行为及认知状况部分 - BioMed Central
advertisement

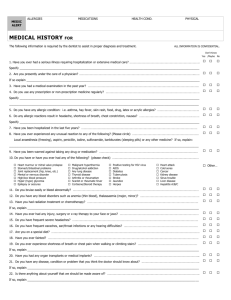
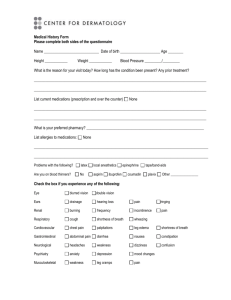
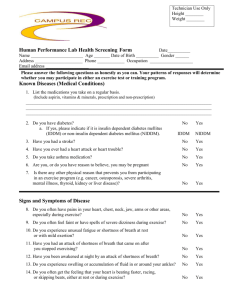
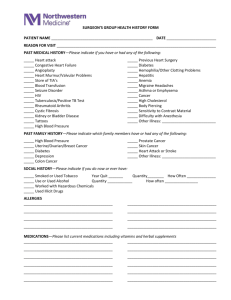
The questionnaires of the vulnerability of patients with COPD. How do you do? I am a staff of the study group of integrated intervening COPD in community. According to the informed consent signed by you, now I ask you something about your illness. After considering it, please answer me seriously. A. General characteristics 1. Address : Province Municipality County Town ; Village 2. Name: 3. Gender: (1) male (2) female 4. Nation: 5. blood type: 6.Date of birth: 7. Level of education: Illiteracy or semiliterate, elementary school, junior middle school, senior high school and technical secondary school, above junior college, unknown. 8. Marital status: Unmarried, Marriage, Divorce, Widowed, Separation, Unknown. 9.Occupation: Workers, Peasants, Herdsmen, Medical personnel, Clerks, Staff members, Cadres, Teachers, Cook, Policemen, Drivers, Businessmen, Retirees, Housework, Jobless, Students, Others 10.Average monthly household income : . Yuan. Total members in household person(s) B. Cognition for COPD 1. Have you heard of COPD? (1) heard (2) Not heard(Go to 4) (3) Not remember 2. The level of your understanding of the knowledge of COPD. (1) More systematic understanding (2) known (3) Understanding a little (4) Not known 3. Do you know the meaning of acute exacerbation of COPD? (1) More systematic understanding ( 2) Known (3)Understanding a little (4) Not known 4. You think you suffer from what disease? 1)COPD 2)Bronchitis 3)Asthma 4)Emphysema 5. The doctor had told you what disease you were suffering from? 1)COPD 2)Bronchitis3)Asthma 4)Emphysema 6. You think that your own health caused by which disease. (1) COPD (2)Bronchitis (3) Asthma (4) Emphysema 7.You think that the attack of your disease was caused by which risk factors (Maybe multi-select). (1) Got a cold (2) Tired smoking (6) Air pollution (3) Cold weather (7) Others (4) Smoking (5) Passive . 8. Do you have a family history of chronic bronchitis (Do your parents, brothers and sisters have chronic bronchitis). (1) Yes (2) No (3) Not known 9. You think the impact degree of passive smoking on your disease. (1) Very large (2) Larger (3) Common (4) Smaller 10. Do you think the view that “The patient with chronic obstructive pulmonary disease was frail? In order to reduce physical exertion, he should be resting.” is right? (1) Right (2) Incorrect (3) Not known 11. You think to participate in appropriate physical exercise for your disease. (1) Very useful (2) Useful (3) Little effect (4) Not useful (5) Not known 12. You think the role of controlling chronic bronchitis for preventing emphysema and Cor pulmonale. (1) Very large (2) Larger (3) Common (4) No role (5) Not known 13. Your attitude towards own disease. (1) Very concerned about concerned about (2) More concerned about (3) Ordinary (4) Don’t matter 14. For the slow development of your disease, whether you took the relevant measures ( Such as the prevention of cold, vaccination). (1) Yes ( 2) No 15. For the slow development of your disease, whether you are willing to change or control your behaviors (Such as quitting smoking, physical exercise). (1)Very willing (2)Willing (3)Not willing (4)Don’t matter C. Behaviors 1. Do you have smoking? (1) No (Go to 6) (2) Current smoking (3) Past smoking 2. How many years have you smoked year(s) 3. The average number of your daily smoking branch(es) 4. How long the time was from your last smoking to now month(s).(Not suit (2)) 5. The mainly reason of your quitting smoking. (Not suit (2)) (1) Sick limits (2) Economic difficulties (5) Public education (3) Family against (4) Environmental (6) Others 6. Last year, did you often inhale the smoke exhaled by smokers (i.e. passive smoking), and more than 15 minutes / day. (1) Almost every day (2) More than three days per week weekly (4) Less than one day per week (5) (3) Average of 1-3 days No 7. How often did you cook? (1) No(Go to 9) (2) Less than one day per week weekly (4) More than three days per week 8. How many years have you cooked (3) Average of 1-3 days (5) Almost every day year(s) 9. Have you been in contact with dust or soot in the work in the past. (1) Yes (2) No 10. You think you lived in air pollution of your ambient. (1) Very severe (2) More severe (3) Common severe (4) Less severe 11. Did you participate in physical exercise such as walking/ exercise/ dance/ play/ swimming/ running/ cycling/ Tai chi Etc.