clinical interpretation of enzyme activities and concentrations:
advertisement

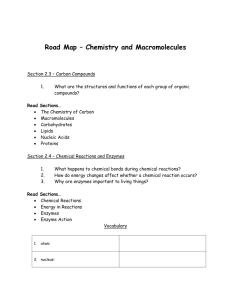
ISRAEL JOURNAL OF VETERINARY MEDICINE Vol. 63 - No. 1 2008 CLINICAL INTERPRETATION OF ENZYME ACTIVITIES AND CONCENTRATIONS: A REVIEW OF THE MAIN METABOLIC FACTORS AFFECTING VARIATION Braun JPa,b ,Médaille Cc ,Trumel Ca (a) Département des Sciences Cliniques, (b) UMR181 Physiopathologie et Toxicologie Expérimentales, INRA, ENVT, Ecole Nationale Vétérinaire, 23 Chemin des Capelles-67013 ,Toulouse Cedex 3, France, (c) Laboratoire Vébiotel, 41bis Av Aristide Briand, 94110 Arcueil, France Corresponding author: JP Braun jp.braun@envt.fr +33 561 193 844 Keywords: dog, horse, cattle, enzyme, plasma, metabolism Summary The activity of enzymes in plasma and other body fluids can be altered by their rate of release from organs, by the distribution of the enzyme in the extracellular compartment, and by the rate and routes of enzyme elimination and inactivation. These factors are influenced by individual variability, disease, drugs, exercise, etc., which need to be considered to ensure a more efficient diagnostic use of enzymes in veterinary clinical practice. INTRODUCTION The diagnostic use of enzymes in veterinary and human clinical pathology is mostly aimed at detecting, evaluating and monitoring organ damage based on the increase in“ organ-specific enzymes( .”See reviews 1, 2). However, enzymes are also used to evaluate the synthetic capacity of an organ, to diagnose the adverse effects of toxic compounds which are enzyme inhibitors, and to monitor the inductive activity of exogenous compounds or enzyme activation by minerals or vitamins (Table I).In all these cases, interpretation is usually based on physiopathological data regarding input of the enzyme into a body fluid, most often blood plasma, and sometimes urine, digestive contents, cerebrospinal fluid, etc., with little consideration for the distribution of enzymes within the body and the clearance of enzymes from the body fluids. When interpreting the decrease in plasma activity of an enzyme used as a marker of organ damage, the plasma half-life of enzymes is sometimes used to address their clearance . 1. Criteria of interpretation of an enzyme activity or concentration Enzyme activities in plasma and other body fluids should be interpreted by integrating all the factors that may influence them, i.e. rate of release from the organ or tissue, distribution within the body, and rate and route(s) of clearance from the body (Figure 1). Unfortunately the answers to some of the following questions are often lacking, e.g. in which organ is the enzyme located in the species of interest? What is the concentration of the enzyme in this organ? By which route does the enzyme reach the plasma ?Is the enzyme (or an isoenzyme) present in blood cells and can haemolysis interfere with interpretation? In which body compartments is the enzyme distributed? Does it remain in the plasma ,urine, or CSF or is it distributed into the extracelllular compartment? Is it internalized by organs, for example, the liver ?What are the mechanisms of enzyme clearance? Which organs are involved in enzyme clearance? What is the route of elimination ? What is the kinetics of elimination or inactivation? 2. Normal mechanisms .1.2.2 Diffusion from intact cells Cells have long been viewed as impermeable structures allowing only limited exchanges between the intracellular and extracellular compartments. More specifically, protein escape from cells has been considered to be abnormal except for secreted proteins and enzymes such as coagulation factors or digestive enzymes. It is now accepted that all cells‘ leak ’some of their contents including proteins, without any sign of cell damage. Only a few precise data are available. For instance, it has been calculated that about 0.1% to 0.01 % of the total amount of trypsinogen synthesized leaks from canine pancreas acinar cells into the extracellular compartment and thence into the plasma where it is measured as TLI (Tryspin-Like Immunoreactivity). Using pharmacokinetic tools, it was shown that the normal release of CK from muscles in the horse was in the range of 0.30 ± 4..2 U.kg.7-h 7, while the intracellular concentration