Insertion of fine bore Naso-Gastric feeding tubes in Adults.
advertisement
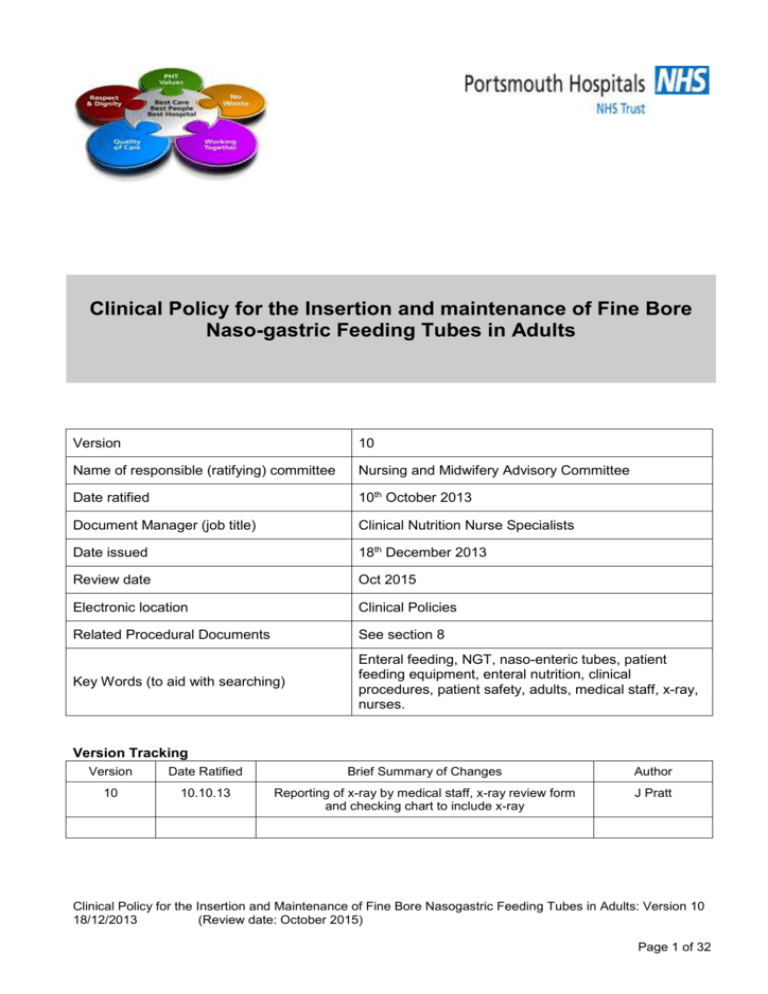
Clinical Policy for the Insertion and maintenance of Fine Bore Naso-gastric Feeding Tubes in Adults Version 10 Name of responsible (ratifying) committee Nursing and Midwifery Advisory Committee Date ratified 10th October 2013 Document Manager (job title) Clinical Nutrition Nurse Specialists Date issued 18th December 2013 Review date Oct 2015 Electronic location Clinical Policies Related Procedural Documents See section 8 Key Words (to aid with searching) Enteral feeding, NGT, naso-enteric tubes, patient feeding equipment, enteral nutrition, clinical procedures, patient safety, adults, medical staff, x-ray, nurses. Version Tracking Version Date Ratified Brief Summary of Changes Author 10 10.10.13 Reporting of x-ray by medical staff, x-ray review form and checking chart to include x-ray J Pratt Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) Page 1 of 32 CONTENTS Quick Reference Guide…………………………………………………………………….…………3-4 1. Introduction………………………………………………………………………………………………...5 2. Purpose…………………………………………………………………………………………………….5 3. Scope……………………………………………………………………………………………………….5 4. Definitions…………………………………………………………………………………………………..6 5. Duties and Responsibilities………………………………………………………………………… …7-8 6. Process …………………………………………………………………………………………… 8-16 7. Training Requirements……………………………………………………………………………………..16 8. References and Associated Documentation ……………………………… …17 9. Equality Impact Assessment…………………………………………………………………………….17 10. Monitoring Compliance ………………………………………………………………… ….18 APPENDICES: 1. Indications, Contraindications and Considerations……………………………………… …………....19 2. Anatomy and Physiology of swallowing...……………………………………………………………....20 3. Finebore nasogastric tube insertion (Adults) Flowchart……………………………………………….21 4. NG X-ray review form…………………………………………………………………………………..…22 5. NG Insertion and Checking Chart ….…………………………………………………………………. 23 , 6. NG Competency………………………………………………………………………….. .. 24, 25, 26, 27 7. Product and ordering information……………………………………………………………………......28 8. NG Feeding starter regime……………………………………………………………………....29, 30, 31 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) 2 QUICK REFERENCE GUIDE This policy must be followed in full when developing or reviewing and amending Trust procedural documents. For quick reference the guide below is a summary of actions required. This does not negate the need for the document author and others involved in the process to be aware of and follow the detail of this policy. The quick reference can take the form of a list or a flow chart, if the latter would more easily explain the key issues within the body of the document This policy must be followed in full when developing or reviewing and amending Trust procedural documents. For quick reference the guide below is a summary of actions required. This does not negate the need for the document author and others involved in the process to be aware of and follow the detail of this policy. 1. Before a decision is made to insert a nasogastric tube, an assessment is undertaken to identify if nasogastric feeding is appropriate for the patient, and the rationale for any decisions is recorded in the patients medical notes 2. Nasogastric feeding tubes should be used for short-term (4-6 weeks) enteral feeding in patients with a functioning gastrointestinal tract. 3. Nasogastric tubes used for feeding, medication and fluid administration should be radioopaque throughout their length and have externally visible length markings. 4. NG tube insertion must be documented in the patients’ notes and on the NG checking chart at the bedside. 5. Aspirate with a pH of 4.5 or below should be obtained to confirm gastric placement prior to using the tube. 6. NG tubes must not be flushed or have anything introduced into them until gastric placement has been confirmed. Internal guidewires must not be flushed with water prior to insertion 7. NG tubes should be checked (using the pH aspirate test) at the bedside for correct position prior to each use, if there is any indication that the NG tube may have moved, and at least every 24hrs when in continuous use. This is to be documented on the checking chart. 8. Do not use sterile water to flush NG tubes as this has a pH of 4.5 and could lead to a false positive pH reading. Drinking tap water should be used. 9. X-ray should only be used on initial insertion if aspirate obtained has a pH of above 4.5 or if aspirate cannot be obtained. 10. Before requesting an x-ray ward staff should contact the Nutrition Nurse team to review the patient (0900 – 1600 hrs, Mon-Fri). 11. If x-ray is required to check NG tube position this should be requested between the hours of 0800 – 16.00 (Mon to Fri). 12. Between 0800 -16.00 hrs (Mon to Fri) radiology will report the x-ray direct onto PACS and remove any NG found to be in the lung whilst the patient is in the x-ray department. 13. Ward clinician must review the PACS report and document in the patient’s medical notes that the NG tube is safe to be used for feeding, prior to the NG being used. 14. If x-ray required after 1600 hrs(Mon –Fri), or at weekends, the referring clinical team Consultant/Registrar must be available to review the x-ray and document in the patients medical notes that the NG tube is within the stomach and safe to use for feeding. If the NG is Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) 3 found to be in the lung it must be removed immediately. Consultant/Registrar must have completed the on-line NG x-ray training available through ESR. 15. Patients who repeatedly displace NG tubes should be referred to the CNNS team for assessment for a nasal bridle to prevent displacement. . Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) 4 1. INTRODUCTION Nasogastric tube feeding is common practice and many tubes are inserted daily without incident. However, there is a small risk that the tube can become misplaced into the lungs during insertion, or move out of the stomach at a later stage (1, 4). Auscultation must not be used to check correct nasogastric tube (NGT) placement as studies have shown this method to be inaccurate. NG tubes should be aspirated and the tube position confirmed using pH indicator strips that are CE marked and intended for use on human gastric aspirate (12). X –ray should not be routinely used but is required on NG insertion if the pH test has failed to confirm gastric placement (no aspirate or pH >4.5) (1, 10, 12). If an x-ray is required the film must be interpreted by a competent clinician and confirmation of correct position must be documented in the patients medical notes before the NG is used. NG tubes must not be flushed or have anything introduced into them until gastric placement has been confirmed. Internal guidewires must not be flushed with water prior to insertion (13). 2. PURPOSE This policy is designed to guide all Healthcare Professionals in the safe insertion and maintenance of fine bore naso-gastric feeding tubes in adults. . 