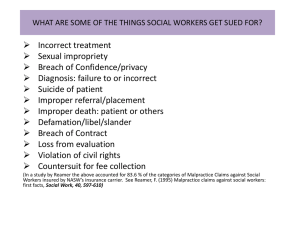
HISTORICAL PERSPECTIVE OF MEDICAL MALPRACTICE
advertisement
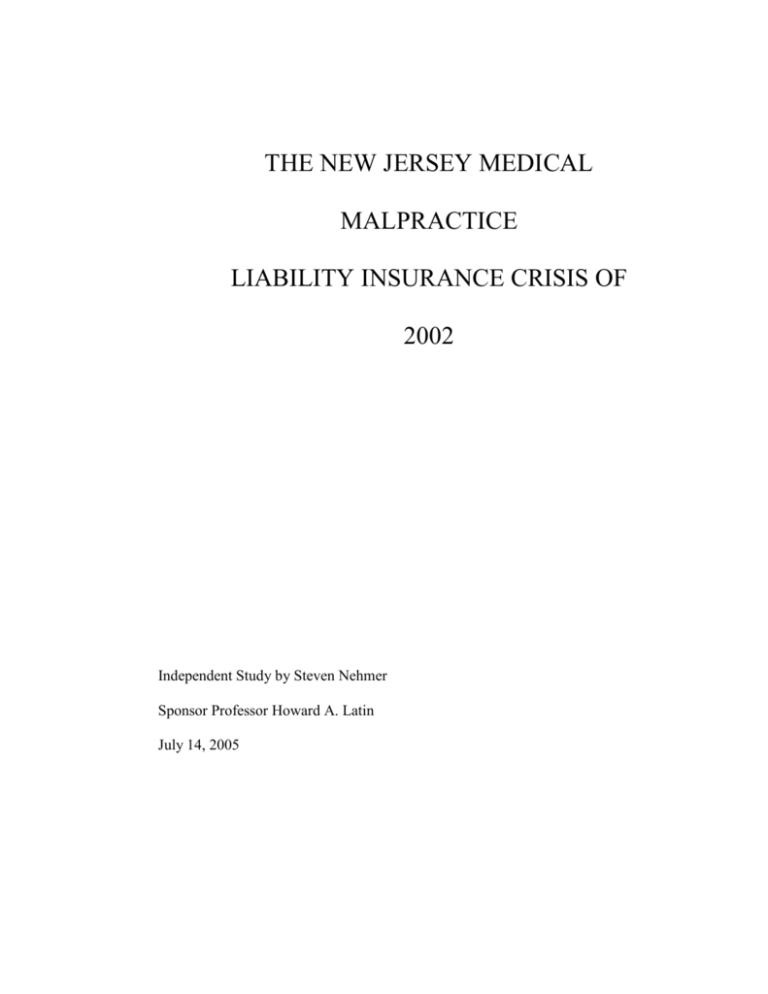
THE NEW JERSEY MEDICAL MALPRACTICE LIABILITY INSURANCE CRISIS OF 2002 Independent Study by Steven Nehmer Sponsor Professor Howard A. Latin July 14, 2005 INTRODUCTION In 2002 the medical community in New Jersey experienced a medical malpractice crisis, in which premiums climbed rapidly at the same time that many physicians faced the prospect of losing their coverage completely as their carrier stopped writing medical liability policies. This paper represents an effort to understand the events that occurred, their causes, and to look at possible changes that would limit future repetition of this crisis. The historical development of medical malpractice litigation, and the subsequent spread of liability insurance to protect physicians, will be described. Recurring “crises” in the system have been the norm. Basic concepts of the industry, including hard and soft markets, the annual premium v. insurer’s surplus ratio, relative effects of premiums and investment income, will be defined. The “perfect storm” of 2002, representing the fallout from years of under-pricing medical malpractice insurance by the carriers in order to widen market share, followed by a drop in investment yield, increasing reinsurance costs, and, finally, the exit of several carriers from the market place, will be discussed. Reactions to the crisis by organized medicine, attorneys, insurers, government and the public are looked at. Several national studies of the parallel medical malpractice crisis, including those of the General Accounting Office, Public Citizen, the Rand Institute, and the Project on Medical Liability in Pennsylvania, are used to delve into the causes of the crisis and to offer alternative thoughts on possible system changes that need to be implemented. 2 This paper concludes with the author’s thoughts on the subject, summarizing the history of the medical malpractice industry, its goals, and what I believe needs to be done to improve the system. HISTORICAL PERSPECTIVE The concept of medical malpractice is first found in the writings of Sir William Blackstone, who explicitly extended the concept to physicians in 1768. He used the term “mala praxis” from which the word malpractice derives.1 It was in the nineteenth century that the legal concept took hold in the United States. The establishment by the American Medical Association in 1849 of a board to determine standards for medical practice was key, since having standards for the profession allowed the existence of a deviation from these standards.2 The first “malpractice crisis” to occur in the United States took place from 1840 to 1860, during which time the state appellate courts saw a 950% rise in the number of medical malpractice cases heard. This was in contrast to a population rise of 85%.3 One prominent litigator in this arena on both the plaintiff and defense sides was Abraham Lincoln.4 Initially the targets of most suits were the more respected and educated physicians, as they had the funds to make them attractive defendants. The charlatans of the age were judgment proof. It was with the rise of medical liability insurance at the end of the nineteenth century that all physicians became prospective targets.5 Patricia Costante and Janet Spicer Puro, “Medical Malpractice: An Historical Perspective,” New Jersey Medicine, 100-7-8, July/August 2003, p. 21. 2 Id. at 22. 3 Id. 4 Id. 5 Id. 1 3 The second medical malpractice crisis occurred around 1970, when claims began to grow suddenly, causing the insurance carriers to dramatically raise their premiums to cover their expenses. At that time most of the carriers were multi-line commercial insurers, and many of them decided to drop out of the market when profitability declined. This caused a crisis in availability, causing the medical community to respond with the creation of physician-owned medical malpractice companies.6 In contrast to the issue of availability, the next crisis to hit was one of affordability. In the 1980’s there was a spike in both the number of claims and the amount of damages awarded, and the insurance carriers responded with increasing premiums.7 This was followed by another decrease in the late 1980’s in incidence of claims and amounts of awards.8 The 1990’s was a period of prosperity for the medical liability insurance industry. The New Jersey legislature, in 1995, did pass a tort reform package with several features. These included a cap on punitive damages at 5 times compensatory damages or $350,000, whichever is greater; a modification of the doctrine of joint and several liabilities, which allowed a defendant to be held 100% liable for damages only if they are 60% or more at fault; exemption of health care providers from certain product liability claims; and the requirement for a certificate of merit signed by an expert declaring a deviation from the standard of care.9 The attorney fee schedule for contingency awards, effective September 1, 1996, limits fees to “33.3% of the first $500,000, 30% of the second $500,000, 25% of the third 6 Id. at 23. Id. 8 Janet Spicer, MIIX Healthcare Group consultant, New Jersey Medicine, 99-4, April 2002, p. 19. 9 Id. at p. 24-25. 7 4 $500,000, 20% of the fourth $500,000, and a reasonable amount approved by the court for an excess of more than $2 million.10 Contrast this to Newt Gingrich’s statement that “[p]ersonal injury lawyers are earning up to 60% of jury medical-malpractice awards that regularly top $1 million.”11 BACKGROUND At the present time, most physicians nationally purchase medical liability coverage in the amount of $1 million per event and $3 million per year aggregate. Sixty percent of the coverage is obtained from physician-owned or operated companies.12 The functioning of medical malpractice liability insurance is very similar to other types of insurance. The physician pays a premium in return for the insurance company’s promise to defend claims and to be financially responsible for any damages incurred up to the limits of the policy. The most common type of policy sold is the claims made, which limits the insurer’s liability to those claims made within the time frame of the policy. This is not as open ended as the older occurrence type policy, in which the insurer was responsible for any events occurring within the time frame of the policy, even if the claim was made years later. The claims made policy allows the insurer to better plan for the future and more accurately determine the premiums that it needs to collect. The ratio of total annual premiums to insurer’s surplus is an important one, and is used by state insurance departments to measure the financial soundness of insurers. The annual premiums is the sum total of monies collected within the year, and the surplus is 10 Id. Newt Gingrich, senior fellow at AEI, USA Today, “Excessive Jury Awards Endanger Medical System,” August 13, 2002. 