of this enzyme ranged from 3800 to 5440 U/g of fresh equine muscle (3). Similar studies on cows showed a rate of release of 0.69 0.74 ± U.kg.7-h 7-and a muscle concentration of 2900 U/g (4). This amounts to a daily total release of the amount of enzymes present in a few mg of muscle tissue, e.g. 5.8 ± 7.0mg/kg BW in the cow (5.) Little information is available about the factors of variation in enzyme release by normal tissues . Intra-individual variations are moderate; for instance in cows individual CVs ranged from 6% to 29 %, which probably accounts for its moderate variability in plasma enzyme activity (6). Even if release by cells is only one of the factors determining plasma activity ,its variability is likely significant as shown by relatively high day-today variations in healthy animals. For instance, it was shown in healthy dogs that the CV of intra-individual variability was 31% and 36 % for plasma ASAT and ALAT respectively, as compared to 10% for plasma glucose concentrations .)1( Inter-individual variability is high: CK release from muscle in 6 normal resting horses ranged from 1.6 to 3.7 U.kg.7-h .)6( 7-One possible reason for this difference may be the inter-individual variation of enzyme concentration in organs which is high in horses and other species (8-12). This may be one of the causes of the large reference intervals for plasma enzyme activities, for instance 60 to 280 U/L for ASAT in sheep according to Kaneko (13 .) Enzyme release from tissues can be increased by factors such as physical activity or decreased by inactivity. In dogs, the kinetics of CK entry into the thoracic duct following experimental muscle damage to the hind leg is accelerated by movement of the leg (14). Physical effort( without any clinical sign of damage) leads to an increased enzyme release by muscles. In trotting horses, this increase was scarcely measurable for distances less than 30 km but became more intense after 60 km, although it caused only a twofold increase of plasma CK in this case (3). Similar effects were observed in untrained Beagle dogs after a 1hr run at 9 km/h (15, 16 .) Nutritional factors can influence enzyme concentration in organs and their release. This has been especially studied in the fattening of birds and ruminants .)47-71( Drug treatment may also increase the intracellular concentration of enzymes and their release from tissues. This has long been known for canine liver enzyme induction by phenobarbital and glucocorticoids in dogs (22, 23), which induce the synthesis of GGT and ALP, thus increasing the plasma activity of these enzymes ,even after topical application of glucocorticoids (24, 25.) Induction of enzyme synthesis can also be caused by cancer. As a consequence, the increased concentration of enzymes leads to their increased leakage and thus of their plasma activity. This is the case of liver GGT in rats and mice for which the activity is high in foetuses and newborns and low in adults (26). When liver cancer is induced or grafted ,the hepatocytes synthesize more GGT which leads to an increase in plasma GGT activity. In contrast, the amount of enzyme synthesized by an organ can decrease when most of its cells have been destroyed, in the case of liver fibrosis or cirrhosis or in pancreatic insufficiency of the dog. In these cases, leakage of enzymes from the cells is reduced causing a decrease in their activities or concentrations. For instance ,in dogs and cats, a decrease in TLI concentration is the gold standard for pancreatic insufficiency (27, 28), and an increase in coagulation times is a diagnostic criterion for liver insufficiency. .1.2.1 Absorption from the digestive tract This is a minor cause of increased plasma enzyme activity which is only observed in newborns, especially ruminants. During the first hours of life, the intestinal mucosa is still permeable to macromolecules, thus allowing absorption of colostrum proteins, including enzymes. If the concentration of a given enzyme in the colostrum is high, the resulting plasma increase is very high. In cattle, sheep, goats ,and buffaloes the increase of plasma GGT in newborns can be used as an efficient and inexpensive test of colostrum intake (29-32), as the concentration of plasma immunoglobulins