21 year old male with bilateral hip pain and difficulty walking
advertisement

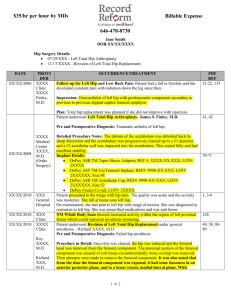
Brian Daines Rheumatology Paper 2/4/2007 Treatment avascular necrosis of the hip with Alendronate A 21 year old male presented to the Rheumatology clinic with bilateral hip pain and difficulty walking. Previously he had been treated with high-dose steroids for suspected auto-immune disease. Bilateral hip x-rays showed femoral head changes consistent with osteonecrosis of the hip. Osteonecrosis is a devastating disease that typically strikes patients in their third to fifth decade. Commonly called avascular necrosis, it literally means bone death. There are a variety of theories on the pathogenesis of osteonecrosis. Most likely it is the combined effect of metabolic factors, local factors affecting the blood supply, increased intraosseous pressure, and mechanical stresses.1 These stresses cause a decrease in blood supply to the bone. The adjacent areas become hyperemic. Demineralization causes trabecular thinning which has the potential to lead to eventual collapse. Campbells Orthopaedics refers to osteonecrosis as an “end condition” that is the result of many pathologies including alcohol abuse, gout, caisson disease, Gaucher disease, renal osteodystrophy, sickle cell anemia, systemic steroid use, and trauma.2 However, it is important to realize that most people with these risk factors do not acquire the disease and some without it do. Our patient presented with progressively worsening hip pain on ambulation. He reported that he was only able to walk several blocks before the pain forced him to rest. On physical exam, he had increased pain on bilateral internal rotation. Patients with osteonecrosis are typically asymptomatic during the early stages of disease. As the disease progresses, some may have pain with ambulation. Physical signs are generally non-specific. On exam, patients may present with decreased internal rotation and hip abduction. Our patient had bilateral sclerosis noted on his pelvis x-rays. The most common classification system was developed by Ficat and Arlet.2 Based on x-ray changes, it ranges from stage 0 with normal x-rays, no symptoms and no pathologic findings to stage 4 with joint spacing narrowing and acetabular changes, moderate to severe hip pain, and osteoarthritic pathology. Stage 1 is associated with mild hip pain and no x-ray changes. Stage 2 is associated with mild hip pain and x-ray changes range from density changes in the femoral head to flattening of the femoral head (crescent sign). Stage three is associated with mild to moderate pain and collapse of the femoral sphere. Our patient’s x-rays therefore corresponded to subgroup “A” of Stage 2, where sclerosis or cysts are noted on the x-ray with out collapse. The natural history of osteonecrosis before subchondral collapse is unknown. However, studies suggest that the rate of femoral collapse in symptomatic patients is rapid. Campbell’s Operative Orthopaedics notes that there is no effective treatment for arresting the disease process before subchondral collapse or in slowing the progression of femoral head destruction and osteoarthritis after subchondral collapse. They did, however, cite the unpredictable rate and progression of the disease.2 Surgical management of osteonecrosis is unsatisfactory. Currently, core decompression is used for treatment of Ficat stages I and IIA small central lesions in young, nonobese patients who are not taking steroids. Core decompression is thought to relieve intraosseous pressure caused by venous congestion and thereby improve vascularity and slow the progression of the disease. Vascularized fibular grafting is a relative newer technique that has achieved some good success. Urbaniak recommended vascularized fibular grafting in patients 50 years of age or younger.3 Osteostomies are used for small- or medium-sized lesions (less than 30% femoral head involvement) in young patients in whom it is optimal to delay a total hip arthroplasty. Treatment of large lesions and advanced disease is limited to resurfacing hemiarthroplasty, unipolar and bipolar hemiarthroplasty, and total joint replacement. For the most part, surgical management of osteonecrosis appears to be technically difficult with moderate success. Recently, there have been several studies supporting the use of bisphosphonates to slow progression of avascular necrosis. Bisphosphonates seem to slow bone reabsorbtion. In 2005 Agarwala reported the results of an uncontrolled study with sixty patients and one hundred hips treated with 70 mg of weekly alendronate.4 He found that treatment with alendronate decreases pain, improves function and retards progression of avascular necrosis. Also in 2005, Lai evaluated forty patients with Steinberg stage-II or III nontraumatic osteonecrosis of the femoral head and a necrotic area of >30% (class C) and randomly divided them into alendronate and control groups of twenty patients each.5 Patients in the alendronate group took 70 mg of alendronate orally per week for twentyfive weeks, while the patients in the control group did not receive this medication or a placebo. They found that alendronate appeared to prevent early collapse of the femoral head in the hips with Steinberg stage-II or IIIC nontraumatic osteonecros We decided to start our patient on alendronate 70 mg qweekly with the hopes that this would slow his avascular necrosis and even prevent collapse of his femoral head. Works Cited 1. Chang, C, Greenspan, A, Gershwin, M. Osteonecrosis: Current perspectives on pathogenesis and treatment. Semin Arthritis Rheum 1993; 23:47. 2. Canale, Terry S. Campbell's Operative Orthopaedics, 10th ed. Mosby Inc. 2003. 3. Urbaniak et al., 1995. Urbaniak JR, Coogan PG, Gunneson EB, Nunley JA: Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting: a long-term follow-up study of one hundred and three hips. J Bone Joint Surg 1995; 77A:681. 4. Agarwala, S, Jain, D, Joshi, VR, Sule, A. Efficacy of alendronate, a bisphosphonate, in the treatment of AVN of the hip. A prospective open-label study. Rheumatology (Oxford) 2005; 44:352. 5. Lai, KA, Shen, WJ, Yang, CY, et al. The use of alendronate to prevent early collapse of the femoral head in patients with nontraumatic osteonecrosis. A randomized clinical study. J Bone Joint Surg Am 2005; 87:2155.