12 GAO-03-702, Medical Malpractice Insurance, p. 6. 11 5 the insurer’s assets in excess of the liabilities, both current and future estimated. Generally, the surplus should at least equal the annual premium. It is more difficult for the medical malpractice insurance industry, than the property/casualty insurance industry in general, to accurately predict losses on claims for three reasons: (1) claims take on average more than five years to resolve, (2) the range of cost of claims is very wide, and (3) past data is limited due to the small size of the pool of insured.13 Another key factor for the insurance company is the return it realizes on the funds during the time between its collection of premiums, and the paying of expenses. In 2001 the largest United States insurers had on average 79 percent of their assets invested in bonds.14 Returns of 6% or more were common in the mid-1990’s, but the rate had fallen to 4% by 2002.15 An insurance company’s income is primarily made up of premium collection and yield from investments. In 2001, the average insurance carrier had assets that were approximately 4.5 times as large as their annual premium income. Therefore a 1% drop in investment income would necessitate a 4.5% rise in insurance premiums to keep income stable.16 The medical malpractice insurance industry, like most financial sectors, has repetitive cycles, alternating between ‘hard’ and ‘soft’ markets. Hard markets are characterized by increasing premiums and decreasing availability of coverage. Hard markets generally occur in parallel with downturns in the overall economy, when insurers are obtaining lower yields from their investment portfolios. Soft markets, by contrast, typically have stable or even decreasing premium rates as the supply of insurers increase 13 Id. at 8. Id. at 24. 15 Id. at 25. 16 Id. at 27. 14 6 and there is competition for writing policies. Often the investment returns are sufficient to allow a cut in premiums while still maintaining profitability. The period from the late 1980’s until 1998 was a classic soft market for medical malpractice insurance. From 1998 on, profitability decreased and premiums began to increase, heralding the switch to a hard market. NEW JERSEY 2002 In 2002 New Jersey physicians saw a rapid rise in their medical malpractice premiums, with some doctors even having difficulty in obtaining coverage. An article in The Star Ledger of Newark dated February 18, 2002 was entitled “Jersey physicians run for coverage- Malpractice insurers vanishing.”17 Three carriers in New Jersey had stopped writing policies for medical liability: Phico declared bankruptcy, St. Paul Fire and Marine terminated its medical liability line of business, and Zurich ended its New Jersey business.18 In May of 2002 the largest single insurer of New Jersey physicians, Medical Inter-Insurance Exchange (MIIX), went into “voluntary solvent runoff.”19 The response to this crisis was varied, with physicians, attorneys, and carriers all blaming each other for responsibility. Abbott Brown, a certified civil trial attorney and adjunct professor at Seton Hall University School of Law, wrote an editorial in which he blamed the carriers, specifically Princeton and MIIX for using the absence of competition to drive up their prices and compensate for losses in other arenas.20 He called for 17 Carol Ann Campbell, The Star Ledger, p. 1. Id. 19 NJHA Medical Malpractice Insurance Survey, January 28, 2003. 20 Abbott Brown, The Star Ledger, March 14, 2002, p. 15. 18 7 governmental regulation of the medical malpractice insurance industry, and for a reduction in the incidence of medical malpractice by the medical community. 21 The chairman of the medical liability task force for the Medical Society of New Jersey, Bernard Saccaro, blamed the system and the trial attorneys, declaring that the result of the “out of control” costs would be a shortage of physicians.22 His recommendations included expert panels to review claims prior to trial, caps on awards, plaintiff attorney compensation limits, legislation to provide relief to physicians in those specialties hardest hit by the increases, and a more stringent statute of limitations.23 Angelo S. Agro, M.D., the president of the Medical Society of New Jersey, stated that “[t]here has been no increase in true malpractice. Moreover, the number of jury awards, which in itself is a poor indicator of malpractice, has not gone up; the amount of those awards has exploded.”24 The insurance carriers responded with statements that their increasing premiums were a reflection of increasing expenses defending medical malpractice claims. Patricia Costante, president and CEO of MIIX, called it “the business of economics. We look at someone and decide, based on their losses, whether we are able to insure them.”25 Bob Schultz, a Princeton Insurance executive, blamed the exit of other carriers on their selling policies with “irresponsibly low” premiums.26 The New Jersey Hospital Association (NJHA) became a strong supporter of legislation that would place a cap on non-economic damages. Gary Carter, president and 21 Id. Bernard Saccaro, The Star Ledger, April 2, 2002, p. 23. 23 Id. 24 Angelo S. Agro, MD, “A Primer on Medical Economics,” New Jersey Medicine, 99-4, April 2002, p. 7. 25 Campbell, February 18, 2002. 26 Id. 22 8 CEO of the NJHA, stated in January 2003 “any solution that doesn’t include a $250,000 cap on pain and suffering settlements would fall short and lead to diminished access of care.”27 A public poll was conducted by the New Jersey Chapter of the American College of Cardiology, asking the following questionBecause of rising malpractice insurance, many New Jersey doctors are not performing certain procedures, or leaving practice altogether. Ultimately, this means that in New Jersey, we could start to see a shortage of certain types of doctors. Who do you feel is the most responsible for this situation? Insurance companies got the most votes with 33%, lawyers and juries 30%, everyone involved 11%, the state of New Jersey 9%, doctors 6%, and others 2%.28 Analysts had other theories for the crisis. Janet Spicer discussed “legal developments” including lengthening of the statute of limitations in some states, broadening of the legal grounds for bringing suits in other states, “more liberal court decisions, the tendency for juries to return larger rewards, and the rapid rise of higher out-of-court settlements.”29 She then mentions the declining personal nature of the physician-patient relationship and the “reluctance of some state medical boards to discipline their own members.”30 Statistics appeared to offer conflicting views of the severity of the crisis, and whether in fact there even was one. Depending upon the time frame referenced, and the measure used to determine events, different conclusions could be drawn. “The St. Paul 27 http://www.njha.com/paprepresadvertorials/papresadvertorials2003/january.html press release, January 22, 2003 via The Cherenson Group of Livingston, New Jersey. 