is highly correlated to plasma GGT activity. .1.1 Routes of abnormal enzyme release into body fluids .1.1.2 Cell damage Cell damage can range from total irreversible cell necrosis to moderate reversible alteration of membrane impermeability. In any case, the flux of enzymes released from the intracellular compartment is increased, but the extracellular compartment is not the same for all organs or tissues ,as shown in the three following examples. Hepatocytes are in direct contact with plasma of the sinusoid capillaries, the fenestrae of which allow complete exchange of macromolecules with the pericellular space of Disse. Thus in the case of liver damage the total amount of enzyme released from cells immediately enters the plasma compartment. Muscle cells are irrigated by capillaries which have very small pores precluding direct transfer of macromolecules into the plasma. When muscle cell damage occurs, enzymes such as CK (Mr ~85000) are first released into the pericellular compartment from which they are collected by lymphatics into the plasma .Thus there is a delay between cell damage and plasma enzyme activity increase, and this delay varies with physical activity which causes increased lymph drainage. Moreover, enzymes can be degraded or inactivated during their transfer, so their bioavailability is less than .7 The estimated CK in cows, dogs, and horses was ,3. ,.1 and 75 % respectively (4 .) The kidney tubular cells lie on a basal membrane with their apical membrane facing the tubule lumen. In the case of tubular cell damage ,there is no increase in plasma enzyme activity, as enzymes are released immediately and completely into the urine (33), except in the case of very intense kidney damage. This allows early and sensitive detection of even moderate kidney damage. Moreover ,as urine enzymes are cleared with each urination, the amount of enzymes present in urine at any one time precisely reflects the damage which has occurred very recently. This means that the progress of kidney damage can be monitored. This has applications in experimental toxicology (34, 35) (Figure 2.) .1.1.1 Reflux from excretion route In practice the only case is reflux from bile in the case of cholestasis. When the bile flux is slowed down or blocked, the pressure in the bile ducts and ductules is increased. This causes paracellular reflux of the bile contents from the interhepatocyte ductules into the sinusoid capillaries. This is the route by which enzymes such as GGT and ALP, which are present in high concentrations in the membrane of the biliary pole of the hepatocytes, reach the plasma in the case of cholestasis. Moreover ,their transfer to the plasma is increased by the detergent effect of bile acids which solubilise the enzymes from the membranes and induce their synthesis by hepatocytes in the case of cholestasis. .3 Distribution of enzymes in the extracellular compartment When enzymes reach a body fluid, it is assumed that they stay in this compartment, especially in the blood in which exchanges with blood cells do not seem to occur . The volume of distribution of enzymes after injection of purified enzyme preparations was reported to be approximately the same as the plasma volume, i.e. about 5% of the body weight. This has been verified for creatine kinase in the dog (36.) In vivo leakage of enzymes from blood cells to plasma seems to be of little practical relevance, even when their intracellular concentration is high (e.g. LDH). In vitro, this leakage can be quantitatively significant, especially when some degree of haemolysis occurs during coagulation for serum preparations in species with fragile RBCs, such as dogs. In healthy dogs ,serum CK activity is about twice higher than in heparinated plasma (37); however, this is not of relevance in muscle damage assessment because the increases in this case are much more than 2-fold (38.) .4 Elimination/inactivation/degradation of enzymes in the vascular compartment .4.2 Inactivation or degradation in plasma? During their distribution in blood, enzymes are degraded or inactivated to various extents depending on the enzyme. Sometimes these modifications are limited to moderate intravascular proteolysis by circulating proteases or proteases bound to