Supplementary Information (doc 86K)
advertisement
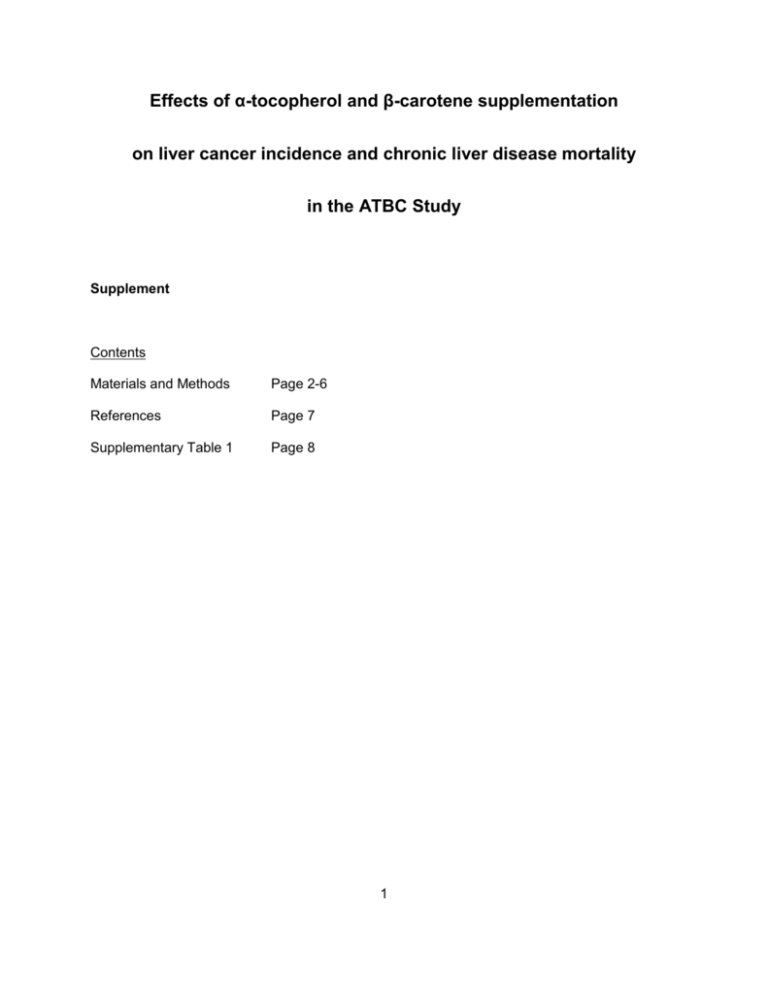
Effects of α-tocopherol and β-carotene supplementation on liver cancer incidence and chronic liver disease mortality in the ATBC Study Supplement Contents Materials and Methods Page 2-6 References Page 7 Supplementary Table 1 Page 8 1 Materials and Methods Participants Details about the ATBC study have been reported previously (The Alpha-Tocopherol Beta Carotene Cancer Prevention Study Group, 1994; The ATBC Cancer Prevention Study Group, 1994; Virtamo et al, 2003). Study participants were men living in southwestern Finland, aged 50-69, who reported smoking five or more cigarettes per day and agreed to participate in the study. Those with a prior malignancy, severe angina on exertion, chronic renal failure, severe liver cirrhosis, alcoholism, anticoagulant therapy, or were currently using vitamin E (>20 mg/day), vitamin A [>20,000 IU/day (>6000 microgram/day)], or β-carotene (>6 mg/day) supplements were excluded. A total of 29,133 eligible participants were randomly assigned to one of four intervention groups: 1) α-tocopherol (DL-α-tocopheryl acetate, 50 mg/day, 2) β-carotene (20 mg/day), 3) both agents, 4) or placebo. The men were enrolled between 1985 and 1988, and intervention continued until April 30, 1993. For the purposes of this study, we excluded 28 men who reported at baseline having mild liver cirrhosis, resulting in a final analytic cohort of 29,105. All participants provided written and informed consent before randomization. The institutional review boards of the National Public Health Institute, Finland, and the National Cancer Institute, USA approved the study. Data collection At baseline, information such as medical history, smoking, and alcohol intake were collected. An overnight fasting blood sample was also drawn from each participant and stored at -70°C. Serum α-tocopherol and β-carotene levels were obtained via high performance liquid chromatography (Milne & Botnen, 1986) while total and high-density lipoprotein (HDL) 2 cholesterol were measured using an enzymatic assay (CHOD-PAP method, Boehringer Mannheim, Germany). Over the course of the trial, participants visited local study centers every four months during the active intervention to complete follow-up questionnaires, return any unused study capsules, and receive a new capsule supply. Adherence was evaluated by counting the remaining capsules. Both compliance and drop-out rates were comparable across all intervention arms. Compliance among those taking supplements was high (median 99%) and approximately 80% of participants took over 95% of their capsules while in the trial. Compliance was subsequently confirmed by serum measurement of α-tocopherol and β-carotene after three years of supplementation. Follow-up and outcome ascertainment Incident liver cancer cases (n=208; ICD-9=155 and ICD-10=C22) were identified through the Finnish Cancer Registry which provides close to 100% case ascertainment (Korhonen et al, 2002). The medical records of 80% of the cases were reviewed by a study physician to confirm the diagnosis of liver cancer while Finnish Cancer Registry data only was available for the remaining 20%. Mortality from chronic liver disease (n=237; ICD-9=571 and ICD-10=K70, K73, or K74) was identified through the Finnish Register of Causes of Death. Validation studies of the register have found it to be excellent (Lahti & Penttila, 2001). The noted underlying cause of approximately 90% of the chronic liver disease deaths was alcohol-related liver diseases. For liver cancer, follow-up time began at the date of their randomization and continued until the date of cancer diagnosis, death, or until December 31, 2009, whichever came first. For liver disease mortality, follow-up time began at the date of their randomization and continued until the date of death (from chronic liver disease for the cases, or other causes for the controls), or until December 31, 2009, whichever came first. 