( Over 30 minutes /time/day) (1) Every day(Once per day) (2) Regular( More than three days per week) 3)) Irregular(Average of 1-3 days weekly) (4) Occasionally (Less than one day per week (5) No 12. Not to participate in physical exercise,what is the main reason. (1) No time (2) Tired for work conditions (3) Do not like sports (4) No place and (5) Severe disease (6) Others 13. Did you participate in the rehabilitation exercises (such as breathing exercises, hardy training, etc.). (1) No (2) Less than 1 time per week More than 3 times per week (3) Average of 1-3 times weekly (4) (5) Almost once a day 14. Why you did not participate in the rehabilitation exercises? (1) No time (2) Tired for work (3) Not willing (4) Not do (5) Severe disease (6) Others 15. Did you fear the onset of your disease, or because of your cough, sputum symptoms that other people dislike, so you do not want to go to public places(such as weddings, funerals , listening to the story, theatre). (1) Yes 2)No (3) Don’t matter D. Quality of life Ⅰ.Self-assessed physical strength (1) The same as common people. (2) Shortness of breath with common work (3) Shortness of breath with climbing stairs (40 Shortness of breath with light activities. (5) Shortness of breath when walking for one hundred steps. Note: (1) ~(5) were 0 to 4 points. Ⅱ.Activities of Daily Living (10 items) 1. Dressing, washing , brush teeth, combing, shaving ,haircut, etc. (1)No shortness of breath, finishing by oneself(2)A little shortness of breath, and can still finishing by oneself(3)More shortness of breath, need other people to help complete(4)Obvious shortness of breath ,totally dependent on someone else help complete 2. Bath (1)Taking a bath alone(2)Alone in bathing, felt shortness of breath(3)Because of shortness of breath, need someone else to help with bathing at home (4) Because of shortness of breath, need someone else to help complete absolutely 3. Cook, housekeeping, laundry, sweeping, wiping tables, washing dishes and other. (1)No shortness of breath(2)A little shortness of breath(3)More shortness of breath, and less to do. (4)Obviously gasp, and not to do. 4. Outdoor walking (1) No shortness of breath,can walk more than 2000 meters away alone.(2)A little shortness of breath, can walk 1 ~ 2 km away alone.(3)More shortness of breath, can walk less than 1km away alone.(4)obviously gasp, can not walk over one hundred steps. 5. Physical strength (Carry goods) (1)No shortness of breath,can carry more than 10kg goods walking.(2)A little shortness of breath, can carry 5 ~ 10kg goods walking.(3)More shortness of breath, can carry 2 ~ 5kg goods walking.(4)Obviously gasp, can not nearly carry goods to walk . 6. Upstairs (1)Without a break, go upstairs 3rd floor or above.(2)Without a break, go upstairs 2 to 3 floor(3)Having a beak, go upstairs 2nd floor(4)Obviously gasp, can not go upstairs alone. 7. Appetite (1)Good appetite, have taste to eat(2)Common appetite(3)Bad appetite(4) Do not want to diet. 8. Sleeping (1)Sleep well(2)Because of shortness of breath and cough, poor sleep(3)Because of shortness of breath and cough, wore sleep(4)Because of cough and dyspnea, can not sleep all night or can not be supine. 9. Taking medicine (1)Taking medicine consciously according to prescribed medication (2) Occasionally need to be reminded taking drug (3)Often need to be reminded taking drug(4)After reminding by someone else, often forgotten to take drug or refused to take medicine. 10. Entertainment(reading newspaper, watching TV, listening to the radio, playing chess, playing cards, etc.). (1)Often(More than 1 h per day, over 4d per week); (2)Sometimes(0.5h per day, over 3d per week)(3)Seldom(10 ~ 20 min per day,1~3d per week.);(4)No. Ⅲ.Social activities (4 items) 1. With neighbors , colleagues, relatives and friends and other. (1)Often(Over 4 times monthly) (2)Many times(2 ~ 3 times monthly)(3) Seldom (1 time monthly)(4)No. 2. Friends (1)Liking to make friends and keep in close contact.(2)Having a friend, to maintain general contact.(3)Little contact with friends.(4)No friends contact. 3. Social activities (neighborhood activities , public activities, social part-time, etc.). (1)Participating all activities.(2)Regular participation (1 time or above per month) (3)Sometimes participating(Less than 1 time per month)(4)No participating 4. Relationship with family (1)Family members concern each other, mutual support, and often heart-to-heart talk.