Control The Body Weight
advertisement
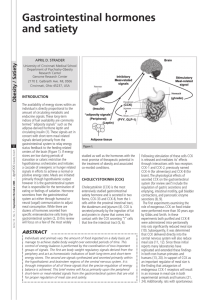
Introduction The control of energy balance requires an understanding of the terms hunger, appetite and satiety. Hunger is the craving for food that is associated with objective sensations and is a general sensation localized to the stomach region; it appears when the stomach is empty and coincides with contractions detected by mechanoreceptors in the stomach wall. Appetite by contrast is the desire for specific types and quantity of food and satiety is the opposite of hunger resulting from a filling meal. The latter can be divided be divided into two components, pre and post absorptive. As in drinking, food consumption ceases before absorption of food from the gastrointestinal tract (GIT) has corrected any energy imbalance. In addition, a post absorptive component prevents hunger. For the body to be in energy balance the energy content of food must correspond to energy expenditure of muscular work, growth, reconstruction and loss of heat from the body. Although these notes will be limited to control of food intake we do have appetites for minerals if they are lacking. For example you can show a preference for saline to water if you lack adrenal glands or calcium to water if you lack parathyroid function. What are the factors influencing food intake? increased plasma glucose concentration (-) increased production of hormones such as insulin and glucagon and the GIT hormones (-) increased body temperature (-) increased palatability of food (+) stress (+/-) conditioned responses (+/-) activation of stomach/ duodenal receptors, stretch receptors and chemo receptors (-) Physiological control mechanisms. The physiological control mechanisms can be broadly divided into short or long term regulation. There are two theories that are reported to be important in the short term regulation: glucostatic theory of hunger plasma amino acid levels In the first, the glucostatic hypothesis suggests that the availability of glucose appears to play a crucial role in eliciting hunger. There is ample evidence for glucoreceptors in the CNS. In addition the hypothalamus is known to receive afferent information from the liver, stomach & small intestine via the vagus. It has also been shown that depletion of glucoreceptors causes severe disturbances of feeding but there is some question as to whether glucose is the only regulator. In contrast there is only one theory that is reported to be important in long term regulation, the lipostatic hypothesis. Lipostatic hypothesis: Fat (adipose tissue) of mammals represents an organ which is widely distributed throughout the body and fluctuates according to metabolic energy demands. Mature adipocyte tissue communicates with the central nervous system via a hormone circuit that controls satiety. Excessive food intake leads to the deposition of fat, insufficient food intake decreases fat deposits. One can therefore assume that the body can monitor the products of fat metabolism. Obesity comprises complex interactions of genetic and environmental factors and so the mechanism that balances food intake and energy expenditure determines those of us that will be obese and those that will be lean. One of the molecules that regulates energy balance is the product of the obese (ob) gene, LEPTIN, a 16kD protein (from the prefix LEPT- or LEPTO- meaning thin and the suffix -IN commonly given to proteins) which is probably able to function as part of the signalling pathway from adipose tissue that acts to regulate body fat deposits due to its action on satiety. Leptin, via its action on metabolism and appetite, is able to; lower body weight lower percentage body fat reduce food intake reduce serum concentrations of glucose reduce serum concentrations of insulin increase metabolic rate increase body temperature increase activity inhibit neuropeptide Y (NPY) synthesis and release. The thermostatic hypothesis The third hypothesis implicated in the control of body weight is the thermostatic hypothesis. It has been shown that warm-blooded animals consume food in amounts inversely proportional to environmental temperature. Central thermoreceptors could act as sensors of overall energy balance. This theory is supported by evidence that local cooling of the CNS can alter feeding behaviour although cooling could, in theory alter the activity of any neurones and may not be specific. The main evidence for this hypothesis involves the reaction to fever when there is a reduction in food intake. This is more likely to be the result of the action of cytokines - cf cytokines later in this account. Sensory mecahnisms involved in the control of food intake The sensory mechanisms involved in control of food intake include those from olfactory, taste and mechanoreceptors in the mouth, throat & esophagus. Evidence from animals with esophageal fistulae show that they have more meals but do spontaneously stop eating. Much of the sensory information from the thorax and abdomen travels via the Xth cranial nerve (vague) which is able to