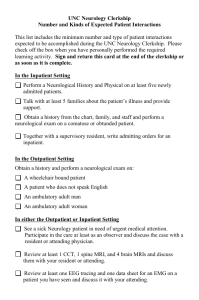
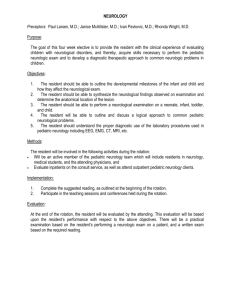
NEUROLOGY CLERKSHIP MANUAL
advertisement

NEUROLOGY CLERKSHIP MANUAL & SURVIVAL GUIDE WASHINGTON UNIVERSITY SCHOOL OF MEDICINE Rob Naismith, M.D. Clerkship Director V6.15.11 1 Contents The Central Axiom ................................................................................................................................ 3 Why Should We Study the Brain ........................................................................................................... 3 What Makes Neurology Different .......................................................................................................... 3 Dispelling Some Myths ......................................................................................................................... 4 Neurology Clerkship Goals and Objectives ........................................................................................... 6 Neurology Clerkship Requirements and Expectations .......................................................................... 8 Days Off ................................................................................................................................................ 8 Grading ............................................................................................................................................... 10 Teams and Presentations ................................................................................................................... 11 Patient Logs ........................................................................................................................................ 11 Textbooks ........................................................................................................................................... 12 Pre-Printed H&P Forms ...................................................................................................................... 12 Dress .................................................................................................................................................. 12 Computers .......................................................................................................................................... 13 Clinics ................................................................................................................................................. 13 The OSCE ....................................................................................................................................... 13 CONFERENCES ............................................................................................................................. 15 ROTATION DESCRIPTIONS AND REQUIREMENTS ....................................................................... 16 INPATIENT ADULT NEUROLOGY ................................................................................................. 16 NEUROSURGERY .......................................................................................................................... 19 PEDIATRIC NEUROLOGY CONSULTS ......................................................................................... 22 WEEKLY GENERAL NEUROLOGY CLINICS ................................................................................ 23 SURVIVAL GUIDE for the NEUROLOGY CLERKSHIP ...................................................................... 24 The Neurological History ................................................................................................................. 24 The Neurological Exam ................................................................................................................... 25 Write-Ups ........................................................................................................................................ 25 Presentations .................................................................................................................................. 26 SUPPLEMENTARY MATERIAL ......................................................................................................... 28 Neurological Diagnosis ....................................................................................................................... 28 Presentation of the Patient with Neurological Disease ........................................................................ 33 Steps to Approaching the Neurological History ................................................................................... 37 Steps to Approaching the Neurological Examination .......................................................................... 38 General considerations.................................................................................................................... 38 Mental Status .................................................................................................................................. 39 Cranial Nerves ................................................................................................................................. 39 Motor exam ..................................................................................................................................... 41 Reflexes .......................................................................................................................................... 41 Sensation ........................................................................................................................................ 42 Coordination and gait ...................................................................................................................... 43 Meningeal Signs .............................................................................................................................. 43 The Neurological Write-Up .................................................................................................................. 44 Exam ............................................................................................................................................... 46 Assessment and Plan ...................................................................................................................... 46 Step-by-Step Guide to the Neurological Examination ......................................................................... 48 Sample neurological H & P ................................................................................................................. 57 NEUROLOGY CLERKSHIP MID-ROTATION FEEDBACK FORM ..................................................... 60 NEUROLOGICAL EXAM FEEDBACK FORM..................................................................................... 62 NEUROLOGY CLERKSHIP EVALUATION FORM ............................... Error! Bookmark not defined. V6.15.11 2 ORIENTATION FOR NEUROLOGY CLERKSHIP Welcome to your Neurology Clerkship. Please read this manual before orientation. It will also help clarify your first few days of the rotation, which can be the most confusing and stressful days. The Central Axiom Everything you have worked for has been for this moment. The brain lies at the center of our personal universe. It transforms a chaotic world of hurling particles into the perception of sense and stability. In addition to creating a sensory representation of reality, the brain also allows us to be aware of ourselves and others. Every nervous system process can be deconstructed into sensation, movement, emotion, memory, and communication. The brain allows humans to create, explore, interact, and yearn for something better. It contains our greatest dreams and hopes, as well as our fears and nightmares. It is where life and religion originate. It is where good and evil reside. It is where life ends. The central axiom of medicine is simple. Support and protect the brain. Everything you have learned in medical school has directly or indirectly been for this purpose. The TCA cycle, G proteins, anatomy of the heart, acid/base balance and the kidney, and oxygen transport with the blood and lungs are all critical to keep the brain alive. Do not misinterpret this to mean that everyone should become a Neurologist. That would be foolish, and not in the brain’s best interest. We need cardiologists, nephrologists, and pulmonologists. In the game of chess, the pawns are important as well. If every piece was the king, then chaos would reign. Just as the body has divided the organs to protect and support the brain, so must the field of medicine emulate this division of labor for the greater good. So rest assured. The goal of this clerkship is not to transform every medical student into a Neurologist. Why Should We Study the Brain “Hearts and kidneys are Tinkertoys! I’m talking about the central nervous system”. -Gene Wilder, Young Frankenstein The brain is by far the most complex and fascinating organ of the body. Although some may try to argue, it is the organ most worthy of a lifetime of study. The brain can be contrasted with the heart, which undoubtedly plays a key supportive role. The heart, in all its intricacy, comes down to 4 chambers, 4 valves, and some electrical wire. Of note is that it can also be replaced, by a man-made rendition. The heart of one person can be transplanted into another person within a matter of hours. Now, how complicated can that be? There remains much to be known about the brain. Although tremendous strides are made each year, the study of the brain remains in its infancy. This black box is intimidating for many medical students, but has also been the source of fascination for the world’s greatest scientists, writers, and philosophers. It’s true that you cannot measure pressure or volume or electrical conductance for the brain as you can with the heart. As quoted by Emerson Pugh: “If the human brain were so simple That we could understand it, We would be so simple That we couldn't.” What Makes Neurology Different As you make your way through your clerkships, you will note that each field has a particular approach to patients, and also tends to attract a certain personality. You will find most neurologists are both curious and content. Primary importance continues to be placed upon a proper history in order to arrive at the correct diagnosis and course of action. Although there are pressures upon everyone in medicine to see more patients, the initial evaluation cannot be short-rift. In clinic, a new patient visit can take an hour, and a follow-up can take 30 minutes. For a complicated new patient in the hospital with an acute problem, it may take well over an hour to do the initial assessment. We learn medicine by talking with patients. Textbooks serve as a guide, but patients translate the medical terminology into the human experience. No one is an expert by reading a book chapter and seeing a V6.15.11 3 single person with a given condition. It will take many patients with a given condition and followed over years until you begin to realize how a disease presents and affects someone. The contact with your patients is invaluable and needs to be fully appreciated. If you know how to listen and make observations, it will enrich your practice and the rest of your life. A good history takes time. Over several years, you will learn to ask open-ended and non-leading questions. Neurologists from a previous generation would say that you get nothing meaningful in the history during the 1st half hour! Unfortunately, there are some time constraints, so most histories should be completed in 20-30 minutes unless they are complicated. As you obtain the history, you start to form a hypothesis about what is going on. Additional questions will further test your hypothesis and develop concepts relating to localization. You will then ask additional questions to help refine your localization. The history is a dynamic process that does require some skill and experience. You need to be flexible to get the information, and you need to scrutinize that information for further clarification to help with medical decision making. You also need the know how to phrase each openended question so that the patient will provide a description in their own words. Computers can ask questions, physicians elicit a history. It is also crucial to understand something about the patient’s environment, and how their illness has impacted their ability to function. The physical exam is also a dynamic process. Every patient will get a complete examination, but you need to be flexible and scientific as well. You will carefully scrutinize key parts to test your hypotheses and convince yourself whether a sign is truly present or absent. If you are unsure, you need to repeat the exam maneuver until you are sure. An Attending can spend either 10 seconds on the reflexes or 5 minutes, depending upon the clinical scenario. This need to think on-your-feet becomes very enjoyable once comfortable with the concept. In addition to talking, Neurologists like to examine patients. The neurological exam is very important and serves many purposes. Most patients, unless they have headaches or seizures, will have many interesting neurological findings. If you come to movement disorders or multiple sclerosis clinic, then almost everyone has an abnormal physical exam. The exam can take a substantial part of the office visit. Since you spend time touching the patient, it also helps to solidify the physician-patient relationship. Some medical specialties see the exam as a necessary formality that doesn’t yield much useful information. This is not so for Neurology, and is an inextricable component of a proper assessment. The neuro exam will not often give you an answer as to the diagnosis, because the findings are typically not that specific. However, it will give you an idea as to where to localize, how much the person is functionally affected, and also a differential diagnosis. One can really appreciate how people have difficulties in their everyday lives by examining them. Some may find it frustrating that most neurological diseases do not have a laboratory test that gives a ‘yes’ or ‘no’ answer. Parkinson’s disease is based solely upon the clinical characteristics of a unilateral tremor with bradykinesia, rigidity, and postural instability. Despite strides in neurodiagnostic testing, it also remains true that migraines, epilepsy, M.S., and stroke remain a diagnosis based on predominantly on clinical grounds. It is not like doing a cardiac catheterization to determine if they have coronary disease. Neurologists know how to spend money on tests, this is for sure. However, a test without the proper reasoning will often create more confusion than illumination. Finally, neurologists tend to enjoy talking about their specialty. Since the brain is so interesting, it is hard not to teach and discuss. Patient rounds can be long, but hopefully you will find them both educational and enjoyable. Rounds are your opportunity to observe the experienced attending, who has been doing this for some years. Basically, everything the attending says and does with the patient is for a particular reason. There is a lot of learning that can be accomplished on rounds, even though it may not seem like there is specific ‘teaching’. Dispelling Some Myths Neurology is depressing. Untrue. The first reason for this misconception is that 2nd year medical school courses are often taught based upon pathology. While our Pathologists do a wonderful job at explaining the basis and the structural changes associated with neurologic diseases, pathology is biased to those patients who did not do well. What you learn about are the large strokes that herniated and died. And the HSV-Encephalitis that herniated and died. And the end-stage Alzheimer’s that aspirated and died. V6.15.11 4 Second, medical school clerkships are often based on inpatient experiences. There is no doubt that inpatient neurology contains its fair share of neurological catastrophes. But that experience should not be construed as typical. When you go to outpatient clinic, you will notice strokes and MS and headaches and epilepsy and Parkinson’s disease, with people who are doing remarkably well. Third, even some of the neurological catastrophes do remarkably well. You are seeing these patients in their darkest hour. They are comatose, paralyzed, cannot speak or understand. You don’t always get to see them in 6 or 12 months. For many, recovery can be remarkable. Finally, this all needs to be placed into perspective. Unless you are doing well-visits in family practice, every field in medicine has its depressing side. Pediatric oncology can also be depressing. Many people with heart and lung and kidney disease are severely disabled and not doing well. Sometimes we mistake our impression of control and our ability to prescribe modest therapies as equivalent to being effective. Diagnose, then adios. Again, false. The charge is two-fold: that Neurologists are only interested in the processes of localization and diagnosis, and that there are no treatments. As the joke goes, the neurologic therapeutic arsenal contains phenytoin, steroids, and heparin. First, you need to understand that your power as a doctor is not just because you can prescribe medications. Listening to patients is the most important thing you can do, and it can be very therapeutic. Patients can discuss their inner-most concerns without fear of reprisal or judgment. And they can discuss their varied symptoms with someone who understands them. Many people feel uncomfortable telling this stuff even to their spouse, family, or close friends. Some worry that they are crazy or that their experience is unique. Conveying their experience can be cathartic. Second, neurology does have many therapeutic agents. Whether it is MS or epilepsy or headache or movement disorders, there has been tremendous development of effective medicines. Third, what we can do for our patients is not limited to supporting the pharmaceutical company. We teach and provide information. We serve as a liaison for support groups. We coordinate multi-disciplinary teams for dealing with serious illness. Rehabilitation medicine strives to keep people ambulating, mobile, working, and doing all those other things in their life which they care about. We can offer clinical trials that may help the patient, and will hopefully lead to new therapeutic options. Neurology is too complicated. Wrong. The first week of the rotation might be a bit intimidating. Between remembering your neurosciences, neuroanatomy, diseases of the nervous system courses, localizing the lesion, and prioritizing a differential diagnosis, there is definitely much information to consider. However, within a week, you will be doing all these things. By the end of the 4 weeks, you should have a very good appreciation of how to recognize and communicate neurological issues to other physicians. The MRI will replace Neurologists. Yeah. Right. They’ve been saying this since the first head CT scanner was created in the ‘70s. I’m not too worried. Expectations For This Rotation This will not be an easy rotation. There is much work expected of you. Between taking care of patients, preparing for different rounds, and keeping with the reading assignments, it will definitely be a challenge. This is the type of rotation where you will get-out whatever you put in. If you take ownership and responsibility for your patients, then you should definitely feel like an important part of the team. You should be proactive about obtaining additional experiences during your brief time. Time flies when you are busy. This month will go by very quickly. You might want to consider petitioning the school to make it a 6week rotation. Until that happens, you are always welcome back for another month in your final year. V6.15.11 5 Neurology Clerkship Goals and Objectives Proficiency in obtaining a complete history in patients with the following neurological complaints: Disorders of consciousness Mental status and/or behavioral changes Memory complaints Pain in the head, neck, and back Numbness, paresthesias, and neuropathic pain Weakness and clumsiness Dizziness and vertigo Disorders of language Neurogenic bladder and bowel Vision loss and diplopia Dysarthria and dysphagia Abnormal movements Sleep-related complaints Understand the patho-physiology and treatments for the following neurological conditions: Ischemic stroke Hemorrhagic stroke Subarachnoid hemorrhage Subdural and epidural hemorrhage Structural coma Metabolic encephalopathies Neuro-toxicology and vitamin deficiencies Meningitis and encephalitis Dementia and memory disorders Seizures and epilepsy (including status epilepticus) Syncope Vertigo Headache disorders (Migraine, cluster, tension, analgesia-overuse, neuralgias) Neck and back pain Myelopathies Radiculopathies (including cauda equina syndrome) Nerve compression Neuropathies Multiple Sclerosis and other immunologic diseases (sarcoid, SLE, paraneoplastic disorders) Movement disorders (Parkinson’s disease, essential tremor, Huntington’s disease, tics, medication-induced dyskinesias) Neuromuscular disorders (Myasthenia, Lambert-Eaton, botulism) Myopathies Brain tumors Head trauma Comfort with the neurological examination, so that you could communicate medical problems to a neurologist regardless of your chosen field. Complete neurological exam Focused neurological exam Coma exam Localization based upon the history and examination Understand the neurological tests that are available and what purpose they serve: MRI, including a basic understanding of reading. Lumbar puncture CT, including a basic understanding of reading. EEG Nerve conduction studies / Electromyography Evoked potentials V6.15.11 6 Myelogram Sleep studies Demonstrate a commitment for reading about your patients and lifelong learning Core reading throughout the clerkship Reading in-depth about your patients Ability to discuss pertinent topics on rounds Concepts of Evidence-Based Medicine Ability to put your patients at ease and establish an effective relationship. Take a complete history with open-ended non-leading questions. Understanding the disease in the context of a person’s life and the way it affects them. Professional and empathetic first encounter Speaking with families Keeping your patients informed about upcoming tests and treatment plans See how residents and attendings hold family discussions and deliver bad news Communicate effectively and efficiently to other physicians and health care members regarding patients. Informal and formal patient presentations Initial H&P Notes Progress and Follow-up Notes Coordinating disposition with PT, OT, ST, Social work, and Case manager Writing orders, discharge papers, and prescriptions Demonstrate a mature and professional demeanor to patients, peers, residents, and attendings. Presentation skills Participation in discussion during rounds and conferences Taking ownership of your patients Interest and learning from other patients you are not directly following Paying attention during rounds Understand the reasons for patient admissions, consults, transfers, disposition, and follow-up appointments. How to decide on whether to admit a patient, and to which service they should be admitted to When to transfer someone to another service or to the ICU When to call and not to call a consult Reasons for discharge to home (including appropriateness of home-based services), rehab, skilled nursing/extended care facility, and long-term nursing facility . Awareness of social, ethical, and privacy issues within medicine. HIPAA Communication Insurability Economics of health care Research Confidentiality Altruism, beneficence, autonomy, paternalism, duty, rights, equality, justice, liberty, nonmaleficence Advanced directives Vegetative states V6.15.11 7 Neurology Clerkship Requirements and Expectations Pre-round on your patients. Be aware of the results for all tests, consultant notes, problems overnight, etc. Pick-up at least two patients on call-days, one patient on a non-call admitting day. (May vary according to census) When on call, be available all night to work-up patients and assist your resident. Be well-prepared to present your patients precisely and completely during rounds, including localization, prioritized differential, and your plan. Pay attention to what is happening on rounds. Everything the attending says and does is for a reason. Participate in discussion on rounds and in conferences. Keep your patients informed, check-in with them at the end of the day. Politely excuse yourself when you have to leave for a required teaching session. Have your H&P in the chart on the day of admission, before morning rounds if admitted overnight. Have your notes complete and ready to be evaluated by your resident by approximately noon. Write orders, help coordinate disposition and follow-up. Request critical feedback from your resident in the second week of your rotation. Respond to deficiencies with a plan for improvement. Have your resident witness your physical exam on a patient, and fill-out your sheet. Come to conferences prepared and ready for discussion. Hand back feedback forms preferably by the 2nd week, and no later than the 3rd week. This includes mid-term feedback, witnessed exam, H&P. Hand in your patient and required circumstance logs at the end of the clerkship. Michelle Aubuchon can collect these, and she is on the 3rd floor. Be pro-active about seeing patients and creating learning opportunities. V6.15.11 8 First Day, Call, and Days Off BEGIN PATIENT CARE ON DAY ONE. After you meet with your resident to review expectations and procedures, run the patient list and ask which patients you should begin to follow. All patients whose work-up is ongoing should be divided among the students on the team. If these patients have already been presented on rounds, you need not do an initial H&P. Rather perform a thorough chart review and meet with each patient to review their history and physical exam so you will have a first-hand understanding of their situation. Help with a progress note and any coordination of care for that day. The next day, pre-round, update the team on rounds, and assist with their medical care. It is absolutely critical that you become very involved in patient care on day 1, because the adult inpatient rotation is so short! You must not wait until your call day to receive patients. Short-calls are admissions, transfers, or hand-offs that occur between 7AM-5PM. You should pick-up at least 1 short-call patient whenever your resident receives such a patient. If a short comes during the morning, and you have conference and clinic, then you need to return after clinic to finish the work-up and get the note in the chart. You should pick-up at least 2 patients while on-call. You should take the first 2 available patients on your call day. Do not wait for the “perfect” patient. You will take both general neurology and stroke patients when on-call. You should also work-up patients from faculty members (who may not be presented on rounds). Your resident will play a crucial role in the grading process, so working-up a patient who may not necessarily be presented on morning rounds will definitely count towards your clinical assessment. Out of a 6-day schedule on adult inpatient, your goal is to work-up a minimum of 5 new patients with full H&Ps. Your call day will begin with rounds that day. While your assigned resident will start at 5pm, you should prepare for rounds and help provide continuity. Post-call, you are done at 1pm if there is a required student conference, or noon if there is not a required student conference. You are excused from post-call conferences after 1pm. You are not to be in the hospital for over 30 hours on your call day. Your resident will stay the remainder of the day to complete the patient care without your assistance because they started their call time later than yours. When you return on the morning of your post-post-call day, be sure to update yourself before rounds on what transpired on your patients the previous afternoon. If something significant happened that you don’t know about, it will not look good on rounds that you are out of the loop. Everyone will have at least 5 days off over the rotation. These will be specified on the schedule. Everyone will have the same number of calls (2). Residents are on call every 6th evening. The residents have 44 hours off each week, which includes their pre-call day, and ends when they start call at 5 pm. Because we are desynchronizing the student/resident schedule, you will need to spend time working with another resident on your assigned resident’s day off. When your resident is off, first check with the floor chief resident to see if there are any particular patients you should follow, or particular teams you should assist. The chief resident may know of an interesting patient that does not yet have a student. The busiest team on the service is usually the post-call team, followed by the post-post-call team. Your job is to provide continuity for your team’s group of patients that day, and to assist one of the busier other teams. If your first day coincides with your residents day-off, then review the charts and patients from that team, and help with the progress notes. If you are finishing inpatient adult during the 1st half of the rotation, you will be done Friday evening unless you are on call Friday. If you are finishing call on Friday, then you stay through rounds on Saturday, Sunday is a day off, and you start the next half on Monday. If you are starting inpatient adult service during the 2nd half of the rotation, you will begin on the weekend (Saturday). Someone will take call on Friday starting at 5pm. Because the 2nd half is shorter due to the OSCE and written exam, we need to start Friday evening so no one needs to take a test post-call. You should still be on consults Friday during the day if you are on-call that evening for your switch. For the student taking call the 1st Friday of the 2nd half, you may be overlapping with the student finishing their last call, which is not bad for continuity and orientation. There are several options for call rooms. The first is the main call room area on 11400. There are 2 rooms, one for the on-call resident, and another room which may be available. There are also call rooms behind 4321 Rand Johnson. The 4324 call suite has two entrances on its north side. In the corridor between these doors, there is a brass-colored drinking fountain. Across the hall from this fountain is an unmarked door with a card reader. This is the western entrance to 4321, and the medical student call rooms are just inside that door. The call rooms are accessed by card swipe. Also let us know whether your card does not work, because there have occasionally been delays in having this activated. Here’s a pearl of wisdom on being post-call. You will feel much less tired if you take a few minutes to shower, dry your hair, and change into fresh clothes. Everyone else will appreciate it as well. Taking a few minutes for breakfast is also worthwhile. Coffee helps, too. The combination of all these things is probably equivalent to 2-3 hours sleep. You are done with your clinical rotation at 1pm on the final Thursday. If you are going to be absent for whatever reason, you need to inform your Supervising Resident and the Clerkship Director immediately. If you are sick for more than 2 days, we will need a note from student health. We follow the absence policy in the online Bulletin of WUSM Admissions and Educational Program Guide. V6.15.11 9 Duty Hour Policy for Medical Students The Neurology Clerkship follows the Washington University duty hour policy for medical students. This policy is similar to what the ACGME has instituted for residents. If your Neurology Clerkship experience is not consistent with this policy, please let Dr. Naismith know. The policy is: 1) Students must not have more than 80 clinical duty hours during a 7 day week, averaged over a 4 week period. 