Implementation - Self Learning Module.doc
advertisement

The PEP uP Protocol
Self-learning Module
Your ICU is one of 20 sites across North America participating in the PEP uP Protocol. The main
objective of this study is to evaluate the effect of an innovative enteral feeding protocol and
nursing education program on the adequacy of enteral feeding delivery. Each ICU will recruit 30
patients at baseline prior to implementing the protocol and another 30 patients after implementation of
the protocol to evaluate your success with it. We will also document safety incidents related to enteral
nutrition (EN), evaluate the protocol from the perspective of the nurses who use it, and capture 60 day
hospital outcomes i.e. length of stay, mortality, etc.
Why is this important?
Adequate nutrition is very important to support the optimal recovery of critically ill patients. Sufficient
nutrition helps to:
Provide fuel for cellular metabolism
Prevent protein loss and muscle wasting
Decrease ventilator time
Help prevent infection including ventilator associated pneumonia
Promote healthy wound healing
Decrease ICU length of stay
Reduce mortality
Did you know?
International audits of nutrition practices have found that ICU patients only receive 40-50% of their
nutritional requirements. This means that ICU patients worldwide are iatrogenically malnourished – in
other words, we made them that way!
1
What’s New?
There a few things about the PEP uP Protocol that may be quite different from how you are providing EN
currently. These include:
All patients will initially receive an enteral formula called Peptamen 1.5
All patients will start on the protein supplement Beneprotein®:
o 2 packets (14 g) mixed in 120 ml water administered bid via OG/NG
All patients will be given metoclopramide on Day 1 of enteral feeding - 10 mg IV q 6h
The gastric residual volume threshold is 300 ml
The enteral feeding initiation orders shown in Appendix 1 is the form that the admitting physician or
resident will use to order the appropriate feeding option for your patient. You will notice that NPO is
rarely an option; this should be chosen only when there is an absolute contraindication to enteral
feeding. You will see some examples of contraindications given in the pre-printed orders. Even the
sickest patient should be started on a low level of feeding, trophic feeds, to help maintain gut health. Gut
disuse (aka NPO) causes loss of functional and structural integrity of the GI tract and is associated with
increased complications.
The other big difference you will see is that your patients’ feeds will now be based on a 24 hour target
volume rather than the traditional hourly rate you are likely used to. This means that you may be
changing hourly rates throughout the day to make up for times when the feeds are off.
The case studies that follow will help you to work through these changes and become familiar with the
PEP uP protocol. As you work through the case studies, we will ask you questions to test your
knowledge. For the first case study, the answers are provided immediately after the questions. For the
second case study, answers are found in the Appendix and there is an answer key at the end. If you are
completing the electronic version of the learning module, when you come to red text, place your mouse
over the text, then control/click and this will link directly to the highlighted area of the learning module.
If you are completing the paper based version of the learning module, refer to the appropriate section of
the Appendix.
If you have any questions, please contact your Protocol Implementation Team (PIT) Crew:
{ Add contact details}
2
Case Studies
Case Study Number 1
A 35 year old male was admitted at 0400h following a gunshot wound to chest. His injuries include
massive trauma to right arm, left chest and left shoulder. He experienced 3 intra-operative cardiac
arrests. On arrival to the ICU he is in pulmonary edema, right heart failure , vasopressin at 0.04 units/hr
and his levophed continues to be titrated up to maintain a MAP of 60 mmHg; the current rate is 25
mcg/min. His weighs 70Kg and he is 1.74m tall.
Questions:
1. On admission you inform the medical team that the patient is NPO. Which of the following
interventions do you anticipate?
a. Continue NPO
b. Volume based enteral feeds
c. Enteral feeds at 25/hr
d. Trophic feeds
If you chose trophic feeds you are correct. Because he is still requires vasopressors to
maintain a MAP of 60 mmHg he may not be ready to start on volume based feeds. Starting on
trophic feeds at 10 ml/hr will help protect his gut until he is stable.
2. He is oliguric, and his creatinine and urea continue to rise. What dose of metoclopramide
will you administer ?
a. Metoclopramide 10 mg q6h
b. Metoclopramide 5 mg q6h
c. Metoclopramide 10 mg q8h
d. Metoclopramide not indicated
Did you find the correct answer in the ENTERAL FEEDING INITIATION ORDERS?
3
On day 2 his levophed and vasopressin are discontinued. His enteral feeds are at 10 ml/hr.
