Cannulation of an Arteriovenous Fistula / Graft Document
advertisement
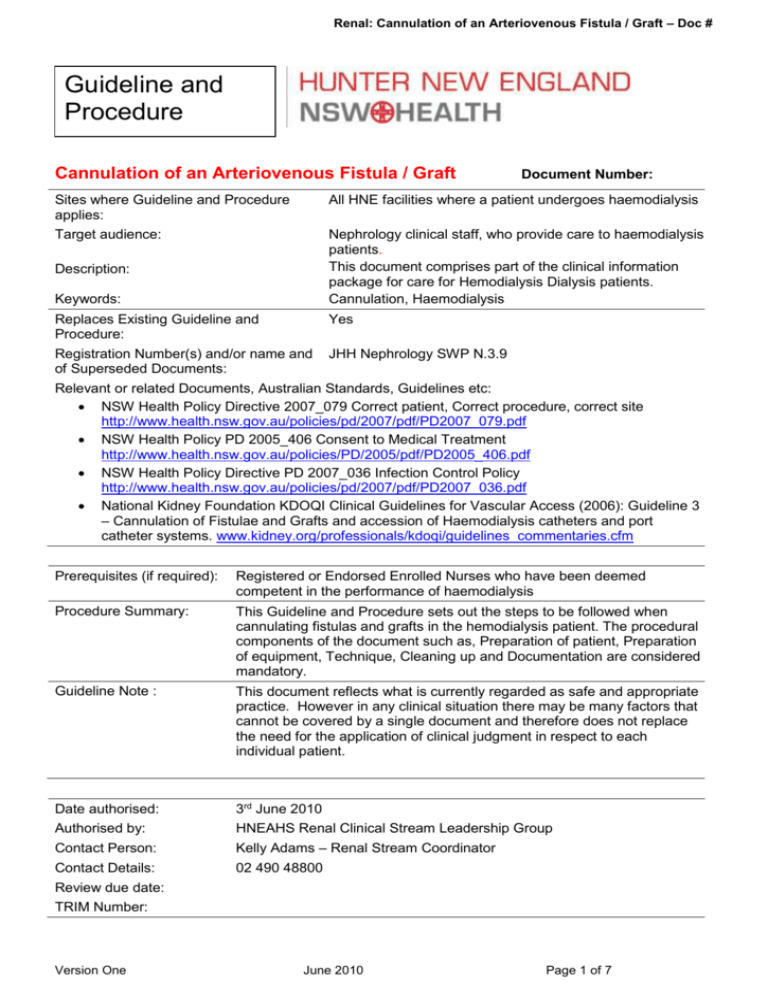
Renal: Cannulation of an Arteriovenous Fistula / Graft – Doc # Guideline and Procedure Cannulation of an Arteriovenous Fistula / Graft Document Number: Sites where Guideline and Procedure applies: All HNE facilities where a patient undergoes haemodialysis Target audience: Nephrology clinical staff, who provide care to haemodialysis patients. This document comprises part of the clinical information package for care for Hemodialysis Dialysis patients. Cannulation, Haemodialysis Description: Keywords: Replaces Existing Guideline and Procedure: Yes Registration Number(s) and/or name and of Superseded Documents: JHH Nephrology SWP N.3.9 Relevant or related Documents, Australian Standards, Guidelines etc: NSW Health Policy Directive 2007_079 Correct patient, Correct procedure, correct site http://www.health.nsw.gov.au/policies/pd/2007/pdf/PD2007_079.pdf NSW Health Policy PD 2005_406 Consent to Medical Treatment http://www.health.nsw.gov.au/policies/PD/2005/pdf/PD2005_406.pdf NSW Health Policy Directive PD 2007_036 Infection Control Policy http://www.health.nsw.gov.au/policies/pd/2007/pdf/PD2007_036.pdf National Kidney Foundation KDOQI Clinical Guidelines for Vascular Access (2006): Guideline 3 – Cannulation of Fistulae and Grafts and accession of Haemodialysis catheters and port catheter systems. www.kidney.org/professionals/kdoqi/guidelines_commentaries.cfm Prerequisites (if required): Registered or Endorsed Enrolled Nurses who have been deemed competent in the performance of haemodialysis Procedure Summary: This Guideline and Procedure sets out the steps to be followed when cannulating fistulas and grafts in the hemodialysis patient. The procedural components of the document such as, Preparation of patient, Preparation of equipment, Technique, Cleaning up and Documentation are considered mandatory. Guideline Note : This document reflects what is currently regarded as safe and appropriate practice. However in any clinical situation there may be many factors that cannot be covered by a single document and therefore does not replace the need for the application of clinical judgment in respect to each individual patient. Date authorised: Authorised by: 3rd June 2010 HNEAHS Renal Clinical Stream Leadership Group Contact Person: Kelly Adams – Renal Stream Coordinator Contact Details: 02 490 48800 Review due date: TRIM Number: Version One June 2010 Page 1 of 7 OUTCOMES 1 To successfully cannulate a fistula and/or graft for the purpose of performing hemodialysis and prolonging the life and patency of the fistula/graft 2 To minimize fistula/graft cannulation complications, ensure optimal patient care and decrease the incidence of hospitalizations due to cannulation related incidences ABBREVIATIONS & GLOSSARY Abbreviation/Word Definition AVF Arteriovenous fistula AVG Synthetic arteriovenous grafts PPE Personal Protective Equipment CVC Central Venous Catheter GUIDELINE An arteriovenous fistula is the surgical joining of an artery and a vein resulting in vein dilatation due to the redirected blood flow. An arteriovenous graft is the surgical placement of a synthetic tube between the artery and the vein and the graft material is where cannulation occurs (Ball, 2006). Haemodialysis associated cannulation involves inserting two large bore steel needles into the arteriovenous fistula or graft. One needle is used to take blood out of the patient and the other needle is used to simultaneously return the filtered blood back to the patient. Blood flow needs to be at least 200mls/minute for effective haemodialysis to occur. A new arteriovenous fistula should not be cannulated until maturation is specified by the Vascular Surgeon, Nephrologist or Vascular Access Nurse. Vascular access related complications contribute to significant morbidity. Safe cannulation practise is essential to minimise these complications and therefore provide optimal patient care and vascular access care maintenance. Ultrasound guided cannulation enables real time visualisation of the vascular anatomy of the patient’s fistula or graft and enhances accurate, safe cannulation practises. Due to length of time needed for appropriate application as well as recent