2) Students must have four 24-hour periods off over four weeks. 3) Students must not be on overnight call more than every third night. 4) Students cannot be on call for more than 24 successive hours, with an added period of up to 6 hours for continuity, educational debriefing, and didactic activities. No new patients should be assigned to students after 24 hours. 5) For a WU holiday, students are dismissed at 5pm the day prior, and return the day following the holiday. 6) Planned days-off need to be cleared well in advance with the clerkship director, and shall follow the absence policy for Clerkships. Make-up days will likely be required for any time off. The resident and the rest of the team need to be informed if you are not coming for any planned or unplanned reasons. Grading I take my responsibility to oversee the grading process very seriously. I still appreciate how important grading is for everyone. We actually enjoy giving honors. When we give honors, everyone feels good. However, we don’t want to trivialize this highest achievement. Nonetheless, if every student during the clerkship does honors-level work, then every student will get honors since there are no quotas. You are not in competition with your fellow classmates. Based upon past experience, roughly 30% will get honors. We have had blocks where all have gotten honors, and other blocks where none have. High-pass encompasses a wide-range of performances. There are many students who do a great job, but are just short of honors. If you hear feedback that you are doing a great job, but get a high-pass in the end, then this is not incongruous. High-pass is an ‘average’ WUSM performance, which is excellent. About 50% will get High-Pass. Pass is for someone who meets basic expectations, but does not improve, take initiative, contribute, or has some other deficiency. About 20% will get a Pass. Fail is for someone with considerable deficiencies that puts into question their ability to care for patients, has a systematic lapse in professionalism, and/or does something to seriously jeopardize the team approach and apprenticeship system. Our grades are based on a committee discussion. I believe that this committee discussion, which can consist of up to 15 people in the room, is to your benefit. That is because the people that know you the best will speak on your behalf. Much more constructive information comes out of this discussion rather than just having everyone turn in their sheet without putting together the whole picture. What if you had a bad day when you happened to present to your attending, but your resident saw how hard you worked during the rest of your rotation? This will come-out during the meeting and things are put into proper perspective. In addition, I will often speak directly with those not able to come to the grading session. So what distinguishes an honors student? This is a very easy question, and also a very hard question to answer. Of course, different attendings will have different criteria. I would distinguish someone who performs at the honors level as: 1) Someone who is very motivated and enthusiastic, with an unquenchable thirst for self-directed knowledge. 2) Someone who understands their role on the team. They can identify what needs to be done without overstepping their bounds, becoming obtrusive to the residents, or abrasive to their fellow students. They are pleasant to be around, even if they didn’t sleep the night before (we understand that some of us need our sleep, though). 3) Someone who uses the literature and self-directed learning to help answer questions. When it comes to the patients that you work-up, it is not good enough just to read about them in a paperback text, or even a general neurology text. You should use the available computers to pull-up articles that are relevant to that patient’s particular situation. ‘What is the evidence?,’ is a phrase that repeatedly comes up in this hospital. 4) Someone who shows tremendous respect for their patients. She/he ensures their comfort and privacy, speaks with them before leaving for the day to discuss test results and plan for the next day, and is available to meet with the family under their residents’ supervision. 5) Someone who is efficient at getting their work done while being thorough. 6) Someone who responds to feedback in a way that shows a desire for self-improvement and that you value the opinion of those supervising you. 7) Someone who displays respect for their colleagues, residents, and attendings. There is something to learn from everyone. We all have strengths and weakness. As a student, you should determine what things someone does that are admirable and can be emulated, even if you may not agree with everything that says and does. Likewise, complaining or V6.15.11 10 criticizing serves little useful purpose. You have a responsibility to learn and become a good doctor. Getting into a rut of cynicism or negativity can be a very destructive thing. The NBME (shelf) examination will comprise 20% of your grade. Scores are based on national percentiles. A grade of 75%tile is required for honors (less than the average score for WUSM). Students under the 10th percentile are required to retake the exam to Pass the rotation. Though not recognized by the school, we do use H-HP for those students who did a great job on their clinical performance, but are not quite at the honors level. If you are in this category and score over the 85th percentile, then your final grade will move up to honors. This grade designation has increased the number of honors that we give, and has not detracted from those who are truly clear honors. Likewise, we use the HP-P for those students who gave a pass performance, but we want to give the student a chance to demonstrate proficiency with the material. If you are in this category and score over the 75th percentile, then your final grade will move up to high-pass. Every month, there will be a patient-simulated examination or an OSCE that covers neurology. You will be required to pass this in order to pass your rotation. On occasion, I have used a very good OSCE performance to help pullup a student to the higher grade if they are truly between grades. If you do not pass the OSCE, you will get an incomplete clerkship grade until this is properly remediated. More information is found below in the section on the OSCE. For those of you who are shy, soft-spoken, quiet, or observe from the periphery, PLEASE make an effort to make your presence known. Perhaps the most troubling thing about grading is that there are excellent students who just blend into the background. These people do not distinguish themselves in the eyes of the attending or resident, and often get high-pass even though some are talented enough to be deserving of honors. You need to make a point to contribute to the discussion during the conferences and on rounds and make yourself heard. If no attending knows you at grading session, then this is a big problem that suggests your presence was not memorable. As a teacher, I find it gratifying when everyone participates. No teacher likes a group where pulling out discussion is like pulling teeth. Of course, no one likes someone who monopolizes the discussion or thinks they know everything, so you have to find the correct balance. Finally, I do not determine the grade. Please do not be mad at me if you did not get honors. After the rotation, I may see you in the hallway, and while I may not remember what grade you received, I often can tell by whether I get a hello or not. I realize that everyone is very smart and everyone is working hard. I supervise the process to ensure it is fair. As you just read, there are many components that need to be factored. Teams and Presentations The Neurology Service is divided into two teams: General Neurology and Stroke. Each team has an attending, a chief resident, and three neurology residents. You will be assigned to one team. Call alternates between the two teams. When on-call, you may work-up a patient who will be handed-off to the opposite team (e.g. you are on the stroke service, and you admit a general neurology patient). When you work-up a patient to be handed-off, discuss with your 2nd year neurology resident and your chief resident so you can present both patients at table rounds AND round on both patients at the bedside. Because the teams round at the bedside concurrently, you will not be directly following the patient after your post-call day. To facilitate bedside rounds on both your patients for the post-call day, your team should round first on your patients, and the opposite team will move your handed-off patient to the end of the rounds list, so that you are able to join. You should help with the work-up and tests for the handed-off patient on your post-call day, but then you should follow the patient peripherally. Once a patient is handed-off, you can still visit with the patient, read the chart, and discuss with others. You do not write notes on the patient once post-call, and you will not be expected to be actively engaged in patient care. When you work-up a new patient on-call or on short-call, you should staff the patient with the proper attending when the attending is physically present. You should not call an attending to staff a new patient. Patient Logs You must enter your patients into ESEL on a daily basis. If you let your patient list accumulate without entering, then it will only become more tedious and painful. If you are seeing a patient in the hospital, you can put their sticker on an index card each day, and enter these at the end of the day (be sure to properly dispose of the card). Although this may seem to be a bit of a nuisance, most of you will be doing this for the rest of your career, as attending physicians also need to turn-in billing cards. The purpose of tracking patients is to ensure you are seeing a large number of diverse patients on your clerkship. It is also important to establish your involvement in key symptoms, diagnoses, and situations in neurology. If you performed a work-up on a patient that included an H&P, such as on the Inpatient or Consult Services, please note that on ESEL. If you picked-up a patient on your first day or as a hand-off, and wrote daily progress notes on them, please indicate that. If students are in between grades, I may use the logs to see how involved you were in patient care in relation to the specific services you were on. Do not enter falsified ‘worked-up’ and ‘followed’ patients into ESEL, because if caught, I will personally guarantee that you will be very sorry. If you rounded on a patient, discussed a patient in V6.15.11 11 conference, or observed a patient in clinic, then do enter them into ESEL, but do not check that you worked-up and followed the patient. Be proactive in seeking out these diagnoses. Ask other students and residents so that you will have these all done by the end of the rotation. Please let me and your residents know if there are any problems seeing adequate patients. Textbooks Lange’s Clinical Neurology by Greenberg, Simon, and Aminoff is a general overview of neurology that is recommended for the clerkship. The chapters are well-organized, and students have generally felt well-prepared for the shelf exam. The grades have been quite high for the shelf, so the correct material is in there. Becker library has an electronic copy which can be accessed on campus, or off-campus through a proxy server. The only downside about the electronic version is the inability to highlight or take notes, which is helpful when you review in the days before the exam. Because the book is very dense, I would advise that you read and highlight/take notes over the first 2 weeks. Then, spend the last 2 weeks reviewing those highlights/notes until they are memorized. Lange book is not ‘required’. I appreciate that students learn differently, and some do not care for this book. I have reviewed a number of neurology books for clerkships, and there is no perfect book. Other books which have been useful for a general overview include Neurology PreTest (highly recommended by many), Neurology Case Files, and Neurology Blueprints. If you would like to use another book, then that would be fine. I would encourage you not to read too many books or delay your reading since the rotation is so short and you will need to master a lot of material. Maybe do Pre-Test plus one of the above paperback texts. I would highly recommend that you review the notes for the Diseases of the Nervous System from 2 nd year. This is an excellent resource, and you should be able to get through this quickly since it is already familiar. When you get your patient, you should read as much about them as possible. This will include using the computers to find good reviews and landmark clinical trials that are pertinent. Emedicine and Up To Date are excellent sources. You should also use Ovid. When presenting a patient in conference, you should be the group expert on this condition. An honors student will be able to demonstrate that they did many of these things. Pre-Printed H&P Forms The residents will use approved forms for their admission notes. You should not use these for your inpatient admission notes, because there is not enough space for you to write on them. You should use handwritten lined paper, or you can type your note on a computer. If you type your note, then you need to leave a 1 ½ inch margin on the left for the hole punch, and have room for addressograph on both front AND back. Be sure to clearly label your note, stamp it with the addressograph, add the date and time, and sign it. You SHOULD use the preprinted forms when you are in clinic or doing consults (i.e. ED, Hospital). This is because being concise and efficient are more important in these very busy settings. You may use them as a guide when talking to your patient during your inpatient work-up. Dress You are a professional, so you should look the part. I’m sorry that I have to include this, but it is important. You want patients to trust you, tell you their deepest secrets, and to take the poisons that you prescribe on a daily basis for the rest of their life. Dressing professionally is easy, patients appreciate it, and it does make a difference. Scrubs are fine when on-call and post-call, but otherwise use good judgment and prudence. You should not come to work in the same dress that you wear to go out with your friends in the evening. Men. You should wear a tie, dress shirt, dress pants, dress socks, and shoes. Clothes should be clean, should fit properly, and not be wrinkled. Everything should be buttoned and tucked. Your white coat should be washed and bleached on occasion. Sometimes a lot of bleach is required. Be careful not to spill the bleach on your other clothes, though. Women. You should dress professionally and modestly. Clothes should fit properly, and not be overly tight. One should not be able to see your backside or your belly, even if reaching for something over your head or picking-up something from the floor. Your chest should not be exposed (button to top of sternum). As a general rule, there should not be exposed flesh from the section from your neckline to your knees. Clothes should be opaque enough to not see underwear. I’m sorry I have to actually write this. Back in my day, seeing someone’s underwear was embarrassing. Phones and PDAs We are fortunate to be able to communicate and use the internet from our phones. Texting can be an effective way to keep the team together and provide updates. However, resist the urge to use your phone during rounds or conference. This is extremely rude because it suggests you are not interested. The attending does not know if you are chatting with your friend, or looking-up a medication, so again, refrain from using these devices during rounds and conferences. V6.15.11 12 Computers To log on to the computers in the 11400 conference room and in the clinics, use username: last name first initial (ie. smithj), password: 1234Abcd. Clinics When on the Adult Inpatient Service, you will go with your resident to their clinic (i.e. LL McMillan, ConnectCare, Peds). You should stay with your resident during clinic, as most clinics are not staffed with enough attendings to facilitate students seeing their own patients. When on the Consult Service, you will not go to a general neurology resident clinic. When on Peds Consults, you should attend 1 half-day clinic that week. Please keep track of your outpatient clinics. At the end of the rotation, please email Michelle a complete list with Dates, Times, Specialty, and Attendings. This would include general adult, peds, and adult subspecialty. We would like to collect this to help determine utilization. We may also use this as another source of student performance feedback, particularly when someone is very close between 2 grades. The OSCE On the final Thursday afternoon of the rotation, there will be a neuro OSCE. This is valuable practice, as the USMLE Step 2 CS will include similar, simulated patient encounters. Based upon past experience, there have been a number of Wash U students who have failed the USMLE 2 CS. You do not want to be one who fails 2CS – it is very expensive! Also, Wash U student have traditionally excelled at the clinical knowledge section (Step 2 CK), but have performed ‘average’ at the national level on Step 2 CS. You can prepare by: (1) Learning what is on USMLE Step 2 CS (http://www.usmle.org/Examinations/step2/step2cs_content.html), (2) using the clerkship OSCEs and CCX to practice, (3) taking the clerkship OSCE and CCX very seriously, (4) asking to view the video of your SP encounters. The exam will consist of 1 patient encounter of 20 minutes. You should come to the OSCE much like you would come to any clinic. You should be on time, appropriately dressed, establish rapport with the patient, and conduct yourself professionally. This exam is partly designed to test your inter-personal skills and professional demeanor. You should bring your equipment. You will be provided a clipboard and piece of paper. There will be a door note with the patient’s name, age, gender, reason for visiting the doctor, and vital signs. You may review the door note and make notes only when the exam begins. The elements needed in the medical history will be determined by the nature of the patient’s problems. Not every part of the history needs to be taken for every patient. You will not have time to do a complete examination on every patient, nor will it be necessary to do so. Pursue the relevant parts of the examination, based upon the patient’s problems and other information you obtain during the history taking. In USMLE Step 2 CS, you will have 15 minutes per patient. Here, you will have 20 minutes per patient. As a rough guideline, you might spent about 10 minutes on history, 7 minutes on the examination, and 3 minutes on discussing diagnoses/tests/advice directed at the patient. You should think about what is necessary for a general screening neurological exam ahead of time and practice this. There will be an announcement at the start of the encounter, at 5 minutes to conclusion, and at the end. At the end of the patient encounter, you will have 10 minutes to complete a patient note on the computer. This should be similar to the medical record you would compose after seeing a patient. You should record (1) your history, including the HPI, PMH, ROS, SH, and FH, (2) your physical exam, (3) up to 3 localizations, (4) up to 5 differential diagnoses in order of likelihood, and (5) up to 5 immediate plans for further diagnostic work-up and management. I would recommend that you type a narrative, just like a real H&P, because this is very familiar for you. If you try to make a list, you will probably forget something, because this is not the way you are used to doing it. The Neuro OSCE will differ from the USMLE CCS2 by (1) 20 minutes for the encounter instead of 15 minutes, (2) inclusion of localization in your note, and (3) inclusion of disease management in your note to include possible treatment, consultations or referrals. Here are some tips: 1) Be sure to knock, introduce yourself, shake hands, wash hands, etc. The interpersonal pleasantries count. You should seek to score highly on professionalism and building rapport, since this is the same regardless of the subject or situation. 2) Focus on the chief complaint listed on the door, but don’t neglect medications, risk factors, potential family history. Do not get bogged-down in ROS. V6.15.11 13 3) Keep moving along on the physical exam. Don’t take 5 minutes for sensory exam. If the patient says something is reduced or numb, take it at face value. They are not trying to trick you. The whole exam should take about 6-8 minutes, the history 10-15 minutes, 2-3 minutes for opening and closing. 4) Do a complete screening neuro exam. Just as if you are seeing a new patient in clinic. Do not dwell on cognition or language unless the history suggests the need. 5) Be sure to give a closing statement about what you think may be going on, and what you are going to do next. Closure counts. 6) Again, for the post-encounter, it is probably best to try to write a mini-H&P. You are familiar with the format, so it should flow OK. If you list out meds, SH, FH, then you will not miss anything. Do not be repetitive. 7) Write-out your exam, just as in clinic. If you don’t write it, you didn’t do it. Be specific and detailed, meaning do not write CN 2-12 intact. You should abbreviate: A+O, conversant. Vision 20/20 OU, VFFTC, Fundi nl, PERRL, EOMI, Face = with nl sensation, hearing intact, tongue/palate straight, shoulders =. Strength 5/5, nl tone, nl FFM/toe tapping. F-N and HKS nl. Sensation intact to pin and vibration, Romberg absent. Reflexes symmetric, down toes. Stance, gait, tandem, hopping nl. 8) Do not panic if the diagnosis is not obvious. Just think through the case and construct a reasonable differential. V6.15.11 14 CONFERENCES Core Clinical Conference (CCC) (All students, generally Mon or Wed 12-1:00) This curriculum reviews cases and problems in neurology, and highlights many topics from the course objectives. It is required, and please come on time. You will get more out of the conference if you look at the appropriate chapters prior to each session. The concept is for an attending to use the dry-erase board and to go through some impromptu cases to highlight important aspects about neurology which should be understood by anyone in any field of medicine. These are supposed to be clinically relevant, and to involve group discussion. I purposely wanted to avoid using PowerPoint and pre-constructed cases. I wanted spontaneity and flexibility, while sticking to some basic pre-defined teaching points. The topics for each of the 4 sessions is listed below, though not necessarily in this order. Topics: 1) Neurologic History and Exam (Clerkship Manual, Ch 11, Appendix A&B) 2) Disorders of Consciousness and Coma (Ch 1 & 10), Seizures and Syncope (Ch 8) 3) Headache and Pain (Ch 2), Motor and Sensory Deficits (Ch 5 & 6) 4) Stroke (Ch 9) Professor's Rounds (All students, Thur 7:30-8:15, 11500 Conference Room) One student will present a case, and one of the attendings will lead a discussion on the dry-erase board. This will highlight the thought process in creating a localization and differential diagnosis as parts of the history and exam are revealed. The participation of the entire group is important. Dr. Van Stavern’s Neurology Essentials Conference (All students, Tue 4:00, 2nd Floor McMillan Choi Conference Room) Please refer to the online clerkship calendar as dates and times are subject to change. Topics can include Anatomic Localization, Neuroradiology, and Emergency Neurology. Location is on Scott Ave across from Olin Hall in the Biotechnology Building at 4559 Scott Ave, Hope Center Conference Room 228 (2nd floor). Neurology Grand Rounds (All students except Neurosurgery, Fri 8:00am) This is the weekly conference for the neurology faculty, residents, and students. It often features a visiting professor or one of the faculty members. It is at 8 am Friday in the West Pavilion Amphitheater, 2 flights below the main floor on the central elevators. Food is available. It runs from September through May. Clinical Conference (All students except Neurosurgery and Peds, Tues 12:00pm) This is a weekly conference for residents and students held September through June. Topics include stroke, epilepsy, outpatient neurology management, etc. Please check with residents for the location of this conference Neuroscience Lectures (All students except Neurosurgery and Peds, Wed 12:00pm, CCC takes precedence) This is the core lecture series covering neurological topics for the residents. It runs over a 2-year course. Please check with residents for the location of this conference Dr. Landau’s Ethics Conference (All students, last Wed 4:00pm) This is held on the last Wednesday of the block at 4 pm in the 3rd floor McMillan Conference Room (307). You will receive a letter from Dr. Landau with more details. Neurosurgery Student Conference (All students, Tue 8:00am) This is for students in the 5th floor conference room on Tuesday 7 – 8. It is mandatory, and a sign-in sheet is provided. No food is allowed. V6.15.11 15 ROTATION DESCRIPTIONS AND REQUIREMENTS INPATIENT ADULT NEUROLOGY Objectives 1) See a variety of acute and serious neurological problems. This will often include strokes, hemorrhages, infections, seizures, encephalopathies, intractable neurological pain conditions, inflammatory neuropathies, and demyelinating disorders. 