Questions:
3. On morning rounds you inform the medical team that the patient no longer requires
vasopressor support and is receiving trophic feeds. What intervention do you anticipate?
a. Increase trophic rate from 10 to 20 ml/hr
b. Start enteral feeds at 25ml/hr and increase to target of 70ml/hr
c. Start volume feeds at a target goal rate determined by dietitian
d. Start volume feeds at 1100 ml/hr over 24 hours
Starting volume feeds at a rate determined by a dietitian is the best choice. The PEP uP
Protocol is meant for initial nutrition orders and reassessment by the dietitian is always the
next step to make sure each patient’s individual nutrition requirements are met.
If this patient was admitted on a weekend however, he could be moved over the volume
feeding of 1100ml per 24 hrs (based on his weight of 70Kg) until Monday when he is stable.
Make sure to bring this up at morning rounds.
4. At 0800 you measured the gastric residual volume and it is 350mls. You replace the
aspirate and continue feeding at target goal rate. At 1200 his gastric residuals are
measured again and it remains at 350 ml. What will you do?
a. Replace 300 ml of aspirate and decrease rate by 50 ml/hr
b. Replace all the aspirate and maintain current feeding rate
c. Replace 300ml of aspirate and decrease rate by 25ml/hr
d. Do not replace aspirate and hold tube feeds
Use the GASTRIC FEEDING FLOWCHART in the Appendix to find the answer.
The correct answer is c. As the previous residual volume measurement was greater than
300ml, replace 300ml of aspirate, discard the remainder and reduce rate by 25 ml/hr
4
He has remained stable throughout Day 3. On Day 4 of his admission the surgical team informs you at
1000h that they will be taking him back to the OR; they request that he be kept NPO after 2400 hours.
Questions:
5. The dietitian has determined that his daily volume goal is 1200ml in 24 hours (starts at
0700h daily) which is a rate of 50ml/hr. What will be his new rate to reach his goal volume
by midnight?
a. 64 ml/hr
b. 75 ml/hr
c. 82 ml/hr
d. 96 ml/hr
Did you calculate 75 ml/hr?
Since he needs to be NPO at midnight all of his feed volume needs to be infused by midnight, or
in 17 hours total. He has received 150 ml since 0700: 50 ml/hr x 3 hours.
1200 – 150 = 1050 ml remaining. 1050ml/14 hours remaining = 75 ml/hr
6. What is the maximum hourly rate that you should infuse on volume based feeding?
a. 125 ml/hr
b. 135 ml/hr
c. 150 ml/hr
d. 160 ml/hr
Refer to the VOLUME BASED FEEDING SCHEDULE to find the answer to this question.
The maximum rate is 150ml/hr.
7. Your 24- hour intake indicates that he received 1100 ml in the last 24 hours. Based on the
daily goal of 1200 ml in 24 hours, what will you report as his nutritional adequacy during
morning rounds?
a. 92%
b. 94%
5
c. 96%
d. 98%
Part of your daily report in rounds should now include nutritional adequacy. This reports
how much of the feed your patient received in the previous 24 hour period compared to what
he/she should have received. This is reported as a percentage. Calculate nutritional
adequacy by dividing the actual amount given by the target volume and multiplying x 100.
Actual volume/target volume x100 = % of target delivered
In this question the calculation would be 1100/1200 x 100 = 92%
8. He continues to receive 5mg metoclopromide as per the enteral feeding initiation orders.
But his gastric residuals have been > 300 ml for 2 consecutive checks. What intervention do
you anticipate?
a. Consider Erythromycin 200 mg Q12h
b. Increase Metoclopramide to 10 mg q4h
c. Increase rate of feeds
d. Hold feeds for 4 hours
Refer to the GASTRIC FEEDING FLOWCHART in Appendix 3 to find the answer to this question.
The correct answer is a. consider erythromycin.
6
One week following his admission he is scheduled for an MRI at 1400h. The enteral feeds are stopped
from 1400h to 1700h. (N.B. In this example the flow sheet start time is 0700h).
Questions:
9. You know that he is to receive 1200 ml in 24 hours which is a rate of 50ml/hr. Upon
returning to the ICU at 1700h, what will be his new rate based on the 24 hour volume
protocol ?
a. 60 ml/hr
b. 65 ml/hr
c. 70 ml/hr
d. 75 ml/hr
Did you calculate the correct rate of 60 ml/hr?
