Experience of application Perchlozone® anti
advertisement
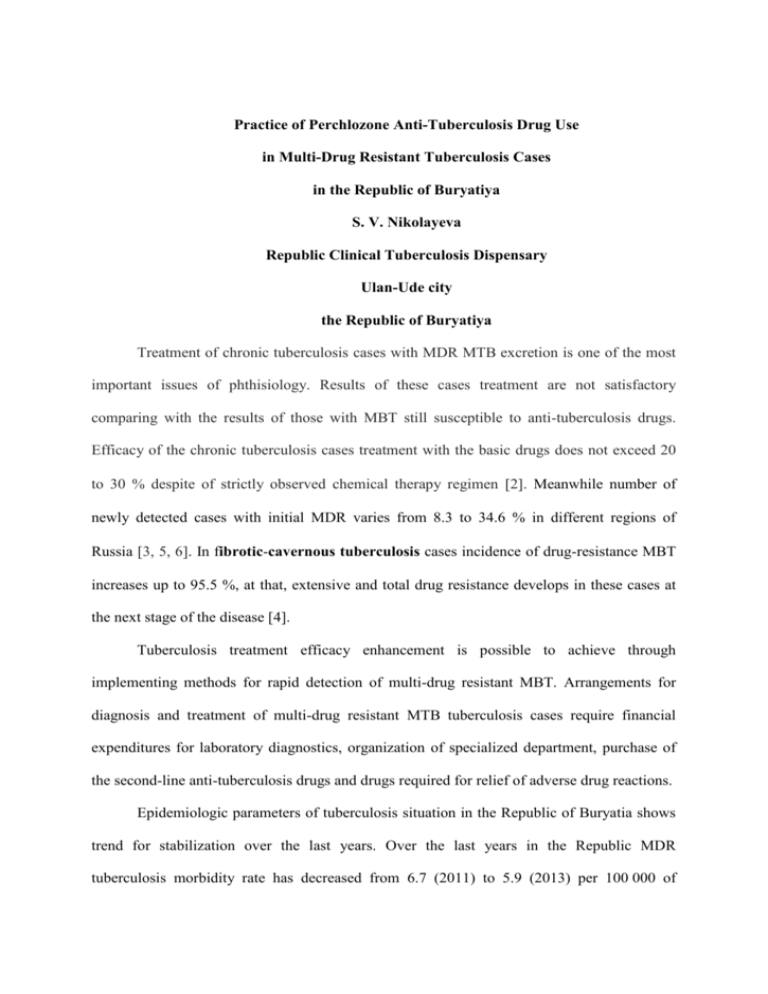
Practice of Perchlozone Anti-Tuberculosis Drug Use in Multi-Drug Resistant Tuberculosis Cases in the Republic of Buryatiya S. V. Nikolayeva Republic Clinical Tuberculosis Dispensary Ulan-Ude city the Republic of Buryatiya Treatment of chronic tuberculosis cases with MDR MTB excretion is one of the most important issues of phthisiology. Results of these cases treatment are not satisfactory comparing with the results of those with MBT still susceptible to anti-tuberculosis drugs. Efficacy of the chronic tuberculosis cases treatment with the basic drugs does not exceed 20 to 30 % despite of strictly observed chemical therapy regimen 2. Meanwhile number of newly detected cases with initial MDR varies from 8.3 to 34.6 % in different regions of Russia 3, 5, 6. In fibrotic-cavernous tuberculosis cases incidence of drug-resistance MBT increases up to 95.5 %, at that, extensive and total drug resistance develops in these cases at the next stage of the disease [4]. Tuberculosis treatment efficacy enhancement is possible to achieve through implementing methods for rapid detection of multi-drug resistant MBT. Arrangements for diagnosis and treatment of multi-drug resistant MTB tuberculosis cases require financial expenditures for laboratory diagnostics, organization of specialized department, purchase of the second-line anti-tuberculosis drugs and drugs required for relief of adverse drug reactions. Epidemiologic parameters of tuberculosis situation in the Republic of Buryatia shows trend for stabilization over the last years. Over the last years in the Republic MDR tuberculosis morbidity rate has decreased from 6.7 (2011) to 5.9 (2013) per 100 000 of population; MDR-MTB prevalence decreased from 62.4 (2011) to 53.9 (2013). In the Republic, treatment of the tuberculosis cases (2011 cohort) with initial MDR-MTB using the 4th regimen was completed with sputum conversion in 78% of cases, and in 41.9 % in cases with acquired MDR. Challenges are faced in treatment of tuberculosis cases with pre-XDR and XDR causative agent applying 5th regimen implying use of backup drugs for bacteriologically proved drug resistance. No external quality control is performed in the Russian Federation concerning reliability of results obtained by pirazinamide and second-line drugs resistance analysis. Moreover, list of anti-tuberculosis drugs purchased for federal budget assignations and used for treatment of MDR-MTB tuberculosis cases does not include drugs of the fifth line. Costly drugs are purchased for assignations from the federation subject budget and therefore treatment as per the 5th regimen in the most cases does not comply with the standards. The study objective is evaluation of perchlozone anti-tuberculosis drug efficacy in the course of complex therapy in pulmonary tuberculosis cases with MDR and XDR in the Republic of Buryatia. Materials and Methods Perchlozone, a new anti-tuberculosis drug, was used in complex therapy of pulmonary tuberculosis cases with MDR and XDR at the facilities of a MDR specialized department of the Republican Tuberculosis Dispensary in 2013-2014. Drug susceptibility of the causative agent was analyzed by method of absolute concentration in solid medium with anti-tuberculosis drugs of the 1st and 2nd line using ВАСТЕС MGIT-960 automated system. Monitoring in the course of therapy included monthly microbiological examination of sputum (smear and inoculation), quarterly thoracic cage roentgenography, multi-layer CT of lungs, control and management of adverse drug reactions, evaluation of liver and kidney function with frequency depending on initial state, age and coexistent diseases of the case. Perchlozone was administered in a daily dose of 600 mg and 800 mg depending on the body weight, totally 120 of doses was administered during the therapy. Two groups of cases were evaluated. The patients selected for the 1st group (n=28) receiving combination standard 4th regimen and perchlozone were chronic tuberculosis cases with MDR and previously