Background paper on Wellness and
advertisement

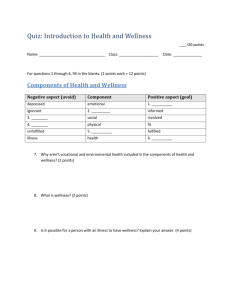
ATTACHMENT A Background paper on Wellness and Reablement approaches to delivering Home and Community Care Services in WA and Victoria 4 June 2010 WA Department of Health Victorian Department of Health Introduction This paper provides and overview on progress made in translating wellness and reablement approaches into practice in delivering Home and Community Care Services in WA and in Victoria. What are wellness and reablement? Wellness is a term that describes an approach to community care delivery that focuses on whole of system support for clients’ independence, by changing the way that all people involved in service delivery work with people receiving services. Reablement refers to short term targeted interventions pitched at tertiary prevention for people who already have a well established level of frailty or disability as a result of age, chronic disease or both. General, these interventions are low intensity and low in cost. In the UK, reablement has been defined as: ‘Services for people with poor physical or mental health to help them accommodate their illness by learning or re-learning the skills necessary for daily living.’ Both terms are used to distinguish the approaches they describe from a medical model of rehabilitation. Reablement programs tend to be led by allied health professionals, particularly physiotherapists and occupational therapists but can be delivered by vocationally qualified workers. They are highly goal focused and time limited. The goals, however, are not so much clinical goals but goals meaningful to the person/client that then motivate them to engage. The interventions tend to be functionally specific programs of exercise, adjusted tasks and physical activity, geared around the activities of daily living that, over a defined period, will increase the person’s strength, balance and physical condition, with consequential and collateral benefits for their ability to continue to perform the activities of daily living without assistance. A wellness approach involves redesigning the model of service delivery in community care, starting from the premise that people who are frail or disabled as a result of chronic disease or injury, have the capacity to make gains in their physical, social and emotional well-being and can continue to live autonomously and independently in the community if positively supported to do so. It involves reorienting the practice of people involved in service delivery and the management of services, so that those services can be tailored to respond to individual needs and goals. More flexible and responsive approaches to service delivery present challenges to the way service delivery is organised through service providers. MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 1 It focuses on achieving a more integrated response across different care settings that delivers a consistent message and expectation of support for people to continue to be self reliant and autonomous taking account the realities of their circumstances and disability. Both reablement and wellness offer potential benefits. If successful, they will maintain people in a stable and reasonably autonomous state in the community, containing their need to seek higher cost services through hospitals and/or residential aged care. In Australia, they leverage work already underway in other areas of the health and community care system including primary care, sub acute and acute services The purpose is to maximise older people’s capacity to self manage as well as their physical and psychosocial function with the expectation that this will reduce their need to use acute services and reduce their call on ongoing services. The evidence base There are two key drivers to this approach: our understanding of the evidence base of what it is to grow old well and increasing demand. Evidence for a ‘wellness’ or ‘active approach’ to service delivery ‘Wellness’ refers to a state of optimal physical and mental health, especially when maintained by proper diet, exercise, and social engagement It is not only dependent on the actions of a particular individual, but also on the dynamic relationship between people and the quality of their physical and social environment (McMurray, 2007). The concept of ‘wellness’ reflects a significant shift from ‘treatment’ to ‘prevention’ that has gradually occurred in health provision over the last 50 years. Even when people are elderly and frail, there is increasing evidence that adopting strategies for ‘wellness’ can make a positive difference to them (Stuck et al., 1999; Peel et al., 2005; Seeman & Crimmins, 2001). These strategies can include exercise (including low level activities such as shopping, cooking and gardening), using aids and equipment, improving nutrition, developing new ways of coping to deal with depressed mood or stress. These strategies often result in an improvement in well-being and morale for the older person and, at least in some cases, may reduce the number of hospital admissions and subsequently delay any need for permanent institutionalisation (McWilliam, Diehl-Jones, Jutai, & Tadrissi, 2000). In Western Australia, the term ‘wellness’ has been used to describe a different approach to people using home and community care services. While the emphasis is mainly on older people the approach is applicable to anyone receiving support. ‘Wellness’ emphasises encouraging independence (in which positive expectations, opportunities for development and positive experiences motivate improvement). It moves away from emphasising illness or dependence (in which there is