the vascular endothelium. In this case ,there is no alteration of catalytic activity. In humans, the creatine kinase M subunit is modified by action of carboxypeptidase N, which hydrolyzes the C-terminal lysine residue of the molecule, thus producing 3 isoforms of the MM isoenzyme : MM1( native, unmodified), MM2 (minus lysine in one subunit), MM3 (minus lysine in the 2 subunits) and 2 isoforms of the MB isoenzyme. This was used in the diagnosis of myocardial damage (39) before the development of new markers such as troponins. Most studies dealing with the fate of intracellular enzymes in plasma were based on measurement of their catalytic activity and not of their true mass concentration. An enzyme molecule can have lost all or part of its activity by losing a cofactor, and not be truly degraded. Thus, most information available today does not allow differentiation of enzyme clearance due to inactivation from that due to degradation. Using porcine malate dehydrogenase labelled with74. I, it was shown that the clearances of activity and radioactivity were the same in rats, but clearance of the mitochondrial isoenzyme was slower than the clearance of the cytosolic isoenzyme. However, these observations were made with heterologous enzyme preparations and may not be representative of what happens with homologous ones. It was also shown that several dehydrogenases compete for degradation (40-43.) Reversible inactivation of enzymes by loss of a cofactor has no consequence on the in vitro measurement of enzyme activity, because most analytical techniques of enzyme activity measurement are optimized by the addition of cofactors, such as pyridoxal phosphate for aminotransferases, and magnesium for alkaline phosphatase (44-46). Similarly, partial in vivo oxidation of thiol radicals of the catalytic site inhibit creatine kinase. This is reversed in vitro by addition of reducing agents such as Nacetylcysteine (47). 4.2. Renal elimination Low molecular weight enzymes circulating in the plasma are cleared by glomerular filtration. This is the case of alpha-amylase, lipase and trypsinogen. As a result: 1. Their clearance is very rapid, with plasma half-lives in the range of 1 to 4 hours; 2.Chronic renal failure, which causes a decrease of glomerular filtration rate, produces increases in their plasma activity of up to 4 times the upper limit of the reference interval. In some species, filtered enzymes are reabsorbed in the tubule and inactivated or degraded after reabsorption, whereas in other species they are eliminated in urine where their output can be monitored, e.g. alpha-amylase in humans but not in dogs (48, 49). 4.3. Internalization and intracellular catabolism Some enzymes circulating in the plasma are cleared by internalization in tissue macrophages, especially the Kupffer cells of the liver. Isolated hepatocytes can also degrade enzymes in vitro (50). The quantitative importance of this mechanism is not known. It is not specific to enzymes but mainly acts on asialoglycoproteins containing sugar residues terminated by galactose, mannose or N-acetyl glucosamine (51, 52) (Figure 3). In cultured rat liver cells, lactate dehydrogenase M4 isoenzyme is internalized by a receptor recognizing mannose containing glycoproteins, for which it competes with creatine kinase and malate dehydrogenase but not with aminotransferases (53, 54). After endocytosis, most enzymes are degraded in the lysosomes, whereas a small proportion of some enzymes can be excreted into the bile e.g., superoxide dismutase or lyzozyme in the rat. The macrophage capture mechanism is modulated by diverse disease states. In mice infected by Riley virus the clearance of LDH is reduced (55). In sheep, inactivation of the macrophage system by gadolinium retarded the clearance of creatine kinase thereby increasing its plasma half-life, whereas activation by lipopolysaccharide administration had reverse effects (56). It is likely that similar effects are also observed in spontaneous diseases of man and animals, especially in the case of infectious disease or of immunodepression, but this has not been documented to our knowledge. Although precise knowledge of the fates of intracellular enzymes in the extracellular compartment is still