(2)Can still communicate and support each other(1 time or above per week) (3)Small of mutual supporting and exchange(Less than 1 time per week)(4)Not mutually exchange. Ⅳ. Psychological symptoms of depression(5 items) 1. Depressed for sick (1)No.(2)Seldom(1 time per week) (3)More(2 ~ 3 times per week);(4) Often (4 times or above per week) 2. Feeling worthless (1)No.(2)Seldom(1 time per week) (3)More(2 ~ 3 times per week);(4) Often (4 times or above per week) 3.Feeling happy and satisfaction to life (1)Very satisfaction (2)Satisfaction(3)Fairly Satisfied(4)Dissatisfied 4. Worrying about COPD affecting self-health (1)No.(2)Seldom worrying(1 time per week) (3)More worrying (2 ~ 3 times per week);(4)Often worrying (4 times or above per week) 5. Feel lonely (1)No.(2)Seldom(1 time per week) (3)More(2 ~ 3 times per week);(4) Often (4 times or above per week) Ⅴ. Psychological symptoms of anxiety (5 items) 1. Feeling easily fatigued (1)No.(2)Seldom(1 time per week) (3)More(2 ~ 3 times per week) (4) Often (4 times or above per week) 2. Feeling agitation (1)No.(2)Seldom (1 time per week) (3)More(2 ~ 3 times per week);(4) Often (4 times or above per week) 3. Feeling impatient (Lost his temper for no reason) (1)No.(2)Seldom (1 time per week) (3)More(2 ~ 3 times per week);(4) Often (4 times or above per week) 4. Feeling fear (1)No.(2)Seldom(1 time per week) (3)More(2 ~ 3 times per week);(4) Often (4 times or above per week) 5. Having nightmares (1)No.(2)Seldom(1 time per week) (3)More(2 ~ 3 times per week);(4) Often (4 times or above per week) Note: ExceptⅠ, : (1) ~(4) of Ⅱ~Ⅴwere 1 to 4 points. The higher the score, the worse the quality of life. “0”score mean that patients felt extremely well, “1~20”scores mean very well, “21~40”scores mean 4 well, “41~60”scores mean normal, “61~”scores mean bad. E. Disease Management 1. Whether the local hold such as tobacco control, reasonable diet and other health education and publicity. (1) yes (2) No (3) Not remember 2. Whether you received, such as tobacco control, reasonable diet and other health education and publicity. (1) yes (2) No (3) Not remember 3. Are you willing to accept reasonable treatment? (1) Willing (2) Unwilling (3)Don’t matter 4. The reason that you do not want to accept reasonable treatment. (1)The disease was not severe (2)Buy medicine by himself. (3)Financial hardship (4)More distant road. (5)Not convenient for hospital services(such as waiting too long.) indicating (6)No time (7)Not curable (8) other(Please ) 5. Which of the following methods you had used for treatment of disease. (1)Inhalation or aerosol agents. (2) Oxygen therapy (3)Pulmonary rehabilitation (4) Surgery (5) No mentioned above.(Go to 7) 6. When you treated your COPD with using inhalation or aerosol agents, oxygen therapy, pulmonary rehabilitation, do you use its according to the doctor orders? (1)yes (2)no 7. The most drugs you used were at stable stage. (1)Bronchodilators(such as aminophylline) 2)Antiinflammatory drugs(Such as corticosteroids) 3)Antibiotics 4) Other (Please indicating 8. The most drugs you used were at acute exacerbation. ) (1)Bronchodilators(such as aminophylline) (2)Antiinflammatory drugs(Such as corticosteroids) (3)Antibiotics (4) Other (Please indicating: ) 9. In daily seeing doctors, which level medical institutions you often go to? (1)County or above. (2)Health Centers (3)Village health clinic (4)Private clinic. 10. When hospitalization, you often chose which level medical institutions (1)Province (2)Municipal level (3)county (4)Health Centers. F. Burden of disease 1. In last year, how many days you could not work due to COPD Days 2. In last year, how many days your family members could not work for accompany you because you got ill. Days 3. In last year, how many traveling expenses you took for going to see doctors Yuan. 4. In last year, how many traveling expenses your family members took for accompanying you to see doctors Yuan. 5. In last year, how many care expenses you took for nursing your disease Yuan. 6. In last year, how many cash you took for special purchase of nutritious food Yuan. 7. In last year, the cost of hospitalization was 8. In last year, the cost of buying drugs was Yuan. Yuan in outpatient (Including pharmacies, private clinics). 9. In last year, the cost of checkup was Yuan for you got COPD. 10. In last year, your monthly net income Yuan. Above 10 items, the investigators should look patients’ records and invoices related to medical treatment, while inquiring about patients. The investigator Name: Year Patients coordinating (1) well month (2)common day. (3) bad