3 Laboratory analyses Measurements for whether participants were ever infected with HBV (anti-HBc) or were currently infected (HBV surface antigen (HBsAg), antibody for hepatitis C virus (anti-HCV), and baseline serum insulin and glucose were performed on a subset of the study participants with sufficient serum. This subset – men who died of chronic liver disease, men with incident liver cancers, and their 2:1 controls matched on age (±5 years) and date of blood draw (±30 days) – were selected and sampled to conserve both costs and serum. Information on HBsAg, anti-HBc, and anti-HCV was available among 212 men who died of chronic liver disease, 167 men with incident liver cancer, and 817 controls. Information on serum insulin and glucose was available for 214 participants who died of chronic liver disease, and 144 who developed liver cancer. Serum insulin was available in 718 controls and serum glucose was available in 721 controls. Testing for presence of HBsAg, anti-HBc, and anti-HCV in fasting serum samples was performed by SAIC NCI-Frederick National Laboratory. HBsAg was assayed using an enzyme immunoassay from Bio-Rad Laboratories (Redmond, WA), while anti-HBC and anti-HCV were tested using enzyme-linked immunosorbent assays from Ortho-Clinical Diagnostics (Raritan, NJ). Both serum insulin and glucose concentrations were measured by the Mayo Clinic. Serum insulin was measured with a two-site immunoenzymatic assay performed on the Dxl automated immunoassay system from Beckman Instruments (Chaska, MN). The inter-assay coefficient of variation was 3.2% (range: 1.5% - 5.7%). Serum glucose was measured on the Hitachi 912 Chemistry Analyzer using a hexokinase reagent from Boehringer Mannheim (Indianapolis, IN). The inter-assay coefficient of variation was 0.6% (range: 0.1% - 2.1%). Statistical analysis 4 All statistical analyses were based on intention-to-treat. Kaplan-Meier survival curves were plotted for the four intervention groups. The effect of intervention was estimated by Cox proportional hazards regression and reported as hazard ratios (HRs) and 95% confidence intervals (CIs). We present the effect for each intervention group (α-tocopherol, β-carotene, αtocopherol + β-carotene vs. placebo) as well as each individual agent (α-tocopherol supplementation [α-tocopherol vs. no α-tocopherol] and β-carotene supplementation [βcarotene vs. no β-carotene]). Results are also provided separately for the intervention and postintervention periods. To consider the possibility that skin yellowing from supplementation might be related to the detection or diagnosis of liver cancer or liver disease, we conducted separate analyses restricting to men who did not report any persistent skin yellowing and results did not change. In addition, we examined results in pre-specified baseline subgroups defined by median age (<57 years, ≥57 years), alcohol use (<26 g/day [~2 drinks/day], ≥26 g/day), median BMI (<26 kg/m2, ≥26 kg/m2), median smoking dose (<20 cigarettes/day, ≥20 cigarettes/day), median serum α-tocopherol (<11.5 mg/L, ≥11.5 mg/L), median serum β-carotene (<170 µg/L, ≥170 µg/L), and median serum total cholesterol levels (<6.15 mmol/L, ≥6.15 mmol/L). In the subset of cases and controls with information on HBV and HCV, we assessed associations among those who were both HBV(-) and HCV(-). In the subset with information on serum glucose and insulin levels, we also assessed associations in pre-specified groups of diabetes status (blood glucose <100 mg/dL and no history of diabetes [without diabetes]: 