11/23/11 - Arkansas Medicaid
advertisement
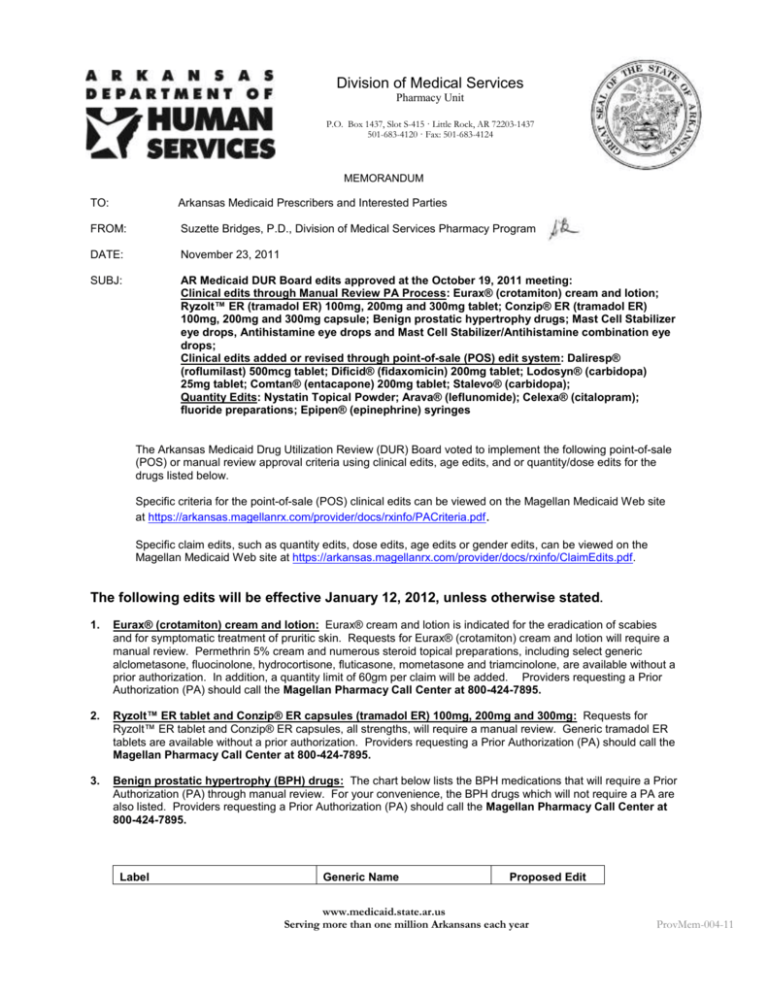
Division of Medical Services Pharmacy Unit P.O. Box 1437, Slot S-415 · Little Rock, AR 72203-1437 501-683-4120 · Fax: 501-683-4124 MEMORANDUM TO: Arkansas Medicaid Prescribers and Interested Parties FROM: Suzette Bridges, P.D., Division of Medical Services Pharmacy Program DATE: November 23, 2011 SUBJ: AR Medicaid DUR Board edits approved at the October 19, 2011 meeting: Clinical edits through Manual Review PA Process: Eurax® (crotamiton) cream and lotion; Ryzolt™ ER (tramadol ER) 100mg, 200mg and 300mg tablet; Conzip® ER (tramadol ER) 100mg, 200mg and 300mg capsule; Benign prostatic hypertrophy drugs; Mast Cell Stabilizer eye drops, Antihistamine eye drops and Mast Cell Stabilizer/Antihistamine combination eye drops; Clinical edits added or revised through point-of-sale (POS) edit system: Daliresp® (roflumilast) 500mcg tablet; Dificid® (fidaxomicin) 200mg tablet; Lodosyn® (carbidopa) 25mg tablet; Comtan® (entacapone) 200mg tablet; Stalevo® (carbidopa); Quantity Edits: Nystatin Topical Powder; Arava® (leflunomide); Celexa® (citalopram); fluoride preparations; Epipen® (epinephrine) syringes The Arkansas Medicaid Drug Utilization Review (DUR) Board voted to implement the following point-of-sale (POS) or manual review approval criteria using clinical edits, age edits, and or quantity/dose edits for the drugs listed below. Specific criteria for the point-of-sale (POS) clinical edits can be viewed on the Magellan Medicaid Web site at https://arkansas.magellanrx.com/provider/docs/rxinfo/PACriteria.pdf . Specific claim edits, such as quantity edits, dose edits, age edits or gender edits, can be viewed on the Magellan Medicaid Web site at https://arkansas.magellanrx.com/provider/docs/rxinfo/ClaimEdits.pdf. The following edits will be effective January 12, 2012, unless otherwise stated. 1. Eurax® (crotamiton) cream and lotion: Eurax® cream and lotion is indicated for the eradication of scabies and for symptomatic treatment of pruritic skin. Requests for Eurax® (crotamiton) cream and lotion will require a manual review. Permethrin 5% cream and numerous steroid topical preparations, including select generic alclometasone, fluocinolone, hydrocortisone, fluticasone, mometasone and triamcinolone, are available without a prior authorization. In addition, a quantity limit of 60gm per claim will be added. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-424-7895. 2. Ryzolt™ ER tablet and Conzip® ER capsules (tramadol ER) 100mg, 200mg and 300mg: Requests for Ryzolt™ ER tablet and Conzip® ER capsules, all strengths, will require a manual review. Generic tramadol ER tablets are available without a prior authorization. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-424-7895. 3. Benign prostatic hypertrophy (BPH) drugs: The chart below lists the BPH medications that will require a Prior Authorization (PA) through manual review. For your convenience, the BPH drugs which will not require a PA are also listed. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-424-7895. Label Generic Name Proposed Edit www.medicaid.state.ar.us Serving more than one million Arkansans each year ProvMem-004-11 AR Medicaid DUR Board tamsulosin hcl 0.4 mg capsule alfuzosin hcl er 10 mg tablet finasteride 5 mg tablet Rapaflo® 4 mg capsule Rapaflo® 8 mg capsule Avodart® 0.5 mg softgel Jalyn® 0.5-0.4 mg capsule 4. 