3. SCOPE This policy applies to all competent Healthcare Professionals inserting and/or maintaining fine bore naso-gastric feeding tubes in Adult patients in Portsmouth Hospitals NHS Trust. They are applicable to adult patients who require short term (4-6 weeks) feeding via a fine bore naso-gastric feeding tube. For administration of medication via a fine bore naso-gastric feeding tube please refer to Administration of Drugs to Adult Patients with Feeding Tube guidelines (12)Administration of Medicine Policy For the administration of Enteral feed via a fine bore naso-gastric feeding tube please refer to Enteral Tube Administration Policy (Adults). Enteral Tube Administration Policy (Adults) For fine/wide bore naso-gastric feeding tubes or orogastric feeding tubes inserted other than at the bedside (ie endoscopy, imaging, and theatres) this policy should be adhered to for the verification of tube position. NG tubes that are placed under direct visualisation or palpation must still be checked using the pH aspirate test prior to use (or x-ray if pH is above 4.5) as there is a risk that the tube may have moved subsequent to placement or that the tip of the tube may be in the oesophagus rather than the stomach. The Department of Critical Care is responsible for producing its own specialty specific guidelines to Trust standards. ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) 5 4. DEFINITIONS Fine bore naso-gastric feeding tube:Defined as between a 6 – 8 french gauge. The length of the tube is measured in cms starting at the distal tip (stomach end = “0” cms). The tube is made of silicone or polyurethane which is passed through the nostril via the naso-pharynx into the oesophagus, then stomach. (See Process 6A). Nasogastric tubes used for the purpose of feeding must be radio-opaque throughout their length and have externally visible length markings(12). In this Trust a Merck Corflo 8fg, 92cm, fine bore feeding tube is the tube of choice as it has easily identifiable cm markings and is radio-opaque along its length without the guidewire insitu. Naso-gastric feeding:The administration of artificial nutrition via a fine bore naso-gastric tube. Feeding via a nasogastric tube is usually a short- term intervention (4-6 weeks). A route for permanent enteral access should be considered if enteral support is required for longer than this. Healthcare Professionals:A registered or trained competent member of staff including (doctors, nurses and midwives.) Competency level 2 and above (Appendix 4). Competence:Competence and competences are job related, being a description of an action, behaviour or outcome that a person should demonstrate in their performance. Competency and competencies are person orientated, referring to a person’s underlying characteristics and qualities that lead to effective/superior performance in their job. . Maintenance of a Naso-gastric tube:Including correctly checking tube position, and maintaining the patency of that tube. Ongoing management including skin care, checking tube position. (See Process 6C) Enteral Syringes:Purple single use non I.V. compatable syringes for enteral use only. Available as female luer slip and catheter tip. PH Aspirate test: Fluid obtained from the stomach via the NGT using an enteral syringe. Aspirate is then checked for pH using indicator strips. PH 4.5 or below indicates gastric placement. Blackcurrant Test: If swallow is intact ask patient to drink 200mls blackcurrant, or other acidic fluid such as lemon or orange squash, and attempt to aspirate via NGT. Aspirate is tested for pH and should be 4.5 or below as an acidic drink has been consumed. Not to be used on dysphagic patients or patients with oespohageal stricture/obstruction. Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) 6 5. DUTIES AND RESPONSIBILITIES Medical Staff:The decision to commence artificial nutrition via a naso-gastric tube is a medical decision to be made in conjunction with the patient, the patients’ family and members of the MDT. Before a decision is made to insert a nasogastric tube, an assessment is undertaken to identify if nasogastric feeding is appropriate for the patient, and the rationale for any decisions is recorded in the patients medical notes (12) Medical staff are responsible for requesting an x-ray to verify the position of a nasogastric tube where aspiration of the tube has failed to verify gastric placement (pH > 4.5 or no aspirate). The x-ray form must clearly state that the purpose of the x-ray is to establish the position of the nasogastric tube for the purpose of feeding(12). 0800 – 1600 hrs (Mon – Fri) : medical staff are responsible for reviewing the x-ray on PACS and documenting in the medical notes that the NG tube is within the stomach and safe to use for feeding. If an x-ray is required to verify NG tube position after 1600 hrs, or at weekends, the referring clinical team Consultant/Registrar must be available to review the x-ray and document in the patients medical notes that the NG tube is within the stomach and safe to use for feeding. If the NG is found to be in the lung it must be removed immediately. Consultant/Registrar must have completed the online NG x-ray training through ESR “Reducing the risk of feeding through a misplaced feeding tube”(search “nasogastric”). The x-ray report should state the following and all 4 criteria should be met in order to correctly identify the NGT as being in the stomach: 1. The NGT follows the oesophagus and avoids the contours of the bronchi 2. The NGT clearly bisects the carina or bronchi 3. The NGT crosses the diaphragm in the midline 4. The NGT tip is clearly visible below the left hemi-diaphragm Radiology Department: Radiographers:- are responsible for ensuring that the nasogastric tube can be clearly seen on the x-ray to be used to confirm tube position. Radiology Consultant/Registrars or Advanced Practitioner Radiographers(with suitable training) are responsible for reporting x-ray films onto PACS between the hours of 0800 -16.00 hours Mon to Fri. Any tube found to be in the lung will be removed immediately by the person reporting the image whilst the patient is in the x-ray department. The x-ray report should state the following and all 4 criteria should be met in order to correctly identify the NGT as being in the stomach: 1. The NGT follows the oesophagus and avoids the contours of the bronchi 2. The NGT clearly bisects the carina or bronchi 3 The NGT crosses the diaphragm in the midline 4 The NGT tip is clearly visible below the left hemi-diaphragm Healthcare Professionals (including Registered Nurses) Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) 7 It is expected that fine bore naso-gastric tubes will be inserted and maintained by a level 2 and above practitioner in a safe and competent manner (Appendix 4) and in accordance with this Policy. Healthcare Professionals are responsible for establishing the gastric placement of NGTs prior to their use and to document this using the NG checking chart. It is the responsibility of the Healthcare Professional to develop and maintain their own level of competency (Appendix 4). Clinical Nutrition Nurse Specialists(CNNS): CNNS team will provide support to clinical areas in the insertion and management of finebore nasogastric feeding tubes between 0900 hrs and 1600 hrs, Monday – Friday. X-ray requests to verify NG tube position will be notified to the CNNS team who will review the patient prior to x-ray. If a pH of 4.5 or below is gained the CNNS will cancel the x-ray request (Mon-Fri 0900-1600 hrs). CNNS team are responsible for the development and review of this policy. CNNS team are responsible for providing training and education to PHT staff on the insertion and management of finebore nasogastric feeding tubes. Clinical Nutrition Nurse Specialists in conjunction with Modern Matrons, Ward Managers, Practice development Nurses and Clinical Educators are responsible for the management and implementation of this policy. 