“Promoting healthy lifestyle is an integral part of the management of
advertisement

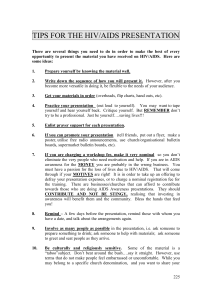
“Promoting healthy lifestyle is an integral part of the management of individuals with long-term conditions.” Discuss. The far-reaching effects of a detrimental long-term medical condition on any given individual are always going to be variable; they are likely to be dependent, mostly, on the individual’s social situation, background, underlying health issues (either related or unrelated to the condition), lifestyle choices, and attitude towards the condition itself. Other variables outside the individual can include attitudes of others towards the long-term condition, available information related to the condition, health policies such as National Service Frameworks, and clinical interventions by healthcare professionals. How far the role of healthcare professionals is pertinent can also be a variable in itself, depending on what they are called upon to do and how they execute their task. Perhaps the first and most crucial thing a healthcare professional needs to consider when tacking an individual with a long-term condition is the condition itself – its nature, severity, risks and related issues are all important, and it is imperative that any discerning professional keeps this in mind while delivering care. When considering a long-term condition like being HIV-positive, it is important to ascertain exactly what the patient is aware of. It is known that infection by the human immunodeficiency virus (HIV) is an acquired one usually transferred through unprotected sexual contact or other means such as shared needles for intravenous drug usage. It is a blood-borne virus, belonging to a group which can pass through shared body fluids ranging from the well-known (such as Hepatitis B and C) to the less commonplace, such as the Ebola virus. Infection by the HIV virus can lead to the acquired immune deficiency syndrome (AIDS), which severely impairs the body’s resistance to pathogens; this is often fatal – as the United Nations programme on HIV and AIDS claims, “In 2005 alone, AIDS claimed an estimated 2.4-3.3 million lives.” While its effects are known, the global prevalence of the virus responsible may not be so acknowledged. Although HIV in humans is considered a pandemic by the WHO, with approximately 0.6% of the world’s population being HIV-positive (United Nations, 2006), that statistic is rarely mentioned. The media is more inclined to report on more ‘current’ pandemics, such as H1N1 (swine flu) in 2009, and in many ways, a social stigma can be attached to the HIV-positive individual, possibly due to the method of its contraction. For someone with HIV, acceptance of their condition is one of the concepts they may have to face, along with its connotations for their future, their lifestyle choices, and the hope to avoid developing full AIDS. Besides its prevalence, there is a good argument, on an individual level, that being HIV-positive is a serious long-term condition. Developing AIDS will almost certainly lead to death, and Buchbinder et al. (1994) state that without [antiretroviral] treatment, approximately nine out of every ten persons with the HIV virus will progress to AIDS after ten to fifteen years, with many progressing much sooner. Even if the individual in question does not progress, they will remain HIV-positive for the rest of their life, as the virus is constant in the bloodstream. Furthermore, a person with HIV will have to both monitor their white blood cell count and, if they elect to, take antiretroviral treatment (highly active antiretroviral therapy, also known as the “AIDS cocktail” [Murphy et al., University of California, 2001]). The treatment suppresses the replication of HIV particles in the blood stream, allowing a patient's immune system to recover (Murphy et al., 2001). While this can be purported to help reduce the morbidity and mortality of an HIV infection (Palella et al., 1998), it may also serve as a reminder to the individual of the serious nature of their condition, especially as it is a lifelong, routine process to take. Palella et al. also state that, when considered on a global scale, the treatment “is not available in all countries”, especially those nations in Africa and the developing world in which HIV is particularly prevalent. Key trends for HIV in the UK on a national level can be found via the Terrence Higgins Trust, set up specifically for dealing with HIV and other sexually transmitted diseases. The THT’s website states that the two groups most affected in the UK are men who have homosexual intercourse