29 Janet Spicer, “Professional Liability Insurance II. The Legal Environment” New Jersey Medicine, 99-4, April 2002, p. 24. 30 Id. 28 9 Companies reported that medical malpractice claims of $1 million or more doubled in 2001, climbing from 27 in 1999 to 54 in 2000.”31 “Jury Verdict Research reports that the median malpractice award rose in four consecutive years from $455,000 in 1996 to $800,000 in 1999.” This represents an increase of 76%.32 Another source also quoting Jury Verdict Research reported “that the median malpractice award from 1992-1996 was $350,000. The figure from 1997 to the present [2/02] jumped to $518,000.”33 It has been reported that “claims have ballooned from $2.6 billion in 1997 to $4.1 billion in 2000, an increase of 58%.”34 However the National Association for Insurance Commissioners (NAIC) released data showing the payments made by insurers in New Jersey were $231 million in 1992 and $235 million in 2001, a modest increase for that time period.35 The NAIC is a voluntary association of state insurance department heads which exists to serve state insurance regulators.36 “The number of malpractice suits in New Jersey has declined from 2200 in 1994 to 1613 in 2001, a decrease of more than 25 percent.”37 Princeton Insurance Co., New Jersey’s largest malpractice carrier, reported 366 cases tried to a conclusion in 1998, 347 Patricia A. Costante, MBA, CHC, “Restoring Stability to the Professional Medical Liability Market,” New Jersey Medicine, 99-4, April 2002, p. 14. 32 Id. 33 Carol Ann Campbell, The Star Ledger, Newark, N.J. February 18, 2002, p. 1. 34 Costante at 13. 35 National Association of Insurance Commissioners, “Medical Malpractice Insurance Net Premium and Incurred Loss Summary,” July 18, 2002. 36 GAO-03-702 Medical Malpractice Insurance, June 2003, FN6. 37 Abbott Brown, The Star Ledger, Newark, N.J. March 14, 2002, Editorial, p. 15. 31 10 in 1999, and 274 in 2000.38 In 2002, there were 205 medical malpractice jury trials and 2 bench trials that went to verdict.39 The actual dollars paid out by insurers on behalf of the physicians of New Jersey were reported by The Star Ledger on June 9, 2004 as a high in 2001 of $214 million, declining to $199 million in 2002 and $162.5 million in 2003.40 The Star Ledger, in a January 8, 2003 editorial entitled “The malpractice muddle,” emphasizes the lack of knowledge as to whether pain-and-suffering awards are inflating the cost of malpractice claims. Four months later it was reported that the New Jersey Assembly was being asked to seek data from insurance companies by the use of subpoena power.41 Assemblyman Neil Cohen, chairman of the insurance committee, stated that attempts to get information from the insurance carriers voluntarily were unsuccessful.42 This quest for subpoena power proved unsuccessful as well, as demonstrated by testimony given before a committee of the New Jersey Assembly in which the vice president and general counsel of Princeton Insurance Company stated “It’s not the kind of data that is needed by the company or its actuaries, and we just never captured it.”43 He was referring to the amount paid out be Princeton Insurance Company for non-economic, pain and suffering damages. The crisis of 2002 is the most recent of a series of crises, and it would be easy to assume that it is only the most recent “upswing of the same pendulum,” in which “malpractice premiums rise, doctors accuse lawyers, lawyers point back at doctors, and 38 Id. Jane F. Castner, Interoffice Memorandum, Administrative Office of the Courts, Civil Practice Division, January 31, 2003. 40 Carol Ann Campbell, p. 1. 41 Robert Schwaneberg, The Star Ledger, Newark, N.J. May 24, 2003, p. 29. 42 Id. 43 The Star Ledger, PERSPECTIVE, “Malpractice madness,” October 5, 2003, p. 2. 39 11 legislatures debate tort reform in arcane and repetitive terms.”44 But many analysts see this hard market as different. William Sage cites four areas in which changes in the health care system have had a significant effect upon the medical malpractice system: (1) patient safety, (2) cost containment, (3) medical progress, and (4) industrialization.45 In previous episodes of medical malpractice premium rises, physicians would blame the legal system, and argue that instances of malpractice were few. However, in the Institute of Medicine’s (IOM) 1999 report To Err is Human, the conclusion is reached that “modern medicine has outgrown its traditional methods of quality control.” Estimates of error are large, for example between 44,000 and 98,000 Americans dying each year secondary to medical errors.46 The report argues for system changes to improve outcomes and to decrease “malpractice.”47 Cost containment has been a constant and ubiquitous process in health care over the past two decades, and this has strained the system. In the past, insurers paid the fees charged without much questioning, and physicians were able to pass along increases in their malpractice premiums by increasing their fees. The increase in malpractice premiums represented primarily an insult to their pride. But with the vast majority of fees paid today fixed by health care insurers, that option no longer exists. Substantial increases in premiums have a direct and significant effect on physician incomes.48 The increase in the size of medical malpractice awards is largely linked to medical progress. In fact, “[m]ore than any single factor, malpractice expense tracks William M. Sage, M.D., J.D. “Understanding the First Malpractice Crisis of the 21 st Century,” available at MAGNETO/NEPTUNE/AUTOMATE01/V_JUR/HLHB/CH1, p. 1. 45 Id. at 3. 46 Id. at 1. 47 Id. at 5. 48 Id. at 20-21. 