6. PROCESS Insertion of fine bore Naso-Gastric feeding tubes in Adults. List of Equipment for Procedure:Clean Tray or trolley 1 x Corflo 8 fg, 92cm, nasogastric tube 1 x glass of drinking tap water and straw 1 x 10ml enteral syringe filled with drinking tap water 1 x 50ml enteral syringe Bioclusive / Hypafix Merck Serono pH Indicator strips 0-6 ACTION RATIONALE EVIDENCE 1. Explain procedure to patient. To obtain patients consent and cooperation. 1,2, 2. If patient does not have capacity to consent to treatment a best interests decision must be made To ensure NG insertion is in the patients best interests. 17 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) 8 How to insert the NG tube 2a. Where possible the patient should be sitting in a semiupright position supported with pillows. This position allows easy swallowing and ensures that the epiglottis is not obstructing the oesophagus. Appendix 2. 2 2b. For the semi-conscious patient it is often easier to be in a lying position. 3. Wash hands and apply gloves. Assemble required equipment, select appropriate tube. To ensure a clean procedure is maintained throughout. Consider fg required depending on diagnosis. 4. Check nose and mouth for any signs of obstruction and ensure both are clean. To aid passage of NGT Check nasal patency by sniff with each nostril occluded in turn. Patient may have one nostril which is clearer than the other e.g. deviated nasal septum. 5. Check that the guidewire moves freely and then secure the guidewire into the end of the NG tube. Close the purple port on the NG tube. To aid correct insertion of tube and to be able to aspirate tube post insertion Manufacturers guidelines. 1 6. Lubricate the NG tube by immersing end of tube in drinking tap water. This will facilitate easy passage when inserting the tube. Sterile water has a pH of 4.5 and its use may lead to a false positive pH reading. Drinking tap water has a pH of > 5 1,2 2. Insert the tube into the clearest nostril and slide backwards and inwards along the floor of the nose to the nasopharynx approx 10-12cm and STOP If any obstruction is felt withdraw tube slightly and try again at a slightly different angle. There are two distinct stages when passing the tube. 8a. If the patient can swallow coincide passing NGT with swallowing a sip of drinking tap water. The passing of the NGT can be coordinated with observing for laryngeal movement. During this phase the epiglottis covers the airway and NGT 2 a. Nose → pharynx → stop and swallow b. Pharynx → stomach. 2 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) 9 can pass into oesophagus. 8b. If the patient is dysphagic but can swallow own secretions- trickle 1-2 mls of drinking tap water into the mouth using a syringe To elicit a swallow. Repeat the water/swallow and advance tube to 50-60cms. If swallow reflex is not initiated DO NOT continue with this method. Risk of aspiration. 8c. If the patient is dysphagic and unable to swallow secretions or the above fails, attempt to pass the tube unaided to 50-60cms. This reduces the risk of aspirating fluids. NB Advance chin forwards and/or turn head to one side. May facilitate tube advancement 9. If you are unsuccessful repeat above procedure in other nostril. Consider smaller bore and/or unweighted tube. Do not repeat procedure more than 3 times. One nostril may be clearer than the other. Smaller gauge or unweighted tube may be easier to pass on specific patients. 10. Once at appropriate measurement secure nasogastric tube in place using hypafix/bioclusive across side of face. Do not apply tape to the nose. T o prevent displacement of tube post insertion 18 Mark NGT with pen at point of entry into nostril. This will provide an easily identifiable mark as a baseline 4,14 DO NOT INSERT ANY FLUID INTO THE TUBE GASTRIC PLACEMENT HAS NOT YET BEEN CONFIRMED 12,13 11.How to verify the position of the NG tube A. Using a 50ml enteral syringe aspirate the NGT by withdrawing plunger on syringe and test the pH using Merck Serono pH indicator strips0-6. The pH of aspirate should be measured using pH indicator strips in the range 06 with ½ point gradations. Merck Serono pH indicator strips are CE marked and intended for use on human gastric acid. Litmus paper must not be used as it does not indicate the degree of acidity. 1,10, 12 3,10 PH aspirate result: Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: 10 Version 10 18/12/2013 (Review date: October 2015) - pH of 4.5 or below means that the NG is safe to use. X-ray is not required. Flush NG tube with 10mls of drinking tap water and remove guidewire Proceed to step 17 below. A pH of 4.5 and below (acid) indicates gastric placement. . Flushing of the NG tube will aid removal of guidewire. NG tube should only be flushed once gastric placement has been confirmed 10 Manufacturers guidelines 13 - If unable to obtain aspirate or pH above 4.5 do not use the NG tube. Follow steps 12, 13 and 14 below. Gastric placement of NG tube has not been confirmed and it is unsafe to use the NG tube 12.If unable to obtain aspirate or pH is above 4.5 try the following: This clears tube of debris and forces the end of the tube away from the stomach mucosa. 6,8 Tip of tube may not be in fluid pool in the stomach- advancing tube should enable aspirate to be obtained as tip of tube should be in gastric fluid pool. 3 Withdrawing tube should allow aspirate to be obtained-by putting tip of tube in gastric fluid pool. 3 A. Inject 20ml of air into the NG tube A. Consider length of NGT. If measurement at nose is 50 55cm consider advancing tube 5-10cms. B. If measurement at nose is above 60 – 65 cm consider withdrawing tube 5-10cms. C. Consider changing the patients position e.g. from sitting to lying, or lying on side. D. If aspirate obtained and pH 4.5 or below then the tube is safe to use. X-ray is not required. Flush NG tube with 10mls of drinking tap water and remove the guidewire. Proceed to step 17. To change the fluid level in the stomach-as this may enable aspirate to be obtained. 