Achilles Tendon Rupture and Repair
advertisement
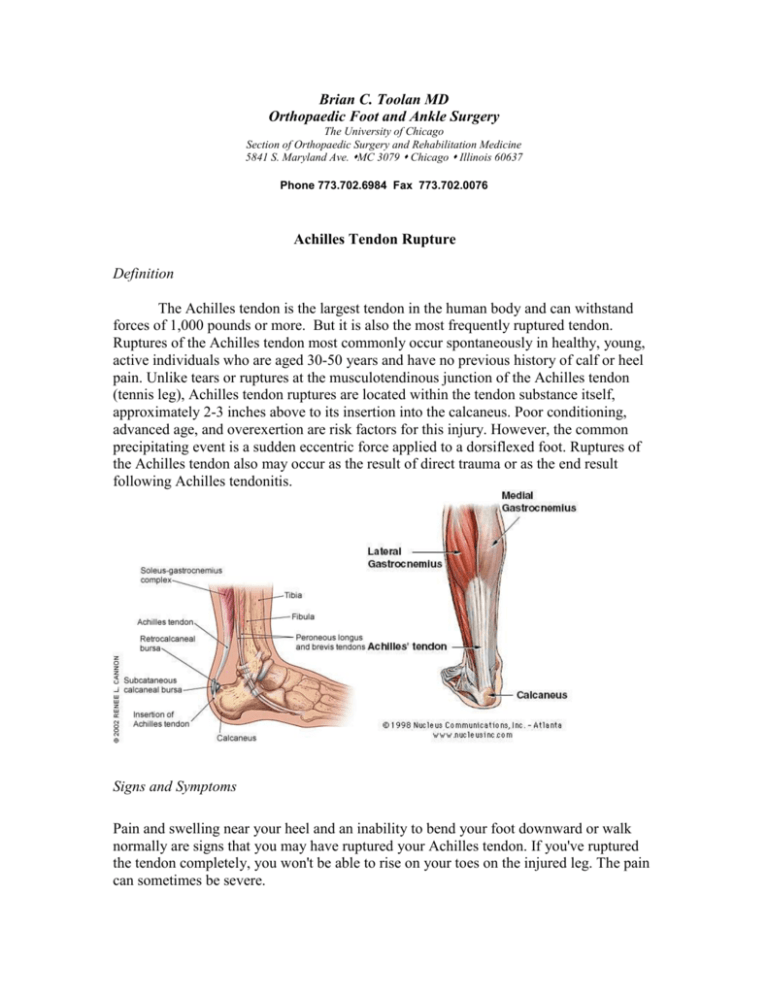
Brian C. Toolan MD Orthopaedic Foot and Ankle Surgery The University of Chicago Section of Orthopaedic Surgery and Rehabilitation Medicine 5841 S. Maryland Ave. MC 3079 Chicago Illinois 60637 Phone 773.702.6984 Fax 773.702.0076 Achilles Tendon Rupture Definition The Achilles tendon is the largest tendon in the human body and can withstand forces of 1,000 pounds or more. But it is also the most frequently ruptured tendon. Ruptures of the Achilles tendon most commonly occur spontaneously in healthy, young, active individuals who are aged 30-50 years and have no previous history of calf or heel pain. Unlike tears or ruptures at the musculotendinous junction of the Achilles tendon (tennis leg), Achilles tendon ruptures are located within the tendon substance itself, approximately 2-3 inches above to its insertion into the calcaneus. Poor conditioning, advanced age, and overexertion are risk factors for this injury. However, the common precipitating event is a sudden eccentric force applied to a dorsiflexed foot. Ruptures of the Achilles tendon also may occur as the result of direct trauma or as the end result following Achilles tendonitis. Signs and Symptoms Pain and swelling near your heel and an inability to bend your foot downward or walk normally are signs that you may have ruptured your Achilles tendon. If you've ruptured the tendon completely, you won't be able to rise on your toes on the injured leg. The pain can sometimes be severe. Often people also report hearing a popping or snapping sound when the injury occurs. It’s not uncommon that people think they got hit in the back of their leg with a ball or racket. With a partial rupture, you may still be able to move your foot, and you may experience only minor pain and swelling. Diagnosis To diagnose Achilles tendon problems, your doctor will likely ask questions about your physical activities and perform an examination of your feet, ankles and legs. If it's clear that your Achilles tendon is ruptured, you may be scheduled for surgery. If there's a question about a partial rupture of your Achilles tendon, your doctor may order a magnetic resonance imaging (MRI) scan, a painless procedure that uses magnetic fields to create a computer image of the soft tissues of your body. Treatment options Treatment for Achilles tendon ruptures can be non-surgical or surgical. Surgical repair of a ruptured Achilles tendon is usually preferable, especially if you're healthy and want to resume your active lifestyle. Surgery is generally very effective, and your risk of complications is typically quite low. Non-surgical treatment. This approach typically involves wearing a cast, which allows the ends of your torn tendon to reattach themselves on their own. This method can be effective, and it avoids the risks, such as infection, associated with surgery. However, the likelihood of re-rupture is higher with a non-surgical approach, and recovery can take longer. The likelihood of re-rupture is approximately 17%. The treatment consists of casting first, in a long leg cast for several weeks, followed by a short leg cast for a total of 6-10 weeks of casting. As a result of the long period of immobilization, therapy to recondition weakened muscles and stiff joints take longer than if you have surgery. Surgery. The usual treatment for a complete rupture of an Achilles tendon is surgery. The procedure generally involves making a gently curved incision in the back of your lower leg and repairing the torn tendon. There are the risks of having surgery which include infection, wound healing problems, and risks associated with having anesthesia. The re-rupture rate after having surgery is approximately 3%. The recovery period is shorter because you begin therapy 1-2 weeks after surgery, to prevent joint stiffness and loss of muscle mass. The surgery takes approximately 90 minutes and can be performed on an outpatient basis, meaning you can go home the same day. You will have an incision on the back of your leg in the shape of an “S”. The tendon edges will be brought close together and sewn tightly with very strong suture material that is not absorbable. Post operative management There are many factors that affect your healing time. The most important is to be patient, YOUR FOOT MAY NOT TOUCH THE GROUND until your surgeon or therapist tell you that it’s o.k. This means you must use assistive devices, like crutches, a walker or roll-a-bout to get around. We do not want you to use a wheel chair because your entire body gets weak and it will lengthen your recovery time. Another factor is smoking. YOU MUST NOT SMOKE while you are recovering. It will delay your healing. This includes second hand smoke. Smoking decreases the blood flow to your surgical site. This means that oxygen and nutrients essential for healing are decreased and will lengthen