Appendix b independent prescribing conversion submission
advertisement

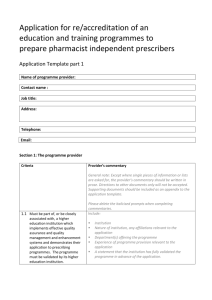
Appendix B Accreditation of an independent prescribing programme to train supplementary prescribers as independent prescribers (conversion) Submission template (parts 1 & 2) This template should be used to demonstrate how the provider meets the GPhC’s accreditation criteria for education and training programmes to train pharmacist supplementary prescribers as independent prescribers (conversion programme) The accreditation submission document should be a single document which includes: This template, completed in full, to include: - A narrative explaining how each criterion is met. The narrative must be written in prose, clearly explaining how the criteria will be met. Reference to links, file names, or module titles on their own are not acceptable. - Full reference to the documents you are providing as evidence. Any other pertinent information. You should provide documentary evidence to support the information that you have provided within the template. Following review of your submission document and associated evidence you may be required to submit additional items of evidence, if this is necessary you will be notified in advance of your accreditation event. The process for reaccreditation of an independent prescribing programme (full or conversion) will follow the same format as described for accreditation. The submission documentation must include, additionally, an introduction section which includes the following: An overview of how the programme has developed since initial accreditation, including a summary of any major changes Information on the number of cohorts of the programme that have been delivered since the last event, including the number of pharmacists per cohort. A summary of the response to any conditions and recommendations that were made by the accreditation team at the previous event. Where a provider opted not to action a recommendation, an explanation of the rationale for this decision should be provided. Please ensure that you refer to the guidance within this template as failure to provide your submission in the correct format, with the required level of detail and clarity, could lead to your accreditation event being cancelled or postponed. Information on how to submit your documentation can be found on the last page of this document. If you have any questions regarding your accreditation submission please contact the GPhC’s Quality Assurance (Education) team on 0203 713 7973 or 7978 Independent prescribing accreditation submission template, 2015-2016 Name of University/Institution: Name of School or Department: Contact name: Job title: Address: Telephone: Mobile: Email: Independent prescribing conversion programme - accreditation submission template, 2015-2016 2 General notes regarding completion of the template Except where single pieces of information or lists are asked for, your commentary must be written in prose. Directions to other documents only will not be accepted. Hyperlinks may be used within your commentary to signpost to evidence but please check that the links are not broken and that external access is permitted. Please ensure that all documentary evidence provided is referred to within your commentary. Referencing additional materials For ease of reference, all supporting material should be numbered and named appropriately (for example, Appendix One – Student Handbook, Appendix Two – Programme Specification) Please ensure the same document name is used throughout the submission and in the appendices. When referencing supporting material within the submission, please indicate the document clearly (for example, in bold) and use the full name and appendix number throughout. For reaccreditation only Provider’s commentary General note: Except where single pieces of information or lists are asked for, the provider’s commentary should be written in prose. Directions to other documents only will not be accepted. Supporting documents should be included as an appendix to the application template. (Please delete the guidance notes when completing commentaries.) Introduction for reaccreditation Include: • An overview of how the programme has developed since initial accreditation, including a summary of any major changes • Information on the number of cohorts of the programme that have been delivered since the last event, including the number of pharmacists per cohort. • A summary of the response to any conditions and recommendations that were made by the accreditation team at the previous event. Where a provider opted not to action a recommendation, an explanation of the rationale for this decision should be provided. Independent prescribing conversion programme - accreditation submission template, 2015-2016 3 Submission template part 1: meeting the accreditation criteria Section 1: The programme provider Criteria Provider’s commentary General note: Except where single pieces of information or lists are asked for, the provider’s commentary should be written in prose. Directions to other documents only will not be accepted. Supporting documents should be included as an appendix to the application template. (Please delete the guidance notes when completing commentaries.) 