2) Work within a large healthcare team, including attendings, fellows, chief residents, junior residents, and Psychiatry/Rehabilitation interns. 3) Present patients concisely and thoroughly on rounds, and participate in discussion for your and other patients. 4) Communicate effectively with your patient, and help to coordinate their care for the duration of their stay. 5) Work closely with your junior resident to develop your skills, work efficiently, and hone your ability to synthesize the history and exam to result in a localization, prioritized differential, and plan for evaluation. 6) Be exposed to outpatient neurology clinics. Description Neurology has its own inpatient service in this hospital. This service is responsible for taking care of acutely ill patients with neurological problems, as well as all the other accompanying medical problems. It is a very concentrated experience, with a tremendous amount of teaching in a single location. Teams: There are two teams, Stroke and General Neurology. An attending and chief resident leads each team, with 3 junior residents on each Figure 1.Call Schedule. You will have 44 hours off, every 6 days. You must go to required team (6 total). Call will be every students conferences if you are off. You do not need to go to resident conferences if you are off. If 6th night, and the on-call team you start on your call day, work with another resident during the day (default is day 6 resident), and also take call starting at 5pm. If you are starting on a day-off, then work with another starts to take patients at 5pm, resident (default is day 3 resident). staying through the end of the next day. A junior resident will supervise 1-2 students, and sometimes an intern from Psychiatry or Rehabilitation. There are 2 Attendings on the floor at any time, one designated to stroke and another designated to general neurology. Admissions: When new patients arrive on the floor, they will be distributed by a short-call (‘shorts’) or ‘on-call’ format. Shorts are admissions distributed to the teams that are neither oncall nor post-call. The on-call resident comes to the hospital at 5 pm. New patients are either direct admits, hospital transfers, or come in through the emergency department. If they came through the emergency department, then they are may be worked-up by the Neurology Consult Resident. The attending for these patients will either be the ward attending or an individual faculty member. The ward patients will be those that will be presented post-call on rounds. Privates and faculty patients are excellent patients to work-up as well, but will not be presented on rounds. You may also get a patient handed-off from the on-call resident if the patient belongs on the opposite Stroke or General Neurology team designation. You will write full H&Ps for new patients. You will write progress notes on handed-off patients, unit transfers, and patients picked-up on the first days of starting Inpatient Adult. You may help with progress notes on other patients whose resident and/or student is off. V6.15.11 16 Pre-Round: You need to see your patient before morning rounds. If you have a conference that ends at the time for rounds, then you need to see your patients before the conference. Pre-Round includes checking with your resident regarding any cross-cover issues, seeing the patient with a pertinent history and exam, checking the computer for test results and final radiology reports (these can change when preliminary report by radiology resident is finalized by attending), review vital signs and notes from PT/OT/ST/SW, see if there are any event notes or consultant recommendations in the chart, and checking telemetry if applicable. Round Structure: Rounds are the primary time when you get to learn about patient care, observe the neurology history and physical, and interact with the rest of the team and the attendings. Thus, it is a very important time, and your 1st responsibility is to be on rounds. Unless there’s a patient emergency, you should be on rounds. Table rounds start in the 11400 conference room at 8AM on M/Tu, 8:30AM on W/Th, 9:15AM Friday if there is Grand Rounds. Table rounds will begin with post-call team and opposite team (i.e. Stroke team post-call, General Neurology Team present) to first hear about the hand-offs. If there were any patients admitted on short call, then these will next be presented to the opposite team. While this is taking place, the other team is rounding on old patients. Once all new patients have been presented to the first attending, then the other attending will hear about new patients at table rounds. During this time, the first attending will see the new patients and follow-ups. Schedule M-F (varies) Morning Rounds The following conferences are required: Monday Core Clinical Conference, Choi Conference Room, 12:00 – 1:00 (may vary) Tuesday Neurosurgery Student Conference, 7 – 8, McMillan 5th Floor Dr. Van Stavern’s Neurology Essentials, Choi Conference Room, 4 – 5pm Wednesday Dr. Landau’s Ethics Conference, 4 – 5:00, last Wednesday of the block only, McMillan 4th floor Conference Room Thursday Professor's Rounds, 7:30-8:15, Choi Conference Room Friday Neurology Grand Rounds, 8 – 9, West Pavilion Auditorium Expectations On your first day, pick-up several patients who will remain in the hospital for a couple days. Present updates about these patients on rounds and start to write progress notes. You should be working-up about 5 new patients each week. Most of these will be done independently, but there will be situations when you might work-up a patient together with your resident. When on-call, you should get at least 2 new patients. These should be the 1st 2 patients in the door. Do not wait for an ‘interesting patient’ or a ‘ward patient’. Don’t worry if you already had a patient with that complaint or diagnosis. Again, take the first ones through the door so you can take your time and be ready to take another patient when you are done. In general, you should take your time when talking with your patients and examining them. Sometimes there might be some time constraints, and your resident will let you know when you have to be most efficient. With no constraints, it might take 1 – 1.5 hours for a complicated patient. For your admission work-up, you should strive to be complete and thorough. You should pre-round on your patients each day. See each patient and do a pertinent neurological exam. If you are not sure what is pertinent, then lean more towards being complete. For example, it would not be a good use of your time to check visual acuity on all of your patients if they did not have a vision problem. Likewise, doing a detailed sensory exam each day is probably not worthwhile unless specifically indicated. But if someone came in with a stroke, you should do a detailed MS, language, CN, motor, and coordination exam because we would like to know if they worsened or if there is evidence for a stroke in a different location. A new field cut or weakness on the other side of the body would really change management in this type of patient. As part of your pre-rounds, check vitals, labs, EMTEK notes, official radiology/cardiology reports, and telemetry for those with a box. As you pre-round, get your note started. Fill in the subjective, vitals, your exam, and labs. Leave a little room in case you need to add or change your exam. If your resident gets different information from the history, or a different finding on the exam, then fix your note and put the correct information in your note. Now your note is ready for the assessment and plan, which will be determined with the rest of the team. You essentially want to have your note done as early as possible. This is because if a ‘short’ admission comes in during the morning, then you want to start on the admission right away. Also, you need to get your work done before you go to additional conferences and also clinic. No resident wants to wait around until 5 pm to review and sign your note. V6.15.11 17 After the note with plan is completed and discussed, you should review the orders for the day with your resident. This might include medications, labs, tests, and consults with therapists. You should also be helping with admission orders on new patients. When on-call, stick with your resident when you are not working-up your own patients. I would encourage you to be readily available if something is happening. This is because your resident might not call you if something significant happens and they don’t see you around. You don’t want to be obtrusive, but you also want to stay where the action is. I would define scut as menial work with no educational value that is done on a patient that you are not following. The thing about scut, though, is sometimes menial work can be educational, and by freeing up time for your resident, then they could spend more time teaching you. If you have a good resident that spends time teaching you, then help out whenever asked. You should not be calling the patient’s neurology attending to discuss the case. This is the job of your resident. For consults, there may be some circumstances where your resident would be better to call the consult rather than you. For example, if a patient needs a surgery consult, but you are unsure why this is necessary, then either your resident will need to tell you or they should make the call. In general, you should not be calling consults on patients you are not following and/or have familiarity. There are people on the floor that assist in evaluating patients and helping with their discharge. These include Physical Therapy, Occupational Therapy, Speech/Swallowing/Cognitive Therapy, and Case Coordination. You should check for their notes in the EMTEK charting system so you know about disposition. The therapists will often make recommendations about the level of rehab upon discharge. Speak with the case coordinator as soon as disposition is approaching so they could make arrangements for home and rehab needs. If you work-up a patient with a ward attending, then you should be prepared to present on team rounds. You can’t expect to do a presentation without preparing. The presentation should be very concise and pertinent, at around 3-5 minutes in total. That means you have to decide ahead of time what is important and what is not important. DO NOT READ FROM YOUR NOTE. The ROS, SH, and FH are usually not important for a focused presentation. The general medical exam should be abbreviated in your presentation (ie. ‘General exam was normal). The neurologic exam should also be abbreviated where appropriate (i.e. mental status and cranial nerves were normal). Your assessment should include localization, a prioritized differential, and a plan for investigation and treatment. You need to go over these things with your resident, read, and practice in front of a mirror or with a fellow student. You shouldn’t use notes except for meds, vitals, and labs. You should make eye contact with those on rounds. Be involved in discharging your patients. If they are going to a rehab or a nursing facility, then they need a transfer form with the medications completed. If they are going home, then they need prescriptions and follow-up appointments. Giving them an actual appointment for follow-up upon discharge is a good practice. You will follow your resident to their weekly general neurology clinic. You need to perform a neuro exam on a patient witnessed by your resident. Your resident will give you feedback afterwards, and you should hand in your feedback form so that we know it got done. It is due by 2 weeks into the rotation, but it is probably best to have it done in the 1st week. You are not graded on this exercise, so this is your chance to work out the kinks in your exam. V6.15.11 18 NEUROSURGERY Objectives 1) Become familiar with structural neurological problems, including brain tumors, spinal cord and nerve root compressions, hemorrhages, trauma, and congenital malformations with hydrocephalus. 2) Round and observe surgeries done by a wide variety of specialized academic neurosurgeons. 3) Assist in the care of neurosurgical patients on your team, and communicate their outstanding issues effectively. 4) Be exposed to outpatient neurosurgery clinic, which will handle new consults as well as post-surgical follow-up. Description Refer to the Neurological Surgery Syllabus for details. You should attend any appropriate Neurosurgery conferences during your block that do not conflict with the required Clerkship conferences. Schedule In addition to the Neurosurgery Conferences, you are required to attend the following Clerkship Conferences: Monday Meet with Dr. Limbrick at 8am on first day of clerkship in Children's Hospital, 4th Floor, Suite 4S20 (Neurosurgery) Core Clinical Conference, Choi Conference Room, 12:00 – 1:00 Tuesday Neurosurgery Student Conference, 7 – 8, McMillan 5th Floor Dr. Van Stavern’s Neurology Essentials, Choi Conference Room, 4 – 5pm Dr. Landau’s Ethics Conference followed by Course Evaluation, 4 – 5:30, last Wednesday of the block only, McMillan 4th floor Conference Room Professor's Rounds, 7:30-8:15, 10500 Conference Room 8:30am Case Discussions with Dr. Grubb on 10400 Neurology Grand Rounds, 8 – 9, West Pavilion Auditorium Wednesday Thursday Friday V6.15.11 19 NEUROLOGY HOSPITAL CONSULTS Objectives 1) See a variety of acute and serious neurological problems, including metabolic encephalopathies, iatrogenic CNS complications, CNS infections, stroke, CNS complications of cancer, headaches and pain, loss of consciousness, postcode prognostication, myopathies. 2) Work within a large team, consisting of an attending, a senior neuro resident, a junior neuro resident, and sometimes a medicine resident. 3) Present patients concisely and thoroughly to attendings on rounds, and participate in discussion for your and other patients. 4) Ensure effective communication of the neurological plan to the requesting physicians, and follow-up on the results. 5) Work closely with your senior (PGY3) and junior resident (PGY2) to develop your skills, work efficiently, and hone your ability to synthesize the history and exam to result in a prioritized differential and plan for evaluation. 6) Be exposed to outpatient neurology, through a weekly general clinic. Clinics You should go to 2 Outpatient Subspecialty Clinics each week while on consults for the 1st three weeks of the clerkship. Since the last week of the clerkship is short, you should only go to 1 clinic. Review the clinic schedule with your senior PGY3 resident and ask for some assistance in picking the clinics based upon your interest and time availability. Your resident will help direct you to some of the better clinics, and will also know when you are not available to take patients or round. Your resident may recommend doing an AM and PM clinic on the same day, or splitting the days. Once the clinics are picked, email the attending ahead of time to introduce yourself, ensure that a full clinic is planned, and to get a firm start time. Some may want you there a few minutes before the 1 st patient to make things run more smoothly. Clinics can also vary with people on vacations, on service, at meetings, etc. At the end of the block, please email Michelle a list of the clinics you attended. This should include the subspecialty clinics during consults AND general clinics during Inpatient Adult. We would like to keep track of which clinics are being utilized. We may ask some clinic attendings for comments during the evaluation process. Resident Lounge The students on consults may be included in the resident lounge on 10400 if there is patient care taking place in that location. Students not on consults should not use the lounge due to space restrictions. Knock on the door, and your resident will let you in. Description Neurology Consults are split between two teams. One team will work-up new consults in the hospital and Emergency Department during the morning (7am – 1pm), and will round with the attending in the afternoon (after 1pm). The second team will round with the attending in the morning (time decided based upon census), and will work-up new consults from the floor and ED in the afternoon (1pm – 7pm). Each consult team will be run by 3rd year neurology resident and an attending. There is usually a 2nd year neurology resident, along with some medicine residents. You should work-up at least 1-2 new patients each day. Some days will be very busy for the resident, and there might not be much time to discuss the patients before it’s time to round with the attending. Some days will be lighter, and the resident can review things with you. You will likely have ample time to independently assess your patients and do some quick reading about their problem. You may use the pre-print H&P notes for your write-up, clearly labeling it as a student note at the top and with your signature. Obviously, never mark a checkbox on the form if you did not perform that part of the exam. If rounds go past 6pm, you are expected to stay until rounds are complete. You do not need to come in during the weekend. Although there is not a designated formal teaching time, you will actually learn a lot in rounding on all the patients. You also have the potential for a lot of direct interaction with the attending. Schedule M – F 7 AM - ? Meet your resident in 11400 Conference Room. The Neurology Consult pager is 294-1326 The following conferences are required: Monday Core Clinical Conference, Choi Conference Room, 12:00 – 1:00 (may vary) Tuesday Neurosurgery Student Conference, 7 – 8, McMillan 5th Floor V6.15.11 20 Wednesday Thursday Friday Dr. Van Stavern’s Neurology Essentials, Choi Conference Room, 4 – 5pm Dr. Landau’s Ethics Conference, 4 – 5:00, last Wednesday of the block only, McMillan 4th floor Conference Room Professor's Rounds, 7:30-8:15, 10500 Conference Room Neurology Grand Rounds, 8 – 9, West Pavilion Auditorium Expectations You should have plenty of time to review the medical record, talk with the patient and examine them, and do a brief write-up. If the story is not clear when talking with the patient, then you should call additional sources. These might include their next of kin, the nursing facility that takes care of them, etc. Just be aware that you cannot give out medical information to family members without the patient’s consent, so ask the patient if it would be OK if you called to get more information. Work efficiently, and contact your resident as soon as you are done. Also be aware that we are not the primary team caring for the patient, and are usually called to answer a specific neurologic question. Most good consults are formulated in a question or a request to evaluate for a specific problem. Your resident will often give you this question when s/he assigns you a patient. Since you are a consultant, in many cases the communication about your findings and opinion will be directed to the physician requesting the consult and not the patient or their family. You also don’t want to get involved in the fine details of medical care outside that within the realm of a neurologist. As two more requirements, you need to perform a neuro exam on a patient witnessed by your resident. Your resident will give you feedback afterwards, and you should hand in your feedback form so that we know it got done. It is due by 2 weeks into the rotation, but it is probably best to have it done in the 1st week. You are not graded on this exercise, so this is your chance to work out the kinks in your exam. V6.15.11 21 PEDIATRIC NEUROLOGY CONSULTS Objectives 1) See a variety of acute and serious pediatric neurological problems. This will often include metabolic encephalopathies, developmental problems, iatrogenic CNS complications, CNS infections, stroke, CNS complications of cancer, headaches and pain, evaluating loss of consciousness and seizures, myopathies. 2) Work with a team of an attending, a pediatric neuro fellow, an adult neurology resident. 3) Present patients concisely and thoroughly to attendings on rounds, and participate in discussion for your and other patients. 4) Ensure effective communication of the neurological plan to the requesting physicians, and follow-up on the results. 5) Work closely with your attending and pediatric neurology fellow to develop your skills, work efficiently, and hone your ability to synthesize the history and exam to result in a prioritized differential and plan for evaluation. 6) Be exposed to outpatient neurology, through 2 weekly ½ day peds clinics. 7) Be comfortable performing a neurological exam on neonates, through teenagers. Description Two week consult rotation at St. Louis Children’s Hospital, covering the hospital and emergency room. You will be asked to evaluate acute neurological problems of a diverse nature. Schedule M-F (varies) Page the consult Peds resident. The pager is 823-0323. On Friday attend Neurology Grand Rounds 0800-0900 unless cancelled. The following conferences are required: Monday Peds Orientation with Dr. Larsen, 12th floor NW Tower, 7:30 – 8am Core Clinical Conference, Choi Conference Room, 12:00 – 1:00 (11:30 on 1st Day) Tuesday Neurosurgery Student Conference, 7 – 8, McMillan 5th Floor Pediatric Neurology Divisional Conference, 7:30 – 8:30am, PL26 SLCH (after Neurosurgery Student Conference) Dr. Van Stavern’s Neurology Essentials, Hope Center Conference Room; 4 – 5pm Wednesday Dr. Landau’s Ethics Conference, 4 – 5:30, last Wednesday of the block only, McMillan 4th floor Conference Room Thursday Professor's Rounds, 7:30-8:15, 10500 Conference Room If no Professor's Rounds, then Pediatric Neuroradiology Conference, 7:00-8:00 am, 3rd floor boardroom SLCH Dr. Larsen Teaching Rounds, 2nd week, 12th floor NW Tower, 8:30 – 9:30am Friday Neurology Grand Rounds, 8 – 9, West Pavilion Auditorium Dr. Larsen Teaching Rounds, 1st week, 12th floor NW Tower, noon – 1pm Expectations Meet with Dr. Larsen for orientation on the first Monday of the 2-week rotation. He is located on the 12th floor of the NW tower. Dr. Larsen will have 2 additional teaching sessions for the 2 rotating students, typically on the 1 st Friday at noon, and the 2nd Thursday from 8:30-9:30am. The time for Attending Rounds will be decided at the start of each day. You will see consults, and this will include reviewing their records, speaking with the patient and family, examining him/her, and communicating the issues to the Neuro Peds Fellow. Since this is a consult service, you need to write thorough notes which communicate the thought process and recommendations clearly to the requesting physician. Rounds will typically last until 5-6 pm. When they occasionally run past 6pm, you are expected to stay until they are complete. You should attend one half-day clinic each week. You will discuss and make your clinic selections for the two weeks during the orientation with Dr. Larsen so that the appropriate attendings can be contacted in order to plan on your attendance in clinic. Do let your Peds Fellow know which clinics you attend so they can plan to distribute new consults appropriately. Refer to Peds Clinic Schedule for cancelations and start times. V6.15.11 22 WEEKLY GENERAL NEUROLOGY CLINICS BARNES CLINIC This is a weekly continuity clinic for the residents located in the basement of McMillan Hospital. It starts at 1:00 and is on Monday, Tuesday, Thursday, and Friday. Both new and follow-up patients are scheduled with the residents. You should stay with your resident during the clinic. CONNECTCARE CLINIC This is a weekly continuity clinic for residents located on Delmar, just east of De Baliviere Ave. It starts at 1:00, and is on Monday and Friday. You should either shadow the attending if he/she is seeing patients, or shadow your resident. V6.15.11 23 SURVIVAL GUIDE for the NEUROLOGY CLERKSHIP Rob Naismith, M.D. The Neurological History The history is the most important part of your work-up. More so in any other field of medicine, the history is instrumental in making the diagnosis in neurology. This is because most diseases in neurology do not have a diagnostic test. The exam is very helpful, but rarely specific. Without a good history, it is usually impossible to come to the correct answer. Some say if you do not have a differential diagnosis by the end of the history, then you should take the history again. The history is also how we learn about disease and how it affects people. Reading a textbook can never replace personally hearing the story and examining 2 or 20 or even 100s of people with a certain disease. This is among the most important aspect of your medical education. View each experience as a chance to learn more about a disease process, and to make personal observations that will be memorable. A proper history will take some time. It should take you at least 20 minutes, and might take up to 40 minutes. You should always sit-down when speaking to patients, and ensure their comfort and privacy. Ask open-ended questions and redirect when they go off on a tangent. Ask clarifying questions where appropriate. Every time you say something, you are essentially interrupting the patient. Asking direct questions may save some time and may be necessary when the patient has difficulty staying organized, but then the patient will not elaborate on the details and will need to interpret your terminology. Since we cannot ask every question, and since there might be confusion about what ‘fatigue’, or ‘dizziness’, or ‘weakness’ means, it’s best for them to describe to you what exactly is happening. If you are unclear what they are describing, ask them to talk more about the circumstances under which it happens and what they notice as it is happening. How you ask something is also crucial. Open-questions are the best way to assure that you are getting the patients experience. Make sure the question is non-leading (ie. You didn’t have any dizziness, did you?) You should use pointed remarks that will keep the patient on tract (ie. You said that you felt dizzy, please tell me more about what that was like). Even the directed questions should be framed in a non-leading way. Sometimes we have to provide a choice to make sure we know what the patient means, but this shouldn’t happen too often. Also be aware that people have different definitions for medical terminology (ie. Did you have