lacking, a consideration of all factors likely to modify plasma enzyme activity should improve clinical interpretation. Table I: Examples of possible diagnostic uses of enzyme levels in animal (P-, E-, F-, B- : activity concentration in plasma, RBC, faeces, blood) ___________________________________________________________________ _______ • Detection of organ damage P-ALT (liver, dog, cat), P-GLDH (liver, ruminants, equids), U-NAG (kidney, dog) Reflux of secreted enzyme P-ALP, P-GGT from bile into plasma • Drug induction P-ALP, P-GGT (glucocorticoids, phenobarbital, dog) • Organ secreting activity P-TLI (exocrine pancreas, dog, cat), F-Elastase (exocrine pancreas dog), BProthrombin time (liver, all species) • Inhibition E-ALAD (lead, all species, esp. cattle), P-Cholinesterases (organophosphate derivatives, carbamates, all species, including wildlife) • Activation E-GSHPx (selenium), E-SOD (copper), E-Tranketolase (thiamin) Figure 1: Main routes of release, distribution and clearance of intracellular enzymes used as markers of cell damage. Figure 2: Variations of total amount of GGT eliminated into the urine of rats before (■) and after (□) IP injection of 0.5 mmol/kg NaF. Data from (34). Figure 3: Effect of the number of galactosyl residues added to the SOD molecule on its uptake by rat liver. Data from (52) Figure 4. Effects of in vivo Kupffer cell activation by lipopolysaccharide (LPS) and inhibition by gadolinium on the plasma activity (P-CK, ■) and clearance (Cl-CK, □) of creatine kinase in sheep. Data from (56). References 1. Moss D, Henderson AR. Clinical enzymology. In: Burtis CA, Ashwood ER, editors. Tietz textbook of Clinical Chemistry, Third Edition. Philadelphia: saunders co; p. 617-721, 1999. 2. Kramer JW, Hoffmann WE. Clinical enzymology. In: Kaneko JJ, Harvey JW, Bruss ML, editors. Clinical Biochemistry of Domestic Animals, Fifth Edition. San Diego: Academic Press; p. 303-325, 1997 3. Volfinger L, Lassourd V, Michaux JM, Braun JP, Toutain PL. Kinetic evaluation of muscle damage during exercise by calculation of amount of creatine kinase released. Am J Physiol; 266(2 Pt 2): R434-41, 1994 4. Lefebvre HP, Laroute V, Braun JP, Lassourd V, Toutain PL. Non-invasive and quantitative evaluation of post-injection muscle damage by pharmacokinetic analysis of creatine kinase release. Vet Res;27 (4-5):343-61, 1996 5. Aktas BM, Vinclair P, Autefage A, Lefebvre HP, Toutain PL, Braun JP. In vivo quantification of muscle damage in dogs after general anaesthesia with halothane and propofol. J Small Anim Pract; 38(12):565-9, 1997 6. Lefebvre HP, Toutain PL, Serthelon JP, Lassourd V, Gardey L, Braun JP. Pharmacokinetic variables and bioavailability from muscle of creatine kinase in cattle. Am J Vet Res; 55(4):487-93, 1994 7. Jensen AL, Aaes H. Critical differences of clinical chemical parameters in blood from dogs. Res Vet Sci ;54:10-14, 1993 8. Keller P. Enzyme activities in the dog: tissue analyses, plasma values, and intracellular distribution. Am J Vet Res; 42(4):575-82, 1981 9. Keller P. [Serum enzymes in cattle: organ analysis and normal values]. Schweiz Arch Tierheilkd ;113(11):615-26, 1971 10. Keller P. Enzymaktivitäten bein kleinen Haus- und Laboratoriumstieren: Organalysen, Plasmaspiegel und intrazelluläre Verteilung. Kleinteirpraxis; 24:5168, 1979 11. Gerber H. [Determination of serum enzyme activities in veterinary medicine. 3. D. Determination of LDH, MDH, SHD, GLDH, ALD and alpha-amylase activity in some horse organs as a basis for the clinical interpretation of serum enzyme activity determinations]. Schweiz Arch Tierheilkd; 107(11):626-31, 1965 12. Lindena J, Friedel R, Rapp K, Sommerfeld U, Trautschold I, Deerberg F. Longterm observation of plasma and tissue enzyme activities in the rat. Mech Ageing Dev; 14(3-4):379-407, 1980 13. Kaneko JJ, Harvey JW, Bruss ML. Appendix VIII. Blood analyte reference values in large animals. In: Kaneko JJ, Harvey JW, Bruss ML, editors. Clinical Biochemistry of Domestic Animals, Fifth Edition. San Diego: Academic Press; 1997. p. 890-894. 