and migrants from regions of the world where HIV is common, such as sub-Saharan Africa (tht.org.uk). It also states that HIV is on the rise: around 97,400 cases of HIV have been reported since the early 1980s - 7,734 in 2007 alone (tht.org.uk). This rising trend is more apparent in some areas than others – dividing the UK into regions, London holds the most cases, with 48% of those diagnosed being in the London area. Other regions have their own trends, but all of these indicate a rise in HIV, those diagnosed living across all areas of the UK and “particularly in major towns and in North West England”, whereas some regions with a previous scarcity of HIV have suffered a sharp increase - in the last ten years, the biggest increases in people living with diagnosed HIV have been in the East of England, the East Midlands and South Central coast (tht.org.uk). Insofar as local levels are concerned, the THT also prepare ‘bulletins’ on these trends – the most recent (as of October 2009), presented in July 2009, states that in inner London, 3,098 new cases were diagnosed in 2008 alone, and although numbers of diagnoses have decreased by 2%, there is still an upward trend in the central London area due to an estimated 28% of undiagnosed HIV carriers. The Department of Health offers a policy for dealing with HIV as part of its “sexual health and HIV strategy” of 2001, the abstract of which “aims to modernise sexual health and HIV services” (DoH, 2001). The impact of HIV on the UK population is mentioned in section one of the strategy; it mentions ways of tackling HIV, stating that there is no cure, and any “highly effective vaccine” will probably not be available “for at least five years” (DoH, 2001). It also mentions the WHO’s epidemic status and states that in the UK alone, an estimated 30,000 people are living with HIV, of whom a third are undiagnosed, although this paper was prepared in 2001, and its statistics out of date. The national statistics website, statistics.gov.uk, places the number at 63,500, indicating a rise of 33,500 – more than doubling the 2001 amount – within eight years. Although an interesting paper, because this is based around sexual health, the Strategy makes no mention of other risks which can lead to the contraction of transferable pathogens such as HIV. In contrast, the introduction to the Department of Health’s “Reducing DrugRelated Harm” action plan, produced in association with the NHS National Treatment Agency for Substance Misuse, mentions “recent data” (as of 2007) showing that blood-borne virus infections among drug users having been on the rise in recent times (DoH, 2007). The action plan states on page one that injecting drug users have a high risk of contracting blood-borne virus infections (DoH, 2007). It also quotes the Health Protection Agency (HPA)’s estimate for 2006 that “almost half of current injecting drug users” have contracted a Hepatitis C infection (HPA, 2006). The harmful effects of illicit drug use notwithstanding – injecting, especially if IV drug users share needles and other equipment, increases one’s chances of acquiring an HIV infection. The case for arguing that sharing of injecting equipment leads to sharing of infections is strong; an Australian leaflet aimed at IV drug users points out that “any sharing of injecting equipment, even tourniquets, is highly discouraged, due to the high danger of transmitting bacteria and viruses via the equipment” (Australian Intravenous League & National Hepatitis C Education and Prevention Program, Safer Injecting, 2000). Mathers et al. claimed in 2008 that an estimated sixteen million people worldwide use intravenous drugs, and that three million of these are believed to be HIV positive. 2.4% of all the UK HIV diagnoses in 2007 accounted for contraction through IV drug usage (Terrence Higgins Trust, tht.org.uk). Heroin – a ‘designer’ drug – is cited by the UK’s youth drugs programme FRANK as a drug well-known for being injected intravenously: “The risks of sharing needles and other works to inject are well-known, putting you in danger of infections like … HIV/AIDS” (FRANK website, accessed 2009). Heroin usage in the United Kingdom appears to be variable over the years, and some references have referred to its decline when compared to cocaine usage – cocaine can also be prepared to make a solution for IV injection, although is it often thought of as being a drug for smoking. Nevertheless, heroin and other IV drugs are still prevalent – as recently as October 2009, an article by journalist Adrian Radnedge in the daily newspaper Metro claims that more Britons than ever are being treated