If not, here is how you would calculate the rate:
50 ml/hr x 7 hours = 350 ml delivered by 1400h.
1200 ml/24 hours – 350 ml = 850 ml remaining
850 ml/14 hours remaining = 60 ml/hr
Now that you have worked through the first set of questions there is a second case study below. To
encourage you to test your new knowledge of the PEP uP protocol, the answers to this study are
found at the end rather than along with each question. See how you do!
7
Case Study # 2
73 year old male is admitted to ICU at 2100 hours with a three day history of shortness of breath and
weakness. He is in respiratory distress with oxygen saturations of 88% on 15 liters with a respiratory
rate of 36/min. He is intubated and placed on FiO2 of 50%, PEEP 15 and PSV of 12. His saturations have
improved and his respiratory rate is 14/min. His past medical history is significant for COPD and alcohol
dependence. He is admitted to ICU with a diagnosis of community acquired pneumonia. He does not
have bowel sounds and is NPO. His weight is 75Kg and height is 1.8m.
N.B. In this example the flow sheet start time is 0700h
Questions:
1. What do you anticipate will be ordered for feeding on admission?
a. NPO because no bowel sounds
b. Volume based feeding because he is not receiving any vasopressors
c. Start trophic feeds at 10 ml/hr
d. Start metoclopramide and wait for bowel sounds
2. Does he require protein supplements?
a. Yes. He requires protein supplements because we want to avoid a nutrition deficit.
b. No. Protein supplements are not required because he is a new admission.
The resident orders volume based feeds for him because he is adequately volume resuscitated and is not
receiving vasopressors. It is now 2200h and you need to calculate his volume based feeding for the
remainder of the 24 hours, his weight is 75 kilograms. (Remember, the 24 hours begin and end at 0700h
daily.)
Questions:
3. Based on his weight, what should his adjusted target volume for the first day of feeding be?
a. 413ml
b. 1100 ml
c. 321 ml
d. 92 ml
8
4. Based on the amount of time that remains in the 24 hour period, what will your hourly rate
be?
a. 46 ml/hr
b. 64 ml/hr
c. 50 ml/hr
d. 45 ml/hr
5. At 0700 hours you will recalculate the hourly enteral feeding rate for the next 24 hours, or
until he is reassessed at rounds. What will this rate be?
a. 46 ml/hr
b. 62ml/hr
c. 67 ml/hr
d. 70 ml/hr
Admission day 2: He continues to receive volume based feeds per PEP uP protocol. He has developed
diarrhea and is having 6-7 loose stools per day.
Question:
6. Which of the following would be an appropriate action?
a. Stopping the tube feeds
b. Stopping the metoclopramide
c. Implement the diarrhea management guidelines
d. Increasing the tube feeding rate
The dietitian reassesses the patient and recommends that he receives 1500 ml over 24 hours. The feeds
were stopped while going for a test and were not started upon return to the unit. At 1700 hours the feeds
have been off for 4 hours.
Question:
7. What rate will you run the feeds for the remainder of the time?
a. 62 ml/hr
b. 75 ml/hr
9
c. 80 ml/hr
d. 115 ml/hr
Congratulations, you have completed the Learning Module!
Thank you for helping us implement the PEP uP Protocol.
If you still have questions about how to implement the PEP uP Protocol please ask the Protocol
Implementation Team (PIT) Crew: {add contact details}
10
Answers:
Case study 2
1. What do you anticipate will be ordered for feeding on admission?
Answer: Volume based feeding because he is hemodynamically stable
2. Does he require protein supplements?
Answer: Yes. He requires protein supplements because we want to avoid a protein deficit.
3. Based on his weight of 75Kg, what should his 24 hour volume based feeding would be?
Answer: (1100 ml target volume x 9 hours left in Day 1) 24 = 413 ml target volume for
day 1
4. Based on the amount of time that remains in the 24 hour period, what will your hourly rate be?
Answer: 413ml target volume for Day 1 9 hrs remaining in Day 1 = 46 ml/hr
5. What will the new rate be?
Answer: 1100 ml 24 hr target volume 24 hrs = 46 ml/hr
6. Which of the following would be an appropriate action?
Answer: Implement the diarrhea management protocol
7. At 1700 hours the feeds have been off for 4 hours. What rate will you run the feeds for the
remainder of the time?