a focus on difficulties, negative expectations and limited opportunities for development) (O’Connell, 2006). Developments in understanding ‘wellness’ are paralleled with more recent shifts in thinking that emphasise ‘successful ageing’: this focuses on promoting physical activity and active participation in society to maximise the physical and mental MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 2 well being of people as they age. It contrasts with a view that older adults disengage and withdraw from activities or society as they age (Buys & Miller, 2006). The World Health Organisation ‘Active Ageing’ framework (WHO, 2002) has been developed to overcome key criticisms of previous models. The term ‘active ageing’ was chosen in order to emphasise the valuable contribution older people make to their families, communities and society. It is defined as “the process of optimising opportunities for physical, social and mental well being throughout the life course, in order to extend healthy life expectancy, productivity and quality of life in older age (WHO, 2002, p. 12.) It emphasises the value of continued involvement across six life domains: social, economic, civic, cultural, spiritual and physical. The WHO definition of active ageing comprises three key pillars: • Participation: lifelong learning, paid and unpaid work; • Health: achieving and maintaining good physical and mental health in later life; and, • Safety: ensuring the “protection, safety and dignity of older people by addressing the social, financial and physical security rights and needs of people as they age”. There are some similarities between an Active Service Model and the WHO ‘Active Ageing Framework’; they both aim to keep older adults “engaged in life” for as long as possible. They both emphasise a focus on the quality of older people’s lives and their engagement in the community (Wistow, Waddington, & Godfrey, 2003). They are consistent with an ecological approach to wellness, which suggests that well being comes from family, community and social engagement, stepping outside ourselves and becoming enmeshed in a web of reciprocal relationships and interests (McMurray, 2007). From this perspective, improvements in a person’s health and functional capacity are necessary but not sufficient. Measures to (re)connect people into community involvement and social relationships are essential. Evidence for the efficacy of reablement programs Reablement has been the approach used in both the Silver Chain Home Independence Program and in the United Kingdom Homecare Reablement Program. In WA, the Silver Chain experience with its Home Independence Program demonstrated that it is possible in many cases, to reverse, slow down or prevent inability to continue to undertake the activities of daily living and that a person’s capabilities can be maintained, with modest interventions. The Home Independence Program aimed to develop and test a cost effective model of home care by designing services that would improve participants’ functional independence and thus reduce or limit their need for formal services. Over a six-year period, Silver Chain has trialled two new home care reablementfocussed programs (Home Independence Project (HIP) and Personal Enablement Program (PEP) aimed at persons aged 65years and over. The Home Independence Project (HIP) had a specific objective of developing and testing a more cost-effective model for home care by designing services that would maintain or improve individuals’ functional independence and thus reduce, or limit, their need for formal services. It was targeted at clients with low to medium needs at two points: either when they were first referred to home care or when they were being re-referred for increased home care services. MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 3 The Personal Enablement Program (PEP) was established on the success of the HIP project targeting clients being discharged from hospital. The programs were designed as a short-term intervention (up to 3 months) directed at “optimising functioning, preventing or delaying further functional decline, promoting healthy ageing and encouraging self-management of chronic diseases” (Lewin et al, 2008:15). The HIP model’s aim of promoting independence was designed both as a means of reducing an individual’s immediate need for services, and therefore reducing the demand for services, and as part of a longer term prevention strategy to assist the individual to maximise their health status and quality of life. It is about optimising function and promoting successful ageing. Some key features of the programs were: interdisciplinary team; comprehensive multi-dimensional assessment; goal-orientated care planning in partnership with client; targeted evidenced-based interventions (see below); minimised face-to-face contact, including telephone support and follow-up; use of participatory language with clients and families; recognition of importance of social support aspect of home care services and supporting clients to develop other avenues to gain this support; and use of local resources (Silver Chain, 2007) Areas of functioning and types of targeted, evidence-based interventions included: promotion of active engagement in activities of daily living (ADLs) and instrumental activities of daily living (IADLs). chronic disease self-management; falls prevention strategies; improvements or maintenance of skin integrity; and medications, continence and nutrition management. Benefits for people participating in these programs included: Improving their ability to self care and to perform everyday activities of daily living Minimising their need for ongoing home care services Reducing the likelihood that they will fall and injure themselves Increasing their "healthy ageing" behaviours Increased feelings of independence, autonomy and self efficacy Increasing involvement in the management of their health and abilities Avoiding hospital admission for reasons directly addressed by this program, for example, falls, medication or chronic disease mismanagement As part of its research, in 2002-04 Silver Chain conducted a randomised controlled trial of HIP. Some of the key findings were that: the HIP group demonstrated better ADLs, better mobility, reduced falls and higher morale; clients receiving HIP made it 15 times more likely that a client at three months would no longer be receiving assistance, and at 12 months, seven times more likely not to be needing ongoing services.