14. Lindena J, Kupper W, Trautschold I. Enzyme activities in thoracic duct lymph and plasma of anaesthetized, conscious resting and exercising dogs. Eur J Appl Physiol Occup Physiol; 52(2):188-95, 1984 15. Chanoit GP, Lefebvre HP, Orcel K, Laroute V, Toutain PL, Braun JP. Use of plasma creatine kinase pharmacokinetics to estimate the amount of excerciseinduced muscle damage in Beagles. Am J Vet Res; 62(9):1375-80, 2001 16. Chanoit GP, Concordet D, Lefebvre HP, Orcel K, Braun JP. Exercise does not induce major changes in plasma muscle enzymes, creatinine, glucose and total protein concentrations in untrained Beagle dogs. J Vet Med A; 49(4):222-224, 2002 17. Bogin E, Sommer H. Enzyme profile of healthy and fatty liver of cows. Zentralbl Veterinarmed A;25(6):458-63, 1978 Bogin E, Avidar J, Rivetz B, Israeli B. Fatty liver in fattened geese. Enzyme profile of liver and serum. Zentralbl Veterinarmed A; 25(9):727-33, 1978 19. Bogin E, Avidar Y, Israeli B. Enzyme profile of turkey tissues and serum. Zentralbl Veterinarmed A 1976;23(10):858-62. 20. Bogin E, Avidar Y, Merom M. Biochemical changes in liver and blood during liver fattening in rats. J Clin Chem Clin Biochem; 24(9):621-6, 1986 21. Bogin E, Avidar Y, Merom M, Soback S, Brenner G. Biochemical changes associated with the fatty liver syndrome in cows. J Comp Pathol; 98(3):337-47, 1988 22. Braun JP, Guelfi JF, Thouvenot JP, Rico AG. Haematological and biochemical effects of a single intramuscular dose of 6 alpha-methylprednisolone acetate in the dog. Res Vet Sci; 31(2):236-8, 1981 23. Abraham G, Gottschalk J, Ungemach FR. Evidence for ototopical glucocorticoidinduced decrease in hypothalamic-pituitary-adrenal axis response and liver function. Endocrinology; 146(7):3163-71, 2005 24. Meyer DJ, Moriello KA, Feder BM, Fehrer-Sawyer SL, Maxwell AK. Effect of otic medications containing glucocorticoids on liver function test results in healthy dogs. J Am Vet Med Assoc; 196(5):743-4, 1990 25. Hadley SP, Hoffmann WE, Kuhlenschmidt MS, Sanecki RK, Dorner JL. Effect of glucocorticoids on alkaline phosphatase, alanine aminotransferase, and gammaglutamyltransferase in cultured dog hepatocytes. Enzyme; 43(2):89-98, 1990 26. Braun JP, Rico A, Bernard P. [Changes in the distribution of gamma-glutamyl transferase in the organs of the mouse as a function of development]. C R Acad Sci Hebd Seances Acad Sci D; 286(20):1483-5, 1978 27. Williams DA, Batt RM. Sensitivity and specificity of radioimmunoassay of serum trypsin-like immunoreactivity for the diagnosis of canine exocrine pancreatic insufficiency. J Am Vet Med Assoc; 192(2):195-201, 1988 28. Batt RM. Exocrine pancreatic insufficiency. Vet Clin North Am Small Anim Pract; 23(3):595-608, 1993 29. Braun JP, Tainturier D, Laugier C, Benard P, Thouvenot JP, Rico AG. Early variations of blood plasma gamma-glutamyl transferase in newborn calves--a test of colostrum intake. J Dairy Sci; 65(11):2178-81, 1982 30. Bogin E, Avidar Y, Shenkler S, Israeli BA, Spiegel N, Cohen R. A rapid field test for the determination of colostral ingestion by calves, based on gammaglutamyltransferase. Eur J Clin Chem Clin Biochem; 31(10):695-9, 1993 31. Lombardi P, Avallone L, d'Angelo A, Bogin E. gamma-Glutamyltransferase and serum proteins in buffalo calves following colostral ingestion. Eur J Clin Chem Clin Biochem; 34(12):965-8, 1996 32. Lombardi P, Avallone L, Pagnini U, d'Angelo D, Bogin E. Evaluation of buffalo colostrum quality by estimation of enzyme activity levels. J Food Prot; 64(8):12657, 2001 33. Shaw FD. The effect of mercuric chloride intoxication on urinary gamma-glutamyl transpeptidase excretion in the sheep. Res Vet Sci; 20(2):226-8, 1976 34. Kessabi M, Braun JP, Benard P, Burgat-Sacaze V, Rico AG. Acute kidney toxicity of sodium fluoride in the rat. Toxicol Lett; 5(2):169-74, 1980 35. Bret L, Hasim M, Lefebvre H, Fournie GJ, Braun JP. Kidney tubule enzymes and extracellular DNA in urine as markers of nephrotoxicity in guinea pig. Enzyme Protein; 47:27-36, 1993 36. Aktas M, Lefebvre HP, Toutain PL, Braun JP. Disposition of creatine kinase activity in dog plasma following intravenous and intramuscular injection of skeletal muscle homogenates. J Vet Pharmacol Ther; 18(1):1-6, 1995 37. Aktas M, Auguste D, Concordet D, Vinclair P, Lefebvre H, Toutain PL, et al. Creatine kinase in dog plasma: preanalytical factors of variation, reference values and diagnostic significance. Res Vet Sci; 56(1):30-6, 1994 38. Aktas M, Auguste