completed course of 4th regimen treatment with failure or XDR tuberculosis cases. There were 24 (85.7 %) males and 4 (14.3 %) females in the 1st group. The second group (n=30) received the standard 4th regimen i.e. levofloxacin, capreomycin, terizidone, prothionamide, PAS and pyrazinamide or ethambutol depending on susceptibility. There were 22 (73.3%) males and 8 (26.7%) females in the 2nd group. The groups were identical with regards to age (average age of the 1st group = 34.6 years, the 2nd group = 36.2 years). Severity of the tuberculosis clinical manifestations in the groups was significantly different (p<0.05). Chronic form of tuberculosis significantly prevailed in the 1st group of cases (85.6 %) i. e. 13 (46.4 %) of patients suffered fibrotic-cavernous tuberculosis, 11 (39.2 %) of patients suffered disseminated tuberculosis. The 2nd group was characterized by more favourable forms of tuberculosis prevailing i.e. infiltrative process prevailed occurring in 17 (56.7 %) of cases, fibrotic-cavernous tuberculosis was detected in 7 (23.3 %) of cases and disseminated form was detected in 4 (13.3 %) of cases. There was significant difference between the groups with regards to drug resistance pattern. A statistically more wide resistance pattern was observed in the 1st group (р<0.05): HRS was in 2 (7.1%), НRSЕ was in 10 (35.7%), НRSЕZ was in 16 (57.1%) of cases. Extensive second-line drug resistance was observed in 76.8 % of patients receiving perchlozone (р<0.01). Resistance to 3 basic drugs was prevailing in the 2nd group i. e. HRS was in 20 (66.7%) of cases, HRSE was in 5 (16.7%) and HRSK was in 2 (6.6%) of cases and HREZ was in 1 case. There were single cases of resistance to fluoroquinolones, PAS, prothionamide observed. Study Results Clinical findings at the pre-admission stage in the most (17 (60,7%)) of the 1st group cases were moderate symptoms of intoxication, respiratory compromise; the patients’ condition was referred to moderate grade severity comparing with 11 patients with moderate severity condition in the 2nd group (36.6. %). Roentgenological findings were evaluated after the perchlozone administration course was completed. Taking into consideration low probability of cavern closure in the 1st group consistent mainly of chronic tuberculosis cases as well as impossibility of surgical treatment due to tuberculosis prevalence and high risk of complication development after surgery, infiltration resorption, stable roentgenological findings as well as forming of cicatrix and cirrhotic changes were considered as the positive roentgenological dynamics. Positive clinical dynamics included complete resolution of intoxication symptoms and respiratory compromise manifestation relief along with roentgenological regress of inflammatory changes in lungs by the time of transition to maintaining phase; this positive clinical dynamics of the patients’ condition was observed with statistical significance in the 2nd group (in 22 (73.3 %) of cases comparing with 12 (42.9 %) of cases in the 1st group) (p<0.05). There were no significant difference in tolerance to perchlozone and anti-tuberculosis drugs of the backup line; the tolerance was dependent on such factors as age, coexistent diseases, cacoethes and it was higher in the 2nd group than in the 1st group with statistical significance i.e. 21.5 % and 43.4 % respectively (р<0.05). After 4 months from the treatment beginning smear test results became negative in 10 (35.8 %) of cases in the 1st group comparing with 17 (56.6 %) of cases in the second group. Conclusion It is possible to achieve recovery of the most tuberculosis cases despite presence of the drug-resistant MBT, coexistent diseases and development of adverse drug reactions. Use of perchlozone in complex treatment of tuberculosis cases with XDR of the causative agent, unfavourable prognosis of the tuberculosis treatment outcomes allows to stabilize clinical and roentgenological manifestations of chronic tuberculosis process in 42.9 % of cases and achieve negative results of microbiological tests in 35.8 % of cases, which is proved by statistically significant data. List of References 1. Мишин В.