(Lewin and Vandermeulen, 2006b). MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 4 In 2008, Lewin et al produced a peer-reviewed paper in Geriaction outlining the findings from a pilot and an operational trial of HIP (these were in addition to the controlled trial above). The purpose of the pilot was to test the program’s effectiveness in increasing participants ’independence (i.e. increased functionality and reduced need for services) and identifying any refinements required to the program. The program was found to be effective in both areas, with demonstrated gains in functioning of 41 clients who completed the program: 71% had less difficulty performing IADLs, 33% no longer needed ongoing services and 39% needed a lower level of service. In the UK, Homecare Reablement is now offered by 148 of 152 Councils, which have responsibility for community or social care. The program, similar to the HIP run by Silver Chain, targets people at the point of entry to social care and provides time limited (up to 2 months) programs of rehabilitation in the person’s home. Evaluations have shown that the reablement programs resulted in a reduction in the need for ongoing care packages compared with care as usual. A recently published retrospective longitudinal study found that 53-68% of people left reablement requiring no immediate home care package. Of that group, 3648% continued to require no formal assistance 2 years later. 34-54% had maintained or reduced their levels of assistance 2 years after reablement. In New Zealand, the Restorative Home Support program is based on care management, comprehensive assessment, and functional and repetitive ADL training. A key concept of the service is to base a support program on the goals and aspirations of the older person. The model relies on a multidisciplinary team (primarily registered nurse, physiotherapist and occupational therapist) providing an in depth support plan delivered by trained support workers or therapy aides under the supervision of the team. Analysis revealed a reduction in mortality, in comparison to usual care; an apparent reduction in risk of entry to residential care in comparison with usual care; no rise in carer stress in the intervention groups, despite people with complex needs continuing to live at home and an improvement in functional capacity of older adults. What has been done in WA? Following the success of the Home Independence Program pilot study, the WA Department of Health, via the Home and Community Care (HACC) Program funded Silver Chain to undertake a two year operational trial. The trial involved 418 participants14 and was again implemented by the same multidisciplinary team of allied health professionals that implemented the pilot. The key outcome measure for the trial was whether clients required ongoing home care services immediately after completing the program, and when assessed again after one year. At service end, 70% of clients no longer needed ongoing home care services and 7% of clients needed a lower level of service than at referral. One year later, 62% of those clients who had ceased services were still not using any home support services (Lewin et al, 2008). 2 The Wellness Approach to Community Home Care In March 2006, the WA HACC Program adopted a wellness approach as its policy position for the future delivery of HACC services across the state. From 2008/09 all growth applications from HACC-funded agencies needed to reflect a wellness approach in their service delivery models. MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 5 Wellness is a new organisational approach to HACC service delivery and requires organisational and attitudinal change (O’Connell, 2008, podcast). Wellness can be seen as the foundation stone of implementing a reablement program and whilst it is possible to take a wellness approach and not implement a reablement program it would be very difficult to implement a reablement program without also undertaking the accompanying organisational change towards a ‘wellness’ approach. Essentially a Wellness Approach is a shift away from a dependency model of care and support predominate in the HACC sector to one that enables an individual receiving a HACC service to build on their capacity by working with their abilities as opposed to their disabilities. Thereby supporting them to continue to do as much as appropriate for themselves. Currently the majority of services provided by HACC can be described as utilising a dependency model, in other words they provide services mainly to support or maintain an individual at an appropriate level. Services, including prepared meals, domestic care, personal care and social support are often provided in a standardised way to all eligible clients, and typically act as a substitute for client’s participation in caring for themselves. Emerging research over the last 10 years suggests that this way of delivering support, which is largely passive, with too much emphasis on task completion and doing as much as possible for a client may work against improving functional status and promoting independence. Refocussing of the current community care service model towards wellness/capacity building approach is one of many initiatives for WA Health. a The Wellness Approach also fits within the broader policy direction of The Model of Care for the Older Person developed by the WA Aged Care Network in response to initiatives undertaken by WA Health Networks. 