1.1 Must be recognised by the General Pharmaceutical Council (GPhC) or the Pharmaceutical Society of Northern Ireland (PSNI) as a provider of an accredited independent prescribing programme or as a previous provider of an accredited supplementary prescribing programme. 1.2 Must be part of, or be closely associated with, a higher education institution which implements effective quality assurance and quality management and enhancement systems and demonstrates their application to prescribing programmes. The programme must be validated by its higher education institution. State which prescribing programmes your institution is/has been accredited to offer including relevant dates. Include: Institution Nature of institution, any affiliations relevant to the application Department(s) offering the programme Experience of programme provision relevant to the application A statement that the institution has fully validated the programme in advance of the application. Details of quality assurance procedures for example student feedback and input from external examiner Independent prescribing conversion programme - accreditation submission template, 2015-2016 4 1.3 Must have adequate physical, staff (academic and administrative) and financial resources to deliver the programme including facilities to teach clinical examination skills. 1.4 Must have identified staff with Include: Accommodation allocated to/used by the programme (include explicit mention of facilities for teaching clinical examination skills) Equipment Support service Planned student numbers (and maximum student numbers (including ratio of pharmacists to other health professionals, where applicable) How the programme will be funded Include: Details of each member of staff associated with the programme (include names/titles/qualifications/professional affiliations/contribution(s) to the programme/employment status (institutional employee/external) Calculate WTE/FTE assigned to programme Provide Curricula Vitae for each member of staff associated with the programme (summary format is acceptable) appropriate background and experience to teach the programme, ideally including practising pharmacists with teaching experience and staff with clinical and diagnostic skills. 1.5 Must have an identified practising Include evidence of how this person(s): pharmacist with appropriate has/have contributed to the design of the programme and will contribute to its delivery. background and expertise who will contribute to the design and delivery of the programme. The identified pharmacist must be registered with the General Pharmaceutical Council (GPhC), and where possible should be a pharmacist independent prescriber. Section 2: Pre-requisites for entry Criteria Provider’s commentary 2.1 Entrants must be a registered Include a description of how this will be checked. pharmacist with the GPhC or the Pharmaceutical Society of Northern Ireland (PSNI). As evidence of meeting the criteria in section 2 the provider should include documentation to demonstrate how they ensure that applicants are suitable for entry to the programme (e.g. copy of the programme application form). Independent prescribing conversion programme - accreditation submission template, 2015-2016 5 2.2 Entrants must currently be annotated as a supplementary prescriber and able to provide evidence of prescribing experience within the UK that is no longer than 2 years’ old. 2.3 Entrants must provide a statement of support from a medical practitioner that confirms their competence as a supplementary prescriber. 2.4 The provider must ensure that the DMP, identified by the pharmacist, has training and experience appropriate to their role. This may be demonstrated by adherence to the Department of Health Guidance (2001). The DMP must have agreed to provide supervision, support and shadowing opportunities for the student, and be familiar with the GPhC’s requirements of the programme and the need to achieve the learning outcomes. 2.5 Entrants should demonstrate how they reflect on their own performance and take responsibility for own CPD. Include a description of how this will be established and agreed Explain how: training will be provided experience will be established and validated the DMP’s service level is agreed DMPs become familiar with the programme the DMP is made aware of the GPhC requirements and learning outcomes Explain how this will be demonstrated on application and its role in the programme. Section 3: The programme Independent prescribing conversion programme - accreditation submission template, 2015-2016 6 Criteria Provider’s commentary 3.1 Must be taught at least at Include information on how the programme was benchmarked against the relevant academic level in the FHEQ (2008). bachelor’s degree level (FHEQ (2008), level 6 ) and reflect the fact that since June 2002, pharmacists have graduated and practise at master’s degree level (FHEQ (2008), level 7). 3.2 Must achieve the learning outcomes identified in the curriculum for an independent prescribing conversion programme. 3.3 Must include teaching, learning and support strategies which allow pharmacists to build on their background knowledge and experience and acquire competence in prescribing. 3.4 Must provide opportunities for pharmacists to demonstrate how they will apply their learning to the conditions for which they will be prescribing. 