2,3,6 . A pH of 4.5 and below (acid) indicates gastric placement 10 Flushing of tube will aid removal of the guidewire. NG tube should only be flushed once gastric placement has been confirmed Manufacturers guidelines 13 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: 11 Version 10 18/12/2013 (Review date: October 2015) 13. If still unable to obtain aspirate or ph is above 4.5 AND ONLY IF THE PATIENTS SWALLOW IS SAFE.: A. Ask patient to drink 200mls of blackcurrant ORALLY. Blackcurrant should then be in the patients’ stomach. 10 B. Using a syringe attempt to gain aspirate from NGT. If tip of NGT is in gastric fluid pool blackcurrant will be aspirated. 10 C.If aspirate is obtained- check the Ph using Merck Serono pH indicator strips0-6 PH of aspirate should be 4.5 or below as blackcurrant is acidic. D. If aspirate obtained and pH 4.5 or below then the tube is safe to use. X-ray is not required. Flush NG tube with 10mls of drinking tap water and remove the guidewire. Proceed to step 17. A pH of 4.5 and below (acid) indicates gastric placement DO NOT USE THIS METHOD UNLESS PATIENTS SWALLOW IS SAFE. It is not safe to ask patient to drink if swallow is NOT intact. DO NOT USE ON PTS WITH OESOPHAGEAL STRICTURE OR CA OESOPHAGUS. The NG tube may be sitting above the stricture /tumour. Fluid taken orally may pool above the stricture/tumour and lead to a false positive pH aspirate test: pH 4.5 or below but NG tube is actually in oesophagus and unsafe to use 14 In the absence of a positive aspirate test contact the CNNS team for review before requesting an x-ray. CNNS team may be able to obtain aspirate of pH 4.5 or below and x-ray will not be required. 15. If after following steps 11 14, a positive aspirate test cannot be obtained an x-ray will be required to verify the position of the NG tube prior to its use. On initial insertion only- x-ray will provide confirmation of position and a baseline from which to base ongoing clinical judgments on whether the NG is safe to use. 10 The x-ray form must clearly state that the purpose of the xray is to establish the position of the nasogastric tube for the purpose of feeding X-ray need to know this as a specific density is required – on a standard chest x-ray the tube may not be visible and the x-ray may not go down far enough to see the tip of the NG tube. 8, 12 Flushing of tube will aid removal of the guidewire. NG tube should only be flushed once gastric placement has been confirmed 10 Manufacturers guidelines 13 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: 12 Version 10 18/12/2013 (Review date: October 2015) 16. i X-ray 0800 - 1600 hrs(MonFri) NPSA alert 2011/PSA 0002: main causal factor in the use of misplaced NG tubes was misinterpretation of x-ray 12 a.Radiology will report x-ray direct onto PACS b.If tube is in lung it will be removed in x-ray dept To provide documentation in the patients medical notes that the tube is safe to use c.Post x-ray the ward Doctor must review the x-ray report on PACS and document in the patients medical notes that the NG tube is safe to use for feeding, before it is used. X-ray 1600 – 0800 hrs, or at weekends a.Defer x-ray unless a competent clinician is available to interpret the x-ray Evidence from Never Events reports suggest that there are increased risks with x-ray checking at night due to a lack of senior support. 12 b. Competent Consultant/Registrar must interpret the x-ray and remove the NG tube if it is in the lung c. Consultant/Registrar must document in the patients medical notes that the tube is within the stomach and safe to use prior to use 16. ii If you have not been able to obtain any aspirate prior to xray you will need to flush the NG with 10mls of drinking tap water and then remove the guidewire once x-ray has confirmed correct position of the NG tube. . To ensure patient safety In order to remove the guidewire the lubricant within the tube must be activated by fluid. The NG tube must not be flushed until gastric placement has been confirmed Manufacturers guidelines 13 1 17. Document the insertion procedure in the patients medical notes. This should include: - date and time - patient consent - type of tube used -nostril tube inserted into -length of tube at nostril -outcome of aspiration test -if tube is safe to use or not and further actions required Recording the procedure is a requirement in law and provides a baseline for further measurement Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: 13 Version 10 18/12/2013 (Review date: October 2015) Implement NG tube checking chart (Appendix 4) at bedside. To ensure documentation of NG position checks. 12 6A Ongoing checking of NG tube position As the healthcare professional caring for the patient with an NGT it is your responsibility to ensure the tube is in the correct position. i) Tube position should be checked by aspiration and documented on the NG checking chart:- ACTION RATIONALE EVIDENCE 1. Each bolus feed or drug administration. 2. At least once every 24 hrs when continuous feeds are used. 3. If the patient complains of discomfort or feed reflux into the mouth. 4. After vomiting or violent retching. 5. After severe coughing bouts / respiratory distress. To confirm correct position prior to use. 1 To ensure tube has not displaced. 1,4 To ensure tube has not displaced. Tube may be coiled in back of throat. 1,4 To ensure tube has not displaced. To ensure tube has not displaced. Check back of throat to ensure that tube is not coiled. To ensure tube has not displaced. 1,4,6 1,4,6,10 To ensure tube has not displaced. 1 6. After endotracheal or tracheostomy tube suctioning. 7.If tube has obviously displaced on checking measurement. 8. Following a patient slip/trip/fall To ensure tube has not displaced 9.On return to the ward if the patient has been for an investigation or procedure 10. On receipt of patient being transferred prior to using tube. To ensure tube has not displaced To ensure tube has not displaced. 1,6 1 ii)Tube position should be monitored by visual check of measurement at nostril and documented on NG checking chart:- ACTION 1. On changing a bag of feed if patient on continuous feeding 2.On administration of medication if patient on continuous feeding 3. When moving/turning/transferring the patient if on continuous feeding 4. Every 8 hours if none of the above occur RATIONALE To ensure tube has not displaced EVIDENCE To ensure tube has not displaced To ensure tube has not displaced To ensure tube has not displaced If any of the visual checks indicate that the tube has moved then an aspiration test must be carried out and gastric position confirmed as for tube insertion. Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: 14 Version 10 18/12/2013 (Review date: October 2015) 6B Problem solving for Ongoing NG Checking (not to be used on placement of NG) It is recognized that obtaining aspirate for ongoing checking may at times be difficult. In the absence of aspirate pH 4.5 or below a clinical decision should be made as to whether the tube is safe to use in conjunction with the NG checking chart. A level 2 practitioner may need to refer to a Level 3 or 4 practitioner for advice. The following is provided to assist in your decision making. Follow the guidance below ONLY for NGTs that have previously been confirmed to be in the correct position by pH aspiration test/x-ray. ACTION 1. Check that a level 2 practitioner has followed the process for tube verification on insertion (above). 2. Review NG checking chart: 3. Obtain patient history: Check measurement at nose, has patient vomited, violently coughed, or complained of feed reflux? Look in patients mouth to check if tube is coiled at back of throat 4. If patient has an intact swallow use the blackcurrant test. 5. Only if tube position has not moved and pt has not vomitted, inject 5/10mls of drinking tap water into NG tube. Attempt to re-aspirate using a 20ml enteral syringe. 6. Contact the Nutrition Nurses for advice EVIDENCE RATIONALE To ensure correct procedure has been followed on initial insertion. To aid clinical judgment and guide decision whether tube is safe to use To check if tube has moved. To ensure tube has not displaced. If measurement is the same at the nose, no vomiting or violent coughing, tube not coiled in throat - assume tube position is unchanged. If tip of tube is in stomach blackcurrant will be aspirated via the NGT and can then be pH tested. This has been shown to ease the procedure for obtaining aspirate. Do not use sterile water as this has a pH of 4.5 and could lead to a false positive result 1 10 3 6C. Ongoing Management Skin Care:ACTION DAILY Check that tape securing tube is To ensure tube is safely intact and not in need of secured in position. replacement. Check around nostril for any signs of pressure necrosis. An adverse incident form needs EVIDENCE RATIONALE 18 Tape may need to be changed to secure tube in a different position. Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: 15 Version 10 18/12/2013 (Review date: October 2015) to be completed if any pressure necrosis is found 18 Tape should be placed across patients cheek To safely secure tube in position If patient is NBM ensure mouth care is maintained 2 hourly. To ensure oral hygiene is maintained reducing risk of infections. Maintaining Patency:ACTION RATIONALE Flush tube with 30ml-50mls water before and after feed using a 50ml enteral syringe. To ensure tube does not become blocked. If fluid restricted may need to reduce these amounts. To ensure fluid in 24hr period does not exceed restrictions. EVIDENCE 4,7 If continuous feeding flush every 4-6 hrs. Where possible medications should be given in liquid / dispersible form. To aid administration of medication via the NG. 4,7,18 If feed in progress tube MUST be flushed with water prior to giving medications via the tube. To reduce the risk of tube blockage. 4,7,18 Medications to be given individually with a water flush in between To reduce the risk of tube blockage 4,7,18 Flush tube with water at end of medications and prior to recommencing feed. To reduce the risk of tube blockage 4,7,18 Administration of Medicine Policy 7. TRAINING REQUIREMENTS It is expected that fine bore naso-gastric tubes will be inserted and maintained by a level 2 and above practitioner in a safe and competent manner (see Appendix 4: NG Competency, also available on learning and development pages (intranet) Departmental/Specialty Competencies: Care of fine bore NG tube). Ward Managers, Clinical Educators and Modern Matrons are to ensure staff are aware of Policy and that it is adhered to at ward level. Ward managers are responsible for ensuring staff complete competency to required level CNNS to maintain a high profile in clinical areas to support implementation of this policy. Teaching by CNNS team: Patient Safety Day; RN Induction; NG Workshops; Nutrition Champion Day; Nutrition Support Study Day; ward teaching. Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: 16 Version 10 18/12/2013 (Review date: October 2015) CNNSs to provide training on Preceptorship, RN Induction, Patient Safety Day, Nutrition Champion Study Days and Artificial Feeding Study Days. Specific training also provided as required by individual ward areas. 8. REFERENCES AND ASSOCIATED DOCUMENTATION 1. Stroud, M. Duncan, H & Nightingale, J. (2003) Guidelines for Enteral Feeding in Adult Hospital Patients. Gut, 52 (suppl. Vii), Vii-Vii 12. 2. Burham,P. (2000). A Guide to Nasogastric Tube Insertion. Nursing Times Plus 96 (8), 6-7. 3. Reid, W. (2002. Clinical Governance: Implementing a Change in Workplace Practice. Nasogastric Tube Placement. Professional Nurse, 17 (12), 734-737. 4. Cannaby, A. Evans, L. & Freeman, A. (2002). Nursing Care of Patients with Nasogastric Feeding Tubes. British Journal of Nursing, 11 (6), 366-372. 5. Chrestiensen, M. (2001). Bedside Methods of Determining Nasogastric Tube Placement: A literature Review. Nursing in Critical Care 6(4), 192-199. 6. Colagiovanni, L. (1999) Taking the Tube. Nursing Times 95 (21), 63-71. 7. Colagiovanni, L. (2000). Preventing and Clearing Blocked Feeding Tubes. Nursing Times Plus, 96 (17), 3-4. 8. Ellett, M.L.C. (2004). What is known about methods of correctly placing gastric tubes in adults and children? Gastroenterology Nursing, Vol 27 (6) 253-259. 9. Metheny, n. & Tiler, M.G. (2001). Assessing Placement of Feeding Tubes. American Journal of Nursing, 101 (5), 36 – 45 10. Great British National Patient Safety Agency (2005). Reducing the harm caused by Misplaced Nasogastric Feeding Tubes. 11. Great Britain. National Patient Safety Agency (2007). Promoting safer measurement and administration of liquid medicines via oral and enteral routes. 12. Great Britain. National Patient Safety Agency (2011). PSA002: Reducing the harm caused by misplaced nasogastric feeding tubes in adults, children and infants. 13. Great Britain. National Patient Safety Agency (2012). Rapid Response Report NPSA/2012/RRR001: Harm from flushing of nasogastric tubes before confirmation of placement. 14. Portsmouth NHS Trust (2005). Administration of Drugs to Adult Patients with Feeding Tubes. Drug Therapy Guideline No 52.01, p1-25. 15. Metheny, N. et al. (2005) Indicators of Tubesite during Feedings. Journal of Neuroscience Nursing, 37 (b), 320-325. 16. Taylor, S & Clemente, R. (2005). Confirmation of nasogastric tube position by pH testing. Journal of Human Nutrition and Dietetics, 18, 371-375. 17. Great Britain. National Institute for Health and Clinical Excellence. (2006). Nutrition Support in Adults (Clinical Guideline 32) London: NICE. 18. Pickering, K. (2003). The administration of drugs via enteral feeding tubes. Nursing Times. 99 (46) 46-48. 19. Portsmouth NHS Trust (2010). Consent to examination or Treatment Policy. 9. EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly All policies must include this standard equality impact statement. However, when sending for ratification and publication, this must be accompanied by the full equality screening assessment tool. The assessment tool can be found on the Trust Intranet -> Policies -> Policy Documentation Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: 17 Version 10 18/12/2013 (Review date: October 2015) 10.MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS This document will be monitored to ensure it is effective and to assurance compliance. Minimum requirement to be monitored On insertion NG position is confirmed as per policy Lead Jo Pratt Tool Audit Data collection Frequency of Report of Compliance 2 years Reporting arrangements Policy audit report to: Lead(s) for acting on Recommendations Jo Pratt Nutrition Support Team Correct use of NG checking charts NG tubes are checked at least daily X-ray is only performed on insertion when aspirate of 4.5 or below cannot be obtained X-ray taken between 0800 -1600, Mon to Fri, are reported onto PACS by radiology Jo Pratt Jo Pratt Audit Data collection 2 years Audit Data collection 2 years Policy audit report to: Jo Pratt Nutrition Support Team Policy audit report to: Jo Pratt Nutrition Support Team X-ray taken after 1600, or at weekends, are interpreted by a competent Consultant or Registrar from the patients referring clinical team NG tubes are removed immediately if found to be in the lung on x-ray Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 Page 18 of 32 (Review date: October 2015) APPENDIX 1: A INDICATIONS Indication for feeding Unconscious patient Swallowing disorder Physiological anorexia Upper GI obstruction Partial intestinal failure Increased nutritional requirements Psychological problems GI, gastrointestinal: Example Evidence Head injury, ventilated patient Post-CVA, multiple sclerosis, motor neurone disease. Liver disease (particularly with ascities) Oesophageal stricture Postoperative ileus inflammatory bowel disease, short bowel syndrome. Cystic fibrosis, renal disease, critical illness Severe depression or anorexia nervosa Cerebrovascular accident. 1. B CONTRADINDICATIONS Fractured Base of skull Bleeding Oesophageal Varices Perforated oesophagus Perforated pharyngeal pouch C CONSIDERATIONS NGT insertion may be problematic if the patient is known to have: Head & Neck malignancy/obstruction Upper Gastrointestinal Malignancy/obstruction/surgery i.e. Gastrectomy Pharyngeal pouch Hiatus Hernia Fractured cervical spine COMPLICATIONS Type Complication Insertion Nasal damage, intracranial insertion, pharyngeal/oesophageal pouch perforation, bronchial placement, variceal bleeding. Post insertion trauma Discomfort, erosions, fistulae, and strictures. Displacement Reflux Tube falls out, bronchial administration of feed. *See below. Potential aspiration pneumonia. GI intolerance Oesophagitis, aspiration Metabolic Nausea, bloating, pain, diarrhoea. Refeeding syndrome, hyperglycaaemia, fluid overload, electrolyte disturbance. Evidence 1. *In a patient with a functioning Gastro-Intestinal Tract, who repeatedly displaces NGTs it may be possible to insert a nasal retaining loop which will prevent displacement (See Nasal Retaining Loop guideline). Nasal Retaining Loop guideline Please contact the Clinical Nutrition Nurse Specialist. Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) APPENDIX 2: ANATOMY AND PHYSIOLOGY OF SWALLOWING Upper Oesophageal sphincter contracted (a) Upper Oesophageal sphincter contracted Pass NG tube into pharynx Upper Oesophageal sphincter relaxed (b) Upper Oesophageal sphincter relaxed When patient swallows upper Oesophageal sphincter relaxes, epiglottis closes over trachea sealing off airway, therefore NG tube more likely to pass into Oesophagus. Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 2015) (Review date: October Appendix 3 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) Name Appendix 4 D.O.B. Hospital Number Ward Nasogastric tube X-ray review form Date of x-ray………………….. Time of x-ray ……….. Part A: to be completed if x-ray has been taken Mon –Fri 0900-1600 and has been reported onto PACS This is the most recent CXR for this patient. I have read the PACS report. YES / NO YES / NO The NG tube is within the stomach and safe to use for feeding. YES / NO If NG is not in stomach and /or unsafe to use state action taken:…………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… Part B: to be completed if x-ray taken after 1600 hrs Mon-Fri or at the weekend. This is the most recent CXR for this patient. YES / NO The x-ray meets the following 4 criteria: 1. NGT follows the oesophagus and avoids the contours of the bronchi 2. NGT clearly bisects the carina or bronchi 3. NGT crosses the diaphragm in the midline YES / NO YES /NO YES / NO 4. NGT tip is clearly visible below the left hemi-diaphragm YES / NO If the above criteria are not met you should seek senior review before deciding if the NG is safe to use or not. The NG tube is in the stomach and safe to use for feeding. YES / NO If NG is not in stomach and /or unsafe to use state action taken…..................................... ………………………………………………………………………………………………………. ………………………………………………………………………………………………………. Note: if NG is in the lung it must be removed immediately PHT policy is that Registrars and Consultants, who have completed the online NG x-ray training, should interpret x-rays to confirm NG position. Form completed by:…………………………… Sign:……………………………… Designation: ………………………………… Date:…………………................. Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) Appendix 5 NG TUBE INSERTION AND CHECKING CHART Adult Patients Name: D.O.B POSITION OF NG TUBE MUST BE CHECKED ON INSERTION AND THEN DAILY IF CONTINUOUSLY FEEDING OR BEFORE EACH USE IF INTERMITTENTLY FEEDING Hospital Number: Ward; Please document on chart a visual check of cm measurement at the tip of the nose every 8 hours Date Time New NGT Insertion Y/N Length of NGT in cms at tip of nose PH of aspirate Is x-ray needed Did x-ray confirm NG is in stomach? Y/ N Y/ N/ NA (NG safe to use if pH 4.5 or less) pH No aspirate Is the NGT safe to use? Y/ N Use this box to explain the reasons for your decision If pH is above 4.5 the NGT must be x-rayed prior to use: on insertion, if pt vomits, or if NGT moves out at the nose. Sign and print name and designation *Do not use blackcurrant test if patient has an unsafe swallow or Oesophageal stricture/Ca. If unsure seek senior guidance and refer to policy for The Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults. Contact CNNS on ext 5918 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) Appendix 6 Name: APPENDIX 5: NG Competency Competency Statement: Care of a patient with a fine bore Naso-gastric feeding Tube 1.1. Competency Indicators Achieved Assessor Signature Competency Indicators 2nd Level 1st Level After obtaining consent from the patient (as appropriate) a) Understands the implications of having an NG tube from a patient perspective b) Assist healthcare professional with the insertion of NG tube as per NG Policy c) Has knowledge of and acts in accordance with enteral administration policy d) Records information /intervention accurately in patient record e) Completes MUST score on admission and weekly thereafter