clinical studies (Daarouiche, Wall, Itani et al, 2010) it is recommended that 2% Chlorhexidine gluconate / 70% isopropyl alcohol antiseptic be used for skin preparation as it has a rapid (30sec) and persistent (up to 48hr) microbial activity on the skin. The solution should be applied using a back and forth friction scrub for 30 seconds and then allowed to air dry (KDOQI, 2006). It is recommended that when available, the nursing staff should use hand held ultrasounds to improve visualisation of new vessels when first cannulated and for any ongoing difficult cannulations to decrease the risk of trauma to the vessel. Nursing Alert: Cannulated venous access and cannula connections must be visible at all times and not be covered ie. Bed clothes PROCEDURE The procedure requires mandatory compliance. Patient Preparation It is mandatory to ensure that the patient has received appropriate information to provide informed consent and, that patient identification, correct procedure and correct site process is completed Version One June 2010 Page 2 of 7 prior to any procedure. Note: If able patient should wash their access with antimicrobial soap and water before being seated for treatment Staff Preparation It is mandatory for staff to follow relevant: “Five moments of hand hygiene”, infection control, moving safely/safe manual handling, and documentation practices. New fistula’s / grafts should be accessed by experienced staff only. The staff allocation for this procedure should be in consultation with the Nursing Unit Manager or Team Leader of the shift. If a patient is initiating onto dialysis the Renal Stream Clinical Protocol on Initiating Chronic Dialysis takes precedent in blood flow rates to minimise risk of disequilibrium syndrome Equipment Requirements Alcohol hand gel PPE Dialysis Pack Tape AVF/AVG cannulas x 2 (select appropriate size) Alcohol and Chlorhexidine solution (Must wait 60 seconds for the solution to dry (KDOQI Guideline 3)) Normal Saline ampoules 10ml x 2 to flush cannulas Local anaesthetic as prescribed 3ml syringe and 25g Magellan needle if local anaesthetic is required Tourniquet (for AV fistulas, not for AV grafts) Sharp disposal container Procedure Steps for Cannulation 1. Identify correct patient, introduce yourself and explain procedure to patient. 2. For initial cannulation or post surgical revision of fistula or graft surgeon or Nephrologist approval for cannulation is essential 3. Check for allergies to tapes or local anaesthetics, topical antimicrobial solutions 4. Instruct patient to wash their access site with antimicrobial soap and water 5. Wash your hands 6. Place tourniquet loosely on arm if AVF. Never use a tourniquet for an AVG. 7. Expose entire access limb and assess fistula for location, audible bruit (with stethoscope), cannulation sites, pain, redness, bruising, oedema, exudate, capillary refill. Notify MO of any concerns. In AVG roll fingers over the graft to determine location, width and depth 8. If available (and required) use hand-held ultrasound equipment for precise vascular access visualization 9. Wash your hands 10. Prepare cannulation tray, chlorhexidine, 2 x 10ml Saline flushes, 2 x fistula cannula, anaesthetic as prescribed, one 3ml syringe with magellan 25g needle if using local anaesthetic (Note: topical anaesthetic must be applied 30 minutes prior to cannulations) tapes, sharps container Select appropriate needle size (refer to algorithm) For new fistula 16g for three hemodialysis treatments and gradually increase to 15g as successful cannulations achieved (Van Loon 2009) Cannulating the new fistula with a CVC insitu Insert arterial cannula only (decreases risk of infiltration) and use CVC for venous return for three Version One June 2010 Page 3 of 7 successful cannulations Then use fistula for venous return only for three successful cannulations Then cannulate with arterial and venous cannula and arrange removal of CVC 11. Don PPE 12. Attend hand wash 13. DON gloves 14. Disinfect fistula/graft with Chorhexidine 2% and allow to dry for 1 minute before needle insertion* Alert: Repeat Prep if skin is touched by patient or staff after then skin prep has been applied but prior to commencement of cannulation (KDOQI, 2006) 15. Select arterial cannulation site. Needle Placement 