2 (a) Key principles and components driving the approach The Wellness Approach is an initiative which explicitly focuses on building client capacity. HACC ‘clients’ in this context include both service recipients and their carers. The core components of the Approach are: Capacity building and social connectedness to maintain or promote a client’s capacity to live as independently as possible with or without HACC support A strength based holistic assessment and approach to support that promotes clients’ wellness and active participation in goal setting and decisions about their support needs Support and planning that can respond to people’s goals and are capable of maximising the client’s independence. Support focussed on functional and social goals with a focus on community connections Collaborative partnerships between individuals and providers; and, between providers for the benefit of clients Time limited support as appropriate Planned review process and changes to support plans to accommodate progress, including ongoing appropriateness of service MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 6 To support this process of change, WA HACC and CommunityWest Inc., a not forprofit organisation, began a partnership initiative in 2006 to develop the model and resources to support the philosophical and cultural change across the Program. As a result of this partnership, CommunityWest has: developed an Information Booklet – Wellness Approach to Community Home Care; developed Equipment & Resource Guide developed Client Case study examples developed a DVD – The Wellness Approach in WA developed change management and other materials to support organisations to commence a change process developed documentation for assessment and care planning; conducted training workshops for HACC agencies to assist them to adopt this new approach and made various presentations on the wellness approach; including The HACC National Forum, held in Melbourne in February 2008, which brought together over 400 key stakeholders to explore the evidence base and implications for more thoroughly adopting a wellness, capacity building and restorative care approach to HACC service provision A small team of experienced community care professionals work directly with organisations using the materials developed to support organisations through the change process. The teams work with providers cross a broad spectrum of resource development, consultations and partnerships, marketing, change management facilitation and quality improvement. Key Features Through this work CommunityWest identified some key features/strategies that have assisted agencies to implement a wellness approach. They can be categorised into two broad areas, organisational and service delivery, which have the following features: Organisational changing the mind set of all stakeholders, i.e. management, staff, volunteers clients and their families, about the views they hold in relation to the capacity of older people and people with disabilities to improve in their functioning; building staff awareness, skills and confidence to promote the wellness approach; undertaking staff training in the principles of the wellness approach and how to undertake assessments and develop client support plans using the approach. “Time spent at beginning, working with staff to gain confidence in new skills is well spent” (CommunityWest, 2008). Service Delivery looking at the reason behind the request for assistance or change in support instead of just providing services or increasing services; undertaking ability-based assessments and support plans; undertaking goal planning in partnership with client; undertaking time-limited interventions and services; client and carer education in principles of optimising function and wellbeing; regular reviews and changes to support plans to accommodate progress, MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 7 including looking at the appropriateness of continuing service; an emphasis on social networks and community connections to link clients back to their communities; and at the end of service, looking at the appropriateness of connecting clients with mainstream community programs /services. 2 (b) Evaluation In 2008 a small evaluation (25 Providers) of the Wellness Approach was conducted by independent researchers from Edith Cowan University. The purpose of the evaluation was to ascertain the process of change to date with regard to knowledge, attitudes and beliefs about Wellness, organisations commitment to the approach, and organisational impacts of the implementation of the approach. The evaluation findings suggested that West Australian HACC agencies associate Wellness with the concept of maximising client independence and believed it provided a sound philosophical basis for service delivery. HACC agencies that had made progress with the implementation of Wellness generally cited multiple benefits of the change process, including increased staff satisfaction, client and carer benefits, and greater equity in service delivery. 