3.5 Must contain learning activities equivalent to 2 days including a minimum of one day of face to face learning activities. The programme will be expected to contain a range of appropriate delivery methods Note: The learning outcomes should be interpreted at the correct academic level for the programme (either level 6, level 7 or both). Level 6 and 7 learning outcomes should be differentiated and it should be made clear how assessments test the correct academic levels). Complete submission template part 2. Describe: The programme’s teaching and learning strategy Overall learning time (specify the balance between, taught, directed, self directed and private study) How students’ background knowledge and experience will be established How that knowledge and experience will be developed to acquire competence in prescribing If the programme relies on web-based learning materials the provider should arrange short-term access so that the panel may review the materials before the accreditation event. Describe how each student’s learning will be contextualised in their chosen prescribing field and how they will demonstrate clinical competence. Describe and quantify the learning activities equivalent to 2 days and confirm the period of delivery. Provide the proposed timetable for pharmacists undertaking the programme. Independent prescribing conversion programme - accreditation submission template, 2015-2016 7 3.6 Must have a clear policy on attendance and participation and the obligations of pharmacists who miss part of the programme. Pharmacists must attend all scheduled teaching and learning sessions that provide instruction on clinical examination and diagnosis. 3.7 Candidates will be subject to the full assessment process for the conversion programme. State the programme policy on attendance and the requirements on pharmacists who miss parts of the programme. Confirm that pharmacists must attend all clinical sessions and that they will not pass the programme if they do not. Include how students are made aware of the policy. State the programme policy on attendance and the requirements on pharmacists who miss parts of the programme. Confirm that pharmacists must attend all clinical sessions and that they will not pass the programme if they do not. Section 4: Learning in Practice Criteria Provider’s commentary 4.1 The provider must support the Include: DMP with clear and practical guidance on helping the pharmacist successfully to complete the period of learning in practice including arrangements for quality assurance of summative assessments. The roles of the programme provider and the DMP for teaching the skills for clinical assessment of patients must be clearly set out. 4.2 The provider must support the DMP with clear and practical guidance on their role in the assessment of the student. guidance issued to DMPs relating to successfully completing the period of learning in practice arrangements for the quality assurance of summative assessments of learning in practice the roles of the programme provider and DMP for teaching clinical assessment skills Describe how DMPs are supported in the assessment students, providing a copy of any relevant documentation. Independent prescribing conversion programme - accreditation submission template, 2015-2016 8 4.3 The provider must obtain formal evidence and confirmation from the DMP using the specified wording; “the pharmacist has satisfactorily completed at least 2x7.5h days supervised practice”. 4.4 The provider must obtain a professional declaration from the DMP using the specified wording; “In my opinion as the DMP, the skills demonstrated in practice confirm the pharmacist as being suitable for annotation as an Independent Prescriber”’ 4.5 Failure in the period of learning in practice cannot be compensated by performance in other assessments. Describe the nature of the formal evidence from DMPs that pharmacist students have completed at least 2x7.5h days supervised practice and how the relevant wording will be obtained. Describe how the relevant wording will be obtained. Confirm this is the case and describe where and how students will be made aware of this. Section 5: Assessment The programme provider should ensure that assessment strategies meet the requirements of the curriculum particularly: Criteria Provider’s commentary 5.1 Evidence from a range of Describe what range of assessments will be used and how that range will test learning outcomes securely. assessments that the student has achieved the intended learning outcomes for the conversion programme. 5.2 The programme is freestanding and will be assessed separately Confirm this and explain how relevant assessments will be run separately if parts of the programme are shared. Independent prescribing conversion programme - accreditation submission template, 2015-2016 9 from any other programmes or programme. 5.3 The assessment scheme should demonstrate that the criteria for pass/fail and any arrangements for compensation between elements of assessment, together with the regulations for resit assessments and submissions, are consistent with safe and effective prescribing and the achievement of all learning outcomes. 