for drug abuse, claiming the rise is “being fuelled by a so-called ‘Trainspotting generation’ of over-35s who are addicted to heroin.” The article also cites figures from the NHS National Treatment Agency for Substance Misuse: it claims 207,580 adults are seeking treatment for complications related to drug abuse. “One in five under-25s seeking treatment has problems with cocaine,” claims Radnedge. “That is up from one in ten four years ago.” His article includes contrasting views: NTA chief executive Paul Hayes said young people are “very savvy”, and that using heroin is “no longer seen as having any glamour attached to it at all” (quoted in Radnedge/Metro, 2009), while Drugscope chief executive Martin Barnes rejected any suggestion heroin use was in terminal decline as ‘premature’. Harry Shapiro of Drugscope, quoted in an Observer article, places the number of problem drug users in the UK as 300,000. The injection of intravenous drugs may, at first, seem like it would not cause much harm to an individual who already has HIV. As it is a lifetime infection with a high mortality rate, there is no possibility of becoming re-infected with the virus. However, with a decreased immune system, the dangers of co-infection with other diseases are amplified. The aforementioned hepatitis, an infection that is known for possible transmission via intravenous drug usage, “has become a major source of mortality among HIV-infected persons” (Reese et al., 2009). According to the study by Reese et al., individuals who are HIV positive should be screened for HCV [Hepatitis C] routinely on account of the fact that the course of liver disease can be more rapid in individuals who are co-infected with HIV and HCV. The risk of liver cirrhosis is nearly twice that in persons who have a hepatitis “mono-infection”. Wagner et al. (2009) conducted twenty-two interviews with “primary care providers and support staff” at three HIV clinics in Los Angeles, California, in which rates of HCV treatment uptake were variable (from 10% to 38%). The general agreement was that “stable HIV disease, favourable genotype, and significant signs of liver disease progression” are all signs of need for immediate treatment. The associated article reiterates the fact that liver disease “is a leading cause of death among patients with HIV co-infected with hepatitis C” (Wagner et al., 2009), yet it also claims that studies show that less than 10% receive treatment for HCV. There is also a large psychosocial aspect to consider, especially if the individual in question indulges in drug injection as a communal activity, or other aspects of their lifestyle choice or even day-to-day routine could present a risk. Rapid transmission of the virus has occurred globally among sex workers, despite increasing knowledge of its prevalence (Hilton et al., 2001). A literature review of strategies for control of HIV claims that there is a danger of a greatly increased transmission “to anyone associated with [HIV-positive individuals who inject drugs]”, such as sexual partners who do not have the infection or also take intravenous drugs, children of intravenous drug users, and eventually “the population at large”. The psychological effects which may occur to someone as a result of their realisation that they have infected others – especially friends and/or family members – could be devastating. Additionally, with regards to the law on giving somebody HIV, whether accidentally or deliberately, UK residents can risk prosecution for ‘recklessly inflicting grievous bodily harm’ due to transmission of HIV under section 20 of the Offences Against the Person Act 1861 (information via Terrence Higgins Trust website, tht.org.uk), with a maximum prison sentence of five years. Tones and Telford (1994) claim that “health promotion and health education [are] concerned with promoting change”, which can be taken to refer to a positive change in lifestyle for the affected individuals. Indeed, the role played by a nurse can be pivotal in promoting a lifestyle change to prevent continuing IV drug usage and the associated spread of HIV, although with IV drug usage, the access to resources and information available to the individual themselves could be considered necessary to effect the change. As with the AIDS cocktail for protection against progression to the syndrome, there are treatments and support for IV drug users; however, as Fornataro and Obermeyer (1992) state, HIV-positive IV drug users – specifically “those with little or no scientific training” – may have difficulty understanding existing treatments. They are also unlikely to read educational