2 (c) WA Assessment Framework 2009 In 2009 The WA HACC Program developed an Assessment Framework document that provides a broad outline of the redesign of HACC services to support the streamlining of access, information, eligibility screening and face to face assessment for people needing support to remain living independently in the community. The overall goal of the Assessment Framework is to develop, support and build on best practice that builds formal linkages between all key community care service providers to effectively manage client pathways, provide appropriately targeted service responses and refocus service delivery towards an approach that supports the implementation of the philosophy of Wellness to maintain and improve client independence wherever possible. The framework will be implemented in the metropolitan area from 1 January 2011. 3 Where is WA now To date over 80% of HACC providers in West Australia have commenced organisational changes towards implementing a Wellness Approach. The evaluation found that among the forces for progress with implementation was a clearly expressed view by most organisations that Wellness was the best philosophy for services and that sound progress was being made with implementation, The WA Assessment Framework amongst other reforms in WA will support the bedding down of the approach as Access to community care is streamlined, assessment practices become more consistent and support is delivered consistently in a manner that focuses on building the client’s capacity and enabling them to remain at their optimal level of independence. What has been done in Victoria? MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 8 The Victorian HACC Active Service Model (ASM) is characterised as a quality improvement initiative that explicitly focuses on promoting capacity building and restorative care in community care service delivery. It has taken as its point of departure the work on wellness undertaken in WA with some elements of reablement programs in the UK and NZ. The Victorian HACC Active Service Model is based on the premise that all clients have the potential to make gains in their wellbeing and that Home and Community Care services can support improvement. Our approach is to strengthen good practice and build capability through quality improvement. The goal of the Active Service Model is for people in the HACC target group to live in the community as independently and autonomously as possible. In this context, independence refers to the capacity of people to manage the day to day activities of their daily life. Autonomy refers to making decisions about one’s life. Not all HACC clients will be able to live independently and autonomously, but the goal of this initiative is to ensure that clients are able to gain the greatest level of independence they can and want to achieve, and equally, that they can be as actively involved in making decisions about their life as they can and want to be – such as the type of services they receive and the goals they wish to achieve. The principles underpinning the Active Service Model are that: people wish to remain autonomous people have the potential to improve their capacity people’s needs should be viewed in an holistic way HACC services should be organised around the person and his or her carer, that is, the person should not be simply slotted into existing services, and a person’s needs are best met where there are strong partnerships and collaborative working relationships between the person; their carers and family; support workers and between service providers. From a service delivery perspective core components are: promoting a ‘wellness’ or ‘active ageing’ approach that emphasises optimal physical and mental health of older people and younger people with disabilities and acknowledging the importance of social connections to maintain wellness an holistic and family-centred approach to care that promotes wellness actively involving clients in setting goals and making decisions about their care and providing timely and flexible services that support people to reach their goals. Projects to test approach in practice – results of evaluations Victoria has undertaken a broad range of developmental work and pilot projects over the past three years relevant to this approach. A major focus has been strengthening assessment as good quality home based assessment and care planning are key enablers for the ASM approach. The Victorian Assessment Framework foreshadowed this and its implantation has now been integrated with the ASM. Strategies have included: strengthening working relationships between HACC Assessment Services and Allied Health through: o Co-locating allied health staff with assessment staff o Developing joint training opportunities o Promoting opportunities for joint assessment, secondary consultation and case conferencing MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 9 Developing a range of partnership protocols and practices within local service systems to enhance practice. Strengthening the understanding of practice through the development of a HACC Assessment Practice guide that helps to put approach into operation. Other areas of pilot project focus have included: Developing models of home care that better support clients to do things for themselves Exploring how low maintenance gardens can contribute to greater independence for clients Providing social support options from a perspective that enhances nutrition, physical activity and emotional well being Focussing district nursing on how clinical services can adapt to this approach, with a particular focus on continence Building partnerships and alliances