Answer: 80 ml/hr
1500ml/24 hr = 63 ml/hr. 63 x 6 hr = 378 ml infused.
1500 – 378 = 1122 ml remaining to be infused. 1122 ml/14 hr = 80 ml/hr
11
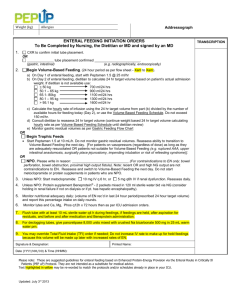
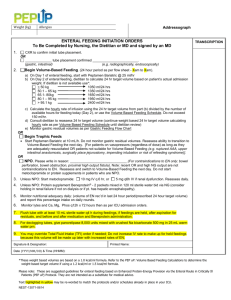
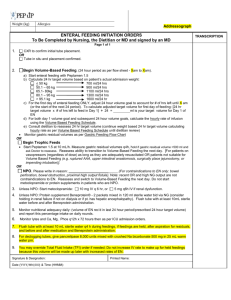
Appendix 1
Weight (kg)
Allergies
Addressograph
ENTERAL FEEDING INITIATION ORDERS
To Be Completed by Nursing, the Dietitian or MD and signed by an MD
Page 1 of 1
Use this order in all patients meeting the following criteria:
Include if:
- Adult patients (≥18 years)
- Mechanically ventilated at or within 6 hours of ICU
admission in whom you would normally initiate
enteral nutrition
1.
OR
Exclude if:
- Enteral or parenteral nutrition initiated before ICU
admission
- Patients on mask ventilation
CXR to confirm initial tube placement.
______________ tube placement confirmed ________________________.
(gastric, intestinal)
(e.g. radiographically, endoscopically)
2.
Begin Volume-Based Feeding. (24 hour period as per flow sheet - Xam to Xam).
a) Start enteral feeding with Peptamen 1.5
b) Calculate 24 hr target volume based on patient’s actual admission weight:
< 50 kg
700 ml/24 hrs
50.1 – 65 kg
900 ml/24 hrs
65.1- 80kg
1100 ml/24 hrs
80.1 – 95 kg
1300 ml/24 hrs
> 95.1 kg
1600 ml/24 hr
c) For the first day of enteral feeding ONLY, adjust 24 hour volume goal to account for # of hrs left until X am (or
the start of the next 24 period). To calculate adjusted target volume for first day of feeding: [24 hr target
volume x # of hrs left to feed in Day 1] ÷ 24 =
ml is your target volume for Day 1 of EN
d) For both day 1 volume goal and subsequent 24 hour volume goals, calcluate the hourly rate of infusion using
the Volume Based Feeding Schedule.
e) Consult dietitian to reassess 24 hr target volume (continue weight based 24 hr target volume calculating hourly
rate as per Volume Based Feeding Schedule until dietitian review)
Monitor gastric residual volumes as per Gastric Feeding Flow Chart
OR
Begin Trophic Feeds
Start Peptamen 1.5 at 10 mL/h. Do not monitor gastric residual volumes. Reassess ability to transition to VolumeBased Feeding the next day. [For patients on vasopressors (regardless of dose) as long as they are adequately
resuscitated OR patients not suitable for Volume Based Feeding (e.g. ruptured AAA, upper intestinal anastomosis,
surgically place jejunostomy, or impending intubation)].
OR
NPO. Please write in reason: _________________ ______.(For contraindications to EN only: bowel perforation, bowel
obstruction, proximal high output fistula). Note: recent OR and high NG output are not contraindications to EN.
Reassess and switch to Volume-Based Feeding the next day. Do not start metoclopramide or protein supplements in
patients who are NPO.
3.
Unless NPO: Start metoclopramide:
4.
Unless NPO: Protein supplement Beneprotein® - 2 packets mixed in 120 ml sterile water bid via NG (consider holding
in renal failure if not on dialysis or if pt. has hepatic encephalopathy).
5.
Monitor nutritional adequacy daily: (volume of EN rec’d in last 24 hour period/prescribed 24 hour target volume) and
report this percentage intake on daily rounds.
6.
Monitor lytes and Ca, Mg, Phos q12h x 72 hours then as per ICU admission orders.
10 mg IV q 6 hr, or
5 mg q6h IV if renal dysfunction. Reassess daily.
12
TRANSCRIPTION
7.