detect gastrointestinal filling by use of mechanoreceptors in the stomach wall and chemoreceptors in stomach, upper small intestine & hepatic portal bed. We all know that the effect of a "full" stomach gives us the feeling of satiety therefore we can assume that gastric mechanoreceptors are involved. We also know that if we tube feed animals before their mealtimes then there is a reduction in subsequent meals. This is due not only to stretching of mechanoreceptors but also chemoreceptors sensitive to glucose or amino acids. The arrival of nutrients in the GIT supresses intake. It is therefore highly probable that vagal coeliac afferents are critical for preabsorptive detection of food. HYPOTHALAMIC CENTRES. The hypothalamus is thought to be the most important central relay and integration centre for both the sense of hunger and satiety but is not involved in the basic mechanical features of the feeding process i.e. salivation, preparation of food and swallowing. These are all controlled by the brainstem. The involvement of the hypothalamus results from studies where regions have been either electrically stimulated or destroyed and the effect on eating observed. Evidence has also been provided from experiments where the activity of neurones has been recorded whilst sensory systems associated with food consumption have been activated. Two main areas have been proposed; SATIETY CENTRE (ventromedial hypothalamus) bilaterally destroy the ventromedial hypothalamus, rise in plasma insulin concentration, inhibition of lipolysis, overeating electrical stimulation increases sympathetic outflow, inhibits pancreatic insulin secretion, stimulates lipolysis in adipose tissue and stops eating. HUNGER CENTRE (lateral hypothalamus) receives olfactory, gustatory & visual inputs senses changes in glucose concentration bilaterally destroy the lateral hypothalamus, refusal to eat. If you stimulate it you overeat. inhibited by glucose, insulin, CCK and vagal afferents Neuropeptides as satiety factors; Many peptides have been shown to modulate nutrient intake. Broadly speaking these can be divided into hormones from the pancreas, GIT or the pituitary. Gastrointestinal hormones - all decrease food intake. Cholecystokinin (CCK) is a prototypic satiety agent which decreases feeding. Although CCK is a GIT hormone it is extensively distributed within the central nervous system (CNS). The role of CCK is complex since there is evidence that it interacts with dopamine and opiate systems to also modulate psychoses and anxiety. GIT hormone CCK (cholecystokinin) which is released mainly in response to fat entering the duodenum plays an important role in satiety released by duodenal mucosa when food is present in it CCK injected into hungry animals causes them to stop eating cutting the vagus nerves block the action of CCK. although there are other peptides, including gastrin-releasing peptide and bombesin, known to be "satiety factors" CCK appears to be the most important. Pancreatic hormones - all decrease food intake insulin (unless accompanied by hypoglycaemia) appears to play a role in the physiological control of feeding. glucagon and glucagon-like peptide amide (GLP-1), the latter, when injected intracereboventicularly (ICV) inhibits feeding and GLP-1 receptors are present in the hypothalamus, particularly PVN and parts of the amygdala AMYLIN (also known as Islet amyloid polypeptide - IAPP) is a hormone co-stored and coreleased with insulin. It interferes with glucose metabolism and may act as a "satiety" factor. pancreatic polypeptide enterostatin. Pituitary hormones The evidence for the normal involvement of pituitary hormones in the control of food intake is limited and is based on observations of eating habits when there is excessive hormonal production. Vasopressin and thyrotropin-releasing hormone (TRH) decrease food intake. Melanocyte stimulating hormone (dMSH), growth hormone and prolactin have all been shown to increase food intake. The Cytokines The cytokines are released from activated cells during acute and chronic pathological conditions of infection and malignancy. Most of us have experienced the former with its accompanying suppression of feeding. This suppression is also a familiar problem in the latter. The intracerebroventricular (ICV) injection of interleukin 1 (IL-1) decreases short and long term food intake, interferon has a similar influence. The cytokines bring about their action via the hypothalamus by acting directly on glucosesensitive neurones in the ventromedial hypothalamus (the "satiety" centre) and the lateral hypothalamus (the "hunger" centre). Methods of Measuring Body Composition. BMI- Body Mass Index is measure of body fat based on height and weight that applies to both adult men and woman. BMI = weight (kg)/ (height*height) Underweight < 18.5 Normal weight = 18.5-24.9 Overweight = 25-29.9 Obesity = or greater 30 Functions of fat. 1. stored energy 2. structural ( cell membrane) 3. involve in nerve conduction 4. critical for absorption of fat-soluble vitamins 5. backbone for steroids