44 12 overall health care spending as technology improves, expectations rise, sources of avoidable error proliferate, and the costs of caring for those who suffer harm grow.”49 The failure to promptly diagnose a disease is of much more significance as the ability to treat that disease, when diagnosed early, improves. As our ability to work longer into our lives increases, the economic damages from malpractice-generated disability grows. The costs involved in the treatment of conditions caused by malpractice have a direct bearing upon the awards at time of trial.50 Industrialization has resulted in a dimunition of the patient-physician relationship, especially in urban areas. It has also resulted in a loss of control by the physician, who is often held responsible when the actions taken were dictated by health care insurances.51 NATIONAL STUDIES While no comprehensive, rational investigation of the medical malpractice crisis has occurred in New Jersey to date, there has been a federal study. The United States General Accounting Office (GAO), responding to Congressional Requesters, in June of 2003 issued a report seeking to determine the causes of the recent surge in medical malpractice premiums.52 This study should serve as a template for New Jersey government officials seeking to understand and quantify the problem in New Jersey. The report studied a sample mix of seven states, gathering information from the state insurance regulator, state medical association, state hospital association, state association of trial attorneys, the largest one or two active insurance companies, data 49 Id. at 7. Id. 51 Id. at 12. 52 GAO-03-702 Medical Malpractice Insurance, available at www.gao.gov/cgi-bin/getrpt?GAO-03-702. 50 13 from NAIC, and from A.M. Best.53 The states were chosen on the basis of obtaining a mix of status as a crisis state as defined by the American Medical Association (AMA), population, presence of damage caps, and extent of recent increases in malpractice insurance rates. Those chosen were Florida, California, Pennsylvania, Texas, Mississippi, Nevada and Minnesota.54 The medical malpractice insurance companies reported raising their rates beginning in 1999, after a period of relative price stability. There was a great deal of variability in the raises, depending upon the medical specialty and geography, even within states. For example, physicians in Philadelphia paid 83% more than those outside of the city.55 It was the opinion of the GAO that the cause of these raises was multifactorial, but that the largest factor was an increase in losses on claims. Other important factors cited were the decrease in investment income experienced nationally, the loss of price competition among insurance carriers when some left the market place, and the increase in reinsurance rates generally subsequent to the events of September 11, 2001.56 Insurers reported that 78 percent of their expenses consisted of the costs of defending and paying claims. Increasing losses cause premiums to rise in several ways: direct immediate increased expenditures, higher anticipated losses, and an effect upon the plaintiff’s expectations of awards. This change in plaintiff attitude can result in more frequent claims as well as higher settlement amounts in those cases that do not go to trial.57 53 A.M. Best is a rating agency working in the insurance industry. GAO-03-702 at 2. 55 Id. at 13. 56 Id. at 15. 57 Id. at 22. 54 14 It was noted that “settlement amounts are not formally divided between these two types of damages [economic and non-economic] and that consistent, comprehensive information on trial judgments is not collected.”58 In sum, the GAO study concludes without recommending any specific remedial action by the Congress for the current situation. They believe that it is difficult to predict how the medical malpractice insurance arena would respond to any change in legislation. The current market is different from previous ones due to the presence of physician owned carriers instead of commercial entities; due to many states having passed laws to influence the industry; and due to a lack of meaningful data. The GAO does recommend that Congress encourage the NAIC and state insurance regulators to collect more information in the future.59 At the same time the GAO was publishing a report on the causes of the rise in medical malpractice premiums, they also issued a statement on “Implications of Rising Premiums on Access to Health Care.”60 They sought to determine whether the rising premiums had resulted in physicians retiring or relocating, a reduction in high-risk services, or the practice of ‘defensive’ medicine. Nine states were studied, five of which were considered as experiencing malpractice insurance problems and four of which were not.61 The study did find examples of decreased local access to health care services in the five states that were experiencing liability insurance increases, and did not in the other four states. Two examples of diminished availability of services were: (1) a loss of 58 Id. at 23. Id., highlights. 60 GAO-03-836, August 2003. 61 Id. at 3. 59 15 orthopedic on call services at a rural hospital in Pennsylvania when three of the five orthopedists left in 2002 due to increasing malpractice rates, and (2) family practitioners in rural Mississippi stopped delivering babies in order to control their rising premiums, which necessitated the local women to travel 65 miles to obtain obstetric care. It was noted that the majority of cases of decreased health care access were in rural locations where there had been a chronic problem with maintaining adequate medical coverage. The report also did note that there were anecdotal reports of physicians retiring or leaving an area which upon investigation were not verified. The study also looked at Medicare claims to determine if certain high risk procedures were performed, such as mammograms, spine surgery, and total joint revisions. There was no evidence of decreased delivery of these services.62 The organization Public Citizen published in August 2004 an analysis entitled “Medical Malpractice Briefing Book: Challenging the Misleading Claims of the Doctors’ Lobby.”63 This paper concludes that lawsuits are not the primary cause of rising medical malpractice premiums, but that the insurance cycle is. They believe that inadequate patient safety is the real medical malpractice crisis, that patient access to care is not in danger, and that caps are unjust and would not offer relief from rising premiums.64 The first claim, that the medical malpractice premium rise is not primarily due to increasing lawsuits, is based upon statistics from the National Practitioner Data Bank stating that the number of payouts in 1994 was 15,166 and in 2003 was 15,295, an 62 Id. at 5. Public Citizen is a non-profit organization founded in 1971, based in Washington, D.C. It has 160,00 members and its stated purpose is to represent consumer interests. 