between providers to support the approach Implementation steps Victoria is approaching the implementation of the ASM as a longer term quality improvement strategy building on existing strengths of the system. It is a major change management project. Victoria released an ASM implementation plan in February 2010. This set out a range of strategies and tasks to support implementation until the end of the current HACC triennium in 30 June 2010. The first task for HACC funded agencies is to assess their strengths and weaknesses in taking an ASM approach and develop an initial implementation plan for change. The Victorian Department of Health is developing a range of resources to assist them in this process including the development of a practice review tool to use within their agencies. Regional Industry Consultants have been established to provide capacity building support to organisations and Regional staff in implementing the approach. Planning and development is coordinated with a range of other related initiatives being put into place such as implementation of the Victorian HACC Assessment Framework, the Diversity Planning Framework and a major review of social support and respite services. The direction is also consistent with other measures taken in other related settings such as chronic disease management and disability services. Next steps Victoria is now considering ways of mobilising resources in the HACC program to enable a targeted reablement focus within the broader context of a wellness or active service model approach to service provision. We are also developing an evaluation framework, based on the HACC MDS and incorporating other measures to track the impact of the change. Lessons from this experience Key learnings from HACC agencies in WA that have begun implementing a wellness approach can be categorised under organisational, staff and clients: Organisational wellness is a philosophical change and needs to be part of an agency’s overall vision and approach to service delivery (ie organisational culture needs to support this way of working and put structures in place to ensure change takes place at all staffing levels; MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 10 Staff the receptive context is important, it needs senior management to be key drivers; there needs to be a ‘can do’ organisational culture; and a history of successful change; good communication is critical; there must be both early and ongoing consistent messaging and dissemination of information to all stakeholders; there should be a steering group, led by a Senior Manager and including a cross-section of staff, which has decision-making powers and oversees implementation; policies and procedures need to support this new way of working (ie referral processes, reviews and staff feedback mechanisms; and a strategy for staff education and training in the approach and how to implement it needs to be developed. having the support of home care coordinators/supervisors is critical in persuading support workers of the merits of the approach. Service Delivery approach staged implementation is important to allow for development and testing; mapping the processes and having action items helps the implementation process; and it is easier to implement a wellness approach with new HACC clients but it is also possible to implement with existing HACC clients but the changes need to be implemented more slowly. (CommunityWest, 2008). Findings from work to date in Victoria have been: the majority of clients involved in pilots have embraced the concept and made good progress through the approach. Identifying and harnessing the motivation of clients is crucial in moving to this approach and goal setting that is meaningful to clients as part of the assessment process generates client motivation. There are no clear indicators, based on the evidence available that this approach is only good for a particular target group and evidence that this approach can benefit all recipients of community care services. It is more difficult to engage people who are already in receipt of community care services so the approach taken is to work with new clients to a service to enable more positive expectations to be set from the start of service engagement. For many staff, this approach represents a major philosophical shift and challenges traditional habits and assumptions about how they work and make decisions. Although some staff find this challenging, Victoria’s work to date and overseas experience find that most are enthused by the philosophy and find increased job satisfaction through the approach. The nature of successful change requires a whole of organisation engagement, with managers playing a crucial role. For implementation to be sustained, each organisation needs to review its systems and supports, across the clients experience of the service Conclusions The implementation of the Wellness Approach in WA and the Active Service Model in Victoria is based on the premise that clients have the potential to make gains in their wellbeing and that the range of HACC services can facilitate this. The approach supports the core aims of the HACC Program but also offers a way of building on the Program’s intent of enabling people to maintain or maximise their independence. MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 11 Targeted enablement programmes combined with a sector wide philosophical change towards a Wellness Approach or Active Service Model, can deliver the core aims of the HACC program by more effectively meeting the needs of future clients and carers. MACA Meeting 10 June 2010 – Agenda Item 9 – Attachment A (Issued 8 June 2010) 12