vertigo or just dizziness? vs. Did it feel like the room was moving or spinning, much like on an amusement park ride, or did you feel woozy or light-headed, like you just heard some really bad news or felt faint). You should seek additional informants when indicated. These might include family, the nurse at the nursing facility, the manager at Walmart who witnessed the seizure, etc. Patients with impaired consciousness or attention, those with seizures, and those with dementia always need an additional informant. Elicit a chief complaint by asking them what is currently troubling them the most. You might be surprised what people will tell you here, but it’s their chance to state what is most important to them. Now your job is to recreate a chronological line of all their symptoms starting from the very beginning. If someone has had MS for 10 years, and they are coming in with an exacerbation over the past 2 weeks, then their history really begins 10 years ago. Delve into each symptom to obtain all the details. These include things such as the ‘PQRST’ questions – provocative factors, quality, relieving factors, severity, and time line. Include historical details when informative, such as what they were doing at the time. You want to ask how things resolved. If they fell, were they able to get up by themselves, did they have to lay there for 2 hours until someone came in, or did they have to crawl over to the phone to call someone. Quantify whenever possible – how many times did they fall last year, how many times did they fall this year. Include hard measures of disability – 3 years ago they started using a walker, last year they started to use a wheelchair, this year they cannot transfer out of the wheelchair without assistance. Inquire on how the symptoms have led to changes in work, relationships, taking care of the home, and in hobbies and travel. We are a little bit interested in treatments prescribed and their perceived benefit. We are less interested in testing or doctors opinions about the diagnosis. We want to take a fresh and independent approach to the patient’s complaints. Do not assume the diagnosis for which they are coming to see you is the correct one. Perhaps the diagnosis was made years ago, but new symptoms suggest a different disorder. Perhaps the doctor who initially diagnosed them did so in haste. You also need to have a sense of the patients social and support structure. If someone is a single mother of 3, doesn’t have a high school education, is 3 months behind on paying her utilities, and is not on good terms with her family, then this is important. If someone lives on the 5th floor of an apartment without an elevator, then this is important. Lastly, a good history will provide clues as to what you will find when you examine them. If they are complaining of stiffness and weakness in the legs, then you would expect brisk reflexes and weakness. If they are complaining of numbness of the hand, ask them whether it is the whole hand or just part of it. If they are having double vision, ask if it is worse looking in a certain direction, and how are the 2 objects oriented. Being able to make a ‘telephone diagnosis’ takes some skill in asking the right questions that will allow the patient to accurately report what you will find objectively. V6.15.11 24 At the end of the history, you should have a clear picture of their symptoms and how they have unfolded over time. You should also have some hypotheses about what you will find on exam and a start to your differential. You should also have some inside knowledge about who is this person, how has their disease affected them, and what is their social support and living situation. The Neurological Exam One of the great things about neurology is the physical findings and their tremendous usefulness for localizing and deciding about the diagnosis. Almost everyone with a neurological disease (except seizures and headaches) will have some abnormalities on their exam. Some of these are quite striking, and some can be very subtle. You cannot learn these in a book or a single lecture, so we learn this by seeing patients together with those who are more experienced. When you round with attendings, they will point out the subtle findings. Watch carefully how your attending does the exam, because everything has a purpose. You should do a complete neuro exam on all your patients, at least for the initial work-up. The chief or the attending might do a more focused exam, but that’s not the goal for you at this time. You need to have a firm grasp of what is normal and what is abnormal, and that takes much practice. Mental status can be a large or a short part of the exam. On every patient, you should specifically check orientation (person, place, time, situation), recall, short-term memory, attention, calculations, and long-term memory. You should take the persons educational level into context here. These can be expanded upon depending on the story and other findings. Language consists of 6 components. These include comprehension, fluency, naming, repetition, reading, and writing. Cranial nerves should include visual acuity and funduscopic exam. You need to be able to readily see the optic nerve before the end of the rotation. For the motor exam, you need to be able to pick-up subtle weakness. This would include having people do fine finger movements, toe tapping, walking on heels and toes, and hopping on each foot if safe to do so. When you check power, be sure that you have the mechanical advantage so that you will know if they have mild weakness. Remember that for reflexes, you are trying to detect subtle differences, not just whether they are present or absent. When you perform the exam, it is much like an experiment where you are hypothesis testing. After you obtain the history, go wash your hands and use that time to create your hypotheses. Think about the localization(s), and the possible diagnoses on your differential. Do not bias the exam too much by leading the patient. You can conduct it as an objective experiment, and be convinced that the abnormality is really there. If you are not sure, repeat the test until you are convinced. Do more detailed testing when indicated by the history. For example, it may take 15 seconds to elicit the reflexes if they have no symptoms referable to that system, or it may take 2-3 minutes if you are really trying to discern a difference. Write-Ups Your write-ups on neurology should be clear and concise. There is no reason to write a textbook summary as your assessment. The history should be very detailed and lengthy. This is because it is the most important part of your work-up. If the history is 1-2 short paragraphs, then this is not enough. The social history should give an indication of the person’s living situation and social support. Even though alcohol, drug abuse, and tobacco use are really medical problems, they have been traditionally included under social history. The real social history will include educational level, job position with specific details, living situation, financial situation, important hobbies, etc. Your assessment should contain a brief, 1-2 sentence statement which summarizes the entire work-up. Write this statement as if no one will read your write-up except the assessment. For example, “This is a 67 y/o man with cardiac disease who presents with sudden onset of slurred speech and left-sided weakness, and is found to have a left hemiparesis and neglect on exam. CT showed evidence of previous strokes, but nothing identified as acute”. The next part of your assessment should include localization. Be only as specific as you can. For example, if there is left hemiparesis alone, then you could only say that it could be in the right hemisphere or brainstem. If someone has left hemiparesis densely involving arm and leg with a dense field cut and gaze deviation and a global aphasia, then you know that there is a stroke in the entire MCA territory on the right. The next part of your assessment discusses the differential diagnosis. You should prioritize your differential, and not just make it into a long laundry list. What are the most possible diagnoses that are pertinent to this person’s story? That is, you need to integrate the whole story, and demonstrate that you understand what is going on here. Always include things that are common, treatable, and/or dangerous. Have a brief discussion as to why something is higher in the differential than another, or why it is less likely. This will include reviewing the diagnoses in a textbook and the medical literature. Review papers are a good place to start. V6.15.11 25 In constructing differentials, it is good to have a framework in working-through the different categories of disease. The following mnemonic is good to use: D – Degenerative and hereditary V – Vascular (infarct, ischemia, hemorrhage) I – Infectious (immunocompetent, immunocompromised, bacterial, viral, fungal, parasitic) C – Cancer (mass effect, paraneoplastic) T – Trauma and surgical I – Immunologic (autoimmune, allergic) M - Metabolic (nutritional deficiency or excess, organ dysfunction, electrolyte disturbance) Finally, put your plan and the reason for doing these things. For example, obtain MRI to see if there is evidence of acute infarcts in both hemispheres, consult PT to assist in gait training, obtain cardiac echo to evaluate for thrombus or valvular abnormality. Don’t put in plans for neurological emergencies if you aren’t going to do them. For example, don’t write to consider an LP if bacterial meningitis is a possibility, or consider EEG if non-convulsive status is a possibility. If you thought these were possibilities, you probably would have done the test before doing the write-up. Presentations Your job for a presentation is to clearly and concisely reconstruct the timeline from the beginning, giving details about their symptoms as you go along. There are 2 types of presentations. The first is the 3-5 minutes variety, and the second is the full-blown conference variety. You should be able to do either presentation without reading from your notes. You could have a list of the medicines with doses, the vitals, and the labs, but reading the history is bad. You need to be able to look people in the eye and grab their attention. Remember, everyone is going to be tired and thinking about the other 10 things they need to do at the moment. If you give a boring presentation, then no one will pay attention. I would always try to put the story in the proper context when relevant, even for the 3-5 minute presentation. For example, if someone went to the county fair and rode the roller coaster, and an hour later developed vertigo, slurred speech, and inability to walk, then this gives us the context in which a vertebral dissection might have occurred. It also makes the story unique and memorable. If someone developed a headache while having sex, then this might be relevant for subarachnoid hemorrhage. If someone was in church singing in the choir and they passed out, then this is relevant. If you were to just list the symptoms without the context, then it is more boring and the patients start to sound the same. The 3-5 minute presentation will be what is used during Team Rounds. This is a bare-bones presentation, but it is very dense with relevant material. It is really the ‘tip of the iceberg’ in terms of what you know about the patient. You cannot tell us everything, so you have to decide on what you do tell us. It consists of a chief complaint and the history. You should state pertinent positives and negatives along the way depending upon the differential diagnosis. There is no review of systems in the 3 minute presentation. If the family history is not relevant, then don’t even both to mention it. If the social history is relevant, then include it in the history. If a past medical problem is relevant, then include it in the identifying information For example, “This is a 67 y/o RH white man who presents with acute onset of slurred speech. His history is significant for atrial fibrillation, congestive heart failure, coronary artery disease, and a previous stroke in 2005 with residual mild left hemiparesis.” We do not care whether they had their gallbladder or tonsils out, or if they have seasonal allergies unless it is relevant. We do not care if they take Prilosec unless it is relevant. Bottom line is that the attending should have a very clear picture of what is going on with this person within a few moments. There are no guessing games or cards to be kept up ones sleeves. Just go ahead and say it like it is. When presenting to the attending on rounds, put the chief complaint up front and in medical terms. Do not use the patients words unless they are particularly relevant or insightful. Consider the following example, “Mr. Jones is a 72 y/o RH black man with CAD, HTN, hypercholesterolemia, GERD, and arthritis who presents because his daughter insisted he come to the hospital.” You are now 15 seconds in the presentation and the attending has no clue. By giving the medical complaint up front, the attending can start to organize your presentation. Now consider the opening statement in the paragraph above. Right from the start, the attending knows the complaint (slurred speech), along with age and gender. Is it ALS? Is it a Bell’s palsy? Is it a stroke? These are going through the attending’s mind. Next s/he hears a list of cardiovascular risk factors, and immediately stroke goes to the top of all considerations. That is how the brief presentation should work. You should present the details, almost anticipating what needs to be heard at that given time. The exam should be abbreviated to convey what is important. Also, remember to stay organized: 1) mental status, 2) language, 3) cranial nerves, 4) motor, 5) reflexes, 6) sensory, 7) coordination and gait. We are all going on the assumption that you did a complete general and neurological exam. It would be fine to list out the vitals and then say that the general medical exam is unremarkable if that is what you found. For a stroke, you might say mental status and language are intact. Cranial nerves are relevant for left lower facial droop and dysarthria, but no field cut. Motor is relevant for a left hemiparesis 3-4/5 in severity affecting the arm greater than the leg. Reflexes are brisk on the left with an upgoing toe. Coordination on the left was appropriate for that degree of weakness. He had diminished sensation on the V6.15.11 26 left, but was able to reliably perceive touch. He had both visual and sensory neglect. He needed assistance to walk due to the hemiparesis. You generally don’t want to get bogged down in listing out all the cranial nerves, all the numbers for the muscle testing, and all the numbers for reflexes. You want to include pertinent negatives here based on your differential. This is how your attending will know you are smart. If bacterial endocarditis is on the differential, then you should specifically state in the general exam that there were no conjunctival or extremity lesions and no murmur. Because the presentation is brief, you shouldn’t have to give a summary statement of what you just said. You should give a statement about the localization, and then the differential diagnosis. The differential should be ranked to include things that are common, things that are treatable, and things that are dangerous. Next you can state your plan for evaluating the differential and for helping the patient get better. You will need to prepare for the 3-5 minute presentation. Don’t think you could do it otherwise. It takes practice to condense 1-2 hours of your work-up into 5 minutes. The attending realizes you spent a lot of time with your patient, but doesn’t want to hear every last detail. You will show the attending how smart you are by how well you are able to do this. Losing focus and going on a tangent with your presentation will not impress. Some of your grade will come from this interaction. Rehearse out loud in your call room, or find another student to help practice. The conference presentation is quite different, and is not often used on neurology. This is typically done sitting at the table with the attending and all the students. It is primarily a forum for discussion and teaching. Here, there is sometimes a sense of drama, because we want to have a good discussion based on the symptoms. Again, you shouldn’t read off your note, but the presentation will be constructed much like your note. You want to give a chief complaint and the history. Here, the chief complaint would probably be best in the patient’s words for the sake of discussion. The attending might ask you to stop along the way so that there can be some discussion. You should give the complete PMH and Meds. You should include the social history and family history. Give the neuro exam in detail, by listing out the specifics. You also need to prepare for this, but not in the same way as the 3-5 minute presentation. This is because your classmates will be asked to contribute to the discussion and to help ask the relevant questions. You need to be sure that you have all the answers. You also need to be an expert in this person’s diagnosis. This would include reviewing the relevant literature and evidence. Lastly, don’t forget that your attending will like to hear the neuro exam in order. This is 1) Mental status, 2) Language, 3) Cranial nerves, 4) Motor, 5) Reflexes, 6) Sensory, 7) Coordination & gait. V6.15.11 27 SUPPLEMENTARY MATERIAL Neurological Diagnosis Allyson R. Zazulia, M.D. I’m sure you’ve heard the stereotype that sure, the brain is fascinating, but all neurologists do is "mental masturbation," spending their time in the useless intellectual exercise of pinpointing which nucleus or tract or other structure is involved in a patient’s illness when we all know that it doesn’t matter anyway because there are virtually no treatments for neurological disease. My job today is not to try to convince you that there is no greater specialty than neurology or to dispel the belief that we have nothing to offer patients with neurological disease. Rather, I am going to focus on the process of neuroanatomical localization, why it is unique, and how it is central to neurological diagnosis. Understanding neurological pathophysiology is important not only for neurologists and neurosurgeons: Many neurological disorders are commonplace in general medical practice or other specialty. Patients with headache, stroke, or carpal tunnel syndrome are often managed without a neurological specialist ever being consulted. A number of neurological diseases are caused by or worsened by general medical disorders or occur as complications in patients hospitalized for other reasons. Similarly, neurological disturbances may occur as part of or may even be the first sign of a systemic medical condition. How do you make a neurological diagnosis? In many ways the strategy is the same as making any diagnosis in medicine. First, you locate the patient’s symptoms and signs anatomically. Second, you interpret temporal features in terms of pathophysiological principles. Third, you use the results of these two exercises to formulate an etiological hypothesis. Localization Simply defined, localization means "where," i.e., where within the nervous system is the lesion responsible for a patient’s symptoms and signs. (Understand that "lesion" does not necessarily imply a visible structural defect rather, it is used synonymously with "dysfunction.") Thus, localization requires a thorough understanding of the anatomy and physiology of the nervous system, its blood supply, and the disease processes that affect it. The process of localization begins during history taking, is refined during the general and neurological examinations, and is re-assessed after any relevant diagnostic studies are completed. Although sophisticated neuroimaging and laboratory studies are in continuous development, technology cannot replace the clinician’s anatomical localization based on history and examination. Lesions may go undetected on standard imaging studies unless the studies are specifically focused on the anatomical region hypothesized to be involved. Similarly, neuroimaging or laboratory studies may disclose incidental abnormalities that have no bearing on the patient’s symptoms and the further pursuit of which can lead to unnecessary time, expense, and potentially even patient harm. Take the case of a patient with back pain and difficulty walking. In the absence of a thorough H & P and lesion localization, an MRI of the lumbar spine is obtained, showing a left L5 disc herniation. The patient is sent to an orthopedist and undergoes discectomy. At best, his symptoms do not improve with surgery or continue to progress. At worst, he develops a serious post-operative complication. Here’s the way it should have worked: Further history reveals that the pain was not radicular (as would occur with a disc); walking was difficult because his legs felt stiff and he couldn’t feel the ground with his feet, and he had been having urinary urgency and incontinence as well as impotence for the past 6 months. Based on these symptoms, your hypothesis at this point is that he has a spinal cord lesion. Since you know that the spinal cord ends at L2, you know that there is no role for imaging of the lumbar spine. Examination reveals tenderness over the lower thoracic spine, full strength, bilateral lower extremity spasticity and hyperreflexia with extensor plantar responses (upgoing toes), and sensory loss below T9. You can now further refine your localization to the thoracic spinal cord and order the appropriate imaging study, which shows an extradural mass at T7 compressing the spinal cord. The moral of the story is not that you don’t need an imaging studyit’s that your clinical skills and your knowledge of neuroanatomy are essential to guiding appropriate diagnostic evaluation and to determining the significance of any abnormalities detected in that evaluation. Localization involves two separate steps: (1) type localization and (2) topographical localization. Type localization identifies the type of dysfunction present within the nervous system. There are five possibilities: focal, multifocal, diffuse, specific system, and combination. 1. A focal lesion is one in which a single, discrete neuroanatomical locus can account for all the patient’s symptoms and signs. Examples include (a) a left cerebral hemispheric infarction in a patient with sudden onset right hemiplegia and aphasia; (b) a pituitary tumor in a patient with papilledema and subacute onset amenhorrhea and bitemporal hemianopia; and (c) a right median neuropathy in a patient with weakness of the right abductor pollicis brevis and numbness of the first 3½ digits on the right hand. 2. A multifocal process involves more than one locus, but the loci remain discrete. Modification of the previous examples that would indicate multifocal localization include (a) multiple cardiac-origin emboli in a patient with a V6.15.11 28 new systolic heart murmur and sudden onset right hemiplegia and aphasia (left cerebral hemisphere) and left superior quadrant visual field cut (right posterior temporal hemisphere); (b) metastases in a smoker with chronic cough, papilledema, and subacute onset left arm and leg dysmetria (left cerebellar hemisphere) and left homonymous hemianopia (right optic tract); and (c) mononeuritis multiplex (neuropathy involving multiple discrete nerves) in a patient with weakness of the right abductor pollicis brevis and numbness of the first 3 ½ digits on the right hand (right median nerve), tingling in the fifth digit and the ulnar half of the fourth digit on the left hand and weakness of the left first dorsal interosseus (left ulnar nerve), and numbness of the left lateral leg and dorsal foot and weakness of left ankle dorsiflexion and eversion (left superficial peroneal nerve). 3. Diffuse localization indicates widespread dysfunction of a part of the nervous system. Examples include (a) encephalopathy due to a variety of metabolic or toxic causes; (b) dementia; and (c) numbness and pain in a stocking and glove distribution due to diabetic small fiber peripheral neuropathy. Note that in both a multifocal and a diffuse process, there is involvement of more than one discrete physical location. But in multifocal, the lesions remain discrete, whereas in diffuse, the dysfunction is generalized. In the case of neuropathy, for example, a multifocal process will be evident by signs and symptoms in the distribution of multiple specific nerves (e.g., median, ulnar, and femoral), as discussed in the example of mononeuritis multiplex above. Some nerves are involved and some aren't. In axonal neuropathy (a form of diffuse nerve disease), on the other hand, the distal-most portions of all axons are involved, resulting in stocking and glove distribution sensory and motor loss. a. Specific system localization is a subset of diffuse localization. In specific system processes, there is diffuse dysfunction of a particular pathway or neurotransmitter system. The progressive diffuse weakness, atrophy, fasciculation, and spasticity in amyotrophic lateral sclerosis (Lou Gehrig's disease) occur because of loss of the anterior horn cells and degeneration of the corticospinal tracts. The progressive loss of vibration and proprioception in vitamin B12 deficiency is a manifestation of posterior column dysfunction. The delirium, mydriasis, hypertension, dry mouth, urinary retention, and constipation of atropine overdose reflect blockade of muscarinic cholinergic receptors. V6.15.11 29 Topographical localization involves determining the anatomical level within the nervous system that accounts for all the patient’s findings. Often, it is best to start from the periphery and work centrally, considering each of the possible sites listed in the table below. The middle column lists the terms commonly used to describe the disease processes affecting these areas and the right column lists the symptoms and signs typical of lesions at these sites. Typical symptoms/signs Site Dysfunction Peripheral Proximal weakness (motor only) Muscle Myopathy Fatigable weakness (motor only) Neuromuscular junction Pain; motor, sensory, and reflex loss in Peripheral nerve Neuropathy specific nerve distribution, OR distal symmetric sensory loss and/or weakness Mixed nerve and root distribution Plexus (brachial or lumbosacral) Plexopathy Radicular pain; motor, sensory and reflex Spinal nerve root Radiculopathy loss in specific root distribution Nerve cell body LMN weakness and reflex loss Anterior horn cell "LMN disease" Dorsal root ganglion Sensory neuronopathy Sensory loss and reflex loss Spinal cord LMN weakness at level of lesion; UMN Myelopathy below level of lesion; sensory level; dissociated sensory loss; neurogenic bladder Posterior fossa Cranial nerve deficits; impaired LOC; Brainstem crossed or bilateral motor or sensory deficits Ataxia; tremor; nystagmus Cerebellum Supratentorial LOC or memory disturbance; Thalamus hemisensory loss and/or pain; hemiataxia; neglect or aphasia Chorea; athetosis; dystonia; tremor; Basal ganglia rigidity Hemiplegia (UMN) and/or hemisensory Cerebral cortex Encephalopathy loss; aphasia; neglect; hemianopia; dementia; seizure Other Headache, altered LOC, cranial nerve Subarachnoid space/meninges deficits LMN=lower motor neuron: weakness, atrophy, reflex loss, fasciculations. UMN=upper motor neuron: weakness, spasticity, hyperreflexia, extensor plantar response. LOC=level of consciousness. This is where your knowledge of neuroanatomical pathways and the signs and symptoms that go along with damage to these pathways comes in. Since the nervous system is a continuum, a particular symptom may represent a lesion at multiple levels. Thus, a complaint of weakness may represent dysfunction at the level of the muscle, neuromuscular junction, peripheral nerve, plexus, spinal nerve root, lateral column of the spinal cord, pyramidal tract in the brainstem, internal capsule, or cerebral motor cortex. It is the pattern of weakness (e.g., proximal vs. distal, unilateral vs. bilateral, face vs. limbs), associated symptoms (e.g., numbness, visual disturbance, language dysfunction), and examination findings (e.g., atrophy, fasciculations, and hyporeflexia or spasticity and hyperreflexia) that allow you to narrow down the possibilities. So, for example, weakness, numbness, and reflex loss within the distribution of a particular spinal nerve root implies a radiculopathy, whereas weakness of the face, arm, and leg all on the same side of the body implies a lesion within the motor pathways above the level of the facial nucleus in the mid-pons. During the process of localization, ask yourself three questions: 1. What is the necessary minimal amount of neuroanatomy that must be damaged in order to produce the patient’s symptoms/signs? A patient with monocular blindness must have a lesion on the same side somewhere between the cornea and optic chiasm. A patient with an absent tendon reflex must have a lesion within the afferentefferent arc serving that reflex. A patient with aphasia must have a lesion of the dominant (95% left) cerebral hemisphere. V6.15.11 30 2. If the lesion is here, does it explain all the findings? If the answer is no, you should carefully re-examine the data and your conclusions. Either the localization is wrong or the disease process is multi-focal or diffuse. 