64 Public Citizen’s Congress Watch, www.citizen.org. 63 16 increase of only 0.85%.65 When the number of physicians is factored in, the number of payouts per 100 physicians went down 11% in the same time period. Using the United States population, malpractice filings per 100,000 people decreased 1% from 19922001.66 The actual cost of payouts has increased from $184,787 in 1994 to $291,378 in 2003; when adjusted for medical services inflation, which is the basis for much of the economic damages awarded, the rise is 1.1% per year.67 When compared to the inflation of medical services, which was 125% from 1987 to 2001, malpractice premiums increased 76%.68 Public Citizen blames the 2001 hardening of the medical malpractice insurance market for the increasing premiums.69 They quote the director of insurance for the Consumer Federation of America, J. Robert Hunter, as stating that “premiums charged do not track losses paid, but instead rise and fall in concert with the state of the economy.”70 The Congressional Budget Office also related the increase in premiums to the drop in investment returns.71 The problem of individuals with multiple claims is brought to light in the Public Citizen publication as well. Prorating statistics drawn from To Err is Human, they attribute to New Jersey 1316-2930 deaths per year and $508-$867 million in annual costs that result due to preventable medical errors. This is compared to $415.8 million in New Jersey health care provider medical malpractice premiums in 2002.72 Using National Practitioner Data Bank data, 1990 to 2003, 56.2% of all payouts was made on behalf of 65 Id. at 2. Id. at 3. 67 Id. at 4. 68 Id. at 6. 69 Id. at 24. 70 Id. at 25. 71 Id. 72 Id. at 39. 66 17 5.4% of doctors, and 31.1% on behalf of 2% of doctors.73 Public Citizen goes on to criticize state medical boards for not taking disciplinary action against these physicians,74 but no mention is made of the difficulties that would be involved in this process, including assessment of practice patterns- certainly some procedures on certain in some geographic locations involve higher risk (e.g. obstetrics for high risk pregnancies in an urban setting), and society does need someone function in that role. The Public Citizen report relied upon the GAO report (see above) for evidence that access to healthcare was not impaired as a result of medical malpractice rates. It found no correlation between the presence of caps and the per capita number of physicians in individual states.75 William Sage listed six problems that need to be addressed by those that would seek to correct the chronic recurrent issues that plague the medical malpractice insurance industry: (1) high costs as well as the volatility of premiums, (2) the potential for decreased access to care, (3) compensation for the injured, which he feels is presently inadequate, (4) decreasing the incidence of errors, (5) speeding up the entire process which takes years under the present tort system, and (6) improving the climate for health care and the incentive to innovate.76 SOLUTIONS The current medical malpractice system in the United States serves several purposes: to compensate patients who sustain injuries as a result of medical error, to 73 Id. at 41. Id. at 42. 75 Id. at 61. 76 William Sage, supra at 28-29. 74 18 encourage the healthcare system to develop new and safer methods of delivering care, and to select out those healthcare providers in need of further training. The tort system currently in place has both its supporters and its detractors. The medical community has traditionally condemned malpractice suits, while the legal community defends them. Among the most common criticisms of the system is that it causes errors to be unreported due to a fear of sanction, resulting in systemic problems not being addressed and corrected.77 This concept has been supported by the AMA, which “asserts that ‘for error reporting systems to be successful, they must be constructed in a non-punitive manner that provide[s] appropriate confidentiality protections.’ The AMA’s official position is that liability has no proper role to play in the regulation of health care professionals.”78 This position was supported in 1999 when the IOM issued its report on patient safety and medical error, in which it concluded in part that “[t]he focus must shift from blaming individuals for past errors to a focus on preventing future errors by designing safety into the system … blaming an individual does little to make the system safer and prevent someone else from committing the same error.”79 The report goes on to say “patient safety is [] hindered through the liability system and the threat of malpractice.”80 There is contradictory evidence, however, which does show a positive relationship between the existence of malpractice liability and improved patient safety. Probably the most convincing example is that of the specialty of anesthesiology. In David A. Hyman and Charles Silver, “The Poor State of Health Care Quality in the U.S.: Is Malpractice Part of the Problem or Part of the Solution?” p. 3. University of Maryland School of Law, 2004, available at http://ssrn.com/abstract=526762. 78 Id. at 16. 79 To Err Is Human, Institute of Medicine, executive summary p. 4, 1999. 80 To Err Is Human, p. 37. 77 19 response to high malpractice rates and negative publicity, the American Society of Anesthesiologists (ASA) in 1983 created a Committee on Patient Safety and Risk Management which included a study of malpractice claims.81 As a result of this study multiple steps were taken to improve patient safety, including widespread safety equipment use, mandatory safety guidelines, decreased resident hours, and improving the designs of machines used.82 The application of quality standards to the field of anesthesiology has led to a mortality rate decrease from 1 in 10,000-20,000 to 1 in 200,000. The medical malpractice liability decrease is demonstrated by the fact that premiums in 2002 are virtually the same as they were in 1985, and that “the fraction of total medical malpractice insurance costs attributable to anesthesia-related claims fell from 11 percent to 3.6 percent over fifteen years.”83 Another example of openly addressing errors and seeking to improve systems to prevent errors and enhance patient safety is that of the United States Veterans Health Administration (VHA). In response to GAO reports finding poor quality of care, the Congress mandated increased external controls, including a “comprehensive risk management program requiring disclosure of medical errors to patients.”84 This has resulted in a significant improvement in the VHA system’s quality indicators.85 An effort was made to investigate this issue by the Harvard Medical Practice Study (HMPS). They sought to correlate the risk of malpractice suit with the frequency of negligent injuries. There was a decrease found in the incidence of negligence-related 81 Hyman and Silver at 25. Id. at 24. 83 Id. 84 Id. at 38. 85 Id. at 39. 82 20 injuries as the risk of medical liability increased, but it was not statistically significant. 