Implementation - Powerpoint - Short Version
advertisement

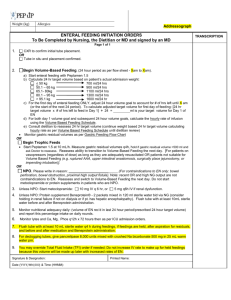
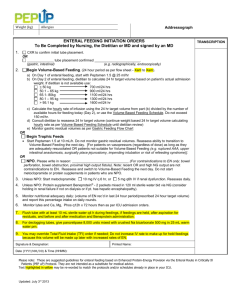
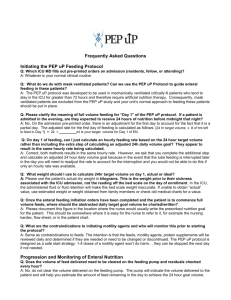
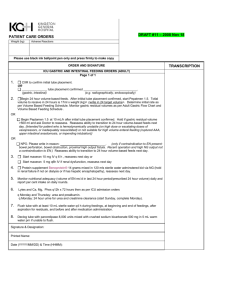
The PEP uP Protocol I’M HUNGRY!! Adequate Nutrition Provides fuel for cellular metabolism Prevents protein/muscle wasting Decreases ventilator time Helps prevent infection/VAP Decreases ICU length of stay Promotes healthy wound healing Reduces mortality GUT disuse causes loss of functional and structural integrity of the GI tract and is associated with increased complications These changes are time dependent; the longer they are left NPO, the greater the complications. Main Features the PEP uP Protocol All patients will receive Peptamen 1.5 initially All patients will start on Beneprotein® • 2 packets (14 g) mixed in 120ml water administered bid via NG All patients will be given metaclopromide on Day 1 of enteral feeding • 10 mg IV q 6h ……. Reassess formula, protein supplement, and motility agent daily Get PEPPED UP! Option 1: Begin Volume-Based feeds. The 24 hour period begins at XXXXh daily. Patient is to receive Peptamen 1.5 initially. The total target volume for Day 1 of EN is based on the patient’s weight in kilograms. Consult dietitian to reassess 24 hr target volume as soon as possible Determine hourly rate as per Volume Based Feeding Schedule. Monitor gastric residual volumes as per Gastric Feeding Flowchart and Volume Based Feeding Schedule . Get PEPPED UP! Option 2: Trophic feeds Begin Peptamen 1.5 at 10 mL/h after initial tube placement confirmed. Do not monitor gastric residual volumes. Reassess ability to transition to Volume-Based feeds next day. Intended for patient who is: On vasopressors (regardless of dose) as long as they are adequately resuscitated Not suitable for high volume enteral feeding (ruptured AAA, surgically place jejunostomy, upper intestinal anastomosis, or impending intubation) Get PEPPED UP! Option 3: NPO NPO Only if contraindication to EN present: bowel perforation, bowel obstruction, proximal high output fistula. Recent operation and high NG output are not a contraindication to EN. Reassess ability to transition to VolumeBased feeds next day. Gastric feeding flowchart Place feeding tube or use existing gastric drainage tube. X-ray to confirm placement (as required) Elevate head of bed to 45° (or as much as possible) unless contraindicated. Start feed at initial rate or volume ordered. Measure gastric residual volumes q4h. Is the residual volume > 300 ml? NOTE: Do not aspirate small bowel tubes. Replace up to 300mL of aspirate, discard remainder. Set rate of EN based on remaining volume and time until X am (max rate 150mL/hr). Reassess motility agents after feeds tolerated at target rate for 24 hours. No Yes Replace 300 mL of aspirate, discard remainder. Reduce rate by 25 mL/h to no less than 10 mL/h. Step 1: Start metoclopramide 10mg IV q 6 hr. If already prescribed, go to Step 2. Step 2: Consider adding erythromycin 200 mg IV q12h (may prolong Qt interval). If 4 doses of erythromycin are ineffective, go to Step 3. Step 3: Consider small bowel feeding tube placement and discontinue motility agents thereafter. Yes No Was the residual volume greater than 300 mL the last time it was measured? Case Study 73 year old male is admitted to ICU at 2100 hours with a three day history of shortness of breath and weakness. He is in respiratory distress with oxygen saturations of 88% on 15 liters with a respiratory rate of 36/min. He is intubated and placed on FiO2 of 50%, PEEP 15 and PSV of 12. His saturations have improved and his respiratory rate is 14/min. Case Study His past medical history is significant for COPD and alcohol dependence. He is admitted to ICU with a diagnosis of community acquired pneumonia. He does not have bowel sounds and is NPO. His weight is 75Kg and height is 1.8m. Case Study Admission What do you anticipate will be ordered for feeding on admission ? a. NPO because no Bowel Sounds b. Volume based feeding because he is not receiving any vasopressors c. Start trophic feeds at rate per PEPuP protocol d. Start metoclopramide and wait for bowel sounds Case Study PEP uP Initial Orders: Protein Supplements Does he require protein supplements? a. Yes. He requires protein supplements because we want to avoid a nutrition deficit. b. No. Protein supplements are not required because he is a new admission. Case Study Admission Orders The resident orders volume based feeds for him because he is adequately volume resuscitated and is not receiving vasopressors. It is now 2200 hours and you need to calculate his volume based feeding for the remainder of the 24 hours. *Remember: The 24 hours begin and end with the flow sheet which in this example is 0700hrs. Case Study Volume Based Feeds: Getting Started Based on his weight, what should his adjusted target volume for the first day of feeding be? a. 413 ml b. 1100 ml c. 321 ml d. 92 ml Case Study Calculating the adjusted rate Based on the amount of time that remains in the 24 hour period, what will your hourly rate be ? a. 46 ml/hr b. 64 ml/hr c. 50 ml/hr d. 45 ml/hr Case Study Setting the 24 hour rate At 0700 hours you will recalculate the hourly enteral feeding rate for the next 24 hours, or until he is reassessed at rounds. What will the new rate be? • 46 ml/hr • 62ml/hr • 67 ml/hr • 70 ml/hr Case Study Admission Day 2 He continues to receive volume based feeds per PEP uP protocol. He has developed diarrhea and is having 4 to 5 loose stools per day. Which of the following would be an appropriate action? • Stop the tube feeds • Stop the metoclopramide • Implement the diarrhea management guidelines • Increasing the tube feeding rate Case Study Admission day 3 He is now receiving 1500 ml in 24 hours volume based feeding after the dietitian reassessed. The feeds were stopped while going for a test and were not started upon return to the unit. At 1700h the feeds have been off for 4 hours. What rate will you run the feeds for the remainder of the time? • 62 ml/hr • 75 ml/hr • 80 ml/hr • 115 ml/hr Questions?