materials on the subject, although the study concluded that many individuals requested relevant information [on clinical research studies relating to early intervention] specifically from the person from whom they had first received information ‘fact sheets’ (Formataro & Obermeyer, 1992), suggesting that in numerous cases, a nurse – or other healthcare professional – who delivers pertinent information may be viewed as a helpful port of call for the individual in question. It is also important to remember that a nurse whose role is the promotion of a healthier lifestyle should not place all their emphasis on the patient’s HIV-positive status. Specialist HIV nurses would almost certainly be on hand to deal with the needs of the diagnosed individual, ergo: while it is still an issue, other factors – in this case, the persistent IV drug usage, can be brought to the fore by ‘other’ nurses. The nurse who is implementing interventions is potentially dealing with a very sensitive issue for their patient, so it would be important to first gain an understanding of the situation at hand. The individual may have gained an HIV infection through IV drug usage, although it could have also been contracted by unprotected sex. (It may even be a deliberate infection – evidence suggests that ‘bugchasing’ – an activity within the LGBT community subculture of homosexual men who actively pursue sex with HIV infected individuals in order to contract HIV – is on the rise [Grov & Parsons, 2006].) It is important not to rule out any possibility – nor is it important to rule out any reason for the IV drug addiction. If an individual has contracted HIV through sexual activity, then they may have turned to illicit drug use to provide a psychological tranquiliser as a way of coping with the stress. It is also entirely possible that, if uneducated, the individual may believe that they are at no further risk, since they are already HIV-positive. A nurse’s role in the first instance should therefore be the transfer of relevant information before promoting a new, healthier lifestyle. A useful model for a nurse to consider is presented by Downey et al. (1996) as the “Tannahill” model (the name is derived from two of Downie’s co-authors, both named Tannahill), which visually comprises three concentric circles representing health education, health protection and prevention, each overlapping with the other two, suggesting that once one ‘circle’ has been tackled, the nurse can bring others into play while still considering the former. The first circle, health education, links nicely to the aforementioned information transfer. A useful intervention, albeit not a strictly nursing-related one, could be a reminder that injecting intravenous drugs is an illegal act. Patient confidentiality should be maintained, however, a nurse could briefly “educate” their patient as to the law on illicit drug usage. Under the Misuse of Drugs Act 1971, any injectable form of a Class B or C drug comes under Class A due to the associated risk, while heroin and cocaine are Class A regardless (Misuse of Drugs Act, 1971, via Lambeth PCT literature). While it may seem unlikely that reiteration of this fact may change the patient’s attitude towards IV drug usage (Tones and Tilford [1994] claim that while a lesson on drugs may improve knowledge, it does not take into account factors which influence drug misuse, such as poor self-esteem), a reminder of their Class A status may prove to be a useful aide memoire as to their potentially dangerous effects. Health education overlaps with prevention, another circle in the Tannahill model, which suggests promotion of healthy living – with supporting information – in order to prevent further risks to the individual’s health. Caplan (1961) defined three ‘levels of prevention’, the primary stage of which being action taken to prevent the onset of disease; namely: said promotion of healthy living. For the theoretical patient with an established diagnosis of HIV, the secondary stage is concerned with halting the progress of disease at an early stage (antiretroviral treatment and cessation of IV drug usage fall under this category), while the tertiary stage involves the rehabilitating individuals with an established disease. Caplan states that, even if the disease process cannot be halted, improving the quality of life is important. For an individual with a terminal condition such as AIDS, this can be a fundamental concept. Once again, we are returned to the promotion of a healthy lifestyle. For an IV drug user, a nurse can promote the lifestyle change in one of two main ways: they can promote and work