86 This contradicts the IOM conclusion that patient safety is harmed by the existence of the liability system. The HMPS did find that the poor and elderly, the least likely to sue, were the most likely to suffer from negligence-related injury, and that doctors who had been sued were more likely to take increased time explaining risks v. benefits to their patients.87 It is the conclusion of Hyman and Silver that the current tort liability medical malpractice system has a beneficial effect upon the delivery of health care in the United States, and that market forces should be allowed to govern the industry. They therefore recommend that malpractice premiums be allowed to rise without governing forces such as caps, predicting that such a rise will result in a response by the medical community analogous to that of the ASA in the 1980’s.88 Caps could be used as a method for promoting disclosure of errors by providers, which would be the first step in addressing errors in a systemic manner. For example, disclosure within a specified time period would result in a limit on non-economic damages. Conversely, failure to disclose would result in an increase in the award.89 Other ideas include allowing health care workers to bring suits on behalf of patients and to share in the awards; allowing standards to be created, that would provide an absolute defense to allegations of malpractice if adhered to; and subjecting repeat defendants to institutional scrutiny.90 Probably the most prevalent legislative reform to address increasing medical malpractice premiums is that of caps, limits to the amount of award given to plaintiffs. It 86 Id. at 21. Id. at 22. 88 Id. at 81. 89 Id. at 82. 90 Id. at 84-85. 87 21 is the non-economic portion of the award which most proponents feel should be capped. Most cited as an example of this type of reform is California. California’s state legislature passed its tort reform act, MICRA (Medical Injury Compensation Reform Act) in 1975, but it did not really take effect until the 1985 decision of the Supreme Court of California which upheld its constitutionality.91 Under the MICRA statute, a jury can award as much money as it desires for non-economic loss, but the judge will then lower that portion of the award to $250,000. Also, MICRA limits attorney fees on a sliding scale based upon the amount of damages awarded.92 In contrast, the passage of a similar law in Texas in 1977 was found to be unconstitutional in 1988 by the Texas Supreme Court. A 2003 reform bill in Texas required the voters to pass a constitutional amendment in September 2003 to allow the measures to take effect.93 In both states, the reforms that were passed were comprehensive and not just limits on the award for non-economic damages. Both states limited attorney contingency compensation, defined expert witness qualifications, and changed the definitions of bad-faith claims.94 The success of California’s MICRA in lowering rates is controversial. Its effect was most pronounced following the 1988 passage of Proposition 103 in California, in which the voters reformed the entire property-casualty insurance industry, including medical malpractice.95 The California Department of Insurance was given increased powers to review all rate changes and to limit profits. Further, anti-trust exemptions were 91 Dr. Lena Chang, Founder and President, NJ PURE, Malpractice Monthly, April 2005, p. 2. RAND Institute for Civil Justice, “Changing the Medical Malpractice Dispute Process: What Have we Learned from California’s MICRA?” 6/6/2005 available at http://www.rand.org/publications/RB/RB9071/ 93 Chang, supra at 2. 94 Id. 95 Public Citizen, p. 74. 92 22 taken away from the industry, and a law prohibiting brokers from negotiating their rates with consumers was repealed.96 The RAND study examined 257 plaintiff verdicts from 1995 to 1999 in California malpractice trials. Cases resolved by settlement were not included. They found that MICRA reductions in non-economic damages were triggered 45% of the time, causing a reduction overall in defendant’s liabilities of 30%. The plaintiffs had a 15% reduction in recoveries, while plaintiff attorneys experienced a 60% reduction in their fees due to a combination of lower awards and a lower contingency rate.97 Of note, cases in which the injury resulted in death had the awards lowered 58% of the time, compared to 41% for injury cases. Cases with the most severe non-fatal injuries, e.g. brain injury or paralysis, were decreased more often than other injury cases and for significantly larger amounts. When the plaintiff was less than one year of age, caps occurred 71% of the time.98 Weiss Ratings, Inc. analyzed the medical malpractice insurance industry from 1991 through 2002,99 and came to the following conclusions regarding the presence of caps on non-economic damages: the 19 states with caps had physician premiums climb 48.2% compared to a 35.9% increase in the 32 states without caps in place (Washington D.C. was counted as a state), 2 of the 19 states with caps had declining or flat premiums compared to 6 of the 32 without caps, and the median payouts increased 71.3% in the states without caps compared to 37.8% in those states with caps.100 This would seem to indicate that while the insurance companies benefited from lowered disbursements in the 96 Id. at 75. RAND, supra at 2. 98 Id. 99 three high risk specialties were included, general surgery, obstetrics/gynecology, and internal medicine. 100 Weiss Ratings, Inc., “Medical Malpractice Caps Fail to Prevent Premium Increases, According to Weiss Ratings Study,” June 2, 2003, p. 1. Available at http://www.weissratings.com/News/Ins.General/20030602pc.htm 97 23 states that had caps in place, the physicians did not see a corresponding decrease in their medical malpractice costs. Six factors were offered by Weiss as explanations for the increase seen in medical malpractice rates: (1) the 75% rate of medical inflation from 1991 to 2002, (2) the end of a 12 year soft market in the insurance cycle, during which marketing was overemphasized and high investment yields used to compensate for losing operations, (3) a lack of adequate reserves by the insurance companies from 1997 to 2001, with large premium increases needed to rapidly restore reserves to safe levels, (4) a decline in investment income of 23% in 2001 and a further decline of 2.5% more in 2002, (5) a finding by Weiss Ratings of 34.4% of the nation’s insurers being “vulnerable to financial difficulties,” and (6) the number of medical malpractice insurance carriers falling from a peak of 274 in 1997 to 247 in 2002.101 Weiss concludes that “caps have been ineffective in reducing medical malpractice premiums for medical professionals.”102 Recommendations for the national problem of surging malpractice insurance rates included the medical profession taking increased responsibility for policing itself, insurance companies utilizing more prudent decisionmaking when balancing marketing with rate setting, and legislators abstaining from action on caps until definitive evidence of their benefit to medical providers.103 The value caps would have on the cost of medical malpractice insurance in New Jersey was brought up by New Jersey Assemblyman Paul D’Amato when he asked Patricia Costante, “[A]re you telling the insured physicians in New Jersey that if this State Legislature passes caps that you’ll guarantee that you won’t raise your premiums, in 101 Id. at 2. Id. at 3. 