f) Report significant changes to trained nurse, e.g tube moved at nose, pt vomiting, pump alarming. g) Provide information to patients, relatives and significant others regarding care provided h) Maintain patient comfort and a) b) c) d) e) After obtaining consent from the patient (as appropriate) Level 1+ Has an understanding of ethical issues surrounding enteral tube feeding. Demonstrates knowledge of complications associated with NG insertion and maintenance Following medical /MDT decision is able to insert NG tube as per Policy On insertion is able to check NG position and document as per policy prior to use. Maintains pt safety by checking NG Achieved Assessor Signature Competency Indicators 3rd level After obtaining consent from the patient (as appropriate) Level 1 and 2+ a) Manage and ensure that all nutritional interventions are provided by the appropriate Health Care Professional in accordance with Trust Policies. b) Ensure clinical area has appropriate equipment pertaining to NG insertion and feeding. c) Lead multidisciplinary discussion involving patient, relative and significant others, Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 Achieved Assessor Signature Competency Indicators 4th level After obtaining consent from the patient (as appropriate) Level 1, 2 and 3+ a) Act as a resource to support and lead the multidisciplinary team in the planning of further treatment and intervention. b) Member of Nutrition Support Team and Nutrition Support Group c) Undertake audit, set Trust wide standards and policies for the care of the patient with a fine bore feeding tube. d) Lead regular (Review date: October 2015) Achieved Assessor Signature i) j) safety e.g skincare. Knows how to access and maintain supplies at ward level, e.g ordering feed, admin sets, enteral syringes, NG tubes ,indicator strips and feeding pumps Attends appropriate training position as per policy, e.g daily if on continuous feeding, before each use if intermittent. f) Competently uses NG checking chart to document tube position g) Has received training on and can competently use enteral feeding pump h) Demonstrate ability to maintain tube patency and ensure correct feed regime is administered. i) Has knowledge of and acts in accordance with Policy for the Administration of Medicines j) If competent to administer medications, is able to correctly give medicines via an NG tube. k) Is able to respond appropriately to any significant changes in the ethical issues and the appropriateness of planned intervention. d) Able to manage difficult tube insertions on a range of patients. e) Utilising experience and knowledge, manage any complications, referring to Nutrition Nurse Specialist/Nutrition Support Team as required. f) Participates in discharge planning, supporting the patient in self management g) Facilitate learning and practice development within clinical area. Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 reviews of equipment in use and update a s required e) Leads on innovation and change in response to national and organisational strategies/priorities e.g NPSA alerts, NICE Act as an expert resource, advising, teaching and supporting members of Portsmouth NHS Trust. g) Advanced clinical skills: Nasal Retaining Loop Insertion h) Coordinates and facilitates discharge for patients with NG tubes i) Management of patients in the community with NG tubes f) (Review date: October 2015) Recognises when patients require referral onto other HCP e.g Nutrition Nurse Specialist., Dietitian m) Initiate discharge planning as per Discharge Policy Education resources to support your development l) - - Policy & Guidelines for gaining Consent Policy for The Insertion and Maintenance of Fine bore Nasogastric Feeding Tubes in Adults. Enteral Administration Policy Administration of Medications Policy Discharge Policy Infection ControlPolicy CNNS webpage via intranet Access Clinical Nutrition Nurse Specialists Contact No 023 9228 6000 ext 5918 Author: Jo Pratt - PHT Artificial Feeding Study Day (bi-annual) Nutrition Champion Study Day Department: Nutrition Nurses Web Site: British Association of Enteral & Parental Nutrition (BAPEN) www.bapen.org.uk Review Date: Aug 2014 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) Record of Achievement. To verify competence please ensure that you have the appropriate level signed as a record of your achievement in the boxes below. Level 1 Level 2 Level 3 Level 4 Date Date Date Date Signature of Educator/ Trainer Signature of Educator/ Trainer Signature of Educator/ Trainer Signature of Educator/ Trainer Date: Date: Date: Date: Signature of Assessor Signature of Assessor Signature of Assessor Signature of Assessor References to Support Competency 1. Cannaby, A et al. (2002) Nursing Care of Patients with Nasogastric Tubes British Journal of Nursing 11 (6) 366-372 2. Christensen, M. (2001) Bedside Methods of Determining Nasogastric Tube Placement: A literature review. Nursing in Critical Care 6 (4) 192-199 3. Colagiovanni, L. (1999). Taking the Tube Nursing Times 95 (21) 63-71 4. Great Britain. National Patient Safety Agency (2005). Reducing the harm caused by misplaced Nasogastric Feeding Tubes. 5. Great Britain. National Patient Safety Agency (2007). Promoting safer measurement and administration of liquid medicines via oral and other enteral routes. 6. Great Britain National Patient Safety Agency (2011). PSA002: Reducing the harm caused by misplaced nasogastric feeding tubes. 7. Great Britain. National Patient Safety Agency(2012). NPSA/2012/RRR001. Rapid Response Report: Harm form flushing of nasogastric tubes before confirmation of placement. 8. .Great Britain. National Institute for Health and Clinical Excellence (2006). Nutrition Support in adults (Clinical Guideline 32) London: NICE 9. .Metheny, N., et.al. (2005). Indicators of Tube site during Feedings. Journal of Neuroscience Nursing 37 (b), 320-325. 10. Stroud, Duncan & Nightingale (2003). Guidelines for enteral feeding in Adult Hospital Patients GUT 52 (suppl. V111) V11-1 – V11-12 11.. Taylor, S. & Clemente, R. (2005). Confirmation of Nasogastric tube position by pH testing. Journal of Human Nutrition and Dietetics 18 371-375. Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) APPENDIX 7: PRODUCT INFORMATION / TUBE SELECTION / ENTERAL SYRINGES PRODUCT COST HOW TO ORDER (NHS SUPPLY CHAIN) Merck Corflo 8fg weighted NG tube £10.97 FWM 301 Merck Corflo 6fg weighted NG £10.97each FWM243 Merck Serono pH Indicator Strips 0-6 £10.07 pack (100) FWM 1216 Catheter tip 60ml enteral syringe £18.48 (box of 50) 60ml enteral syringe (female luer lock) £18.39 (box of 50) 20ml enteral syringe (female luer lock) £17.38 (box of 100) 10ml enteral syringe (female luer lock) £13.31 (box of 100) FTA189 FTA 149 FTA 156 FTA 148 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) DEPARTMENTS OF NUTRITION AND DIETETICS AND CLINICAL NUTRITION STARTER REGIMEN FOR NASO-GASTRIC TUBE FEEDING IN ADULTS The following instructions have been devised to enable competent Healthcare Professionals (level 3) to commence artificial feeding via a naso-gastric tube. Refer patient as soon as possible to the Dietitians for assessment and an individualised Feeding Regimen – see telephone extensions on page 2 or use OrderComms if you have access. The decision to commence artificial feeding is a medical decision. If a naso-gastric tube has been inserted for feeding, this document will provide a regimen until the Dietitian has assessed the patient and provided a regimen tailored to their individual needs. Do not withhold feeding until the Dietitian is available to provide a feeding regimen. The starter regimen is designed to avoid starvation and to introduce feed slowly and safely so as not to cause harm to the patient, not to meet the patients total nutritional requirements. Prior to commencement of feed you must request that the medical team review the patient to ensure there are no contraindications or special measures that may apply (for example: renal failure/congestive cardiac failure/fluid restricted patients/gastro-intestinal obstruction). You and the medical team will need to assess if the patient is at risk of Refeeding Syndrome. If the patient is at risk you must use the feeding regimen on page 3. Please see PHT Guidelines for the Prevention and Treatment of Adult Patients at Risk of Developing Refeeding Syndrome for further details. If the patient is not at risk use the regimen on page 2. If the patient is very underweight i.e. less than 40 kg you must follow the Refeeding regimen as the patient will need to be fed very small amounts to start with. The following starter regimens have been designed to be used at the end of the patient’s bed as a stand-alone document outside of this policy. Patient Experience Service Tel: 023 9228 6757 PRODUCED BY Registered Dietitians and Clinical Nutrition Nurse Specialists DATE: June 2006 REVIEWED: April 2013 REVIEW DATE: June 2014 Portsmouth Hospitals NHS Trust 1 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) Portsmouth Hospitals NHS Trust – Departments of Nutrition and Dietetics AND Clinical Nutrition NASOGASTRIC TUBEFEEDING STARTER REGIMEN FOR ADULTS Ward:…………... Name:……………..………………… DOB:.…. DATE:….. Sheet No:…….. Fluid Balance should be closely monitored. Feed should be delivered within the context of careful fluid balance with intravenous fluids being reduced or discontinued as required*. Biochemistry (within last 48 hours) should be checked before starting and regularly monitored during feeding. Recommended rates are for guidance and not to contravene medical opinion. REFER PATIENT TO DIETITIAN AS SOON AS POSSIBLE For patients 40 kg weight and over (if patient less than 40 kg use regimen for Refeeding Syndrome – see over) Date/Day number DAY 1 Feed Type Rate (ml/hour) 30 20 Duration (hours) 4 20 Volume (ml) 120 400 Water Fresubin Original DAY 2 Water 30 4 Fresubin 30 20 Original DAY 3 Water 50 4 Fresubin 50 20 Original Patient may require additional intravenous fluids* - please assess fluid balance 120 600 200 1000 Continue as Day 3 until Dietetic Review - Ensure the patient’s head is elevated to at least 30 degrees during feeding, and for one hour after feeding has stopped. Feeding tubes should be flushed before and after medication and whenever the feed is started/stopped with 30 ml water. Giving sets should be changed daily. If symptoms of intolerance occur (vomiting, abdominal distension, diarrhoea etc) – consult medical staff. If problems with tube management occur eg tube choice, insertion techniques, position check and ongoing care; please contact the Nutrition Nurses ext 5918. Further information: Policy on Insertion and Maintenance of Fine Bore Naso-gastric feeding Tubes in Adults, Clinical Guidelines, PHT Intranet. This Starter Regimen is Appendix 6 of this Clinical Policy. Marsden Manual Chapter 27 pp385-401 – Nutrition Support - located on ward and PHT Intranet. NICE Clinical Guideline 32 – Nutrition Support in Adults - (URI on PHT Intranet). 2 Drug Therapy Guideline No: 52.01 – Administration of Drugs to Adult Patients with Feeding Tubes. 3 Drug Therapy Guideline No: 46.00 – Guidelines for the Prevention and treatment of Adult Patients At Risk of Developing Refeeding Syndrome. Dietitians x 7700 6150 QAH x 7701 3720 SMH Nutrition Nurses x 7700 2 Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) FOR ADULT PATIENTS AT RISK OF REFEEDING SYNDROME Ward:…………... Name:……………..………………… DOB:.…. DATE:….. Sheet No:…….. Occasionally patients will be at risk of Refeeding Syndrome. They can be identified from the following list. Patients with: ONE OR MORE OF THE FOLLOWING: Little or no nutritional intake for more than 10 days Unintentional weight loss greater than 15% within the last 3-6 months Body Mass Index less than 16 Low levels of potassium, phosphate or magnesium prior to feeding TWO OR MORE OF THE FOLLOWING: Little or no nutritional intake for more than 5 days Unintentional weight loss greater than 10% within last 3-6 months Body Mass Index less than 18.5 A history of alcohol abuse or drugs including insulin, chemotherapy, antacids or diuretics Fluid Balance should be closely monitored. Feed should be delivered within the context of careful fluid balance with intravenous fluids being reduced or discontinued as required.* Thiamine - 100 mg three times daily (the first dose 30 minutes prior to starting feeding3) either orally OR crushed via feeding tube2. Vitamin B compound strong - 1 tablet three times daily orally if appropriate, DO NOT ADMINISTER VIA TUBE. AND Forceval Soluble – 1 tablet a day, dissolved in at least 50 ml water via feeding tube. 1, OR Sanatogen Gold – 1 tablet daily orally2 3 DO NOT ADMINISTER VIA TUBE. . Biochemistry should be closely monitored BEFORE STARTING (within last 24 hours) and DAILY during feeding, especially Potassium, Magnesium, Phosphate, and Corrected Calcium. If any of these are low do not increase feed rate – do inform medical staff and dietitian when available. Recommended rates are to guide but not contravene medical opinion. Recommend not to start nutritional supplement drinks (eg Fresubin Energy, Fresubin Jucy etc) at same time as starter regimen if patient at risk of Refeeding syndrome. REFER PATIENT TO DIETITIAN AS SOON AS POSSIBLE. Feeding must be increased slowly in accordance with the regimen below following thiamine administration, see above. For patients At Risk of Refeeding Syndrome or below 40 kg in weight Date/Day number Day 1 Feed Type Rate (ml/hour) 30 15 Duration (hours) 4 20 Volume (ml) 120 300 Water Fresubin Original Day 2 Water 30 4 120 Fresubin 20 20 400 Original Day 3 Water 30 4 120 Fresubin 25 20 500 Original Patient will require additional intravenous fluids* SEE INFORMATION REGARDING DAILY PATIENT MANAGEMENT WHILST FEEDING DEPARTMENTS OF NUTRITION AND DIETETICS AND CLINICAL NUTRITION Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015) Clinical Policy for the Insertion and Maintenance of Fine Bore Nasogastric Feeding Tubes in Adults: Version 10 18/12/2013 (Review date: October 2015)