towards a complete cessation of the IV drug usage, or they can suggest ways in which the individual may continue to use IV drugs in a way that presents less of a risk (although they should be careful to make sure they do not appear to be promoting further drug usage), and the two also intersect at various points. With regards to the latter strategy, Hilton et al. (2001) state quite well that the “main challenge” should be to get intravenous drug users to protect themselves [and, in this case, others] while “suffering privations both physical and social” and feeding their own dependencies. Methods to achieve this goal can be implemented in a number of ways. If the nurse is going to take it upon themselves to begin by making sure the IV drug usage carries as little risk of cross-infection as possible, they need to start by advising the individual about cleanliness of the equipment they use, á la the above Safer Injecting leaflet which advises against sharing of equipment. Used sharp needles are a large risk of cross-infection, especially if they are not withdrawn properly from the vein following injection of the substance before re-use. Cleaner, unused needles may therefore be provided to the IV drug user. Although ‘needle exchange’ programmes are in place, some UK trusts do not have a policy detailing their stance on needle exchange, which may make it ethically difficult for the nurse to make a decision on actually providing clean needles – however, there is much evidence to suggest that needle exchange is effective; Hilton et al. (2001) state that such programmes have reduced HIV transmission by 70% in New York City, and in Australia (where the first-ever needle ‘heroin injecting room’ was implemented), data collected by needle exchange clinics found that a reduction in the amount of needles given out coincided with a shortage of heroin in 2001, as well as the number of reported IV drug users and incidences of Hepatitis C, suggesting the services are used ( Day et al., 2004). For UK nurses, there is a National Needle Exchange Forum online (nnef.org.uk) with many useful links – one of which leads to a set of guidelines on needle exchange prepared by “Turning Point”, Somerset’s needle exchange programme. According to Turning Point, the purpose of needle exchange is “to reduce drug-related deaths by controlling the spread of blood-borne viruses and other potential infections through the provision of sterile injecting equipment to intravenous drug users,” which is an accurate interpretation of its purpose, and very pertinent to inhibiting the spread of HIV to others, or hepatitis C to the individual. Needle exchange is most prominent on a local level, largely due to the need for a localised location to be available to IV drug users. Each London Borough provides small facilities for needle exchange (for those unable or unwilling to do so by visiting participating surgeries or hospitals) via small pharmacies. The London Borough of Enfield provides small leaflets with not only safer injecting tips (“if possible, do not inject / if you have to inject, please observe the following…”) but the location of eight different pharmacies within the borough, in addition to the Borough’s main drug service centre itself, with a needle exchange scheme in place. These leaflets could be very useful for a nurse with a patient in a specific local area. Assuming that the patient wishes to continue IV drug usage, the nurse should also advice safer methods of disposal on account of the fact that there is a risk of any equipment, once used, being a potential carrier or the HIV virus. The Enfield leaflet has a section on safer disposal, claiming that the IV drug user should not attempt to clean works or place used works in rubbish bins; rather, they should return used works to the local exchange and/or place them in a sharps bin (also something supplied by the LBE). It also offers a handy alternative to a sharps bin – use an old drinks can (as the metal is more protective than a bin liner). However, supporters of programs promoting total abstinence from drugs as a healthy lifestyle change stress that effectively enabling further drug use – even by making it safer – would lead to prolonged drug use, rather than cessation, leading to a risk of further addiction and complications relating to addiction (Bejerot, 1988), not to mention the harmful effects of the drugs themselves. The third circle of the Tannahill model is, after all, health protection. Critics may argue that not aiming for a complete cessation of the IV drugs would be counterproductive to protecting any individual’s health, HIV-positive or