103 Id. 102 24 fact, you’ll reduce them?”104 Costante, Chairwoman and CEO of MIIX, replied “No, I’m not telling you that.”105 According to actuarial analysis by the firm of Tillinghast-Towers Perrin, “[a] cap of $500,000 is likely to be of very little benefit to physicians,” while a cap of $250,000 on non-economic damages would result in savings in the range of 5 to 7%.106 Catherine M. Sharkey, Associate Professor of Law at Columbia University, has taken the position that legislating caps on non-economic damages does not result in the desired effect of lowering malpractice awards.107 She describes a “crossover effect,” which states that when the non-economic portion of the award is limited by a cap, plaintiff attorneys seek, and juries award, larger economic damages. Sharkey conducted a multi-year and multi-state study of jury awards, and found no significant effects on overall damages as a result of the imposition of caps. She also states that her theory explains the recent trend of increasing economic damages awarded in medical malpractice cases.108 Public Citizen reiterates the following recommendations of J. Robert Hunter, Director of Insurance for the Consumer Federation of America: (1) a complete investigation of the medical liability insurance industry, including setting appropriate levels for surplus, realistic rates of premiums which reflect risk, and annual audits by state insurance regulators, (2) require individuals be evaluated using claims history when determining their premiums, as in other types of insurances, (3) reduce the percentage of 104 Public Citizen, supra, p. 30. Id. 106 Id. 107 Catherine M. Sharkey, “Unintended Consequences of Medical Malpractice Damages Caps,” NYU Law Review, Vol. 80, May 2005. 108 Id. 105 25 investment allowable in stocks, and to (4) the creation of a standby public insurer to provide coverage during hard markets and avoid situations where health care providers cannot find carriers.109 The argument is made against caps that they are discriminatory in that they most affect women, children, minorities and seniors. All of these groups statistically suffer less economic damages when injured since they sustain less loss of income.110 Lucinda M. Finley, professor at the University of Buffalo School of Law, authored “The Hidden Victims of Tort Reform: Women, Children, and the Elderly,” in which she performed a study of California jury verdicts 1992 to 2002 and concluded that MICRA reduced awards to women by 48% compared to 40% for men. Gynecologic cases in particular (not obstetric) showed a 64% reduction in awards.111 “The IOM proposal, which draws on established though largely untested reform ideas, recommends replacing much of current malpractice law with an administrative system of strict liability for clearly avoidable injuries.”112 This would result in a “notrial” system, capping non-economic damages according to a predetermined schedule (according to duration and severity of injury), but maintaining financial incentives to the provider to encourage patient safety.113 With regard to Congress passing a law instituting caps, Sage comments “[i]f Congress enacts MICRA-style caps on damages, no national tragedy will follow. But neither will any lasting benefit to health care be achieved.”114 109 Public Citizen, supra, p. 32-33. Id. at 68. 111 Id. at 72. 112 William Sage, supra at 29. 113 Id. at 30. 114 Id. at 31. 110 26 Bryan A. Liang offers an insightful and innovative solution to the issue of medical liability by addressing the concept of medical errors, which is clearly central to the entire issue.115 He labels the current system as “Shame and Blame,” which is individuallyoriented and based upon tort law to hold individuals responsible. “This culture places tremendous pressure on providers not to make any errors, or, more realistically, not to admit to any errors made.”116 Liang criticizes this system as “highly ineffective and even antithetical to error reduction.”117 Further, it does not fully compensate the injured, who have needs beyond financial awards, e.g. an explanation, an apology, and a chance to vent.118 Liang recommends a new paradigm, one of system accountability based upon public policy. The goals of this paradigm would be a reduction in error and a compensation of those injured. First, Liang proposes the establishment of incentives for health care providers to “collect, analyze, and share error information” on a national basis, with protection from lawsuit liability. This would serve the purpose of error reduction and system improvement. Second, a no fault or strict liability system would be created to compensate injured parties including mediation with the providers that would allow explanations or apologies to be given.119 Corrective actions on individuals might be necessary, but the goal of these would be “improvement of the system” and not “delivery of individual punishment as a fear-based incentive.”120 Brian A. Liang, MD, PhD, JD, “A Policy of System Safety: Shifting the Medical and Legal Paradigms to Effectively Address Error in Medicine,” Harvard Health Policy Review, Vol. 5, No. 1, Spring 2004. 116 Id. at 9. 117 Id. at 8. 118 Id. at 9. 119 Id. at 10. 120 Id. at 12. 