2.5cm hub to hub if antegrade (with blood flow - facing venous anastomosis) /retrograde (against blood flow – facing arterial anastomosis) 7.5cm hub to hub if antegrade/antegrade Needle tip must be 4cm from anastomosis 16. Check cannula caps and clamps are secure to prevent blood leakage when inserting needles 17. Pull skin taut and inject anaesthetic subcutaneously as prescribed. Withdraw plunger to observe for blood return and ensure needle is not in the blood vessel. In the absence of blood return, inject anaesthetic. If blood return evident reposition needle before injecting. Repeat for venous site 18. Tighten tourniquet 19. Hold cannula in dominant hand and pull skin taut in opposite direction of needle insertion 20. Insert arterial cannula at 25 degree angle for fistulas and 45 degree angle for grafts with bevel up, until flash back of blood is evident in tubing. 21. If no signs of resistance, pain or infiltration reduce angle of needle and advance into the vessel. 22. Release the tourniquet 23. If blood flash back is not evident on cannulation but proper placement is suspected, release the cap of the cannula to check for blood flow. 24. Secure cannula with tape across and under wings 25. Allow blood to prime cannula tube 26. Tighten cap and clamp cannula 27. Remove cap 28. Connect Saline syringe, unclamp cannula and draw back to remove air. 29. Flush to check for resistance and flow as well as patients pain rating. 30. Reclamp cannula 31. Repeat for second cannulation 32. Place platypus guards on cannula tubing 33. Commence haemodialysis but ensuring that pressures are checked 34. Dispose of PPE and equipment Version One June 2010 Page 4 of 7 35. Document appropriately Unsuccessful Cannulation Remove needles at the same angle as the angle of insertion. Never apply pressure before the needle is completely out. Apply pressure for 10 minutes with sterile gauze. * Number of attempts Two cannulation attempts by one nurse only for each needle site. Then seek assistance from another cannulator. If infiltration occurs, apply ice and rest for one week or until swelling or bruising resolved. If required instruct patient to use appropriate ointment. If hemodialysis is essential recannulate above area of infiltration. APPENDICES Cannulation Flow Chart Five Moments for Hand Hygiene REFERENCES Ball, L (2005) Improving Arteriovenous Fistula Cannulation Skills. Nephrology Nursing Journal Nov-Dec 2005 Vol 35, No 6. P 1-7 Ball, L (2006) Determining Maturity of New Arteriovenous Fistula. Nephrology Nursing Journal Mar-Apr 2006 Vol 33, No 2. P 1-2 Brouwer, D (1995) Cannulation Camp: Basic Needle Cannulation Training for Dialysis Staff. Dialysis and Transplantation Vol 24, No 11. P 1-7 Darouiche, R.O., Wall, M.J., Itani, K.M.F., Otterson, M.F., Webb, A.L., Carrick, M.M., Miller, H.J., Awad, S.S., Crosby, C.T., Mosier, M.C., Alsharif, A. and Berger, D.H. (2010) Chlorhexadine Alcohol versus Povidone Iodine for surgical site antisepsis. The New England Journal of Medicine, 362(1). p18-26. Hand Hygiene Australia 2008: Five Moments for Hand Hygiene National Kidney Foundation KDOQI Clinical Guidelines for Vascular Access (2006): Guideline 3 – Cannulation of Fistulae and Grafts and accession of Haemodialysis catheters and port catheter systems. www.kidney.org/professionals/kdoqi/guidelines_commentaries.cfm Van Loon, M (2009) Cannulation practice patterns in HD vascular access. Journal of Renal Care EDTNA Version One June 2010 Page 5 of 7 Appendix 1 1. Cannulation of new fistula without CVC Week 1 16g Needles 200 BFR VP <160 mmHg infiltration If significant infiltration rest for 1 week before attempting recannulation Notify Nephrologist to discuss urgency of hemodialysis and vascular access Absence of infiltration Week 2 15g Needles 250-300 BFR VP <160 mmHg 2. New fistula cannulation with CVC insitu Week 1 16g Needles arterial access CVC for venous return 200-250 BFR Absence of infiltration Week 2 15g needles venous return CVC for arterial access 200 – 250 BFR Absence of infiltration Week 3 15g venous and arterial cannulations 250 – 300ml/min BFR Absence of infiltration Arrange removal of CVC Version One June 2010 Page 6 of 7 Appendix 2 Adopted from the World Health Organization and Hand Hygiene Australia. Version One June 2010 Page 7 of 7