not. Becker (1974) claimed that the presence of “a cue or a trigger” was a major contributing factor towards whether an individual will make a change. A nurse’s presence may be enough of a trigger to effect such a change; however, for the longterm IV drug user, such a major action as attempted complete cessation would probably not come from their mere presence and advice. The nurse may wish to consider, therefore, Becker’s health belief model. This consists of interconnected boxes forming a flow diagram, starting with the individual’s perceptions of their condition and ending with the likelihood of ‘taking action’. The middle of the diagram consists of modifying factors – demographic, psychosocial and structural variables – which may affect this likelihood. Initial individual perceptions are important. Pender (1996), building upon Becker’s ideas, purports the idea that feelings of vulnerability the individual may have can combine with the seriousness of their condition, combining to effectively produce a threat to the condition. Modifying factors may appear to help or hinder the desired action, or the individual may jump directly to the ‘likelihood of action’ stage, in which Pender balances perceived benefits or barriers, the potential benefit in this case being the improved health following IV drug cessation. An effective intervention that a nurse can take, therefore, may be to introduce some modifying factors, indirectly affecting the decision-making process. Fornataro and Obermeyer (1992) state that IV drug users generally feel more comfortable discussing treatment options with their peers, so again, a nurse as a source of information on such treatments may be a good starting point, especially if the subject is brought up in discussion with other drug users – hypothetically being a route for cessation in more than one person. Fornataro and Obermeyer’s study showed that fact sheets – similar to the ones discussed above – were also effectively distributed by the IV drug users themselves. This sort of peer communication (positive peer pressure) may aid treatment as well as being a way for the HIV-positive individual to overcome the social stigma they may be concerned about and reconnect with their contemporaries. Demographic variables are unalterable – the nurse cannot change gender, ethnicity, social background or age (although for long-term treatment that varies over time) – although considering such factors may help (in 2009, the youngest age groups [16-19 and 20-24 year olds] reported the highest levels of drug use [22.2% and 22.9% respectively], according to the NHS Information Centre); however, various critics have stated that methods of therapy can help any group if the patient is willing – person-centred therapy (Ward et al., 2000) is “effective and popular”, and cognitive behavioural therapy (Butler et al., 2006) can treat “a variety of problems” including substance abuse. It is up to the nurse to judge what to implement, so a knowledge of their patient is helpful. They could also point out “cues to action” (referenced by Becker) such as mass media campaigns. Although drug usage has been a taboo subject in the British media, more anti-drug campaigns, such as drug driving posters,1 have started to be used more publicly, and hopefully the observant patient may pick up on these without much prompting. In conclusion, although being HIV-positive is a long-term condition with no chance of recovery and will, in many cases, progress to AIDS and become the individual’s cause of death, the intravenous drug-using individual can either take the measures outlined above to either terminate the drugs’ usage entirely or use preventative methods against acquisition of co-infections such as Hepatitis C, which 1 For reference: http://www.psfk.com/wp-content/uploads/2009/08/craig_ward_cocaine-525x742.jpg would increase their mortality risk, and transference of the HIV virus to other IV drug-users, which would have a psychosocial impact and possibly lead to stigmatisation and/or survivor guilt. Weber et al. (1990) conclude from a study that cessation of IV drug usage lowers both the spread and progression of HIV and associated diseases, providing a strong argument for drug treatment programmes, summarising these findings concisely. Despite their continuing HIV-positive status, the ex-drug user would hopefully be able to find an improved quality of life, and possibly look on their treatments for continuing treatments for HIV more positively without their former vice. References "Turning Point Somerset" Needle Exchange Guidelines, Turning Point Somerset, 2006. Accessed online. Australian