Mastopexy with Autologous Augmentation after Massive Weight
advertisement

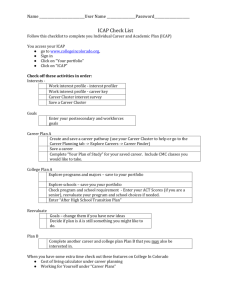
Mastopexy with Autologous Augmentation after Massive Weight Loss: the Intercostal Artery Perforator (ICAP) Flap Stephanie Kwei, M.D., Loren J. Borud, M.D., Bernard T. Lee, M.D. INTRODUCTION: Patients who have achieved massive weight loss (MWL) are left with significant areas of redundant skin and subcutaneous tissue secondary to fat atrophy. Loss of breast volume and additional skin secondary to a tissue expander effect from morbid obesity both contribute to severe breast ptosis after MWL. Furthermore, patients commonly have considerable lateral and posterior tissue surplus of the upper trunk, necessitating an upper body dermolipectomy for the treatment of “back rolls”. Mastopexy with autologous tissue augmentation using a fasciocutaneous flap based on the intercostal artery perforator (ICAP) vessels provides restoration of the upper body and breast deformities of the MWL patient. The ICAP flap combined with a Wise pattern mastopexy allows reduction of lateral and posterior tissue excess with restoration of breast volume and contour. METHOD: Five massive weight loss patients were selected for mastopexy with ICAP flap augmentation. A Doppler probe was used preoperatively and intra-operatively to identify the ICAP vessels along the anterior axillary line. The length of the flap was typically 1520cm according to the amount of lateral and posterior excess tissue. The axis of the flap followed the ribs posteriorly with a slight superior oblique slant at the distal end (Figure 1). The ICAP flaps were elevated in a posterior to anterior fashion, including the muscle fascia. Care was taken to identify and preserve the intercostal perforators located along the lateral chest wall. Next, a Wise-pattern inferior pedicle was dissected and deepithelialized. A subcutaneous pocket was created over the pectoralis muscle fascia up to the clavicle to accommodate the ICAP flap. After sufficient mobilization of the ICAP flap was achieved, the flap was rotated 90 degrees around the previously created inferior pedicle. Once adequate rotation and positioning were accomplished, the ICAP flap was de-epithelialized. The ICAP flap was anchored to the chest wall superiorly and attached to the inferior pedicle. Closure of the breast followed the typical Wise pattern with a lateral extension of the ICAP flap donor site along the inframammary fold. A drain was placed around the ICAP flap, and the patient was placed in a surgical bra at the conclusion of the procedure. RESULTS: All patients were seen approximately one week, one month, three months, and six months after surgery. The early and late postoperative courses were uneventful with respect to mastopexy and ICAP flap autologous augmentation. Postoperative edema and mild ecchymosis of the breasts were observed in the first week after surgery, but these features resolved within one to three months with the use of a sports bra. There was no incidence of infection, hematoma, or seroma. In all cases, there was no evidence of fat necrosis, flap loss, wound dehiscence, or skin necrosis. CONCLUSION: Mastopexy with autologous augmentation using a pedicled fasciocutaneous flap based on the intercostal artery perforator (ICAP) vessels offers restoration of breast volume and body contour after massive weight loss. The lateral and posterior excessive skin and subcutaneous tissues are eliminated by rotation into the breast, effectively performing an upper body lift. Breast ptosis is corrected with standard mastopexy, and an overall improvement in breast contour is achieved. The ICAP flap has demonstrated consistency and durability with minimal morbidity in the five massive weight loss patients presented in this series. Figure 1. Schematic presentation of the ICAP flap and the vascular anatomy of the intercostal artery perforators.