2051-2055. 1974 51 Tan R et al. Radiotherapy for postoperative recurrent uterine cervical carcinoma. Acta-Oncol. 30: No 3. 353-356. 1991 52 Grogan M, Thomas G M, Melamed I, Wong F L, Pearcey R G, Joseph P K, Portelance L, Crook J, Jones K D. The importance of hemoglobin levels during radiotherapy for carcinoma of the cervix. Cancer 1999 Oct 15, VOL: 86 (8), P: 1528-36 53 Sardi JE et al. Long term follow up of first randomised trial using neoadjuvant chemotherapy in stge 1b squamous cell crcinoma: the final results. GynaecolOncol.67 (1): 61-69, 1997 54 Benedetti-Panici P et al. Long-term survival following neoadjuvant chemotherapy and radical surgery in locally advanced cervical cancer. Eur J Cancer 32 (3): 341346, 1998 55 Smith HO et al Treatment of advanced or recurrent squamous cell carcinoma of uterine cervix with Mitomycin-C, Bleomycin and Cisplatin chemotherapy. GynaecolOncol. 48 (1): 11-15, 1993 56 Buxton EJ. Experience with bleomycin, ifosfamide, and cisplatin in primary and recurrent cervical cancer. Semin-Oncol 19. (2S): 9-17, 1992 31 | P a g e