Intravenous League & National Hepatitis C Education and Prevention Program (2000): Safer Injecting (educational leaflet), accessed online Becker, M.H. (1974): The health belief model and personal health behaviour. New Jersey: Slack Bejerot, N. (1988): "The Swedish Addicton Epidemic in Global Perspective" (speech given in France, the Soviet Union and the USA). Stockholm: Carnegie Institute. Buchbinder, S.P., Katz, M.H., Hessol, N.A., O'Malley, P.M., Holmberg, S.D. (1994): "Long-term HIV-1 infection without immunologic progression." AIDS 8 (8): 1123-8 Butler, A.C., Chapman, J.E., Forman, E.M., Beck, A.T. (2006): "The empirical status of cognitive-behavioural therapy: a review of meta-analyses." Clinical Psychological Review 26 (1): 17-31 Campbell, Denis (2009): "UK addicts may be given free foil for 'safer' heroin smoking". Article in The Observer, issue dated 20/09/2009 (accessed online via guardian.co.uk) Caplan, G. (1961): An approach to community mental health. New York: Grunne & Stratton. Day, C., Degenhardt, L., Gilmour, S., Hall, W. (2004): "Effects of reduction in heroin supply on injecting drug use: analysis of data from needle and syringe programs". BMJ (British Medical Journal) 329 (7463): 428–429 Downie, R.S., Tannahill, C., Tannahill, A. (1996): Health Promotion: Models and Values (Second Edition). Oxford: Oxford University Press. Fornataro, K., Obermeyer, T. (1992): "Informational materials for HIV-positive intravenous drug users." International Conference on AIDS (July 19-24, 1992): 8 (210) Grov, C., Parsons, J. T. (2006): "Bugchasing and Giftgiving: The potential for HIV transmission among barebackers on the Internet." AIDS Education and Prevention 18: 490-503. Health Protection Agency. “Shooting Up – Infections among injecting drug users in the United Kingdom 2005, An update: October 2006” Hilton, B.A., Thompson, R., Moore-Dempsey, L., Janszen, R.G. (2001): "Human reduction theories and strategies for control of human immunodeficiency virus: a review of the literature." Journal of Advanced Nursing 33 (3): 357-70 Joint United Nations Programme on HIV/AIDS (2006): "Overview of the global AIDS epidemic". 2006 report on the global AIDS epidemic. Viewed online. Lambeth PCT policy on alcohol and drug misuse. Lambeth PCT: author and year unspecified (updated regularly). London and Inner London bulletins and other information, Terrence Higgins Trust (accessed online via tht.org.uk, 2009) London Borough of Enfield's Pharmacy Needle Exchange leaflet. Rugby House community alcohol & drug services, LBE (author and date unspecified on leaflet) Mathers, B.M., Degenhardt, L., Phillips, B., et al. (2008): "Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review." Lancet 372 (9651): 1733-45 Murphy, E., Collier, A., Kalish, L., Assman, S., Para, M., Flanigan, T., Kumar, P., Mintz, L., Wallach, F., Nemo, G. (2001): "'AIDS Cocktail' Therapy Helps Even Most Advanced Patients." Annals of Internal Medicine, July 3, 2001 (via universityofcalifornia.edu) National Strategy for Sexual Health and HIV, Department of Health, 2001 (accessed online via dh.gov.uk, 2009) Palella, F.J.Jr, Delaney, K.M., Mooman, A.C., Lacless, M.O., Fuhrer, J., Satten, G.A., Aschman, D.J., Holmberg, S.D. (1998): "Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection." Journal of Infectious Diseases 48 (1): 1-12 Pender, N.J. (1996): Health Promotion in Nursing Practice (Third Edition). Stamford: Appleton and Lange Radnedge, Aidan (2009): “Trainspotting chic sees drug use rise”. Headline article in Metro, issue dated 09/10/2009 Reducing Drug-Related Harm: An Action Plan, Department of Health, 2007 (accessed online via dh.gov.uk, 2009) Reese, L., Chasan, R., Fishbein, D.A. (2009): “HIV and hepatitis C virus coinfection: approach to management.” Journal of Clinical Outcomes Management 16 (9): 415-28 Statistics on Drug Misuse: England 2009, published by The NHS Information Centre (via statistics.gov.uk) Talk To FRANK (accessed online via talktofrank.com, 2009) Tones, K., Tilford, S. (1994): Health Education: effectiveness, efficiency and equity (Second Edition). London: Chapman and Hall Ward, E., King, M., Bower, P., Sibbald, B., Farrelly, S., et al. (2000): "Randomised controlled trial of non-directive counselling, cognitive-behavious therapy, and usual general practitioner care for patients with depression." I: Clinical effectiveness. British Medical Journal, 321, 1383-88 Weber, R., Ledergerber, B., Opravil, M., Luthy, R., International Conference on AIDS (1990): "Cessation of intravenous drug use reduces progression of HIVinfection in HIV+ drug users." International Conference on AIDS 20-23 (6): 142