5.4 In any assessment, a failure to identify a serious problem or an answer which would cause the patient harm should result in overall failure of the programme. Describe: Compensation arrangements (see 4.5) Resit regulations (which must be demonstrably consistent with safe and effective prescribing) Mechanisms in place to ensure assessments are valid, reliable and robust Provide a copy of the assessment marking criteria and explain how this is consistent with safe and effective practice. Confirm this and identify mechanisms for identifying such problems/answers. Explain how students are made aware of this. Section 6: Details of Award Criteria Provider’s commentary 6.1 The provider should award Confirm that this will be the case and provide a sample certificate successful candidates a ‘Practice Certificate in Independent Prescribing’ confirming that the candidate has successfully completed the programme and the period of learning in practice. 6.2 The provider should send a certified copy of the pass list to the Registrar of the GPhC, via the Applications Team, containing the Describe the mechanism for doing this. Include: How the pass list will be certified. How the pass list will be sent to the General Pharmaceutical Council. The name and job title of individual responsible for submitting pass lists to the GPhC Independent prescribing conversion programme - accreditation submission template, 2015-2016 10 names and registration numbers of the pharmacists who have successfully completed the programme and confirming that they are eligible for annotation on the GPhC Register as independent prescribers. Independent prescribing conversion programme - accreditation submission template, 2015-2016 11 Submission template part 2: Mapping of independent prescribing learning outcomes to programme learning outcomes and assessments Level of Study: (eg level 6 / level 7) Note: If the programme is offered at both bachelor’s degree level (FHEQ level 6) and master’s level (FHEQ level 7) please complete a separate mapping table for each including a list of the appropriate learning outcomes for that level. General Pharmaceutical Council (GPhC) Learning Outcomes Following qualification, Pharmacist Independent Prescribing will be able to: Programme Learning Outcomes Assessments Translate the GPhC’s learning outcomes into programme learning outcomes at the relevant FHEQ level (6, 7 or both) Describe how each learning outcome will be assessed. Describe the purpose of each component of assessment, its length and its weighting. 1. Understand the responsibility that the role of independent prescriber entails, be aware of their own limitations and work within the limits of their professional competence – knowing when and how to refer / consult / seek guidance from another member of the health care team. 2. Describe the pathophysiology of the condition being treated and recognise the signs and symptoms of illness, take an accurate history and carry out a relevant clinical assessment where necessary. 3. Use common diagnostic aids e.g. stethoscope, sphygmomanometer 4. Able to use diagnostic aids relevant to the condition(s) for which the pharmacist intends to prescribe, including monitoring response to therapy. 5. Apply clinical assessment skills to: inform a working diagnosis Independent prescribing conversion programme - accreditation submission template, 2015-2016 12 formulate a treatment plan for the prescribing of one or more medicines, if appropriate carry out a checking process to ensure patient safety. monitor response to therapy, review the working differential diagnosis and modify treatment or refer consult/seek guidance as appropriate 6. Demonstrate an understanding of the legal, ethical and professional framework for accountability and responsibility in relation to prescribing. Assessment Summary Assessment Method Overall percentage contribution to the assessment of the programme (Expand table as necessary) Total 100% Independent prescribing conversion programme - accreditation submission template, 2015-2016 13 Documentary evidence List below the documentary evidence that you are providing Note: You do not need to duplicate evidence - you may find that you need to refer to one piece of documentary evidence multiple times across more than one section. Please give each piece of evidence a clear and meaningful title. Use the same title when referring to the evidence within your commentary. Each item listed should be referred to within your commentary. Expand table as necessary Independent prescribing conversion programme - accreditation submission template, 2015-2016 14 Submitting your accreditation documentation to the GPhC You must send the following by post: 4 Hard copies of your submission document Each copy should be bound or stapled (No box files, ring binders or lever arch files). 4 USB memory sticks each containing: - A .PDF version of your submission document - A .PDF version of each item of documentary evidence Quality Assurance (Education) Team General Pharmaceutical Council 25 Canada Square London E14 5LQ and the following by email: A Word and a .PDF version of your completed submission template education@pharmacyregulation.org Please ensure that the hard copies and electronic copies arrive with the GPhC’s Quality Assurance (Education) Team on, or before, the submission deadline. The deadline for submission documentation is normally six weeks in advance of the accreditation event (four weeks for reaccreditation); however, you will be notified of your exact deadline date once the date of your accreditation event is agreed. Independent prescribing conversion programme - accreditation submission template, 2015-2016 15