your recovery. It is also possible that the tendon will not heal, or your wound will not heal and the skin dies. In the event that you do not heal, you will require additional surgery to get the tendon to heal. Another factor is swelling. This is something that can be avoided by elevating your foot above heart level. Swelling can also be controlled with ice therapy. Icing for 20-30 minutes in intervals will significantly decrease your swelling. The best thing to use for ice therapy is crushed ice or frozen vegetables because they can conform around your cast or splint. By eliminating swelling, you can reduce or eliminate your pain. Elevate and ice your foot 20-30 minutes for pain control first. If elevation and ice do not adequately control the pain, you may then take your pain medication. It is important to only take your pain medication when you need it. Just because the prescription says you may take it every 4-6 hours, does not mean that you have to. Pain management The first 2-3 days after surgery will be the most uncomfortable. You will have both swelling and pain. During this time it is very important that you decrease your activity level, elevate the operated foot above heart level, and use ice therapy. You will notice when you put your foot down, it will begin to swell immediately and you will experience a throbbing pain, your toes my turn a dark bluish-purple. To treat this, elevate and ice and it should go away. Over the next two weeks, you will be able to increase the amount of time you can have your leg down. It is still important to keep your leg elevated as much as possible. After surgery, you will be given a prescription for pain medication. You should not need any refills. If you are out of pain medication, perhaps you are being too active and need to decrease your activity level. Before taking a pain pill, we suggest that you try elevation and ice for 20-30 minutes and if this fails to resolve you pain, you should take your pain medication. Casting Immediately after surgery, you will be placed into a splint. This is to help protect the surgical repair and allow for skin healing. It is like a cast, made of plaster and is open in the front to accommodate for swelling. At one week after surgery you will return and get a CAM Boot, which is a removal brace much like a ski boot. This is so that you can take it off to start your physical therapy exercises. At two weeks after surgery you will return and have your sutures removed. You may desire to take some of you pain medication before having your sutures removed. Physical Therapy The goals of rehabilitation are wound healing, range of motion with emphasis on neutral dorsiflexion, regaining muscle strength, normalize gain and return to previous functional level. After the first week, you will be placed into a CAM Boot so that you can remove it to start physical therapy. For the first 4 weeks, you will not be allowed to walk on your surgical side. All exercises are done within the limits of pain. You will work on range of motion to neutral dorsiflexion (bending your ankle toward your head). We do not want you to move your ankle past neutral, so that you do not stretch out the repair and have difficulty with strength and gait. Once you have achieved neutral dorsiflexion, you may begin strengthening in plantarflexion (bending your ankle down toward your toes) only and your surgeon may allow partial weight-bearing. You may do non-weight bearing strengthening in high repetition with low resistance, like riding a stationary bike. You may swim as soon as the wound is healed. It is important to do scar massage once the sutures are removed and everything is healed. They will also use modalities like heat, ice and ultrasound to help control you swelling and pain. The next 6 weeks will include increasing your range of motion past neutral and strengthening in all planes of motion. You will increase weight bearing directed by your therapist. First you will be off the crutches and then out of the CAM Boot. You will begin working on normalizing your gait. At 3-6 months you can begin jumping and doing more polymetric exercises. You can begin preparing to return to your sports activities. You can begin running if you gait is normal and you can do 10 single toes raises. It is important to remember that you may still have good and bad days after your treatment is completed. It can take six to nine months to return to your normal level of activity. Although there will be some bad days, over time you will get progressively better. We will see you back at the six month anniversary of your surgery. At six months, the foot should “feel normal”, range of motion is greatly improved, swelling is decreased and there are no problems with the foot with normal daily activities. At any time during your treatment, you may call the office at (773) 702-6984 with any questions or concerns, or call the nurse at 773-834-0355.