5. Meeting October 19, tamsulosin hcl alfuzosin hcl finasteride silodosin silodosin dutasteride dutasteride/tamsulosin hcl Page 2011 2 of 5 NO PA NO PA NO PA Manual Review Manual Review Manual Review Manual Review Antihistamine eye drops, Mast Cell Stabilizers, and combination Mast Cell/Antihistamine eye drops: The chart below lists the eye drop medications indicated to treat allergic conjunctivitis that will require a Prior Authorization (PA) through manual review. For your convenience, the eye drop medications indicated to treat allergic conjunctivitis which will not require a PA are also listed. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-424-7895. Label cromolyn 4% eye drops Generic Name cromolyn sodium Pkg Size 10ml azelastine hcl 0.05% drops azelastine hcl 6ml ketotifen fum 0.025% eye drops (Brand reference: Zaditor eye drops, Alaway eye drops) ketotifen fum 0.025% eye drops ketotifen fumarate 5ml ketotifen fumarate 10ml Alomide® 0.1% eye drops lodoxamide tromethamine 10ml Alocril® 2% eye drops nedocromil sodium 5ml Alamast® 0.1% drops pemirolast potassium 10ml Emadine® 0.05% eye drops emedastine difumarate 5ml Bepreve® 1.5% eye drops bepotastine besilate 5ml Bepreve® 1.5% eye drops bepotastine besilate 10ml Patanol® 0.1% eye drops olopatadine hcl 5ml Pataday® 0.2% eye drops olopatadine hcl 2.5ml Elestat® 0.05% eye drops epinastine hcl 5ml epinastine hcl 0.05% eye drops epinastine hcl 5ml Proposed Edit NO PA NO PA NO PA NO PA Manual Review Manual Review Manual Review Manual Review Manual Review Manual Review Manual Review Manual Review Manual Review Manual Review Growth Hormone Continuation Criteria: Point-of-sale continuation criteria have been added to the current growth hormone criteria for certain diagnoses. The following point-of-sale continuation criteria were implemented on Nov. 16, 2011: a. For recipients < age 13 years for females and < age 14 for males with a billed diagnosis of pituitary dwarfism within the previous 2 years AND a paid claim in Medicaid history for growth hormone in the previous 6 months. b. For recipients < age 18 years with a billed diagnosis of panhypopituitarism, Turner’s syndrome, PraderWilli syndrome OR septi-optic dysplasia within the previous 2 years AND a paid claim in Medicaid history for growth hormone within the previous 6 months. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800424-7895. 6. Lupron-Ped® criteria revision: The criteria revisions include: The point-of-sale approval requirement of the GnRH stimulation test for CPP will be removed. Point-of-sale continuation criteria will be added to Lupron-Ped® injections for those CPP recipients previously approved who have 3 Lupron-Ped® paid claims in the previous 6 months AND who are < age 11 years for females and < age of 12 years for males. The continuation criteria were implemented on Nov. 16, 2011. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-424-7895. ProvMem-004-11 AR Medicaid DUR Board Meeting October 19, 2011 Page 3 of 5 7. Dificid® (fidaxomicin) 200mg tablet: DIFICID is a macrolide antibacterial drug indicated in adults (≥18 years of age) for treatment of Clostridium difficile-associated diarrhea (CDAD). Point-of-sale criteria will require one billed claim of vancomycin (oral or injectable compounded for oral use) in the previous 10-30 days. In addition, an age edit of ≥18 years of age and quantity limit of 20 tablets per claim will also be added. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-424-7895. 8. Lodosyn® (carbidopa) 25mg tablet: Lodosyn® is indicated for use with SINEMET (Carbidopa-Levodopa) or with levodopa in the treatment of the symptoms of idiopathic Parkinson’s disease (paralysis agitans), postencephalitic parkinsonism and symptomatic parkinsonism which may follow injury to the nervous system by carbon monoxide intoxication and/or manganese intoxication. Point-of-sale criteria will require a billed claim for Sinemet® (carbidopa-levodopa) or Stalevo® (carbidopa-levodopa-entacaptone) in the previous 60 days. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-4247895. 9. Comtan® (entacapone) 200mg tablet: Comtan® (entacapone) is indicated as an adjunct to levodopa/carbidopa to treat recipients with idiopathic Parkinson’s disease who experience the signs and symptoms of end-of-dose “wearing-off.” Point-of-sale criteria will require a billed claim of Sinemet® in the previous 60 days. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-424-7895. 10. Stalevo® (carbidopa/levodopa/entacapone) tablet: Stalevo® (carbidopa, levodopa and entacapone) is indicated to treat patients with idiopathic Parkinson's disease: a. To substitute (with equivalent strength of each of the three components) for immediate-release carbidopa/levodopa and entacapone previously administered as individual products. b. To replace immediate-release carbidopa/levodopa therapy (without entacapone) when patients experience the signs and symptoms of end-of-dose “wearing-off” (only for patients taking a total daily dose of levodopa of 600 mg or less and not experiencing dyskinesias). Point-of-sale rejection criteria will add a therapeutic duplication edit between Comtan® and Stalevo®. A claim for one will reject if there is a recent claim in billed history with overlapping days’ supply for the other medication. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-4247895. 11. Firazyr® (icatibant acetate) 30mg/3 ml syringe: Firazyr® (icatibant) is indicated for the treatment of acute attacks of hereditary angioedema (HAE) in adults 18 years of age and older. Requests for Firazyr® will require a manual review PA. In addition, an age edit of >17 years old and a quantity limit of one syringe per claim will be added. Providers requesting a Prior Authorization (PA) should call the Medicaid Pharmacy Program, 501-6834120. 12. Daliresp® (roflumilast) 500mcg tablet criteria revision: Daliresp® tablet is indicated as a treatment to reduce the risk of COPD exacerbations in patients with severe COPD associated with chronic bronchitis and a history of exacerbations. The point-of-sale approval criteria that were implemented June 21, 2011 will be revised as follows: Recipients to be 18 years or older; AND Have both a billed diagnosis of Chronic Airway Obstruction AND a diagnosis of Chronic Bronchitis in the previous 2 years; AND Have 4 claims in the previous 6 months of two different inhaled LABAs, inhaled corticosteroids (ICS), combination LABA/ICS OR oral steroids. The cumulative quantity limit of 31 tablets per 31 days and a daily dose edit of one tablet per day will remain. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-4247895. 13. COPD inhaled long-acting bronchodilator drugs, ICS and LABA/ICS drugs: According to the GOLD COPD guidelines, an inhaled corticosteroid (ICS) or inhaled corticosteroid/long-acting beta-agonist combination (ICS/LABA) should not be added to therapy until the patient has reached Stage 3 Severe COPD. The current criteria for patients with a billed diagnosis of COPD have been revised as follows: The new criteria will require a billed diagnosis of COPD; AND 3 claims in Medicaid history in the previous 4 months of a long-acting beta-agonist agent (tiotropium bromide (Spiriva® inhaler), arformoterol (Brovana® inhalation solution), formoterol (Perforomist® inhalation solution, Fordil® inhaler), indacaterol (Arcapta® Neohaler), salmeterol (Serevent® Diskus® inhaler)) before a claim for an ICS or ICS/LABA combination inhaler will pay. Providers requesting a Prior Authorization (PA) should call the EBRx PA Call Center Toll Free at 1-866-2502518 or Local at 501-526-4200. ProvMem-004-11 AR Medicaid DUR Board Meeting October 19, 2011 Page 4 of 5 14. Nystatin Topical powder: Nystatin