3. If the lesion is here, what else should be present? That’s another way of saying, does the patient have the expected neighborhood signs to go along with your proposed localization? Let’s take the complaint of unilateral facial weakness. With this small amount of information (face and unilateral), we can already narrow down the possible sites of involvement to peripheral nerve (cranial nerve VII) within subarachnoid space or temporal bone, brainstem (pontine lesion affecting the VII nerve nucleus or fascicles), or supranuclear motor pathways supplying the face (e.g., genu of internal capsule or lateral motor cortex). But we obviously need to do better than this before beginning to address what the patient has. The first question should be what is the pattern of weakness? If the patient has lower facial weakness (drooping at the corner of the mouth or inability to raise the corner of the mouth when smiling) with relative sparing of the upper face, this is consistent with an upper motor neuron lesion (a.k.a. supranuclear or above the level of the facial nucleus in the pons). If instead the patient has weakness that involves the entire half of the face equally (facial droop as well as inability to close the eye), this is consistent with a lower motor neuron lesion (at the level of the VII nerve or the VII nerve nucleus in the pons). Our patient complains of both facial droop and inability to close the eye. So now we need to differentiate between a pontine lesion and a peripheral nerve lesion. What neighborhood signs would you expect with a lesion of the facial nucleus or intrapontine nerve fibers? If you remember your brainstem anatomy (or pull out a diagram of the pons, see Figure 1), you’ll recall that the facial nerve fibers course around the abducens nucleus and that the abducens nerve fibers course just medial to the facial nucleus as they exit the pons. The parapontine reticular formation lies just ventromedial to the abducens nucleus. So an associated ipsilateral lateral rectus palsy or conjugate gaze palsy would localize the lesion to the pons. Since the facial nerve fibers pass between bundles of corticospinal tract fibers, an associated contralateral hemiparesis would also localize the lesion to the pons. What if instead of associated diplopia or contralateral arm and leg weakness, the patient complains of hearing loss and tinnitus? This suggests involvement of the auditory nerve. The two places that the facial nerve is in close proximity to the auditory nerve are within the cerebellopontine angle (Figure 2) and within the temporal bone. If we wanted to, we could localize a VII nerve lesion even more precisely in terms of where the lesion is in relation to the departure of the nerve to the stapedius muscle, the chorda tympani, and the greater superficial petrosal nerve (based on the presence or absence of hypersensitivity to sound, loss of taste, and impaired lacrimation, respectively). Why bother doing this? It is not a simple exercise in mental masturbation; rather it is an exercise that allows us to begin to address etiology. The pathophysiological processes underlying an intrinsic pontine lesion (e.g., vascular or demyelinating disease) differ from those underlying a cerebellopontine angle lesion (e.g., tumor), which differ from those underlying a peripheral facial nerve lesion (e.g., trauma, infection, or idiopathic). Figure 1. Axial section through pons at level of facial nucleus. V6.15.11 31 Figure 2. CN VII and CN VIII at cerebellopontine angle. Pathophysiology In neurology, a patient's dysfunction is not only the expression of where the disease occurs, i.e., a consideration of which cross-section of circuits is down, but also a reflection of the particular disease process causing the disability. A neoplasm, an infarct, and demyelination in the right frontal lobe will all cause left-sided weakness, but at different rates (time-intensity profile) and with different individual features (headache, seizures, papilledema, episodic waxing and waning, aggravation by heat, etc.). Time-intensity Profile So the next step in neurological diagnosis is to interpret temporal features of the patient’s symptoms in terms of pathophysiological principles. You need to know what the very first symptom was. Patients often pick the most dramatic events and play down earlier subtle details. Don't let them. Ask for earlier, perhaps less obvious symptoms of the same thing. Warning signs. Ask if they were absolutely 100% normal before this started. "Oh yeah, come to think of it, I did have an episode of dizziness and vomiting a month ago. It must have been something I ate." Maybe, but perhaps more likely is that it was the first episode of a recurring pathophysiological process at the same anatomical site. This piece of history is crucial. You must dig for it. On the other hand, don’t be fooled when patients draw connections that aren’t true, e.g., "It all happened after I slipped in the Wal-Mart parking lot . . ." Just take all the information in and draw your own conclusions at the end. Over what period of time did the symptoms develop? Seconds, minutes, hours, days? What happened next? Many clues about etiology become clear from constructing a time-intensity profile because this teaches us about disease processes through anatomy. 1. Acute: minutes to hours. This implies acute metabolic dysfunction as occurs with ischemia, seizure, trauma, etc. 2. Subacute: days to weeks. May be smooth, stair-step, or crescendo. This suggests an expanding lesion, as occurs with tumors, abscess, etc. 3. Recurrent-remittent: episodic attacks of symptoms with rapid recovery to normal health. This implies repeating episodes of a single process as occurs with transient ischemic attacks (TIA), seizures, migraine, and multiple sclerosis. In the case of seizures, migraine, and often TIAs, the symptoms are highly stereotypical. In the case of multiple sclerosis, symptoms vary depending on the lesion site, and the process may evolve to a secondarily progressive one in which there is only partial recovery from each attack. 4. Chronic-progressive: months to years. This implies gradual deterioration as occurs with degenerative diseases like Alzheimer's dementia, Huntington's chorea, etc. Symptom types can also provide a clue as to pathophysiology: 1. Negative symptoms. Reduction (weakness, numbness) or complete loss (paralysis, analgesia) of function. Implies at least partial or complete failure of impulse conduction in a functional system. This can be reversible (e.g., TIA) or irreversible (e.g., infarction). V6.15.11 32 2. Positive symptoms. Exaggeration of a physiological phenomenon. These can be brief and very intenseparoxysmal (as in epileptic seizures) or episodic and recurrent (as in hemifacial spasm or trigeminal neuralgia). These examples imply abnormal excessive discharges in gray matter or ephaptic excitation in a fiber pathway and are considered "irritative." Positive symptoms can also be slow and continuous: chorea, dystonia, nystagmus, tremor. Here positive symptoms imply chronic imbalance in complex integrated motor pathways, perhaps reflecting the effect of degeneration or removal of one component part. 3. Secondary symptoms. Symptoms referable to "mass effect." A lesion (e.g., tumor, infarct) causes primary symptoms by local destruction and secondary symptoms as the lesion "grows" through development of edema, pressure on adjacent brain (new, more severe symptoms), herniation (stupor, coma, midbrain signs), blockage of CSF pathways (papilledema, stupor), and stretching of vessels and meninges (headache, stiff neck). 4. Behavioral symptoms. Complex changes in personality and behavior. Occasionally these can be described as dementia, depression, or temporal lobe seizures. Although complex, disorders of perception (neglect and denial), motor behavior (apraxia), language (mutism, aphasia) or mood can usually be approached by the same stepwise method used for any neurological dysfunction. In these cases, however, it is imperative to interview relatives, neighbors, or other independent observers to obtain the historical data. But the process is the same: symptom analysis, anatomy, pathophysiology. Etiology Determination of etiology is the last step in neurological diagnosis, occurring after lesion localization and consideration of pathophysiology. Once the patient’s symptoms, illness time course, demographic factors (age, sex, occasionally ethnicity), risk factors, and other medical conditions are put together with the exam findings and predicted anatomical localization, you will discover that the etiological possibilities are reduced to just a few. If this step-by-step diagnostic method is not followed, on the other hand, you will be left with a long list of remote etiologies. Categories of etiology in neurological disease are similar to those of non-neurological disease genetic, congenital, infectious, immune, endocrine, metabolic, toxic, traumatic, vascular, mechanical, neoplastic, degenerative, psychological except for the addition of demyelination, epilepsy, and migraine in neurological disease. Presentation of the Patient with Neurological Disease Going through the above process of localization will be essential to you as a third year student on Neurology and as a physician who encounters any patient with neurological complaints. The neurological H&P is structured to reflect this by expanding on the Assessment section that is common to all other areas of medicine. Whenever you present or write up an H&P on a patient with neurological disease, your history and exam should always be followed by a paragraph consisting of (1) a brief summary of the patient's history and exam findings, (2) a statement about anatomical localization, (3) the diagnosis, and finally (4) the management plan. The brief summary of history and exam serves two purposes: to distill all the information you have collected on the patient into the essential facts and to review the highlights of your presentation for any listener whose mind may have been wandering. It should include the patient's age, gender, any relevant past medical history, symptoms (including a time course for them), and exam findings. This is the time you should use words such as "rapidly progressive" or "in a stepwise fashion over the past 6 months" to describe the time-intensity profile and the time you can use medical terminology to interpret the patient's symptoms and exam findings. An example: You report that your 64-year-old female patient with a history of asthma, hypertension, diabetes, renal insufficiency, and tubal ligation complains of waking up this morning with blurred vision and seeing two of everything except when she looks to the left. You report on the exam that the patient has limitation of abduction of the right eye, an increase in the separation of the two images when looking to the right, vibratory loss at the great toe bilaterally, and retinopathy. Your summary statement would be something like, "This 64-year-old woman with a history of hypertension and diabetes had the acute onset of horizontal diplopia upon awakening this morning and on exam has a right sixth nerve palsy." I include hypertension and diabetes because these are causes of sixth nerve palsies and are thus relevant to the problem. I leave out the medical conditions (asthma, renal insufficiency, tubal ligation) and exam findings (mild vibratory loss in the toes and retinopathy) that likely have no direct link to the problem. The anatomic localization is a single sentence defining the structures and pathways involved and where the lesion must be to explain them. In our example, you might say, "This localizes to the right sixth nerve anywhere along its course [including the subarachnoid space, cavernous sinus, superior orbital fissure, and orbit] or to the right sixth nerve nucleus in the pons." If there are multiple findings, your localization would be the unifying localization for all of them. The diagnosis statement should clearly indicate the diagnosis you believe to be most likely and include a short list of other important possible diagnoses and a short explanation for why you believe them to be less likely. "The most likely V6.15.11 33 diagnosis in this hypertensive and diabetic patient is vasculopathic sixth nerve palsy. A small right pontine ischemic stroke could also be responsible, but this is less likely given the lack of associated neighborhood signs." Note that while you should consider every condition in the differential diagnosis (and may be questioned on them in rounds), you do not need to list them all in your H&P. But if you feel compelled to discuss more, you could add a sentence like, "Based on the patient's age, symptom time course, lack of preceding trauma, and lack of associated neurological or systemic abnormalities, other causes of sixth nerve palsy such as trauma, intracranial tumor, multiple sclerosis, meningitis, and giant cell arteritis would be exceedingly unlikely." The management plan then discusses how you intend to rule out or rule in potential diagnoses and the treatment you will offer. "Since the vast majority of sixth nerve palsies due to vasculopathy [i.e., damage to the microscopic blood vessels supplying the nerve] or unknown causes resolve spontaneously without treatment in 3-6 months, the plan is to monitor the patient on a monthly basis until resolution, looking for new signs or symptoms that would suggest an alternative diagnosis. In the absence of additional signs or symptoms, no further work-up is needed. If diplopia persists beyond 6 months, she will be referred to an ophthalmologist for Fresnel prisms. In the meantime, she will be given an eye patch for symptomatic relief. Finally, since the possibility of a small pontine infarct cannot be entirely excluded, even if no lesion were seen on MRI, she will be started on an aspirin a day and should see her internist for better management of hypertension and diabetes." So, I like to think of the presentation as "building a case for the verdict" (verdict=diagnosis you believe the patient has). First you present the raw facts (history and exam findings), then you summarize and interpret the facts in a logical fashion (summary and anatomical localization), next you state what you believe to be the correct conclusion and discount all other conclusions (diagnosis), and finally you say what you're going to do about it (management plan). V6.15.11 34 Performing a Lumbar Puncture on Neurology 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. Check coags/plts, INR < 1.5, plts > 50, don’t forget about the PTT. Make sure there is no risk of herniation (look for papilledema and check the HCT). Obtain consent, place it in the chart, and explain the procedure to the patient. Give IV Ativan to anxious patients. Obtain a LP kit. Gather what is not in the LP kit: a. sterile gloves (bring an extra pair) b. non-sterile gloves c. pen d. extra lidocaine (only 2mL is in the kit; write an order for either a 1% or 2% 5mL bottle, and ask the nurse to get it out of pyxis) e. sprotte needle f. betadine g. plenty of extra 4 x 4 gauze. h. chuck pad i. sterile towels (optional) j. yellow face mask Place the yellow sticker from the LP kit on the card inside the red binder at the nurses station. Place all equipment on a food tray table, with a trash can at arms length. Adjust the height of the bed to your comfort level. Positioning is key. If opening pressure is needed, the patient needs to be in the lateral decubitus position. Otherwise LPs can be done sitting up much more easily, particularly for the obese. If sitting up, have the patient rest his/her legs on the side of the bed, then have them lean over the food tray table. Wash your hands. Put on your non-sterile gloves. Mark with your pen the exact location where you will insert the spinal needle. The superior iliac crest lines up with the L4 spinous process. With the pad of your thumb you should be able to simultaneously feel both the spinous process and the interspace. Get a feel for the interspace along both the vertical and horizontal plane. Always make your first attempt at L4-L5 before moving up to L3-L4. Tuck the chuck pad under the patients back and buttocks so the betadine will not get on the bed. Open the LP kit and the sterile glove packet. Open the betadine bottle and pour into the reservoir inside the kit. Make sure you squirt away from yourself. Betadine will stain and ruin your clothes. Open the top of the lidocaine bottle (the larger one that did not come with the kit) and place on the outer sterile white covering that surrounds the kit. Make sure to not touch the top of the bottle with your non-sterile hands. Open up the extra gauze packets and drop them into the sterile field. Put on your face mask. Put on the sterile gloves. Unscrew the caps of all of the CSF collection tubes and place them in order that they are to be collected. Set up the manometer and turn the stopcock 180o away from the narrower end. Using all of the pink sponges in the kit, apply betadine in concentric circles. Take a large piece of gauze from your sterile field and use it to pick up the non-sterile lidocaine bottle Draw lidocaine into the syringe. Clean off the betadine directly above the chuck and the patient’s back with a sterile piece of gauze. There are two sterile drapes in the LP kit. Take the tape off the blue drape (the one with a square in the middle), and stick it directly on the patient’s back where you have just removed the betadine. Slightly fold the blue drape so the middle square is not exposed. This drape will lie over the chuck and will serve as a sterile area where you can rest your hands. Place the white sterile drape over the iliac crest, this will allow you to find your interspace while still remaining sterile. In the interim the patient has likely moved and the markings you have previously made with your pen will no longer be accurate. Find your spot once again. Apply lidocaine to the exact spot overlying the desired interspace. Cut the skin with the needle included in the sprotte needle packet. Reconfirm the spot of the intervertebral space. Use your nondominate thumb as a guide, having the middle aspect of the pad of your thumb on the spinous process, and the tip of your thumb simultaneously pressing deeply into the interspace. The needle should be inserted immediately adjacent to the tip of your thumb, at 15 degrees cephalad, as if aiming at the patient’s umbilicus. The needle will pass through, in order, the skin, subcutaneous tissue, supraspinous ligament, interspinous ligament between the spinous processes, ligamentum flavum, epidural space (location of the internal vertebral venous plexus), dura, arachnoird, and into the subarachnoid space between the nerve roots of the cauda equina. V6.15.11 35 35. As the needle passes through the ligamentum flavum, you may feel a popping sensation. 36. If attempt is unsuccessful and bone is encountered, withdraw the needle to the subcutaneous tissue, without exiting the skin, and redirect the needle. Make sure the stylet is hubbed against the needle whenever you pull out and redirect. 37. Once you are in the space, withdraw the stylet in 2-mm intervals to assess CSF flow. If flow is poor, you may rotate the needle 90o, since a nerve may be obstructing the opening. 38. If the tap is traumatic, the CSF may be tinged with blood. The blood should clear as additional CSF is collected, unless the source of the blood is a subarachnoid hemorrhage. If you encounter frank blood and you are uncertain of being in the subarachnoid space, you have probably hit a vein in the internal vertebral venous plexus. Pull out the needle and redirect. 39. Use the flexible tube to connect the manometer (stopcock already turned toward you) to the hub of the needle. A measurement can be made after the column of fluid stops rising. 40. After measuring the opening pressure, turn the stopcock 180o toward the patient so the CSF in the manometer can be collected in your first tube. 41. Remove the manometer and collect 3-4 cc of CSF in each tube. ~10 cc should be collected for either cytology or Trotter studies. 42. Put the stylet back into the LP needle and remove the needle. Make sure the stylet has not been contaminated. 43. Betadine left on the patient’s body is irritating to the skin. Thoroughly clean the betadine off the patient’s back by using hand foam and paper towels. 44. Write a procedure note in Compass. Print it, sign it, and place in chart. If someone supervised, they need to write an addendum to that effect and also sign it. 45. Label all tubes. All labels must be initialed and dated/timed by you. 46. Write order for labels to be made, or make up requisitions yourself. Cytology requires a different form. 47. Hand deliver all CSF to the lab. Following are the labs where each study goes. You will need to send separate tubes to each lab, but you can get multiple labs on the same tube if they are going to the same place (except separate cell counts). Call 2-1470 or 2-1108 with specific questions): Test Tube Location Cell Count/Diff 1&4 Hematology Glucose/Protein 2 or 3 Chemistry Cultures 2 or 3 Microbiology Trotter Studies 2 or 3 Chemistry Viral PCR studies 2 or 3 Microbiology Arbovirus Panel 2 or 3 Chemistry VDRL 1 or 4 Hematology FTA-Ab 2 or 3 Chemistry ACE level 2 or 3 Chemistry Cytology* Any Surgical Pathology 14-3-3/NSE 2 or 3 Chemistry, Don’t forget special form*** NMO Antibody 2 or 3 Chemistry Flow cytometry Any Hematology * Cytology can only be done on weekdays before 3 pm. DON’T FORGET TO REQUEST TO SAVE A TUBE! V6.15.11 36 Neurological History and Exam and the Neurological Write-up Neurology Clerkship Allyson Zazulia, MD and Mark Goldberg, MD Revised 6/05 Much of the following guide to the neurological history and exam should be a review for you. What you learned as a first year student first practicing the neurological exam on a classmate and as a second year student first practicing obtaining a neurological history and performing a neurological exam on a hospitalized patient still holds true as a third year student first taking care of patients with neurological diseases. The neurological history and exam provide the information necessary to anatomically localize your patient’s “lesion,” which is the most important step in neurological diagnosis Once your patient’s symptoms, illness time course, demographic factors, risk factors, and other medical conditions are put together with the exam findings and predicted anatomical localization, you will discover that the etiological possibilities in the differential diagnosis are reduced to just a few. (As you were warned last year, you will hear quite a bit about localization during this rotation. It wouldn’t be a bad idea for you to review the handout from the first lecture in DNS on Neurological Diagnosis.) Steps to Approaching the Neurological History As you were instructed in your pre-clinical years, do not skimp on the neurological history! With a carefully obtained history, it is not uncommon to be able to make a diagnosis before you even take out your reflex hammer and tuning fork—thus the commonly quoted saying that if you have one hour to do an H&P, 50 minutes should be spent on the history and 10 minutes on the exam. 1) Document a careful chronological history of the patient’s symptoms. Start with the very first symptom and work forward from there. Remember that patients often pick the most dramatic events and play down earlier subtle details. Don't let them. Knowing what occurred first allows for knowing how and where the illness started. Ask patients for earlier, perhaps less obvious symptoms. Ask them if they were absolutely 100% normal before this started. "Well, come to think of it, I did have an episode of dizziness and vomiting a month ago. It must have been something I ate." Maybe, but perhaps more likely is that it was the first episode of a recurring pathophysiological process at the same anatomical site. This piece of history is crucial. a. Determine the circumstances surrounding the onset of symptoms. What was the patient doing? Many important pathophysiological clues can be discovered by eliciting these details. "Well Doc, the first time it happened I woke up with numbness on the left side of my face. I had been to my chiropractor the day before and ..." There is the answer! The patient doesn't know that chiropractic manipulation of the neck can traumatize the vertebral arteries and compromise blood flow to the brainstem. You will only get this kind of data by going after all the details of the patient's story. On the other hand, don’t be fooled when patients draw connections that aren’t true, e.g., “It all happened after I slipped in the Wal-Mart parking lot…” Just take all the information in and draw your own conclusions at the end. b. Construct a time-intensity profile of symptom progression. Did everything come on over minutes to hours (acute process, e.g., ischemia)? Was it more of a crescendo progression occurring over days to weeks (subacute process, as with an expanding lesion such as a tumor or abscess)? Were there repeated distinct episodes (recurrent-remittent process, as with transient ischemic attacks, migraines, or seizures)? Was there a steady downward deterioration occurring over months to years (chronic progressive process, e.g., Alzheimer’s dementia)? Note when disability occurred, e.g., when the patient was no longer able to read, walk, drive, go to work. Again, many clues about etiology become clear through this exercise. 