D, Lefebvre HP, Toutain PL, Braun JP. Creatine kinase in the dog: a review. Vet Res Commun; 17(5):353-69, 1993 39. Hossein-Nia M, Kallis P, Brown PA, Chester MR, Kaski JC, Murday AJ, et al. Creatine kinase MB isoforms: sensitive markers of ischemic myocardial damage. Clin Chem; 40(7):1265-1271, 1994 40. Bijsterbosch MK, Duursma AM, Bouma JM, Gruber M. Plasma clearance and endocytosis of cytosolic malate dehydrogenase in the rat. Biochem J; 210(2):41928, 1983 41. Bijsterbosch MK, Duursma AM, Bouma JM, Gruber M. Endocytosis and breakdown of mitochondrial malate dehydrogenase in the rat in vivo. Effects of suramin and leupeptin. Biochem J; 208(1):61-7, 1982 42. Bijsterbosch MK, Duursma AM, Bouma JM, Gruber M, Nieuwenhuis P. Plasma clearance and endocytosis of mitochondrial malate dehydrogenase in the rat. Biochem J; 200(1):115-21, 1981 43. Bijsterbosch MK, Duursma AM, Smit MJ, Bos OJ, Bouma JM, Gruber M. Several dehydrogenases and kinases compete for endocytosis from plasma by rat tissues. Biochem J; 229(2):409-17, 1985 44. Schumann G, Bonora R, Ceriotti F, Ferard G, Ferrero CA, Franck PF, et al. IFCC primary reference procedures for the measurement of catalytic activity concentrations of enzymes at 37 degrees C. International Federation of Clinical Chemistry and Laboratory Medicine. Part 4. Reference procedure for the measurement of catalytic concentration of alanine aminotransferase. Clin Chem Lab Med; 40(7):718-24, 2002 45. Schumann G, Bonora R, Ceriotti F, Ferard G, Ferrero CA, Franck PF, et al. IFCC primary reference procedures for the measurement of catalytic activity concentrations of enzymes at 37 degrees C. International Federation of Clinical Chemistry and Laboratory Medicine. Part 5. Reference procedure for the measurement of catalytic concentration of aspartate aminotransferase. Clin Chem Lab Med; 40(7):725-33, 2002 46. Tietz NW, Rinker AD, Shaw LM. IFCC methods for the measurement of catalytic concentration of enzymes Part 5. IFCC method for alkaline phosphatase (orthophosphoric-monoester phosphohydrolase, alkaline optimum, EC 3.1.3.1). J Clin Chem Clin Biochem; 21(11):731-48, 1983 47. Horder M, Elser RC, Gerhardt W, Mathieu M, Sampson EJ. International Federation of Clinical Chemistry, Scientific Division Committee on Enzymes: approved recommendation on IFCC methods for the measurement of catalytic concentration of enzymes. Part 7. IFCC method for creatine kinase (ATP: creatine N-phosphotransferase, EC 2.7.3.2). Eur J Clin Chem Clin Biochem; 29(7):435-56, 1991 48. Jacobs RM. Relationship of urinary amylase activity and proteinuria in the dog. Vet Pathol; 26(4):349-50, 1989 49. Jacobs RM. Renal disposition of amylase, lipase, and lysozyme in the dog. Vet Pathol; 25(6):443-9, 1988 50. Kopitz J, Kisen GO, Gordon PB, Bohley P, Seglen PO. Nonselective autophagy of cytosolic enzymes by isolated rat hepatocytes. J Cell Biol; 111(3):941-53, 1990 51. Stockert RJ. The asialoglycoprotein receptor: relationships between structure, function, and expression. Physiol Rev; 75(3):591-609, 1995 52. Staud F, Nishikawa M, Takakura Y, Hashida M. Liver uptake and hepato-biliary transfer of galactosylated proteins in rats are determined by the extent of galactosylation. Biochim Biophys Acta; 1427(2):183-92, 1999 53. Smit MJ, Duursma AM, Bouma JM, Gruber M. Receptor-mediated endocytosis of lactate dehydrogenase M4 by liver macrophages: a mechanism for elimination of enzymes from plasma. Evidence for competition by creatine kinase MM, adenylate kinase, malate, and alcohol dehydrogenase. J Biol Chem; 262(27):13020-6, 1987 54. De Jong AS, Duursma AM, Bouma JM, Gruber M, Brouwer A, Knook DL. Endocytosis of lactate dehydrogenase isoenzyme M4 in rats in vivo. Experiments with enzyme labelled with O-(4-diazo-3,5-di[125I]iodobenzoyl)sucrose. Biochem J; 202(3):655-60, 1982 55. Mahy BW, Rowson KE, Parr CW. Studies on the mechanism of action of Riley virus. IV. The reticuloendothelial system and impaired plasma enzyme clearance in infected mice. J Exp Med; 125(2):277-88, 1967 56. Giraudel JM, Bousquet-Mélou A, Laroute V, Braun JP, Toutain PL. Involvement of Küpffer cells in plasma clearance of creatine kinase in sheep. In: Eighth International Congress of the EAPVT; 2000 July 30 - August 2; Jerusalem, Israel; 2000.