115 27 Another alternative analysis of the medical malpractice liability crisis is found from Peter D. Jacobson, who states that it is “the culture of technology [which] drives medical liability.”121 From his perspective, technology is the principal driver of health care policy and delivery as well as of negligence law. It is the American culture which prizes high technology interventions that leads to unrealistic expectations on the part of patients and pressure on physicians to perform procedures using the newest technology.122 In his recommendations to ameliorate the increasing medical malpractice premium situation, Jacobson suggests the establishment of “court-appointed experts” with “an independent judicial panel to review and monitor expert testimony.”123 He calls the imposition of caps for non-economic damages “an illusory fix.”124 Jacobson advocates a no-fault approach in cases of “indeterminate causation,”125 without stating which cases would fall into this category and who would make that determination. The New Jersey Department of Banking and Insurance currently administers the Medical Malpractice Liability Insurance Premium Assistance Fund, offering practitioners in the fields of obstetrics, neurosurgery, and diagnostic radiology (including mammogram interpretation) rebates in the range of $10-15,000. This was established by the state in May 2004 in order to alleviate the burden of soaring malpractice premiums on those specialties. The program is funded through a $75 tax on health care providers and attorneys, and a $3 per year assessment on all workers who pay into the state unemployment insurance fund.126 Peter D. Jacobson, “Medical Liability and the Culture of Technology,” Pew Project on Medical Liability, 2004, available at www.medliabilitypa.org. 122 Id. at 2. 123 Id. at 4. 124 Id. at 3. 125 Id. at 4. 126 NJ Medical Malpractice Monthly, April 2005, p. 3. 121 28 The Medical Society of New Jersey (MSNJ) has responded to the crisis in part by the establishment of expert witness review panels. They “will review the testimony of expert witnesses in trials and will make determinations as to whether the expert testimony was ethically given.”127 The panel will produce a report that may be used to file ethics complaints against physician experts.128 NJPURE, a not-for-profit medical malpractice insurance provider founded in 2002, has introduced its own type of cap. It will not sell policies in excess of $1 million/$3 million, operating under the assumption that physicians are often over-insured, and “that the larger the policy limit, the larger the plaintiff attorney will seek in damages, the so-called ‘deep pocket’ theory.”129 CONCLUSIONS Medical malpractice has arisen as an industry out of the tort system of English law. Its cyclical history of crises in liability insurance availability and affordability continues, having just passed the most recent crisis. The events of 2002 were a “perfect storm,”130 and responsibility for those events falls on the insurance industry, our government, healthcare providers, attorneys, and society in general. Yet no group has been willing to accept its share of the responsibility and seek meaningful dialogue and change. 127 Physician Advocate, publication of the MSNJ, May 2005, v. 1, n. 1, p. 4. Id. 129 Lena Chang, supra, p. 2. 130 The inaccuracy of estimate of losses, and resultant low premiums leading to lack of adequate surplus; the bond market decline, causing a significant fall in investment income; the events of 9/11, which resulted in an increase in the reinsurance rates that medical malpractice insurance carriers had to pay; and the loss of carriers in the New Jersey market, which exacerbated the situation by decreasing supply and allowing those carriers remaining in the market to raise their rates without much concern about losing customers. 128 29 During the 1990’s, before the storm, malpractice rates were stable and the insurance industry under-estimated the funds that would be needed to satisfy claims to be made. Their concern was with increasing market share and profits. They acted as though the high bond rates would never drop. The government, which should have been regulating the industry, watched. Even in 2002 the New Jersey state legislature lacked the resolve to force the insurance industry to turn over its data, in order to allow the legislators to make informed decisions regarding changes needed in the system. The answer that the data did not exist was permitted, and no change regarding collection of that data has occurred. Health care providers can do more to lessen the incidence of medical errors, and to educate the public with regard to realistic expectations from health care in 2005. Attorneys have a vested interest in the litigation system and do not seek to discourage its use. Both the medical and legal professions could do better at policing themselves. This needs to occur in a way that allows practitioners with disproportionate numbers of errors to be retrained, to be given opportunities to improve their knowledge, skills, and techniques. It should not be what Liang called a “shame and blame system.”131 Greater emphasis in the calculation of compensation for medical services has to be given to the risk of error, and the costs involved. Reading mammograms, or practicing high-risk obstetrics, cannot be so expensive that we discourage people from choosing those careers. The present system of handling medical errors through malpractice litigation as a tort within the judicial system is expensive, inefficient, and ineffective. The goals of the 131 Liang, supra. FN 116. 30 system should be to reduce the incidence of medical errors, and to compensate those patients who sustain injuries as a result of errors that do occur. The first system change that needs to occur is a change in attitude in our society away from holding human beings to the standards of perfection. Medical care is largely delivered by people, and there will always be some mistakes made. There needs to be mechanisms in place to insure accurate reporting of events to allow for systemic problems to be documented and appreciated, and for corrections to be attempted. The actions of the American Society of Anesthesiologists, as described above, was exemplary and should serve as a template for other medical societies. The present litigation system does encourage under-reporting of errors, and misses the opportunity to improve the safety of patients. We need to have opportunities for patients to voice their concerns about the care they have received, other than seeking satisfaction through litigation. Health care providers, by listening and by explaining, can affirm their patients’ sense of worth. Rather than jury decisions on liability and damages, arbitration panels could be set up and their findings used to encourage resolution of disputes pre-trial. Mediation would also be very helpful in many of these cases. It seems probable to this author that now that the crisis of 2002 has passed, the chance for meaningful change has been lost. The Star Ledger no longer runs front page stories nor editorials on the subject, and neither government nor medical nor legal groups have it high on their agendas. But the insurance industry is cyclical, and another crisis will come. Now is the time when data should be collected in an objective fashion, and 31 laws that regulate the system put in place. When emotions are not too high is the time to seek dialogue between the involved groups, and improvement in the system. 32