2) Think about localization and pathophysiology while taking the history in order to guide what other questions to ask and what parts of the exam to focus on (i.e., think about “neighboring signs”). For example, if the patient tells you he woke up with facial droop and inability to close his eye, ask if he experienced double vision or hearing loss. The facial nucleus is very close to the 6th nerve in the pons, and the facial nerve lies right next to the 8th nerve at the cerebellopontine angle. Different pathophysiological processes occur at different locations within the nervous system. Finding out that the patient has no double vision or hearing V6.15.11 37 loss but does have hypersensitivity to sound, loss of taste, and impaired lacrimation localizes the lesion specifically to the facial nerve within the facial canal and allows you to rule out intrinsic brainstem disease and mass lesions within the cerebellopontine angle. No laboratory test or imaging study is needed to tell you this! 3) Use the patient’s own words, but be sure you understand what those words mean to the patient. Do not substitute your words for the patient’s—writing “hemiplegia” instead of “weakness on my left side” adds little to the accuracy of the information and invites error in interpretation. Similarly, do not accept another doctor’s diagnosis or interpretation, which patients often like to give you in place of details about their actual symptoms. “I was dizzy last week. My doctor said it must have been my blood pressure.” But don’t simply accept the patient’s own words without clarifying what those words mean to the patient. You must insist on a detailed description of symptoms so that you can be sure the two of you are on the same wavelength. You would be surprised what some patients actually mean when they say they have numbness or dizziness. With further questioning, “dizzy” may be described as “my head was swimmy,” and with still further questioning, refined to “things spinning around like when you get sea sick.” This is much more useful, as it suggests vertigo rather than light-headedness or unsteadiness. You can set aside your Holter monitor and tilt table test and focus on causes of labyrinthine dysfunction. 4) Since neurological illness may affect the patient’s level of consciousness, ability to attend, or cognitive function, sometimes it is necessary to involve family members or witnesses in history taking. If you see a patient who was “found down” and has no memory for what happened, it is imperative to speak with somebody who witnessed the event. Finding out that the patient complained of an excruciating headache prior to losing consciousness or that there was jerking of his right face and arm just prior to his falling to the ground is indispensable information. Steps to Approaching the Neurological Examination General considerations 1) After only a limited exposure to the neurological exam in your first and second year coursework, it is to be expected that the exam will still take you a long time to do. Speed should not be your goal. You will be expected to perform a relatively complete neurological exam on your initial evaluation of all patients. In the case of stable patients with clear diagnoses, you may be able to perform a more focused exam (focusing on those exam tests relevant to the patient’s particular complaints) on subsequent evaluations. But this is not appropriate if the diagnosis is unclear or if there is any concern for the development of new findings due to the disease process or your team’s interventions. If in doubt, discuss it with your resident. 2) Remember that even doctors who are proficient at the complete neurological exam perform certain parts of the “screening exam” on all patients. In a patient who has no neurological complaints, you are looking for unexpected findings that may lead to an early diagnosis and possibly treatment of a pre-symptomatic disease, just as you would do by listening to a patient’s lungs even if he has no pulmonary symptoms. Or you may find neurological abnormalities that point towards a specific cause for a systemic disease. For patients with specific neurological complaints, the goal is to test your hypotheses about the nature of the patient’s illness. You should perform not only those tests that will support your hypothesis, but also those tests that will refute it. For example, weakness may be due to a lesion anywhere within the neuroaxis from the cerebral cortex down to the muscle. Finding associated hyperactive reflexes and extensor plantar responses gives you very different information (upper motor neuron dysfunction) than finding hypoactive reflexes, atrophy, and fasciculations (lower motor neuron dysfunction). And if you examine only the muscles and reflexes and ignore the sensory exam because the patient has no sensory complaints, you may miss vital clues to the diagnosis: the presence of associated sensory deficits excludes isolated muscle or neuromuscular junction disease. 3) A great deal of information can be learned about the patient’s neurological function by simple observation. Does he swing his arms symmetrically when walking into your office? Does she interact with you when you stand on the right side of her bed, but ignore you when you stand on the left? Is the sole of one of his shoes worn and the other not? Much of the mental status exam can be completed during history taking. Asking a patient his name as part of a test of orientation may be needless and insulting when he just finished giving you a coherent, detailed chronological description of his illness. V6.15.11 38 4) The neurological exam can be organized into 7 categories: (1) mental status, (2) cranial nerves, (3) motor system, (4) reflexes, (5) sensory system, (6) coordination, and (7) station and gait. It will help if you approach the exam systematically and establish a routine. Some people prefer the standard order listed above. Many test gait first. Others like to work from head to toe. There is no right way to do it, as long as you cover all the categories and keep your patient’s comfort in mind (e.g., minimize the number of times he needs to move from the supine to the seated or standing position). During the course of the exam pay attention to the distribution of abnormalities (proximal vs. distal, arms vs. legs, left vs. right). Mental Status In addition to its value in helping to localize lesions, the mental status exam is required to establish the reliability of the rest of your exam. You must determine that the patient is alert, attentive, oriented, cooperative, and not debilitated by depression or psychosis before you can appropriately interpret other exam findings. If a patient is severely inattentive, he may fail to follow commands, mistakenly leading you to diagnose aphasia. If he is uncooperative and combative, your sensory exam will likely be unreliable. (This does not mean you cannot do any sensory exam, just that you will have to substitute techniques that do not rely on cooperation, i.e., response to pain.) a. Level of awareness: e.g., awake and alert (If not alert, quantify with statement of stimulus required to evoke response, e.g., voice, touch, pain) b. Attentiveness: Is the patient paying attention to you and your questions or is he distractible and requiring re-focusing? Test with serial 7s, WORLD backwards, counting backwards, saying months backwards c. Orientation to self, place, time (Remember that disorientation to time typically occurs before disorientation to place or person and that disorientation to self is typically a sign of psychiatric disease.) d. Speech & language: fluency (does patient speak spontaneously in full sentences without hesitation?), repetition (e.g., “I went to the store and forgot my wallet”), comprehension (is the patient able to follow a 1-, 2-, or 3-step command?), reading (a written command), writing (a complete sentence), naming (objects around the room, including parts of objects) e. Memory: includes registration and retention i. Immediate recall (what did I just say to you?): Test with 3 objects (e.g., apple, table, penny), digit span ii. Recent: current events, home address, what was eaten for breakfast iii. Remote: date of birth/marriage, military experience, birthplace, presidents f. Higher intellectual function: general knowledge, abstraction, judgment, insight, reasoning g. Mood and affect The primary purpose of assessing mood and affect in the neurological exam is to determine if psychiatric disease may be interfering with the neurological assessment. Cranial Nerves The cranial nerves consist of nerves that exit through foramina in the skull, not necessarily nerves that originate in the brain (though most do). The following table lists the various testable functions of each of the cranial nerves. The functions in bold are those that should be tested in a screening exam. I cannot stress enough the importance of the fundoscopic exam in all patients from the standpoint of both the general physical exam and the neurological exam. Visual acuity is certainly a vital part of the general exam, but I did not include it as vital in the screening neurological exam because the vast majority of impairment in visual acuity is due to refractive errors rather than optic nerve dysfunction. Examination I II III, IV, VI V VII Smell (use coffee, lemon, vanilla, etc; avoid peppermint, menthol, and ammonia since they may stimulate taste buds or trigeminal nerve endings and do not specifically test smell) Visual fields, ocular fundi, visual acuity (Snellen chart) Eye movements, pupillary reaction to light and accommodation, convergence Facial sensation, jaw movements, corneal reflex (afferent limb) Facial movements—both spontaneous and to command (raising eyebrows, closing eyes, smiling), taste (e.g., salt, sugar, lemon) V6.15.11 39 VIII IX, X XI XII Hearing (finger rub or whisper—not tuning fork) Palate movement, pharyngeal sensation, voice, swallowing; gag not usually necessary Shrugging shoulders, turning head against resistance Tongue position and movements Please note that while the above table lists the various testable functions of each of the cranial nerves, some of the tests are rarely performed in routine practice because 1) their absence does not necessarily provide useful information (e.g., sense of smell and taste may be absent or reduced in the setting of an upper respiratory infection; gag reflex is absent in many hospitalized patients as well as normal elderly patients) or 2) testing multiple functions of a particular cranial nerve may not add new information (e.g., if pupillary reaction to light is present, then assessing pupillary reaction to accommodation does not give any new information). Again, though, you need to know how to perform these tests in the event that they are relevant to the patient’s complaints or illness. Olfaction must be assessed if the patient complains of a disturbance in taste or smell or if a lesion of the olfactory groove is suspected. Similarly, taste should be assessed when there is a pertinent complaint (though the complaint usually turns out to be due to loss of smell). Pupillary response to accommodation must be assessed if the pupils do not react to light. Corneal reflex must be tested if the patient complains of sensory disturbance in the face (because it is an objective indication of trigeminal nerve dysfunction whereas sensory complaints are subjective) or if the patient is comatose (because you cannot ask the patient if facial sensation is symmetric). However, repeatedly brushing a wisp of cotton across the eye can potentially scratch the cornea, so you don’t need to be checking a corneal reflex every day on your patient with facial numbness. Additional points: - The best way to test visual fields is to cover one of the patient’s eyes and move a finger or penlight into the periphery of each quadrant, asking the patient to indicate when movement is detected. Failing to test each eye individually risks failing to differentiate a deficit present in one eye from that present in both eyes. Having the patient report the number of fingers you are holding up in both of your hands simultaneously requires not only visual field function but also language and calculation; thus you may erroneously diagnose a visual field deficit in the presence of impairment of one of these functions. - For the fundoscopic exam, tell the patient to fix vision on a distant target, and be sure that your head is not obstructing the patient’s view of that target. Remember that the temporal edge of the optic disc is usually quite sharp, but the nasal edge is sometimes not so distinct. Visualizing venous pulsations can be good evidence of normal intracranial pressure. - For visual acuity testing, use a manufactured (not a photocopied) Snellen chart for near vision. The chart should be held at the distance specified on the card. Any glasses should be kept on, and the patient should close one eye and read the smallest line possible. Push patients to keep reading smaller lines—even if they say they can’t—until they make more than 2 errors in a line. - Normal pupillary size is about 2-5 mm. Describe size, equality, and if there is any irregularity. Test the pupillary light reaction in a dark room. Have the patient fix vision on a distant target in order to eliminate the effects of accommodation. Pay attention to both the direct (same eye) and consensual (opposite eye) response. - Extraocular movements should be tested in all six cardinal directions of gaze (a big “H”). Both smooth pursuit (smooth following movements) and saccades (discrete, rapid movements from one object to another) should be assessed. - You should know the boundaries of the trigeminal sensory distribution. V1 extends far back to the top of the skull—it does not end at the hairline. V3 ends just above the jaw line inferiorly and just before the ear laterally. - Assessment of cranial nerves IX and X involves examining palate movement with phonation. A nucleus ambiguous lesion will result in a lower palate ipsilaterally. Do not focus on the uvula, which can deviate to one side or the other in the normal person. Gag need only be tested if the patient’s complaints suggest a cranial nerve IX or X lesion or if the patient is comatose and the palate cannot be assessed. - Sternocleidomastoid strength is tested by placing your hand on the patient’s jaw and having the patient rotate the head towards your hand. With this maneuver, you should be able to see and feel contraction of the opposite SCM. V6.15.11 40 Motor exam The motor exam is affected not only by muscle strength, but also by effort, coordination, and extrapyramidal function. Tests of dexterity and coordination are most sensitive to picking up upper motor neuron and cerebellar abnormalities whereas direct strength testing is more sensitive to lower motor neuron dysfunction. Other important aspects of the motor exam include assessment of muscle tone (e.g., spastic, rigid, flaccid), patterns of muscle atrophy or hypertrophy, disturbances of kinesis (e.g., the hypokinesia [poverty of movement] and bradykinesia [loss of speed and spontaneity of movement] of parkinsonism), and endurance of the motor response (e.g., the fatigability of myasthenia gravis). With regard to muscle strength testing, there are several points to remember. First is the importance of proper positioning. The limb must be positioned in such a way as to permit the muscle being examined to act directly and to avoid as much as possible the recruitment of other muscles having similar function (e.g., biceps and brachioradialis). The proximal portion of the limb must be fixed when movements of distal muscles are being tested. The humerus should be fixed when testing pronation so that the patient is unable to use his shoulder to compensate for weak pronation. Weakness of grip may be erroneously diagnosed if the wrist of a patient with radial nerve palsy is not placed into a position of wrist extension. Second, always give yourself the advantage when testing individual muscle strength. For example, test the iliopsoas by pushing down on the foot of the outstretched leg rather than on the thigh. Do not be afraid to push hard! Even more subtle weakness can be detected by having the patient walk on toes (ankle plantar flexion) and heels (ankle dorsiflexion) and do a knee bend (predominantly iliopsoas). Third, be aware of normal variability in strength based on age, sex, handedness (i.e., the muscles on the dominant side are usually stronger), and muscle (e.g., in a patient with normal strength, you should never be able to overcome the ankle plantar flexors but you will likely be able to overcome the abductor digiti minimi). Fourth, placing a hand on the muscle being tested can confirm whether effort is consistent. If you believe the patient is giving sub-maximal effort (e.g., due to pain), encourage maximal effort for at least “a second.” Grade 0 1 2 3 4 5 Description No muscular contraction Barely detectable muscle contraction Active movement/strength present Active movement/strength against gravity Active movement/strength against gravity & against some resistance Normal muscle strength; active movement against full resistance *Note: “+” or “-“ after the number may be used to further distinguish between items on the scale You should know how to test the following muscles: Upper extremity: 1. Deltoid—abduction (elevation) of upper arm (C5-6, axillary nerve) 2. Biceps—flexion of forearm at elbow (C5-6, musculocutaneous nerve) 3. Triceps—extension of forearm at elbow (C6-8, radial nerve) 5. Extensor carpi radialis—dorsiflexion of hand at wrist (C5-6, radial nerve) 6. Abductor pollicis brevis—palmar abduction of thumb (with thumb at right angle to palm) (C8-T1, median nerve) 7. Interrosei—finger abduction (dorsal) & adduction (palmar) (C8-T1, ulnar nerve) Lower extremity: 1. Gluteus maximus—hip extension (L5-S2, inferior gluteal nerve) 2. Iliopsoas—hip flexion (L1-3, femoral nerve) 3. Quadriceps—knee extension (L2-4, femoral nerve) 4. Hamstrings—knee flexion (L5-S2, sciatic nerve) 5. Tibialis anterior—foot dorsiflexion (L4-5, deep peroneal nerve) 6. Gastrocnemius/soleus—foot plantar flexion (S1-2, tibial nerve) Reflexes Reflex testing is important because it is the most objective part of the neurological exam, it is the least dependent on cooperation (but note that reflexes can be reinforced or decreased voluntarily to some extent, as occurs in guarding), and it may provide an early indication of neurological dysfunction. The muscle stretch reflexes are obtained by placing the muscle in slight tension, tapping the tendon or the periosteum to which the V6.15.11 41 muscle is attached, and observing the vigor and briskness of the response. Muscle contraction should be seen and felt. Pay attention to any asymmetry between right and left. If reflexes are brisk, try to bring out subtle asymmetry by using the lightest tap that will elicit the reflex. If reflexes are diminished or absent, try reinforcing the reflex by distraction or having the patient contract other muscles (e.g., clench teeth). Note, however, that symmetrically brisk, diminished, or even absent reflexes may be found in normal people. The superficial (cutaneous) reflexes are elicited by applying a stimulus to either the skin or mucous membranes and include, among others, the superficial abdominal, cremasteric, anal, and plantar reflexes. Plantar reflexes are often considered to be the most important test in the neurological armamentarium because an abnormal response (i.e., extensor plantar response, Babinski sign, “upgoing toe”) is a specific indicator of corticospinal tract dysfunction and may be the only sign of ongoing disease or the only residual sign of previous disease. Grade 0 1+ 2+ 3+ 4+ Description No response Diminished response Normal/average response Brisker than average response Markedly hyperactive, often with sustained clonus (rhythmic oscillations of flexion/extension) and/or spreading to other muscles You should know how to test the following reflexes (nerve root in bold is the predominant contributor): 1. Biceps (C5, C6; musculocutaneous nerve) 2. Triceps (C6, C7; radial nerve) 3. Knee (L2, L3, L4; femoral nerve) 4. Ankle (S1, S2; tibial nerve) Sensation The sensory exam can be frustrating at times because of its subjective nature and reliance on cooperation. It is prudent to test sensation early in your exam if you anticipate poor cooperation to be a factor. Explain to your patients what you are going to do and what you expect of them, then have them close their eyes for the testing. Be aware of the fact that patients may report differences in sensation in the presence of normal sensory function because of actual differences in the stimulus intensity applied—you are not a machine and cannot apply identical pressure each time you poke with a pin. Both superficial and deep sensation should be tested in all four limbs. Always compare side-to-side, asking, “Are these about the same?” rather than leading questions like, “Is this sharp?” or “Which is stronger?” Remember that thresholds for detecting a stimulus are very low in distal or hair-covered areas and higher over thick skin. Superficial sensation (pain and temperature) is mediated by unmyelinated and small myelinated nerve fibers via the spinothalamic tract. Pain sensation can be tested with a safety pin; temperature sensation can be tested with a cool metal object (like a tuning fork). In the patient complaining of sensory symptoms, demonstrate what the pin/temperature should feel like in an uninvolved area. Since the boundary between “dull” and “sharp” or “warm” and “cool” is usually more readily perceived by the patient if you move your stimulus from the abnormal area to the normal area rather than vice versa, asking the patient to report when the stimulus begins to feel stronger is the best way to identify the margins of a hypesthetic area. Sometimes it is useful to apply the stimulus to an uninvolved part of the body and say, “If this sharpness/coolness is worth $1, how much is this worth?” and then apply the pin/cool object elsewhere. Deep sensation (pressure, position sense, and vibration) is mediated by large fibers via the dorsal and lateral columns. Vibration and position sense (proprioception) should be tested at the most distal joint of the limb. If sensation at this joint is impaired, increase the intensity of the stimulus and/or move proximally. Emphasis should be on the toes and feet, where the longest, large myelinated fibers are most likely to be impaired. The appropriate tuning fork to use in testing vibration is 128-Hz. You should know your own tuning fork perception and the usual time it takes to fade away. But there are no absolutes for how long a normal person should be able to feel a vibratory stimulus at a particular joint because this is dependent on how hard you strike the tuning fork, the patient’s age, etc. It is most important to compare side-to-side perception. For position sense testing, stabilize the joint with one hand and avoid a push-pull stimulus that lets the patient cheat. For example, in the great toe, steady the interphalangeal joint with one hand and hold the sides of the distal phalanx with the other to move it up and down. Make sure the patient understands the only choices are up or down—there is no sideways or middle. Normal thresholds should be no more than 2 or 3 degrees. V6.15.11 42 There is a third category of sensation, integrative sensation, which requires higher level processing of the above primary sensory modalities and includes such functions as stereognosis (ability to recognize objects by touch), graphesthesia (ability to recognize letters or numbers drawn on the finger or palm), 2-point discrimination (ability to differentiate stimulation applied to the skin by one blunt point from stimulation by two points), and constructional ability (copying simple and complex forms, drawing a clock). Extinction is the loss of the ability to perceive sensation on one side of the body when both sides of the body are stimulated simultaneously. Finger agnosia is the inability to recognize, name, and select individual fingers when looking at the hands. The Romberg test is another maneuver that is used to detect impaired sensory input. The patient is first asked to stand with the feet together and eyes open and then to close the eyes. An abnormal response (“positive Romberg sign”) is for the patient to be able to stand upright when the eyes are open, but to sway/fall when the eyes are closed. Contrary to popular belief, a positive Romberg sign is not an indication of cerebellar disease—the patient with cerebellar or other motor dysfunction will have a hard time maintaining an upright posture with the feet together regardless of whether the eyes are open or closed. Rather, it is an indication of either impaired proprioception or vestibular function. (Remember there are three sensory inputs to maintain truncal stability—vision, proprioception, and vestibular function. Patients with impairment of one of these systems are usually able to compensate and maintain truncal stability. They cannot usually compensate when a second system (vision, when the eyes are closed) is removed. For the screening sensory exam, you should perform one test of superficial sensation and one of deep sensation in each limb. Since the majority of asymptomatic sensory deficits you will pick up are neuropathies and the majority of these begin distally, testing at the most distal aspect of the limb is usually sufficient. Coordination and gait Test coordination at rest and with action, in the trunk (e.g., ability to maintain an erect posture while sitting and standing), and in the limbs. Impairment of coordination may be detected through simple observation of the patient performing routine acts such as signing his name, reaching for objects, or getting onto the examination table. Specific tests to look for impaired coordination in the limbs include finger-to-nose (patient alternately touches your outstretched finger and his nose), heel-knee-shin (patient runs the heel of one foot down the shin of the other), rapid alternating movements (patient alternately taps the dorsal and plantar surface of one hand onto the other hand), and finger or toe tapping. In all cases, you should focus on rhythm, steadiness, speed, and precision of movements. Loss of the ability to judge and control distance, speed, and power of a motor act is termed dysmetria. The presence of extraneous movements (e.g., tremor, chorea, myoclonus) should be noted somewhere in your H&P, whether here or in the motor section. Since walking requires proper functioning of the cerebellum and motor, sensory, and vestibular systems as well as a whole host of reflexes, assessment of gait can provide important information to guide the focus of the rest of the neurological exam. It is for this reason that many physicians like to watch the patient walk at the very beginning of the exam. The specific aspects of gait for you to pay attention to include body and extremity posture; length, speed, and rhythm of steps; base of gait (how far apart the legs are); arm swing (is it symmetric?); steadiness; and turning. Testing tandem gait (walking heel to toe) can be helpful, though many otherwise normal elderly patients cannot perform the task. Having the patient hop on each foot is a good way to pick up on subtle problems with strength or coordination. If you hop along with them, they won’t feel stupid doing it. Examples of abnormal gaits include the ataxic gait, which is irregular, jerky, and broad based and is due to either proprioceptive or cerebellar dysfunction and the spastic hemiparetic gait resulting from contralateral corticospinal tract injury, which involves flexion of the upper extremity and extension and internal rotation of the lower extremity with hip hike, circumduction, and scraping of the toes on the ground. The screening exam must include an assessment of gait. Meningeal Signs Neck stiffness often accompanies the meningeal irritation of meningitis or subarachnoid hemorrhage. This is assessed by observing for palpable stiffness on either active or passive flexion and extension at the neck. V6.15.11 43 There are a couple other meningeal signs (Brudzinski’s and Kernig’s) that you may hear mentioned, but since they provide no additional information beyond simple testing for neck stiffness, you do not need to know them. Testing for meningeal signs is not necessary in a screening exam. The Neurological Write-Up Your write-up must include the patient’s complete neurological history and examination. The history section should include the standard categories: Chief complaint History of present illness Past medical history Medications Allergies Social history Family history Review of systems Chief Complaint The chief complaint should be a brief summation of why the patient came to the hospital. Some attendings expect this to be in the patient’s own words. However, in neurology this is frequently impossible and sometimes it is not informative. It is