100-<126 mg/dL and no history of diabetes [prediabetes]; ≥126 mg/dL or history of diabetes [with diabetes]) and insulin levels (<4.7 µU/mL, ≥4.7 µU/mL). For these subset analyses, the effect of intervention was estimated by unconditional logistic regression and reported as odds ratios (ORs) and 95% CIs. We used all controls for each endpoint to conserve power. However, sensitivity analyses restricted to cases and their matched controls were similar though less precise. The P values for all 5 statistical tests were 2-sided, and statistical significance of 0.05 was used. All analyses were performed using SAS 9.2 (SAS Institute, Cary, NC). 6 References Korhonen P, Malila N, Pukkala E, Teppo L, Albanes D, Virtamo J (2002) The Finnish Cancer Registry as follow-up source of a large trial cohort--accuracy and delay. Acta oncologica (Stockholm, Sweden) 41(4): 381-8 Lahti RA, Penttila A (2001) The validity of death certificates: routine validation of death certification and its effects on mortality statistics. Forensic science international 115(1-2): 15-32 Milne DB, Botnen J (1986) Retinol, alpha-tocopherol, lycopene, and alpha- and beta-carotene simultaneously determined in plasma by isocratic liquid chromatography. Clinical chemistry 32(5): 874-6 The Alpha-Tocopherol Beta Carotene Cancer Prevention Study Group (1994) The Effect of Vitamin E and Beta Carotene on the Incidence of Lung Cancer and Other Cancers in Male Smokers. The New England journal of medicine 330(15): 1029-35 The ATBC Cancer Prevention Study Group (1994) The alpha-tocopherol, beta-carotene lung cancer prevention study: design, methods, participant characteristics, and compliance. Annals of epidemiology 4(1): 1-10 Virtamo J, Pietinen P, Huttunen JK, Korhonen P, Malila N, Virtanen MJ, Albanes D, Taylor PR, Albert P (2003) Incidence of cancer and mortality following alpha-tocopherol and beta-carotene supplementation: a postintervention follow-up. Jama 290(4): 476-85 7 Supplementary Table 1: Baseline characteristics of the cohort in the four intervention arms of the ATBC Study No. of participants Age, years† Placebo α-tocopherol only β-carotene only α-tocopherol + βcarotene 7282 56 (53-61) 7280 57 (53-61) 7274 57 (53-61) 7269 57 (53-61) BMI, kg/m2† 26.0 (23.6-28.6) 26.0 (23.7-28.5) 25.9 (23.6-28.5) Age when starting to smoke, years† 19 (17-21) 19 (17-21) 19 (17-21) Elementary school education, % 75.5% 75.2% 75.3% Alcohol intake, g/day† 10.8 (2.6-25.4) 11.3 (2.5-25.9) 11.0 (2.6-25.3) Years of smoking† 36 (31-42) 36 (31-42) 37 (31-42) Number of cigarettes smoked/day † 20 (15-25) 20 (15-25) 20 (15-25) Serum α-tocopherol, mg/L† 11.5 (9.8-13.5) 11.4 (9.7-13.6) 11.5 (9.7-13.6) Serum β-carotene, µg/L† 171 (111-260) 168 (109-261) 170 (106-263) Serum cholesterol, mmol/L† 6.14 (5.43-6.92) 6.15 (5.42-6.94) 6.15 (5.46-6.92) History of diabetes mellitus, n, % 278, 3.8% 297, 4.1% 329, 4.5% Serum glucose, mg/dL*† 99 (93-107) 98 (92-104) 100 (93-109) Serum insulin, µU/mL**† 4.2 (3.0-6.1) 4.0 (2.6-6.5) 4.4 (3.0-7.1) Hepatitis B surface antigen, n, %*** 3/188, 1.6% 2/220, 0.9% 0/216, 0% Hepatitis B core antigen, n, %*** 16/188, 8.5% 13/220, 5.9% 17/216, 7.9% Hepatitis C, n, %*** 2/188, 1.1% 0/220, 0% 1/216, 0.5% † Presented as medians (interquartile range) * In a subset of 721 men who did not die of chronic liver disease or was diagnosed with incident liver cancer ** In a subset of 718 men who did not die of chronic liver disease or was diagnosed with incident liver cancer *** In a subset of 817 men who did not die of chronic liver disease or was diagnosed with incident liver cancer 8 26.0 (23.7-28.6) 19 (17-21) 74.5% 10.8 (2.5-25.6) 36.5 (31-42) 20 (15-25) 11.6 (9.8-13.6) 172 (111-260.5) 6.18 (5.45-6.97) 335, 4.6% 100 (93-107) 4.5 (2.9-6.7) 1/193, 0.5% 11/193, 5.7% 2/193, 1.0%