Flush tube with at least 10 mL sterile water q4 h during feedings, if feedings are held, after aspiration for residuals,
and before and after medication and Beneprotein administration.
8.
For declogging tubes, give pancrelipase 8,000 units mixed with crushed Na bicarbonate 500 mg in 25 mL warm water
prn.
9.
You may override Total Fluid Intake (TFI) order if needed; Do not increase IV rate to make up for held feedings
because this volume will be made up later with increased rates of EN.
Signature & Designation:
Printed Name:
Date (YYYY/MM/DD) & Time (HHMM):
* The examples included in the learning module refer to a ICU flow sheet starting at 700h*
13
Appendix 2
Volume Based Feeding Schedule
Hours remaining in the day to feed 24h volume
Goal total
mL formula
per 24h
2400
2350
2300
2250
2200
2150
2100
2050
2000
1950
1900
1850
1800
1750
1700
1650
1600
1550
1500
1450
1400
1350
1300
1250
1200
1150
1100
1050
1000
950
900
850
800
24
23
22
21
20
19
18
17
16
15
14
13
12
11
10
9
8
7
6
5
4
3
2
1
100
104
109
114
120
126
133
141
150
150
150
150
150
150
150
150
150
150
150
150
150
150
150
150
98
102
107
112
118
124
131
138
147
150
150
150
150
150
150
150
150
150
150
150
150
150
150
150
96
100
105
110
115
121
128
135
144
150
150
150
150
150
150
150
150
150
150
150
150
150
150
150
94
98
102
107
113
118
125
132
141
150
150
150
150
150
150
150
150
150
150
150
150
150
150
150
92
96
100
105
110
116
122
129
138
147
150
150
150
150
150
150
150
150
150
150
150
150
150
150
90
93
98
102
108
113
119
126
134
143
150
150
150
150
150
150
150
150
150
150
150
150
150
150
88
91
95
100
105
111
117
124
131
140
150
150
150
150
150
150
150
150
150
150
150
150
150
150
85
89
93
98
103
108
114
121
128
137
146
150
150
150
150
150
150
150
150
150
150
150
150
150
83
87
91
95
100
105
111
118
125
133
143
150
150
150
150
150
150
150
150
150
150
150
150
150
81
85
89
93
98
103
108
115
122
130
139
150
150
150
150
150
150
150
150
150
150
150
150
150
79
83
86
90
95
100
106
112
119
127
136
146
150
150
150
150
150
150
150
150
150
150
150
150
77
80
84
88
93
97
103
109
116
123
132
142
150
150
150
150
150
150
150
150
150
150
150
150
75
78
82
86
90
95
100
106
113
120
129
138
150
150
150
150
150
150
150
150
150
150
150
150
73
76
80
83
88
92
97
103
109
117
125
135
146
150
150
150
150
150
150
150
150
150
150
150
71
74
77
81
85
89
94
100
106
113
121
131
142
150
150
150
150
150
150
150
150
150
150
150
69
72
75
79
83
87
92
97
103
110
118
127
138
150
150
150
150
150
150
150
150
150
150
150
67
70
73
76
80
84
89
94
100
107
114
123
133
145
150
150
150
150
150
150
150
150
150
150
65
67
70
74
78
82
86
91
97
103
111
119
129
141
150
150
150
150
150
150
150
150
150
150
63
65
68
71
75
79
83
88
94
100
107
115
125
136
150
150
150
150
150
150
150
150
150
150
60
63
66
69
73
76
81
85
91
97
104
112
121
132
145
150
150
150
150
150
150
150
150
150
58
61
64
67
70
74
78
82
88
93
100
108
117
127
140
150
150
150
150
150
150
150
150
150
56
54
59
57
61
59
64
62
68
65
71
68
75
72
79
76
84
81
90
87
96
93
104
100
113
108
123
118
135
130
150
144
150
150
150
150
150
150
150
150
150
150
150
150
150
150
150
150
52
54
57
60
63
66
69
74
78
83
89
96
104
114
125
139
150
150
150
150
150
150
150
150
50
52
55
57
60
63
67
71
75
80
86
92
100
109
120
133
150
150
150
150
150
150
150
150
48
50
52
55
58
61
64
68
72
77
82
88
96
105
115
128
144
150
150
150
150
150
150
150
46
48
50
52
55
58
61
65
69
73
79
85
92
100
110
122
138
150
150
150
150
150
150
150
44
46
48
50
53
55
58
62
66
70
75
81
88
95
105
117
131
150
150
150
150
150
150
150
42
43
45
48
50
53
56
59
63
67
71
77
83
91
100
111
125
143
150
150
150
150
150
150