sufficient to describe the primary symptoms—without interpreting them or adding medical jargon—and the time course. This is a 35-year-old man with back pain and progressive difficulty walking over three weeks. If the source of the history is not the patient, it is appropriate here to say how the information is derived. Source: Since the patient was unable to speak on admission, the history was obtained from his wife and review of the outside medical record. HPI Your initial sentence should indicate the patient’s handedness. This is important for interpretation of the physical exam (e.g., a right-handed person would be expected to have better dexterity with the right hand) and for lesion localization (e.g., a left-handed person may have right hemisphere dominance for language, so a lesion of the left frontal or temporal lobe might not produce the expected aphasia in such a patient). It is often useful to include any medical history relevant to the patient’s complaint in the first sentence as long as you keep it brief. But avoid the habit of including the entire medical history in the first breath. The patient is a 55-year-old right-handed woman with long-standing hypertension, diabetes, and tobacco use who was standing at the kitchen sink washing dishes 12 hours after having her neck manipulated by a chiropractor when she suddenly developed nausea, spinning sensation, and inability to feel the temperature of the dish water with her left hand. The remainder of the HPI should chronicle the temporal course of the patient’s symptoms: The patient reports that one day prior to admission, she saw a chiropractor for chronic neck pain, who stretched and “popped” her neck. She awakened on the morning of admission feeling well, ate breakfast without difficulty, and was washing dishes at 8 AM when she suddenly realized that the hot water did not feel hot on her left hand. She was immediately overcome with nausea and felt as if the room were spinning around her. She needed to grab onto the sink to keep from falling. She staggered back to her bedroom, tending to fall into the wall on her right side, and lay down to wait for the feeling to pass. The spinning sensation persisted regardless of the position she was in, and she continued to feel nauseated. At noon, she tried to pick up the telephone with her right hand but kept reaching her hand out too far or too near and knocked over the lamp and clock on the nightstand. She was eventually able to dial 911 with her left hand and noticed that her voice sounded raspy on the phone. Upon arrival to the emergency room at 1 PM, she vomited once. Otherwise, there was no change in her symptoms. V6.15.11 44 This first part of the HPI should conclude with a statement of how the patient presented for the current admission: The patient’s wife found him unresponsive on the bathroom floor at 9:45 AM. She called 911, and the patient was transported by EMS to the BJH ED. Or The patient was referred to the neuromuscular clinic for further evaluation of progressive weakness. Sometimes students are not sure how to organize the history when the current complaint is part of a longstanding disease process. Do you start from the very first manifestation of the disease even if it was 10 years ago and work chronologically forward to the present day? Do you simply state the long-standing diagnosis and then focus only on the current complaint? A much better solution is to first discuss the current complaint chronologically: The patient reports that her right hand hasn’t been “working right” for two days. She first noticed it Monday morning when she had a little difficulty buttoning her shirt. She was able to eat her breakfast and drive to work, but when she tried to sign her name on a credit card receipt at lunchtime, she couldn’t grip the pen well and her handwriting was almost illegible. She had to call her husband to pick her up because she couldn’t turn the key in the car’s ignition. When she touched that hand, the sensation seemed normal. On Tuesday, her hand was about the same, but she noticed some burning on urination and had a temperature of 101, so she called her doctor and was told to go come to the hospital. and then, in a subsequent paragraph, discuss the previous manifestations of the disease: The patient initially sought medical attention 10 years ago when she awoke with blurred vision and noticed that when looking through the right eye, light seemed dim and colors dull. She also experienced right eye pain when looking to extremes of direction. Her symptoms gradually improved over the next several days without treatment and had completely resolved within two weeks. Three months later, she developed numbness in her legs “like someone had shot them up with some novacaine” that started in both anterior thighs and then spread down her legs and into her feet over the span of a couple weeks. Within a few days, she began to have difficulty holding her urine. She was seen at St. Luke’s Hospital where she underwent an MRI of the brain and spine. According to the medical record, the MRI of the brain demonstrated > 20 areas of T2 hyperintensity measuring < 1 cm scattered throughout the periventricular and callosal white matter, none of which enhanced after gadolinium administration. The MRI of the spine demonstrated a focal area of T2 hyperintensity in the cervical cord at the C6-7 level that enhanced after gadolinium administration. She did not have a lumbar puncture. She was treated with a 5-day course of IV methylprednisolone and had complete resolution of her symptoms within several days. She had no new symptoms until 2 years ago when she started “walking like a drunk.” This improved after another course of steroids, but never resolved, and she still needs to walk with a cane when on uneven ground or in the dark. In this case, the previous history supported the diagnosis of multiple sclerosis that the admission facesheet indicated the patient had. But you would be surprised how many patients labeled with a diagnosis are passed down from resident to resident for years before someone finally takes a complete history and realizes that the diagnosis was incorrect. It is appropriate to describe medical details leading up to the current admission, including previous testing, treatment, and effects of treatment. However in most cases, reporting what diagnosis some other doctor gave the patient is unnecessary and even undesirable since it biases your approach to the patient. For example, saying, “Mr. Jones saw Dr. Brown who told him he had Parkinson’s disease” is unnecessary and may steer you down the wrong path. But saying, “Mr. Jones has been taking Sinemet for the past 6 months up to a dose of 3 grams per day without any improvement in his symptoms” is very useful information and should certainly be included in your history. Following the chronological description of each problem in the HPI, a new paragraph should include a description of the patient’s current state including disabilities: V6.15.11 45 The patient states that his jaw pain has been continuous for the last week. He has been able to eat only liquids and has lost 25 pounds in the last month. He can walk short distances but uses a wheelchair outside his home and requires assistance to dress or cook. Finally, the HPI should include any pertinent positives and negatives relevant to the differential diagnosis. Mr. Smith denies previous episodes of weakness or sensory loss. He is unaware of any family members or co-workers with similar problems. He denies exposure to insecticides or industrial toxins, insect bites, and recent travel. On further questioning he notes that he recently completed construction of a wooden deck and has been using the treated scrap wood in his fireplace. Documenting the rest of the history: Avoid repetition. There is no need to repeat information in the PMH or ROS that was already stated in HPI. The social history should include information about the patient’s living situation and ability to return there. Document whether the patient lives alone, needs help for activities of daily living, must climb steps to get to apartment, etc. This information will be essential for discharge planning. Exam The exam section should include a screening general physical exam as well as the seven categories of the neurological exam. The general physical exam should also address any specific areas relevant to the patient’s symptoms or diseases in the differential diagnosis. In the first example above, relevant general physical findings would include the neck exam and the cardiac exam. Assessment and Plan The next step is to put together the data you have collected and work through the anatomic localization of the problem, a differential diagnosis, and management plan. Your assessment and plan should always begin with a brief summary of the patient’s history and exam findings: In summary, the patient is a 55-year-old woman with multiple cerebrovascular risk factors who had the acute onset of nausea, vertigo, and right hand numbness one day after chiropractic manipulation. On exam she has a right Horner’s syndrome, right-sided dysmetria, right facial and left hemibody sensory loss to pinprick, and hoarse voice. This should always be followed by anatomic localization of the process. These symptoms and signs localize to the right lateral medulla with involvement of the vestibular nuclei, spinal trigeminal nucleus, sympathetic fibers, spinothalamic tract, inferior cerebellar peduncle, and nucleus ambiguus. Explain why other localizations are or aren’t possible. The lack of tongue and limb weakness and joint position and vibration impairment indicates that the medial medulla is spared. Next, you should put all these data together to come up with the most likely diagnosis followed by a short list of other possible diagnoses as well as how you are going to prove or disprove them. Given the acute onset of symptoms and the fact that the signs and symptoms are all referable to a specific vascular territory, the most likely diagnosis is a stroke. The patient has multiple risk factors for vascular disease, so there may be atherosclerosis of the vertebral artery as a source for distal embolism. Alternatively, the recent chiropractic manipulation raises the possibility of a vertebral dissection with distal embolism. A cardiac source for embolism is unlikely since she V6.15.11 46 has no history of cardiac disease and has a normal cardiac exam, EKG, and chest x-ray. Other processes, such as multiple sclerosis and tumor, may involve the medulla, but are much less likely based on the patient’s age and time course of symptom development. An MRI scan showing restricted diffusion in the left lateral medulla would confirm the diagnosis of acute ischemic stroke. It may also provide evidence for a vertebral dissection, though angiography would be the definitive test if a dissection were not seen on MRI. Lastly, you should address the management plan. The patient will be admitted to the neurology floor. She is not a candidate for t-PA because her symptom onset was more than 3 hours ago. She will be started on aspirin for stroke treatment/stroke prevention and on subcutaneous heparin for deep venous thrombosis prophylaxis since her mobility is impaired. Because of her impaired pharyngeal function, she will have a swallow evaluation before being permitted to take anything by mouth. She will have speech, occupational, and physical therapy. She will be counseled on smoking cessation. Her antihypertensive medications and insulin will be continued, and diabetes control will be assessed with accuchecks and a hemoglobin AIC. A cholesterol panel will be obtained. MRI of the brain and neck will be performed tomorrow. You are strongly encouraged to use a problem-based plan for initial and subsequent notes. It is uncommon that a patient has only a single problem, and a problem-based plan gives you a framework for daily work. Formatting issues. You may write your note on standard chart paper or print it out on blank pages. neurology forms, you may not create a new form for your notes. Aside from the standard All notes must begin with the heading “WUMS 3 Admission Note” or “WUMS 3 Progress Note.” All notes must start with the date and time. If there is more than one page, number each page (“page 2/6” etc). Sign and date each page. If your signature is not easily legible, you should print your name as well. Correct errors with a single strikethrough and add your initials. Do not use white-out or erasures. Notes must be in the chart on the day of admission. It is your responsibility to have your resident review and sign each note before leaving at the end of the day. V6.15.11 47 Step-by-Step Guide to the Neurological Examination Allyson Zazulia, M.D. Mental Status. A. Level of consciousness. 1. If awake and alert, say that. 2. If not, describe what level of stimulation is needed to arouse and keep patient awake. B. Attentiveness. 1. Patient is attentive if able to attend to you and the examination without getting easily distracted. 2. Have patient go through the months or days of the week backwards or spell WORLD backwards. Note how long it takes, any mistakes, perseveration (repeats self), impersistence (fails to finish), or getting stuck-in-set (going forward instead of backward). C. Orientation. 1. When you initially introduce yourself, you should ask the patient their full name. 2. Ask patient location (city, building, floor), and full date. 3. Patient is “oriented x 3” if all 3 are entirely correct. 4. If not oriented x 3, write out patient’s responses. Do not say “oriented x 2 (or 1)”. D. Speech and language. Listen to patient’s verbal output: motor ability to produce words, quantity of spontaneous speech, rate of speech production, sentence structure, accuracy/appropriateness of words used, and ability to repeat a sentence, follow commands, and come up with the right words for things 1. Fluency is normal if patient speaks in complete sentences without hesitancy between words. Patients who are not fluent may use short, simple, and concrete sentences, and may drop modifier words such as adjectives. They might speak only when prompted by the examiner. 2. Comprehension is normal if patient is able to answer your questions appropriately and follow exam instructions. a. “Do what I say: Look to the door and then look to the window.” b. If not done perfectly, give simpler command: “Show me your thumb.” c. A three-step command that utilizes a crossed command (touch your right earlobe with your left thumb) is most sensitive. 3. Repetition a. “Repeat after me: I went to the store and forgot my wallet.” b. Use compound and complex sentences. “No ifs, ands, or buts” is not a good sentence because it is nonsense. 4. Naming a. Point to objects around room, asking what they are: watch, pen, telephone b. If done well, ask more difficult ones, such as the specific parts of an object: (watch) band, (pen) cap, (telephone) receiver 5. Reading a. Have patient read and follow a written command: Close Your Eyes. 6. Writing a. Have patient write a complete sentence of their choosing. If they are unsure what to write, suggest something about the weather, or how much they like their doctor. E. Memory. 1. Registration: “Repeat these words after me: apple, table, penny.” Do not proceed to memory testing until patient says them all correctly. 2. Immediate Recall: 1-3 minutes later, “What were those 3 words I asked you to remember?” 3. Recent memory: “What did you have for breakfast this morning?” Be sure to ask something that you can confirm. 4. Remote memory: “Where did you grow up/go to school? When was your wedding/child born/military service?” Ask a family member to confirm. F. Higher intellectual function. 1. General knowledge: “Name the last 5 presidents.” 2. Abstraction: “What does ‘People in glass houses shouldn’t throw stones’ mean?” 3. Judgment: “What would you do if you found a sealed, stamped, addressed envelope lying on the ground?” V6.15.11 48 4. Insight: “Why did your daughter bring you to the hospital?” 5. Reasoning: “How do a lie and a mistake differ?” Note: the examples of commands and questions used in assessing mental status that are provided in the preceding section are merely examples, not specific instructions you are expected to follow. Cranial Nerves. G. CN I Olfactory. 1. Have patient close eyes. 2. Occlude one nostril and test other using nonirritating substances (e.g., vanilla, cloves, coffee). Avoid those that stimulate trigeminal nerve endings or taste buds (e.g., peppermint, menthol, ammonia). 3. Compare 2 sides. H. CN II Optic. 1. Visual acuity. a. Be sure your Snellen chart is a manufactured card. Those that are copied or printed in handbooks have poor contrast sensitivity or are not standardized. Always test acuity and visual fields before shining a bright light in patient’s eyes. Be sure to have good lighting in the room. b. Hold Snellen chart at distance specified on the card. (usually 14 inches). c. Cover 1 eye and have patient read chart. d. For each eye, record smallest line patient can read. Push patient to continue reading smaller lines until mistakes occur. Some patients make careless mistakes if they read too fast—ask them to try the next line or read more slowly if you think they can do better. e. Glasses should be left on (looking for optic nerve lesion, not refractive error). f. If vision is worse than 20/25, do the pinhole test to determine whether poor vision is due to a refractive error or to a visual pathway lesion. Repeat steps b through d while patient is looking through a 1 mm pinhole in a sheet of cardboard or a plastic card (e.g., old ID or credit card). Looking through a pinhole allows only central rays of light to enter the eye, which improves vision with a refractive error but not with a visual pathway lesion. 2. Visual fields. a. Stand directly in front of patient and have patient look at your nose. b. Hold your hands ~1 ft. away from patient’s ears and wiggle a finger on one hand. c. Ask patient to indicate on which side the finger is moving. d. Repeat in upper and lower temporal quadrants. e. If abnormality is suspected or is found on screening test above, test all 4 quadrants of each eye individually. i. Have patient close one eye; you should close your own eye that is opposite the patient’s closed eye, since you will be serving as the normal control. ii. Move a finger or penlight into the periphery of each visual quadrant (upper and lower temporal and nasal), asking patient to indicate when movement is detected. It should be seen by you and patient at the same time. 3. Fundoscopy. a. Have patient focus on distant wall. b. Be sure your head is not obstructing patient’s view of that target. c. View optic disc using ophthalmoscope. d. Note disc color and presence of venous pulsations, papilledema (disc hyperemia, blurred margins, absent venous pulsation), or hemorrhages. 4. Pupillary function (CN II and CN III). a. Test pupillary reaction to light. i. The room should be as dark as possible. ii. Ask patient to look into distance to avoid effect of accommodation. iii. Shine bright light obliquely into each pupil. iv. Look for both direct (same eye) and consensual (other eye) constriction. Note whether pupillary reactivity is prompt, sluggish, or absent. v. Record pupil size in mm (normal is about 2-5 mm) and any asymmetry or irregularity. b. If pupillary reaction to light is abnormal, test pupillary reaction to accommodation. V6.15.11 49 i. Hold finger 10 cm from patient’s nose. ii. Have patient alternate looking into distance and at finger. iii. Observe pupillary response. I. CN III, IV, VI Oculomotor, Trochlear, Abducens. 1. Visual inspection. a. Look at ocular alignment at rest (primary gaze). Does light reflex hit at same location in each eye? Is one eye deviated in, down and out, or up? Are there any jerking movements in primary position (looking straight ahead)? b. Observe for ptosis (lid droopiness). 2. 6 cardinal directions of gaze. a. Stand 3-6 feet in front of patient. b. Ask patient to follow your finger with the eyes without moving the head. Place your hand on top of head to keep it still if necessary. c. Move your finger slowly in the six cardinal directions (see figure) and observe whether movements are full in each eye. Note whether the eyes follow your finger smoothly (smooth pursuits) and whether there is any horizontal, vertical, or rotary nystagmus (involuntary oscillation of the eyeball). Have patient hold eyes at end-gaze for a few seconds to be sure there is no nystagmus or slippage. 3. Convergence. a. Ask patient to follow your finger with the eyes without moving the head. Hold lids up if necessary. b. Move your finger (or the patient’s thumb) toward bridge of patient's nose and observe eye movements. 4. Smooth pursuits (smooth following movements). a. This was tested with eye movements (#2, above). 5. Saccades (discrete, rapid movements from one object to another). a. Place your index finger at a position just short of lateral end-gaze. Position your nose slightly lateral to mid-position in the opposite direction. Ask patient to look alternatively at your finger and then your nose.. b. Observe accuracy with which eyes reach target. Do they consistently overshoot or undershoot? Do eyes move conjugately? c. Repeat on other side. 6. Nystagmus. a. Observe for nystagmus on primary gaze and with smooth pursuits (#1 and 2, above). b. If present, note direction of movement and whether movement persists or fatigues (over what time period). c. (a few beats of nystagmus at extremes of gaze is a normal finding) 7. Pupillary light response. (see CN II) J. CN V Trigeminal. 1. Facial sensation. a. Explain to patient what you intend to do. b. Use sharp end of a broken cotton swab or a pin to test pain sensation on forehead, cheek, and jaw of each side of face. c. Ask patient to tell you whether it feels about the same on both sides. d. If not, map out where abnormality is to see if it conforms to distribution of trigeminal nerve. Specifically, march stimulus from forehead back past hairline, from cheek to tragus of the ear, and from jaw to neck. (V1 extends far back to the top of the skull—it does not end at the hairline. V3 ends just above the jaw line inferiorly and just before the ear laterally.) V6.15.11 50 e. For mapping areas of diminished sensation, start in the numb area and ask patient to indicate when sensation becomes normal. 2. Corneal reflex (CN V and CN VII). a. Lightly touch peripheral aspect of cornea with fine wisp of cotton. b. Look for normal blink reaction of both eyes. c. Repeat on other side. d. If response is less than brisk, touch cornea more centrally (over the iris). 3. Temporalis and masseter strength. a. Ask patient to open mouth and clench teeth. b. Palpate temporalis and masseter muscles. K. CN VII Facial. 1. Observe for any facial asymmetry at rest in forehead wrinkles, palpebral fissure width, nasolabial folds, or corner of mouth. 2. Ask patient to do the following and note any lag, weakness, or asymmetry: a. Smile. b. Puff out cheeks. c. Close both lips and resist your attempt to open them. d. Close both eyes and resist your attempt to open them. e. Raise eyebrows. 3. Corneal reflex (see CN V). L. CN VIII Acoustic. 1. Screen hearing a. Face patient and hold out your arms with your fingers near each ear. b. Rub your fingers together on one side. c. Ask patient to tell you when and on which side the rubbing is. d. Increase intensity as needed. e. Note any asymmetry. M. CN IX & X Glossopharyngeal & Vagus. 1. Listen to patient’s voice. Note any hoarseness, nasal, or breathy quality. 2. Ask patient to say “Ah” and watch movement of soft palate and pharynx. (Do not pay attention to uvula, which can deviate to one side or another in the normal person.) a. Note any asymmetry of palate elevation. 3. Ask patient to swallow and to cough. 4. In the unconscious or uncooperative patient, test gag reflex. a. Stimulate back of throat with a cotton swab on each side. b. Look for gagging after each stimulus. N. CN XI Spinal Accessory. 1. Trapezius. a. From behind patient, look for atrophy or asymmetry of trapezii. b. Ask patient to shrug shoulders against resistance and note strength. c. Ask patient to push head back against resistance and note strength. 2. Sternocleidomastoid. a. Place hand on lower face and ask patient to turn head towards that side against resistance. b. Observe contraction of opposite sternocleidomastoid. O. CN XII Hypoglossal. 1. Note tongue position at rest in the mouth and on protrusion. Does tongue deviate in either position? V6.15.11 51 2. Ask patient to stick out tongue and move it quickly from side to side. Note strength and rapidity of movements. 3. Have patient push tongue into each cheek while you push from the outside. Note strength. Motor System. P. Visual inspection. 1. Note muscle bulk. Look for generalized or focal muscle wasting or hypertrophy. 2. Look for extraneous movements, e.g., tremor (At rest? With action?), fasciculation (muscle twitching). 3. Note speed of movement, e.g., slow to initiate (bradykinesia) Q. Tone (muscle tension at rest). 1. Ask patient to relax. 2. Flex and extend patient’s wrists, elbows, shoulders, ankles, and knees. 3. Look for resistance that is decreased (hypotonia) or increased (throughout range of motion=rigidity; spring-like=spasticity). R. Strength and Endurance. 1. Isolate muscle you are testing so patient can’t use strong muscles that have similar function to compensate for weak one being tested. 2. Fix proximal joint when testing distally. E.g., if testing pronation, fix the humerus, so patient can’t use shoulder to compensate for weak pronation. 3. Give yourself the advantage. E.g., when testing deltoid, press on outstretched hand rather than on elbow. You need to test with adequate power to detect a subtle abnormality, especially if the patient is larger than you. 4. Have patient walk on heels and toes and do deep knee bend or get out of chair without using arms. 5. Test at least the following muscles on both sides: a. Deltoid: abduction (elevation) of upper arm (C5-6; axillary nerve) b. Biceps: flexion of forearm at elbow (C5-6; musculocutaneous nerve) c. Triceps: extension of forearm at elbow (C6-8; radial nerve) d. Extensor carpi radialis: dorsiflexion of hand at wrist (C5-6; radial nerve) e. Abductor pollicis brevis: palmar abduction of thumb with thumb at right angle to palm (C8-T1; median nerve) f. Interossei: finger abduction (dorsal) and adduction (palmar) (C8-T1; ulnar nerve) g. Iliopsoas: hip flexion (L1-3; femoral nerve) h. Quadriceps: knee extension (L2-4; femoral nerve) i. Hamstrings: knee flexion (L5-S2; sciatic nerve) j. Tibialis anterior: foot dorsiflexion (L4-5; deep peroneal nerve) k. Gastrocnemius/soleus: foot plantar flexion (S1-2; tibial nerve) 6. Assign score of 0-5 for each muscle based on Medical Research Council scale. Pluses and minuses are sometimes used to note asymmetries or to further refine the scale. Grade Description 0/5 No muscular contraction 1/5 Visible muscle contraction, but no movement at the joint 2/5 Movement at the joint, but not against gravity 3/5 Movement against gravity, but not against added resistance 4/5 Movement against resistance, but less than full 5/5 Movement against full resistance; normal strength 7. Note if strength fatigues after sustained muscle contraction. Reflexes. S. Muscle stretch reflexes. 1. Position patient so that you can access the reflex on both sides with the same angle and hammer speed. Have patient relax the limb. V6.15.11 52 2. Tap the tendon/periosteum to which muscle is attached. 3. Observe vigor and briskness of response and compare side-to-side. Asymmetry is very important to note and may be subtle. 4. If reflexes are diminished or absent, try reinforcing the reflex by distraction or via isometric contraction of other muscles (clenched teeth). 5. If reflexes are very brisk, try to bring out subtle asymmetries by using the lightest tap that will elicit the reflex. 