Ю. Современная стратегия лечения лекарственно- устойчивого туберкулеза легких // Лечащий врач.- 2000.- № 3.- С.1-7.1. (Mishin V. Y. Modern Strategy of Drug-Resistant Pulmonary Tuberculosis Treatment) 2. Х. М. множественной Даутова, Б.Т.Кумисбаева, лекарственной П.М. резистентности у Джазыбекова. больных Проблема хроническим туберкулезом легких (обзор литертуры) // Научно-практический журнал. – Вестник КАЗНМУ. – 2012. – № 3. (H. M. Dautova, B. T. Kumisbayeva, P. M. Dzhazybekova Problem of Multi-Drug Resistance in Chronic Pulmonary Tuberculosis Cases (Publications Review)) 3. Дауров Р.Б. «Клинико-рентгенологическая динамика у впервые выявленных больных туберкулезом легких с множественной лекарственной устойчивостью микобактерий при раннем назначении резервной схемы химиотерапии по данным тестсистемы «ТБ-Биочип»». // Туберкулез и болезни легких. – 2010. – № 4. – С. 10 – 13. (Daurov R. B. Clinical and Roentgenological Dynamics in Newly Detected Cases of Pulmonary Tuberculosis with Multi-Drug Resistance of Micobacterium Tuberculosis at Early Use of Backup Chemical Therapy as per “TB-Biochip" Test System Data) 4. Марьяндышев, А. Множественная лекарственная устойчивость микробактерий туберкулеза / А. Марьяндышев // Мед. газ. – 2009. - № 17. – С. 8-9. (Maryandyshev A. Multi-Drug Resistance of Micobacteriom Tuberculosis) 5. Самойлова А.Г., Марьяндышев А.О. Лекарственная устойчивость микобактерий туберкулеза – актуальная проблема фтизиатрии – Пробл. туб. – 2005. - № 7. – С. 3 – 9. (Samoylova A. G., Maryandyshev A. O., Drug Resistance of Micobacterium Tuberculosis – Urgent Problem of Phthisiatry) 6. Шилова М.В. Туберкулез в России в 2003 г. – М., 2004. – 104 с. (Shilova M. V. Tuberculosis in Russia) Summary Epidemiologic parameters of tuberculosis situation in the Republic of Buryatia shows trend for stabilization over the last years. A study of perchlozone anti-tuberculosis drug efficacy in the course of complex therapy in pulmonary tuberculosis cases with MDR and XDR was carried out in 2013-2014. The first group of the study (n=28) receiving combination of a standard 4th regimen and perchlozone included 85.7 % of chronic tuberculosis cases with MDR and XDR. The second group (n=30) received the standard 4th regimen. Extensive second-line drug resistance was observed in 76.8 % of patients receiving perchlozone (р<0.01). Resistance to 3 basic drugs was prevailing (66.7 %) in the 2nd group; there were single cases of resistance to fluoroquinolones observed. Tolerance to perchlozone was not significantly different from tolerance to the backup line anti-tuberculosis drugs. The result of the treatment was positive clinical dynamics of the patients' condition including complete resolution of intoxication symptoms and respiratory compromise manifestation relief along with roentgenological regress of inflammatory changes in lungs by the time of transition to maintaining phase; this positive clinical dynamics of the patients’ condition was observed with statistical significance in the 2nd group (in 22 (73.3 %) of cases comparing with 12 (42.9 %) of cases in the 1st group) (p<0,05). After 4 months from the treatment beginning smear test results became negative in 10 (35.8 %) of cases in the 1st group comparing with 17 (56.6 %) of cases in the second group. Use of perchlozone in complex treatment of tuberculosis cases with XDR of the causative agent, unfavourable prognosis of the tuberculosis treatment outcomes allows to stabilize clinical and roentgenological manifestations of chronic tuberculosis process in 42.9 % of cases and achieve negative results of microbiological tests in 35.8 % of cases in the first group which is proved by statistically significant data. Key words: tuberculosis, multi-drug resistance, extensive drug resistance, perchlozone Author: Nikolayeva Sayzhina Vasilievna Head Physician Deputy, medical practice, Candidate of Medicine 670045, Russia, the Republic of Buryatia, Ulan-Ude city, Klenovaya st., 146 nachmed_rptd@mail.ru Phone: 8 (301 – 2) 27-14-47 Fax: 8 (301 – 2) 26-71-00