40
41
43
45
48
50
53
56
59
63
68
73
79
86
95
106
119
136
150
150
150
150
150
150
38
39
41
43
45
47
50
53
56
60
64
69
75
82
90
100
113
129
150
150
150
150
150
150
35
37
39
40
43
45
47
50
53
57
61
65
71
77
85
94
106
121
142
150
150
150
150
150
33
35
36
38
40
42
44
47
50
53
57
62
67
73
80
89
100
114
133
150
150
150
150
150
14
Hours remaining in the day to feed 24h volume
Goal total
mL formula
per 24h
750
700
650
600
550
500
24
23
22
21
20
19
18
17
16
15
14
13
12
11
10
9
8
7
6
5
4
3
2
1
31
33
34
36
38
39
42
44
47
50
54
58
63
68
75
83
94
107
125
150
150
150
150
150
29
30
32
33
35
37
39
41
44
47
50
54
58
64
70
78
88
100
117
140
150
150
150
150
27
28
30
31
33
34
36
38
41
43
46
50
54
59
65
72
81
93
108
130
150
150
150
150
25
26
27
29
30
32
33
35
38
40
43
46
50
55
60
67
75
86
100
120
150
150
150
150
23
24
25
26
28
29
31
32
34
37
39
42
46
50
55
61
69
79
92
110
138
150
150
150
21
22
23
24
25
26
28
29
31
33
36
38
42
45
50
56
63
71
83
100
125
150
150
150
Nursing Instructions for Physician Ordered 24 hour Volume-Based Enteral Feeding
Example:
Order for volume based enteral feeding will be the total volume goal for 24 hours. The 24 hour period corresponds to the flow sheet
(i.e X am to X am each day).
If the total volume ordered is 1800 mL, the hourly rate is 75 mL/hour. If the patient was fed 450 mL of feeding (6 hours) and the
tube feeding is on “hold” for 5 hours, then subtract from the goal volume the amount of feeding the patient has already received.
Volume Ordered per 24 hours 1800 mL – Tube feeding in (current day) 450 = Volume of feeding remaining in day to feed
1800
–
450
= 1350 mL
Patient now has 13 hours left in the day to receive 1350 mL of tube feeding.
Check the chart for the new goal rate based on the number of hours remaining in the current 24 hr period. Select the goal rate closest
to volume needed.
In this example it would be 1350. Next go to column 13 (the number of hours remaining to feed) and the amount of feeding to provide
will be 104 mL/hour. In this example the patient will receive a total volume of 1352 mL for the remaining hours in the day.
Please contact your ICU dietitian or PIT Crew if you have any questions
Important Nursing Assessment
Volume based feeding should be used with caution. Nurses should always assess for feeding intolerance. Examples of intolerance include:
abdominal distention, abdominal cramping, nausea & vomiting, diarrhea defined as 5 stools or 750 mL per 24h period, and gastric residuals
greater than 300 mL.
15
Appendix 3
Gastric Feeding Flow Sheet
Place feeding tube or use existing
gastric drainage tube.
X-ray to confirm placement (as required)
Elevate head of bed to 45° (or as much
as possible) unless contraindicated.
Start feed at initial rate or volume
ordered.
Measure gastric residual volumes q4h.
Is the residual volume > 300 ml?
NOTE: Do not aspirate small bowel tubes.
Replace up to
300mL of aspirate,
discard remainder.
Set rate of EN
based on
remaining volume
and time until X
am (max rate
150mL/hr).
Reassess motility
agents after feeds
tolerated at target
rate for 24 hours.
No
Yes
Replace 300 mL of aspirate, discard
remainder. Reduce rate by 25 mL/h to
no less than 10 mL/h.
Step 1: Start metoclopramide 10mg IV
q 6 hr. If already prescribed, go to
Step 2.
Step 2: Consider adding erythromycin
200 mg IV q12h (may prolong Qt
interval). If 4 doses of erythromycin
are ineffective, go to Step 3.
Step 3: Consider small bowel feeding
tube placement and discontinue
motility agents thereafter.
Yes
Was the residual
volume greater than
300 mL the last time it
was measured?
No
16