Topical Powder, USP is indicated in the treatment of cutaneous or mucocutaneous mycotic infections caused by Candida albicans and other susceptible Candida species. The Nystatin powder 100,000 units per gram bottles are available in 15 gram, 30 gram, 56.7 gram and 60 gram package sizes. The billing unit for the 100,000 units per gram strength packages is “per gram.” A maximum quantity limit per claim of 60 grams will be added for the 100,000 unit/gm strength packages. Nystatin topical powder is also available in other strengths: 500,000,000 units per container, 150,000,000 units per container and 50,000,000 units per container. The billing unit for these strengths is “per each” container. In order to prevent billing errors, these nystatin powder strengths will be limited to one container per claim. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-4247895. 15. Arava® (leflunomide) tablets: Arava® (leflunomide) is indicated in adults for the treatment of active rheumatoid arthritis (RA): a. To reduce signs and symptoms b. To inhibit structural damage as evidenced by X-ray erosions and joint space narrowing c. To improve physical function A quantity limit of one tablet per day and a cumulative quantity of 31 tablets per 31 days will be added. In addition, a limit of one dose pack per year will implemented. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-424-7895. 16. Celexa® (citalopram) tablets: Celexa® (citalopram HBr) is indicated for the treatment of depression. On Aug. 24, 2011, the FDA notified healthcare professionals and patients that the antidepressant Celexa® (citalopram hydrobromide) should no longer be used at doses greater than 40 mg per day because it can cause abnormal changes in the electrical activity of the heart. Studies did not show a benefit in the treatment of depression at doses higher than 40 mg per day. The entire announcement can be found at this link: http://www.fda.gov/Drugs/DrugSafety/ucm269086.htm#sa. The quantity edits allowed for citalopram will be adjusted to a maximum dose of 40mg per day for all new starts. Recipients currently on citalopram above the recommended maximum dose will be able to continue the dose as long as the recipient is stable and adherent to prescribed therapy, which is defined as 4 billed claims at the higher dose in the previous 6 months. Providers requesting a Prior Authorization (PA) should call the EBRx PA Call Center Toll Free at 1-866-250-2518 or Local at 501-526-4200. 17. Fluoride preparations: Topical and oral fluoride preparations are indicated to aid in the prevention of dental cavities. The topical dental fluoride creams, pastes, gels, drops and rinses are billed on a “per ml” or “per gram” basis. A quantity limit will be added to these products that will allow pharmacists to dispense one (1) package size per claim and will allow pharmacists to bill up to the maximum number of billing units for the package size dispensed. All chewable and oral tablets will have a maximum allowable quantity of one tablet per day and 31 tablets per claim added. 18. Epipen® (epinephrine) syringes: Epipen® (epinephrine) syringes have changed their packaging from single syringes to a pack of 2 syringes. The quantity limit will be changed from three (3) syringes per claim to two (2) syringes per claim. Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-424-7895. FRIENDLY REMINDERS: 1. Incarcerated Persons: The Medicaid Pharmacy Program is prohibited by federal regulations, 42 C.F.R. §435.1009 and §435.1010, from paying for drug claims for Medicaid recipients who, on the date the prescription is filled, are incarcerated in a correctional or holding facility for individuals who are prisoners, including juvenile correctional facilities, are detained pending disposition of charges or are held under court order as material witnesses. If medications are requested for incarcerated Medicaid recipients, the medications cannot be billed to Medicaid Pharmacy Program and are subject to recoupment. Pharmacists should contact the correctional facility regarding the facility’s reimbursement procedures for the requested medications. 2. The AR Medicaid Pharmacy Program reimburses for covered outpatient drugs for Medicaid beneficiaries with prescription drug benefits. Only medications prescribed to the individual beneficiary can be billed using the beneficiary’s Medicaid ID. Sanctions may be imposed against a provider for engaging in conduct that defrauds or abuses the Medicaid program. This could include billing a child’s medication to a parent’s Medicaid ID number and vice-versa. ProvMem-004-11 AR Medicaid DUR Board Meeting October 19, 2011 Page 5 of 5 3. On Oct. 1, 2010, the U.S. Food and Drug Administration (FDA) ordered a halt to marketing of unapproved singleingredient oral colchicine products. Therefore, all unapproved colchicine NDCs do not meet the definition of a covered outpatient drug as defined in the Social Security Act §1927(k) and are subsequently no longer eligible for inclusion in the AR Medicaid Pharmacy Program. The Centers for Medicare & Medicaid Services (CMS) mandated Medicaid agencies to discontinue coverage of all unapproved colchicines products as of Nov. 16, 2010. 4. Hepatitis C Medication Therapy Information Sheet has been revised to include the protease inhibitors. The revised information sheet is located at: https://www.medicaid.state.ar.us/Download/provider/forms/pharm/HepCTreatmntForm.pdf 5. FOR ALL PDL DRUGS OR FOR REQUESTS FOR ANTIPSYCHOTIC DRUGS: Providers requesting a Prior Authorization (PA) for a drug on the PDL or requesting a Prior Authorization (PA) for an antipsychotic medication should contact the Evidence-based Prescription Drug Program PA Call Center Toll Free at 1-866-250-2518 or Local at 501-526-4200 or Fax 501-526-4188. Please include any supporting documentation for the request with the fax, and include recipient ID number, recipient name and Medicaid Provider ID with your request. 6. FOR NON-PDL AND NON-ANTIPYSCHOTIC DRUG REQUESTS: Providers requesting a Prior Authorization (PA) should call the Magellan Pharmacy Call Center at 800-424-7895. For Prior Authorization (PA) requests requiring manual review, you may fax your request to the Magellan Pharmacy Call Center Fax 800-424-7976 or to the state office Fax at 501-683-4124. Please include any supporting documentation for the request with the fax, and include recipient ID number, recipient name and Medicaid provider ID with your request. An approval, denial or request for additional information will be returned by the close of business the following business day. This advance notice is to provide you the opportunity to contact, counsel and change patients’ prescriptions. If you need this material in an alternative format, such as large print, please contact our Americans with Disabilities Act Coordinator at 501-682-0593 (Local); 1-800-482-5850, extension 2-0593 (Toll-Free) or to obtain access to these numbers through voice relay, 1-800-877-8973 (TTY Hearing Impaired). If you have questions regarding this transmittal, please contact the Provider Assistance Center at 1-800-457-4454 (Toll-Free) within Arkansas or locally and out-of-state at (501) 376-2211. Arkansas Medicaid provider manuals (including update transmittals), official notices and remittance advice (RA) messages are available for downloading from the Arkansas Medicaid Web site: www.medicaid.state.ar.us. ProvMem-004-11