6. Test at least the following reflexes: (spinal nerve root in bold is the predominant contributor) a. Biceps (C5, C6; musculocutaneous nerve) i. Patient's arm should be partially flexed at the elbow with palm down. ii. Place your thumb or finger firmly on biceps tendon. iii. Strike your finger with reflex hammer. iv. You should feel the response even if you can't see it. b. Triceps (C6, C7; radial nerve) i. If patient is seated: support upper arm and let forearm hang free. ii. If patient is lying down, flex arm at elbow and hold it close to chest. iii. Strike the triceps tendon above the elbow. c. Knee (L2, L3, L4; femoral nerve) i. Have patient sit or lie down with knee flexed. ii. Strike patellar tendon just below patella. iii. Note contraction of the quadriceps and extension of the knee. d. Ankle (S1, S2; tibial nerve) i. Dorsiflex foot at ankle to keep muscle in slight tension. ii. Strike Achilles tendon. Alternatively, you can strike the ball of the foot if the patient is lying in bed. iii. Watch and feel for plantar flexion at the ankle. 7. Test for clonus (rhythmic oscillations of flexion/extension) at the ankle i. Support knee in a partly flexed position. ii. With patient relaxed, quickly dorsiflex foot. iii. Observe for rhythmic oscillations. 8. Assign grade on scale of 0-4. Grade Description 0 Absent 1 Hypoactive (increased threshold; decreased speed, vigor, & range of response) 2 Normal 3 Brisk/hyperactive (decreased threshold; increased speed, vigor, & range of response) 4 Markedly hyperactive with clonus and/or spreading to other muscles T. Plantar response (L4-S2, especially S1; tibial nerve). 1. Using the end of a reflex hammer, the tines of the tuning fork, a broken tongue blade, or a key, stroke lateral aspect of the sole of each foot from heel to toes, then drag the stimulus across the foot just beneath the toes. 2. Note movement of toes. 3. If no response, increase pressure of stroking. 4. If patient ticklish or withdrawing whole foot, either have patient stroke own foot or apply stimulus along lateral aspect of foot only. 5. Flexion of all toes (downgoing toe) is a normal response. Extension of the great toe (upgoing toe; positive Babinski) with fanning of the other toes is abnormal. V6.15.11 53 II. Sensory System. A. General points. 1. Explain each test before you do it. If the patient is aware of any numb areas, you can ask them to indicate these before you start. However, don’t assume or be biased in your more detailed testing. 2. Unless otherwise specified, the patient's eyes should be closed during testing. 3. Test all 4 extremities. 4. Compare side to side and ask if the two sides are about the same. Avoid leading questions like “Is this sharp?” 5. Compare distal and proximal areas of the extremities. 6. When you detect an area of sensory loss, map out its boundaries in detail. Start in the area of diminished sensation, and move to the area of more normal sensation. B. Vibration. 1. Use a 128-Hz (low-pitched) tuning fork a. Lightly strike tines against your hand and place stem of the fork over most distal joint of patient’s great toe. b. Ask whether patient feels anything and what the sensation is. c. If vibration is felt, ask when it goes away. Count number of seconds. d. Repeat on other side, being sure to strike the fork with about equal force, and compare duration vibration is felt. e. If vibration sense is impaired, move proximally one joint at a time until it is felt. f. Test the fingers in a similar fashion. C. Joint position sense. 1. Grasp patient's great toe on sides of distal phalanx and hold it away from other toes to avoid friction. 2. Demonstrate to patient what "up" and "down" feel like and tell patient you will move the toe in one of these two directions only. 3. Move toe a few degrees and ask patient to identify direction in which toe was moved. 4. If position sense is impaired, increase stimulus intensity (move toe a greater distance); if still impaired, test at more proximal joint (anklekneehip). 5. Test fingers in a similar fashion. D. Pain. 1. Use a safety pin or sharp end of a broken cotton swab. 2. Test for a distal gradient of sensory loss in leg by applying stimulus at toes and marching your way up to knee. a. Ask patient if the sensation is “about the same” or if it changes as you move up the leg. 3. Test for sensory loss in most commonly affected nerve and nerve root distributions. a. Test the following areas: i. Palmar aspect of index finger (median nerve). ii. Palmar aspect of 5th finger (ulnar nerve). iii. Web space between thumb and index finger on dorsal surface of hand (radial nerve). iv. Lateral surface of foot (L5). v. Posterior aspect of leg (S1). b. Apply stimulus to one and then another of these locations in the upper or lower extremity, asking patient if the two areas are “about the same.” 4. In the patient complaining of sensory symptoms, move stimulus from abnormal area to normal area, asking patient to report when stimulus begins to feel stronger. a. Another technique is to apply stimulus to an uninvolved part of the body and say, “If this sharpness/coolness is worth $1, how much is this worth?” and then apply stimulus to the involved part. 5. If there is any suspicion of a spinal cord lesion (e.g., bladder complaints, brisk lower extremity reflexes) or if there is patchy sensory loss in the legs, test for a “spinal level.” This is done by marching up each side of the back with a pin, looking for a consistent level below which sensation is impaired. E. Temperature. V6.15.11 54 F. G. H. I. J. 1. Testing of temperature is usually reserved for the patient in whom testing of pain sensation is abnormal. 2. Press a cold tuning fork against the skin to make sure there is temperature loss in same distribution as pain loss. Light touch. 1. Touch the skin lightly with a piece of cotton. 2. Ask patient to respond whenever a touch is felt (e.g., “left arm”). 3. Test face, arms, and legs in random order. Double simultaneous stimulation (test for extinction/tactile neglect). 1. Can be performed only when light touch is intact. 2. Touch both sides of patient’s face or body simultaneously. 3. Ask patient to indicate whether touch is felt on the left, right, or both. Graphesthesia (integrative sensation). 1. Can be performed only when light touch is intact. 2. Using a pen cap, paper clip, or your finger, draw a number in patient’s palm or, for more sensitivity, on the index finger. Be sure to draw the number so it is facing the patient. 3. Ask patient to identify the number. Stereognosis (integrative sensation). 1. Can be performed only when light touch and position sense are intact. 2. Place a familiar object (e.g., coin, paper clip, key) in patient’s hand. 3. Ask patient to move it around using fingers and to identify it. Romberg. 1. Have patient stand with feet together and eyes open. Watch for swaying and compensating movements of the feet and toes. 2. Have patient close eyes. 3. Hold your arms out to steady/catch patient if necessary. 4. Watch for development of swaying or falling when eyes are closed (“positive Romberg”)—indicates either impaired proprioception or vestibular dysfunction. 5. It is normal for the feet and toes to move and shift weight. This indicates that proprioceptive sense is intact. Patients who have lost proprioceptive sense will not compensate, and will start to fall, only knowing that they are falling because their vestibular sense has been triggered. Coordination. K. Truncal stability. 1. Observe patient sitting on a chair or side of bed with hands in lap. (Make sure if patient sitting on side of bed that bed is reclined flat.) 2. Note any leaning towards one side or falling backwards. L. Fine finger movements (finger tapping). 1. Have patient tap thumb to tip of index finger as big and fast as possible. 2. Observe rhythm, speed, and precision of movements. 3. Repeat on other side. M. Toe tapping. 1. Have patient tap your hand with ball of each foot as fast as possible. 2. Observe rhythm, speed, and precision of movements. 3. Repeat on other side. N. Finger-nose-finger. 1. Have patient alternately touch your outstretched finger and own nose. 2. Be sure your finger is far enough away that patient’s arm must fully extend to reach it. If the elbow is bent, you may miss subtle deficits. 3. Observe speed, and precision of movements. Note any tremor, especially one that worsens as patient’s finger nears the target. Note if patient consistently passes (overshoots), fails to reach (undershoots), or is off to left or right of target. 4. Repeat on other side. O. Heel-knee-shin. 1. Patient can be lying or sitting. Place heel of one foot just below knee of the other leg. 2. Have patient run that heel up and down shin of other leg. 3. Observe speed, and precision of movements. Note any tremor. V6.15.11 55 4. Repeat on other side. P. Rapid Alternating Movements 1. Have patient alternately tap dorsal and plantar surface of one hand onto other hand, the thigh, or the bed (as fast as possible). 2. Observe rhythm, speed, and precision of movements. Station and Gait Q. Observe the patient do the following: 1. Rise from a seated position. 2. Walk across room, turn, and come back. 3. Walk on toes. 4. Walk on heels. 5. Walk heel to toe (tandem gait) in a straight line. (Many otherwise normal elderly people cannot perform this task.) 6. Hop on each foot. R. Be prepared to catch the patient if necessary. If there is any doubt in your mind as to whether the patient may fall, get assistance (nurse, patient care technician, resident) before testing gait. Do not use this doubt as a reason not to test gait, however. S. Pay attention to the following: 1. Posture of body and extremities (e.g., leaning or pulling towards one side or backwards, twisting or holding back one arm). 2. Length, speed, and rhythm of steps. 3. Base of gait (how far apart are the legs). 4. Arm swing (is it reduced unilaterally or bilaterally). 5. Steadiness. 6. Turning (steadiness of turns and number of steps required to complete the turn). Meningeal Signs. T. Ask patient to flex and extend neck. U. Passively flex and extend patient’s neck. V. Observe for palpable stiffness on either active or passive movement. V6.15.11 56 Sample neurological H & P CC: The patient is a 50-year-old right-handed woman with a history of chronic headaches who complains of acute onset of double vision and right eyelid droopiness three days ago. History of present illness: Mrs. Smith states that on Sunday evening (7/14/03) about 20 minutes after sitting down to work at her computer, she developed blurred vision, which she describes as the words on the computer looking fuzzy and seeming to run into each other. When she looked up at the clock on the wall, she had a hard time making out the numbers. At the same time, she also noted a strange sensation in her right eyelid. She went to bed and upon awakening the following morning, she was unable to open her right eye. When she lifted the right eyelid with her fingers, she had double vision with the objects appearing side by side. The double vision was most prominent when she looked to the left, but was also present when she looked straight ahead, up, down, and to the right, and went away when she closed either of her eyes. She also noted that she had pain in both of her eyes that increased if she moved her eyes around, especially on looking to the left. She was seen in the Alton Memorial Hospital ER and subsequently transferred to BJH by ambulance. Mrs. Smith also notes that for the past two to three weeks, she has been having intermittent pounding bifrontal headaches that worsen with straining, such as when coughing or having a bowel movement. The headaches are not positional and are not worse at any particular time of day. She rates the pain as 7 or 8 on a scale of 1 to 10, with 10 being the worst possible headache. The pain lessened somewhat when she took Vicodin that she had lying around. She denies associated nausea, vomiting, photophobia, loss of vision, seeing flashing lights or zigzag lines, numbness, weakness, language difficulties, and gait abnormalities. Her recent headaches differ from her “typical migraines,” which have occurred about 4-6 times per year since she was a teenager and consist of seeing shimmering white stars move horizontally across her vision for a couple minutes followed by a pounding headache behind one or the other eye, photophobia, phonophobia, and nausea and vomiting lasting several hours to two days. She has never taken anything for these headaches other than ibuprofen or Vicodin, both of which are partially effective. The last headache of that type was two months ago. Her visual symptoms have not changed since the initial presentation. She denies previous episodes of transient or permanent visual or neurologic changes. She denies head trauma, recent illness, fever, tinnitus or other neurologic symptoms. She is not aware of a change in her appearance, but her husband notes that her right eye seems to protrude; he thinks that this is a change in the last few days. Past medical history: 1) Migraine headaches, as described in HPI. 2) Depression. There is no history of diabetes or hypertension. Medications: Zoloft 50 mg daily, ibuprofen 600 mg a few times per week, and Vicodin a few times per week. Allergies: None. Social history: The patient lives with her husband and 16-year-old daughter in a 2-story single-family house and has worked as a medical receptionist for 25 years. She denies tobacco or illicit drug use and rarely drinks a glass of wine. Family history: Her mother had migraines and died at the age of 70 after a heart attack. Her maternal grandfather had a stroke at age 69. There is no other family history of stroke or vascular disease, but she has no information about her father’s side of the family. Review of systems: She states that she had an upper respiratory infection with rhinorrhea, congestion, sore throat, and cough about 6 weeks ago. She denies fever, chills, malaise, weight loss, neck stiffness, chest pain, dyspnea, abdominal pain, diarrhea, constipation, urinary symptoms, joint pain, or back pain. Neurologic complaints as per HPI. General physical examination: V6.15.11 57 The patient is obese but well-appearing. Temperature is 37.6, blood pressure is 128/78, and pulse is 85. There is no tenderness over the scalp or neck and no bruits over the eyes or at the neck. There is no proptosis, lid swelling, conjunctival injection, or chemosis. Cardiac exam shows a regular rate and no murmur. Neurologic examination: Mental status: The patient is alert, attentive, and oriented. Speech is clear and fluent with good repetition, comprehension, and naming. She recalls 3/3 objects at 5 minutes. Cranial nerves: CN II: Visual fields are full to confrontation. Fundoscopic exam is normal with sharp discs and no vascular changes. Venous pulsations are present bilaterally. Pupils are 4 mm and briskly reactive to light. Visual acuity is 20/20 bilaterally. CN III, IV, VI: At primary gaze, there is no eye deviation. When the patient is looking to the left, the right eye does not adduct. When the patient is looking up, the right eye does not move up as well as the left. She develops horizontal diplopia in all directions of gaze especially when looking to the left. There is ptosis of the right eye. Convergence is impaired. CN V: Facial sensation is intact to pinprick in all 3 divisions bilaterally. Corneal responses are intact. CN VII: Face is symmetric with normal eye closure and smile. CN VII: Hearing is normal to rubbing fingers CN IX, X: Palate elevates symmetrically. Phonation is normal. CN XI: Head turning and shoulder shrug are intact CN XII: Tongue is midline with normal movements and no atrophy. Motor: There is no pronator drift of out-stretched arms. Muscle bulk and tone are normal. Strength is full bilaterally. Deltoid L 5 R 5 Biceps Triceps Wrist extensio n 5 5 5 5 5 5 Finger Hip Hip abduction flexion extensio n 5 5 5 5 5 5 Knee flexion Knee Ankle Ankle extension flexion extension 5 5 5 5 5 5 5 5 Reflexes: Reflexes are 2+ and symmetric at the biceps, triceps, knees, and ankles. Plantar responses are flexor. Sensory: Light touch, pinprick, position sense, and vibration sense are intact in fingers and toes. Coordination: Rapid alternating movements and fine finger movements are intact. There is no dysmetria on finger-to-nose and heel-knee-shin. There are no abnormal or extraneous movements. Romberg is absent. Gait/Stance: Posture is normal. Gait is steady with normal steps, base, arm swing, and turning. Heel and toe walking are normal. Tandem gait is normal when the patient closes one of her eyes. Laboratory Data: (Record here all available lab data; circle any abnormal values). CT (non-contrast) 7/17: no abnormalities. Orbits not well seen. MRI 7/18: Multi-focal areas of increased signal on T2 and FLAIR in the deep white matter bilaterally. These range in size from 1 to 10 mm and do not enhance after administration of gadolinium. There are no signal abnormalities in the brain stem or in the corpus callosum. No abnormalities in orbits, sinuses, or venous structures. Assessment: V6.15.11 58 In summary, the patient is a 50-year-old woman with longstanding headaches who has had an acute onset of pupil-sparing partial third nerve palsy on the right (involving levator palpabrae, superior rectus, and medial rectus) associated with a bifrontal headache. Because this is an isolated third nerve palsy without involvement of other cranial nerves or orbital abnormalities, the lesion is localized to the nerve itself, e.g. in the subarachnoid space. Ophthalmoplegic migraine remains a likely diagnosis given the history of migraine with aura, even though the current headache is different in character from her usual headaches and is not associated with visual aura, nausea/vomiting, or photophobia. However, other potentially serious causes of third nerve palsy must be excluded. If a third nerve palsy is due to a compressive lesion, the pupillary fibers will generally become involved within about one week of the onset of symptoms. So the fact that her pupil is normal in size and reactive to light weighs against the diagnosis of a compressive lesion such as an aneurysm or tumor, but does not eliminate the possibility. The MRI does not show evidence of a mass lesion, but an aneurysm cannot be completely excluded without an angiogram. Another potentially serious cause of the third nerve palsy is meningitis. The patient is afebrile, has no meningeal signs, is well-appearing, and has been stable over three days, making bacterial meningitis highly unlikely, but atypical meningitis including fungal, Lyme, sarcoid or carcinomatous meningitis are possibilities. Finally, the patient may have a vascular lesion of the third nerve due to unrecognized diabetes. The appearance of the MRI abnormalities is non-specific. The lesions are potentially explainable by migraines, but are also consistent with hypertension or a vasculopathy. The patient denies a history of hypertension, is not currently hypertensive, and has no risk factors for vascular disease, but the possibility of a genetic disorder such as CADASIL cannot be excluded given the lack of paternal history. Plan: Problem 1. R IIIrd nerve palsy. The patient will undergo a cerebral angiogram to evaluate for an aneurysm, particularly a posterior communicating aneurysm. Patient has been informed of risks and benefits of this procedure and it is scheduled for AM. She will be kept NPO for the procedure. A lumbar puncture will be performed with opening pressure assessed and CSF sent for cell count and differential, protein, glucose, cultures and cytology. She will have her glucose and hemoglobin A1C drawn to evaluate for diabetes. She will have close observation for possible neurologic worsening including neuro checks every 4 hours for first 24 hours. She will be given an eye patch for comfort to eliminate the diplopia. Problem 2. Headache. She will be given a trial of naprosyn 400 mg po bid; if this is ineffective, she may require narcotic analgesia while her evaluation is being completed. If the cerebral angiogram and lumbar puncture are negative and her headache does not improve, she may be a candidate for IV dihydroergotamine treatment. Despite the infrequency of her migraines, the occurrence of a debilitating migraine with neurological deficits warrants the use of a prophylactic agent. A tricyclic antidepressant would be a good choice given her history of depression. Problem 3. Depression. The patient denies current symptoms and will continue Zoloft at current dose. Problem 4. Obesity. The patient requests referral to a dietician. V6.15.11 59 NEUROLOGY CLERKSHIP MID-ROTATION FEEDBACK FORM Student:_________________________ Date:___________ Resident:_________________________ A Problem Below Average Average Above Average 1 1 1 1 1 1 2 2 2 2 2 2 3 3 3 3 3 3 4 4 4 4 4 4 5 5 5 5 5 5 N/A N/A N/A N/A N/A N/A 1 1 1 1 1 1 2 2 2 2 2 2 3 3 3 3 3 3 4 4 4 4 4 4 5 5 5 5 5 5 N/A N/A N/A N/A N/A N/A 1 1 2 2 3 3 4 4 5 5 N/A N/A Motivation 1) Is dedicated to doing their best on this rotation 2) Identifies what needs to be done independently 3) Willing to work-up patients 4) Available for teaching and discussion 5) Follows-through on tasks and assignments 6) Effectively uses down-time for learning 1 1 1 1 1 1 2 2 2 2 2 2 3 3 3 3 3 3 4 4 4 4 4 4 5 5 5 5 5 5 N/A N/A N/A N/A N/A N/A Knowledge 1) Outstanding knowledge of diseases and pathophysiology 2) Outstanding knowledge of diagnostics and therapeutics 3) Assimilates and uses new information 4) Recognizes and corrects knowledge deficiencies 5) Demonstrates self-directed learning 1 1 1 1 1 2 2 2 2 2 3 3 3 3 3 4 4 4 4 4 5 5 5 5 5 N/A N/A N/A N/A N/A Professionalism 1) Is punctual and stays until work is finished 2) Displays modesty appropriate for level of training 3) Dress and hygiene are appropriate 4) Respectful of patients, displays compassion, empathy, and advocacy 5) Respectful of team, understands role 6) Responds well to criticism 1 1 1 1 1 1 2 2 2 2 2 2 3 3 3 3 3 3 4 4 4 4 4 4 5 5 5 5 5 5 N/A N/A N/A N/A N/A N/A Clinical Skills 1) Obtains a thorough and complete history 2) Is efficient and flexible as the situation requires 3) Performs a thorough exam with all findings elicited 4) Able to obtain information from difficult patients and other pertinent people 5) Reviews records and ancillary information 6) Has appropriate interpersonal skills with patients and their families Analytical Skills 1) Is able localize the lesion 2) Constructs a pertinent and prioritized differential 3) Excellent logic and reasoning in assessments 4) Constructs a logical and thorough plan 5) Admission note is neat, thorough, pertinent, and timely 6) SOAP note is neat, thorough, pertinent, and timely 7) Oral presentation is pertinent, rehearsed, and demonstrates excellent knowledge of the patient and the assessment 8) Able to synthesize data and keep ‘big picture’ in mind Exemplary V6.15.11 60 1) What are this student’s top 3 strengths? _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ 2) What are 3 items that require improvement over the next 2 weeks? Write down specifically how the student will improve upon these. _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ 3) Is the student making progress on the stated Clerkship Goals and Objectives (review these)? If not, how will they remedy this? _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ 4) Is the student meeting the Clerkship Requirements and Expectations (review these)? If not, how will they remedy this? _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ 5) Are there any additional comments or qualifiers to note? _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ 6) If the student is struggling, are there any personal or special circumstances to note (ie. health problems, family problems, personal issues, mental health problems, learning difficulties, other commitments, etc)? _____________________________________________________________________________ _____________________________________________________________________________ 7) Are there any professionalism concerns? This includes attendance, punctuality, completing assignments on time, treating others with respect, etc. _____________________________________________________________________________ _____________________________________________________________________________ This student’s current performance might encompass a ‘pass’ grade at the end of the clerkship (check this box if there is a chance for ‘pass’ so we can discuss how to remedy this). ____________________________________ ____________________________________ Resident Signature Clerkship Director Signature Date Date ____________________________________ Student Signature Date V6.15.11 61 NEUROLOGICAL EXAM FEEDBACK FORM Student:_________________________ Date:___________ Resident:_________________________ You will be required to hand in this form or a copy to the clerkship administrator by the 2nd Thursday of your rotation. Have resident fill-out the form and review the comments. For students on Neurosurgery, you should have this done by the Neurology teaching resident or chief resident. This form is required, and serves as instant feedback for you. If you are having trouble finding a time to do this with your resident, let the clerkship director know at your next meeting. Needs Improvement Satisfactory Exemplary 1) Introduced self to patient and others in the room 1 2 3 N/A 2) Demonstrates concern for patient comfort and modesty 1 2 3 N/A 3) Positions the patient properly 1 2 3 N/A 4) Uses instruments correctly 1 2 3 N/A 5) Follows a logical sequence of examination 1 2 3 N/A 6) Modifies the exam to adapt to the patients limitations 1 2 3 N/A 7) Focuses on most relevant parts of the exam 1 2 3 N/A a) Mental Status 1 2 3 N/A b) Language 1 2 3 N/A c) Cranial Nerves 1 2 3 N/A d) Motor 1 2 3 N/A e) Reflexes 1 2 3 N/A f) Sensory 1 2 3 N/A g) Coordination 1 2 3 N/A h) Station and Gait 1 2 3 N/A 1 2 3 N/A 8) Examines each of the following correctly OVERALL EVALUATION Formative Comments: _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ V6.15.11 62 NEUROLOGY CLERKSHIP EVALUATION FORM Clerkship Dates:___________ Inpatient Neurology (4 weeks) Neurology Consults (2 weeks) Block:________ Neurosurgery (2 weeks) Pediatric Consults (2 weeks) I am interested in Neurology as a career (does not affect grade). Unsatisfactory Fair Good V. Good Exemplary 1) Attending Teaching:____________________________ 1 2 3 4 5 N/A 2) Attending Teaching:____________________________ 1 2 3 4 5 N/A 3) Attending Teaching:____________________________ 1 2 3 4 5 N/A 4) Attending Teaching:____________________________ 1 2 3 4 5 N/A 1) Senior Resident:____________________________ 1 2 3 4 5 N/A 2) Senior Resident:____________________________ 1 2 3 4 5 N/A 3) Junior Resident:____________________________ 1 2 3 4 5 N/A 4) Junior Resident:____________________________ 1 2 3 4 5 N/A Clinics 1) General Neurology Continuity Clinic ( Barnes or ConnectCare) 2) Pediatric Clinics 3) Epilepsy Clinic 4) Multiple Sclerosis Clinic 5) Movement Disorders Clinic 6) Stroke Clinic 7) Memory & Aging Clinic 8) General Neurology Clinic 1 1 1 1 1 1 1 1 2 2 2 2 2 2 2 2 3 3 3 3 3 3 3 3 4 4 4 4 4 4 4 4 5 5 5 5 5 5 5 5 N/A N/A N/A N/A N/A N/A N/A N/A Student Conferences 1) Neurology Core Teaching Conferences 2) Professor’s Rounds 3) Dr. Van Staverns Neurology Essentials 4) Dr. Landau’s Ethics Conference 1 1 1 1 2 2 2 2 3 3 3 3 4 4 4 4 5 5 5 5 N/A N/A N/A N/A Clerkship 1) Organization 2) Patient mix 3) Feedback 4) Ability to meet clerkship and personal objectives 1 1 1 1 2 2 2 2 3 3 3 3 4 4 4 4 5 5 5 5 N/A N/A N/A N/A Attending(s) Resident(s) Compared to Other Clerkships… 1) Work load 2) Priority on teaching 3) Ability to partake in meaningful patient care 4) Expectations Much Less 1 1 1 1 Similar 2 2 2 2 3 3 3 3 Much More 4 4 4 4 5 5 5 5 N/A N/A N/A N/A Would you like to recommend a Neurology or Neurosurgery resident for a teaching award? :________________________ Please use the back of this sheet for additional comments or suggestions. V6.15.11 63